Abstract
The aim of this study was to evaluate the validity of sleeping hours of young children as reported by their parents. The subjects were 21 healthy children aged 3 to 4 years. They were asked to attach a small instrument for calculating sleeping hours objectively, over 3 consecutive nights. Parents reported the sleeping hours of their children during the study periods. The mean values were used in the analysis. Pearson’s correlation coefficients and paired t-tests were used to evaluate the correlations and differences between the reported and objectively measured sleeping hours. The correlation coefficient and difference between the reported and assumed (objective sleeping hours representing the difference between times for falling asleep and waking) sleeping hours were 0.90 (p<0.001) and 0.79 hours (95% confidence interval: 0.59-0.99), respectively. The correlation coefficient and difference between the reported and actual (the assumed, sleeping hours minus the sum of epochs being scored as awake during the assumed sleep) sleeping hours were 0.90 (p<0.001) and 0.92 hours (0.73-1.10), respectively. Although parents tended to overestimate the sleeping hours of their children, the correlation between the reported and objective sleeping hours is high, which indicates that reported sleeping hours could be used in a survey that requires data on relative differences in sleeping hours amongst a given population.
Keywords: validity, sleep, questionnaire, children, parents, Actiwatch®
INTRODUCTION
The importance of sleeping habits in young children has been increasingly recognized1-5). In addition to the well-known association between sleeping habits and psychiatric problems1-3), several epidemiological studies have recently mentioned the relationship between short sleeping hours and the development of somatic problems such as child obesity4,5).
Many previous epidemiological studies in children have widely used self-reported or parent-reported sleeping habits1-7). However, the validity of the sleeping habits of young children as reported by their parents has not been established. The accuracy of sleeping habits, particularly of young children as reported by their parents, may be unreliable for several reasons. Firstly, sleeping habits dramatically change in preschool years7,8). While typical infantile sleep is characterized by frequent intermittent short sleeps, amounting to 12 hours sleep or more per day, the impact of aging on sleeping habits is characterized by a sizable long sleep and shortening of sleeping hours7,8). Secondly, because parents may tend to report periods between times for going to bed and rising rather than times for falling asleep and waking, sleeping hours as reported by parents may be longer than the accurate sleeping hours of their children as evaluated by electroencephalogram (EEG). Thirdly, different children may have a different quality of sleep9,10), which may result in the misclassification of sleeping hours. For example, the sleeping hours of children with sleeping problems may be characterized by fragmented short sleeps and intermittent waking during the night9,10). Then actual sleeping hours may be much shorter than the period between bedtime and rising time. In considering the detailed background biological mechanisms for the above-mentioned psychiatric and somatic problems, changes in hormonal secretion and autonomic nerve activity may play a crucial role in the development of such diseases11,12). However, these pathophysiological changes are highly dependent on sleep quality and quantity as evaluated by EEG11,12). Therefore, the accuracy of the sleeping hours of young children as reported by their parents should be clarified, in order to apply the data of reported sleeping hours to a large epidemiological study.
The purpose of this study is to evaluate the validity of the sleeping hours of young children as reported by their parents, with the use of a small instrument capable of assessing sleeping hours objectively.
METHODS
We are currently conducting a birth cohort study comprising of approximately 10000 children born in 19895,13). The present study was conducted in July and August 2001 as a sub-study of the follow-up study.
Subjects
An introductory letter was sent to the parents of 55 children aged 3 to 4 years, belonging to a public nursery school in Toyama prefecture. Of those parents, 24 agreed to participate and provided written informed consent. Of the participants, 1 child was reluctant to continue attaching the instrument and we terminated the measurement. Data from the 2 other children were not successfully measured and were excluded in the analysis. The remaining 21 children (12 boys and 9 girls) with a mean age of 3.81 (SD: 0.28) years were the subjects of the present study. These subjects did not have any chronic disease nor any obvious sleeping problem and did not take any medication during the measurement days.
Anthropometric measurements
All the anthropometric measurements were performed by one examiner. The heights and weights of children were measured wearing shorts. The heights of children were measured using a stadiometer, to the nearest 0.1 cm. The weights of children were measured using a balance scale to the nearest 0.1 kg. Body mass index (BMI; the weight in kilograms divided by the squared height in meters) was calculated as an index of obesity. The anthropometric measurements were conducted twice. The means were used in the analysis.
Assessment of sleeping habits in children
The sleeping habits of children were assessed by the use of a questionnaire and small instrument capable of assessing sleep quality and quantity.
We asked parents to complete a questionnaire containing the following questions on the sleeping habits of children, for 3 consecutive nights during the measurement days: get up time: when does your child get up? ; bedtime: when does your child go to bed? ; sleeping hours: how long does your child take a sleep? The sleep questionnaire values were expressed in hours and minutes. The means of the values from the 3 nights were used in the analysis.
For the objective measurement of sleeping habits, we used a small instrument capable of assessing sleeping quality and quantity by measuring activity, named Actiwatch® (Mini Mitter Company Inc., Bend, OR)14). Detailed information on the methodology for calculating the activity indices by this small instrument has been published elsewhere14). In summary, the Actiwatch® is a small (27mm x 26mm x 9 mm in size), light weight (17grams), limb worn, activity and sleep-wake pattern monitoring device, which contains an omni-directional sensor capable of detecting acceleration in two planes with a sensitivity of 0.01 gravity (0.098 m/sec2). This sensor integrates the degree and speed of motion and produces an electrical current that varies in magnitude. An increased degree of speed and motion produces an increase in voltage. The instrument stores this information as activity counts. The maximum sampling frequency is 32Hz. In the present study, the instrument was attached to a subjects’ ankle on the non-dominant leg. The subjects and parents were asked to keep the instrument attached for 3 consecutive days. After the researcher has entered bedtime and rising times and selected the length of sampling epoch and the sensitivity threshold, the device automatically estimates various sleep parameters according to the algorithm. We selected a sampling epoch of 1 minute and automatic sensitivity, in which the software automatically scores an epoch as sleep if the total activity value is equal to or less than the threshold sensitivity value calculated by (mean score in activity period x K (constant=0.888)) / (epoch length). The parameters calculated by the instrument are the following: sleep start: time of sleep onset; sleep end: the time of sleep termination; assumed sleeping hours: the difference in time between the end and start of sleep; actual sleeping hours: the assumed sleeping hours minus the sum of the epochs being scored as awake during the assumed sleep; sleep latency: the period between bedtime and sleep start; sleep efficiency: actual sleeping hours divided by the time in bed and multiplied by 100. All values, other than sleep efficiency, are expressed in hours and minutes. The unit of sleep efficiency is %.
The instrument has been validated using polysomnography (PSG) as the reference15-17). The percentages of the agreement of sleep/wake detection between PSG and the instrument ranged from 85 to 92 %15,16). There was a significant positive association between PSG and the instrument for sleep latency and sleep efficiency17). The instrument has been used in sleep studies18,19).
Statistical analysis
The sex differences in the reported and objective sleep parameters and anthropometric data were compared by unpaired t-tests. The differences and correlations between the reported and objective sleeping hours were analysed by paired t-tests and Pearson’s correlation coefficients. All statistical analyses were performed with the SPSS (7.5.1J) statistical package. A two-tailed P value of less than 0.05 was considered to be significant.
RESULTS
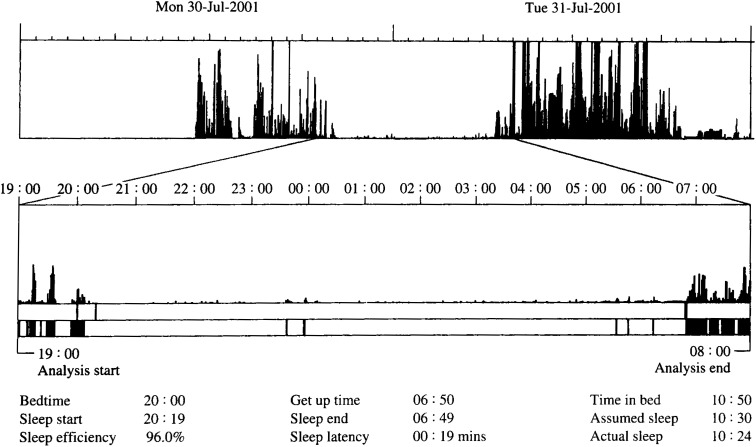
Figure 1 shows a representative actogram obtained from a subject. The data shows the 2 objective sleeping hours including the assumed and actual sleeping hours were calculated as 10:30 and 10:24, respectively.
Figure 1. A representative actogram obtained from a subject.
A representative actogram obtained from a subject is shown. The spikes in the upper actogram represent the activity counts per epoch. The higher spikes indicate higher activity. The lower actogram is an expanded window from the upper actogram in the nighttime. The solid bars in the lower actogram represent bouts considered as wake, according to the algorithm. Bedtime and get up time were manually entered. The other sleep parameters were automatically calculated.
Table 1 shows the characteristics of the study subjects by gender. There were no significant differences in ages of children, anthropometric data, and reported and objective sleep parameters between boys and girls. Reported sleeping hours during the measurements, and assumed and actual sleeping hours, as evaluated by the instrument, were 9.42, 8.63, and 8.51 hours, respectively. The mean sleep latency was 26.0 min. The mean sleep efficiency was 90.5%. Data from boys and girls were combined in the later analysis because there were no significant sex differences in the sleeping parameters. Table 2 presents the correlation and difference between the reported and objective sleeping hours. The correlation and difference between the reported sleeping hours during the measurement days and assumed or actual sleeping hours were 0.90 (p<0.001) and 0.79 hours (95%confidence interval: 0.59-0.99) and 0.90 (p<0.001) and 0.92 hours (0.73-1.10), respectively. The correlation and difference between the assumed and actual sleeping hours were 0.99 and 0.12 hours (0.06-0.19), respectively.
Table 1. Characteristics of the subjects of the present study.
| boys (n=12) | boys (n=12) | girls (n=9) | p value | |
|
|
||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age and anthropometric data | ||||
| age (years old) | 3.81 (0.28) | 3.79 (0.24) | 3.84 (0.33) | 0.728 |
| height (cm) | 98.8 (3.00) | 99.5 (2.98) | 97.9 (2.95) | 0.236 |
| weight (kg) | 15.4 (1.28) | 15.5 (1.18) | 15.3 (1.47) | 0.783 |
| BMI (kg/m2) | 15.8 (0.78) | 15.6 (0.69) | 16.0 (0.88) | 0.353 |
| Reported sleeping habits during the measurement days | ||||
| bedtime (hours:minutes) | 21:39 (0:59) | 21:43 (0:59) | 21:34 (1:01) | 0.745 |
| get up time (hours:minutes) | 7:04 (0:35) | 7:04 (0:38) | 7:04 (0:34) | 0.993 |
| sleeping hours (hours) | 9.42 (0.96) | 9.36 (1.16) | 9.51 (0.67) | 0.734 |
| Objective sleeping habits | ||||
| sleep start (hours:minutes) | 22:06 (1:02) | 22:10 (1:05) | 21:59 (1:00) | 0.685 |
| sleep end (hours:minutes) | 6:44 (0:34) | 6:45 (0:34) | 6:43 (0:37) | 0.900 |
| sleep latency (minutes) | 26.0 (17.0) | 27.0 (18.0) | 25.0 (17.0) | 0.733 |
| assumed sleeping (hours) | 8.63 (0.95) | 8.56 (1.09) | 8.73 (0.79) | 0.698 |
| actual sleep (hours) | 8.51 (0.91) | 8.44 (1.04) | 8.60 (0.75) | 0.700 |
| sleep efficiency (%) | 90.5 (4.13) | 90.5 (3.75) | 90.4 (4.83) | 0.965 |
The values are expressed as mean (SD). The sleep parameters between boys and girls are compared by unpaired t-tests.
Table 2. Correlations and differences between the reported and measured sleeping hours.
| correlation coefficients | differences and 95%confidence intervals | |||
|
|
|
|||
| r | p value | difference (95%CI) | p value | |
| reported vs assumed sleeping hours | 0.90 | <0.001 | 0.79 (0.59-0.99) 1 | <0.001 |
| reported vs actual sleeping hours | 0.90 | <0.001 | 0.92 (0.73-1.10) 1 | <0.001 |
| assumed vs actual sleeping hours | 0.99 | <0.001 | 0.12 (0.06-0.19) 2 | <0.001 |
The correlations and differences between the reported and measured sleeping hours are evaluated by Pearson’s correlation coefficients and paired t-tests. The data are expressed as hours. 1The differences between reported and objective sleeping hours are calculated by using objective sleeping hours as a reference. 2The differences between assumed and actual sleeping hours are calculated by using actual sleeping hours as a reference. Abbreviations: r: Pearson’s correlation coefficient, 95%CI: 95%confidence interval
DISCUSSION
The present study indicates that the sleeping hours of young children as reported by their parents are strongly related to the assumed sleeping hours (r=0.90) as estimated by the Actiwatch® instrument. Furthermore, the mean difference between the reported and assumed sleeping hours is small, 0.79 hours (47.4 min). The difference between the reported and assumed sleeping hours may be explained by the sum of the difference between times for going to bed and falling asleep (sleep latency) and the difference between times for waking and rising (early morning waking). Coble et al.20) reported that sleep latency and early morning awakening of young children aged 6 to 7 years, as evaluated by EEG, were 18.4 min and 6.3 min on average, respectively. In the present study, sleep latency and early morning awakening were 27 min and 20.4 min, respectively. Therefore, if the difference in experimental settings (laboratory vs field study, etc.) is taken into consideration, our findings are not so inconsistent with those of the previous study.
In the present study, we also evaluated the correlation and difference between the reported and actual sleeping hours. The correlation coefficient was also high (r=0.90), although a slightly larger difference between the reported and actual sleeping hours was observed than the difference between the reported and assumed sleeping hours.
Our results indicate, therefore, that the reported sleeping hours are strongly associated with the objective sleeping hours, although parents tend to uniformly overestimate the sleeping hours of their children. This means that the sleeping hours of healthy young children as reported by their parents could be used to evaluate the relative difference in sleeping hours in healthy young children and could be applied to a large epidemiological survey, which requires data of relative differences in sleeping hours amongst a given population.
In the present study, however, subjects with a sleeping problem were not included. Hence, the correlation between the assumed and actual sleeping hours was high (r=0.99) and the difference between the 2 objective sleeping hour measurements was small. Sleep efficiency, one of the indices representing sleep quality, was high, 90.5 % on average. If subjects with a sleeping problem had been included, the correlation and difference between reported and assumed or actual sleeping hours would have been weaker and larger, respectively. This is because the measurement of actual sleeping hours was calculated from assumed sleeping hours and the sum of epochs being scored as awake during sleep, which indicates that actual sleeping hours may largely reflect sleep quality. Furthermore, in considering the biological mechanisms responsible for the development of psychiatric and somatic problems caused by short sleeping hours, recent studies have mentioned that sleep quality as well as quantity play a crucial role in the development of such diseases through changes in hormonal secretion and autonomic nerve activity11,12). For instance, nocturnal growth hormone secretion starts immediately after the onset of sleep and is secreted markedly in the first half of the night, during which slow wave sleep predominates in EEG11,21). In addition to a decrease in sleep quantity such as caused by sleep deprivation, a decrease in sleep quality such as fragmented sleep, as seen in patients with obstructive sleep apnea syndrome, results in a remarkable decrease or absence of GH secretion11,21,22). Sympathetic nerve activity, evening cortisol secretion, and glucose tolerance are also dependent on sleep quality and quantity12). Thus, the measurement of actual sleeping hours may be a more important index in subjects with sleeping problems than assumed sleeping hours. Therefore, reported sleeping hours should be cautiously used in a survey that includes subjects with sleeping problems.
As a limitation of the present study, this study included a relatively small number of subjects and may have tended to include subjects of parents who were interested in the sleeping habits of their children. The validity of reported sleeping hours in a general population might be lower than that found in the present study. Furthermore, these parents might have paid particular attention to the sleeping habits of their children during the study periods. These factors may affect the accuracy of the sleeping hours of their children. Further study is necessary, therefore, to clarify a more accurate assessment of the validity of sleeping habits of young children as reported by their parents.
In conclusion, the sleeping hours of young children as reported by their parents was strongly associated with objective sleeping hours. Furthermore, although parents tended to overestimate the sleeping hours of their children, the difference between the reported and objective sleeping hours was not so large. These results indicate that the sleeping hours of healthy young children as reported by parents could be used in a survey that required data of relative differences in sleeping hours amongst a given population.
ACKNOWLEDGMENTS
We are indebted to the principals and teachers of the nursery school for their agreement to take part and their cooperation in this study. We also thank all parents and children participating in this study. This study was supported by grants from the Ministry of Health and Welfare (H10-Child-020) and Toyama Medical Association. The funding organizations were not involved in the design, conduct, interpretation, and analysis of the study, nor in the review or approval of this manuscript.
REFERENCES
- 1.Meijer AM, Habekothe HT, Van Den Wittenboer GL. Time in bed, quality of sleep and school functioning of children. J Sleep Res, 2000; 9: 145-153. [DOI] [PubMed] [Google Scholar]
- 2.Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbances in elementary school-aged children. J Dev Behav Pediatr, 2000; 21: 27-36. [DOI] [PubMed] [Google Scholar]
- 3.Aronen ET, Paavonen EJ, Fjallberg M, Soininen M, Torronen J. Sleep and psychiatric symptoms in school-age children. J Am Acad Child Adolesc Psychiatry, 2000; 39: 502-508. [DOI] [PubMed] [Google Scholar]
- 4.Locard E, Mamelle N, Billette A, Miginiac M, Munoz F, Rey S. Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes Relat Metab Disord, 1992; 16 :721-729. [PubMed] [Google Scholar]
- 5.Sekine M, Yamagami T, Hamanishi S, Chen X, Handa K, et al. A 6-year longitudinal study on the relationship between parental or lifestyle factors at age 3 on childhood obesity at age 9: results of the Toyama birth cohort study. J Welfare Stat, 2001; 48: 14-21. (in Japanese) [Google Scholar]
- 6.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep, 2000; 23: 1043-1051. [PubMed] [Google Scholar]
- 7.Armstrong KL, Quinn RA, Dadds MR. The sleep patterns of normal children. Med J Aust, 1994; 161:202-206. [DOI] [PubMed] [Google Scholar]
- 8.Segawa M. Sleep regulation in infants. In; Torii S ed. Sleep and environment. Asakura Shoten, Tokyo, 1999: 110-123. (in Japanese) [Google Scholar]
- 9.Rosen CL. Obstructive sleep apnea syndrome (OSAS) in children: diagnostic challenges. Sleep, 1996; 19 (10 Suppl): S274-S277. [PubMed] [Google Scholar]
- 10.Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol, 2000; 36: 291-301. [DOI] [PubMed] [Google Scholar]
- 11.Scheen AJ, Byrne MM, Plat L, Leproult R, Van Cauter E. Relationship between sleep quality and glucose regulation in normal humans. Am J Physiol, 1996; 271(2 Pt1): E261-E270. [DOI] [PubMed] [Google Scholar]
- 12.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet, 1999; 354: 1435-1439. [DOI] [PubMed] [Google Scholar]
- 13.Kagamimori S, Yamagami T, Sokejima S, et al. The relationship between lifestyle, social characteristics and obesity in 3-year-old Japanese children. Child Care Health Dev, 1999; 25: 235-247. [DOI] [PubMed] [Google Scholar]
- 14.Instruction manual, software version 3.2 and earlier. Bend, Mini Mitter Company, Inc, OR USA, 2000
- 15.Lotjonen JM, Korhonen I, Hirvonen K, Rekola M, Myllymaki M, Partinen M. Sleep/wake detection using an active security device. Sleep, 2001; 24(Suppl): S399. [Google Scholar]
- 16.Chang A, Kushida C, Palombini L, Carrillo O, Hindman J, Hong S, Hyde P, Guilleminault C. Comparison study of actigraphic, polysomnographic, and subjective perception of sleep parameters. Sleep, 1999; 22(Suppl): S43 [Google Scholar]
- 17.Pilsworth SN, King MA, Shneerson JM, Smith IE. A comparison between measurements of sleep efficiency and sleep latency measured by polysomnography and wrist actigraphy. Sleep, 2001; 24(Suppl): S106. [Google Scholar]
- 18.Randazzo AC, Schweitzer PK, Walsh JK. Cognitive function following three nights of sleep restriction in children 10-14. Sleep, 1998; 21(Suppl): S249. [PubMed] [Google Scholar]
- 19.Zhdanova IJ, Taylor JA, Leclair OU, Wurtman RJ. Effects of melatonin on blood pressure in people 50 years old. Sleep, 1998; 21(Suppl): S213 [Google Scholar]
- 20.Coble PA, Kupfer DJ, Taska LS, Kane J. EEG sleep of normal healthy children. Part I: Findings using standard measurement methods. Sleep, 1984; 7: 289-303. [DOI] [PubMed] [Google Scholar]
- 21.Van Cauter E, Caufriez A, Kerkhofs M, Van Onderbergen A, Thomer MO, Copinschil G. Sleep, awakenings, and insulin-like growth factor-I modulate the growth hormone (GH) secretory response to GH-releasing hormone. J Clin Endocrinol Metab 1992; 74: 1451-1459. [DOI] [PubMed] [Google Scholar]
- 22.Grunstein RR, Handelsman DJ, Lawrence SJ, Blackwell C, Caterson ID, Sullivan CE. Neuroendocrine dysfunction in sleep apnea; reversal by continuous positive airway pressure therapy. J Clin Endocrinol Metab, 1989; 68: 352-358. [DOI] [PubMed] [Google Scholar]