Abstract
The health-related quality of life (HRQoL) among long-term Adolescent and Young Adult Cancer Survivors (AYACS) and an age- and sex-matched normative population was examined. Although the HRQoL of AYACS was worse compared to the normative population before and during the COVID-19 pandemic, the scores of AYACS improved over time in contrast to the normative population. Presumably, AYACS are used to adjusting their lives to stressful life events. Furthermore, the lockdown may have been beneficial for AYACS who face difficulties fully participating in society due to the impact of cancer. AYACS who encounter HRQoL issues could benefit from support interventions to empower them and build resilience.
Supplementary Information
The online version contains supplementary material available at 10.1186/s41687-023-00629-0.
Keywords: Adolescents and young adults, COVID-19, Health-related quality of life, Social functioning, Survivorship, Cancer
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had a great impact on the capacity of patients and healthcare systems. At the peaks of the pandemic, many appointments and treatments were cancelled or postponed. There is emerging research on the psychological impact of COVID-19 on the general population, but especially on vulnerable populations such as cancer patients [1–7].
Adolescent and Young Adult cancer survivors (AYACS), in this manuscript defined as adolescents and young adults who had been diagnosed with primary cancer between ages 18–39 years, might be particularly vulnerable to the effects of the pandemic, because of their unique developmental, educational, social and emotional needs [8]. Studies conducted before the start of the COVID-19 pandemic show that AYACS experience a lower health-related quality of life (HRQoL) compared to the general population [9–11]. AYACS already face significant challenges and psychological distress due to a cancer diagnosis, which are possibly exacerbated by COVID-19.
Cancer patients in general have a higher risk of developing complications from COVID-19, which can be partly ascribed to factors such as older age, higher smoking rates, comorbidities, frequent healthcare exposures and the effects of cancer therapies [4]. During the COVID-19 pandemic, cancer patients also experienced more mental health concerns as well as an enduring sense of fear and worry about their potential health risks and changes in their follow-up care [5]. Furthermore, quarantine and social isolation contribute to feelings of isolation and loneliness among cancer patients which further compromised their mental health [2, 6, 7]. Studies among AYACS investigating the impact of the COVID-19 pandemic show high levels of insomnia, loneliness and psychological distress, with feelings of anxiety reported more prominently than depressive symptoms [12–14].
Previously conducted studies on the impact of COVID-19 on AYACS focus on adolescents and young adults who had active treatment or were within 5 years after diagnosis. To the best of our knowledge, there are no existing studies that investigate the impact of the COVID-19 pandemic on the HRQoL among long-term (5 or more years) AYACS. Moreover, other studies do not have a longitudinal research design and do not include data of an age- and sex-matched normative population. Insight into the impact of the COVID-19 pandemic on HRQoL of long-term AYACS is warranted. Understanding the unique challenges that this population may experience currently as a result of the COVID-19 pandemic is necessary in order to support and treat AYACS optimally. Therefore, within a subsample of the SURVAYA study [15], we investigate the differences in HRQoL between AYACS and an age- and sex-matched normative population (1) before-, (2) during the COVID-19 pandemic and (3) over time.
Methods
Setting and population
The cross-sectional population-based SURVAYA study was conducted among long-term survivors (5–20 years) of cancer on AYA-age (18–39 years) [15]. They received primary cancer treatment between 1999 and 2015 and were treated at the Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital or at an academic hospital in the Netherlands.. The SURVAYA study was approved by the Institutional Review Board of the Netherlands Cancer Institute (IRBd20-115) and registered within clinical trial registration (NCT05379387).
Data collection
Data was collected between May 2019 and June 2021 and the data collection process is described in more detail elsewhere [15]. Patients who participated in the SURVAYA study before the start of the first COVID-19 lockdown (March 23, 2020), and who gave consent to be invited for additional questionnaire studies (n = 1089), were invited to complete a COVID-19 specific questionnaire between 16 April and 14 May 2020 (Additional file 1: Fig. S1).
Normative population
The normative population was derived from a reference cohort of the general Dutch population (CentER panel), which is representative for the Dutch-speaking population in the Netherlands [16]. Members of this panel received online questionnaires in November 2017 (wave 1) and May 2020 (wave 2) (n = 907). This normative population was matched based on the age and sex distribution of the SURVAYA-COVID-19 study. A frequency matching method was used with age strata (18–30 years, 30–40 years and 40–60 years) and sex strata (females and males) to maximize the number of control participants matched to AYACS. This resulted in 108 matched cancer-free individuals for the 407 AYACS.
Study measures
Self-reported sociodemographic data included sex, marital status (with or without a partner) and educational level (no education or primary education, secondary (vocational) education and higher (vocational and University education). Linkage with the Netherlands Cancer Registry (NCR) provided information on age at questionnaire completion, time since diagnosis, type of cancer, tumor stage and primary treatment modality (surgery, chemotherapy, radiotherapy, hormone therapy, targeted therapy and stem cell therapy). HRQoL was assessed with the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30) [17]. Linear transformation was used to obtain scores ranging from 0 to 100, where a higher score represents a higher (“better”) level of functioning (physical functioning, role functioning, emotional functioning, cognitive functioning, social functioning and global quality of life) or higher (“worse”) level of symptoms (fatigue, pain, dyspnea and insomnia). Clinically relevant differences were determined using the evidence-based guidelines for interpretation of the EORTC QLQ-C30. These guidelines define a minimum number of points that are required to detect a clinically relevant difference [18, 19]. Thresholds of clinical importance were used for social functioning (58), cognitive functioning (75), fatigue (39) and pain (25) to identify patients with impaired/within normal functioning before and during the COVID-19 pandemic [20].
Statistical analyses
All statistical analyses were performed using SAS (version 9.3 for Windows; SAS institute Inc., Cary, NC). Differences between socio-demographic and clinical characteristics between AYACS and the normative population were assessed with a chi-square test (categorial variables) or independent sample t-test (continue variables). The HRQoL mean changes of AYACS and normative population over time were assessed with paired sample t-tests. Analyses of covariance (ANCOVA) were carried out to compare HRQoL between AYACS and the normative population, adjusted for educational level (high-medium/low) and partner status (yes/no). Due to the multiple statistical tests conducted in this study and to avoid type 1 errors, all differences with a P-value < 0.01 were indicated as statistically significant. A graphical representation of the intraindividual longitudinal changes over time is displayed for HRQoL scales that showed medium and small clinically relevant differences.
Results
Sample characteristics
In the SURVAYA study, 4010 AYACS participated, of whom 1089 participated before the COVID-19 pandemic and were eligible to participate in the additional COVID-19 questionnaire study (Additional file 1: Fig. S1). In the additional COVID-19 questionnaire study, 407 AYACS participated (37%). The demographic and clinical characteristics of the included AYACS (n = 407) and age- and sex-matched normative population (n = 108) are summarized in Table 1. AYACS were significantly more likely to be married/partnered (p < 0.0001) and were higher educated (p < 0.0001) than the matched normative population.
Table 1.
Socio-demographic and clinical characteristics of AYA cancer survivors and matched normative population
| AYA cancer survivors (N = 407) | Matched normative Population (N = 108) | P value | ||
|---|---|---|---|---|
| n (%) | n (%) | |||
| Gender | Male | 129 (31.7%) | 34 (31.5%) | 0.9 |
| Female | 278 (68.3%) | 74 (68.5%) | ||
| Age (at time of questionnaire), (mean (SD) in years) | 45.5 (6.9) | 44.4 (10.3) | 0.2 | |
| 23–40 years | 78 (19.2%) | 21 (19.4%) | ||
| 40–50 years | 220 (54.1%) | 58 (53.7%) | ||
| 50–60 years | 109 (26.8%) | 29 (26.9%) | ||
| Married/partnered | Partner | 334 (82.1%) | 59 (54.6%) | < .00011 |
| Education level | No education or primary education | 2 (0.5%) | 4 (3.7%) | < .00011 |
| Secondary (vocational) education | 117 (28.7%) | 71 (66.36%) | ||
| Higher (vocational) and University education | 288 (70.8%) | 32 (29.9%) | ||
| Treatment/follow up status | Currently being treated or have to start treatment | 16 (3.9%) | NA | |
| Completed treatment, now in follow-up | 194 (47.7%) | |||
| Completed treatment, not in follow-up | 197 (48.4%) | |||
| Time since diagnosis, (mean (SD) in years) | 12.4 (4.3) | NA | ||
| 5–10 years | 131 (32.2%) | |||
| ≥ 11–15 years | 151 (37.1%) | |||
| ≥ 16–20 years | 125 (30.7%) | |||
| Type of cancer | Bone and soft tissue sarcoma | 19 (4.7%) | NA | |
| Melanoma | 24 (5.9%) | |||
| Colon and rectum | 11 (2.7%) | |||
| Breast | 153 (37.6%) | |||
| Female genitalia | 29 (7.1%) | |||
| Germ cell tumors | 55 (13.5%) | |||
| Lymphoid haematological malignancies | 44 (10.8%) | |||
| Myeloid hematological malignancies | 13 (3.2%) | |||
| Thyroid gland | 15 (3.7%) | |||
| Central nervous system | 22 (5.4%) | |||
| Other3 | 22 (5.3%) | |||
| Primary treatment modality | Surgery | 338 (83.0%) | NA | |
| Chemotherapy | 237 (58.2%) | |||
| Radiotherapy | 231 (56.8%) | |||
| Hormone therapy | 84 (20.6%) | |||
| Targeted therapy | 40 (9.8%) | |||
| Stem cell therapy | 14 (3.4%) |
1Chi-square p-value, 2Independent sample t-test, 3Head and neck: 5 (1.2%); Digestive tract, other: 4 (1.0%); Respiratory tract: 6 (1.5%); Male genitalia: 1 (0.2%); Urinary tract: 5 (1.2%); Eye: 1 (0.2%)
HRQoL before and during COVID-19 pandemic
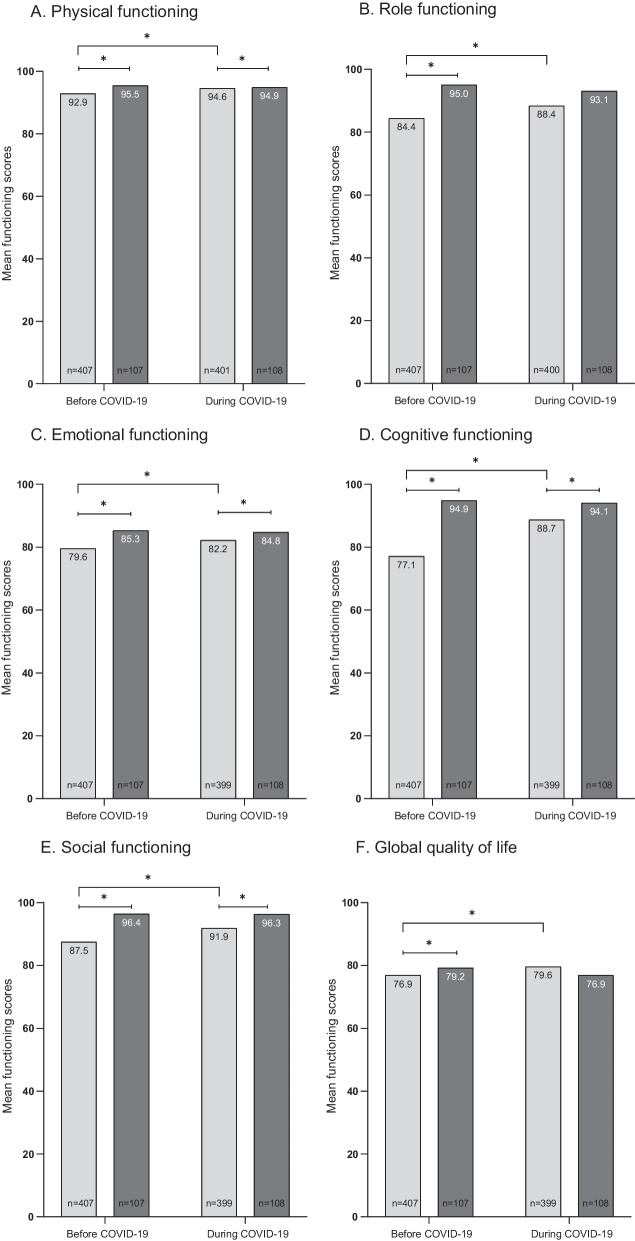
Before COVID-19, compared to an age- and sex-matched normative population, AYACS reported on average, worse scores on the EORTC QLQ-C30 functioning and symptoms scales (Fig. 1A–J). These differences between AYACS and the normative population were considered of medium clinical relevance for fatigue (− 18.5 score points, p-value: < 0.0001) and small for role-functioning (+ 10.6 score points, p-value: < 0.0001), social-functioning (+ 8.9 score points, p-value: < 0.0001), pain (− 6.1 score points, p-value: < 0.0001), dyspnea (− 4.2 score points, p-value: 0.0079) and insomnia (− 6.5 score points, p-value: 0.00554).
Fig. 1.
A–J HRQoL scores of AYACS and age- and sex-matched normative population before and during the COVID-19 pandemic. Note. A higher score on the functioning scales refers to a better HRQoL (physical functioning, role functioning, emotional functioning, cognitive functioning, social functioning and global quality of life). A higher score on symptoms scales refers to more symptoms (fatigue, pain, dyspnea and insomnia). *Significant difference (p < 0.001)
During the COVID-19 pandemic, physical-functioning, emotional-functioning, cognitive-functioning, social-functioning, and insomnia scores of AYACS were significantly worse compared to the normative population. However, these differences were smaller than before the start of the COVID-19 pandemic. During the COVID-19 pandemic, only a small clinically relevant difference was found for cognitive functioning (+ 5.4 score points, p-value: 0.0004) and insomnia (− 5.1 score points, p-value: 0.0098) between AYACS and the normative population.
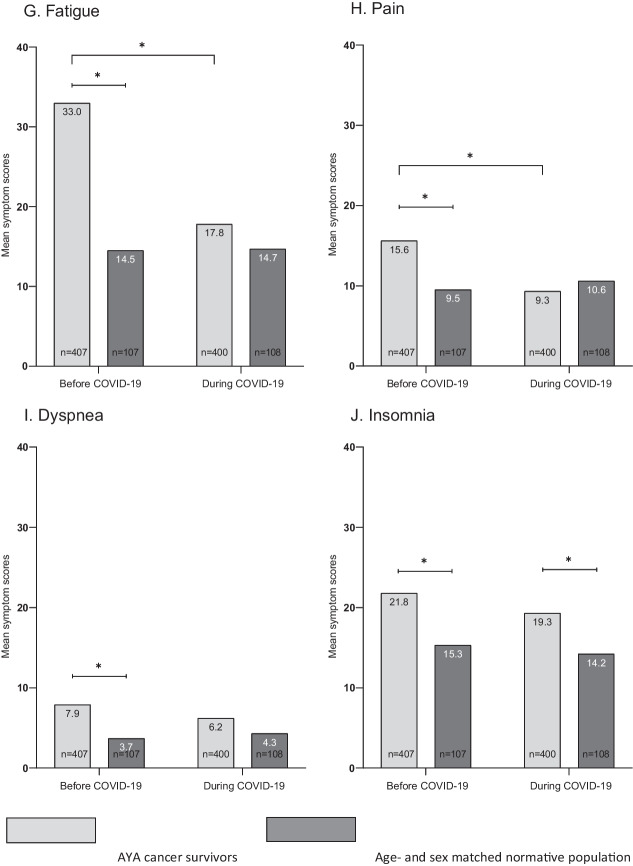
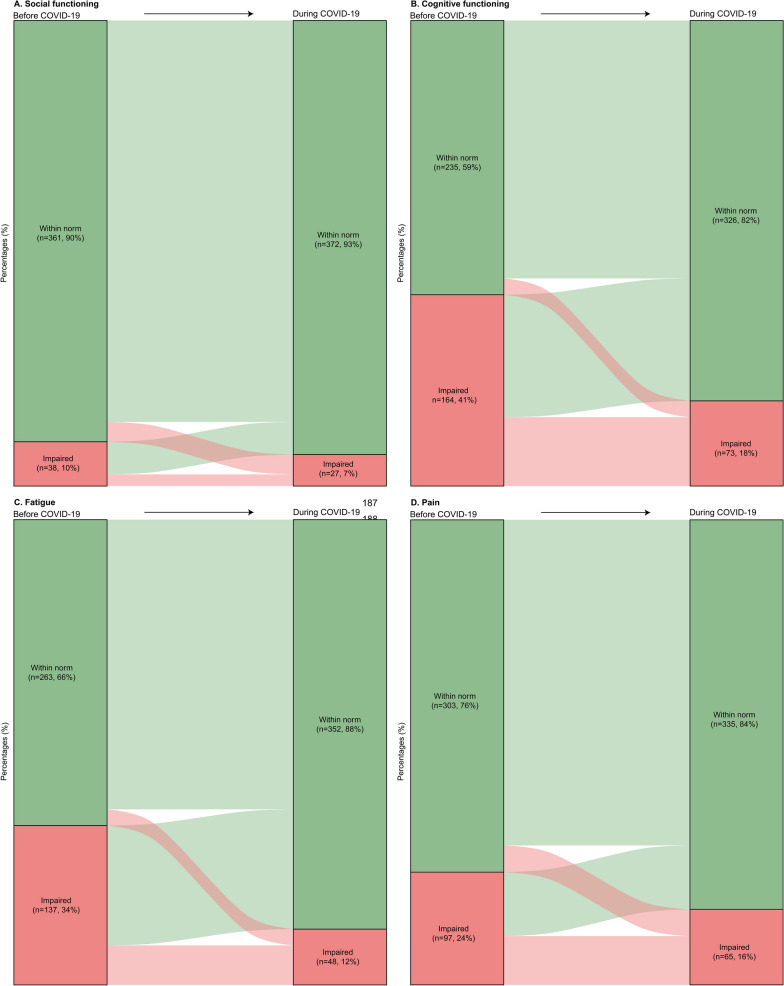
AYACS reported better HRQoL scores during the COVID-19 pandemic than before its start. The improvements in cognitive functioning (+ 11.6 score points, p-value: < 0.0001) and fatigue (− 15.2 score points, p-value: < 0.0001) were of medium clinical relevance. Differences in social functioning (+ 4.4 score points, p-value: < 0.0001) and pain (− 6.3 score points, p-value: < 0.0001) were considered of small clinical relevance. The HRQoL scores of the normative population remained stable over time. Figure 2A–D shows the intraindividual longitudinal changes in social-functioning, cognitive-functioning, fatigue and pain among AYACS.
Fig. 2.
A–D Graphical representation of intraindividual longitudinal changes in A social functioning, B cognitive functioning, C fatigue and D pain among AYACS. Note. A Within norm (before COVID-19) to within norm (during COVID-19): 344 AYACS (86%); Within norm (before COVID-19) to impaired (during COVID-19): 17 AYACS (4%); Impaired (before COVID-19) to within norm (during COVID-19): 28 AYACS (7%); Impaired (before COVID-19) to impaired (during COVID-19): 10 (3%). B Within norm (before COVID-19) to within norm (during COVID-19): 221 AYACS (55%); Within norm (before COVID-19) to impaired (during COVID-19): 14 AYACS (4%); Impaired (before COVID-19) to within norm (during COVID-19): 105 AYACS (26%); Impaired (before COVID-19) to impaired (during COVID-19): 59 (15%). C Within norm (before COVID-19) to within norm (during COVID-19): 249 AYACS (62%); Within norm (before COVID-19) to impaired (during COVID-19): 14 AYACS (4%); Impaired (before COVID-19) to within norm (during COVID-19): 103 AYACS (26%); Impaired (before COVID-19) to impaired (during COVID-19): 34 (9%). D Within norm (before COVID-19) to within norm (during COVID-19): 280 AYACS (70%); Within norm (before COVID-19) to impaired (during COVID-19): 23 AYACS (6%); Impaired (before COVID-19) to within norm (during COVID-19): 55 AYACS (14%); Impaired (before COVID-19) to impaired (during COVID-19): 42 (11%)
Discussion
This study aimed to investigate the longitudinal impact of the COVID-19 pandemic on the HRQoL of long-term AYACS and to compare their HRQoL with the general population before and during the pandemic. AYACS experienced worse HRQoL scores, before and during the COVID-19 pandemic compared to the normative population. However, in contrast to the normative population, the HRQoL of AYACS improved during the pandemic with the largest differences in social functioning, cognitive functioning, fatigue and pain.
Our results showed that long-term AYACS experienced better HRQoL scores during the pandemic than before it. To the best of our knowledge, no studies exist regarding the impact of COVID-19 on HRQoL in long-term AYACS. There are several studies with a cross-sectional study design among adolescents and young adults in active treatment or shortly after diagnosis that investigate the impact of the COVID-19 pandemic on psychological well-being. High levels of psychological distress during the COVID-19 pandemic were reported [12, 14, 21]. Specifically, the cross-sectional study of Košir et al. found that 30% of the adolescents and young adults experienced more psychological distress and 60% reported more anxious feelings during the COVID-19 pandemic than previously [14]. Moreover, adolescents and young adults who were undergoing treatment or were within 6 months of treatment completion reported higher levels of psychological distress on average. This was supported by a study where the lowest elevated psychological distress was found in those off treatment, for whom healthcare was also the least affected by the pandemic [14]. Adolescents and young adults who are undergoing treatment likely experience more distress than long-term AYACS due to uncertainty about beginning or continuing treatment under the COVID-19 restrictions during treatment in the first five years after cancer diagnosis.
In the long-term, AYACS reported worse HRQoL outcomes in all HRQoL domains overall compared to the general population. This is in line with results from a review by Quinn et al. and other recent international studies [9, 10, 22, 23]. However, our study found no adverse impact on HRQoL attributed to COVID-19 specifically, even though cancer survivors are more at risk of developing serious illnesses from the disease. Two possible explanations are that the ability of AYACS to deal with abnormal life-situations is obviously already high and better than their peers. A study by Jacobsen et al. found that high levels of resilience acted as protective factor for psychological distress in AYACS with cancer during the COVID-19 pandemic [13]. Another explanation could be that some AYACS experienced more difficulties (e.g. stress because they were not able to work the required hours or manage all the work because of cognitive or physical problems) to participate fully in society before COVID-19. The societal changes that were implemented by governments to decrease the spread of highly infectious COVID-19, including travel restrictions and nationwide quarantine, resulted in a lockdown of society. This shut down could have been beneficial for those who struggled to fully participate in society just like their peers, such as those who experience the long-term physical and mental effects of cancer.
Future implications
Considering that the HRQoL reported by long-term AYACS was still lower than that of the normative population, there are fruitful avenues for future research and interventions in AYA care are needed. Psychological and physical support is important for those at risk of poor HRQoL scores, even 5–20 years after diagnosis. To assess whether there are differences in HRQoL between subgroups of AYACS, additional analyses of HRQoL outcomes in a larger sample of AYACS would enable greater insight into the characteristics of those AYACs at greater risk of poor HRQoL outcomes. Analysing subgroups of AYACS stratified by age, education level, time since diagnosis and cancer type can inform health care services by informing the development and planning of interventions that take the needs of AYACS into consideration. Psychological and physical support interventions must address empowerment and building resilience to help AYACS live with the short- and long-term effects of cancer.
Strengths and limitations
The interpretation of the findings of this study must consider some limitations. Among the SURVAYA respondents, participants were asked to complete the COVID-19 specific questionnaire study. Selection bias was reported within the SURVAYA study, since study participation was significantly lower among specific subgroups, such as males and survivors with a lower socio-economic status [15]. Non-response may have caused selection bias, limiting the generalizability of the results this study. Moreover, in this study, the AYACS study population obtained higher levels of education compared to the normative population and were more likely to be married/partnered. Previous research has shown that cancer survivors who obtained lower levels of education and/or cancer survivors who are unmarried or do not have a partner tend to have worse HRQoL outcomes and experience more distress [24, 25]. Therefore, this may have influenced our results and HRQoL scores of the AYACS might be overestimated in the cross-sectional comparisons between AYACS and normative population.
Conclusion
Compared to an age- and sex matched normative population, AYACS experience worse HRQoL scores, both before and during the COVID-19 pandemic. However, the HRQoL of AYACS improved during the pandemic in contrast to the matched normative population. The lockdown of the society could have been beneficial for AYACS who experience short-and long-term effects of cancer which can hinder full participation in society just like their peers. Moreover, AYACS may be more adept at coping with abnormal life-threatening situations than the general population.
Supplementary Information
Additional file 1. Fig. S1: Flowchart of the data collection process of the SURVAYA-COVID-19 study.
Acknowledgements
The authors wish to thank all the patients for their participation in the study. We wish to thank the registration team of the Netherlands Comprehensive Cancer Organisation (IKNL) for the collection of data for the Netherlands Cancer Registry and the PROFILES registry group for the data collection support.
Abbreviations
- AYACS
Adolescent and Young Adult Cancer Survivors
- COVID-19
Coronavirus Disease 2019
- EORTC QLQ-C30
European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire C30
- HRQoL
Health-related quality of life
Author contributions
Conceptualization, C.V., L.V.v.d.P.-F., W.T.A.v.d.G. and O.H.; data curation, C.V.; formal analysis, C.V.; funding acquisition, L.V.v.d.P.-F., W.T.A.v.d.G. and O.H.; investigation, C.V., S.H.M.J., R.B., S.E.J.K., J.M.K., J.M.T., M.E.M.M.B., R.I.L., J.N., M.C.M.K. and O.H.; methodology, C.V., L.V.v.d.P.-F., W.T.A.v.d.G. and O.H.; project administration, C.V. and O.H.; resources, C.V. and S.H.M.J.; software, C.V.; supervision, L.V.v.d.P.-F., W.T.A.v.d.G. and O.H.; validation, C.V. and O.H.; visualization, C.V., S.H.M.J. and O.H.; writing—original draft preparation, C.V. and O.H.; writing—review and editing, C.V., S.H.M.J., L.V.v.d.P.F., R.B., S.E.J.K., J.M.K., J.M.T., M.E.M.M.B., R.I.L., J.N., M.C.M.K., W.T.A.v.d.G. and O.H. All authors read and approved the final manuscript.
Funding
Carla Vlooswijk Msc is supported by the Dutch Cancer Society (#11788 COMPRAYA study). Dr. Olga Husson and Silvie Janssen MSc are supported by the Netherlands Organization for Scientific Research VIDI grant (198.007). Data collection of the SURVAYA study was partly supported by the investment Grant (#480-08-009) from the Netherlands Organization for Scientific Research. These funding agencies had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the paper; or in the decision to submit the paper for publication.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to privacy issues but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The SURVAYA study and COVID-19 specific questionnaire study were approved by the Institutional Review Board of the Netherlands Cancer Institute (IRBd18-122 and IRBd20-115). Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang Y, Kala MP, Jafar TH (2020) Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS ONE 15(12):e0244630. 10.1371/journal.pone.0244630 [DOI] [PMC free article] [PubMed]
- 2.Amaniera I, Bach C, Vachani C, Hampshire M, Arnold-Korzeniowski K, Healy M, et al. Psychosocial impact of the COVID-19 pandemic on cancer patients, survivors and caregivers. J Psychosoc Oncol. 2021;39(3):485–492. doi: 10.1080/07347332.2021.1913780. [DOI] [PubMed] [Google Scholar]
- 3.Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020 doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun L, Surya S, Le AN, Desai H, Doucette A, Gabriel P, et al. Rates of COVID-19-related outcomes in cancer compared with noncancer patients. JNCI Cancer Spectr. 2021;5(1):Pkaa120. doi: 10.1093/jncics/pkaa120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Momenimovahed Z, Salehiniya H, Hadavandsiri F, Allahqoli L, Günther V, Alkatout I. Psychological distress among cancer patients during COVID-19 pandemic in the world: a systematic review. Front Psychol. 2021;12:682–154. doi: 10.3389/fpsyg.2021.682154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miaskowski C, Paul SM, Snowberg K, Abbott M, Borno HT, Chang SM, et al. Loneliness and symptom burden in oncology patients during the COVID-19 pandemic. Cancer. 2021;127(17):3246–3253. doi: 10.1002/cncr.33603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van de Poll-Franse LV, de Rooij BH, Horevoorts NJE, May AM, Vink GR, Koopman M, et al. Perceived care and well-being of patients with cancer and matched norm participants in the COVID-19 crisis: results of a survey of participants in the Dutch PROFILES Registry. JAMA Oncol. 2021;7(2):279–284. doi: 10.1001/jamaoncol.2020.6093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrari A, Stark D, Peccatori FA, Fern L, Laurence V, Gaspar N, et al. Adolescents and young adults (AYA) with cancer: a position paper from the AYA Working Group of the European Society for Medical Oncology (ESMO) and the European Society for Paediatric Oncology (SIOPE) ESMO Open. 2021;6(2):100096. doi: 10.1016/j.esmoop.2021.100096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schulte FSM, Chalifour K, Eaton G, Garland SN. Quality of life among survivors of adolescent and young adult cancer in Canada: a Young Adults With Cancer in Their Prime (YACPRIME) study. Cancer. 2021;127(8):1325–1333. doi: 10.1002/cncr.33372. [DOI] [PubMed] [Google Scholar]
- 10.Harju E, Roser K, Dehler S, Michel G. Health-related quality of life in adolescent and young adult cancer survivors. Support Care Cancer. 2018;26(9):3099–3110. doi: 10.1007/s00520-018-4151-z. [DOI] [PubMed] [Google Scholar]
- 11.Husson O, Prins JB, Kaal SEJ, Oerlemans S, Stevens WB, Zebrack B, et al. Adolescent and young adult (AYA) lymphoma survivors report lower health-related quality of life compared to a normative population: results from the PROFILES registry. Acta Oncol. 2017;56(2):288–294. doi: 10.1080/0284186X.2016.1267404. [DOI] [PubMed] [Google Scholar]
- 12.Yan A, Howden K, Mahar AL, Scott I, Glidden C, Deleemans J, et al. Experiences of adolescent and young adult cancer survivors during the COVID-19 pandemic. J Cancer Surviv. 2022 doi: 10.1007/s11764-021-01158-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobson C, Miller N, Mulholland R, Baker L, Glazer D, Betts E, et al. Psychological distress and resilience in a multicentre sample of adolescents and young adults with cancer during the COVID-19 pandemic. Clin Child Psychol Psychiatry. 2022;27(1):201–213. doi: 10.1177/13591045211056923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Košir U, Loades M, Wild J, Wiedemann M, Krajnc A, Roškar S, et al. The impact of COVID-19 on the cancer care of adolescents and young adults and their well-being: Results from an online survey conducted in the early stages of the pandemic. Cancer. 2020;126(19):4414–4422. doi: 10.1002/cncr.33098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vlooswijk C, Poll-Franse LVvd, Janssen SHM, Derksen E, Reuvers MJP, Bijlsma R et al (2022) Recruiting adolescent and young adult cancer survivors for patient-reported outcome research: experiences and sample characteristics of the SURVAYA study. Curr Oncol 29(8):5407–5425 [DOI] [PMC free article] [PubMed]
- 16.van de Poll-Franse LV, Mols F, Gundy CM, Creutzberg CL, Nout RA, Verdonck-de Leeuw IM, et al. Normative data for the EORTC QLQ-C30 and EORTC-sexuality items in the general Dutch population. Eur J Cancer. 2011;47(5):667–675. doi: 10.1016/j.ejca.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 18.Cocks K, King MT, Velikova G, de Castro G Jr, Martyn St-James M, Fayers PM et al (2012) Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur J Cancer 48(11):1713–1721. 10.1016/j.ejca.2012.02.059 [DOI] [PubMed]
- 19.Cocks K, King MT, Velikova G, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. J Clin Oncol. 2011;29(1):89–96. doi: 10.1200/jco.2010.28.0107. [DOI] [PubMed] [Google Scholar]
- 20.Giesinger JM, Loth FLC, Aaronson NK, Arraras JI, Caocci G, Efficace F, et al. Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research. J Clin Epidemiol. 2020;118:1–8. doi: 10.1016/j.jclinepi.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Glidden C, Howden K, Romanescu RG, Hatala A, Scott I, Deleemans JM, et al. Psychological distress and experiences of adolescents and young adults with cancer during the COVID-19 pandemic: a cross-sectional survey. Psychooncology. 2022;31(4):631–640. doi: 10.1002/pon.5849. [DOI] [PubMed] [Google Scholar]
- 22.Quinn GP, Gonçalves V, Sehovic I, Bowman ML, Reed DR. Quality of life in adolescent and young adult cancer patients: a systematic review of the literature. Patient Relat Outcome Meas. 2015;6:19–51. doi: 10.2147/prom.S51658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murnane A, Gough K, Thompson K, Holland L, Conyers R. Adolescents and young adult cancer survivors: exercise habits, quality of life and physical activity preferences. Support Care Cancer. 2015;23(2):501–510. doi: 10.1007/s00520-014-2446-2. [DOI] [PubMed] [Google Scholar]
- 24.Warner EL, Kent EE, Trevino KM, Parsons HM, Zebrack BJ, Kirchhoff AC. Social well-being among adolescents and young adults with cancer: a systematic review. Cancer. 2016;122(7):1029–1037. doi: 10.1002/cncr.29866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gil-Lacruz M, Gil-Lacruz AI, Gracia-Pérez ML. Health-related quality of life in young people: the importance of education. Health Qual Life Outcomes. 2020;18(1):187. doi: 10.1186/s12955-020-01446-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Fig. S1: Flowchart of the data collection process of the SURVAYA-COVID-19 study.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to privacy issues but are available from the corresponding author on reasonable request.