Abstract
Background
The adoption of virtual consultations, catalyzed by the COVID-19 pandemic, has transformed the delivery of primary care services. Owing to their rapid global proliferation, there is a need to comprehensively evaluate the impact of virtual consultations on all aspects of care quality.
Objective
This study aims to evaluate the impact of virtual consultations on the quality of primary care.
Methods
A total of 6 databases were searched. Studies that evaluated the impact of virtual consultations, for any disease, were included. Title and abstract screening and full-text screening were performed by 2 pairs of investigators. Risk of bias was assessed using the Mixed Methods Appraisal Tool. A narrative synthesis of the results was performed.
Results
In total, 30 studies (5,469,333 participants) were included in this review. Our findings suggest that virtual consultations are equally effective to or more effective than face-to-face care for the management of certain conditions, including mental illness, excessive smoking, and alcohol consumption. Overall, 4 studies indicated positive impacts on some aspects of patient-centeredness; however, a negative impact was noted on patients’ perceived autonomy support (ie, the degree to which people perceive those in positions of authority to be autonomy supportive). Virtual consultations may reduce waiting times, lower patient costs, and reduce rates of follow-up in secondary and tertiary care settings. Evidence for the impact on clinical safety is extremely limited. Evidence regarding equity was considerably mixed. Overall, it appears that virtual care is more likely to be used by younger, female patients, with disparities among other subgroups depending on contextual factors.
Conclusions
Our systematic review demonstrated that virtual consultations may be as effective as face-to-face care and have a potentially positive impact on the efficiency and timeliness of care; however, there is a considerable lack of evidence on the impacts on patient safety, equity, and patient-centeredness, highlighting areas where future research efforts should be devoted. Capitalizing on real-world data, as well as clinical trials, is crucial to ensure that the use of virtual consultations is tailored according to patient needs and is inclusive of the intended end users. Data collection methods that are bespoke to the primary care context and account for patient characteristics are necessary to generate a stronger evidence base to inform future virtual care policies.
Keywords: remote consultations, primary care, telemedicine, systematic review, teleconsult, quality care, efficiency, socioeconomic status
Introduction
Background
The onset of the COVID-19 pandemic in 2020 resulted in the rapid expansion of virtual consultations in primary care [1]. The shift from a primarily face-to-face (F2F) model of health care provision led to approximately 70% [2] and 65% [3] of primary care contacts happening virtually in the United Kingdom and United States, respectively.
Virtual consultations can be defined as real-time communication between patients and clinicians through telephone or videoconferencing [4]. It is argued that not only have virtual consultations helped minimize COVID-19 transmission, but they may also improve the efficiency of and access to care [5]. This may be particularly important in rural areas with geographical disparities in service provision [6] and resource-constrained settings with workforce shortages [4]. In addition, virtual care may improve patient-provider communication and engagement [7] and better facilitate multiperson involvement in care [8].
However, concerns have been raised over the speed at which virtual consultations were implemented, with both patients and clinicians reporting lack of confidence in the underlying technology and poorer clinical decision-making as key issues. [9]. Patients have expressed concerns regarding confidentiality, privacy, and the safety of their data [7,8]. Virtual care limits clinicians’ capacity to conduct physical examinations [10] and increases reliance on patients’ abilities to articulate their symptoms [5], posing potential safety risks. Moreover, those with limited access to technology or with lower digital literacy may be at risk of “digital exclusion” [11].
Previous reviews have investigated the impact of virtual consultations on the effectiveness [3,12-15] and efficiency [16,17] of care, often focusing on specific clinical conditions or taking broad definitions of remote services. However, there is a notable lack of systematic reviews assessing the impacts on safety, patient-centeredness, timeliness, and equity, with much of the existing literature limited to scoping or rapid reviews of the evidence [18-21]. Furthermore, although some systematic reviews investigated the impact of virtual care on aspects of quality exclusively in primary care settings [13,16,17,22], others examined heterogeneous evidence, including data on interventions delivered in secondary care facilities or by specialists [3,15]. There is, therefore, a need to comprehensively evaluate the impact on all aspects of care quality specifically in primary care settings.
Aim of This Review
The aim of this review was to systematically evaluate the impact of virtual consultations on the quality of primary care. We chose to use the Institute of Medicine (IOM)’s theoretical framework to map the impact across 6 domains of quality, including efficiency, effectiveness, safety, patient-centeredness, timeliness, and equity [23]. This widely accepted model for describing care quality has been previously used in other systematic reviews investigating the effects of digital health interventions on the quality of care [24,25]. When evaluating the impact of virtual consultations on quality, it is essential that all quality domains are assessed, as what is beneficial in one domain may be detrimental in another. Therefore, the IOM’s quality of care framework provides a comprehensive model for evaluating the impact of virtual consultations across all aspects of care quality.
Methods
This systematic review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist [26]. The study protocol was registered with the International Prospective Register of Systematic Reviews (CRD42022362380).
Search Strategy
Six databases (MEDLINE, Embase, HMIC, PsycINFO, CINAHL, and Cochrane) were searched on June 20, 2022. The search included studies published between January 2017 and June 2022, as the last 5 years have seen most of the shift toward virtual care. Concepts covered in the search strategy primarily included (1) virtual consultations, (2) primary care, and (3) the IOM’s 6 domains of care. The concepts of virtual consultations and primary care were intentionally kept broad to address variations in language, and search terms for the domains of quality were adapted from a previous review [24].
A detailed breakdown of the exact combination of free text and Medical Subject Headings terms used can be found in Multimedia Appendix 1. The reference lists of relevant systematic reviews and gray literature sources were also screened.
Study Selection Criteria
Studies were included if they focused on adult patients accessing primary care services (including care homes), involved telephone or videoconference consultations delivered by health care professionals, compared outcomes with F2F consultations, and reported outcomes that fit under any of the IOM’s quality of care domains. Detailed descriptions of the inclusion and exclusion criteria are provided in Textboxes 1 and 2, respectively. Studies focusing on specific health conditions were not excluded to characterize the general use of virtual consultations in primary care.
Inclusion criteria.
Population (and setting)
Adult patients (mean age ≥18 y) with any health condition accessing primary care services in any geographical location
Intervention
Two-way, synchronous patient-provider virtual consultations delivered via telephone or videoconference by primary care health care professionals or multicomponent interventions involving synchronous remote consultations
Comparator
Consultation delivered face-to-face or the outcomes assessed indicate comparison with previous experience of face-to-face care (survey questions)
Outcomes
Studies reporting any quantitative measures related to (1) efficiency (eg, service costs and follow-up care), (2) effectiveness (eg, health outcomes), (3) patient safety (eg, misdiagnoses), (4) patient-centeredness (eg, patient satisfaction measures), (5) timeliness (eg, wait times), and (6) equity (eg, disparities in access or outcomes between different patient subgroups)
Study type
Randomized controlled trials, cluster randomized trials, quasi-experimental studies, case-control studies, cohort studies, cross-sectional studies, and cost-effectiveness studies
Exclusion criteria.
Population (and setting)
Patients accessing secondary, tertiary, or quaternary care; direct-to-consumer services; care delivered in retail clinics; or care that is not integrated into primary care
Intervention
Consultations involving only asynchronous communication, synchronous web-based messaging, remote patient monitoring, automated services, or interventions for education or administrative purposes; consultations delivered by non–health care professionals or specialist clinicians; or consultations delivered in retail clinics or via direct-to-consumer models
Comparator
No face-to-face comparison group or no indication of comparison with face-to-face care
Outcomes
Studies reporting only qualitative outcomes; studies reporting outcomes that do not fit under any of the Institute of Medicine’s quality framework domains; or studies evaluating only prescribing outcomes, as changes in prescription patterns are not necessarily reflective of the quality of care and are highly context-specific
Study type
Incomplete studies, commentary articles, systematic reviews, interim reports, scoping reviews, case series, case reports, opinion pieces, or trial protocols
Screening and Data Extraction
Duplicates were automatically excluded using Covidence web-based screening software (Veritas Health Innovation [27]). During the subsequent title, abstract, and full-text screening processes, the decision to exclude a study was made through consensus between the first and second independent reviewers. Iterative meetings were held to discuss any discrepancies that arose. Only when consensus was not able to be reached, a third reviewer, the most senior member of the research team, made the final decision. Cohen κ was used to measure the intercoder agreement in title and abstract screening and full-text screening (0.22 and 0.65, respectively). Disagreements were resolved through discussion with a third investigator. Data extraction was conducted using a standardized data extraction form (Multimedia Appendix 2). Effect sizes such as mean differences, odds ratios, and risk ratios were extracted. Where available, the rates of intervention adherence, follow-up, and survey response were also extracted.
Risk of Bias Assessment
Risk of bias was assessed using the Mixed Methods Appraisal Tool (version 18) [28] by 2 independent reviewers (Multimedia Appendix 3 [29-58]). Disagreements were resolved through consensus with a third reviewer. A study was considered high risk if it scored “yes” in ≤2 dimensions, moderate risk if it scored “yes” in 3 dimensions, and low risk if it scored “yes” in 4 or all dimensions.
Data Synthesis
A narrative synthesis of the selected studies was performed. The overall characteristics of the included studies are summarized. Pertinent findings across the studies were mapped onto the IOM framework to comprehensively illustrate the evidence for all the quality of care domains. For each domain, relevant outcome data were compiled into summary tables to facilitate the comparison of results across the studies (Multimedia Appendix 4 [29,30,32-34,36,37,41-45,50,51,53,56], Multimedia Appendix 5 [31,36,42,54,55,57,58], Multimedia Appendix 6 [29,45,46,50,52], Multimedia Appendix 7 [39,40,57], and Multimedia Appendix 8 [35,38,43,47-49]). The key findings for the 6 IOM care quality domains are presented.
Results
Search Results
Our initial searches retrieved a total of 6272 records (Figure 1). After title, abstract, and full-text screening, 30 (0.48%) papers met the inclusion criteria. No relevant records were found from searching gray literature or from the reference lists of relevant articles.
Figure 1.
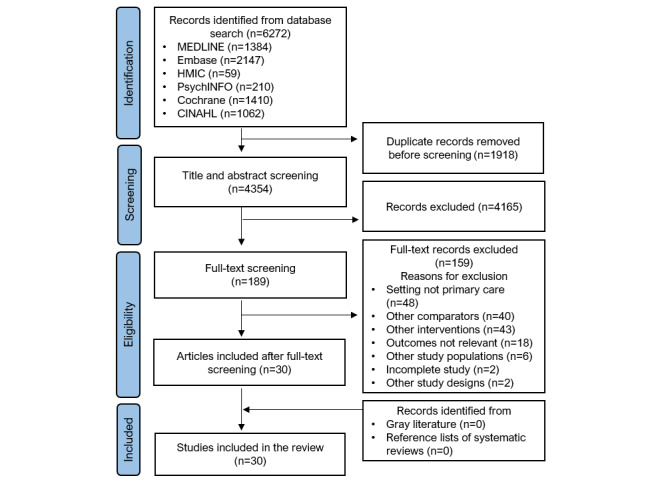
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the included studies.
Description of the Included Studies
The 30 included studies (Table 1) comprised a total of 5,469,333 participants. Sample sizes ranged from 28 [29] to 1,490,734 [30] participants, and publication year ranged from 2017 to 2022. The 30 studies included 14 (47%) retrospective cohorts [30-43], 6 (20%) cross-sectional studies [44-49], 4 (13%) quasi-experimental studies [29,50-52], 3 (10%) randomized controlled trials (RCTs) [53-55], 2 (7%) cohort studies [56,57], and 1 (3%) cluster RCT [58]. Most studies were conducted in the United States (20/30, 67%) [30-34,36-44,46-49,53,58], whereas the rest were conducted in Australia (2/30, 7%) [35,45], Canada (2/30, 7%) [50,52], Kenya (1/30, 3%) [54], the United Kingdom (1/30, 3%) [51], Japan (1/30, 3%) [55], Singapore (1/30, 3%) [29], New Zealand (1/30, 3%) [56], and Sweden (1/30, 3%) [57].
Table 1.
Characteristics of the included studies.
| Study, year | Country | Time period | Study design | Participants (setting) | Sample size (N) | Study design | Consultation description | Risk of bias |
| Baughman et al [31], 2023 | United States | April 2020-September 2021 | Retrospective cohort study | Primary care patients aged 26 to 70 years with abnormal BMI scores (<18.5 or >25 kg/m2) | 287,387 (VCa: 1556; blended: 63,489; F2Fb: 222,333) | Comparison of outcomes among initial visit modalities: VC (Zoom [Zoom Video Communications, Inc] video), blended VC (patients with VC and F2F visits within the time frame), and F2F | Initial BMI screening visits | Moderate |
| Baughman et al [32], 2022 | United States | July 2019-June 2021 | Retrospective cohort study | Primary care patients aged 18 to 50 years with a lower back pain diagnosis | 20,624 (VC: 5334; F2F: 15,290) | Comparison of outcomes between initial visit modalities: VC (Zoom video) and F2F | Initial primary care consultation | Moderate |
| Befort et al [58], 2021 | United States | February 2016-October 2017 | Cluster RCTc | Primary care patients aged 20 to 75 (mean age 54.7; SD 11.8) years with BMI scores of 30 to 45 residing in rural locations | 1407 (group VC: 466; individual F2F: 473; group F2F: 468) | Practices (n=36) randomly assigned to group VC (telephone conference call), group F2F, and individual F2F | Individual F2F: 15-minute behavioral therapy; group VC and F2F: 60-minute group behavioral therapy (14 patients/group) | Moderate |
| Bernstein et al [33], 2021 | United States | November 2015-March 2019 | Retrospective cohort study | Ambulatory care patients aged >60 years with urgent or nonemergent conditions | 1088 (VC: 115; F2F: 973) | Comparison of outcomes between index visit modalities: VC (video) and F2F | Visit with physician, including clinical assessment, prescriptions, or referrals if appropriate | Moderate |
| Chavez et al [34], 2022 | United States | April 2019-March 2021 | Retrospective cohort study | Patients (mean age 54.1; SD 17.8 y) accessing general care at an academic family medicine practice | 57,006d (VC: 7577; F2F: 49,429) | Comparison of outcomes between index visit modalities: VC (video or telephone) and F2F (stratified by prepandemic and pandemic time frames) | Consultation with a physician | High |
| Dai et al [35], 2022 | Australia | March 2020-August 2021 | Retrospective cohort study | Geriatric primary care patients (general care) aged >65 years in residential aged care facilities | 27,980 | Assessment of the associations between sociodemographic characteristics and visit modality: VC (video or telephone) or F2F | GPe consultation | Low |
| Egede et al [53], 2017 | United States | September 2006-October 2012 | RCT | Older veterans aged >58 years (mean age 63.9; SD 5.1 y) with depression | 241 (VC: 120; F2F: 121) | Comparison of outcomes between consultation modalities: VC (videophone) and F2F | 60-minute behavioral activation for depression delivered weekly for 8 weeks | Moderate |
| Frank et al [36], 2021 | United States | March 2019-December 2020 | Retrospective cohort study | Patients with mental health conditions at an academic primary care practice aged 4 to 73 (mean age 28.32, SD 15.46) years | 173 | Comparison of outcomes between 2 waves of consultation modalities: VC (video or telephone; March-December 2020) and F2F (March-December 2019) | 30-minute mental health appointments | High |
| Gordon et al [37], 2017 | United States | January 2014-May 2015 | Retrospective cohort study | Primary care patients aged <65 years receiving care for acute, nonurgent conditionsf | 18,516 (VC: 4635; F2F: 13,881) | Comparison of outcomes between consultation modalities: VC and F2F | Primary care consultations | Moderate |
| Govier et al [38], 2022 | United States | March 2019-July 2021 | Retrospective cohort study | Primary care patients aged >18 years diagnosed with COVID-19 between March and July 2020 | 11,326 (VC: 1360; F2F: 9966) | Assessment of the associations between sociodemographic characteristics and visit modality: VC or F2F | Primary care consultations | Moderate |
| Graetz et al [39], 2022 | United States | January 2016-May 2018 | Retrospective cohort study | Primary care patients of all ages (22.2%>65 y; general care) | 1,131,722 | Comparison of outcomes among consultation modalities: VC (video), VC (telephone), and F2F | Primary care consultations requested by patients using a web-based portal | Moderate |
| Haderlein et al [40], 2022 | United States | March 2018-October 2021 | Retrospective cohort study | Veterans (mean age 48.7, SD 16.4 y) seeking mental health care in an urban VAg primary care mental health integration clinic | 2479 | Comparison of outcomes between consultation modalities: VC (video or telephone) and F2F | Primary care mental health consultations | Low |
| Harder et al [54], 2020 | Kenya | September 2014-December 2015 | RCT | Primary care patients (mean age 38 y) with alcohol use disorders in rural primary health center | 300 (VC: 104; F2F: 92; waitlist control: 104) | Comparison of outcomes among consultation modalities: VC (mobile phone call), F2F, and waitlist control | One 30-minute motivational interviewing session | High |
| Li et al [30], 2022 | United States | June 2019-September 2020 | Retrospective cohort study | Primary care patients (mean age 39.2, SD 22.2 y; general care) | 1,490,734 | Comparison of outcomes among different levels of VC use in medical practice: high VC use, medium VC use, and low VC use | Primary care consultations | High |
| Lovell et al [44], 2021 | United States | April 2016-March 2017 | Retrospective cohort study | Primary care patients aged <64 years accessing care for low-acuity, urgent conditionsh | 5919 (VC: 1531; F2F: 4388) | Comparison of outcomes between consultation modalities: VC (video call) and F2F | Primary care consultations | High |
| Manski-Nankervis et al [45], 2022 | Australia | October 2020-May 2021 | Descriptive cross-sectional study | Primary care patients (mean age 31.8, SD 11.4 y) who completed a videoconference call with a health care professional (general care) | 499 | Web-based survey on the experience with the most recent VC visit (videoconference) in comparison with past experiences of F2F visit | Primary care consultations | High |
| McGrail et al [50], 2017 | Canada | 2013-2014 | Quasi-experimental (interrupted time series) study with a cross-sectional survey component | Primary care patients aged >18 years living in British Colombia (general care) | Interrupted time series: 29,267 (VC: 7286; F2F: 21,981); survey: 399 | Comparison of outcomes between consultation modalities: VC and F2F; web-based survey on the experience with the most recent VC visit in comparison with past experiences of F2F visit | Primary care consultations | Moderate |
| Miller et al [51], 2019 | United Kingdom | June 2014-May 2017 | Quasi-experimental (interrupted time series) study | Primary care patients of all ages at an urban general practice in a socioeconomically deprived area (general care) | 27,589 (VC: 9113; F2F: 18,476) | Comparison of outcomes between the 2 study phases: F2F (preintervention phase) and VC (telephone-first phase) | Primary care consultations | Moderate |
| Mohan et al [46], 2022 | United States | April-December 2020 | Descriptive cross-sectional study | Primary care patients (mean age 48.7, SD 17.67 y) at an academic medical center (general care) | 797 | Web-based survey on the experience with the most recent VC visit in comparison with past experiences of F2F visit | Primary care consultations | High |
| Neufeld et al [52], 2022 | Canada | September 2020-February 2021 | Quasi-experimental study | Primary care patients aged 18 to 87 years (general care) | 66 (VC: 32; F2F: 34) | Comparison of outcomes between consultation modalities: VC (telephone) and F2F | Family physician consultations | Moderate |
| Nomura et al [55], 2019 | Japan | March-June 2018 | RCT | Primary care patients (mean age 55, SD 11 y) with nicotine dependence | 115 (VC: 58; F2F: 57) | Comparison of outcomes between consultation modalities: VC (internet-based video call) and F2F | 5 sessions of smoking cessation counseling over 24 weeks with access to a smoking cessation mobile app and an exhaled COi checker | Low |
| Pierce and Stevermer [47], 2023 | United States | March-April 2020 | Analytical cross-sectional study | Primary care patients (mean age 45 y) at an academic family medicine center (general care) | 6984 | Assessment of the associations between sociodemographic characteristics and visit modality: VC (audio or video) or F2F | Family medicine consultations | High |
| Quinton et al [48], 2021 | United States | March 2019-March 2021 | Analytical cross-sectional study | Patients aged >18 years presenting for ambulatory visits at a rural health care provider (general care) | 54,559 | Assessment of the associations between patient characteristics and visit modality: VC (audio or video) or F2F | Ambulatory care visits | Moderate |
| Reed et al [49], 2020 | United States | January 2016-May 2018 | Analytical cross-sectional study | Primary care patients of all ages at a large integrated health care delivery system (general care) | 1,131,722 | Assessment of the associations between patient characteristics and visit modality: VC (telephone or video) and F2F | Index primary care consultations (no visits within the past 7 days) | Moderate |
| Reed et al [41], 2021 | United States | January 2016-May 2018 | Retrospective cohort study | Primary care patients of all ages (mean age 43, SD 22 y) at a large integrated health care delivery system (general care) | 1,131,722 | Comparison of outcomes between consultation modalities: VC (telephone or video) and F2F | Index primary care consultations (no visits within the past 7 days) | Moderate |
| Rene et al [42], 2022 | United States | October 2019-May 2020 | Retrospective cohort study | Primary care patients aged >18 years with depression, anxiety, or both | 338 (VC: 181; F2F: 157) | Comparison of outcomes between consultation modalities: VC (pandemic cohort: April-May 2020) and F2F (prepandemic cohort: October-November 2019) | Initial behavioral health consultation, followed by 30-minute visits for behavioral activation, motivational interviewing, and psychoeducation | Moderate |
| Ryskina et al [43], 2021 | United States | March 2020-May 2020 | Retrospective cohort study | Primary care patients aged >65 (mean age 75.1, SD 7.5 y; general care) | 17,103 (VC: 10,311; F2F: 6792) | Comparison of outcomes between consultation modalities: VC (telephone or video) and F2F | Primary care consultations | Moderate |
| Tan et al [29], 2022 | Singapore | April 2019-May 2019 | Quasi-experimental (prospective and self-controlled) study | Active military servicemen (93% aged 18-24 y) accessing primary care at a military medical center (general care) | 28 | Comparison of outcomes between consultation modalities: VC (on-premises Zoom video) and F2F (immediately following VC) | Primary care consultations with an assistant present to perform auscultations and physical examinations; a symptom collection app was used before VC, and the collected data were available to the VC physician | Moderate |
| Ure [56], 2022 | New Zealand | May-July 2021 | Cohort study | Primary care patients of all ages (25% aged <5 y) at a general practice medical center (general care) | 454 (VC: 133; F2F: 321) | Comparison of outcomes between consultation modalities: VC and F2F | Primary care consultations following triage via telephone | Moderate |
| Wickström et al [57], 2018 | Sweden | October 2014-September 2016 | Cohort study | Primary care patients (VC: mean age 77, SD 13 y; F2F: mean age 75, SD 14 y) with hard-to-heal ulcers | Healing time study: 1988 (VC: 100; F2F: 1888); waiting time study: 200 (VC: 100; F2F: 100) | Comparison of outcomes between consultation modalities: VC (Skype [Skype Technologies] video) and F2F | Consultations involved ulcer diagnosis and discussion of the treatment strategy | Moderate |
aVC: virtual consultation.
bF2F: face-to-face.
cRCT: randomized controlled trial.
dNumber of index visits (number of participants was not reported).
eGP: general practitioner.
fConditions included sinusitis, upper respiratory infection, urinary tract infection, conjunctivitis, bronchitis, pharyngitis, influenza, cough, dermatitis, digestive symptoms, and ear pain.
gVA: Veterans Affairs.
hConditions included sinusitis, conjunctivitis, urinary tract infection, upper respiratory infection, influenza or pneumonia, bronchitis, dermatitis or eczema, ear pain, digestive symptoms, and cough.
iCO: carbon monoxide.
Studies considered patients with a range of health conditions (ie, mental illnesses [36,40,42,53]; urgent and nonemergent conditions [33,44]; overweight and obesity [31,58]; lower back pain [32]; alcohol use disorders [54]; nicotine dependence [55]; hard-to-heal ulcers [57]; and acute, nonurgent conditions [37]). The remaining studies (17/30, 57%) considered primary care users in general. All consultations were delivered in primary care settings. Of the 30 included studies, 3 (10%) studies specified occurring in rural locations [48,54,58], and 1 (3%) study was conducted in an urban, socioeconomically deprived area [51].
Summary of the Risk of Bias Assessment
Of the 30 included studies, 19 (63%) studies had a moderate risk [29,31-33,37-39,41-43,48-53,56-58], 3 (10%) had a low risk [35,40,55], and 8 (27%) had a high risk of bias [30,34,36,44-47,54] (Figure 2). For quantitative descriptive studies, the main sources of bias were poor sample representativeness and risk of nonresponse bias (ie, potential lower engagement from those with lower digital literacy) [45,46,50]. Main sources of bias for RCTs included issues with blinding [54,55,58], low or unclear adherence to the intervention [53,54,58], lack of details on randomization [54], and differences between groups at baseline [53]. Nonrandomized studies had globally a high risk of bias stemming from the uncertain accuracy of the measurements of exposure and outcome [30-35,37,38,41,44,47-49], unaccounted confounders [30,32,33,43,44,47,48], the overrepresentation of certain subgroups [52], and selection bias [39,41,49].
Figure 2.
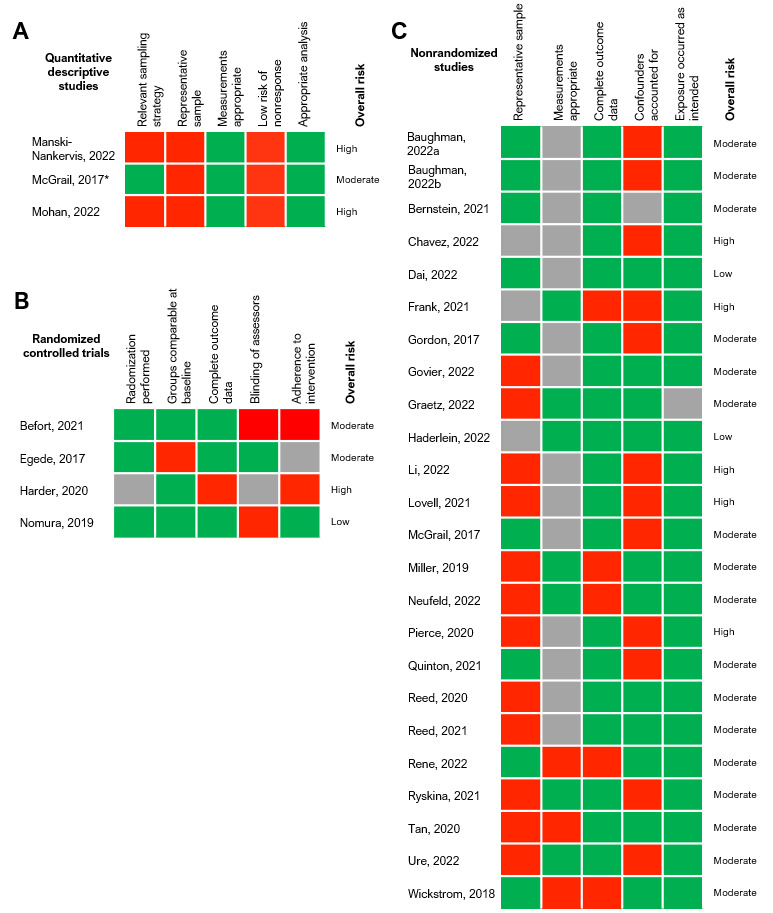
Risk of bias assessments [29-58]. Cells were color coded green for “yes,” gray for “can’t tell,” and red for “no.” *The study by McGrail et al [50] is categorized as both a quantitative descriptive study and nonrandomized trial because of the 2 distinct cross-sectional survey and quasi-experimental components of the study.
Interventions
Of the 30 included studies, 4 (13%) investigated only telephone consultations [51,52,54,58], and 10 (33%) assessed consultations delivered only via videoconference using a range of platforms (ie, Skype [Skype Technologies], Zoom [Zoom Video Communications, Inc], video call, or bespoke telehealth portals) [29,31-33,44-46,53,55,57]. The remaining 16 (53%) of the 30 studies considered consultations via both telephone and videoconference as interventions. In almost all studies, the consultations were the first in an episode of care. Other studies consisted follow-up consultations, including behavioral therapy [42,53,58], motivational interviewing [54], and smoking cessation counseling [55].
Outcomes
Overview
A summary of the main findings of this study can be found in Table 2.
Table 2.
Summary of the main findings.
| Domain of quality | Main findings |
| Efficiency |
|
| Effectiveness |
|
| Safety |
|
| Patient-centeredness |
|
| Timeliness |
|
| Equity |
|
aF2F: face-to-face.
bSES: socioeconomic status.
Efficiency
Of the 30 included studies, 16 (53%) evaluated outcomes related to efficiency [29,30,32-34,36,37,41-45,50,51,53,56], including rates of follow-up visits and hospitalizations, patient costs, and appointment characteristics (ie, length, attendance, cancelation, and no-shows; Multimedia Appendix 4). Of these 16 studies, 11 (69%) found a positive impact (n=6, 55%) or no impact (n=5, 45%) on efficiency in at least half of the outcomes extracted [29,32,36,37,41,43-45,50,51,53]. Of the 8 studies comparing rates of follow-up visits in primary care, 5 (63%) found that virtual consultations resulted in a greater need for additional care [33,34,41,44,56], whereas 3 (38%) found no differences [37,50,51].
Out of 7 studies evaluating the rates of follow-up consultations in secondary or tertiary care, 3 (43%) found no changes in the rates of emergency department follow-up visits or hospitalizations [41,44,51]; 3 (43%) other studies [37,43,50] found a significant reduction in follow-up visits after a virtual consultation (including emergency department visits [37], hospitalizations [37,43], and ambulatory care sensitive condition visits [43]); and only 1 (14%) study found that high use of virtual consultations was associated with more annual ambulatory care sensitive condition visits compared with low use of virtual consultations [30].
In terms of appointment characteristics, one study found that virtual consultations led to a higher number of appointments attended and fewer cancelations [36]. However, another study reported lower rates of attendance and increased cancelations in the context of mental health appointments that took place remotely during the pandemic [42]. One study found that the use of virtual consultation and a symptom checker app resulted in a shorter appointment duration when compared with F2F care [29]. Finally, 4 (80%) out of the 5 papers assessing the impact on patient costs demonstrated a reduction in the costs associated with virtual consultations compared with F2F visits [37,44,45,50].
Effectiveness
Among the 30 included studies, 7 (23%) assessed the effectiveness of virtual consultations (Multimedia Appendix 5). Of these 7 studies, 6 (86%) found a noninferior impact on effectiveness for at least half of the outcomes [36,42,54,55,57,58]. Furthermore, 2 studies investigating the effectiveness of virtual mental health care in improving anxiety and depression symptoms also demonstrated its noninferiority [42] or superiority [36] to F2F care. Virtual consultations were found to be more effective for the care of hard-to-heal ulcers [57] and as effective as F2F care for reducing alcohol consumption [54], abstinence from smoking [55], and weight management [58].
Safety
From the total 30 studies, only 1 (3%) small study (with 28 participants) considered outcomes related to the safety of care, finding an overall diagnostic agreement rate of 92% between virtual and F2F assessments [29]. The agreement rate was 100% for headache, gastroenteritis, and conjunctivitis but lower for dermatological conditions and upper respiratory tract infections (87.5% and 93.3%, respectively) [29].
Patient-Centeredness
Of the 5 studies assessing the impact on patient-centeredness, 4 (80%) indicated that virtual care had a positive or equivalent effect compared with F2F care (Multimedia Appendix 6). One (20%) of the studies found that those seen virtually reported lower perceived autonomy support [52]. Three (60%) studies asked patients to compare their recent virtual consultations with past experiences of F2F care [45,46,50], with most respondents agreeing that virtual care was “as good” (84%) [45] and “as thorough” (79%) [50] as F2F care, more convenient (91%) than F2F care, and of equal value to or better value than (67%) F2F care [46]. In another study, most patients (39.9%) had no preference regarding the consultation modality [29].
Timeliness
Of the 3 studies evaluating the impact on timeliness, 2 (67%) found an improvement when consultations were delivered virtually (Multimedia Appendix 7). Graetz et al [39] reported that both video and telephone consultations were more likely to occur within 1 day of scheduling. Similarly, a study at a wound healing clinic found that virtual consultations took place significantly sooner after referral [57]. By contrast, a study at a primary care mental health clinic reported that patients who were initially assessed virtually were less likely to receive same-day mental health care [40].
Equity
Out of the 30 studies, 6 (20%) assessed the impact on the equity of care through stratification of the use of services based on sex, age, ethnicity, socioeconomic status (SES), and rural or urban residence (Multimedia Appendix 8). Of the 5 studies comparing service use by sex, 2 (40%) studies found that women were more likely to use virtual care than men [47,49]. Regarding age, 2 (n=4, 50%) studies reported that the likelihood of having virtual consultations decreased with increasing age [35,49]. Interestingly, 1 (n=4, 25%) study performed in the first month of the pandemic found that those aged >65 years were more likely to have virtual consultations than those aged 18 to 44 years [47].
Lower use of virtual consultations was reported to be associated with both lower [48,49] and higher SES [35,47]. Notably, 2 (n=5, 40%) studies found that those of lower SES were less likely to have video consultations than they were to have telephone consultations [47,49].
Findings regarding the impact of ethnicity on the use of virtual care were also mixed. Among the 5 studies investigating this, 2 (40%) suggested that Black patients were less likely to use virtual consultations than White patients [47,48], whereas 3 (60%) other studies found the opposite effect [38,43,49]. Asian patients residing in the United States were more likely to use video consultations than White patients but were slightly less likely to use telephone consultations [49].
Finally, a US study reported that patients living in rural areas had lower virtual care use [47], whereas an Australian study found the inverse effect [35].
Discussion
Summary of the Main Findings
Our findings suggest that virtual consultations are equally effective to or more effective than F2F care for the management of conditions, including mental illness, excessive smoking, and alcohol consumption. Evidence for the impact on clinical safety is extremely limited. Only 5 studies investigated patient-centeredness, and of these, 4 (80%) found positive impacts on some aspects of patient-centeredness; however, a negative impact was noted on patients’ perceived autonomy support (ie, the degree to which people perceive those in positions of authority to be autonomy supportive). Virtual consultations may reduce waiting times, lower patient costs, and reduce rates of follow-up in secondary and tertiary care settings. However, there is evidence that virtual consultations may increase the need for additional general practitioner visits compared with F2F consultations. Evidence regarding equity was considerably mixed. Overall, it appears that virtual care is more likely to be used by younger, female patients, with disparities among other subgroups depending on contextual factors.
Interpretation of the Findings in the Context of Previous Research
Efficiency
The indication that virtual consultations may increase the rate of follow-up visits in primary care is consistent with previous evidence [3,16]. This negative impact on efficiency may to some extent be explained by the time frames during which the studies were conducted. In those occurring shortly after the onset of the pandemic [34,56], when the rapid transition to virtual care was necessary, the increased rate of follow-up may be a consequence of lower clinician or patient confidence in virtual care owing to its initial unfamiliarity [37].
Previous reviews have not specifically assessed the impact of virtual consultations on follow-up at the secondary or tertiary levels of care. This review’s finding that they may reduce or have no impact on follow-up at these higher levels of care might be explained by retrospective study designs precluding adequate adjustment for confounders and by the heterogeneity of the interventions included [33,37,41,43].
The finding that virtual care may be associated with lower patient costs is in line with previous research [3,17]. Although this evidence is most relevant to countries in which patients pay for services out of pocket, it appears that patients accessing publicly funded health systems may also financially benefit from virtual care, mainly because of reductions in travel expenses and time costs from loss of work [3,44,45]. Furthermore, this review and wider evidence indicate that virtual consultations are generally shorter than F2F visits [3,16,29]. The decrease in consultation length reported by Tan et al [29] may be explained by the use of a symptom checker app before the virtual consultation, which could have improved efficiency for clinicians. However, it is so far unclear whether shorter appointments are indeed more cost-effective than longer appointments and whether they allow enough time for patients to discuss more complex matters.
Effectiveness
Virtual care seems to be as effective as F2F visits for certain clinical outcomes (ie, depression and anxiety symptoms, alcohol use disorder scores, smoking abstinence rates, and ulcer healing times). Existing reviews have similarly found noninferior outcomes when virtual care was delivered by specialists [3,12], combined with remote patient monitoring [13], or offered in addition to F2F care [15]. However, this study suggests that virtual consultations may be an effective substitute for F2F consultations in primary care settings.
Patient-Centeredness
The wider literature has reported similarly positive findings in terms of patient satisfaction across various types of secondary care and remote patient monitoring for diabetes. [18,19]. One possible explanation is that the use of virtual consultations can lead to less time pressure for physicians and more patient-centric consultations. However, the notable positive impact on patient-centeredness (ie, convenience and preference) should be interpreted with caution owing to the significant risk of bias in these studies and the heterogeneity of measures used. Many of the included studies relied on nonvalidated surveys to assess satisfaction. In this review, the only study using validated questionnaires found that virtual care led to lower perceived autonomy support, possibly because of the absence of nonverbal cues and decreased relational competence [52].
Timeliness
There is some evidence that opting for virtual care may reduce wait times for initial consultations compared with F2F care [39,57], possibly facilitated by removing the barriers of job flexibility and travel times [39]. Shorter wait times are a key benefit of virtual care perceived by patients [21]. However, the finding that wait times for mental health care were increased following a virtual appointment may reflect the possibility that patients with lower clinical need chose virtual consultations to begin with (and thus their concerns were assessed as less urgent) or indicate logistical issues in transitions of care [40].
Equity
Our findings regarding age and sex are in line with previous research [22] and reflect older patients’ lower average digital literacy and access to technology [47]. Evidence concerning the impacts of SES, ethnicity, and location of residence on the use of virtual care was inconsistent across studies, potentially because of differences in populations and study settings. To this end, access to and use of care are highly context-specific and will be shaped by both community- and practice-level features. As engagement and participation in care are generally lowest for socially disadvantaged populations, disentangling the patient characteristics that may exclude them from virtual care services, at the local level, is essential.
Safety
Limited conclusions can be drawn regarding the safety of virtual consultations, as only 1 (n=30, 3%) study investigating outcomes in this domain was identified in this review.
Strengths and Limitations
This study provides insight into the recent changes in the delivery of primary care and the impact of virtual consultations on care quality. The review uses the IOM’s comprehensive quality framework and maps findings to this model, lending a structured approach to the evaluation of the impact of virtual consultations.
This review did not consider pediatric populations, care delivered by non–health care professionals (eg, community health workers), or outcomes related to medication prescriptions. Many of the included studies considered patients who were part of specific subpopulations, such as older veterans [53] or young military servicemen [29], which may limit the generalizability of the findings.
Eligible studies were restricted to those published within the last 5 years; although this time frame was considered reasonable in line with the changing health care landscape, this might have potentially led to some earlier papers being missed. The decision to conduct the literature search only up to June 2022 may have excluded some more recently studies published in the past year. However, this should not substantially impact our review’s findings, given that it is largely in line with the median time of approximately 8 months as reported in other literature reviews [25].
It is important to note that this study was neither specifically designed to evaluate changes after the COVID-19 pandemic nor optimized to detect those differences. In addition, the studies that covered the COVID-19 pandemic were conducted when the pandemic was in its early stages and, therefore, cannot provide additional information on how the pandemic accelerated adoption, or its impact, after the COVID-19 pandemic.
All but one of the included studies were from high-income countries, and most were from the United States, highlighting the lack of research from low- and middle-income countries. Therefore, many of the findings of this review will have limited relevance outside of the United States and certainly will lack generalizability in low-income regions with dissimilar health system financing structures or technological infrastructure. The lack of studies evaluating safety aspects, such as medication safety incidents, demonstrates the gap in knowledge previously highlighted by Gleeson et al [20]. Similarly, current evidence has common limitations of bias introduced through the lack of adjustment for confounders and selection bias toward the inclusion of patients with greater digital literacy or engagement with health care.
Finally, the apparent lack of studies investigating the effectiveness of virtual care for a wider range of morbidities in primary care highlights a key area for further research.
Implications for Research, Policy, and Practice
Although evidence of improved efficiency is likely to keep driving the implementation of virtual care, it is critical to ensure that the transition to new service delivery models does not pose additional patient harm. However, even within this domain, the results were sometimes broad and unspecific, making it difficult for readers to contextualize the reported findings. Future research could benefit from a more focused approach when defining the contexts in which evaluations were taking place to aid in the generalizability of the insight gained. The apparent lack of studies investigating the safety of virtual consultations highlights a concerning gap in the literature, and future evaluations should focus on the evaluation of diagnostic error and medication safety in this context. Furthermore, health technology assessments investigating the impact on patient-centeredness should capitalize on the use of validated patient-reported measures whenever possible to allow a rigorous comparative approach.
Policy efforts to support improvements in data collection in primary care (ie, consultation type, duration, and quality outcomes) will be critical to developing a strong evidence base capitalizing on real-world data. The mixed findings on the impact on equity highlight the need for investigations at the local level, which will be vital to develop context-specific strategies tailored to community health needs and characteristics. Data collection should adopt an intersectional approach, considering a breadth of patient characteristics, to inform the design of locally appropriate interventions and ensure equitable access to care. Importantly, virtual consultation interventions and access schemes must incorporate participatory approaches in their research and design, encouraging input from marginalized voices and including community knowledge, values, and preferences in decision-making processes.
Acknowledgments
This work is independent research supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration Northwest London. ALN and EL are also funded by NIHR Patient Safety Research Collaborative, with infrastructure support from Imperial NIHR Biomedical Research Centre. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or Department of Health and Social Care. The funders did not play a role in the study design; collection, analysis, or interpretation of data; manuscript writing; or decision to submit for publication. The researchers were independent of the funders. All authors had full access to all the data included in this study and can take responsibility for the integrity of the data and accuracy of the data analysis.
Abbreviations
- F2F
face-to-face
- IOM
Institute of Medicine
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
randomized controlled trial
- SES
socioeconomic status
MEDLINE search strategy and gray literature search.
Data extraction form template.
Mixed Methods Appraisal Tool assessment with justifications for decisions.
The efficiency of virtual versus face-to face consultations.
The effectiveness of virtual versus face-to-face consultations.
The impact of virtual consultations on patient-centeredness.
The timeliness of virtual versus face-to-face consultations.
The impact of virtual consultations on the equity of care.
Data Availability
The search strategy and extracted data contributing to the narrative synthesis are available as multimedia appendices. Any additional data are available on request.
Footnotes
Authors' Contributions: KC, EL, NO, and ALN performed the study selection and reviewing processes. KC, GG, and ALN wrote the first manuscript. All the authors reviewed, edited, and approved the version of the manuscript submitted for publication.
Conflicts of Interest: BH is an employee of eConsult Health Ltd, a provider of electronic consultations for National Health Service primary, secondary, and urgent and emergency care. All other authors declare no other conflicts of interest.
References
- 1.Dhaliwal JK, Hall TD, LaRue JL, Maynard SE, Pierre PE, Bransby KA. Expansion of telehealth in primary care during the COVID-19 pandemic: benefits and barriers. J Am Assoc Nurse Pract. 2021 Jun 07;34(2):224–9. doi: 10.1097/JXX.0000000000000626.01741002-900000000-99379 [DOI] [PubMed] [Google Scholar]
- 2.GP consultations post-COVID should be a combination of remote and face to face, depending on patient need, says College. Royal College of General Practitioners. 2021. May 11, [2022-07-10]. https://www.rcgp.org.uk/news/2021/may/gp-consultations-post-covid .
- 3.de Albornoz SC, Sia KL, Harris A. The effectiveness of teleconsultations in primary care: systematic review. Fam Pract. 2022 Jan 19;39(1):168–82. doi: 10.1093/fampra/cmab077. https://europepmc.org/abstract/MED/34278421 .6323555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kadir MA. Role of telemedicine in healthcare during COVID-19 pandemic in developing countries. Telehealth Med Today. 2020 Apr 30;5(2):1–5. doi: 10.30953/tmt.v5.187. [DOI] [Google Scholar]
- 5.Colbert GB, Venegas-Vera AV, Lerma EV. Utility of telemedicine in the COVID-19 era. Rev Cardiovasc Med. 2020 Dec 30;21(4):583–7. doi: 10.31083/j.rcm.2020.04.188. https://www.imrpress.com/journal/RCM/21/4/10.31083/j.rcm.2020.04.188 .1609227830581-487274076 [DOI] [PubMed] [Google Scholar]
- 6.Flumignan CD, Rocha AP, Pinto AC, Milby KM, Batista MR, Atallah AN, Saconato H. What do Cochrane systematic reviews say about telemedicine for healthcare? Sao Paulo Med J. 2019 Jul 15;137(2):184–92. doi: 10.1590/1516-3180.0177240419. https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-31802019000200184&lng=en&nrm=iso&tlng=en .S1516-31802019000200184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mold F, Hendy J, Lai YL, de Lusignan S. Electronic consultation in primary care between providers and patients: systematic review. JMIR Med Inform. 2019 Dec 03;7(4):e13042. doi: 10.2196/13042. https://medinform.jmir.org/2019/4/e13042/ v7i4e13042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mold F, Cooke D, Ip A, Roy P, Denton S, Armes J. COVID-19 and beyond: virtual consultations in primary care-reflecting on the evidence base for implementation and ensuring reach: commentary article. BMJ Health Care Inform. 2021 Jan 12;28(1):e100256. doi: 10.1136/bmjhci-2020-100256. https://informatics.bmj.com/lookup/pmidlookup?view=long&pmid=33436372 .bmjhci-2020-100256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verma P, Kerrison R. Patients’ and physicians’ experiences with remote consultations in primary care during the COVID-19 pandemic: a multi-method rapid review of the literature. BJGP Open. 2022 Jan 14;6(2):BJGPO.2021.0192. doi: 10.3399/bjgpo.2021.0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez AM, Lam K, Thota R. Barriers and facilitators to telemedicine: can you hear me now? Am Soc Clin Oncol Educ Book. 2021 Mar;41:25–36. doi: 10.1200/EDBK_320827. https://ascopubs.org/doi/10.1200/EDBK_320827?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PubMed] [Google Scholar]
- 11.Pagliari C. Digital health and primary care: past, pandemic and prospects. J Glob Health. 2021 Jul 02;11:01005. doi: 10.7189/jogh.11.01005. https://europepmc.org/abstract/MED/34221352 .jogh-11-01005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scott AM, Bakhit M, Greenwood H, Cardona M, Clark J, Krzyzaniak N, Peiris R, Glasziou P. Real-time telehealth versus face-to-face management for patients with PTSD in primary care: a systematic review and meta-analysis. J Clin Psychiatry. 2022 May 23;83(4):21r14143. doi: 10.4088/JCP.21r14143.21r14143 [DOI] [PubMed] [Google Scholar]
- 13.Mabeza RM, Maynard K, Tarn DM. Influence of synchronous primary care telemedicine versus in-person visits on diabetes, hypertension, and hyperlipidemia outcomes: a systematic review. BMC Prim Care. 2022 Mar 21;23(1):52. doi: 10.1186/s12875-022-01662-6.10.1186/s12875-022-01662-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Batsis JA, DiMilia PR, Seo LM, Fortuna KL, Kennedy MA, Blunt HB, Bagley PJ, Brooks J, Brooks E, Kim SY, Masutani RK, Bruce ML, Bartels SJ. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc. 2019 Aug 08;67(8):1737–49. doi: 10.1111/jgs.15959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015 Sep 07;2015(9):CD002098. doi: 10.1002/14651858.CD002098.pub2. https://europepmc.org/abstract/MED/26343551 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Downes MJ, Mervin MC, Byrnes JM, Scuffham PA. Telephone consultations for general practice: a systematic review. Syst Rev. 2017 Jul 03;6(1):128. doi: 10.1186/s13643-017-0529-0. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-017-0529-0 .10.1186/s13643-017-0529-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Guzman KR, Snoswell CL, Caffery LJ, Smith AC. Economic evaluations of videoconference and telephone consultations in primary care: a systematic review. J Telemed Telecare. 2021 Oct 07;:1357633X211043380. doi: 10.1177/1357633X211043380. (forthcoming) [DOI] [PubMed] [Google Scholar]
- 18.Agbali R, Balas AE, Beltrame F, De Leo G. A review of audiovisual telemedicine utilization and satisfaction assessment during the COVID-19 pandemic. Int J Technol Assess Health Care. 2021 Dec 20;38(1):e2. doi: 10.1017/s026646232100060x. [DOI] [PubMed] [Google Scholar]
- 19.Sim R, Lee SW. Patient preference and satisfaction with the use of telemedicine for glycemic control in patients with type 2 diabetes: a review. Patient Prefer Adherence. 2021 Feb;Volume 15:283–98. doi: 10.2147/ppa.s271449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gleeson LL, Clyne B, Barlow JW, Ryan B, Murphy P, Wallace E, De Brún A, Mellon L, Hanratty M, Ennis M, Holton A, Pate M, Kirke C, Flood M, Moriarty F. Medication safety incidents associated with the remote delivery of primary care: a rapid review. Int J Pharm Pract. 2022 Dec 31;30(6):495–506. doi: 10.1093/ijpp/riac087.6967748 [DOI] [PubMed] [Google Scholar]
- 21.Lindenfeld Z, Berry C, Albert S, Massar R, Shelley D, Kwok L, Fennelly K, Chang JE. Synchronous home-based telemedicine for primary care: a review. Med Care Res Rev. 2023 Feb 05;80(1):3–15. doi: 10.1177/10775587221093043. [DOI] [PubMed] [Google Scholar]
- 22.Parker RF, Figures EL, Paddison CA, Matheson JI, Blane DN, Ford JA. Inequalities in general practice remote consultations: a systematic review. BJGP Open. 2021 Mar 12;5(3):BJGPO.2021.0040. doi: 10.3399/bjgpo.2021.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolfe A. Institute of medicine report: crossing the quality chasm: a new health care system for the 21st century. Policy Polit Nurs Pract. 2001 Aug;2(3):233–5. doi: 10.1177/152715440100200312. [DOI] [Google Scholar]
- 24.Neves AL, Freise L, Laranjo L, Carter AW, Darzi A, Mayer E. Impact of providing patients access to electronic health records on quality and safety of care: a systematic review and meta-analysis. BMJ Qual Saf. 2020 Dec 12;29(12):1019–32. doi: 10.1136/bmjqs-2019-010581. http://qualitysafety.bmj.com/lookup/pmidlookup?view=long&pmid=32532814 .bmjqs-2019-010581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sockalingam S, Kirvan A, Pereira C, Rajaratnam T, Elzein Y, Serhal E, Crawford A. The role of tele-education in advancing mental health quality of care: a content analysis of project ECHO recommendations. Telemed J E Health. 2021 Aug 01;27(8):939–46. doi: 10.1089/tmj.2021.0122. [DOI] [PubMed] [Google Scholar]
- 26.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021 Apr;88:105906. doi: 10.1016/j.ijsu.2021.105906. https://linkinghub.elsevier.com/retrieve/pii/S1743-9191(21)00040-6 .S1743-9191(21)00040-6 [DOI] [PubMed] [Google Scholar]
- 27.Covidence systematic review software. Veritas Health Innovation. [2022-06-01]. https://www.covidence.org/
- 28.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, Vedel I, Pluye P. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inform. 2018 Dec 18;34(4):285–91. doi: 10.3233/EFI-180221. [DOI] [Google Scholar]
- 29.Tan NG, Yang LW, Tan MZ, Chng J, Tan MH, Tan C. Virtual care to increase military medical centre capacity in the primary health care setting: a prospective self-controlled pilot study of symptoms collection and telemedicine. J Telemed Telecare. 2020 Oct 04;28(8):603–12. doi: 10.1177/1357633x20959579. [DOI] [PubMed] [Google Scholar]
- 30.Li KY, Ng S, Zhu Z, McCullough JS, Kocher KE, Ellimoottil C. Association between primary care practice telehealth use and acute care visits for ambulatory care-sensitive conditions during COVID-19. JAMA Netw Open. 2022 Mar 01;5(3):e225484. doi: 10.1001/jamanetworkopen.2022.5484. https://europepmc.org/abstract/MED/35357448 .2790571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baughman D, Baughman K, Jabbarpour Y, Waheed A. Comparable quality performance between telemedicine and office-based care for abnormal BMI screening and management. Obes Sci Pract. 2023 Apr 14;9(2):87–94. doi: 10.1002/osp4.625. https://europepmc.org/abstract/MED/37034569 .OSP4625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baughman D, Ptasinski A, Baughman K, Buckwalter N, Jabbarpour Y, Waheed A. Comparable quality performance of acute low-back pain care in telemedicine and office-based cohorts. Telemed J E Health. 2022 Mar 28;28(11):1579–86. doi: 10.1089/tmj.2021.0535. [DOI] [PubMed] [Google Scholar]
- 33.Bernstein P, Ko K, Israni J, Cronin AO, Kurliand MM, Shi JM, Chung J, Borgo L, Reed A, Kosten L, Chang AM, Sites FD, Funahashi T, Agha Z. WITHDRAWN: Urgent and non-emergent telehealth care for seniors: findings from a multi-site impact study. J Telemed Telecare. 2021 Jan 18;:1357633X20985389. doi: 10.1177/1357633X20985389. [DOI] [PubMed] [Google Scholar]
- 34.Chavez A, Pullins C, Yennie J, Singh C, Kosiorek H. Association of telehealth with short-interval follow-up. J Am Board Fam Med. 2022 May 31;35(3):485–90. doi: 10.3122/jabfm.2022.03.210520. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=35641054 .35/3/485 [DOI] [PubMed] [Google Scholar]
- 35.Dai Z, Sezgin G, Li J, Franco G, McGuire P, Datta S, Pearce C, McLeod A, Georgiou A. Telehealth utilisation in residential aged care facilities during the COVID-19 pandemic: a retrospective cohort study in Australian general practice. J Telemed Telecare. 2022 May 11;:1357633X221094406. doi: 10.1177/1357633X221094406. https://europepmc.org/abstract/MED/35544365 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frank HE, Grumbach NM, Conrad SM, Wheeler J, Wolff J. Mental health services in primary care: evidence for the feasibility of telehealth during the COVID-19 pandemic. J Affect Disord Rep. 2021 Jul;5:100146. doi: 10.1016/j.jadr.2021.100146. https://linkinghub.elsevier.com/retrieve/pii/S2666-9153(21)00073-1 .S2666-9153(21)00073-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gordon AS, Adamson WC, DeVries AR. Virtual visits for acute, nonurgent care: a claims analysis of episode-level utilization. J Med Internet Res. 2017 Feb 17;19(2):e35. doi: 10.2196/jmir.6783. https://www.jmir.org/2017/2/e35/ v19i2e35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Govier DJ, Cohen-Cline H, Marsi K, Roth SE. Differences in access to virtual and in-person primary care by race/ethnicity and community social vulnerability among adults diagnosed with COVID-19 in a large, multi-state health system. BMC Health Serv Res. 2022 Apr 15;22(1):511. doi: 10.1186/s12913-022-07858-x. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-07858-x .10.1186/s12913-022-07858-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Graetz I, Huang J, Muelly E, Gopalan A, Reed ME. Primary care visits are timelier when patients choose telemedicine: a cross-sectional observational study. Telemed J E Health. 2022 Sep 01;28(9):1374–8. doi: 10.1089/tmj.2021.0528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Haderlein TP, Dobalian A, Raja PV, Der-Martirosian C. Association between virtual care use and same-day primary care access in VA primary care-mental health integration. J Prim Care Community Health. 2022 Apr 15;13:21501319221091430. doi: 10.1177/21501319221091430. https://journals.sagepub.com/doi/10.1177/21501319221091430?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reed M, Huang J, Graetz I, Muelly E, Millman A, Lee C. Treatment and follow-up care associated with patient-scheduled primary care telemedicine and in-person visits in a large integrated health system. JAMA Netw Open. 2021 Nov 01;4(11):e2132793. doi: 10.1001/jamanetworkopen.2021.32793. https://europepmc.org/abstract/MED/34783828 .2786184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rene R, Cherson M, Rannazzisi A, Felter J, Silverio A, Cunningham AT. Transitioning from in-person to telemedicine within primary care behavioral health during COVID-19. Popul Health Manag. 2022 Aug 01;25(4):455–61. doi: 10.1089/pop.2021.0292. [DOI] [PubMed] [Google Scholar]
- 43.Ryskina KL, Shultz K, Zhou Y, Lautenbach G, Brown RT. Older adults' access to primary care: gender, racial, and ethnic disparities in telemedicine. J Am Geriatr Soc. 2021 Oct 08;69(10):2732–40. doi: 10.1111/jgs.17354. https://europepmc.org/abstract/MED/34224577 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lovell T, Albritton J, Dalto J, Ledward C, Daines W. Virtual vs traditional care settings for low-acuity urgent conditions: an economic analysis of cost and utilization using claims data. J Telemed Telecare. 2021 Jan 25;27(1):59–65. doi: 10.1177/1357633X19861232. [DOI] [PubMed] [Google Scholar]
- 45.Manski-Nankervis JA, Davidson S, Hiscock H, Hallinan C, Ride J, Lingam V, Holman J, Baird A, McKeown E, Sanci L. Primary care consumers’ experiences and opinions of a telehealth consultation delivered via video during the COVID-19 pandemic. Aust J Prim Health. 2022 Mar 15;28(3):224–31. doi: 10.1071/py21193. [DOI] [PubMed] [Google Scholar]
- 46.Mohan S, Lin W, Orozco FR, Robinson J, Mahoney A. Patient perceptions of video visits in a fee-for-service model. J Am Board Fam Med. 2022 May 31;35(3):497–506. doi: 10.3122/jabfm.2022.03.210459. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=35641049 .35/3/497 [DOI] [PubMed] [Google Scholar]
- 47.Pierce RP, Stevermer JJ. Disparities in the use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2023 Jan 21;29(1):3–9. doi: 10.1177/1357633X20963893. https://journals.sagepub.com/doi/abs/10.1177/1357633X20963893?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Quinton JK, Ong MK, Vangala S, Tetleton-Burns A, Webb A, Sarkisian C, Casillas A, Kakani P, Han M, Pirtle CJ. The association of broadband internet access and telemedicine utilization in rural western tennessee: an observational study. BMC Health Serv Res. 2021 Aug 03;21(1):765. doi: 10.1186/s12913-021-06746-0. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-021-06746-0 .10.1186/s12913-021-06746-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reed ME, Huang J, Graetz I, Lee C, Muelly E, Kennedy C, Kim E. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020 Jun 01;3(6):e205873. doi: 10.1001/jamanetworkopen.2020.5873. https://europepmc.org/abstract/MED/32585018 .2767244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McGrail KM, Ahuja MA, Leaver CA. Virtual visits and patient-centered care: results of a patient survey and observational study. J Med Internet Res. 2017 May 26;19(5):e177. doi: 10.2196/jmir.7374. https://www.jmir.org/2017/5/e177/ v19i5e177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Miller D, Loftus AM, O'Boyle PJ, McCloskey M, O'Kelly J, Mace D, McKeon N, Ewan SL, Moore L, Abbott A, Cunning S, McCarron MO, Paget AM. Impact of a telephone-first consultation system in general practice. Postgrad Med J. 2019 Nov;95(1129):590–5. doi: 10.1136/postgradmedj-2019-136557.postgradmedj-2019-136557 [DOI] [PubMed] [Google Scholar]
- 52.Neufeld A, Bhella V, Svrcek C. Pivoting to be patient-centered: a study on hidden psychological costs of tele-healthcare and the patient-provider relationship. Internet J Allied Health Sci Pract. 2022:1–10. doi: 10.46743/1540-580X/2022.2112. [DOI] [Google Scholar]
- 53.Egede LE, Gebregziabher M, Walker RJ, Payne EH, Acierno R, Frueh BC. Trajectory of cost overtime after psychotherapy for depression in older Veterans via telemedicine. J Affect Disord. 2017 Jan 01;207:157–62. doi: 10.1016/j.jad.2016.09.044.S0165-0327(16)31153-3 [DOI] [PubMed] [Google Scholar]
- 54.Harder VS, Musau AM, Musyimi CW, Ndetei DM, Mutiso VN. A randomized clinical trial of mobile phone motivational interviewing for alcohol use problems in Kenya. Addiction. 2020 Jun 03;115(6):1050–60. doi: 10.1111/add.14903. https://europepmc.org/abstract/MED/31782966 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nomura A, Tanigawa T, Muto T, Oga T, Fukushima Y, Kiyosue A, Miyazaki M, Hida E, Satake K. Clinical efficacy of telemedicine compared to face-to-face clinic visits for smoking cessation: multicenter open-label randomized controlled noninferiority trial. J Med Internet Res. 2019 Apr 26;21(4):e13520. doi: 10.2196/13520. https://www.jmir.org/2019/4/e13520/ v21i4e13520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ure A. Investigating the effectiveness of virtual treatment via telephone triage in a New Zealand general practice. J Prim Health Care. 2022 Apr 3;14(1):21–8. doi: 10.1071/HC21125.HC21125 [DOI] [PubMed] [Google Scholar]
- 57.Wickström HL, Öien RF, Fagerström C, Anderberg P, Jakobsson U, Midlöv PJ. Comparing video consultation with inperson assessment for Swedish patients with hard-to-heal ulcers: registry-based studies of healing time and of waiting time. BMJ Open. 2018 Feb 15;8(2):e017623. doi: 10.1136/bmjopen-2017-017623. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=29449288 .bmjopen-2017-017623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Befort CA, VanWormer JJ, Desouza C, Ellerbeck EF, Gajewski B, Kimminau KS, Greiner KA, Perri MG, Brown AR, Pathak RD, Huang TT, Eiland L, Drincic A. Effect of behavioral therapy with in-clinic or telephone group visits vs in-clinic individual visits on weight loss among patients with obesity in rural clinical practice: a randomized clinical trial. JAMA. 2021 Jan 26;325(4):363–72. doi: 10.1001/jama.2020.25855. https://europepmc.org/abstract/MED/33496775 .2775448 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
MEDLINE search strategy and gray literature search.
Data extraction form template.
Mixed Methods Appraisal Tool assessment with justifications for decisions.
The efficiency of virtual versus face-to face consultations.
The effectiveness of virtual versus face-to-face consultations.
The impact of virtual consultations on patient-centeredness.
The timeliness of virtual versus face-to-face consultations.
The impact of virtual consultations on the equity of care.
Data Availability Statement
The search strategy and extracted data contributing to the narrative synthesis are available as multimedia appendices. Any additional data are available on request.


