Abstract
Objectives:
Maternal alcohol misuse during the postpartum period is associated with negative maternal and infant outcomes. This study examined whether greater stress exposure in the year before the baby’s birth and maternal post-traumatic stress disorder (PTSD) were associated with postpartum alcohol misuse among a sample of women veterans. Maternal PTSD was also examined as a moderator of the association between stress exposure and postpartum alcohol misuse.
Methods:
Data were drawn from the Center for Maternal and Infant Outcomes Research in Translation study, a multisite prospective cohort study of pregnant and postpartum women veterans. Interviews were conducted within 12 weeks after birth. At this post-birth interview, women reported whether they experienced stressful events (e.g., loss of job, military deployment, separation/divorce) in the year before birth. PTSD diagnosis and postpartum scores on the Alcohol Use Disorders Identification Test (AUDIT-C) were derived from the Department of Veterans Affairs medical records.
Results:
Models testing main and interaction effects showed a statistically significant association of both PTSD (p = .02) and stress exposure (p = .04), as well as significant interaction of PTSD and stress exposure (p =.03) with AUDIT-C scores postpartum, after controlling for marital status, age, and race. Specifically, compared with women without PTSD, those with PTSD had higher overall AUDIT-C scores postpartum, regardless of stress exposure. For women without PTSD, more stress exposure before birth was associated with higher AUDIT-C scores during the postpartum phase.
Conclusions:
PTSD diagnosis and life stressors before infant birth predicted maternal alcohol misuse during the post-partum period. Identifying such risk factors is an initial step in preventing alcohol misuse, with the goal of enhancing postpartum health for the birthing parent and infant.
Much attention has been paid to maternal alcohol use during pregnancy, given the negative effects of prenatal alcohol exposure on the fetus and infant development (Patra et al., 2011). Maternal alcohol misuse during the postpartum period is less attended to, despite findings that the postpartum life phase can be a period of increased stress and risky behavior for the mother, especially if she has a history of trauma (Chung et al., 2010; Epifanio, Genna, De Luca, Roccella, & La Grutta, 2015; Morland et al., 2007). Maternal substance misuse after a child is born has been associated with negative infant outcomes (Johnson, Fulco, & Augustyn, 2019; Pajulo et al., 2012) and, for breastfeeding women, there is a risk of passing alcohol on to their infant through breast milk if drinking postpartum (Giglia & Binns, 2006). In addition to potential negative impacts for children, there are substantial negative effects of alcohol misuse on maternal postpartum health, particularly for women coping with psychological conditions. For instance, there is a causal and reciprocal effect of stress and trauma with alcohol misuse among women (Peltier et al., 2019); in other words, although stress reactivity and symptoms of post-traumatic stress disorder (PTSD) contribute to alcohol misuse, drinking also intensifies daily stress levels and can maintain symptoms of PTSD. Additionally, both substance use history and substance use during the postpartum period have been identified as risk factors for post-partum depression (Chapman, & Wu, 2013; Ross & Dennis, 2009).
Postpartum alcohol misuse may be an especially important issue for women veterans for several reasons. The rates of problem drinking are rising among the general population of women veterans and there are higher rates of alcohol use disorders (AUDs) in veteran compared with civilian women (Evans et al., 2018), including women veterans with PTSD (Hoggatt et al., 2015). Pregnant veterans in Department of Veterans Affairs (VA) care have high rates of mental health conditions compared with nonpregnant veterans, including alcohol misuse and PTSD (Mattocks et al., 2010). Stress exposure, traumatic experiences, and symptoms of PTSD may put women veterans at particularly high risk of having a difficult postpartum transition and post-partum alcohol misuse.
Given that stress and PTSD are established risk factors for unhealthy alcohol use in women generally, it is plausible that they would play important roles in postpartum alcohol misuse specifically; however, this association has been less widely examined. Indeed, for many women, having a newborn is protective against alcohol misuse (Laborde & Mair, 2012) and having children is overall predictive of less heavy drinking (Patrick et al. 2020), but this is not the case for all new mothers. Demographic factors including marital status, race, income, and maternal age have been identified as predictors of postpartum alcohol misuse (Laborde & Mair, 2012; Patrick et al., 2020), but underlying intrapersonal factors such as stress exposure and PTSD have not been studied.
Exposure to stressful life events (independent of PTSD) has been shown to predict substance use during pregnancy (Hamilton Boyles et al., 2000; Nelson et al., 2003), but those studies did not examine postpartum alcohol misuse. A cross-sectional study that was conducted among postpartum adolescents found an association between stress and alcohol use, with those who used substances during their child’s first months of life also being more likely to report depression, high stress, and an increased need for social support during that time, compared with those who did not use substances postpartum (Barnet, Duggan, Wilson, & Joffe, 1995). Thus, there may be a correlational association of stress and postpartum alcohol use, but additional research is needed. One study that examined PTSD as a predictor of postpartum alcohol use found that women with PTSD or subthreshold PTSD were more likely than those without PTSD to have depression, anxiety, and higher perceived stress, and to binge drink during the postpartum period (Onoye, Goebert, Morland, Matsu, & Wright, 2009).
The effect of stress exposure and PTSD on postpartum alcohol misuse may also be synergistic. Stress exposure is associated with women’s alcohol misuse generally (Peltier et al., 2019) and difficulties coping with that stress exposure may be heightened among women veterans with PTSD. This possibility is supported by research showing that women (and men) with PTSD have greater difficulty regulating stress and negative emotion (Fairholme et al., 2013; Fitzgerald, Digangi, & Phan, 2018; Hien et al., 2017; Kashdan, Breen, & Julian, 2010; Weiss, Tull, Viana, Anestis, & Gratz, 2012). Greater stress exposure and difficulty coping (conferred by PTSD symptoms) may enhance risk of alcohol use, an unhealthy coping strategy, during the postpartum period.
Current Study
The current study sought to examine stress exposure during the prenatal period, 1 year before birth (aim 1), and after a military PTSD diagnosis, according to VA medical records (aim 2), as potential predictors of postpartum alcohol misuse. Based on the research outlined showing that stress and PTSD are associated with more drinking among women generally and during pregnancy, it was hypothesized that exposure to stressful life events during the year before giving birth and having PTSD would both increase likelihood of alcohol misuse during the postpartum period. It was additionally examined whether the association of stress exposure and increased drinking postpartum was moderated by a post-military PTSD diagnosis (aim 3). It was expected that PTSD and stressful life events would have an interactive effect, whereby the association of stress exposure with alcohol misuse would be greater for those who also had PTSD diagnoses.
Methods
Participants
Data were collected as part of the Center for Maternal and Infant Outcomes Research in Translation (COMFORT) study, a multisite, mixed methods study conducted with women veterans receiving care in the Veterans Health Administration (VHA). COMFORT enrolled women veterans aged 18 years or older. Inclusion criteria included being a VHA patient, positive screen for pregnancy at a VHA facility, fluent in English, and using 1 of the 15 COMFORT VHA facilities for care. These 15 sites were purposively chosen to represent facilities with the following characteristics: variation in the number of deliveries per facility to women veterans using VHA benefits (high, >150 deliveries/year; medium, 50–149 deliveries/year; low, <50 deliveries/year) (Mattocks et al., 2014); regionally and racially diverse; and had membership in the Women’s Practice-Based Research Network, a VA-funded network of VHA facilities that provide care for a substantial number of women veterans and have lead site investigators willing to support recruitment. Veterans who reported a miscarriage, did not complete the post-birth interview, were less than 2 years postpartum, or had an invalid social security number were excluded from the current analyses. Information regarding the first child only was collected for women with multiple deliveries during the study period. Of 884 women enrolled in COMFORT as of January 28, 2020, 450 (50.9%) women had at least one Alcohol Use Disorders Identification Test (AUDIT-C) score in either the 2 years before or after their due date and were included in the current analyses.
Procedure
The VHA’s Central Institutional Review Board approved the study, along with the local Research & Development Committees at each site. Details on the study methods have been described in detail previously (Kroll-Desrosiers, Crawford, Simas, Clark, & Mattocks, 2019). Each eligible participant was mailed a study invitation letter, after which the study team made follow-up calls to gauge the veteran’s level of interest in participating. Participants provided verbal consent. Telephone postpartum interviews were conducted (40 minutes in length) at a median 6 weeks postpartum (mean, 6.6 weeks; standard deviation, 3.3 weeks). Of the interviews, 95% were conducted within 12 weeks postpartum. Owing to scheduling conflicts, a small number of women were interviewed after this time period, with a maximum interview time at 32 weeks postpartum. Interviewers asked the questions from a structured interview and entered the participants’ responses using Research Electronic Data Capture (REDCap) (Harris et al., 2009, 2019). Participants were compensated $25 for each completed interview.
Measures
AUDIT-C
AUDIT-C scores (Singleton, Henningfield, & Tiffany, 1994) were obtained from electronic medical record (EMR) data from the VA Corporate Data Warehouse, a data repository updated nightly (HSR&D Web Team, 2014). AUDIT-C scores were collected for the 2 years after each woman’s due date. The AUDIT-C is a three-item alcohol screen that reliably identifies patients who are hazardous drinkers or have active AUD. The range of potential scores is 0–12, with a score of 3 or higher indicating alcohol misuse among women. For this analysis, if more than one score was available, we used each participant’s maximum AUDIT-C score in each 2-year postpartum period.
Demographics
For the current analyses, we included demographic variables demonstrated to be associated with postpartum substance use as covariates in our regression model. Specifically, we included information on self-reported race (categorized as White, Black, and other) and marital status (categorized as single, married, and divorced/separated/widowed). Birthdate was obtained from EMR data to calculate age at the time of prenatal interview (in years). See Table 1 for participant demographics.
Table 1.
Demographics at Prenatal Interview (n = 450)
| Characteristics | Total |
|---|---|
| Estimated age at prenatal interview, mean ± SD (range) | 32.1 ± 4.5 (20.4–48.7) |
| Race | |
| White | 273 (60.7) |
| Black | 114 (25.3) |
| Other | 71 (15.8) |
| Hispanic or Latina | 69 (15.3) |
| Marital status | |
| Single | 91 (20.2) |
| Married | 287 (63.8) |
| Divorced/Separated/Widowed | 39 (8.7) |
| Service-connected status | 389 (86.4) |
| OEF/OIF/OND | 437 (97.1) |
| Deployed | 271 (60.2) |
| Military branch | |
| Air Force | 87 (19.3) |
| Army | 224 (49.8) |
| Marine Corps | 39 (8.7) |
| Navy | 93 (20.7) |
| Coast Guard | 6 (1.3) |
| Civilian employee | 1 (0.2) |
| Component | |
| Active duty | 305 (67.8) |
| National Guard | 70 (15.6) |
| Reserves | 72 (16) |
| Civilian government employee | 3 (0.7) |
| Urban/rural status | |
| Urban | 326 (72.4) |
| Rural | 115 (25.6) |
| Missing | 9 (2) |
| First pregnancy | 162 (36) |
| Received any VA maternity care coordination services | 353 (78.4) |
| Weeks pregnantwhen first saw prenatal care provider | |
| ≤8 | 185 (41.1) |
| 9–12 | 200 (44.4) |
| ≥13 | 65 (14.4) |
| MST | |
| Harassment | 233 (51.8) |
| Rape | 141 (31.3) |
| Ever diagnosis of mental health conditions in VA EMR | |
| Major depressive disorder | 256 (56.9) |
| Anxiety | 217 (48.2) |
| PTSD | 188 (41.8) |
Abbreviations: EMR, electronic medical record; MST, military sexual trauma; OEF/OIF/OND, Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn; PTSD, post-traumatic stress disorder; SD, standard deviation; VA, Department of Veterans Affairs.
Note: Race categories are not mutually exclusive; cells may not sum to total due to missing values. Values are number (%) unless otherwise indicated.
Stressful events
Stress exposure during the past year was assessed via the postpartum interview, by asking participants whether they experienced any of 14 potentially stressful events in the 12 months before the birth of their baby (Table 2). The number of stressful events experienced was summed for each participant, resulting in a continuous stress score ranging from 0 to 14. The items selected were derived from Holmes-Rahe Life Stress Inventory (Holmes & Rahe, 1967), which measures the impact of stress on illness. The goal was to measure cumulative stress during this time in pregnancy. The 43 items on the original scale were tailored for this study (e.g., “pregnancy” is one item on the original scale) and some items were combined (e.g., separation and divorce are separate items, combined to one item to decrease participant burden).
Table 2.
Stressful Events in the 12 Months Before the Baby’s Birth
| Stressful Events (n = 450) | n | % |
|---|---|---|
| You moved to a new address. | 132 | 29.3 |
| A close family member was sick and had to go to the hospital. | 86 | 19.1 |
| You and your husband/partner argued more than usual. | 73 | 16.2 |
| You had trouble with outstanding bills. | 72 | 16.0 |
| Someone close to you died. | 57 | 12.7 |
| Someone close to you had a problem with drinking or drugs. | 47 | 10.4 |
| You got separated or divorced from your husband or partner. | 41 | 9.1 |
| Your husband/partner lost their job. | 36 | 8.0 |
| You lost your job even though you wanted to keep working. | 35 | 7.8 |
| You had trouble finding reliable childcare for your other children. | 35 | 7.8 |
| You lost a child or baby. | 15 | 3.3 |
| You were homeless. | 11 | 2.4 |
| You or your husband/partner went to jail, prison, or a detention center. | 10 | 2.2 |
| Your husband/partner was deployed for military service. | 9 | 2.0 |
| Stressful events sum, mean ± standard deviation (range) | 1.5 ± 1.9 | (0–9) |
Clinical factors
Data were obtained from EMR regarding whether each participant was diagnosed with PTSD by a VHA professional in her years as a VHA patient.
Data Analysis Plan
We first examined descriptive statistics for our cohort. Analyses were used to examine the bivariate associations of AUDIT-C, PTSD diagnosis, and stressful events. To examine the main effects of number of stressful events and PTSD diagnosis on postpartum AUDIT-C (aims 1 and 2, respectively), as well as the interactive effect of stressful events and PTSD (aim 3), we used linear regression in the form of generalized linear models with all three predictors (PTSD, stressful events, and their interaction) in the same model. If significant, simple slope analyses were performed to test the nature of the interaction effects (e.g., whether the significant interaction is, for example, driven by PTSD status). We then ran the same analyses but controlled for marital status (dichotomizing our categories to married vs. not), age (continuous), and race (dichotomizing our categories to White vs. non-White), given these variables’ association with postpartum drinking. All results are reported at the critical significance level of a p value of less than .05. Analyses were conducted in SAS v9.2 (SAS Institute, Inc., Cary, NC).
Results
Women veterans in our cohort were, on average, 32.1 ± 4.5 years of age (range, 20.4–48.7 years). Sixty-one percent of participants were White, 15% were Hispanic, and 64% were married. On average, women veterans in our sample experienced 1.5 stressful events (±1.9) in the 12 months before their baby’s birth. This score ranged from no to nine stressful events, with a median of one stressful event (Table 2). More than 40% of women had been diagnosed with PTSD by a VHA provider in the past (Table 1). The majority of participants (58% [n = 255]) had only one AUDIT-C score during this 2-year period. The maximum score was used to avoid a large amount of missing data in our analyses. Only 36% of participants (n = 157) had two AUDIT-C scores (with n = 28 having more than two), and of the participants who had two AUDIT-C scores or more within 2 years postpartum, the average difference between the two scores was 0.9 ± 1.0, suggesting consistency across assessment timepoints. Thirty-six women (8%) had at least one AUDIT-C score of 3 or greater during pregnancy. Of women who had been diagnosed with PTSD, 18% had a positive AUDIT-C score in the 2 years after childbirth, compared with 12% of women never diagnosed with PTSD (p = .07) (Table 3). Participants with a positive AUDIT-C score (≥3) had a greater number of stressful events, on average, compared with participants with a negative AUDIT-C score (p = .01), and those with PTSD had greater stressful events than those without PTSD (p < .0001) (Table 3). In terms of diagnosis, 14% of participants (n = 63) were diagnosed with AUD in the VHA EMR and 2.9% (n = 13) were diagnosed with AUD in the 12 months after childbirth. Women diagnosed with AUD in the 12 months after childbirth had higher AUDIT-C scores, on average, compared with women without a diagnosis (3.5 ± 3.3 vs. 1.1 ± 1.4, respectively; p ≤.0001).
Table 3.
AUDIT-C Scores
| Mean ± SD (Range) or No. (%) | p-Value | |
|---|---|---|
| Maximum AUDIT-C 2 years after due date | 1.2 ± 1.5 (0–10) | |
| Positive AUDIT-C 2 years after due date (AUDIT-C ≥3) | 65 (14.4) | |
| Maximum AUDIT-C in 2 years after due date | ||
| Women with lifetime PTSD diagnosis (n = 188) | 1.3 ± 1.8 (0–10) | .23 |
| Women without lifetime PTSD diagnosis (n = 247) | 1.1 ± 1.2 (0–10) | |
| No. of stressful events | ||
| Women with positive AUDIT-C in 2 years after due date | 2.0 ± 2.1 | .01 |
| Women with negative AUDIT-C in 2 years after due date | 1.4 ± 1.8 | |
| Women with PTSD | 1.9 ± 2.1 | <.01 |
| Women without PTSD | 1.2 ± 1.6 | |
| Positive AUDIT-C in 2 years after due date | ||
| Women with lifetime PTSD diagnosis (n = 188) | 34 (18.3) | .07 |
| Women without lifetime PTSD diagnosis (n = 247) | 31 (12.1) |
Abbreviations: AUDIT-C, Alcohol Use Disorders Identification Test; PTSD, post-traumatic stress disorder; SD, standard deviation.
Models regressing PTSD and stressful events on maximum AUDIT-C score in the 2 years after childbirth showed that in unadjusted models, an increase in the number of stressful events during the prenatal period (β = 0.06 ± standard error [SE] = 0.04) and a VHA diagnosis of PTSD (β = 0.18 ± SE = 0.15) were both associated with a higher AUDIT-C score; however, neither of these factors reached statistical significance (p = .13 for stress; p = .24 for PTSD) An additional model with an interaction term between these two factors did not yield a significant finding (p = .31 for interaction). However, in a model controlling for marital status, age, and race, there were significant main effects of both stressful events (β = 0.13 ± SE = 0.06; p =.04) and PTSD (β = 0.46 ± SE = 0.20; p= .02) on postpartum AUDIT-C scores. Additionally, there was a significant interaction effect of number of stressful events and PTSD associated with AUDIT-C score in the 2 years after childbirth (p = .03; Figure 1). Examination of the interaction effect showed that, although those with PTSD had higher AUDIT-C scores overall, women without PTSD had higher AUDIT-C scores if they also reported more stressful events in the year before their baby’s birth. Simple slope analyses showed a significant slope, or association, between number of stressors and AUDIT-C score for women without PTSD (B = 0.13; t = 2.06; p = .04), but not for women with PTSD (B = ‒0.063; t = ‒1.04; p = .30) (Figure 1).
Figure 1.
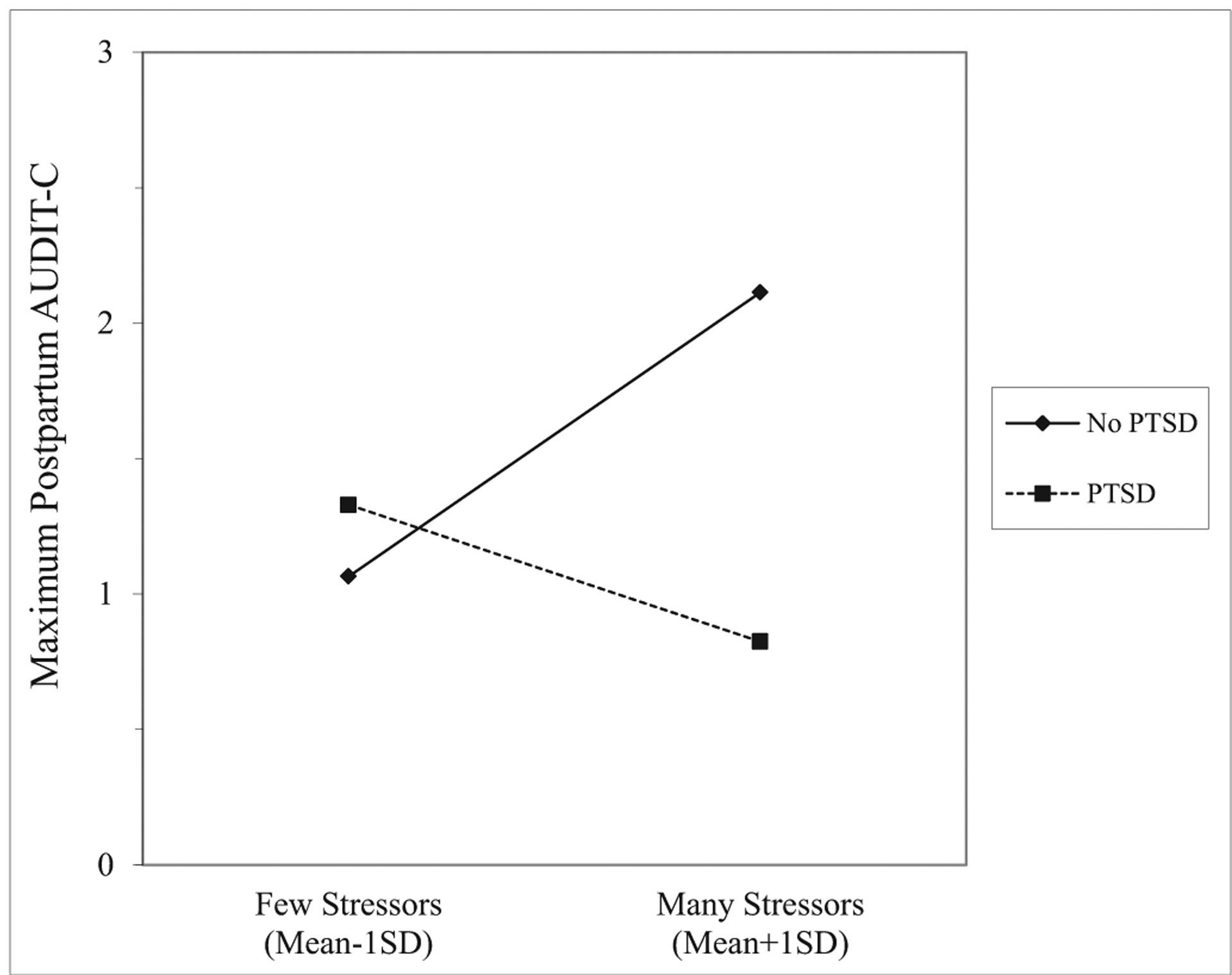
Interaction effect. To illustrate the interaction effect of post-traumatic stress disorder (PTSD) and stressful events on postpartum Alcohol Use Disorders Identification Test (AUDIT-C), the number of stressful events is dichotomized. The number of stressful events variable was, however, entered as a continuous variable in the models tested.
On average, women had their first postpartum AUDIT-C score at 183 ± 137 days after childbirth (median, 141 days; range, 5–707 days). Women with positive scores did have slightly later tests, on average, compared with women with negative scores (226 days [7.4 months] vs. 178 [5.8 months] days postpartum; p = .02). To confirm that the timing of AUDIT-C screens did not affect our findings, models were run with the addition of this timing variable. Our results remained consistent; in our main effects model adjusting for demographic factors, time since childbirth was not a significant predictor of AUDIT-C score (p = .11). In our Stress × PTSD interaction model (aim 3), our interaction term remained significant (p = .03) and time since childbirth was again not a significant predictor (p = .08).
Discussion
The postpartum period is a critical time for both maternal health and infant development. While many women decrease their alcohol use after the birth of their baby relative to before conception, for some this is a time of increased risk. Female service members leaving the military are most often between the ages of 18 and 40 years and, accordingly, there have been significant increases in the number of deliveries to women veterans using maternity benefits from the Veteran Health Administration (Mattocks et al., 2014). Visits related to pregnancy represent opportunities to provide mental health assistance to women who may be struggling (Homish, Cornelius, Richardson, & Day, 2004). Findings from the current study suggest that PTSD and stress exposure in the year before birth are factors that may increase the risk of alcohol misuse in the first 2 years postpartum. Specifically, results demonstrated that, although women with PTSD have higher postpartum AUDIT-C scores overall, women without PTSD had AUDIT-C scores that increased with the number of stressful experiences in the year before the baby’s birth. The stressors queried included family illness, divorce, homelessness, financial difficulties, and partner’s military deployment. These findings are consistent with burgeoning research on the causal association between stress and trauma exposure and the development of problematic alcohol use for women.
It is notable that these findings were significant only after controlling for the effects of the demographic variables of marital status, age, and race. These variables have been associated with postpartum substance use in previous research, and particularly in this population of veterans, it may highly correlate with stress exposure and substance use risk. Race was the only demographic variable to remain a significant predictor after entering our predictors of interest, with White women (61% of the sample) reporting more alcohol use compared with Black women and women in the other race category. The association of demographic variables, particularly marital status and age, with postpartum drinking may be attributable to the association of those factors with stress exposure and PTSD (or traumatic experiences more generally) or may be relevant for veterans specifically. This area requires future research.
In contrast with the study hypotheses, the association of stress and postpartum alcohol misuse was only significant among women without PTSD. The results suggest that, although women with PTSD have heightened AUDIT-C scores overall, women veterans without PTSD may be at increased risk if they had many stressors during their pregnancy. There is a need to better understand the type of support that would mitigate the negative impacts of such stress exposure. A better understanding of how the stress exposure translates to heightened drinking during the postpartum phase is an important avenue for research as well.
The finding that veterans with PTSD had higher overall AUDIT-C scores points to the heightened risk of postpartum alcohol misuse for this population. Although the reasons were not explored in this study, pregnancy and the postpartum phase may be especially difficult life stages for women with PTSD (Muzik et al., 2016). For instance, women with PTSD secondary to sexual assault or childhood abuse histories may have complex concerns or difficulties regarding pregnancy and motherhood (Kendall-Tackett, 2007; Rodgers, Lang, Twamley, & Stein, 2003). For these individuals, pregnancy and childbirth may be especially triggering, increasing anxious and depressed feelings and/or increasing alcohol use. Women with PTSD also reported more stressors overall than women without PTSD, which may contribute to the risk for problematic alcohol use. There are also several biological factors that may account for the potentially higher risk of alcohol misuse among women veterans with PTSD. For example, biological correlates of PTSD that have also been implicated in stress tolerance, alcohol use, and impulsive behavior fluctuate greatly during and after childbirth (e.g., changes in functioning of ovarian hormones and the hypothalamic–pituitary–adrenal axis). Regardless of the mechanism by which PTSD may be related to postpartum alcohol use, this is an important avenue for continued research.
Limitations
This study’s outcome variabled—namely, maximum AUDIT-C score reported in up to 2 years after infant birthd—is based on patient self-report at a medical visit; however, the AUDIT-C has been widely validated, mitigating the absence of an objective measure of alcohol misuse. Not all women in the parent study had presented for a medical appointment at the VA during their postpartum phase, precluding their inclusion. It is feasible that women who drink more heavily or encounter more barriers to care are less likely to attend appointments and therefore may be under-represented in our sample. The severity of PTSD at the time of pregnancy was not assessed in this study, but may be an important factor, and a diagnosis of PTSD was from VA medical records rather than being diagnosed by the study team. Likewise, other psychological factors that may be associated with stress and drinking, such as depression, were not assessed. The study did not assess for stressors after childbirth or during the post-partum period. Given that we had a wide span of time (2 years) during which we were looking at AUDIT-C scores, additional stressors may have contributed to drinking behavior; this is an area for continued research. Last, social desirability was a likely factor in veterans’ reports of their alcohol use and potential alcohol-related problems, but was not assessed in the current study.
Implications for Practice and/or Policy
The current study suggests that women veterans with histories of PTSD or those who have experienced stressful experiences in the year before giving birth may be at higher risk for unhealthy drinking during the postpartum period. These findings have implications for the prevention and treatment of postpartum unhealthy alcohol use among women veterans.
Although alcohol use during the postpartum period is not in and of itself problematic, it may be if it is excessive or if it is combined with other mental health conditions, including PTSD or an alcohol or other substance use disorder. Individuals with these risk factors may require additional support after childbirth. Although there has been increased research and attention to postpartum depression, there is still variation within the VHA in terms of regular, standardized screening (Kroll-Desrosiers et al., 2019), and no research to our knowledge has examined reliability or availability of screening for alcohol-related problems during the postpartum period. This finding is important, given that maternal alcohol and other substance use appears to impact mother–baby bonding as well as child cognitive and socioemotional development (Kingston, Tough, & Whitfield, 2012; Pajulo et al., 2012). Additionally, there is a reciprocal relationship between alcohol use and emotional health in women, and instances of postpartum depression or anxiety are exacerbated by unhealthy alcohol use (Chapman & Wu, 2013).
Although providers have many health outcomes to follow up on after the birth of a baby, the widespread impacts of maternal mental health highlight the importance of screening for behavioral as well as physical health. Additionally, research has suggested that even brief interventions (e.g., two 15-minute sessions each with follow-up phone call) for new mothers who are engaging in risky drinking may be efficacious (Fleming, Lund, Wilton, Landry & Scheets, 2008). VHA providers are in an excellent position to engage veterans who have recently given birth throughout the pre- and post-partum periods, and for maternity care coordinators to screen for unhealthy alcohol use and provide services as needed.
Acknowledgments
Funded by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development Health Services Research & Development grant IIR13-81 and Clinical Services Research & Development grant CX001951. Authors report no conflicts of interest. The opinions expressed here are those of the authors and do not represent the official policy or position of the U.S. Department of Veteran Affairs or the U.S. government.
References
- Barnet B, Duggan AK, Wilson MD, & Joffe A (1995). Association between postpartum substance use and depressive symptoms, stress, and social support in adolescent mothers. Pediatrics, 96(4), 659–666. [PubMed] [Google Scholar]
- Chapman SLC, & Wu LT (2013). Postpartum substance use and depressive symptoms: A review. Women & Health, 53(5), 479–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung EK, Nurmohamed L, Mathew L, Elo IT, Coyne JC, & Culhane JF (2010). Risky health behaviors among mothers-to-be: The impact of adverse childhood experiences. Academic Pediatrics, 10(4), 245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epifanio MS, Genna V, De Luca C, Roccella M, & La Grutta S (2015). Paternal and maternal transition to parenthood: The risk of postpartum depression and parenting stress. Pediatric Reports, 7(2), 5872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans EA, Upchurch DM, Simpson T, Hamilton AB, & Hoggatt KJ (2018). Differences by veteran/civilian status and gender in associations between childhood adversity and alcohol and drug use disorders. Social Psychiatry and Psychiatric Epidemiology, 53(4), 421–435. [DOI] [PubMed] [Google Scholar]
- Fairholme CP, Nosen EL, Nillni YI, Schumacher JA, Tull MT, & Coffey SF (2013). Sleep disturbance and emotion dysregulation as transdiagnostic processes in a comorbid sample. Behaviour Research & Therapy, 51(9), 540–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald JM, Digangi JA, & Phan KL (2018). Functional neuroanatomy of emotion and its regulation in PTSD. Harvard Review of Psychiatry, 26(3), 116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming MF, Lund MR, Wilton G, Landry M, & Scheets D (2008). The Healthy Moms Study: The efficacy of brief alcohol intervention in post-partum women. Alcoholism: Clinical and Experimental Research, 32(9), 1600–1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giglia R, & Binns C (2006). Alcohol and lactation: A systematic review. Nutrition & Dietetics, 63(2), 103–116. [Google Scholar]
- Hamilton Boyles S, Ness RB, Grisso JA, Markovic N, Bromberger J, & CiFelli D (2000). Life event stress and the association with spontaneous abortion in gravid women at an urban emergency department. Health Psychology, 19(6), 510. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, & Consortium RE (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Information, 95, 103–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Information, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Lopez-Castro T, Papini S, Gorman B, & Ruglass LM (2017). Emotion dysregulation moderates the effect of cognitive behavior therapy with prolonged exposure for co-occurring PTSD and substance use disorders. Journal of Anxiety Disorders, 52, 53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoggatt KJ, Jamison AL, Lehavot K, Cucciare MA, Timko C, & Simpson TL (2015). Alcohol and drug misuse, abuse, and dependence in women veterans. Epidemiologic Reviews, 37(1), 23–37. [DOI] [PubMed] [Google Scholar]
- Holmes TH, & Rahe RH (1967). The social readjustment rating scale. Journal of Psychosomatic Research, 11, 213–218. [DOI] [PubMed] [Google Scholar]
- Homish GG, Cornelius JR, Richardson GA, & Day NL (2004). Antenatal risk factors associated with postpartum comorbid alcohol use and depressive symptomatology. Alcoholism: Clinical and Experimental Research, 28(8), 1242–1248. [DOI] [PubMed] [Google Scholar]
- HSR&D Web Team. (2014). Health Services Research & Development: Corporate Data Warehouse (CDW). Available: www.hsrd.research.va.gov/for_researchers/vinci/cdw.cfm. Accessed: September 4, 2021.
- Johnson AK, Fulco CJ, & Augustyn MB (2019). Intergenerational continuity in alcohol misuse: Maternal alcohol use disorder and the sequelae of maternal and family functioning. Psychology of Addictive Behaviors, 3(5), 442–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Breen WE, & Julian T (2010). Everyday strivings in war veterans with posttraumatic stress disorder: Suffering from a hyper-focus on avoidance and emotion regulation. Behavior Therapy, 41(3), 350–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Tackett KA (2007). Violence against women and the perinatal period: The impact of lifetime violence and abuse on pregnancy, postpartum, and breastfeeding. Trauma, Violence, & Abuse, 8(3), 344–353. [DOI] [PubMed] [Google Scholar]
- Kingston D, Tough S, & Whitfield H (2012). Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child Psychiatry & Human Development, 43(5), 683–714. [DOI] [PubMed] [Google Scholar]
- Kroll-Desrosiers AR, Crawford SL, Simas TAM, Clark MA, Bastian LA, & Mattocks KM (2019). Rates and correlates of depression symptoms in a sample of pregnant veterans receiving Veterans Health Administration care. Women’s Health Issues, 29(4), 333–340. [DOI] [PubMed] [Google Scholar]
- Laborde ND, & Mair C (2012). Alcohol use patterns among postpartum women. Maternal and Child Health Journal, 16(9), 1810–1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattocks KM, Skanderson M, Goulet JL, Brandt C, Womack J, Krebs E, & Haskell S (2010). Pregnancy and mental health among women veterans returning from Iraq and Afghanistan. Journal of Women’s Health, 19(12), 2159–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattocks KM, Frayne S, Phibbs CS, Yano EM, Zephyrin L, Shryock H, & Bastian LA (2014). Five-year trends in women veterans’ use of VA maternity benefits, 2008–2012. Womens Health Issues, 24(1), e37–42. [DOI] [PubMed] [Google Scholar]
- Morland L, Goebert D, Onoye J, Frattarelli L, Derauf C, Herbst M, & Friedman M (2007). Posttraumatic stress disorder and pregnancy health: Preliminary update and implications. Psychosomatics, 48(4), 304–308. [DOI] [PubMed] [Google Scholar]
- Muzik M, McGinnis EW, Bocknek E, Morelen D, Rosenblum KL, Liberzon I, & Abelson JL (2016). PTSD symptoms across pregnancy and early postpartum among women with lifetime PTSD diagnosis. Depression and Anxiety, 33(7), 584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson DB, Grisso JA, Joffe MM, Brensinger C, Shaw L, & Datner E (2003). Does stress influence early pregnancy loss? Annals of Epidemiology, 13(4), 223–229. [DOI] [PubMed] [Google Scholar]
- Onoye JM, Goebert D, Morland L, Matsu C, & Wright T (2009). PTSD and postpartum mental health in a sample of Caucasian, Asian, and Pacific Islander women. Archives of Women’s Mental Health, 12(6), 393–400. [DOI] [PubMed] [Google Scholar]
- Pajulo M, Pyykkönen N, Kalland M, Sinkkonen J, Helenius H, Punamäki RL, & Suchman N (2012). Substance-abusing mothers in residential treatment with their babies: Importance of pre-and postnatal maternal reflective functioning. Infant Mental Health Journal, 33(1), 70–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patra J, Bakker R, Irving H, Jaddoe VW, Malini S, & Rehm J (2011). Dose–response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)da systematic review and meta-analyses. BJOG: An International Journal of Obstetrics & Gynaecology, 118(12), 1411–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Evans-Polce R, Wagner AC, & Mehus CJ (2020). High-intensity drinking by parental status: Differences by age and sex. Addictive Behaviors, 102, 106180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltier MR, Verplaetse TL, Mineur YS, Petrakis IL, Cosgrove KP, Picciotto MR, & McKee SA (2019). Sex differences in stress-related alcohol use. Neurobiology of Stress, 10, 100–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers CS, Lang AJ, Twamley EW, & Stein MB (2003). Sexual trauma and pregnancy: A conceptual framework. Journal of Women’s Health, 12(10), 961–970. [DOI] [PubMed] [Google Scholar]
- Ross LE, & Dennis CL (2009). The prevalence of postpartum depression among women with substance use, an abuse history, or chronic illness: A systematic review. Journal of Women’s Health, 18(4), 475–486. [DOI] [PubMed] [Google Scholar]
- Singleton EG, Henningfield JE, & Tiffany SE (1994). Alcohol craving questionnaire: ACQ-Now: Background and administration manual. Baltimore: NIDA Addiction Research Centre. [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, & Gratz KL (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. [DOI] [PMC free article] [PubMed] [Google Scholar]


