Abstract
The purpose of this short report is to illustrate the implementation of a RIS function for balancing radiological activities and workloads between two different teams of radiologists from the same Diagnostic Department during emergency nights and holiday shifts. One group is from the main hospital, Arcispedale S.Maria Nuova di Reggio Emilia, and the other group belongs to the five minor hospitals in the district of Reggio Emilia.
The implementation of a dedicated balancing function in the RIS system successfully allows the balancing of the radiological activity between two or more teams of different radiologists, while preserving the care continuity of care and the involved workers’ experience and confidence in reporting.
Keywords: Workload, Balancing, Nightshifts, RIS function
Introduction
Since 2017, the two public administration institutions (the main one, named ASMN, and the USL which was comprised of 5 smaller hospitals in the district) have been merged into a single unit: the local health authority of Reggio Emilia (Italy). However, the Diagnostic Imaging Department has been unique—cross-company—since 2002.
A shared RIS/PACS system, already installed in 2006, allowed all Diagnostic Department radiologists to access the clinical data and history of patients from the whole 6-hospital group throughout the whole province of Reggio Emilia. In the main institution ASMN, a radiologist worked during holiday and night shifts; a second radiologist worked holiday and night shifts for the whole AUSL 5 hospitals. The Reggio Emilia's Diagnostic Department performs about 40,000 examinations/year during night shifts and about 10,000 examinations/year during Sunday/holiday work shifts (which assists over 532,000 inhabitants).
Before 2017, the ASMN and AUSL radiologists each separately covered their own hospital/hospital system. During night shifts, radiographic and CT exam reports were handled by the two aforementioned on-duty radiologists (one belonging to the ASMN team and the second to the AUSL one). AUSL’s radiologists (25 involved in the night shift in the year 2019) reported only the radiographic and CT examinations (without contrast media) requested from AUSL emergency rooms and AUSL in-patients, in teleradiology only for non-deferrable urgency/emergency exams. The teleradiology access protocol is compliant with the indications of the Italian Society of Medical Radiology (SIRM), of the Italian Higher Institute of Health (ISS) [1]; it adheres to the indications of the European Society of Radiology as well [2]. The ASMN’s radiologists (22 involved in the night shift in the year 2019) reported the radiographic and CT examinations requested from ASMN emergency rooms and in-patients from a PACS workstation placed within the Reggio Emilia hospital. Patients from the peripheral emergency departments requiring CT evaluation with the administration of a contrast medium are also transferred to the main ASMN hospital. Usually, ASMN radiologists reported more complex cases compared to the AUSL institution due to clinical questions, type of patients, and diagnostic methodologies adopted in ASMN routine practice.
Since 1999, the radiographer executing the exam, upon its completion, assigned it through RIS to the on-duty radiologist from their institution.
Methods
Workload Assessment
Since 2012, the Diagnostic Department implemented the average standard reporting times indicated by the Italian Society of Medical Radiology (SIRM) [3], for the quantitative evaluation of workloads.
According to SIRM, the average reporting time (including justification of examination, informed consent, verification of appropriateness—expressed in minutes) is 19.8 min for CTs without contrast medium, 30.4 min for CTs with contrast medium, 7 min for chest radiographs, and 6.7 min for all other plain radiographs—see Table 1 for details.
Table 1.
Average radiologist time per exam including justification of examination, informed consent, and verification of appropriateness (minutes) performance including justification of examination, informed consent, and verification of appropriateness (minutes)—table extracted by reference [3]—“METODOLOGIA DI DETERMINAZIONE DEI VOLUMI DI ATTIVITÀ E DELLA PRODUTTIVITÀ DEI MEDICI RADIOLOGI NOMENCLATORE SIRM-SNR Gruppo di lavoro misto SIRM/SNR. Il Radiologo. 2004”
| Macro-class | Average radiologist time per exam including justification of examination, informed consent, and verification of appropriateness (minutes) performance including justification of examination, informed consent, and verification of appropriateness (minutes) |
|---|---|
| Chest X-Ray | 7.0 |
| x-ray exams (excluding chest) | 6.7 |
| Barium contrast exams | 36.0 |
| X-ray exams with iodinated contrast | 42.5 |
| Mammography (excluding screening) | 22.9 |
| Ultrasound exams | 24.5 |
| CT without contrast medium | 19.8 |
| CT without and with contrast medium | 30.4 |
| MR without contrast medium | 24.2 |
| MR without and with contrast medium | 37.0 |
| Diagnostic angiography | 39.9 |
| Vascular interventions | 82.2 |
| Extravascular interventional | 63.2 |
| US-guided biopsies | 37.1 |
| CT-guided biopsies | 45.0 |
| DEXA | 6.1 |
Description of the Problem
We calculated the mean workload of one radiologist belonging to each of the two teams—ASMN or AUSL—during a night/holiday shift as the sum of their reported exam times (defined by SIRM—Table 1). The workload is calculated as the sum of the reporting times defined by SIRM multiplied for the number of reported exams.
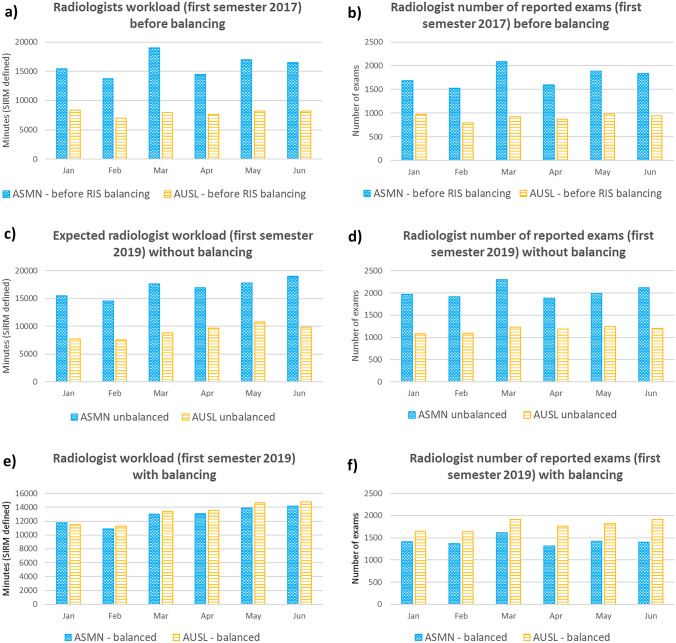
From the above-mentioned evaluation, it was evident that there was an imbalance in the quantitative workload of the two on-duty radiologists, in terms of the number of exams and their complexity (i.e., radiographies vs. CT exams (Fig. 1a, b)).
Fig. 1.
Radiologists’ workload—calculated as the sum of the radiologist’s reported exam weight (intended as average standard reporting times in minutes established by the Italian Society of Medical Radiology) or as the number of exams and grouped by month. a, b A period before intervention (first semester of 2017). c, d The first half of 2019 showing the workload we would have obtained without balancing, and e, f the effective workload due to load balancing
As shown in Table 2, it is clear that the mean workload for the ASMN radiologist (measured in hours) per night shift (ranging from 7.02 to 7.60) was about two times higher than for the AUSL radiologist (which ranged instead from 3.16 to 3.53 h). In terms of exam complexity, the relative percentage of CT exams compared to X-rays was systematically about 35% higher for the ASMN radiologist (e.g., in 2015, the percentage of CT overall examinations was 13.6% for ASMN and 9.9% for AUSL).
Table 2.
Emergency and internal patient radiologist workload [4] per year
| Company | Year | Mean workload per night shift (hours) | Mean number of exams per night shift | Total number of emergency exams | CT (%) | 2D X-rays (%) | Total number of emergency exams during night/holiday shifts |
|---|---|---|---|---|---|---|---|
| ASMN | 2012 | 7.02 | 49.4 | 55,191 | 11.5% | 88.5% | 26,362 |
| AUSL | 3.17 | 22.7 | 58,797 | 8.7% | 91.3% | 15,578 | |
| ASMN | 2013 | 7.29 | 50.8 | 55,407 | 12.5% | 87.5% | 26,443 |
| AUSL | 3.16 | 22.3 | 55,862 | 8.9% | 91.1% | 14,617 | |
| ASMN | 2014 | 7.60 | 52.6 | 56,655 | 12.8% | 87.2% | 27,029 |
| AUSL | 3.53 | 24.9 | 57,424 | 9.9% | 90.1% | 15,964 | |
| ASMN | 2015 | 7.38 | 50.9 | 57,810 | 13.6% | 86.4% | 27,560 |
| AUSL | 3.43 | 24.1 | 60,580 | 9.9% | 90.1% | 17,336 | |
| ASMN | 2016 | 7.02 | 47.4 | 58,266 | 14.6% | 85.4% | 27,599 |
| AUSL | 3.53 | 24.9 | 61,745 | 10.5% | 89.5% | 17,690 |
The mean workload (of one radiologist belonging to each of the two teams—ASMN or AUSL) is calculated as the sum of the reporting times defined by SIRM multiplied for the number of reported exams. Workload per year between ASMN and AUSL p-value is < 0.0001 and t-value is + 28.1 demonstrating that they are statistically different
The workload balance situation we want to achieve is having an equal workload (as defined by SIRM—see the “Workload Assessment” section, calculated as the individual percentages with respect to the total) for the two radiologists, within 5% (i.e., 51–49%).
Adopted Actions and Procedure Details
During the second half of 2017, the head of our Diagnostic Imaging Department, on a mandate from the General Management of the USL Company, commissioned our RIS system supplier (Fenix v. 3.16.0916—Elco Cairo Montenotte SV, Italy) to develop a method to balance the radiologists’ workload during night shifts and holidays. Both radiologists are required to carry out their reporting activities from PACS stations installed at the Arcispedale S.Maria Nuova of Reggio Emilia (the telereporting access protocol remains valid only for the emergency departments of the province).
The new RIS-integrated software uses an algorithm to balance workloads based on the average standard reporting times indicated by the Italian Society of Medical Radiology, mentioned above.
In this new workflow, the radiographer who executes the exams (X-ray and CT scans) does not assign it to the on-duty radiologist of their institution anymore, but, upon exam completion, the exam is assigned to a general fictitious “guardian physician.”
Description of the Algorithm
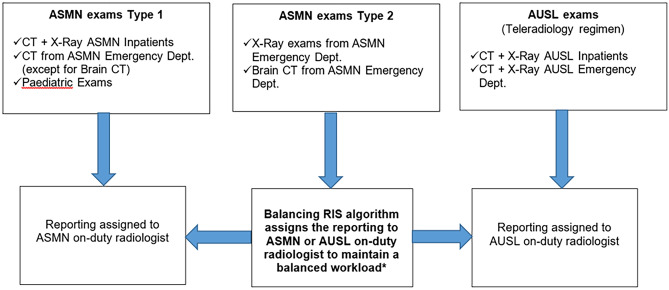
Our RIS-implemented function, based on the incremental amount per individual on-duty radiologist of their workload (based on standard average times of the radiological exams indicated by the SIRM), assigns the completed exams to the ASMN radiologist or the AUSL one, operating as follows:
All exams (X-rays and unenhanced CT) acquired by the radiographers in the peripheral hospitals and requested from AUSL emergency rooms and hospital wards are assigned to the AUSL radiologist operating in teleradiology;
CT exams performed in ASMN emergency rooms and hospital wards and radiographic exams acquired in ASMN requested from internal hospital wards are assigned to the ASMN radiologist;
Conventional X-ray exams and head CT without contrast media coming from the ASMN emergency room can be assigned to both radiologists, in order to balance both radiologists’ workloads;
Contrast-enhanced CT exams requested from emergency rooms in peripheral hospitals are assigned to an AUSL radiologist, even if the patient is transferred to ASMN radiology (as requested by Italian regulations that do not allow to perform contrast-enhanced CT examinations without the presence of a radiologist).
In addition, there are further rules in the assignments to ensure diagnostic continuity. All exams of an episode/request are attributed to the same radiologist. Specific complex cases, namely, pediatric emergency exams, are assigned the ASMN radiologists due to their higher experience in these cases (pediatric patients are usually admitted in Reggio Emilia, both in emergency and daily practice).
The interested readers can see Appendix 1 for further details.
Results and Discussion
Our results confirm a balanced distribution of workloads between the two radiologists, as expected. Figure 1 shows a comparison of the workload data, calculated as the sum of the radiologist’s time or the number of exams, with and without automatic balancing. Figure 1a, b refers to a period before intervention (first semester of 2017). Figure 1c, d refers to the first half of 2019 showing the workload we would have obtained without balancing, and Fig. 1e, f refers to the effective workload due to load balancing. In Fig. 1a, b, it is also worth noting that the two radiologists’ workloads are about 67% for ASMN and 33% for AUSL, while in Fig. 1e, f, the workloads are respectively 49.2% vs. 50.8%.
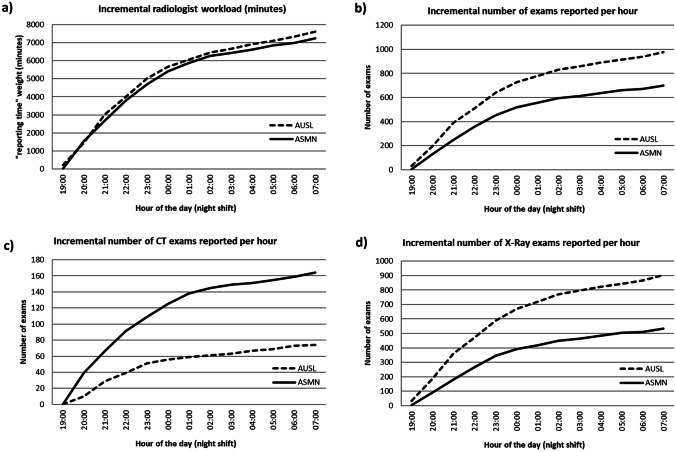
In Fig. 2, we show the effective average values of a night shift (referring to the period 21.04.2019–06.05.2019), where we can highlight the effect of our applied algorithm. Before our algorithm application (first semester of 2017), the mean (standard deviation) shift workload (minutes) for the ASMN radiologist was 530 (110) while for the AUSL radiologist was 290 (80). After our intervention (period 21.04.2019–06.05.2019), the mean shift workload (minutes) for the ASMN radiologist became 460 (90), while for the AUSL radiologist, we obtained 450 (70). From this data, we can confirm that before the intervention, the mean workloads for the two radiologists were statistically different, while after our algorithm application, they balanced out.
Fig. 2.
Average values of a night shift (referring to the period 21.04.2019–06.05.2019). a The value shown on the Y-axis represents the sum of the weights of the exams assigned by the RIS to the AUSL/ASMN radiologist as the shift hours go by. The effect of the algorithm, which equally divides the workload between the two radiologists, is evident. b The value shown on the Y-axis represents the sum of the number of exams assigned by the RIS to the AULS/ASMN radiologist as the shift hours go by. c The value shown on the Y-axis represents the sum of the number of CT scans assigned by RIS to the AUSL/ASMN radiologist as the shift hours pass. d The value shown on the Y-axis represents the sum of the number of X-ray exams assigned by RIS to the AUSL/ASMN radiologist as the shift hours pass
It is worth noting (Fig. 2a) that from the beginning of night work shifts (starting from 19:00) to their end (07:00 of the following day), the examination weight sum (referred to both CT and 2D X-rays, expressed as “reporting time” in minutes) by the ASMN and AUSL radiologists grows almost identically. On the other hand, the number of exams reported in the same work shift (from 19:00 to 07:00 of the following day, Fig. 2b) is different. Assuming that reporting a CT examination is more complex than reporting a 2D X-ray (as mentioned above 19.8 min vs. 6.7 min), we can confirm that the ASMN radiologist remains the one in charge of reporting the former exam category.
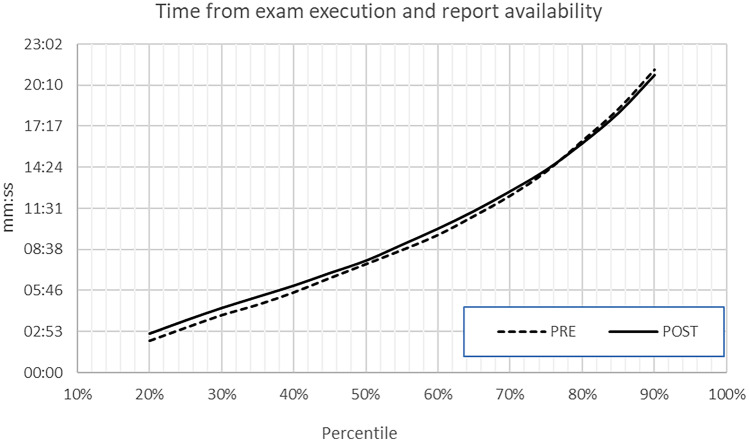
Reporting Efficiency: Effective Cycle Time Analysis
In order to verify that the introduction of our automatic exam assignment function did not change cycle times and, especially, it did not generate adverse effects on the reporting times, we also performed an analysis on pre- and post-intervention situations. To assess that the introduction of our algorithm did not affect the efficiency of our department, we checked a figure of merit, usually employed also in our bi-annual budget assessments. We plot the percentile of reporting exam time (x-axis, calculated as the time between the exam completion and the report generation) vs. the time needed to achieve that percentile (hh:mm), as shown in Fig. 3. The “pre” curve refers to all the emergency exams performed during the night shifts in the second semester of 2016 (pre-intervention) and the “post” curve to the second semester of 2017 (post-intervention). From our results, we did not find statistical differences in those two curves (Wilcoxon’s test p-value < 0.05). From our results, we showed that the balancing process did not increase the effective reporting exam times that is, for sure, an important issue for the patients.
Fig. 3.
Reporting efficiency: effective cycle time analysis: the percentile of reporting exam time (x-axis, calculated as time between the exam completion and the report generation) vs. the time needed to achieve that percentile (hh:mm). The “pre” curve refers to all the emergency exams performed during the night shifts in the second semester of 2016 (pre-intervention) and the “post” curve to the second semester of 2017 (post-intervention)
In late 2021, a further implementation tackled the task of dividing holiday daytime workload among three radiologists instead of two, which is a situation occurring when an event (i.e., large-scale accidents) causes a huge flux of patients to the emergency rooms (fortunately, to date, this feature has not yet been activated).
Our workload balancing function is constantly checked with a dedicated function (dashboard) present on our RIS. The night shift workloads are periodically presented and commented on within the quarterly meetings of the Diagnostic Department committee. During these meetings, we confirmed that the intervention ensured balance in the workload. However, our balancing algorithm assigned to the AUSL radiologist both teleradiology exams from AUSL peripheral hospitals and from the emergency ASMN department which instead need to be reported onsite. The AUSL radiologists sometimes reported some logistical difficulties in reaching the Reggio Emilia hospital for the night shifts [5] Fig. 4.
Fig. 4.
Workload calculation is based on the incremental amount per individual on-duty radiologist based on standard average times of the radiological exams indicated by SIRM
Known Limitations
Our workload-balancing algorithm testing described in this paper is limited to the Reggio Emilia Diagnostic Department performing about 40,000 examinations/year during the night shift. Reggio Emilia's radiologists shared and were allowed to adopt the “exam weighting” (as average standard reporting times in minutes) proposed by SIRM [3].
Conclusion
The implementation of a dedicated function in the RIS system successfully allows the balancing of the radiological activity between two or more teams of different radiologists, while preserving the care continuity of care and the involved workers’ experience and confidence in reporting [4, 6]. This report describes the RIS function actually employed in our institution that assists the entire province of Reggio Emilia (more than 532,000 inhabitants), which could be easily employed even in other Radiology Departments.
In addition, a redistribution of the workload could positively affect the attention spans of the radiologist; this data, however, is not confirmed yet, due to not being able to quantitatively assess how many exams a radiologist can review in any timeframe while maintaining acceptable diagnostic accuracy [7, 8].
Acknowledgements
The authors gratefully acknowledge the support in developing and optimizing the toll described in this paper of Luca Del Giudice and Andrea Silvestri from Elco Company.
Appendix 1
Balancing algorithm rules.
All the “ASMN exams Type 1” are reported only by the ASMN on-duty radiologist.
All the “AUSL exams (teleradiology regimen)” are reported only by the AUSL on-duty radiologist.
At the beginning of the workshifts, if the two on-duty radiologists did not yet report any exams, the first exam belonging to the “ASMN exams Type 2” is assigned by default to the AUSL on-duty radiologist (all exams of an episode/request are attributed to the same radiologist).
The following “ASMN exams Type 2” exam is assigned to the on-duty radiologist who has the lowest workload (SIRM based) at the exam completion time. All exams of an episode/request are attributed to the same radiologist.
Author Contribution
All authors contributed to the study conception and design. Material preparation and data collection were performed by AN and MB. The first draft of the manuscript was written by AN and MB, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study was partially supported by the Italian Ministry of Health—Ricerca Corrente.
Data Availability
The data could be available upon request to the corresponding author.
Declarations
Compliance with Ethical Standards
Institutional Review Board approval was not required because it is a Clinical Audit about a technical development; no patient data were used. Only data relating to the productivity of the radiology department in terms of the number of tests and execution or reporting times were used.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Working Group for Quality Assurance in Diagnostic and Interventional Radiology 2010 – 10/44 Linee guida per l’assicurazione di qualità in teleradiologia. 35 p. (in Italian). https://www.iss.it/web/guest/ricerca?p_p_id=com_liferay_portal_search_web_portlet_SearchPortlet&p_p_lifecycle=0&p_p_state=maximized&p_p_mode=view&_com_liferay_portal_search_web_portlet_SearchPortlet_mvcPath=%2Fview_content.jsp&_com_liferay_portal_search_web_portlet_SearchPortlet_assetEntryId=5192309&_com_liferay_portal_search_web_portlet_SearchPortlet_type=content&p_l_back_url=https%3A%2F%2Fwww.iss.it%2Fweb%2Fguest%2Fricerca%3Fp_p_id%3Dcom_liferay_portal_search_web_portlet_SearchPortlet%26p_p_lifecycle%3D0%26p_p_state%3Dmaximized%26p_p_mode%3Dview%26_com_liferay_portal_search_web_portlet_SearchPortlet_redirect%3Dhttps%253A%252F%252Fwww.iss.it%252Fweb%252Fguest%252Fricerca%253Fp_p_id%253Dcom_liferay_portal_search_web_portlet_SearchPortlet%2526p_p_lifecycle%253D0%2526p_p_state%253Dnormal%2526p_p_mode%253Dview%26_com_liferay_portal_search_web_portlet_SearchPortlet_mvcPath%3D%252Fsearch.jsp%26_com_liferay_portal_search_web_portlet_SearchPortlet_keywords%3D10%252F44%26_com_liferay_portal_search_web_portlet_SearchPortlet_formDate%3D1672224543602%26_com_liferay_portal_search_web_portlet_SearchPortlet_scope%3Dthis-site
- 2.European Society of Radiology (ESR) ESR white paper on teleradiology: an update from the teleradiology subgroup. Insights Imaging. 2014 Feb;5(1):1–8. 10.1007/s13244-013-0307-z. Epub 2014 Jan 18. PMID: 24443129; PMCID: PMC3948905 [DOI] [PMC free article] [PubMed]
- 3.Bellandi, Giuseppe & Dalla, Francesco & Vincenzo, Palma & Ginevra, Antonio & Miele, Vittorio & Rotondo, Antonio & Siani, Alfredo & Vimercati, Franco & Beltrami, Paola & Batistini, Tommaso & Bertozzi, Luca & Ims, Sisto & Borello, Elisabetta & Conti, Pietro & Grignaffini, Guido. 2004. METODOLOGIA DI DETERMINAZIONE DEI VOLUMI DI ATTIVITÀ E DELLA PRODUTTIVITÀ DEI MEDICI RADIOLOGI NOMENCLATORE SIRM-SNR Gruppo di lavoro misto SIRM/SNR. Il Radiologo
- 4.Marla B K Sammer, Andrew Stahl, Eray Ozkan, Andrew C Sher Implementation of a software distribution intervention to improve workload balance in an academic pediatric radiology department 5 J Digit Imaging . 2021 Jun;34(3):741–749. 10.1007/s10278-021-00451-4. Epub 2021 Apr 9. 10.1007/s10278-021-00451-4 [DOI] [PMC free article] [PubMed]
- 5.Rohatgi S, Hanna TN, Sliker CW, Abbott RM, Nicola R. After-hours radiology: challenges and strategies for the radiologist. AJR Am J Roentgenol. 2015;205(5):956–961. doi: 10.2214/AJR.15.14605. [DOI] [PubMed] [Google Scholar]
- 6.Kelleher MS, Jr, Keller J, Blanchette S, Rolen MF, Bokhari SA. The implementation and impact of a quality improvement program in emergency radiology. J Am Coll Radiol. 2016;13(7):878–880. doi: 10.1016/j.jacr.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 7.Alexander R, Waite S, Bruno MA, Krupinski EA, Berlin L, Macknik S, Martinez-Conde S: Mandating limits on workload, duty, and speed in radiology. Radiology. 2022 Aug;304(2):274–282. 10.1148/radiol.212631. Epub 2022 Jun 14. PMID: 35699581; PMCID: PMC9340237 [DOI] [PMC free article] [PubMed]
- 8.Reiner BI, Krupinski E. The insidious problem of fatigue in medical imaging practice. J Digit Imaging. 2012;25(1):3–6. doi: 10.1007/s10278-011-9436-4.PMID:22143410;PMCID:PMC3264708. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data could be available upon request to the corresponding author.