Abstract
Two hundred nineteen Clostridium difficile isolates from 22 serogroups were screened for changes in the genes coding for toxin B (tcdB) and toxin A (tcdA). Parts of the toxin genes were amplified, and the PCR fragments were checked for length polymorphisms and cut with several restriction enzymes to monitor restriction fragment length polymorphisms (RFLPs). For 47 strains (21%), differences in the toxin genes were found compared to the toxin genes of reference strain VPI 10463. Polymorphisms were usually observed in both toxin genes. RFLPs were more commonly found in the tcdB gene, in which a single restriction enzyme could give up to five different patterns. Restriction sites seemed to be less heterogeneous in the tcdA gene, in which for most enzymes only two different RFLPs were recognized. However, deletions were observed in tcdA, and four new types of shortened tcdA genes are described. According to the changes in their toxin genes, variant strains could be divided into 10 groups (toxinotypes I to X). A toxinotype was characterized by similar patterns of changes in the toxin genes and in other regions of the pathogenicity locus and also similar pulsed-field gel electrophoresis patterns. Variant toxinotypes were found in 9 of the 22 serogroups studied, and some toxinotypes were clearly associated with specific serogroups. Toxinotype VIII is characteristic for all strains of serogroup F. Other serogroups in which variant toxinotypes were commonly found are A1, A15, E, and X. Testing of variability in C. difficile toxin genes not only might be useful as a molecular typing system but also could have implications in diagnostics and pathogenesis.
Clostridium difficile is the main etiological agent of antibiotic-associated diarrhea (AAD) and pseudomembranous colitis (PMC) (1, 11). Its virulence factors are two high-molecular-weight toxins, toxin A (enterotoxin; TcdA) and toxin B (cytotoxin; TcdB), whose in vivo synergistic actions have been suggested previously (13, 19). Both toxins are usually found in toxinogenic strains. However, recently, two types of strains which produce toxin B but no toxin A, as far as the latter is detected by immunological methods, have been described. Compared to reference strain VPI 10463, these strains show several differences in their toxin genes (3, 7, 12, 21). Other groups have reported variant strains as well, which suggests that they could be more common. McMillin et al. (14) found a strain which produces a shorter toxin A, but the strain was not further investigated on the molecular level. Another isolate with a modified tcdA gene was observed by Boondeekhun and his group (2), but there again, it was not investigated in detail.
The genes coding for both toxins (tcdB and tcdA) of strain VPI 10463 have been sequenced (25). Together with three accessory genes (tcdC, tcdD, and tcdE), they form the pathogenicity locus (PaLoc), of 19.6 kb, which is found only in toxinogenic strains (4, 9). In nontoxinogenic strains, the pathogenicity locus is replaced by 115 bases. The tcdB and tcdA genes are similar in size (7 and 8 kb, respectively), and both have repetitive sequences at their 3′ ends. A high degree of homology between these two genes has been demonstrated (28). In both of them, three domains corresponding to three functional domains of the toxins could be differentiated: their C-terminal repeats are receptor binding regions, the central part is needed for translocation, and the N-terminal domain has a catalytic function (25, 27).
Most epidemiological studies of C. difficile have been performed by using several typing systems. Serogrouping by slide agglutination with rabbit antisera, together with the protein profiles obtained by polyacrylamide gel electrophoresis (PAGE), enables the differentiation of 14 serogroups, designated by capital letters (A, B, C, D, F, G, H, I, K, S1, S2, S3, S4, and X) (6, 23). In serogroup A, another 20 subgroups (subgroups A1 to A20) can be distinguished by PAGE (6); these subgroups possess serogroup-specific somatic antigens but share a common flagellar antigen responsible for cross-agglutination on slides (5).
In a previous work, we established a PCR protocol for amplifying the whole sequences of C. difficile toxin genes and used it for the characterization of two strains with variations in the toxin genes (21). In the present study, we have extended our analysis to the entire PaLoc and applied it to a large selection of C. difficile isolates in order to search for correlations between such a novel toxinotyping approach and the serotyping scheme reported before.
MATERIALS AND METHODS
Selection of C. difficile isolates.
Two hundred nineteen toxinogenic isolates belonging to 22 different serogroups (serogroups A1 to A6, A8, A9, A11, A13 to A16, C, E, F, G, H, K, S1, S3, and X) were selected from the laboratory collection at the Microbiology Unit (Catholic University of Louvain, Brussels, Belgium), with care taken to choose strains isolated at different times and from different geographical locations. The number of strains in each serogroup was proportional to the epidemiological importance in clinical practice. Up to 25 isolates from large serogroups, such as A1, G, and C, were studied. Two to five isolates were taken from small or newly established serogroups. Two strains were from unknown serogroups: one of them was isolate 8864 (obtained from the Swedish type culture collection; strain 20309), and the other was isolated from a patient suffering from PMC.
Screening for changes in PaLoc.
For PCRs, crude DNA was prepared with Chelex 100 Resin (Bio-Rad, Nazareth, Belgium) as described by O’Neill et al. (18). For strains whose crude DNA did not give good results by PCR, pure DNA was prepared by the standard phenol-chloroform procedure described by van Dijck et al. (24). The PCR fragments used for amplification of the entire PaLoc are summarized in Fig. 1A. Primer sequences and amplification conditions for fragments covering the tcdB and tcdA genes (B1 to B3 and A1 to A3) have been described before (21). Four additional PCRs were performed to cover the upstream and downstream regions of the toxin genes (PL fragments) and to analyze the entire PaLoc. Primer sequences have been described previously (4, 10) and will be summarized again here. For amplification of PL1, primers Tim5 (5′-CACAGATGCTTTTAGCAGGAA-3′) and PrimexD (5′-TCATCTACTGAGTTATTTCTTGCTA-3′) were used; for amplification of PL2 we used Lok3 (5′-TTTACCAGAAAAAGTAGCTTTAA-3′) and PrimexB (5′-ACATATTCATCTTCTTGAGTACGA-3′); for amplification of PL3 the primer pair was Lok6 (5′-GTTGTTTAGATTTAGATGAAAAGA-3′) and PrimexA (5′-CTTGGTCTAATGCTATATGCGAG-3′); for amplification of PL4 we used primers Lok5 (5′-TGGAGTAAAAGCCCCTGGGA-3′) and Lok1 (5′-AAAATATACTGCACATCTGTATAC-3′).
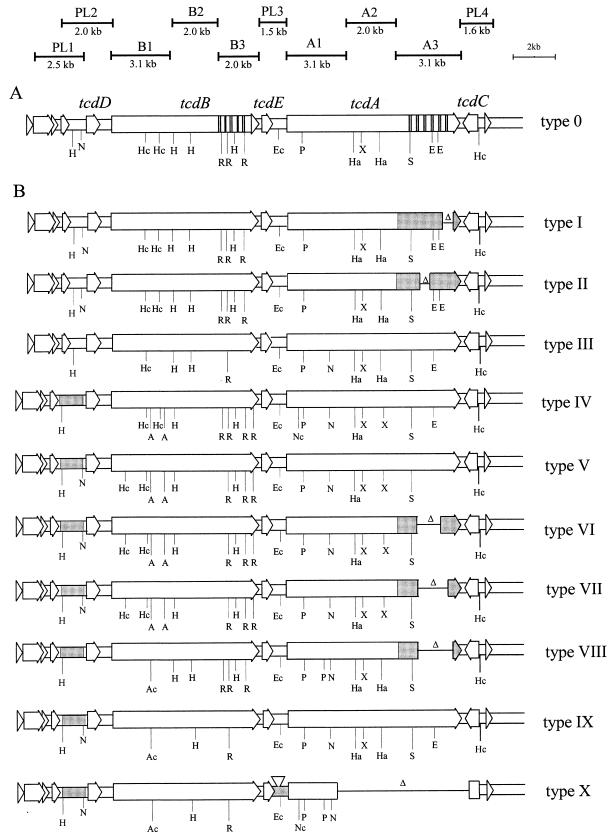
FIG. 1.
Representation of five open reading frames, two toxin genes (tcdA and tcdB), and three additional genes (tcdC, tcdD, and tcdE) of the PaLoc in strain VPI (toxinotype 0) in comparison to those of variant toxinotypes (toxinotypes I to X). The hatched areas represent the repetitive regions of both toxin genes. (A) Relative positions and sizes of 10 overlapping PCR fragments used to amplify the whole PaLoc sequence. (B) Schematic representation of length and restriction site polymorphisms found in different toxinotypes. Gray regions are those in which length polymorphisms were detected: deletions in the A3 fragments of toxinotypes I, II, VI, VII, and VIII or insertions in toxinotypes IV to X. Δ, relative positions and sizes (not in scale) of the deletions. Only some of the restriction sites tested in each PCR fragment are shown, and not all restriction sites of the same enzymes are shown (known for VPI 10463 sequence). A, AccI; Ec, EcoRV; E, EcoRI; H, HindIII; Hc, HincII; h, HaeIII; N, NsiI; Nc, NcoI; P, PstI; R, RsaI; S, SpeI.
PCRs for amplification of PL fragments were performed in a 50-μl volume containing 10 mM Tris-HCl (pH 8.3), 50 mM KCl, 0.001% gelatin, 2 mM MgCl2, deoxynucleoside triphosphates each at a concentration of 0.2 mM, 5 pmol of each primer, and 0.5 U of Taq polymerase (Perkin-Elmer, Zaventem, Belgium). A Perkin-Elmer Cycler 2400 was used. The PCR protocols started with denaturation at 93°C for 3 min, and this was followed by 30 cycles at 52°C for 1 min, 72°C for 1 min, and 93°C for 1 min. The reaction was terminated by a 10-min incubation at 72°C.
Fragments were visualized on 1.5% agarose, and the length polymorphisms of uncut amplicons were checked. To obtain restriction site polymorphisms, each fragment was cut with a set of restriction enzymes. Fragment B1 was digested with HincII, EcoRI, and AccI; B2 was digested with HindIII, RsaI, NsiI, and EcoRV; and B3 was digested with HindIII, RsaI, Sau3AI, and HincII. Digestions of A1 were performed with PstI, NsiI, NcoI, and RsaI; digestions of A2 were performed with AccI, EcoRV, HaeIII, and XbaI; and digestions of A3 were performed with EcoRI and SpeI. PCR fragment PL1 was cut with HindIII, PL2 was cut with NsiI, PL3 was cut with EcoRV, and PL4 was cut with HincII and SpeI.
PFGE.
For pulsed-field gel electrophoresis (PFGE), the strains were grown in peptone-yeast extract-glucose broth for 5 h. Preparation of cultures, digestion of DNA with SmaI, and experimental conditions were as described previously (24). Strains with restriction pattern differences of from one to three bands were considered closely related, and strains with patterns with more than three band differences were considered unrelated.
Serogrouping and in vitro toxin production.
The serogroup of each strain was determined by the method described by Delmée et al. (6) and was confirmed by PAGE as reported previously (6). All C. difficile isolates were tested for in vitro cytotoxin production on HeLa cells. Toxin A production was detected by the Premier C. difficile Toxin A assay (Meridian Diagnostics, Cincinnati, Ohio) according to the instructions of the manufacturer. The results were analyzed by obtaining spectrophotometric readings at wavelengths of 450 and 630 nm.
RESULTS
In a first step, 3 of 10 PCR fragments covering the entire PaLoc (fragments B1, B3, and A3) were selected to screen for the variations in toxin genes (Fig. 1A). These parts of the genes were chosen because they had been shown before to be variable and had been characterized to some extent in two variant strains (strain 8864 and the reference strain of serogroup F, ATCC 53598) (21, 26). Additionally, the repetitive sequences covered by PCR fragments A3 and B3 are prone to homologous recombination and are predestined for deletions or insertions. Fragments B1, B3, and A3 were amplified for all 219 strains studied, and among them, fragment A3 of the tcdA gene was the only one in which deletions were observed. The different types of deletions by comparison to the sequence of strain VPI 10463 are shown in Fig. 2. There was no A3 amplicon in strain 8864 (data not shown). Strains of serogroup F displayed a typical major deletion which was also observed in 12 other strains belonging to serogroup X (type 7; Fig. 2). Four strains shared a similar 800-bp deletion (type 5; Fig. 2). The type 6 deletion was even more extended but was found in only a single isolate.
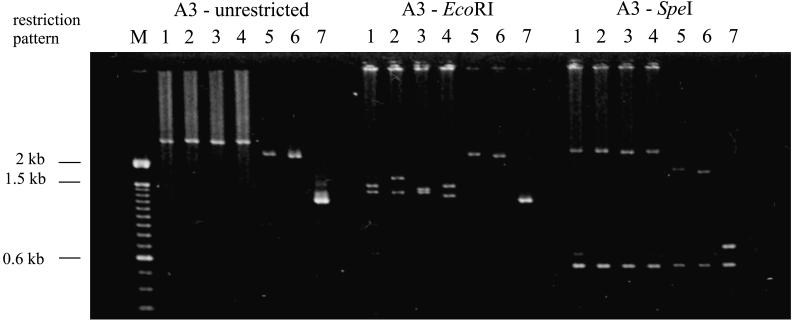
FIG. 2.
Typical length polymorphisms and RFLPs found in repetitive regions of tcdA (A3 PCR). The lane numbers indicate the type of fragment. Type 1 represents strain VPI 10463, type 7 represents the deletion described for serogroup F strains. Two other large deletions are observed in the uncut PCR fragment (types 5 and 6). With EcoRI further differences in this PCR fragment are obtained: the RFLPs in types 3 and 4 are probably due to minor deletions, and in type 2, the restriction fragments are polymorphic because of one missing EcoRI site. Types 5, 6, and 7 were not restrictable with EcoRI. In all A3 fragments the SpeI restriction sites are conserved.
After comparing the amplicon length with that of control strain VPI 10463, the fragments were digested with several restriction enzymes: B1 with HincII, AccI, and EcoRI, B3 with HindIII, RsaI, and HincII, and A3 with EcoRI and SpeI. The restriction patterns were similar to those of the control strain for 172 isolates (79%). Differences were observed in 47 strains. Digestion of A3 amplicons with EcoRI enabled us to identify two additional deletions: one located upstream of the EcoRI restriction site (type 3; Fig. 2) and the other located downstream (type 4). These deletions were found in one and two strains, respectively. Type 2 of the EcoRI restriction was observed in 11 strains. Type 8 was found in only one isolate and represents a fragment of normal length which could not be restricted with EcoRI (data not shown in Fig. 2).
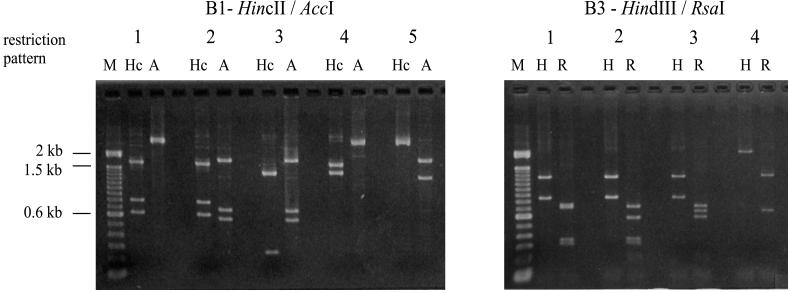
As shown in Fig. 3, HincII and AccI distinguished four restriction patterns different from those of the reference strain (type 1) among the B1 fragments; they concerned 4 (type 2), 6 (type 3), 6 (type 4), and 28 isolates (type 5), respectively. Digestion of B1 with EcoRI resulted in only two different patterns (data not shown). Restriction of B3 with HindIII and RsaI gave three patterns different from that of the reference strain for four (type 2), six (type 3), and nine isolates (type 4), respectively (Fig. 3). Three different restriction patterns were obtained with Sau3AI and two were obtained with HincII (data not shown).
FIG. 3.
Types of polymorphic restriction patterns by B1 PCR and B3 PCR used for toxinotyping. For B1 five patterns (lanes 1 to 5, respectively) of HincII (Hc) and AccI (A) restriction patterns are differentiated, and for B3 four different HindIII (H) and RsaI (R) patterns (lanes 1 to 4, respectively) are obtained. Lane M, 100-bp marker.
In a second step, the 47 strains which had shown differences by comparison with the VPI 10463 strain were studied further; the whole PaLoc regions were amplified with 10 overlapping fragments (fragments B1 to B3, A1 to A3, and PL1 to PL4), and up to four restriction sites per fragment were checked as described in Materials and Methods. Deletions were detected only in the A3 region, and insertions were concentrated outside the toxin genes of PaLoc (Fig. 1B). Among 47 strains that were checked by PL PCRs, 38 had an insertion upstream of tcdD. These were detected in the PL1 PCR or the PL2 PCR. One strain (strain 8864) had a large insertion between tcdB and tcdA (an enlarged PL3 fragment) (data not shown). Among the PL fragments, restriction fragment length polymorphisms (RFLPs) were detected only in PL2 after digestion with NsiI, whereas HindIII in PL1, EcoRV in PL3, and HincII and SpeI in PL4 were conserved.
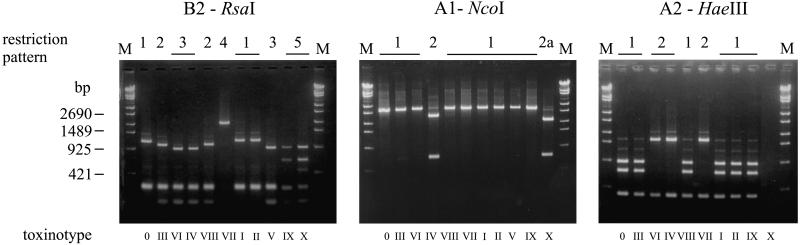
The B2 fragment was polymorphic when it was tested with four different restriction enzymes. Five restriction patterns were obtained with RsaI (Fig. 4), four were obtained with HindIII, and two were obtained with NsiI and EcoRV (data not shown).
FIG. 4.
Restriction patterns obtained with B2, A1, and A2 PCR fragments for the different toxinotypes indicated by Roman numerals. Toxinotype 0 represents reference strain VPI 10463. The RsaI restriction sites in the B2 fragment are very polymorphic, and five different patterns (indicated with Arabic numerals over the lanes) were found. When the same strains were checked for differences by A1 and A2 PCRs, typically only two different patterns were found; here the examples of NcoI digestion of A1 and HaeIII digestion of A2 are shown. For A1 patterns 2 and 2a differ because the A1 fragment is shorter in strain 8864 (see text), but the NcoI restriction site is conserved. Lane M, marker.
In fragments A1 and A2 digested with PstI, NsiI, and NcoI (fragment A1) or EcoRV, XbaI, and HaeIII (fragment A2), the restriction fragments were either the same as those obtained with the standard strain VPI 10463 or changed to a second pattern for all other strains (Fig. 4). Restriction of A1 with RsaI and restriction of A2 with AccI showed no differences in any of the 47 strains.
Definition of toxinotypes.
Among the 219 isolates studied, 47 showed variations in toxin genes when compared with those of the VPI 10463 reference strain. According to the changes in their PaLoc, 10 toxinotypes could be established and were designated by Roman numerals I to X (Fig. 1B). As demonstrated above, the major differences between groups were observed in the B1, B3, and A3 domains of the toxin genes and in the segment upstream of tcdD. Changes characteristic for each toxinotype are summarized in Table 1. Reference strain VPI 10463 was defined as toxinotype 0. A similar toxinotype was observed in the majority of strains (172 of 219). Formerly described variant strains of serogroup F belonged to toxinotype VIII, and isolate 8864 belonged to toxinotype X. For the majority of toxinotypes, more than one isolate was found. The variant strains and their epidemiological data and toxin status are summarized in Table 2.
TABLE 1.
Characteristic changes used for typing of toxin genesa
| Toxino- type | Type of HincII and AccI restrictions for B1 fragment | Type of HindIII and RsaI restrictions for B3 fragment | Type of EcoRI restrictions for A3 fragment | Type of NsiI restrictions for PL2 fragment | Standard strain | No. of strains found |
|---|---|---|---|---|---|---|
| 0 | 1 | 1 | 1 | 1 | VPI 10463 | 172 |
| I | 1 | 1 | 4d | 1 | EX 623 | 2 |
| II | 1 | 1 | 3d | 1 | AC 008 | 1 |
| III | 4 | 4 | 2 | 2 | 44027 | 6 |
| IV | 2 | 2 | 2 | 3i | 55767 | 4 |
| V | 3 | 3 | 8 | 4i | SE 881 | 1 |
| VI | 3 | 3 | 5d | 4i | 51377 | 4 |
| VII | 3 | 3 | 6d | 4i | 57267 | 1 |
| VIII | 5 | 1 | 7d | 3i | 1470 | 25 |
| IX | 5 | 4 | 2 | 4i | 51680 | 2 |
| X | 5 | 4 | NA | 4i | 8864 | 1 |
TABLE 2.
C. difficile strains with variant toxin genes
| Strain | Toxino- type | PFGE type | Serogroup | tcdB | tcdA | Date of isolation (day.mo.yr) | Origina | Patient birth date (yr) | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|
| 38544 | I | NTb | C | + | + | 1.7.1991 | Brussels1, Belgium | 1944 | PMC |
| EX 623 | I | 8 | C | + | + | 19.11.1990 | Brussels2, Belgium | Unknown | AAD |
| AC 008 | II | 9 | A14 | + | + | 7.4.1994 | Paris, France | Unknown | AAD |
| SE 844 | III | 2 | A1 | + | + | 10.4.1995 | Annecy1, France | 1966 | AAD |
| SE 847 | III | 2 | A1 | + | + | 10.4.1995 | Annecy1, France | 1959 | AAD |
| EX 482 | III | 2 | A1 | + | + | 2.1.1990 | Brussels3, Belgium | 1920 | AAD |
| 45129 | III | 2 | A1 | + | + | 7.9.1992 | Brussels4, Belgium | 1939 | AAD |
| 35004 | III | 2 | A1 | + | + | 16.11.1989 | Namur, Belgium | 1932 | PMC |
| 44027 | III | NDc | A1 | + | + | 15.6.1992 | Brussels5, Belgium | 1939 | PMC |
| 55538 | IV | 5a | A1 | + | + | 12.5.1995 | Brussels6, Belgium | 1991 | AAD |
| 55767 | IV | 5b | A1 | + | + | 12.6.1995 | Brussels7, Belgium | 1944 | AAD |
| 40067 | IV | 5b | A1 | + | + | 14.10.1991 | Brussels8, Belgium | 1990 | AAD |
| 7701 | IV | 6 | A5 | + | + | 23.7.1985 | Bouge, Belgium | Unknown | AAD |
| SE 881 | V | 10 | A15 | + | + | 30.8.1995 | Annecy2, France | 1951 | AAD |
| 48489 | VI | 3 | A15 | + | + | 9.4.1993 | Tournai, Belgium | 1931 | PMC |
| 51377 | VI | 4 | A15 | + | + | 11.2.1994 | Mons1, Belgium | 1926 | PMC |
| BR 071 | VI | 3 | A15 | + | + | 3.7.1995 | England | Unknown | AAD |
| 39696 | VI | 4 | E6 | + | + | 19.9.1991 | Brussels6, Belgium | 1980 | AAD |
| 57267 | VII | 4 | E6 | + | + | 21.12.1995 | Brussels9, Belgium | 1946 | AAD |
| 1470d | VIII | 7a | F | + | − | 2.12.1981 | Brussels1, Belgium | 1981 | Asymptomatic |
| 20376 | VIII | 7b | X | + | − | 8.7.1988 | Brussels1, Belgium | 1986 | Asymptomatic |
| 51680 | IX | 11a | A16 | + | + | 17.3.1994 | Mons2, Belgium | 1933 | AAD |
| SE 938 | IX | 11b | A16 | + | + | 5.1.1996 | Annecy2, France | 1931 | AAD |
| 8864d | X | 12 | Unknown | + | − | Unknown | England | Unknown | Unknown |
All toxinotypes except types I and II had changes in both the tcdB and the tcdA toxin genes. Toxinotypes IV to X had an insertion upstream of tcdD, and for toxinotype X another insertion upstream of tcdA was characteristic. The same tcdB type was observed in conjunction with different tcdA genes, like in toxinotypes V, VI, and VII or 0, I, and II. Toxinotypes IX and X had very similar tcdB genes as well. On the other hand, the identical type of tcdA gene was found in toxinotypes IX and III, together with different tcdB genes. These similarities among toxin genes or domains in various toxinotypes probably reflect phylogenetic differences or relationships.
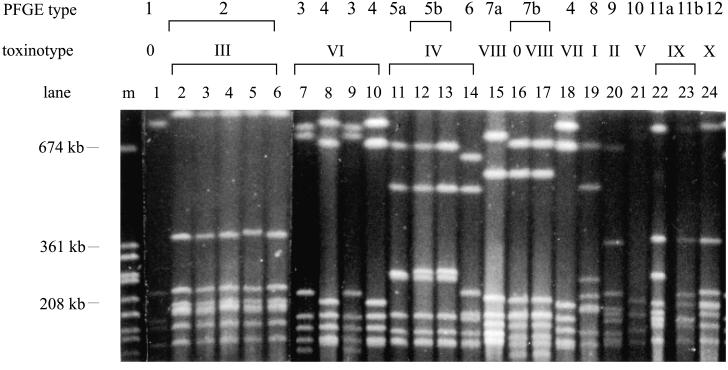
PFGE typing of variant strains.
Twenty-five isolates were subjected to PFGE typing. Two belonged to toxinotype 0 (one of them was VPI 10463 and other was strain 34084, one of a few strains belonging to serogroup X which was not of toxinotype VIII), 2 belonged to toxinotype VIII, 5 belonged to toxinotype III, and the remaining 16 were all variant strains of toxinotypes I, II, IV, V, VI, VII, and IX.
Among 25 strains belonging to 11 different toxinotypes, we could differentiate 15 PFGE patterns (Fig. 5), and isolate 38544 was nontypeable by PFGE because of DNA degradation (data not shown in Fig. 5). Strains belonging to the same toxinotype usually had very similar or identical PFGE patterns. Strains from different toxinotypes could also show identical PFGE profiles. On the other hand, two or three different PFGE types could be recognized in some toxinotypes (toxinotypes IV and VI; Table 2 and Fig. 5).
FIG. 5.
PFGE of SmaI macrorestriction patterns of representative strains from all toxinotypes. Strains grouped together in one toxinotype have identical or closely related PFGE patterns (lanes 2 to 6 or 11 to 13), but in a few cases they show different patterns on PFGE (lanes 7 to 10 and 14). The same PFGE pattern is rarely observed in strains from different toxinotypes (lanes 8, 10, and 18 and lanes 16 and 17).
Prevalence of variant strains in serogroups.
Polymorphic toxin genes were found in strains of 9 of the 22 serogroups studied and in one strain of an unknown serogroup (isolate 8864; Table 3). Toxinotypes II, III, and IX tend to predominate in certain serogroups. Some other toxinotypes (toxinotypes IV, VI, and VIII) are distributed among two different serogroups.
TABLE 3.
Correlation of toxinotypes and serotypes
| Sero- group | No. of strains studied | No. of strains belonging to the following toxinotype:
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | I | II | III | IV | V | VI | VII | VIII | IX | X | ||
| A1 | 25 | 16 | 6 | 3 | ||||||||
| A5 | 3 | 2 | 1 | |||||||||
| A14 | 7 | 6 | 1 | |||||||||
| A15 | 5 | 1 | 1 | 3 | ||||||||
| A16 | 2 | 0 | 2 | |||||||||
| C | 25 | 23 | 2 | |||||||||
| E6 | 3 | 1 | 1 | 1 | ||||||||
| F | 15 | 0 | 15 | |||||||||
| X | 12 | 2 | 10 | |||||||||
| Unknown | 2 | 1 | 1 | |||||||||
With regard to the type of variant strains that they include, serogroups are homogeneous or heterogeneous. In a majority of serogroups (serogroups A2 to A4, A6, A8, A9, A11, A13, G, H, K, S1, and S3) only strains of toxinotype 0 are found. In some serogroups (serogroups C, A14, and A5) variant strains could be found, but they are not common. Other serogroups, like E, F, A15, A1, and X, are more likely to include variant strains. Serogroup F is the only one in which isolates of a single toxinotype and no VPI-like strains were found. A single toxinotype was also found in serogroup A16, but it is a new serogroup and only two isolates were studied. Serogroups A1, A15, and E were heterogeneous because they included VPI-like strains and strains of two additional toxinotypes.
DISCUSSION
Variability in genes coding for virulence factors is not a rare phenomenon. Some examples are the tox and dtxR genes of Corynebacterium diphtheriae (16), cholera toxin subunit B (17), the urease genes of Helicobacter pylori (8, 22), and the flagellin genes of Campylobacter isolates (15). For C. difficile two types of strains with variant toxin genes have been described. For the first type only one isolate is known (strain 8864) (3, 12). The second type was found in strains of serogroup F (7). This serogroup is predominantly found in asymptomatic children. Thus, variant strains were accepted to be rather rare or isolated from populations in which C. difficile is of no clinical significance. However, our study shows that diversity in C. difficile toxin genes is much greater than was previously thought. We have systematically searched for variability in the toxin genes of 219 C. difficile strains and found 47 (21.5%) variant strains. By our screening method we could differentiate 10 groups of polymorphic toxinotypes (Fig. 1B), in addition to the type of the toxin genes found in strain VPI 10463 (toxinotype 0). Strains of one toxinotype are characterized by changes in toxin genes, changes in other regions of the PaLoc, and comparable PFGE macrorestriction patterns for the entire genome. Toxinotyping correlates well with the serotyping scheme because strains with variant types of toxin genes are found in only a few serogroups. Similar to other genotyping methods (24), toxinotyping can further distinguish subgroups within some serotypes (e.g., serogroups A1, E, X, and C).
Two types of changes were already found in the toxin genes of C. difficile: RFLPs and deletions (12, 21, 26). We found that RFLPs are located in both toxin genes, but interestingly, tcdB seems to be much less conserved than tcdA. However, only tcdA has repetitive regions prone to homologous recombination, and deletions are observed only in these parts of the toxin genes. The presence of rather large numbers of different types of toxin genes raises the question of their origin. Although the heterogeneity in C. difficile toxin genes could be due to frequent sporadic mutations, we think that it is more likely that the C. difficile population is, at least with regard to toxin genes, divided into a number of stable subpopulations. Several lines of evidence presented here support the latter hypothesis. (i) For most toxinotypes more than one isolate is known to belong to each toxinotype. With the exception of four strains (see below), the isolates that belong to the same toxinotype are epidemiologically unrelated (Table 2). (ii) Strains allied in one toxinotype show many identical changes in restriction sites or changes in the lengths of their toxin genes. Strains belonging to some toxinotypes also have identical modifications in other regions of the PaLoc. It is rather unlikely that strains with such a high number of identical changes would arise independently as a result of mutations in VPI-like strains. (iii) Strains of the same toxinotype also show identical or similar profiles when they are analyzed by PFGE. This suggests that the whole genome and not only the toxin genes of such strains are similar, which further supports their origination from a common ancestor. Therefore, at least some toxinotypes should be regarded as stable subpopulations of C. difficile isolates, which are spread worldwide.
Certain strains described here might also be sporadic mutants. Strains AC 008, EX 623, and 38544 have toxin genes which differ from VPI-like genes only in small deletions in repetitive regions of tcdA. Isolate 8864 might also be described as a unique mutant since no other strain with the same characteristic deletion in the tcdA gene and an insertion upstream of tcdA was found. The tcdB gene of strain 8864 has several characteristic RFLPs and is, according to the patterns with the restriction enzymes used here, almost identical to the same genes found in strains of toxinotype IX. Therefore, it is possible that isolate 8864 is a mutated strain of toxinotype IX. There might be another reason for the absence of 8864-like isolates. Strain 8864 could not be classified in any serological group known so far. As shown here, strains with the same toxinotypes could be found only among strains in certain serogroups. Other 8864-like isolates might exist, but because they are not included in the known serotyping scheme, they were not included in our study.
The main reason that the heterogeneity of C. difficile toxin genes was not reported before is that variant strains could not be recognized by the diagnostic tests used in a clinical laboratory (culture and the cytotoxicity test [1] and commercial tests [11]). With the exception of strains belonging to toxinotypes VIII and X (3, 7, 12), all variant strains described here produce both toxins and will react with commercially available kits for toxin A detection and all will have toxic effects on cultured cells. Only by certain PCRs could the variations in toxin genes be detected (2, 14). Therefore, variant strains are likely to be detected and correctly identified as C. difficile, but nothing is known at present about their prevalence or their possible connection with some groups of patients, similar to strains belonging to toxinotype VIII, which are found predominantly in asymptomatic children (6).
According to data obtained for known variant strains, they behave similarly to classical C. difficile strains with respect to spreading and causing disease or even relapses (Table 2). Four variant strains of two different toxinotypes described here were isolated from patients confirmed to have PMC, which shows that such strains might also have the potential to cause severe disease. Two isolates of toxinotype III (isolates 45129 and 44027) were isolated from the same patient, but the first isolation was months before the second one, and the patient was hospitalized in different units. Therefore, it is possible that this was an endogenous strain causing a relapse. In another case, two strains of the same toxinotype (strains SE 844 and SE 847) were isolated from the same location on the same day but were isolated from different patients (Table 2). One possibility is that they were transferred from one patient to another or, alternatively, that they were acquired from the environment. This indicates that variant strains spread in a manner similar to that already described for C. difficile (11, 20) and could serve as an explanation for their isolation from geographically remote locations.
Strains with changed toxin genes are also important in studies of molecular biology, biochemistry, and the role of the toxins in disease. Some valuable information has already been obtained from studies of known variants (3, 12, 26). The differences in RFLPs and in the lengths of the toxin genes could eventually correlate with changes in the properties of the variant toxins and, as a consequence, in different pathophysiological effects, as has been shown for toxin B of strain 1470 of serogroup F and for toxin B of strain 8864 (3, 12, 26).
In summary, we have described 10 toxinotypes of C. difficile. Variations in their PaLoc are found in toxin-coding and non-toxin-coding regions. Toxinotypes correlate well with the types obtained by two other typing schemes (serogrouping and PFGE typing), and it is possible that they represent clonal subgroups within C. difficile species. The PCR method for the typing of C. difficile toxin genes could be easily performed in routine laboratory practice, where it could be used to detect and characterize variant strains and to monitor their prevalence. Moreover, it could be useful as a typing method for further discrimination of strains of certain serogroups such as A1 and C, which are often found to cause outbreaks.
ACKNOWLEDGMENTS
This work was supported in part by Deutsche Forschungsgemeinschaft (grant Ei 206/3-2) and the Slovenian Science Foundation (grant ZIT-0056-96).
REFERENCES
- 1.Bartlett, J. G. 1994. Clostridium difficile: history of its role as an enteric pathogen and the current state of knowledge about the organism. Clin. Infect. Dis. 18(Suppl. 4):S265–S272. [DOI] [PubMed]
- 2.Boondeekhun H S, Gurtler V, Odd M L, Wilson V A, Mayall B C. Detection of Clostridium difficile enterotoxin gene in clinical specimens by polymerase chain reaction. J Med Microbiol. 1993;38:384–387. doi: 10.1099/00222615-38-5-384. [DOI] [PubMed] [Google Scholar]
- 3.Borriello S P, Wren B W, Hyde S, Seddon S V, Sibbons P, Krishna M M, Tabaqchali S, Manek S, Price A B. Molecular, immunological, and biological characterization of a toxin A-negative, toxin B-positive strain of Clostridium difficile. Infect Immun. 1992;60:4192–4199. doi: 10.1128/iai.60.10.4192-4199.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braun V, Hundsberger T, Leukel P, Sauerborn M, von Eichel-Streiber C. Definition of the single integration site of the pathogenicity locus in Clostridium difficile. Gene. 1996;181:29–38. doi: 10.1016/s0378-1119(96)00398-8. [DOI] [PubMed] [Google Scholar]
- 5.Delmée M, Avesani V, Delferrière N, Burtonboy G. Characterization of flagella of Clostridium difficile and their role in serogrouping reactions J. Clin Microbiol. 1990;28:2210–2214. doi: 10.1128/jcm.28.10.2210-2214.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delmée M, Laroche Y, Avesani V, Cornelis G. Comparison of serogrouping and polyacrylamide gel electrophoresis for typing of Clostridium difficile. J Clin Microbiol. 1986;24:991–994. doi: 10.1128/jcm.24.6.991-994.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Depitre C, Delmée M, Avesani V, L’Haridon R, Roels A, Popoff M, Corthier G. Serogroup F strains of Clostridium difficile produce toxin B but not toxin A. J Med Microbiol. 1993;38:434–441. doi: 10.1099/00222615-38-6-434. [DOI] [PubMed] [Google Scholar]
- 8.Foxall P A, Hu L-T, Mobley H L T. Use of polymerase chain reaction-amplified Helicobacter pylori urease structural genes for differentiation of isolates. J Clin Microbiol. 1992;30:739–741. doi: 10.1128/jcm.30.3.739-741.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammond G A, Johnson J L. The toxinogenic element of Clostridium difficile strain VPI 10463. Microb Pathog. 1995;19:203–213. doi: 10.1016/s0882-4010(95)90263-5. [DOI] [PubMed] [Google Scholar]
- 10.Hundsberger T, Braun V, Weidman M, Leukel P, Sauerborn M, von Eichel-Streiber C. Transcription analysis of the genes tcdA-E of the pathogenicity locus of Clostridium difficile. Eur J Biochem. 1997;244:735–742. doi: 10.1111/j.1432-1033.1997.t01-1-00735.x. [DOI] [PubMed] [Google Scholar]
- 11.Knoop F C, Owens M, Crocker I C. Clostridium difficile: clinical disease and diagnosis. Clin Microbiol Rev. 1993;6:251–265. doi: 10.1128/cmr.6.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyerly D M, Barroso L A, Wilkins T D, Depitre C, Corthier G. Characterization of a toxin A-negative, toxin B-positive strain of Clostridium difficile. Infect Immun. 1992;60:4633–4639. doi: 10.1128/iai.60.11.4633-4639.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lyerly D M, Saum K E, MacDonald D K, Wilkins T D. Effects of Clostridium difficile given intragastrically to animals. Infect Immun. 1985;47:349–352. doi: 10.1128/iai.47.2.349-352.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMillin D E, Muldrow L L, Leggette S J, Abdulahi Y, Ekanemesang U M. Molecular screening of Clostridium difficile toxins A and B genetic determinants and identification of mutant strains. FEMS Microbiol Lett. 1991;78:75–80. doi: 10.1016/0378-1097(91)90258-c. [DOI] [PubMed] [Google Scholar]
- 15.Mohran Z S, Guerry P, Lior H, Murphy J R, El-Gendy A M, Mikhail M M, Oyofo B A. Restriction fragment length polymorphism of flagellin genes of Campylobacter jejuni and/or C. coli isolates from Egypt. J Clin Microbiol. 1996;34:1216–1219. doi: 10.1128/jcm.34.5.1216-1219.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakao H, Pruckler J M, Mazurova I K, Narvskaia O V, Glushkevich T, Marievski V F, Kravetz A N, Fields B S, Wachsmuth I K, Popovic T. Heterogeneity of diphtheria toxin gene, tox, and its regulatory element, dtxR, in Corynebacterium diphtheriae strains causing epidemic diphtheria in Russia and Ukraine. J Clin Microbiol. 1996;34:1711–1716. doi: 10.1128/jcm.34.7.1711-1716.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olsvik O, Wahlberg J, Petterson B, Uhlen M, Popovic T, Wachsmuth I K, Fields P I. Use of automated sequencing of polymerase chain reaction-generated amplicons to identify three types of cholera toxin subunit B in Vibrio cholerae O1 strains. J Clin Microbiol. 1993;31:22–25. doi: 10.1128/jcm.31.1.22-25.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Neill G L, Ogunsola F T, Brazier J S, Duerden B I. Modification of a PCR rybotyping method for application as a routine typing scheme for Clostridium difficile. Anaerobe. 1996;2:205–209. [Google Scholar]
- 19.Riegler M, Sedivy R, Pothoulakis C, Hamilton G, Zacherl J, Bischof G, Cosentini E, Feil W, Schiessel R, LaMont J T, Wenzl E. Clostridium difficile toxin B is more potent than toxin A in damaging human colonic epithelium in vitro. J Clin Investig. 1995;95:2004–2011. doi: 10.1172/JCI117885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riley T. The epidemiology of Clostridium difficile-associated diarrhoea. Rev Med Microbiol. 1994;5:117–122. [Google Scholar]
- 21.Rupnik M, Braun V, Soehn F, Janc M, Hofstetter M, Laufenberg-Feldman R, von Eichel-Streiber C. Characterization of polymorphisms in the toxin A and B genes of Clostridium difficile. FEMS Microbiol Lett. 1997;148:197–202. doi: 10.1111/j.1574-6968.1997.tb10288.x. [DOI] [PubMed] [Google Scholar]
- 22.Shortridge V D, Stone G G, Flamm R K, Beyer J, Versalovic J, Graham D W, Tanaka S K. Molecular typing of Helicobacter pylori isolates from a multicenter U.S. clinical trial by ureC restriction fragment length polymorphism. J Clin Microbiol. 1997;35:471–473. doi: 10.1128/jcm.35.2.471-473.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toma S, Lesiak G, Magus M, Lo H-L, Delmée M. Serotyping of Clostridium difficile. J Clin Microbiol. 1988;26:426–428. doi: 10.1128/jcm.26.3.426-428.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Dijck P, Avesani V, Delmée M. Genotyping of outbreak-related and sporadic isolates of Clostridium difficile belonging to serogroup C. J Clin Microbiol. 1996;34:3049–3055. doi: 10.1128/jcm.34.12.3049-3055.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.von Eichel-Streiber C. Molecular biology of the Clostridium difficile toxins. In: Sebald M, editor. Genetics and molecular biology of anaerobic bacteria. Berlin, Germany: Springer-Verlag; 1993. pp. 265–289. [Google Scholar]
- 26.von Eichel-Streiber C, Meyer zu Heringdorf D, Habermann E, Sartingen S. Closing in on the toxic domain through analysis of a variant Clostridium difficile cytotoxin B. Mol Microbiol. 1995;17:315–321. doi: 10.1111/j.1365-2958.1995.mmi_17020313.x. [DOI] [PubMed] [Google Scholar]
- 27.von Eichel-Streiber C, Boquet P, Sauerborn M, Thelestam M. Large clostridial cytotoxins—a family of glycosyltransferases modifying small GTP-binding proteins. Trends Microbiol. 1996;4:375–382. doi: 10.1016/0966-842X(96)10061-5. [DOI] [PubMed] [Google Scholar]
- 28.von Eichel-Streiber C, Laufenberg-Feldmann R, Sartingen S, Schulze J, Sauerborn M. Comparative sequence analysis of Clostridium difficile toxins A and B. Mol Gen Genet. 1992;233:260–268. doi: 10.1007/BF00587587. [DOI] [PubMed] [Google Scholar]