Abstract
Background:
Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ACEIs-ARBs) improve outcomes in heart failure (HF). Less is known about this association in nursing home (NH) residents.
Study Question:
Evaluate the association of ACEIs or ARBs with outcomes in NH residents hospitalized for HF.
Study Design:
Propensity score-matched cohort study of NH residents hospitalized for HF receiving and not receiving ACEIs-ARBs and subsequent outcomes.
Methods and Outcomes:
Of the 8024 hospitalized HF patients, 542 were NH residents, of which 252 received ACEIs-ARBs. We assembled a propensity score-matched cohort of 157 pairs of NH residents receiving and not receiving ACEIs-ARBs balanced on 29 baseline characteristics (mean age, 3 years, 74% women, 17% African American), in which we estimated hazard ratios (HR) and 95% confidence intervals (CI) for 30-day all-cause readmission, HF readmission and all-cause mortality associated with ACEI-ARB use. We then checked for interaction in a matched cohort of 5130 patients (378 were NH residents) assembled form 8024 patients.
Results:
Among 314 matched NH residents, HRs (95% CIs) for 30-day all-cause readmission, HF readmission and all-cause mortality were 0.78 (0.47–1.28), 0.68 (0.29–1.60) and 1.26 (0.70–2.27), respectively. Respective HRs (95% CIs) at 1 year were 0.76 (0.56–1.02), 0.68 (0.42–1.09) and 1.04 (0.78–1.38). Among 5130 matched patients, ACEI-ARB use was associated with a significantly lower risk of all outcomes at both times, with no significant interactions, except for 1-year mortality (p for interaction, 0.026).
Conclusions:
We found no evidence that the use of ACEIs or ARBs is associated with improved outcomes in patients with HF in the NH setting. However, we also found on evidence that this association is different in NH residents with HF versus other HF patients. Future larger studies are needed to demonstrate effectiveness of these drugs in the NH setting.
Keywords: ACEIs, ARBs, nursing home, heart failure, mortality, readmission
Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) have been shown to be associated with better outcomes in patients with heart failure and reduced ejection fraction (HFrEF).1 HF is associated with poor outcomes and a leading cause for hospital readmission in older Medicare beneficiaries.2 We have previously demonstrated that a discharge prescription for ACEIs or ARBs may reduce the risk for readmission in these patients.3 Nursing home (NH) residents hospitalized for HF are characteristically and prognostically different from those HF patients living in the communities.4,5 In the current analysis, we examined the association of a discharge prescription of ACEIs or ARBs with outcomes in NH residents hospitalized for HF.
Methods
Data source and study patients
The Alabama Heart Failure Project (AHFP) is a HF registry, the details of which have been previously described.6–8 Charts of 8555 unique fee-for-service Medicare beneficiaries who had primary discharge diagnoses codes for HF were abstracted by trained data abstractors using structured data collection tools.6 These patients were discharged from 106 Alabama hospitals between 1998 and 2001, and of these 545 (7%) were NH residents. Data on demographics and other baseline characteristics, medication use, and in-hospital care were centrally collected by trained chart abstractors.6
Discharge prescription for ACEIs or ARBs
Data on the receipt of ACEIs or ARBs were collected by chart abstraction. Of the 545 patients admitted from a NH, 3 had a history of intolerance to ACEIs and were excluded. Of the remaining 542 patients, 250 received discharge prescriptions for ACEIs or ARBs (Figure 1). Given the small sample size, we did not restrict our analysis to an inception cohort or those with reduced ejection fraction.
Figure 1.
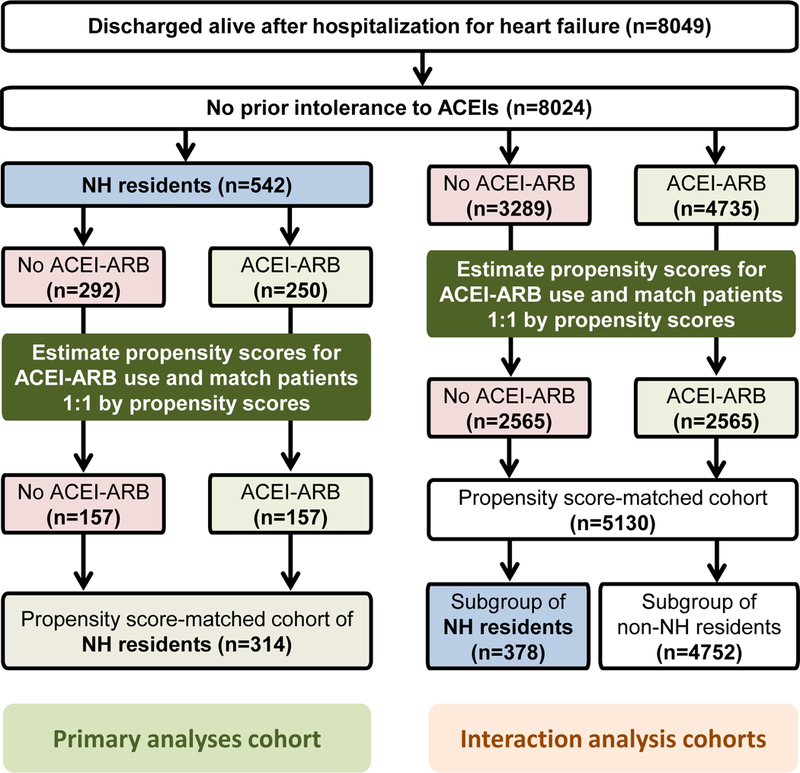
Flow chart displaying (1) assembly of a propensity score-matched cohorts of nursing home (NH) residents hospitalized for heart failure by receipt of angiotensin-converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB) and (2) assembly of a propensity score matched cohort of all patients hospitalized for heart failure, by receipt of ACEIs or ARBs, stratified into NH and non-NH residents
Outcomes
We examined all-cause readmission, HF readmission, all-cause mortality, and the combined end point of all-cause readmission or all-cause mortality at 30 days and 1 year. Data on all outcome variables were obtained from the CMS Medicare data.6,9,10
Assembly of a balanced cohort: Propensity score matching
Because patients were not randomly prescribed ACEIs or ARBs, to minimize indication bias, we used propensity scores for the receipt of ACEIs or ARBs to assemble a matched cohort of patients in which those receiving and not receiving these drugs would be balanced on key measured baseline characteristics.11,12 A non-parsimonious multivariable logistic regression model was used to estimate propensity scores for the receipt of ACEIs or ARBs for each of the 542 patients. The model was adjusted for 29 baseline characteristics presented in Figure 1. We then used the propensity scores to assemble a matched cohort of 157 pairs of patients receiving and not receiving ACEIs or ARBs (Figure 1). Absolute standardized differences were estimated to assess post-match balance, with 0% indicating no residual bias and <10% inconsequential bias.13
Test of interaction
To examine if the lack of association of ACEI or ARB use with outcomes in NH residents was significantly different from that among non-NH residents, we repeated the above process in 8024 patients with no history of intolerance to ACEIs, of which 4735 received discharge prescriptions for ACEIs or ARBs (Figure 1). From these patients, we assembled a matched cohort of 5130 patients, of which 2565 were receiving ACEIs or ARBs, and 378 were NH residents (Figure 1).
Assembly of a sensitivity cohort
The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) is a large national HF registry, which has been described previously.14,15 The current analysis is based on the Medicare-linked OPTIMZE-HF that included 26,376 unique patients discharged from 259 hospitals in 48 states during 2003–2004 with a primary discharge diagnosis of HF. Of these, 471 were NH residents. Because of the small number of NH residents in the OPTIMIZE-HF, we used data from the AHFP for our primary analyses. Furthermore, AHFP have data on variables considered prognostically important in the NH setting such as dementia and pressure ulcer that are not available in OPTIMIZE-HF. Thus, for our sensitivity analysis, we merged the 545 NH residents from AHFP described above with the 471 NH residents from OPTIMIZE-HF to assemble a merged cohort of 1016 NH residents, of whom 483 were receiving ACEIs or ARBs. From the merged data, we were able to identify 23 baseline characteristics that were common to both datasets. Using approaches described above, we assembled a propensity score-matched cohort of 734 patients balanced on these 23 baseline characteristics.
Statistical analysis
For descriptive analyses comparing between-group baseline characteristics, we used Pearson’s Chi-square and Wilcoxon rank-sum tests as appropriate. All associations between the use of ACEIs or ARBs and outcomes were examined in the matched cohort using Cox regression models. Kaplan-Meier survival analyses were used to plot the combined end point of all-cause hospital readmission or all-cause mortality at 12 months. All statistical tests were two-tailed with a p-value <0.05 considered significant. SPSS for Windows version 24 (IBM Corp., Armonk, NY) were used for data analyses.
Results
Baseline characteristics
Matched patients (n=314) had a mean age of 83 (±8) years, 74% were women and 17% were African American. Before matching, more patients receiving ACEIs or ARBs had a lower mean EF and serum creatinine, and were receiving beta-blockers, digoxin and diuretics. However, these and other imbalances were balanced after matching (Table 1 and Figure 2).
Table 1.
Baseline characteristics of nursing home resident Medicare beneficiaries hospitalized for decompensated heart failure, by the receipt of a discharge prescription for angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), before and after propensity score matching
| n (%) or mean (±SD) | Pre-match (N=542) |
Post-match (N=314) |
||||
|---|---|---|---|---|---|---|
| Use of ACE inhibitors or ARBs |
P value | Use of ACE inhibitors or ARBs |
P value | |||
| No (n=292) | Yes (n=250) | No (n=157) | Yes (n=157) | |||
| Age (years) | 83 (±8) | 83 (±9) | 0.978 | 83 (±8) | 83 (±9) | 0.801 |
| Female | 211 (72%) | 192 (77%) | 0.228 | 115 (73%) | 117 (75%) | 0.797 |
| African American | 52 (18%) | 50 (20%) | 0.515 | 27 (17%) | 26 (17%) | 0.880 |
| Current smoker | 15 (5%) | 11 (4%) | 0.689 | 10 (6%) | 6 (4%) | 0.305 |
| LVEF < 45% | 42 (14%) | 79 (32%) | <0.001 | 37(24%) | 31 (20%) | 0.411 |
| Past medical history | ||||||
| History of heart failure | 214 (73%) | 198 (79%) | 0. 108 | 126 (80%) | 125 (80%) | 0.888 |
| Hypertension | 192 (66%) | 183 (73%) | 0.061 | 110 (70%) | 112 (71%) | 0.804 |
| Coronary artery disease | 129 (44%) | 119 (48%) | 0.425 | 73 (47%) | 76 (48%) | 0.735 |
| Diabetes mellitus | 117 (40%) | 120 (48%) | 0.064 | 70 (45%) | 66 (42%) | 0.649 |
| Atrial fibrillation | 75 (26%) | 80 (32%) | 0.105 | 47 (30%) | 46 (29%) | 0.902 |
| Stroke | 116 (40%) | 93 (37%) | 0.547 | 67 (43%) | 58 (37%) | 0.299 |
| Chronic obstructive pulmonary disease | 119 (41%) | 74 (30%) | 0.007 | 60 (38%) | 59 (38%) | 0.907 |
| Dementia | 143 (49%) | 108 (43%) | 0.179 | 69 (44%) | 70 (45%) | 0.910 |
| Clinical findings | ||||||
| Pulse (beats per minute) | 93 (±24) | 90 (±22) | 0.093 | 92 (±24) | 91 (±23) | 0.767 |
| Systolic blood pressure (mmHg) | 143 (±30) | 146 (±33) | 0.230 | 146(±30) | 144 (±33) | 0.595 |
| Pulmonary edema by chest x-ray | 246 (84%) | 207 (83%) | 0.650 | 136 (87%) | 134(85%) | 0.745 |
| Laboratory values | ||||||
| Serum creatinine (mg/dL) | 1.6 (±1.1) | 1.3 (±0.7) | 0.003 | 1.4 (±0.7) | 1.4 (±0.8) | 0.671 |
| In-hospital events | ||||||
| Pneumonia (any) | 134 (46%) | 108 (43%) | 0.530 | 71 (45%) | 71 (45%) | 1.000 |
| Acute myocardial infarction | 15 (5%) | 13 (5%) | 0.974 | 9 (6%) | 10 (6%) | 0.813 |
| Pressure ulcer | 84 (29%) | 62 (25%) | 0.299 | 41 (26%) | 38 (24%) | 0.696 |
| Hospital and care characteristics | ||||||
| Rural hospital | 109 (37%) | 105 (42%) | 0.267 | 66 (42%) | 63 (40%) | 0.731 |
| Cardiology consult | 93 (32%) | 82 (33%) | 0.813 | 56 (36%) | 52 (33%) | 0.635 |
| Intensive care unit | 10 (3%) | 8 (3%) | 0.884 | 6 (4%) | 3 (2%) | 0.310 |
| Length of stay (days) | 7 (±5) | 7 (±6) | 0.893 | 7 (±5) | 8 (±6) | 0.528 |
| Discharge medications | ||||||
| Beta-blockers | 43 (15%) | 64 (26%) | 0.002 | 35 (22%) | 34 (22%) | 0.892 |
| Digoxin | 100 (34%) | 126 (50%) | <0.001 | 69 (44%) | 68 (43%) | 0.909 |
| Loop diuretics | 208 (71%) | 221 (88%) | <0.001 | 130 (83%) | 130 (83%) | 1.000 |
| Potassium-sparing diuretics | 23 (8%) | 41 (16%) | 0.002 | 16 (10%) | 19 (12%) | 0.591 |
| Potassium supplements | 124 (43%) | 114 (46%) | 0.464 | 68 (43%) | 53 (48%) | 0.365 |
Figure 2.
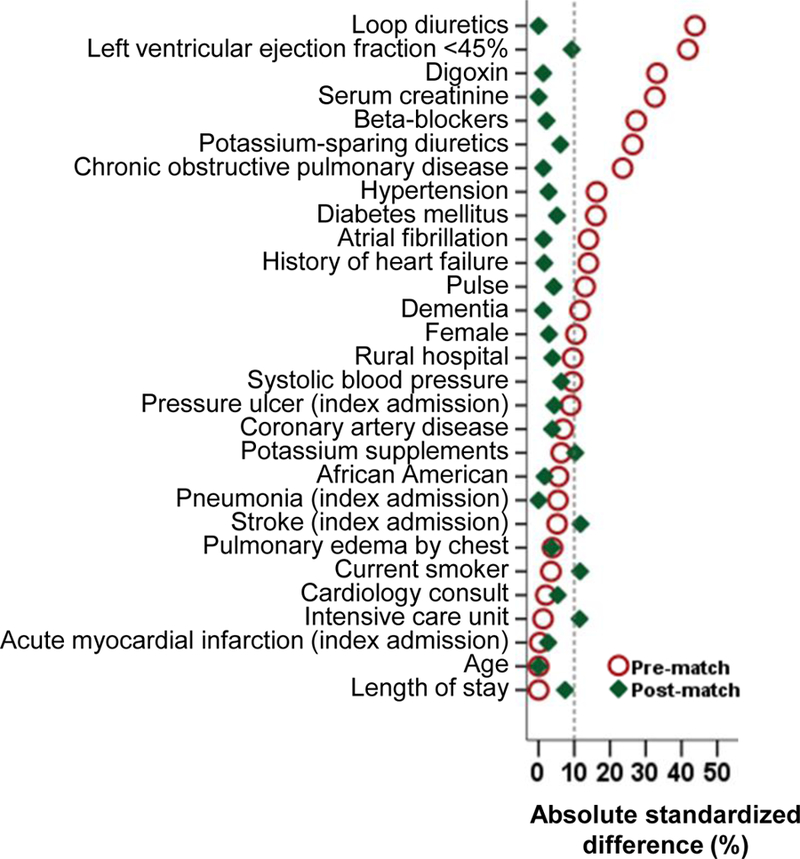
Love plot displaying absolute standardized differences for 29 baseline characteristics between patients receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, before and after propensity score matching
30-day outcomes in propensity score-matched NH residents
Among the 314 propensity score-matched NH residents with HF in the AHFP, the combined end point of 30-day all-cause readmission or 30-day all-cause mortality occurred in 31% (48/157) and 34% (54/157) of matched patients receiving and not receiving a discharge prescription for ACEIs or ARBs, respectively (hazard ratio {HR} when the use of ACEIs or ARBs was compared with their non-use, 0.86; 95% confidence interval {CI}, 0.58–1.27; Table 2 and Figure 3). There was no association with other 30-day outcomes (Table 2).
Table 2 and Table 3.
Association between a discharge prescription for angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) and post-discharge outcomes in a propensity-matched cohorts of nursing home resident Medicare beneficiaries hospitalized for decompensated heart failure
| 30-day outcomes | % (events) |
Absolute risk difference* | Hazard ratio† (95% confidence interval) |
|
|---|---|---|---|---|
| Use of ACEIs or ARBs | ||||
| AHFP Cohort | No (n=157) | Yes (n=157) | ||
| 30-day outcomes | ||||
| All-cause readmission | 22% (35) | 18% (28) | −4% | 0.78 (0.47−1.28) |
| Heart failure readmission | 8% (13) | 6% (9) | −2% | 0.68 (0.29−1.60) |
| All-cause mortality | 13% (20) | 16% (25) | +3% | 1.26 (0.70−2.27) |
| All-cause mortality or all-cause readmission | 34% (54) | 31% (48) | −3% | 0.86 (0.58−1.27) |
| 1-year outcomes | ||||
| All-cause readmission | 62% (97) | 52% (82) | −10% | 0.76 (0.56−1.02) |
| Heart failure readmission | 27% (42) | 18% (28) | −9% | 0.68 (0.42−1.09) |
| All-cause mortality | 62% (97) | 61% (96) | −1% | 1.04 (0.78−1.38) |
| All-cause mortality or all-cause readmission | 89% (139) | 82% (129) | −7% | 0.84 (0.66−1.06) |
|
| ||||
| AHFP + OPTIMIZE-HF Cohorts | No (n=367) | Yes (n=367) | ||
| 30-day outcomes | ||||
| All-cause readmission | 24% (87) | 23% (84) | −1% | 0.94 (0.70−1.27) |
| Heart failure readmission | 8% (28) | 7% (26) | −1% | 0.92 (0.54−1.57) |
| All-cause mortality | 16% (58) | 14% (52) | −2% | 0.89 (0.61−1.30) |
| All-cause mortality or all-cause readmission | 35% (130) | 33% (121) | −2% | 0.91 (0.71−1.16) |
| 1-year outcomes | ||||
| All-cause readmission | 64% (235) | 63% (230) | −1% | 0.95 (0.79−1.14) |
| Heart failure readmission | 26% (97) | 25% (91) | −1% | 0.94 (0.71−1.25) |
| All-cause mortality | 60% (97) | 60% (96) | 0% | 0.99 (0.82−1.19) |
| All-cause mortality or all-cause readmission | 87% (319) | 86% (315) | −1% | 0.96 (0.82−1.12) |
Absolute risk differences were calculated by subtracting percent events in patients receiving no ACEIs or ARBs from those receiving those drugs
The hazard ratios compared patients receiving ACEIs or ARBs versus those not receiving those drugs. These hazard ratios were calculated by treating patients without events during the first 30 days as censored.
Figure 3.
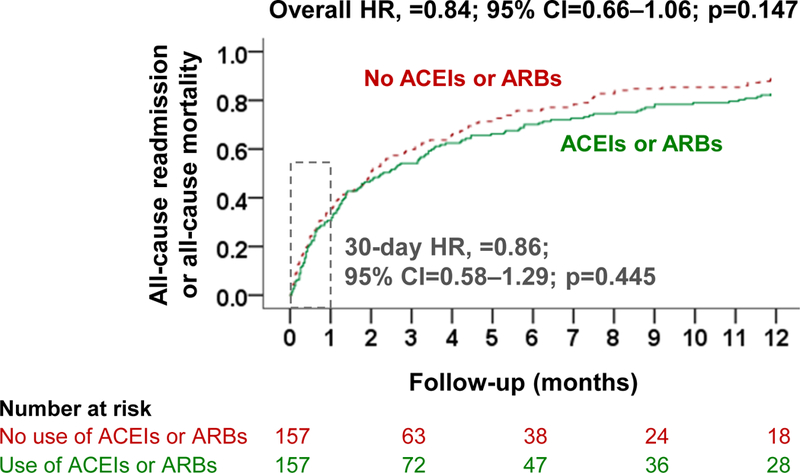
Kaplan-Meier plots for the combined end point of all-cause hospital readmission or all-cause mortality in a propensity-matched cohort of older heart failure patients admitted from nursing homes receiving and not receiving a discharge prescription for angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) (HR=hazard ratio; CI=confidence interval)
12-month outcomes in propensity score-matched NH residents
Among the 314 propensity score-matched NH residents with HF in the AHFP, the combined end point of 1-year all-cause readmission or 1-year all-cause mortality occurred in 82% (129/157) and 89% (139/157) of matched patients receiving and not receiving a discharge prescription for ACEIs or ARBs, respectively (HR associated with ACEI or ARB use, 0.84; 95% CI, 0.66–1.06; Table 3 and Figure 3). Use of ACEIs or ARBs was not associated with other 1-year outcomes (Table 3).
Findings from the interaction tests
Among the 5130 propensity score-matched patients with HF in the AHFP, the use of ACEIs or ARBs was associated with a significantly lower risk of all all-cause readmission, HF readmission, and all-cause mortality at 30 days and 1 year (Figure 4). All associations were significant in the non-NH resident subset of patients and none of the association was significant among NH residents. However, none of these differences were statistically significant except for 1-year all-cause mortality (p for interaction, 0.026; Figure 4).
Figure 4.
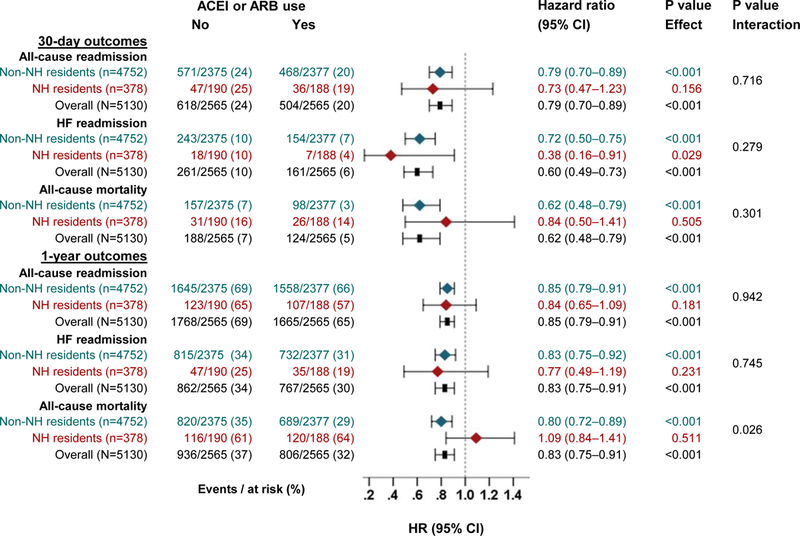
Hazard ratios and 95% confidence intervals (CI) for outcomes by use of angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) in propensity score-matched patients with heart failure, and subgroups of nursing homes (NH) residents versus other patients
Findings from the sensitivity cohort
Among the 734 propensity score-matched NH residents with HF in the combined AHFP and OPTIMIZE-HF datasets, the use of ACEIs or ARBs was not associated with any outcomes at 30 days and 1 year (Tables 2 and 3).
Discussion
Findings from our study demonstrate that there is no evidence that the clinical effectiveness of ACEIs or ARBs in patients with HF varied between NH and non-HF residents. However, our findings also did not reveal that the use of these drugs was associated with improved outcomes in NH residents hospitalized for HF, likely due to small sample size. Considering the lack of power and the fact NH residents are heterogeneous with many competing risks for poor outcomes, these findings need to be interpreted with caution.
ACEIs and ARBs have little effect on sudden cardiac death, one of the more common modes of death in HF, and instead improve outcomes by reducing the risk of hospitalization and death due to progressive pump failure.16 This is important as pump failure death is a relatively more common mode of death in patients with more advanced HF and older NH residents with HF would be expected to have more advanced HF.17–19 Yet, we observed that the use of these drugs had no association with any outcomes in NH residents. One potential explanation for the lack of association of ACEI or ARB use with outcomes in these patients is the high burden of non-cardiovascular morbidity. Most of the morbidity and mortality in older NH residents are due to non-cardiovascular causes, which may help explain why these drugs may not be effective in improving outcomes. Further, our inclusion of patients with HF with preserved ejection fraction may have further attenuated any beneficial association between ACEIs or ARBs with outcomes. Finally, hospitalized NH residents may have a high mortality rate,20 which may in part result in a survivor cohort that may be at a lower risk for poor outcomes and be less responsive to the beneficial effects of ACEIs and ARBs.
Several studies have reported underutilization of ACEIs in the NH settings.21–24 However, there is little evidence from the literature that demonstrate the clinical effectiveness of ACEIs or ARBs in older NH residents with HF.25–27 Findings from our study have important implications. If our results can be replicated in a prospective study with a more contemporary cohort of NH residents with HF, this may help reduce the polypharmacy burden in this population. In contrast, if evidence of their clinical effectiveness can be demonstrated, strategies may need to be developed and tested to achieve their optimal underutilization. Further, more recent evidence suggests the superiority of angiotensin receptor neprilysin inhibitors over ACEIs in HFrEF and these benefits may extend to patients age 75 years of age and older.28 Studies evaluating the clinical effectiveness of these agents in NH residents are needed.
Our study has several limitations. Despite our use of propensity score-matching, bias due to residual confounding or unmeasured confounding such as physical function and patient and family preference is possible. We had considered formal sensitivity analyses but it was not necessary due to the observed null associations. Lack of power and chance are other possibilities given our small sample size. We had no data on post-discharge adherence and crossover of treatment during follow-up and regression dilution may in part explain a null association. Finally, findings of this study based on fee-for-service Medicare beneficiaries from one state from an earlier era of HF therapy may limit generalizability. However, treatment of HF in NH residents has not changed much in the past two decades.
In conclusion, we found no evidence of clinical effectiveness of ACEIs or ARBs in patients with HF in the NH setting. However, we also found no evidence that this association is significantly different between NH residents with HF versus other HF patients. These negative findings, from two relatively large HF registries, albeit with a small subset of NH residents, would need to be interpreted with caution due the modest sample size. Taken together, these findings suggest, future sufficiently powered studies are needed to establish evidence of clinical effectiveness of ACEIs or ARBs in patients with HF in the NH setting.
Acknowledgments
Funding: Dr. Ahmed was in part supported by the National Institutes of Health (NIH) through grants (R01-HL085561, R01-HL085561-S and R01-HL097047) from the National Heart, Lung, and Blood Institute. OPTIMIZE-HF was sponsored by GlaxoSmithKline.
Footnotes
Conflict of Interest and Disclosures: Dr. Fonarow reports consulting with Amgen, Novartis, Medtronic, St Jude Medical and was the Principle Investigator of OPTIMIZE-HF. None of the other authors report any conflicts of interest related to this manuscript.
References
- 1.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810–1852. [DOI] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360(14):1418–1428. [DOI] [PubMed] [Google Scholar]
- 3.Sanam K, Bhatia V, Bajaj NS, et al. Renin-Angiotensin System Inhibition and Lower 30-Day All-Cause Readmission in Medicare Beneficiaries with Heart Failure. Am J Med. 2016;129(10):1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahmed A Clinical characteristics of nursing home residents hospitalized with heart failure. J Am Med Dir Assoc. 2002;3(5):310–313. [DOI] [PubMed] [Google Scholar]
- 5.Gambassi G, Forman DE, Lapane KL, et al. Management of heart failure among very old persons living in long-term care: has the voice of trials spread? The SAGE Study Group. Am Heart J. 2000;139(1 Pt 1):85–93. [DOI] [PubMed] [Google Scholar]
- 6.Feller MA, Mujib M, Zhang Y, et al. Baseline characteristics, quality of care, and outcomes of younger and older Medicare beneficiaries hospitalized with heart failure: findings from the Alabama Heart Failure Project. Int J Cardiol. 2012;162(1):39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheriff HM, Thogaripally MR, Panjrath G, et al. Digoxin and 30-Day All-Cause Readmission in Long-Term Care Residents Hospitalized for Heart Failure . J Am Med Dir Assoc. 2017;18(9):761–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aronow WS, Rich MW, Goodlin SJ, et al. In-hospital cardiology consultation and evidence-based care for nursing home residents with heart failure. J Am Med Dir Assoc. 2012;13(5):448–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmed A, Fonarow GC, Zhang Y, et al. Renin-angiotensin inhibition in systolic heart failure and chronic kidney disease. Am J Med. 2012;125(4):399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed A, Rich MW, Zile M, et al. Renin-angiotensin inhibition in diastolic heart failure and chronic kidney disease. Am J Med. 2013;126(2):150–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenbaum PR RD. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70(41–55. [Google Scholar]
- 12.Rubin DB. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001; 2(169–188. [Google Scholar]
- 13.Wahle C, Adamopoulos C, Ekundayo OJ, Mujib M, Aronow WS, Ahmed A. A propensity-matched study of outcomes of chronic heart failure (HF) in younger and older adults. Arch Gerontol Geriatr. 2009;49(1):165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y, Kilgore ML, Arora T, et al. Design and rationale of studies of neurohormonal blockade and outcomes in diastolic heart failure using OPTIMIZE-HF registry linked to Medicare data. Int J Cardiol. 2013;166(1):230–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fonarow GC, Abraham WT, Albert NM, et al. Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF): rationale and design. Am Heart J. 2004;148(1):43–51. [DOI] [PubMed] [Google Scholar]
- 16.The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325(5):293–302. [DOI] [PubMed] [Google Scholar]
- 17.O’Connor CM, Miller AB, Blair JE, et al. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction: results from Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) program. Am Heart J. 2010;159(5):841–849 e841. [DOI] [PubMed] [Google Scholar]
- 18.Carson P, Anand I, O’Connor C, et al. Mode of death in advanced heart failure: the Comparison of Medical, Pacing, and Defibrillation Therapies in Heart Failure (COMPANION) trial. J Am Coll Cardiol. 2005;46(12):2329–2334. [DOI] [PubMed] [Google Scholar]
- 19.Shen L, Jhund PS, Petrie MC, et al. Declining Risk of Sudden Death in Heart Failure. N Engl J Med. 2017;377(1):41–51. [DOI] [PubMed] [Google Scholar]
- 20.Ahmed AA, Hays CI, Liu B, et al. Predictors of in-hospital mortality among hospitalized nursing home residents: an analysis of the National Hospital Discharge Surveys 2005–2006. J Am Med Dir Assoc. 2010;11(1):52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forman DE, Chander RB, Lapane KL, Shah P, Stoukides J. Evaluating the use of angiotensin-converting enzyme inhibitors for older nursing home residents with chronic heart failure. J Am Geriatr Soc. 1998;46(12):1550–1554. [DOI] [PubMed] [Google Scholar]
- 22.Ahmed A, Weaver MT, Allman RM, DeLong JF, Aronow WS. Quality of care of nursing home residents hospitalized with heart failure. J Am Geriatr Soc. 2002;50(11):1831–1836. [DOI] [PubMed] [Google Scholar]
- 23.Ghosh S, Ziesmer V, Aronow WS. Underutilization of aspirin, beta blockers, angiotensin-converting enzyme inhibitors, and lipid-lowering drugs and overutilization of calcium channel blockers in older persons with coronary artery disease in an academic nursing home. J Gerontol A Biol Sci Med Sci. 2002;57(6):M398–400. [DOI] [PubMed] [Google Scholar]
- 24.Heckman GA, Misiaszek B, Merali F, et al. Management of heart failure in Canadian long-term care facilities. Can J Cardiol. 2004;20(10):963–969. [PubMed] [Google Scholar]
- 25.Ahmed A Treatment of chronic heart failure in long-term care facilities: implications of recent heart failure guidelines recommendations. Arch Gerontol Geriatr. 2003;37(2):131–137. [DOI] [PubMed] [Google Scholar]
- 26.Daamen MA, Hamers JP, Gorgels AP, Tan FE, Schols JM, Brunner-la Rocca HP. Treatment of heart failure in nursing home residents. J Geriatr Cardiol. 2016;13(1):44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jurgens CY, Goodlin S, Dolansky M, et al. Heart failure management in skilled nursing facilities: a scientific statement from the American Heart Association and the Heart Failure Society of America. J Card Fail. 2015;21(4):263–299. [DOI] [PubMed] [Google Scholar]
- 28.McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004. [DOI] [PubMed] [Google Scholar]


