Abstract
Background
Since the connection between muscle atrophy and vitamin D and estradiol status ambiguous, this study was thus conducted to determine whether low skeletal muscle mass (SMM) in middle-aged and elderly women was affected by estradiol and vitamin D levels together.
Methods
Baseline data from a sub-cohort of the China Northwest Natural Population Cohort: Ningxia Project (CNC-NX) were analyzed. Serum 25-hydroxyvitamin D (25(OH) D) and estradiol were measured by chemiluminescence immunoassay analyzer. Bivariate logistic regression and multiplicative interaction analyses were used to assess the impact of estradiol level and vitamin D status on low SMM, as well as the combined impact of estradiol and low vitamin D status on low SMM.
Results
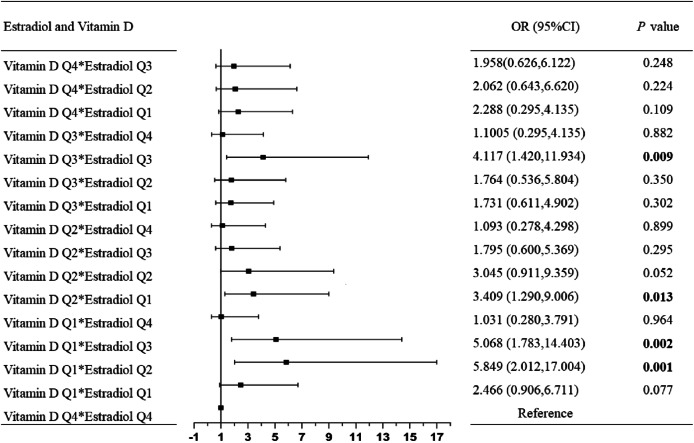
A total of 287 (9.49%) participants had low SMM, which had lower levels of estradiol and vitamin D concentration than normal SMM group. While, after adjusting the confounding variables, these correlations were maintained in estradiol Q1, Q2, Q3 and vitamin D Q1. Furthermore, the significant combined effect of the highest quartile of estradiol concentrations and non-vitamin D deficiency, and interactions between vitamin D Q1 and estradiol Q2, vitamin D Q1 and estradiol Q3, vitamin D Q2 and estradiol Q1, vitamin D Q3 and estradiol Q3 on low SMM were stably reflected (P for interaction < 0.05).
Conclusions
Estradiol and vitamin D were interrelated with low SMM in middle-aged and elderly women. Combination of estradiol and vitamin D supplements should be encouraged for middle-aged and elderly women who are at risk of muscle atrophy or experiencing muscle atrophy.
Keywords: Estradiol, Vitamin D, Low skeletal muscle mass, Muscle atrophy, Women
Introduction
Muscle atrophy is a physiological phenomenon associated with aging, characterized by a normal decline in muscle mass and function, known as sarcopenia, which is manifested in a decrease in skeletal muscle mass, muscle strength, and physical activity, and often coexists with obesity [1, 2]. Sarcopenia can further deteriorate the musculoskeletal health of the elderly by raising the risk of osteoporotic vertebral and hip fractures [3], which ultimately results in mobility restrictions, functional impairment, physical disability, and even a lower quality of life [4]. Sarcopenia not only effects very elderly individuals, but can also be widely observed in middle-aged adults [5]. Sarcopenia currently affects more than 50 million people, and by 2050, it is predicted that number will rise to more than 200 million [1]. Studies have found that skeletal muscle declines substantially from about 30 years old, with an annual loss rate of approximately 0.1–0.5%, while the rate acceleration dramatically post age 65 [6].
The reduction of skeletal muscle mass is not only linked to negative social and financial effects like hospitalization and mortality [7], also connected to comparable gender-neutral alterations, such as heightened inflammation, satellite cell senescence, decreased protein synthesis, and myocyte regeneration [8], as well as some additional gender-specific alterations brought on by a decrease in sex hormones with aging [9]. Furthermore, according to a number of studies, women have physiologically lower levels of skeletal muscle mass than men, which frequently results in sarcopenia [10, 11]. The onset of female sarcopenia appears to be more susceptible to menopause, which may be the cause of this difference between men and women [12].
Menopause is a physiological age-related condition in women that is accompanied by a drop in hormone levels, especially estradiol levels [13, 14]. Estradiol is essential for both female growth and aging, maintaining the sexual characteristics of female. Meanwhile, estradiol can also promote muscle regeneration and contribute to muscle health [1, 15]. Nevertheless, reduction of estradiol during menopause can results in musculoskeletal discomfort [16], resulting in modifications to body composition including skeletal muscle loss and fat accumulation, and even raise the danger of vitamin D deficiency, which might aggravate musculoskeletal discomfort conversely [17]. According to previous studies, the estrogen can stimulate vitamin D metabolism in postmenopausal women by increasing 1,25(OH)2 D levels, which could potentially explain the mechanism behind the interaction between vitamin D deficiency and estrogen regarding low skeletal muscle mass [18, 19].
Indeed, vitamin D deficiency poses a significant health challenge worldwide, especially the elderly. Numerous studies have linked a vitamin D deficiency to skeletal muscle loss and reduction in physical function [20, 21], compromising the strength of muscle in the lower limbs [22], whereas others have indicated that vitamin D has no effect on boosting muscle mass or only a weak correlation with muscle atrophy [23]. Therefore, given the association of vitamin D deficiency and muscle atrophy is still controversial, and estradiol not only plays a key role during women’s menopause but have an effect on muscle atrophy simultaneously. This study was thus conducted to determine whether low skeletal muscle mass in middle-aged and elderly women was affected by estradiol and vitamin D levels together, which may serve as an useful theoretical foundation for future combination of vitamin D and estradiol supplementation therapies.
Materials and methods
Study participants
The current research used cross-sectional data from the China Northwest Natural Population Cohort: Ningxia Project (CNC-NX). A prior study provided a thorough description of the research design and methods [11]. Briefly, 5300 individuals in total (2182 men and 3118 women), a representative sub-cohort consisted of 30% adults randomly selected from CNC-NX, were included in this research [19]. We excluded participants who were male, had missing data on body composition, and those who had been administered hormone therapy prior to analysis (n = 93). Besides, we filled with imputation method, based on the individuals with same demographic and laboratory data, to predict vitamin D levels for 55 participants without vitamin D concentration values. Ultimately, 3025 participants were included in the present analyses.
The present study was evaluated by the Institutional Ethics Committees (IECs) of Ningxia Medical University in accordance with the principles set forth in the Helsinki Declaration (Ethics ID 2018-012, 2020 − 689) and the written informed consent of all participants were obtained at the beginning of the investigation.
Demographic and laboratory data
Each participant underwent all of the following procedures, which were recorded by trained researchers between March 2018 and May 2019.
Demographic data
After signing the informed consent form, all participants received a face-to-face questionnaire to assess demographic data [11]. The dietary intake survey included semi-quantitative food frequency (SFFQ), which made up based on a preliminary study of 24-h dietary review of the local population. No participants were found to have ever experienced eating disorders in this survey. Moreover, the dietary energy and nutrients of the participants were calculated through the Nutrition Calculator v2.8.0 (Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention, Beijing, China).
Anthropometric measurements
All participants were instructed to wear light clothes, no shoes and were forbidden to eat for 12 h, and abstain from alcohol, caffeine and strenuous activity for at least 24 h. Two measurements of weight and height were taken for each individual, rounded to the nearest 0.1 kg and 0.1 cm, respectively. Body composition measurements were obtained by using an octopolar (8 electrodes) bioelectrical impedance analyzer (BIA) (InBody 370, Seoul, Korea). The anthropometric variables such as skeletal muscle mass (SMM), fat mass, and BMI were evaluated. SMM is divided by body height squared to estimate the skeletal muscle mass index (SMI) (kg/m2), using the Janssen’s equation [24]. Appendicular skeletal muscle mass (ASM) is the total of the muscle mass in the arms and legs and served as a good substitute for whole-body skeletal muscle mass [25]. After a 5-minute rest, the brachial blood pressure was assessed using an automated blood pressure monitor (OMRON HEM-801 model).
Laboratory measurements
After a minimum 12-hours fast, venous blood was collected from participants. Biochemical indicators were measured using biochemical auto-analyzers (Mindray BS-430, Shenzhen, China). Moreover, a chemiluminescence immunoassay analyzer (Mindray CL-2000i, Shenzhen, China) was used to measure the levels of estradiol and the fasting serum 25-hydroxyvitamin D (25(OH) D) concentration. vitamin D deficiency was deemed to exist at a 25(OH) D concentration < 20 ng/mL (50nmol/L), and 25(OH) D concentrations ≥ 20 ng/mL (50nmol/L) were regarded as non-vitamin D deficiency [26].
Definition of covariate
Low skeletal muscle mass has been referred to as skeletal muscle mass index (skeletal muscle mass/height2) < 5.7 kg/m2 in female [27]. The menopausal status of participants was divided into three groups: premenopausal (35 ~ 44 years), perimenopausal (45 ~ 54 years), and postmenopausal (≥ 55 years) [28]. Weight/height2 (kg/m2) was used to determine BMI [29]. The definitions of the smoking and alcohol consumption status were as follows: one cigarette per day for six consecutive months, and one drink per week for six consecutive months, respectively [30]. Primary school or below, junior high school, high school or above were the three divisions for the educational level. Physical activity (PA), which was rated as low, moderate, or high, was assessed using the International Physical Activity Questionnaire [31]. The dietary energy and nutrients of the participants were calculated through the Nutrition Calculator v2.8.0.
Statistical analysis
Continuous variables with skewed distributions were presented as median (interquartile range, IQR) and as mean ± standard deviation (SD) for normal. Frequency (percentage) was used to express categorical variables. The Kruskal-Wallis test was used for continuous variables, and the chi-square test was applied to categorical variables. Bivariate logistic regression analyses for evaluating the effect of estradiol level and vitamin D status with low skeletal muscle mass. The combined impact of estradiol and low vitamin D status on low skeletal muscle mass was evaluated using multiplicative interaction. Menopausal status, residence, marital status, educational level, status of drinking and smoking, physical activity, triglyceride, glucose, and dyslipidemia status were included as covariates in the adjusted models. ORs and 95% CIs of low skeletal muscle mass in response to vitamin D deficiency across the quartiles of serum estradiol concentration were estimated, and their interactions were tested. The tolerance and variance inflation factor (VIF) of multicollinearity diagnosis were used to evaluate the validity of regression models. Additionally, we examined the trend of vitamin D quartiles in separate models by using ordinal values.
R 4.0.6 software was used to carry out the statistical analyses. A two-side P value < 0.05 was treated statistically significant.
Results
General characteristics
Table 1 displays the fundamental characteristics of the study participants. All of the 3025 participants, aged 56.27 ± 9.86 years. According to the skeletal muscle mass index, participants were split into two groups based on their levels of skeletal muscle mass: low skeletal muscle mass (low SMM) and normal skeletal muscle mass (normal SMM). A total of 287 (9.49%) participants were reported as low SMM, and had higher age than normal SMM. Moreover, there were notable differences between low and normal SMM in terms of marital status, educational background, and menopausal status (P < 0.001). In terms of anthropometric measurements, participants with low SMM had lower weight, height, BMI, WC, ASMI, and FM values than participants with normal SMM (P < 0.001). In terms of laboratory measurements, low SMM group had lower levels of triglycerides (TGs), estradiol and vitamin D concentration than normal SMM group (P < 0.05). Furthermore, participants with low SMM also had lower values of dietary energy, protein, fat and carbohydrate than with normal SMM (P < 0.001).
Table 1.
General characteristics of study participants
| Characteristics | Total | Low SMM (n = 287) |
Normal SMM (n = 2738) |
P value |
|---|---|---|---|---|
| Age (years) | 56.27 ± 9.86 | 62.59 ± 9.54 | 55.60 ± 9.66 | < 0.001 |
| Marital status | ||||
| Married | 2741 (90.6) | 238 (82.9) | 2503 (91.4) | < 0.001 |
| Widowed | 274 (9.1) | 48 (16.7) | 226 (8.3) | |
| Divorce and unmarried | 10 (0.3) | 1 (0.3) | 9 (0.3) | |
| Education | ||||
| Primary school and below | 2228 (73.7) | 241 (84.0) | 1987 (72.6) | < 0.001 |
| Junior high school | 714 (23.6) | 40 (13.9) | 674 (24.6) | |
| High school and above | 83 (2.7) | 6 (2.1) | 77 (2.8) | |
| Weight (kg) | 60.94 ± 9.19 | 48.88 ± 5.87 | 62.20 ± 8.53 | < 0.001 |
| Height (cm) | 155.95 ± 5.96 | 151.27 ± 5.69 | 156.44 ± 5.77 | < 0.001 |
| BMI (kg/m2) | 25.05 ± 3.45 | 21.42 ± 2.80 | 25.43 ± 3.28 | < 0.001 |
| WC (cm) | 86.39 ± 9.10 | 77.46 ± 7.52 | 87.33 ± 8.74 | < 0.001 |
| ASMI (kg/m2) | 6.58 ± 0.69 | 5.37 ± 0.30 | 6.71 ± 0.59 | < 0.001 |
| FM (kg) | 21.80 ± 6.45 | 16.76 ± 5.43 | 22.33 ± 6.32 | < 0.001 |
| Cholesterol (mmol/L) | 4.93 (4.30, 5.59) | 4.95 (4.27, 5.63) | 4.93 (4.30, 5.58) | 0.925 |
| HDL-C (mmol/L) | 1.37 (1.18, 1.58) | 1.39 (1.21, 1.63) | 1.37 (1.18, 1.58) | 0.211 |
| LDL-C (mmol/L) | 2.86 (2.35, 3.34) | 2.77 (2.27, 3.37) | 2.87 (2.35, 3.34) | 0.446 |
| Triglyceride (mmol/L) | 1.48 (1.05, 2.11) | 1.43 (0.99, 1.91) | 1.49 (1.06, 2.13) | 0.005 |
| Glucose (mmol/L) | 5.44 (4.98, 6.29) | 5.48 (4.96, 6.73) | 5.44 (4.98, 6.27) | 0.315 |
| Dyslipidemia (%) | 1034 (34.2) | 94 (32.8) | 940 (34.3) | 0.592 |
| Estradiol Level (pg/mL) | 14.81 (5.00, 33.94) | 10.75 (5.00, 17.58) | 15.38 (5.00, 36.21) | < 0.001 |
| Vitamin D concentration (ng/ml) | 12.07 (8.91, 15.74) | 10.70 (8.14, 14.61) | 12.20 (8.98, 15.81) | < 0.001 |
| VD deficiency (%) | 2724 (90.0) | 263 (91.6) | 2461 (89.9) | 0.345 |
| Menopausal Status (%) | ||||
| Pre-menopausal | 408 (13.5) | 15 (5.2) | 393 (14.3) | < 0.001 |
| Perimenopausal | 1104 (36.5) | 61 (21.3) | 1043 (38.1) | |
| Postmenopausal | 1513 (50.0) | 211 (73.5) | 1302 (47.6) | |
| Smoking (%) | 36 (1.2) | 5 (1.7) | 31 (1.1) | 0.365 |
| Alcohol intake (%) | 417 (13.8) | 34 (11.8) | 383 (14.0) | 0.317 |
| Physical activity (%) | ||||
| Low | 946 (31.3) | 85 (29.6) | 861 (31.5) | 0.817 |
| Medium | 1563 (51.6) | 152 (53.0) | 1411 (51.5) | |
| High | 516 (17.1) | 50 (17.4) | 466 (17.0) | |
| Dietary energy (Kcal) | 1645.63 (1113.80, 2190.93) | 1456.63 (809.05, 2056.00) | 1660.25 (1132.69, 2202.77) | 0.002 |
| Dietary protein (g) | 59.66 (33.43, 85.88) | 50.34 (22.41, 79.22) | 60.92 (35.21, 86.58) | < 0.001 |
| Dietary fat (g) | 77.70 (50.73, 108.85) | 70.63 (42.72, 102.84) | 78.96 (52.06, 109.36) | 0.001 |
| Dietary carbohydrate (g) | 206.27 (130.79, 331.39) | 177.01 (100.79, 283.36) | 209.21 (131.19, 334.93) | < 0.001 |
Association between estradiol concentration and low skeletal muscle mass
A total of 287 (9.49%) participants with low SMM. Meanwhile, the participants with low estradiol concentrations also had a significantly higher risk of developing low SMM compared to those with normal estradiol concentrations (P < 0.001). Furthermore, the lowest to highest values of the estradiol concentrations were grouped into quartiles (Q1-Q4). The ranges of estradiol concentrations across quartiles were < 5.00, 5.00-<14.81, 14.81-<33.90, ≥ 33.90. As shown in Table 2. The odds of low skeletal muscle mass in estradiol concentration Q1, Q2, and Q3 were 2.354 (95% CI: 1.210–4.614), 2.882 (95% CI: 1.393–5.964), and 2.838 (95% CI: 1.419–5.676), respectively, compared to the odds in the highest quartile of estradiol concentration after adjusting for confounding variables in Model 3.
Table 2.
The association between serum estradiol quartiles and low skeletal muscle mass
| Quartiles of estradiol levels | Unadjusted Model | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | ||||
| Q1 (< 5.00) | 4.724 (2.974, 7.504) | < 0.001 | 2.961 (1.683,5.208) | < 0.001 | 2.995 (1.701,5.272) | < 0.001 | 2.354 (1.210,4.614) | 0.013 | |||
| Q2 (5.00 ~ 14.81) | 4.937 (2.991, 8.147) | < 0.001 | 3.219 (1.764,5.874) | < 0.001 | 3.248 (1.777,5.935) | < 0.001 | 2.882 (1.3935.964) | 0.004 | |||
| Q3 (14.81 ~ 33.90) | 3.674 (2.259, 5.977) | < 0.001 | 2.808 (1.592,4.953) | < 0.001 | 2.847 (1.612,5.026) | < 0.001 | 2.838 (1.419,5.676) | 0.003 | |||
| Q4 (≥ 33.90) | Reference | Reference | Reference | Reference | |||||||
| P for trend | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||||||
Notes: The model 1 adjusted for age, residence, marital status, and educational level; Model 2 adjusted for model 1 and smoking status, drinking status, physical activity; Model 3 adjusted for model 2 and BMI, FM, triglyceride, menopausal status, dietary energy
Relationship between vitamin D concentration and low skeletal muscle mass
As shown in Table 3. The serum vitamin D levels were also split into quartiles, which were < 8.91, 8.91-<12.07, 12.07-<15.74, ≥ 15.74, respectively. When compared to Q4, the adjusted ORs values for low skeletal muscle mass in vitamin D level Q1, Q2, and Q3 were 1.720 (95% CI: 1.201–2.674), 1.386 (95% CI: 0.892–2.154), and 1.142 (95% CI: 0.710–1.835), respectively, adjusted for confounding variables in Model 3.
Table 3.
The association between serum Vitamin D quartiles and low skeletal muscle mass
| Quartiles of vitamin D levels | Unadjusted Model | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | ||||
| Q1 (< 8.91) | 1.617 (1.143, 2.287) | 0.007 | 1.457 (1.016,2.090) | 0.041 | 1.433 (1.005,2.071) | 0.047 | 1.720 (1.201,2.674) | 0.016 | |||
| Q2 (8.91 ~ 12.07) | 1.480 (1.041, 2.104) | 0.029 | 1.281 (0.893,1.838) | 0.178 | 1.272 (0.886,1.825) | 0.192 | 1.386 (0.892,2.154) | 0.146 | |||
| Q3 (12.07 ~ 15.74) | 0.959 (0.658, 1.404) | 0.828 | 0.967 (0.655,1.427) | 0.866 | 0.967 (0.655,1.428) | 0.868 | 1.142 (0.710,1.835) | 0.585 | |||
| Q4 (≥ 15.74) | Reference | Reference | Reference | Reference | |||||||
| P for trend | 0.003 | 0.003 | 0.003 | 0.003 | |||||||
Notes: The model 1 adjusted for age, residence, marital status, and educational level; Model 2 adjusted for model 1 and smoking status, drinking status, physical activity; Model 3 adjusted for model 2 and BMI, FM, triglyceride, menopausal status, dietary energy
The combined association of estradiol and vitamin D deficiency status on low SMM
Participants with the lower quartile of estradiol concentrations and vitamin D deficiency had a higher likelihood of developing low skeletal muscle, compared to those in the highest quartile of estradiol concentrations and non-vitamin D deficiency (Table 4). Considering the applicability of the definition of vitamin D deficiency in the population, we further used the vitamin D quartile to explore the interaction between vitamin D and estradiol on low SMM. The significant interactions between vitamin D Q1 and estradiol Q2, vitamin D Q1 and estradiol Q3, vitamin D Q2 and estradiol Q1, vitamin D Q3 and estradiol Q3 were stably reflected in the three models (P for interaction < 0.05; Table 5; Fig. 1).
Table 4.
Odds ratios for the combined association of estradiol quartiles and vitamin D deficiency status with low SMM.
| Estradiol and Vitamin D deficiency | Unadjusted Model | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | ||||
| Q1 + VD deficiency | 3.849 (1.393, 10.634) | 0.009 | 2.776 (0.985,7.824) | 0.053 | 2.879 (1.021,8.123) | 0.046 | 3.898 (1.155,13.160) | 0.028 | |||
| Q2 + VD deficiency | 3.921 (1.391, 11.059) | 0.010 | 2.946 (1.021,8.502) | 0.046 | 3.047 (1.054,8.802) | 0.040 | 4.801 (1.378,16.721) | 0.014 | |||
| Q3 + VD deficiency | 2.987 (1.068, 8.355) | 0.037 | 2.628 (0.924,7.479) | 0.070 | 2.738 (0.961,7.8025) | 0.059 | 4.709 (1.365,16.251) | 0.014 | |||
| Q4 + VD deficiency | 0.768 (0.255, 2.313) | 0.639 | 0.910 (0.295,2.807) | 0.870 | 0.941 (0.304,2.910) | 0.916 | 1.970 (0.527,7.365) | 0.314 | |||
| Q1 + non-VD deficiency | 3.057 (0.887, 10.538) | 0.077 | 2.389 (0.679,8.405) | 0.175 | 2.530(0.717,8.921) | 0.149 | 3.416 (0.766,15.237) | 0.107 | |||
| Q2 + non-VD deficiency | 4.338 (1.160, 16.226) | 0.029 | 3.437 (0.898,13.148) | 0.071 | 3.637 (0.948,13.955) | 0.060 | 3.948 (0.745,20.935) | 0.107 | |||
| Q3 + non-VD deficiency | 2.548 (0.692, 9.375) | 0.159 | 2.368 (0.631,8.891) | 0.201 | 2.488 (0.650,9.217) | 0.186 | 4.454 (0.914,21.711) | 0.065 | |||
| Q4 + non-VD deficiency | Reference | Reference | Reference | Reference | |||||||
Notes: Bold indicates statistical significance. The model 1 adjusted for age, residence, marital status, educational level, BMI and fat mass; Model 2 adjusted for model 1 and smoking status, drinking status, physical activity; Model 3 adjusted for model 2 and triglyceride, menopausal status, dietary energy
Table 5.
Odds ratios for the combined association of estradiol quartiles and vitamin D quartiles with low SMM.
| Vitamin D and Estradiol | Unadjusted Model | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | ||||
| VD Q1 + estradiol Q1 | 3.339 (1.506,7.404) | 0.003 | 2.140 (0.920,4.982) | 0.077 | 2.178 (0.936,5.073) | 0.071 | 2.466 (0.906,6.711) | 0.077 | |||
| VD Q1 + estradiol Q2 | 7.008 (3.061,6.048) | < 0.001 | 4.915 (2.035,11.871) | < 0.001 | 4.964 (2.054,11.996) | < 0.001 | 5.849 (2.012,17.004) | 0.001 | |||
| VD Q1 + estradiol Q3 | 4.818 (2.128,10.907) | < 0.001 | 3.651 (1.545,8.629) | 0.003 | 3.704 (1.566,8.758) | 0.003 | 5.068 (1.783,14.403) | 0.002 | |||
| VD Q1 + estradiol Q4 | 0.723 (0.232,2.249) | 0.575 | 0.756 (0.239,2.391) | 0.634 | 0.751 (0.237,2.377) | 0.626 | 1.031 (0.280,3.791) | 0.964 | |||
| VD Q2 + estradiol Q1 | 5.154 (2.387,11.130) | < 0.001 | 3.35 (1.485,7.556) | 0.004 | 3.393 (1.503,7.659) | 0.003 | 3.409 (1.290,9.006) | 0.013 | |||
| VD Q2 + estradiol Q2 | 4.452 (1.841,0.767) | 0.001 | 2.731 (1.078,6.918) | 0.034 | 2.742 (1.081,6.955) | 0.034 | 3.045 (0.911,9.359) | 0.052 | |||
| VD Q2 + estradiol Q3 | 2.058 (0.844,5.020) | 0.113 | 1.466 (0.579,3.712) | 0.419 | 1.493 (0.59,3.781) | 0.398 | 1.795 (0.600,5.369) | 0.295 | |||
| VD Q2 + estradiol Q4 | 0.655 (0.194,2.214) | 0.496 | 0.707 (0.208,2.410) | 0.580 | 0.715 (0.210,2.441) | 0.593 | 1.093 (0.278,4.298) | 0.899 | |||
| VD Q3 + estradiol Q1 | 2.703 (1.170,6.244) | 0.020 | 1.856 (0.772,4.458) | 0.167 | 1.879 (0.782,4.518) | 0.159 | 1.731 (0.611,4.902) | 0.302 | |||
| VD Q3 + estradiol Q2 | 1.711 (0.626,4.675) | 0.295 | 1.216 (0.429,3.449) | 0.714 | 1.243 (0.438,3.527) | 0.683 | 1.764 (0.536,5.804) | 0.350 | |||
| VD Q3 + estradiol Q3 | 3.012 (1.310,6.927) | 0.009 | 2.59 (1.096,6.121) | 0.030 | 2.662 (1.125,6.298) | 0.026 | 4.117 (1.420,11.934) | 0.009 | |||
| VD Q3 + estradiol Q4 | 0.681 (0.219,2.118) | 0.507 | 0.713 (0.227,2.237) | 0.563 | 0.731 (0.232,2.297) | 0.591 | 1.101 (0.295,4.135) | 0.882 | |||
| VD Q4 + estradiol Q1 | 3.219 (1.424,7.275) | 0.005 | 2.183 (0.926,5.147) | 0.074 | 2.256 (0.956,5.324) | 0.063 | 2.288 (0.295,4.135) | 0.109 | |||
| VD Q4 + estradiol Q2 | 2.849 (1.130,7.178) | 0.026 | 2.144 (0.818,5.615) | 0.121 | 2.191 (0.835,5.751) | 0.111 | 2.062 (0.643,6.620) | 0.224 | |||
| VD Q4 + estradiol Q3 | 1.816 (0.726,4.544) | 0.202 | 1.685 (0.654,4.339) | 0.280 | 1.721 (0.668,4.436) | 0.261 | 1.958 (0.626,6.122) | 0.248 | |||
| VD Q4 + estradiol Q4 | Reference | Reference | Reference | Reference | |||||||
Notes: Bold indicates statistical significance. The model 1 adjusted for age, residence, marital status, educational level, BMI and fat mass; Model 2 adjusted for model 1 and smoking status, drinking status, physical activity; Model 3 adjusted for model 2 and triglyceride, menopausal status, dietary energy
Fig. 1.
The forest plot of interactions between quartile of vitamin D and estradiol on low skeletal muscle mass. Adjusted for age, residence, marital status, educational level, smoking status, drinking status, physical activity, BMI, FM, triglyceride, menopausal status, and dietary energy. Presented the forest plot of interactions between quartile of vitamin D and estradiol on low skeletal muscle mass among middle-aged and elderly women. The significant interactions between vitamin D Q1 and estradiol Q2, vitamin D Q1 and estradiol Q3, vitamin D Q2 and estradiol Q1, vitamin D Q3 and estradiol Q3 were stably reflected in the final model (P for interaction < 0.05), after adjusting potential confounding factors
Discussion
The primary objective of this study was to determine whether concentrations of vitamin D and estradiol were related to low SMM among middle-aged and elderly women. Our study revealed a negative correlation between low skeletal muscle mass and levels of vitamin D and estradiol. However, when considered confounding factors, including age, residence, marital status, educational level, smoking and drinking status, physical activity, BMI, FM, triglyceride, menopausal status, and dietary energy, these correlations were maintained in estradiol Q1, Q2, Q3 and vitamin D Q1. Furthermore, we evaluated whether there was any combined association of estradiol and vitamin D levels on low SMM. In this respects, we found that participants with the lower quartile of estradiol concentrations and vitamin D deficiency had a higher likelihood of developing low skeletal muscle, compared to those in the highest quartile of estradiol concentrations and non-vitamin D deficiency. Considering the applicability of the definition of vitamin D deficiency in the population, we further used the quartile of vitamin D to explore the interaction between vitamin D and estradiol on low SMM, obtaining similar results.
To our knowledge, not only is the connection between muscle atrophy and vitamin D and estradiol status ambiguous, but also these combined effects on muscle atrophy have not been studied. This study is the first study evaluating the combined association of estradiol and vitamin D levels on low SMM among middle-aged and elderly women. Previous studies have found that the muscle atrophy onset is multifactorial and determined by several promoting factors [32, 33]. Menopause seems to be particularly closely correlated with the beginning of muscle atrophy in women, which brings about hormone changes, especially estradiol [34]. Besides, muscle atrophy may also be triggered by vitamin D [35].
While estradiol levels change throughout life, the majority of women experience the menopausal transition in their mid-40s, a period of time during which the level of female hormones decreases and the menstrual cycle becomes irregular. In fact, estradiol is crucial for preserving muscle health in older people [36]. Previous researches have shown a close relationship between estradiol concentrations decrease and muscle atrophy [37, 38], which is in line with the findings of this investigation. However, controversial results have been reported, indicating that estradiol has no impact on postmenopausal women’s muscle atrophy [39]. Despite all this, several basic experimental studies have confirmed that interleukin (IL)-6, IL-1, and tumor necrosis factor-a (TNF-α) production are all closely associated with menopause [40]. Meanwhile, the IL-6 and TNF-α can impair muscle performance [41, 42], causing sarcopenia [43, 44].
Additionally, vitamin D, a vital hormone linked to muscle physiology, appears to be involved in muscle atrophy [45]. According to prior researches, low muscle strength and physical performance of elderly adults are associated with their low vitamin D concentration [46–49]. Meanwhile, other studies also revealed that older adults with vitamin D deficiency are more likely to develop muscle mass and muscle strength decline [50, 51]. These outcomes are consistent with those from our study, which demonstrated a significant relationship between low vitamin D concentrations and low skeletal muscle mass in relation to recent muscle atrophy. Given the lack of clearly defined mechanisms, the genomic pathway using the nuclear receptor VDR [52] and the non-genomic pathway, where vitamin D enters and affects cells directly through the cell surface fossa [53], are the potential mechanisms. Myofibres and numerous other cell types combine to form the mature skeletal muscle, which also contains vitamin D target cells [54]. As a result, vitamin D may interact intricately with the different skeletal muscle cells and tissues to affect muscle mass and performance [35].
In this study, low concentrations of vitamin D and estradiol have combined effect on muscle atrophy. Estradiol is known to decrease among the menopausal transition and vitamin D deficiency occur at lots of countries worldwide [55]. According to prior research, the relationship between vitamin D and estradiol in female populations remains inconclusive. Some studies have found a significant negative correlation between 25(OH) D and estrogen in fertile women [56], while similar findings were observed in postmenopausal women [57]. On the other hand, other studies have reported a positive correlation between vitamin D and estradiol [58], suggesting that their relationship may be influenced by multiple factors and may involve mutual regulation. Meanwhile, the hormone as a crucial element throughout life and decrease with aging, especially in muscle atrophy development. Notably, other evidences suggested that the hormone replacement therapy is good for muscle mass and strength in postmenopausal women [59, 60]. Nutritional and lifestyle factors may not only benefit muscle mass and performance, but also affordable and secure. However, despite the fact that a lot of research has been done in the past on supplement therapy, more research is required to evaluate the effectiveness and long-term safety of potential therapeutic interventions aimed at improving muscle function.
The present study has several benefits, including the fact that potential confounding factors like socioeconomic status, lifestyle, and macronutrients were taken into account when conducting the analyses. Moreover, from a dietary and nutritional perspective, it should also be pointed out that our research design and analysis methodology can effectively prevented confounding changes in overall macronutrient balance and dietary intake. Simultaneously, in contrast to prior research, this study also explored the impact of low skeletal muscle mass in middle-aged and elderly women, examining the interaction between estradiol and vitamin D. However, constraints on the current study should be taken into account. First, instead of dual-energy X-ray absorptiometry, which is the gold standard method for determining human body composition, BIA was employed because it is a reliable and useful method [61]. Second, we have to emphasize that a relatively small sample of rural women were included in this research, so the more in-depth research is still needed.
Conclusions
In conclusion, vitamin D deficiency is common among middle-aged and elderly women, and estradiol declines during the menopausal transition, both of which have important fundamental biological effects and interactions on muscle mass and performance. We conclude the vitamin D and estradiol were interactively correlated with low skeletal muscle mass in middle-aged and elderly women. Therefore, the combination of estradiol and vitamin D supplements should be encouraged for middle-aged and elderly women who are at risk of muscle atrophy or experiencing muscle atrophy.
Acknowledgements
The China North-West Natural Population Cohort: Ningxia Project (CNC-NX) Study Group, as well as all participants in this study, are gratefully acknowledged by the authors for their assistance.
Author contributions
Conceptualization, Yu-Hong Zhang, Yi Zhao and Lan-Liu; Methodology, Jia-Xing Zhang and Qing-An Wang; Formal analysis, Jia-Xing Zhang and Ya-Long Cheng; Data Curation, Chan-Yang, Jiang-Wei Qiu, Juan-Li and Xiao-Wei Liu; Writing-Original Draft Preparation, Jia-Xing Zhang and Ya-Long Cheng; Writing-Review & Editing, Jia-Xing Zhang and Chen-Chen; Visualization, Qing-An Wang; Supervision, Yu-Hong Zhang and Lan-Liu; Project Administration, Yi Zhao; Funding Acquisition, Yu-Hong Zhang and Yi Zhao. All authors revised the manuscript critically and approved the final article.
Funding
The research was supported by National Key Research and Development Program of China (2017YFC0907204), the Key Research and Development Program of Ningxia (2021BEG02026) and Natural Science Foundation of Ningxia Province (2022AAC03143).
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to privacy or ethical restrictions but are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The present study was evaluated by the Institutional Ethics Committees (IECs) of Ningxia Medical University in accordance with the principles set forth in the Helsinki Declaration (Ethics ID 2018-012, 2020 − 689).
Consent to participate
As noted in the manuscript, the written informed consent of all participants were obtained at the beginning of the investigation.
Consent for publication
Not applicable.
Footnotes
The original online version of this article was revised: the funding section has been updated.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jiaxing Zhang and Yalong Cheng contributed equally to this work.
Change history
10/24/2023
A Correction to this paper has been published: 10.1186/s12905-023-02687-4
References
- 1.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: european consensus on definition and diagnosis. Age Ageing. 2010;39(4):412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised european consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hida T, Shimokata H, Sakai Y, Ito S, Matsui Y, Takemura M, et al. Sarcopenia and sarcopenic leg as potential risk factors for acute osteoporotic vertebral fracture among older women. Eur Spine J. 2016;25(11):3424–31. doi: 10.1007/s00586-015-3805-5. [DOI] [PubMed] [Google Scholar]
- 4.Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50(5):889–96. doi: 10.1046/j.1532-5415.2002.50216.x. [DOI] [PubMed] [Google Scholar]
- 5.Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MAF. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am J Clin Nutr. 2002;76(2):473–81. doi: 10.1093/ajcn/76.2.473. [DOI] [PubMed] [Google Scholar]
- 7.Morley JE, Anker SD, von Haehling S. Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology-update 2014. J Cachexia Sarcopenia Muscle. 2014;5(4):253–9. doi: 10.1007/s13539-014-0161-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bentzinger CF, Rudnicki MA. Rejuvenating aged muscle stem cells. Nat Med. 2014;20(3):234–5. doi: 10.1038/nm.3499. [DOI] [PubMed] [Google Scholar]
- 9.Anderson LJ, Liu H, Garcia JM. Sex differences in muscle wasting. Adv Exp Med Biol. 2017;1043:153–97. doi: 10.1007/978-3-319-70178-3_9. [DOI] [PubMed] [Google Scholar]
- 10.Churchward-Venne TA, Breen L, Phillips SM. Alterations in human muscle protein metabolism with aging: protein and exercise as countermeasures to offset sarcopenia. BioFactors. 2014;40(2):199–205. doi: 10.1002/biof.1138. [DOI] [PubMed] [Google Scholar]
- 11.Zhang JX, Li J, Chen C, Yin T, Wang QA, Li XX, et al. Reference values of skeletal muscle mass, fat mass and fat-to-muscle ratio for rural middle age and older adults in western China. Arch Gerontol Geriatr. 2021;95:104389. doi: 10.1016/j.archger.2021.104389. [DOI] [PubMed] [Google Scholar]
- 12.Yang L, Smith L, Hamer M. Gender-specific risk factors for incident sarcopenia: 8-year follow-up of the English longitudinal study of ageing. J Epidemiol Community Health. 2019;73(1):86–8. doi: 10.1136/jech-2018-211258. [DOI] [PubMed] [Google Scholar]
- 13.Carr MC. The emergence of the metabolic syndrome with menopause. J Clin Endocrinol Metab. 2003;88(6):2404–11. doi: 10.1210/jc.2003-030242. [DOI] [PubMed] [Google Scholar]
- 14.Messier V, Rabasa-Lhoret R, Barbat-Artigas S, Elisha B, Karelis AD, Aubertin-Leheudre M. Menopause and sarcopenia: a potential role for sex hormones. Maturitas. 2011;68(4):331–6. doi: 10.1016/j.maturitas.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 15.La Colla A, Pronsato L, Milanesi L, Vasconsuelo A. 17β-Estradiol and testosterone in sarcopenia: role of satellite cells. Ageing Res Rev. 2015;24:166–77. doi: 10.1016/j.arr.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Geraci A, Calvani R, Ferri E, Marzetti E, Arosio B, Cesari M. Sarcopenia and Menopause: the role of Estradiol. Front Endocrinol (Lausanne) 2021;12:682012. doi: 10.3389/fendo.2021.682012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lerchbaum E. Vitamin D and menopause–a narrative review. Maturitas. 2014;79(1):3–7. doi: 10.1016/j.maturitas.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 18.Huang H, Guo J, Chen Q, Chen X, Yang Y, Zhang W, et al. The synergistic effects of vitamin D and estradiol deficiency on metabolic syndrome in chinese postmenopausal women. Menopause. 2019;26(10):1171–7. doi: 10.1097/GME.0000000000001370. [DOI] [PubMed] [Google Scholar]
- 19.Yang C, Liu X, Li J, Yan N, Dang Y, Chang Z, et al. Association of serum vitamin D and estradiol levels with metabolic syndrome in Rural Women of Northwest China: a cross-sectional study. Metab Syndr Relat Disord. 2022;20(3):182–9. doi: 10.1089/met.2021.0120. [DOI] [PubMed] [Google Scholar]
- 20.Houston DK, Cesari M, Ferrucci L, Cherubini A, Maggio D, Bartali B et al. Association between vitamin D status and physical performance: the InCHIANTI study. Journals of Gerontology Series a-Biological Sciences and Medical Sciences. 2007;62(4):440–6. [DOI] [PMC free article] [PubMed]
- 21.Vaes AMM, Brouwer-Brolsma EM, Toussaint N, de Regt M, Tieland M, van Loon LJC, et al. The association between 25-hydroxyvitamin D concentration, physical performance and frailty status in older adults. Eur J Nutr. 2019;58(3):1173–81. doi: 10.1007/s00394-018-1634-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tomlinson PB, Joseph C, Angioi M. Effects of vitamin D supplementation on upper and lower body muscle strength levels in healthy individuals. A systematic review with meta-analysis. J Sci Med Sport. 2015;18(5):575–80. doi: 10.1016/j.jsams.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 23.Beaudart C, Buckinx F, Rabenda V, Gillain S, Cavalier E, Slomian J, et al. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2014;99(11):4336–45. doi: 10.1210/jc.2014-1742. [DOI] [PubMed] [Google Scholar]
- 24.Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol. 2000;89(2):465–71. doi: 10.1152/jappl.2000.89.2.465. [DOI] [PubMed] [Google Scholar]
- 25.Kim J, Wang ZM, Heymsfield SB, Baumgartner RN, Gallagher D. Total-body skeletal muscle mass: estimation by a new dual-energy X-ray absorptiometry method. Am J Clin Nutr. 2002;76(2):378–83. doi: 10.1093/ajcn/76.2.378. [DOI] [PubMed] [Google Scholar]
- 26.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 27.Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–7. doi: 10.1016/j.jamda.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 28.Gold EB. The timing of the age at which natural menopause occurs. Obstet Gynecol Clin N Am. 2011;38(3). [DOI] [PMC free article] [PubMed]
- 29.Mogren IM. Physical activity and persistent low back pain and pelvic pain post partum. BMC Public Health. 2008;8:417. doi: 10.1186/1471-2458-8-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y, Xiaoqing J, Xinhua T, Xiaoling S, Xiaoling X, Wei Y, et al. Effects of a comprehensive intervention on hypertension control in chinese employees working in universities based on mixed models. Sci Rep. 2019;9(1):19187. doi: 10.1038/s41598-019-55849-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patterson E. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)-Short and Long Forms. 2005.
- 32.Tournadre A, Vial G, Capel F, Soubrier M, Boirie Y, Sarcopenia Joint bone Spine. 2019;86(3):309–14. doi: 10.1016/j.jbspin.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Priego T, Martín AI, González-Hedström D, Granado M, López-Calderón A. Role of hormones in sarcopenia. Hormones and Aging. Vitamins and Hormones2021. p. 535 – 70. [DOI] [PubMed]
- 34.Juppi HK, Sipilä S, Cronin NJ, Karvinen S, Karppinen JE, Tammelin TH et al. Role of menopausal transition and physical activity in loss of lean and muscle Mass: a Follow-Up study in Middle-Aged finnish women. J Clin Med. 2020;9(5). [DOI] [PMC free article] [PubMed]
- 35.Mizuno T, Hosoyama T, Tomida M, Yamamoto Y, Nakamichi Y, Kato S et al. Influence of vitamin D on sarcopenia pathophysiology: a longitudinal study in humans and basic research in knockout mice. J Cachexia Sarcopenia Muscle. 2022. [DOI] [PMC free article] [PubMed]
- 36.Kenny AM, Dawson L, Kleppinger A, Iannuzzi-Sucich M, Judge JO. Prevalence of sarcopenia and predictors of skeletal muscle mass in nonobese women who are long-term users of estrogen-replacement therapy. J Gerontol A Biol Sci Med Sci. 2003;58(5):M436–40. doi: 10.1093/gerona/58.5.m436. [DOI] [PubMed] [Google Scholar]
- 37.Cooper R, Mishra G, Clennell S, Guralnik J, Kuh D. Menopausal status and physical performance in midlife: findings from a british birth cohort study. Menopause (New York NY) 2008;15(6):1079–85. doi: 10.1097/gme.0b013e31816f63a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Geel TA, Geusens PP, Winkens B, Sels JP, Dinant GJ. Measures of bioavailable serum testosterone and estradiol and their relationships with muscle mass, muscle strength and bone mineral density in postmenopausal women: a cross-sectional study. Eur J Endocrinol. 2009;160(4):681–7. doi: 10.1530/EJE-08-0702. [DOI] [PubMed] [Google Scholar]
- 39.Javed AA, Mayhew AJ, Shea AK, Raina P. Association between hormone therapy and muscle Mass in Postmenopausal Women: a systematic review and Meta-analysis. JAMA Netw open. 2019;2(8):e1910154. doi: 10.1001/jamanetworkopen.2019.10154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cioffi M, Esposito K, Vietri MT, Gazzerro P, D’Auria A, Ardovino I, et al. Cytokine pattern in postmenopause. Maturitas. 2002;41(3):187–92. doi: 10.1016/s0378-5122(01)00286-9. [DOI] [PubMed] [Google Scholar]
- 41.Roth SM, Metter EJ, Ling S, Ferrucci L. Inflammatory factors in age-related muscle wasting. Curr Opin Rheumatol. 2006;18(6):625–30. doi: 10.1097/01.bor.0000245722.10136.6d. [DOI] [PubMed] [Google Scholar]
- 42.Buford TW, Anton SD, Judge AR, Marzetti E, Wohlgemuth SE, Carter CS, et al. Models of accelerated sarcopenia: critical pieces for solving the puzzle of age-related muscle atrophy. Ageing Res Rev. 2010;9(4):369–83. doi: 10.1016/j.arr.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leveille SG. Musculoskeletal aging. Curr Opin Rheumatol. 2004;16(2):114–8. doi: 10.1097/00002281-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Dobs AS, Nguyen T, Pace C, Roberts CP. Differential effects of oral estrogen versus oral estrogen-androgen replacement therapy on body composition in postmenopausal women. J Clin Endocrinol Metab. 2002;87(4):1509–16. doi: 10.1210/jcem.87.4.8362. [DOI] [PubMed] [Google Scholar]
- 45.Pojednic RM, Ceglia L. The emerging biomolecular role of vitamin D in skeletal muscle. Exerc Sport Sci Rev. 2014;42(2):76–81. doi: 10.1249/JES.0000000000000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Suzuki T, Kwon J, Kim H, Shimada H, Yoshida Y, Iwasa H, et al. Low serum 25-hydroxyvitamin D levels associated with falls among japanese community-dwelling elderly. J bone Mineral Research: Official J Am Soc Bone Mineral Res. 2008;23(8):1309–17. doi: 10.1359/jbmr.080328. [DOI] [PubMed] [Google Scholar]
- 47.Hirani V, Cumming RG, Naganathan V, Blyth F, Le Couteur DG, Hsu B, et al. Longitudinal Associations between vitamin D metabolites and Sarcopenia in older australian men: the Concord Health and Aging in Men Project. J Gerontol A Biol Sci Med Sci. 2017;73(1):131–8. doi: 10.1093/gerona/glx086. [DOI] [PubMed] [Google Scholar]
- 48.Dodds RM, Granic A, Davies K, Kirkwood TB, Jagger C, Sayer AA. Prevalence and incidence of sarcopenia in the very old: findings from the Newcastle 85 + study. J Cachexia Sarcopenia Muscle. 2017;8(2):229–37. doi: 10.1002/jcsm.12157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sohl E, van Schoor NM, de Jongh RT, Visser M, Deeg DJ, Lips P. Vitamin D status is associated with functional limitations and functional decline in older individuals. J Clin Endocrinol Metab. 2013;98(9):E1483–90. doi: 10.1210/jc.2013-1698. [DOI] [PubMed] [Google Scholar]
- 50.Houston DK, Tooze JA, Hausman DB, Johnson MA, Nicklas BJ, Miller ME, et al. Change in 25-hydroxyvitamin D and physical performance in older adults. J Gerontol A Biol Sci Med Sci. 2011;66(4):430–6. doi: 10.1093/gerona/glq235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huo YR, Suriyaarachchi P, Gomez F, Curcio CL, Boersma D, Muir SW, et al. Phenotype of osteosarcopenia in older individuals with a history of falling. J Am Med Dir Assoc. 2015;16(4):290–5. doi: 10.1016/j.jamda.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 52.Girgis CM, Clifton-Bligh RJ, Hamrick MW, Holick MF, Gunton JE. The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr Rev. 2013;34(1):33–83. doi: 10.1210/er.2012-1012. [DOI] [PubMed] [Google Scholar]
- 53.Haussler MR, Jurutka PW, Mizwicki M, Norman AW. Vitamin D receptor (VDR)-mediated actions of 1α,25(OH) vitamin D: genomic and non-genomic mechanisms. Best Pract Res Clin Endocrinol Metab. 2011;25(4):543–59. doi: 10.1016/j.beem.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 54.Braga M, Simmons Z, Norris KC, Ferrini MG, Artaza JN. Vitamin D induces myogenic differentiation in skeletal muscle derived stem cells. Endocr Connections. 2017;6(3):139–50. doi: 10.1530/EC-17-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stewart JW, Alekel DL, Ritland LM, Van Loan M, Gertz E, Genschel U. Serum 25-hydroxyvitamin D is related to indicators of overall physical fitness in healthy postmenopausal women. Menopause (New York NY) 2009;16(6):1093–101. doi: 10.1097/gme.0b013e3181a8f7ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Donayeva A, Amanzholkyzy A, Abdelazim IA, Saparbayev S, Nurgaliyeva R, Kaldybayeva A, et al. The relation between vitamin D and the adolescents’ mid-luteal estradiol and progesterone. Eur Rev Med Pharmacol Sci. 2023;27(14):6792–9. doi: 10.26355/eurrev_202307_33150. [DOI] [PubMed] [Google Scholar]
- 57.Lerchbaum E, Obermayer-Pietsch B. Vitamin D and fertility: a systematic review. Eur J Endocrinol. 2012;166(5):765–78. doi: 10.1530/EJE-11-0984. [DOI] [PubMed] [Google Scholar]
- 58.Liu C, Kuang X, Li K, Guo X, Deng Q, Li D. Effects of combined calcium and vitamin D supplementation on osteoporosis in postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. Food Funct. 2020;11(12):10817–27. doi: 10.1039/d0fo00787k. [DOI] [PubMed] [Google Scholar]
- 59.Sipilä S, Narici M, Kjaer M, Pöllänen E, Atkinson RA, Hansen M, et al. Sex hormones and skeletal muscle weakness. Biogerontology. 2013;14(3):231–45. doi: 10.1007/s10522-013-9425-8. [DOI] [PubMed] [Google Scholar]
- 60.Dam TV, Dalgaard LB, Ringgaard S, Johansen FT, Bisgaard Bengtsen M, Mose M, et al. Transdermal Estrogen Therapy improves gains in skeletal muscle Mass after 12 weeks of resistance training in early postmenopausal women. Front Physiol. 2020;11:596130. doi: 10.3389/fphys.2020.596130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marra M, Sammarco R, De Lorenzo A, Iellamo F, Siervo M, Pietrobelli A, et al. Assessment of Body Composition in Health and Disease using Bioelectrical Impedance Analysis (BIA) and Dual Energy X-Ray Absorptiometry (DXA): a critical overview. Contrast Media Mol Imaging. 2019;2019:3548284. doi: 10.1155/2019/3548284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available due to privacy or ethical restrictions but are available from the corresponding author on reasonable request.