Abstract
Background and Objectives:
Psychosocial stressors have been implicated in childhood obesity, but the role of racism-related stressors is less clear. This study explored associations between neighborhood inequities, discrimination/harassment, and child body mass index (BMI).
Methods:
Parents of children (n=1,307, ages 5–9 from diverse racial/ethnic backgrounds) completed surveys of their child’s exposure to discrimination/harassment. Census tract data derived from addresses were used to construct index of concentration at the extremes, a measure of neighborhood social polarization. Child height and weight were obtained from medical records. Multiple regression and hierarchical models examined child BMI and racism at the individual and census tract levels.
Results:
Children residing in the most Black-homogenous census tracts had 8.2 percentage units higher BMI percentile (95%CI: 1.5, 14.9) compared to White-homogenous tracts (p=0.03). Household income and home values were lower, poverty rates higher, and single parent households more common among Black-homogeneous census tracts. Almost 30% of children experienced discrimination/harassment in the past year, which was associated with a 5.28 unit higher BMI percentile (95%CI: 1.72–8.84, p=0.004).
Conclusions:
Discrimination and racial/economic segregation were correlated with higher child BMI. Longitudinal studies are needed to understand whether these factors may be related to weight gain trajectories and future health.
Keywords: Racism, Discrimination, Childhood, Obesity
Introduction
Childhood obesity disproportionately affects children from minoritized racial/ethnic backgrounds and is strongly associated with adverse health outcomes in adulthood, including type 2 diabetes and cardiovascular disease.1,2 Decades of research has focused on identifying factors contributing to childhood obesity disparities, with most studies focused on behavioral mechanisms that are the common intervention targets to improve energy balance (e.g., diet, physical activity, screen time).3–5 However, the factors that underlie the persistence of racial/ethnic inequities in childhood obesity are multifactorial in nature and extend well beyond the contributions of individual health behaviors to the role of larger systems, likely rooted in racism.6,7 Structural racism is defined as the macrolevel systems, social forces, institutions, ideologies, and processes that generate and reinforce inequities among racial and ethnic groups8 and have been codified into custom, practice, and law.9 Racial residential segregation is one example of structural racism, resulting from discrimination, steering, and exclusion in housing markets.10–12 Past research has linked neighborhood residential segregation and other structural racism to health and health inequities, including obesity.13–16 In addition to neighborhood forces, the Levels of Racism9 theoretical framework postulates that racism operates at multiple levels, including the individual/interpersonal level, and discrimination can occur on the basis of multiple characteristics (e.g., religion, social class, weight).17,18 Individual experiences of discrimination and harassment, including race discrimination, have been associated with adiposity and body mass index (BMI).19,20 However, the majority of prior studies have examined these relationships among adults or adolescents, without consideration of younger children.21 This is a significant omission given the importance of early life experiences to future health.22 Although there is a considerable body of evidence indicating adversity during childhood is associated with negative health outcomes including obesity,23 few studies have examined the health impact of racism-related stressors during childhood.24,25 Fewer studies still have considered both reported experiences of discrimination and harassment in addition to neighborhood level structural inequities when examining racism-related stressors during childhood.
The current study examined cross-sectional associations between perceived discrimination, neighborhood structural inequities and children’s body mass index (BMI) percentiles in a large cohort of elementary school-aged children from diverse racial/ethnic backgrounds participating in a longitudinal observational study of childhood obesity disparities. Specifically, we sought to characterize what types of discrimination and harassment elementary school-aged children most frequently encounter and whether these experiences are associated with children’s BMI. Secondly, we sought to examine associations between structural environmental inequities at the neighborhood level and children’s BMI percentile. We hypothesized that higher reported levels of discrimination and greater neighborhood inequities would be associated with higher child BMI percentiles, after adjusting for established correlates of child BMI percentile. In examining both neighborhood level and interpersonal discrimination in relationship to children’s BMI percentiles, our study will provide information that can be used to guide the development of systemic and multi-level interventions to address racial/ethnic obesity disparities.
Methods
This is a secondary analysis of data collected as part of the Family Matters study (R01 HL126171; HL156994)26,27, an observational cohort study of risk and protective factors connected to childhood obesity disparities. Parent-child dyads were recruited from primary care clinics in Minneapolis-St. Paul, Minnesota and data collected between 2016–2019. Primary care clinics offer an excellent setting for study recruitment, in that they serve a high proportion of children from racially/ethnically and socioeconomically diverse households, have direct access to parents, and reach participants in a familiar environment. Parents/guardians were eligible if they had a child 5–9 years of age, lived in the Twin Cities, and could read English, Spanish, Somali or Hmong. Potential participants received a follow-up phone call (in their own language) by a research team member matching their race/ethnicity one to two weeks after recruitment letters were sent from their clinic to confirm receipt of recruitment letter, answer any questions, review eligibility requirements, and invite study participation. Exclusion criteria were children with medically necessary dietary restrictions (e.g., feeding tubes), BMI <5th percentile, or diagnosis of serious and persistent mental illness. Study design included purposeful recruitment of children across six racial/ethnic groups (White, Black, Native American, Hmong, Somali, and Latino) to ensure diversity for subpopulation analyses, which was achieved by asking participants at the time of recruitment to select which of these 6 race/ethnicity options best described their household. Once consented, parents completed an online survey independently within approximately 1–2 weeks after enrollment.
The University of Minnesota Institutional Review Board approved all components of the study. All parents provided informed consent to participate in accordance with the Declaration of Helsinki.
Measures:
Body Mass Index.
Age and sex adjusted BMI percentile was the primary outcome of interest for this analysis. Child weight and height data were obtained through electronic medical records from recruiting family medicine clinics. BMI percentiles were calculated for the participating child using an online CDC calculator28.
Perceived discrimination and harassment:
An adapted version of The Everyday Discrimination Scale29 was used to measure parent-reported experiences of their child’s exposure to discrimination on the following dimensions: race, religious, financial, weight, and appearance. Parents reported frequency on a Likert scale (0-Never; 1-Less than once a year; 2-A few times a year; 3-A few times a month; and 4-At least once a week).
Neighborhood-level structural inequities:
Households covered 367 Minneapolis-St. Paul census tracts, which represents a majority of census tracts in the sampling frame. Geospatial analyses operationalized neighborhood privilege using the Index of Concentration at the Extremes (ICE),30,31 a measure of residential segregation, economic disparity, and the intersection of race and economic disparities to capture social polarization. It was computed by attaching census tract ID to participant data using household address.
Where:
Five census tract-level ICE variables were operationalized: 1) White extreme and Black extreme, 2) non-Hispanic White and non-Hispanic Black extreme, 3) high- (>$100,000) and low-income (<$25,000) extremes, 4) White, high-income and Black, low-income extreme, and 5) non-Hispanic White, high-income and non-Hispanic Black, low-income extreme. These variables were constructed as categorical variables of equal quintile sample size. Of note, census tracts do not distinguish Somali or Hmong ethnicity. American Community Survey (ACS) data from 2014–2018 was used for computation of all ICE variables and neighborhood socio-demographic statistics including tract median income, mortgage, rent, and home values as well as tract poverty rate and fraction owner-occupied housing, > 1 person per room of home, single-parent, no access to a vehicle, civil unemployment, and fraction at least a high school education and less than 9th grade education. These items were used to characterize census tracts of participants and linked to parent survey and child BMI percentile using Federal Information Processing Standard (FIPS) code.
Socio-demographics.
Via online survey, parents reported their own and their child’s sex (female or male), their own and the child’s race/ethnicity across eligible groups (White, Black, Native American, Hmong, Somali, Latino—check all that apply), yearly total household income (<$20k, $20k-$34,999, $35k-$49,999, $50k-$74,999, $75k-$99,999, ≥$100k) and their highest level of education completed (middle school or junior high; some high school; high school or GED; vocational, technical, trade or other certification program; associate degree; bachelor degree; graduate or professional degree; Other).
Statistical Analysis
Descriptive statistics and frequency tabulations were used to characterize participating children and their neighborhoods. All mapping was done utilizing Quantum Geographic Information System (QGIS) software version 3.10.10-A Coruña.32–36 The average BMI for each census tract was calculated using the Count Points on Polygon feature within the Analysis Tools section of QGIS. The average BMI for each census tract was overlayed with the percent Black/African American for each specific census tract which was obtained from ACS data. Multiple regression was used to examine the discrimination and harassment correlates of child BMI percentile with controls for parent and child age and sex, household income and race/ethnicity, and parent educational attainment. The unit of analysis was at the child-level for these models. Interaction analyses were conducted to examine if child race modified the discrimination/harassment-BMI percentile associations. However, there was not statistical support for modification at p<0.05. The non-interaction model estimates were retained. Geospatial analyses were analyzed with the census tract as the unit of analysis and utilized hierarchical linear mixed models with a random intercept specified for the census tract FIPS code to address neighborhood correlated error terms. Participant child BMI percentile was collapsed to the census tract-level (n=367) and operationalized as an average tract BMI percentile. ACS data were attached including the ICE predictors as well as socio-demographic tract-level controls to adjust for fraction of households headed by a single parent and the ratio of households making $10,000 relative to those over $50,000. Data management and analysis were conducted in Stata 17.0 MP (College Station, TX).
Results
Sample Demographics
The study sample (Table 1) predominantly consisted of children who were normal weight (i.e., BMI >5th percentile and <85th percentile), with 19% of the sample having obesity, consistent with the population prevalence of childhood obesity in the United States37. Twenty-one percent of households identified as Black, 10% as Somali/Ethiopian, 18% White, 17% Hmong, 16% Hispanic, and 16% Native American. One third of caregivers were immigrants (n=448), 75% of whom had been living in the U.S. for 10 or more years. More than half of participating caregivers reported a high school education or less, and one third had at least some college or had received their bachelor’s degree. Fifty five percent of the sample reported household income <$34,999 annually and 18% of the sample reported annual income of at least $75,000.
Table 1.
Demographic characteristics of the Family Matters cohort
| Children | |
|---|---|
| N (%) | |
| Female | 637 (49%) |
| Mean age in years (SD) | 6.97 (1.5) |
| Mean BMI Percentile (SD) | 66.2 (28.3) |
| Body Mass Index (BMI) Status | |
| Normal Weight (5th to <85th percentile) | 843 (65%) |
| Overweight (85th to < 95th percentile) | 218 (17%) |
| Obesity (≥ 95th percentile) | 246 (19%) |
| Race/Ethnicity | |
| White | 234 (18%) |
| Black or African American | 334 (26%) |
| Hispanic or Latino | 177 (14%) |
| Asian American | 220 (17%) |
| Native Hawaiian or other Pacific Islander | 10 (1%) |
| American Indian or Native American | 116 (9%) |
| Multiracial | 200 (15%) |
| Other | 16 (1%) |
| Primary Caregivers | |
| N (%) | |
| Female | 1171 (90%) |
| Mean age in years (SD) | 35.7 (7.9) |
| Born in the U.S. | 859 (66%) |
| Immigrant time living in the U.S. | |
| Less than 1 year | 8 (2%) |
| 1 to less than 5 years | 52 (12%) |
| 5 – 10 years | 51 (11%) |
| 10+ years | 336 (75%) |
| Not reported | 1 (0%) |
| Race/Ethnicity | |
| White | 272 (21%) |
| Black or African American | 340 (26%) |
| Hispanic or Latino | 186 (14%) |
| Asian American | 223 (17%) |
| Native Hawaiian or other Pacific Islander | 10 (1%) |
| American Indian or Native American | 154 (12%) |
| Multiracial | 103 (8%) |
| Other | 19 (1%) |
| Survey Language | |
| English | 1148 (88%) |
| Spanish | 134 (10%) |
| Hmong/Lus Hmoob | 8 (1%) |
| Somali/Soomaali | 17 (1%) |
| Educational Attainment | |
| Some high school | 183 (14%) |
| High school or Associates | 521 (40%) |
| Some College or Bachelors | 409 (31%) |
| Graduate Degree | 194 (15%) |
| Household Income | |
| Less than $20,000 | 393 (30%) |
| $20,000 - $34,999 | 323 (25%) |
| $35,000 - $49,999 | 203 (16%) |
| $50,000 - $74,999 | 143 (11%) |
| $75,000 - $99,999 | 75 (6%) |
| $100,000 or more | 159 (12%) |
| Not reported | 11 (1%) |
Parent-reported discrimination and harassment of child and adjusted correlates of child BMI percentile
Parents reported on their perceptions of the discrimination that their child experienced over the course of the past year (Table 2). In that time frame, 28% of children in the cohort had reportedly experienced some form of discrimination/harassment, with 16% of children experiencing discrimination/harassment in two or more domains. The experience of any type of discrimination/harassment was associated with a 5.28 unit higher BMI percentile (95% CI: 1.72–8.84, p = 0.004). Black and Native American youth were more likely to have encountered discrimination. In follow-up analyses, the most frequent form of discrimination/harassment reported was related to appearance, followed by weight and race-based discrimination. Weight-related discrimination/harassment correlated with child BMI percentile such that children whose parents reported that their child experienced weight-related discrimination/harassment had BMI percentiles that were 12.3 points higher than those for whom no weight-related harassment was reported (95% CI: 7.5, 17.1; P<0.001).
Table 2.
Adjusted Discrimination and Harassment Item Correlates of BMI Percentile (N=1,307 children)
| Domains of Discrimination and Harassment | n (%) | Child BMI%ile Association | P Value |
|---|---|---|---|
| Any within the past year | 362 (28%) | 5.3 (1.7, 8.8) | 0.004 |
| ∘ Racial | 170 (13%) | 3.8 (−0.8, 8.5) | 0.108 |
| ∘ Religious | 66 (5%) | 2.4 (−4.8, 9.6) | 0.519 |
| ∘ Financial | 85 (7%) | −1.2 (−7.3, 5) | 0.077 |
| ∘ Weight | 183 (14%) | 12.3 (7.5, 17.1) | <0.001 |
| ∘ Appearance | 246 (19%) | 3.8 (−0.2, 7.8) | 0.062 |
|
Frequency
(ref: Never) |
|||
| Racial | |||
| Less than once a year | 100 (8%) | 3 (−2.7, 8.8) | 0.392 |
| A few times a year | 46 (4%) | 5.4 (−2.2, 13) | |
| A few times a month/ at least weekly | 24 (1%) | 4 (−9.2, 17.3) | |
| Religious | |||
| Less than once a year | 35 (3%) | 1.3 (−8.3, 10.9) | 0.277 |
| A few times a year | 22 (2%) | 9.4 (−1.6, 20.4) | |
| A few times a month/ at least weekly | 9 (1%) | −10.7 (−32.3, 10.9) | |
| Financial | |||
| Less than once a year | 49 (4%) | −1.1 (−8.9, 6.7) | 0.585 |
| A few times a year | 23 (2%) | 3.8 (−6.3, 13.9) | |
| A few times a month/ at least weekly | 13 (1%) | −10.2 (−28, 7.5) | |
| Weight | |||
| Less than once a year | 84 (6%) | 9.7 (2.9, 16.4) | <0.001 |
| A few times a year | 60 (5%) | 13.5 (5.9, 21.1) | |
| A few times a month/ at least weekly | 39 (2%) | 16.1 (7, 25.3) | |
| Appearance | |||
| Less than once a year | 134 (10%) | 1 (−4.1, 6.1) | 0.038 |
| A few times a year | 79 (6%) | 8.9 (2.8, 15) | |
| A few times a month/ at least weekly | 33 (2%) | 3.2 (−8.1, 14.4) |
Adjusted Covariates: Parent and child age and sex, race/ethnicity, household income, and parent educational attainment
Non-linear relationships between the frequency of each type of discrimination and BMI percentile were examined. Weight and appearance-related discrimination/harassment were strong predictors of elevated BMI percentile (p<0.001 and p=0.038 respectively). Weight discrimination/harassment exhibited a large threshold effect at low levels of frequency indicated by the less than once a year/never contrast (9.7; 95% CI: 2.9, 16.4), after which the effect size increased at a constant rate. A threshold effect was observed for appearance-related discrimination/harassment at the few times a year/never contrast (8.9; 95% CI: 2.8, 15), such that infrequent appearance-related discrimination/harassment (i.e., less than once a year) was not strongly correlated with BMI percentile, but more frequent discrimination and harassment (i.e., more than few times a year) was strongly correlated with child BMI percentile.
Neighborhood characteristics and adjusted correlates of child BMI percentile
Within this cohort, the prevalence of childhood overweight/obesity appears higher among children residing in neighborhoods that are predominantly Black/African American; neighborhoods which, importantly, experience higher rates of poverty and neighborhood deprivation. Figure 1 shows the Minneapolis – St. Paul neighborhoods of participating families, the percentage of each census tract that is Black/African American and the average BMI percentile of study participants that reside in that census tract. Purple areas represent areas with majority Black/African American residents and higher proportion of children with overweight/obesity. ICE quintiles were computed for five domains of social polarization, and selected results are presented to illustrate the strongest associations between Black homogenous census tracts and child BMI percentile relative to White homogenous census tracts. This conceptualization of ICE characterizes the historical effects of racial residential segregation on child health.30,38 Contrasts at the extreme privilege and deprivation level are the primary effect of interest, and the socio-economic characteristics of Black-homogenous (n=74; least privileged) and White-homogenous (n=73; most privileged) census tracts were compared (Table 3). In the Black-homogenous census tracts, average neighborhood household income (−$70,238) and home values −$137,116 were lower, owner-occupied housing was −37 percentage points (pp) lower, and unemployment was 6pp higher than the White-homogenous census tracts. Poverty rates were 22pp higher in least privileged tracts, single parent households were 32pp more common, no access to a vehicle was 17pp higher, and having a high school education was −20pp lower.
Figure 1.
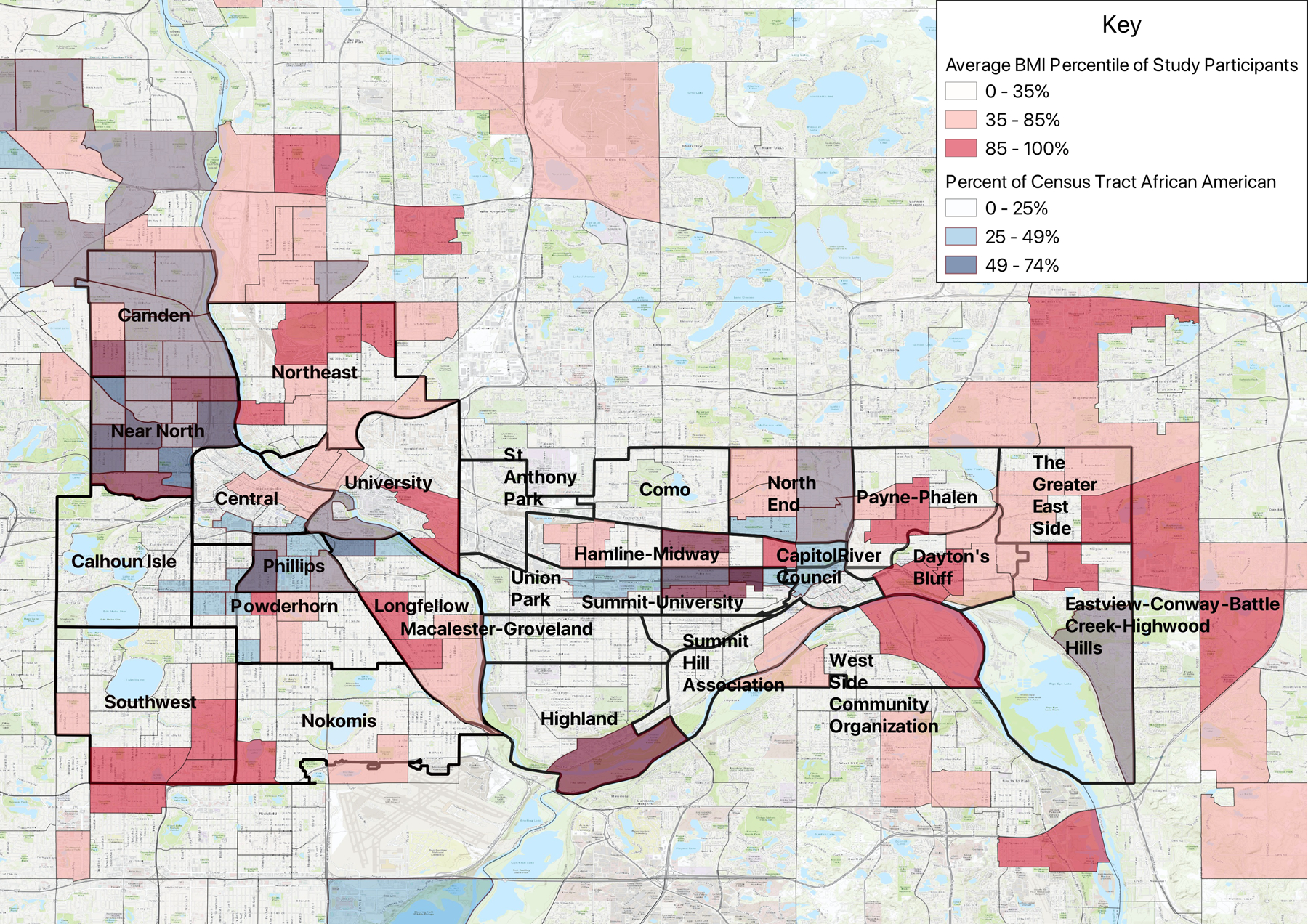
Spatial Distribution of Child BMI Percentile for Black/African American Family Matters Households in Majority-Black/African American Census Tracts
Table 3.
Sociodemographic Census Tract Differences at the Index of Concentration at the Extremes (N=147)
| Contrast 95% CI Black (n=74) vs White Census Tract (n=73) |
|
|---|---|
| Median Family Income | −$70,238 (−$77,468, −$63,008) |
| Median Mortgage | −$539 (−$645, −$434) |
| Median Rent | −$281 (−$379, −$183) |
| Median Home Value | −$137,116 (−$159,579, −$114,653) |
| % Families in Poverty | 22% (19%, 25%) |
| % Owner Occupied Housing | −37% (−43%, −31%) |
| Ratio Income Below 10k to Over 50k | 2.1 (1.8, 2.4) |
| % Living 150% Below Poverty | 35% (31%, 38%) |
| % Single Parent | 32% (28%, 36%) |
| % No Access to Vehicle | 17% (14%, 20%) |
| % White Collar Jobs | −25% (−28%, −21%) |
| % Civil Unemployment | 6% (5%, 7%) |
| % with at Least HS Education | −20% (−22%, −18%) |
| % with Less than 9th Grade Education | 13% (11%, 14%) |
| % of Homes with More than 1 Person/Room | 9% (8%, 10%) |
Interpretation Example: Descriptive characteristics of sample census tracts were computed for the non-Hispanic white homogenous tract quintile (most privileged) compared to the non-Hispanic black tract quintile (least privileged). In the least privileged census tracts, overall household income was lower (−$70,238), home values were lower (−$137,116), owner occupied housing was −37 percentage points (pp) lower, and unemployment was 6pp higher than the privileged census tracts. Poverty rates were 22pp higher in least privileged tracts, single parent households were 32pp more common, no access to a vehicle was 17pp higher, and having a high school education was −20pp lower.
The geospatial relationship between racial and economic polarization (ICE) and child BMI percentile
The structural characteristics of census tracts captured by ICE were examined as predictors of child BMI percentile (Table 4). All characterizations of ICE demonstrated a pattern of increasing child BMI percentile as deprivation increased compared to privileged census groups; however only the Black-homogenous/White-homogenous (abbreviation: BH/WH) and non-Hispanic, Black-homogenous/non-Hispanic, White-homogenous (abbreviation: NH-B/NH-W) had power to statistically detect this non-linear effect at p<0.05. BH/WH-ICE was overall predictive of child BMI percentile (p=0.03) and examination of the pairwise contrasts indicated that the strongest evidence for the effects of racial polarization at the neighborhood level on BMI percentile was at the extremes where privilege is most different (8.2 higher BMI percentile in Black-homogenous tracts compared with White-homogenous; 95% CI: 1.5, 14.9). Results were similar in the NH-B/NH-W ICE measure with respect to overall direction of associations as well as the extreme contrasts. Average child BMI percentile in the privileged BH/WH tracts was 61.7 (95% CI: 56.2, 67.3), and in the privileged NH-B/NH-W tracts it was 62.6 (95% CI: 57.1, 68.1) indicating that children living in these privileged neighborhoods were generally not overweight compared to those in less privileged neighborhoods.
Table 4.
Associations between Index of Concentration at the Extremes (ICE) and Child BMI Percentile
| ICE Independent Predictor of Child BMI Percentile | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ICE Determinant Quintile | White Extreme (5) to Black Extreme (1) | Overall P Value | Non-Hispanic, White Extreme (5) to Non-Hispanic Black Extreme (1) | Overall P Value | High Income Extreme (5) to Low Income Extreme (1) | Overall P Value | White, High Income Extreme (5) to Black, Low Income Extreme (1) | Overall P Value | Non-Hispanic, White, High Income Extreme (5) to Non-Hispanic Black, Low Income Extreme (1) | Overall P Value |
| Quintile 5 (Most Privileged) Predicted Mean BMI%ile: |
61.7 (56.2, 67.3) | 62.6 (57.1, 68.1) | 61.5 (55.9, 67.2) | 62.5 (56.9, 68) | 62.3 (56.8, 67.9) | |||||
|
Quintile Contrasts
(ref: Most Privileged Quintile) |
||||||||||
| Most Different Privilege Contrast (1 vs 5) | 8.2 (1.5, 14.9) | 0.03 | 6.9 (0.2, 13.6) | 0.015 | 6.5 (−0.7, 13.6) | 0.238 | 7.1 (0.2, 14.1) | 0.121 | 7.7 (0.9, 14.4) | 0.072 |
| (2 vs 5) | 6.4 (−0.7, 13.6) | 6.9 (−0.2, 14) | 5.1 (−2.9, 13.1) | 4.4 (−3.2, 11.9) | 4.1 (−3.4, 11.7) | |||||
| (3 vs 5) | 2.2 (−6.1, 10.4) | 1.3 (−7, 9.5) | 4.9 (−3.2, 12.9) | 0.7 (−7.6, 9.1) | 1 (−7.4, 9.5) | |||||
| Most Similar Privilege Contrast (4 vs 5) | −1.7 (−10.2, 6.8) | −4.3 (−12.8, 4.1) | −0.4 (−8.2, 7.4) | −0.8 (−8.8, 7.1) | −0.7 (−8.6, 7.2) | |||||
Models adjusted for 5-year change in census tract median family income between 2010 – 2015
Interpretation Example: Household residency in the sample covered n=367 Minneapolis-St. Paul census tracts allowing for an examination of geographic racial and economic segregation correlated of child BMI%ile. Models were adjusted for American Community Survey (ACS) census tract 5-year, change in median family income. The index of concentration of extremes was computed for five domains of economic and racial tract segregation and operationalized as a categorical variable with quintile category values. Two racial segregation ICE measures of low privilege compared to high privilege were correlated with elevated BMI%ile, which declined as census tracts became more white homogenous (P=0.03) or non-Hispanic, white homogenous (P=0.015). In the white homogenous vs Black homogenous ICE analysis, participant children residing in Black homogenous census tracts had 8.2 units higher BMI%ile (95% CI: 1.5, 14.9) compared to participant children residing in white homogeneous census tracts.
Discussion
Results of this cross-sectional study showed that the experience of any type of discrimination/harassment was associated with a 5.28 unit higher BMI percentile, consistent with our hypothesis. Almost 30% of children in the cohort were reported to have experienced some form of discrimination in the past year. Black and Native American youth were more likely to have encountered discrimination, similar to what has been described in prior studies.39 In follow-up analyses, weight and appearance-based discrimination/harassment were the primary reported types of discrimination associated with child BMI percentile, and even infrequent (e.g., a few times a year) incidences of weight-related discrimination were associated with higher child BMI percentile. Discrimination based on weight had stronger associations with child BMI compared to appearance-related discrimination, suggesting that parents differentiated these two types of experiences from one another. Given the cross-sectional nature of the study, the direction of this association cannot be determined. Discrimination and harassment, like other stressors, may promote weight gain through physiological stress mechanisms or changes in health behavior driven by stress (e.g., decreased physical activity and increased energy consumption or binge eating behavior).40 Additionally, weight stigma is prevalent in society and our findings may reflect that children with higher BMI are more likely to encounter discrimination based on weight and appearance, potentially perpetuating overweight/obesity through the physiological and health behavior mechanisms described above.41 Future studies should examine the intersection of discrimination, weight, and race, and the cumulative impact that multiple forms of discrimination may have on children’s health. Longitudinal studies are needed to better understand the mechanisms through which weight-related discrimination and harassment may be associated with childhood overweight/obesity.
Also consistent with our hypothesis, neighborhood structural factors were strongly associated with child BMI percentile. Even after controlling for known demographic/household contributors, child BMI percentile increased as neighborhood area deprivation increased. Specifically, families residing in neighborhoods that were predominantly Black were much more likely to have children with higher BMI percentiles compared to children residing in White homogeneous neighborhoods. Predominantly Black and Hispanic neighborhoods were also significantly poorer compared to census tracts that were predominantly White, reflecting racism manifested through the longstanding influence of oppressive policies that systematically disadvantage Black, Indigenous People of Color (BIPOC) children and families. These findings are consistent with other studies that have found associations between neighborhood poverty, race, and health outcomes, identifying structural racism as a key factor in the origins of health inequities, including obesity inequities.25,42,43
The current study focused on a racially and ethnically diverse cohort of children in the Twin Cities metro area, where health inequities are prevalent and a major public health concern.44,45 Historical and contemporary policies and legislation have resulted in geographic separation of minoritized groups from Whites, and disproportionate allocation of neighborhood resources and opportunities. Our findings, in the context of previous research, suggest that this history and resulting neighborhood deprivation are associated with children’s health and obesity inequities. The measure of neighborhood environment used in the current study, ICE, measures the extent to which structural racism persists by examining spatial social polarization within neighborhoods that considers race (Black vs. White) and income disparities. Living in deprived neighborhoods was associated with child BMI, such that children residing in neighborhoods with the lowest ICE race and income quintiles had significantly higher BMI percentiles than those residing in the most privileged quintiles. Furthermore, BMI percentiles increased consistently from quintiles with the most to the least privilege. Strengths of our study include the large, racially-ethnically diverse cohort, and the young age range of child participants within which we examined these associations. Unlike prior studies, we also examined both perceived experiences of discrimination as well as neighborhood structural forces that may impact children’s weight, consistent with theoretical frameworks which postulate that racism operates at multiple levels influencing health outcomes.46
Our study also has limitations. The cross-sectional design limits interpretation of the directionality of the associations between children’s BMI, discrimination, and neighborhood structural forces, and the cohort was limited to the Twin Cities metro area in Minnesota, which may limit generalizability of our findings. Additionally, our study examined structural level forces at the neighborhood/census tract level only, did not permit a more detailed approach to examining social polarization by all ethnicities (e.g., Somali), and we did not examine other systems within the life of the child that could influence health and BMI (e.g., school segregation/resources). Finally, we relied on parent-reports of discrimination/harassment of their child and not child self-report which may more accurately represent the child’s personal experience. Across the sample, relatively low levels of reported discrimination in specific domains likely resulted in reduced statistical power for detecting significant correlations with child BMI percentile. Furthermore, other more prevalent forms of discrimination (e.g., microaggressions) may be important sources of stress and impact child health but were not well-captured by our survey.
Conclusions
Racial residential segregation and income inequity were strongly associated with child BMI percentile even after controlling for known demographic/household contributors. Reported discrimination/harassment was also associated with higher child BMI percentiles. Our findings add to the body of literature linking discrimination and structural racism to childhood obesity, and highlight the importance of examining multiple levels of influence of racism-related stressors in regards to child health. Prospective, longitudinal studies are needed to understand whether such structural inequities and perceived discrimination may be related to children’s weight gain trajectories and future health outcomes. Furthermore, the use of a social ecological framework, which acknowledges the multi-level (individual, interpersonal, institutional, systemic), overlapping, and interactive factors that contribute to and maintain racial inequities,47 should be further explored in future studies to better identify avenues through which anti-racism efforts may lead to equitable health outcomes. This information will be important to inform policy and program interventions that can alleviate longstanding societal inequities, promote health equity, and reduce obesity disparities.
Funding/Support:
Research is supported by grant number R01HL126171 and HL156994 from the National Heart, Lung, and Blood Institute (PI: JM Berge) and a grant from the University of Minnesota Clinical Translational Science Institute (PIs: AS Kunin-Batson, MF Troy). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health.
Footnotes
Conflict of Interest: The authors have no conflicts of interest relevant to this article to disclose
References:
- 1.Umer A, Kelley GA, Cottrell LE, Giacobbi P, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. 2017–12-01 2017;17(1)doi: 10.1186/s12889-017-4691-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Isong IA, Rao SR, Bind M-A, Avendaño M, Kawachi I, Richmond TK. Racial and Ethnic Disparities in Early Childhood Obesity. Pediatrics. 2018–01-01 2018;141(1):e20170865. doi: 10.1542/peds.2017-0865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bleich SN, Wolfson JA. Trends in SSBs and snack consumption among children by age, body weight, and race/ethnicity. Obesity. 2015–05-01 2015;23(5):1039–1046. doi: 10.1002/oby.21050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and Race/Ethnicity Are Associated with Adherence to Food-Based Dietary Guidance among US Adults and Children. Journal of the Academy of Nutrition and Dietetics. 2012–05-01 2012;112(5):624–635.e6. doi: 10.1016/j.jand.2011.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dodd AH, Briefel R, Cabili C, Wilson A, Crepinsek MK. Disparities in consumption of sugar-sweetened and other beverages by race/ethnicity and obesity status among United States schoolchildren. Journal of nutrition education and behavior 2013;45(3):240–249. [DOI] [PubMed] [Google Scholar]
- 6.Hardeman RR, Murphy KA, Karbeah JM, Kozhimannil KB. Naming Institutionalized Racism in the Public Health Literature: A Systematic Literature Review. Public Health Reports. 2018–05-01 2018;133(3):240–249. doi: 10.1177/0033354918760574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017/04/08/ 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 8.Gee GC. A Multilevel Analysis of the Relationship Between Institutional and Individual Racial Discrimination and Health Status. American Journal of Public Health. 2002–04-01 2002;92(4):615–623. doi: 10.2105/ajph.92.4.615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. American journal of public health 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: A geography of opportunity perspective for understanding racial/ethnic health disparities. Health & Place. 2010–11-01 2010;16(6):1113–1123. doi: 10.1016/j.healthplace.2010.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Groos M, Wallace M, Hardeman R, Theall KP. Measuring inequity: A systematic review of methods used to quantify structural racism. Journal of Health Disparities Research and Practice 2018. p. 190–206.
- 12.Williams DR. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports. 2001–09-01 2001;116(5):404–416. doi: 10.1093/phr/116.5.404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang VW. Racial residential segregation and weight status among US adults. Social Science & Medicine. 2006/09/01/ 2006;63(5):1289–1303. doi: 10.1016/j.socscimed.2006.03.049 [DOI] [PubMed] [Google Scholar]
- 14.Chang V, Hillier A, Mehta N. Neighborhood Racial Isolation, Disorder and Obesity. Soc Forces 2009. 87(4):2063–2092. doi:doi: 10.1353/sof.0.0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kershaw KN, Pender AE. Racial/Ethnic Residential Segregation, Obesity, and Diabetes Mellitus. Current Diabetes Reports. 2016/09/23 2016;16(11):108. doi: 10.1007/s11892-016-0800-0 [DOI] [PubMed] [Google Scholar]
- 16.Corral I, Landrine H, Hall M, Bess J, Mills K, Efird J. Residential segregation and overweight/obesity among African-American adults: a critical review. Front Public Health 2015;3:169 doi:doi: 10.3389/fpubh.2015.00169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruwanpura KN. Multiple identities, multiple-discrimination: A critical review. Feminist Economics. 2008/07/01 2008;14(3):77–105. doi: 10.1080/13545700802035659 [DOI] [Google Scholar]
- 18.Pearl RL, Wadden TA, Tronieri JS, Chao AM, Alamuddin N, Berkowitz RI. Everyday discrimination in a racially diverse sample of patients with obesity. Clinical obesity 2018;8(2):140–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cozier YC, Yu J, Coogan PF, Bethea TN, Rosenberg L, Palmer JR. Racism, Segregation, and Risk of Obesity in the Black Women’s Health Study. American Journal of Epidemiology 2014;179(7):875–883. doi: 10.1093/aje/kwu004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mwendwa DT, Gholson G, Sims RC, et al. Coping With Perceived Racism: A Significant Factor in the Development of Obesity in African American Women? Journal of the National Medical Association. 2011–07-01 2011;103(7):602–608. doi: 10.1016/s0027-9684(15)30386-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pachter LM, Coll CG. Racism and child health: a review of the literature and future directions. J Dev Behav Pediatr Jun 2009;30(3):255–63. doi: 10.1097/DBP.0b013e3181a7ed5a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social science & medicine 2013;95:115–127. [DOI] [PubMed] [Google Scholar]
- 23.Elsenburg LK, Van Wijk KJE, Liefbroer AC, Smidt N. Accumulation of adverse childhood events and overweight in children: A systematic review and meta-analysis. Obesity. 2017–05-01 2017;25(5):820–832. doi: 10.1002/oby.21797 [DOI] [PubMed] [Google Scholar]
- 24.Goosby BJ, Malone S, Richardson EA, Cheadle JE, Williams DT. Perceived discrimination and markers of cardiovascular risk among low-income African American youth. American Journal of Human Biology. 2015–07-08 2015;27(4):546–552. doi: 10.1002/ajhb.22683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Panza GA, Puhl RM, Taylor BA, Zaleski AL, Livingston J, Pescatello LS. Links between discrimination and cardiovascular health among socially stigmatized groups: A systematic review. PLOS ONE. 2019–06-10 2019;14(6):e0217623. doi: 10.1371/journal.pone.0217623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berge JM, Trofholz A, Tate AD, et al. Examining unanswered questions about the home environment and childhood obesity disparities using an incremental, mixed-methods, longitudinal study design: The Family Matters study. Contemporary Clinical Trials. 2017/11/01/ 2017;62:61–76. doi: 10.1016/j.cct.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berge JM, Tate A, Trofholz A, et al. Momentary Parental Stress and Food-Related Parenting Practices. 10.1542/peds.2017-2295. Pediatrics 2017; [DOI] [PMC free article] [PubMed]
- 28.Body Mass Index BMI (BMI) Percentile Calculator for Child and Teen | DNPAO |. (n.d.). CfDC. https://nccdcdcgov/dnpabmi/Calculatoraspx2021.
- 29.Eisenberg ME, Neumark-Sztainer D, Perry CL. Peer Harassment, School Connectedness, and Academic Achievement. Journal of School Health. 2003-10-01 2003;73(8):311–316. doi: 10.1111/j.1746-1561.2003.tb06588.x [DOI] [PubMed] [Google Scholar]
- 30.Chambers BD, Baer RJ, Mclemore MR, Jelliffe-Pawlowski LL. Using Index of Concentration at the Extremes as Indicators of Structural Racism to Evaluate the Association with Preterm Birth and Infant Mortality—California, 2011–2012. Journal of Urban Health. 2019–04-01 2019;96(2):159–170. doi: 10.1007/s11524-018-0272-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. American journal of public health 2016;106(2):256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.QGIS.org. QGIS Geographic Information System QGIS Association. http://www.qgis.org [Google Scholar]
- 33.Esri. “Minneapolis_Communities” Feature Layer https://services.arcgis.com/afSMGVsC7QlRK1kZ/arcgis/rest/services/Minneapolis_Communities/FeatureServer/0. July 3, 2020.. 2020.
- 34.Esri. “Topographic” [basemap]. “World Topographic Map” http://services.arcgisonline.com/ArcGIS/rest/services/World_Topo_Map/MapServer/tile/%7Bz%7D/%7By%7D/%7Bx%7D&zmax=20&zmin=0.. 2021.
- 35.Census USBot. TIGER/Line: Minnesota Census Tracts 2019. Washington, D.C.: U.S.Bureau of the Census; 2019. [Google Scholar]
- 36.Esri. “St. Paul - District Council - Shapefile - Map.” Feature Layer https://www.stpaul.gov. Link: https://information.stpaul.gov/w/dq4n-yj8b/rg2j-4xhg?cur=IbMJ54tsDsb&from=root.. 2021.
- 37.Stierman B, Afful J, Carroll MD, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes 2021;
- 38.Krieger N, Kim R, Feldman J, Waterman PD. Using the Index of Concentration at the Extremes at multiple geographical levels to monitor health inequities in an era of growing spatial social polarization: Massachusetts, USA (2010–14). International Journal of Epidemiology. 2018–06-01 2018;47(3):788–819. doi: 10.1093/ije/dyy004 [DOI] [PubMed] [Google Scholar]
- 39.Nagata JM, Ganson KT, Sajjad OM, Benabou SE, Bibbins-Domingo K. Prevalence of Perceived Racism and Discrimination Among US Children Aged 10 and 11 Years. JAMA Pediatrics. 2021–08-01 2021;175(8):861. doi: 10.1001/jamapediatrics.2021.1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilson SM, Sato AF. Stress and Paediatric Obesity: What We Know and Where To Go. Stress and Health. 2014–04-01 2014;30(2):91–102. doi: 10.1002/smi.2501 [DOI] [PubMed] [Google Scholar]
- 41.Puhl R, Suh Y. Health Consequences of Weight Stigma: Implications for Obesity Prevention and Treatment. Current Obesity Reports. 2015–06-01 2015;4(2):182–190. doi: 10.1007/s13679-015-0153-z [DOI] [PubMed] [Google Scholar]
- 42.Chae DH, Clouston S, Martz CD, et al. Area racism and birth outcomes among Blacks in the United States. Soc Sci Med Feb 2018;199:49–55. doi: 10.1016/j.socscimed.2017.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Min J, Xue H, Wang Y. Association between household poverty dynamics and childhood overweight risk and health behaviours in the United States: a 8-year nationally representative longitudinal study of 16 800 children. Pediatric Obesity. 2018–10-01 2018;13(10):590–597. doi: 10.1111/ijpo.12292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nanney M, Myers S, Xu M, Kent K, Durfee T, Allen M. The Economic Benefits of Reducing Racial Disparities in Health: The Case of Minnesota. International Journal of Environmental Research and Public Health. 2019–03-01 2019;16(5):742. doi: 10.3390/ijerph16050742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bjur KA, Wi C-I, Ryu E, et al. Socioeconomic Status, Race/Ethnicity, and Health Disparities in Children and Adolescents in a Mixed Rural-Urban Community—Olmsted County, Minnesota. Mayo Clinic Proceedings. 2019–01-01 2019;94(1):44–53. doi: 10.1016/j.mayocp.2018.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jones NL, Breen N, Das R, Farhat T, Palmer R. Cross-Cutting Themes to Advance the Science of Minority Health and Health Disparities. American Journal of Public Health. 2019–01-01 2019;109(S1):S21–S24. doi: 10.2105/ajph.2019.304950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harper Browne C, O’Connor C. Social ecological model of racism & anti-racism. Center for the Study of Social Policy 2021;


