Abstract
Introduction
Stroke survivors spend long periods of time engaging in sedentary behaviour (SB) even when their functional recovery is good. In the RECREATE programme, an intervention aimed at reducing SB (‘Get Set Go’) will be implemented and evaluated in a pragmatic external pilot cluster randomised controlled trial with embedded process and economic evaluations. We report the protocol for the process evaluation which will address the following objectives: (1) describe and clarify causal assumptions about the intervention, and its mechanisms of impact; (2) assess implementation fidelity; (3) explore views, perceptions and acceptability of the intervention to staff, stroke survivors and their carers; (4) establish the contextual factors that influence implementation, intervention mechanisms and outcomes.
Methods and analysis
This pilot trial will be conducted in 15 UK-based National Health Service stroke services. This process evaluation study, underpinned by the Medical Research Council guidance, will be undertaken in six of the randomised services (four intervention, two control). Data collection includes the following: observations of staff training sessions, non-participant observations in inpatient and community settings, semi-structured interviews with staff, patients and carers, and documentary analysis of key intervention components. Additional quantitative implementation data will be collected in all sites. Training observations and documentary analysis data will be summarised, with other observational and interview data analysed using thematic analysis. Relevant theories will be used to interpret the findings, including the theoretical domains framework, normalisation process theory and the theoretical framework of acceptability. Anticipated outputs include the following: recommendations for intervention refinements (both content and implementation); a revised implementation plan and a refined logic model.
Ethics and dissemination
The study was approved by Yorkshire & The Humber - Bradford Leeds Research Ethics Committee (REC reference: 19/YH/0403). Findings will be disseminated via peer review publications, and national and international conference presentations.
Trial registration number
ISRCTN82280581.
Keywords: Stroke, PUBLIC HEALTH, QUALITATIVE RESEARCH, Clinical trials
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The process evaluation is underpinned by the Medical Research Council guidance for process evaluations and addresses all key functions outlined in the guidance including implementation, mechanisms of impact and context.
Theory based, comprehensive process evaluation involving staff, patients and family, friends and carers in intervention and control services.
The process evaluation will be conducted longitudinally, providing information about changes over time.
The in-depth process evaluation will be conducted in a proportion of trial services; however, the implementation team will meet regularly with services not included in the process evaluation to provide an insight into implementation activity. We will also report quantitative implementation data collected across all sites.
Introduction
Sedentary behaviour (SB) is defined as any waking behaviour characterised by low energy expenditure (≤1.5 metabolic equivalents of task) while in a sitting, lying or reclining posture.1 In this study, we use the common approach of interpreting SB as sitting/lying down during waking hours without being otherwise active.2 SB is the focus of considerable clinical, policy and research interest, as the evidence supporting its detrimental effects on health and well-being increases.1 3–6 Higher levels of moderate–vigorous physical activity (MVPA) may reduce risk associated with more daily sedentary time.5 However, achieving recommended levels of MVPA to offset potential harms of high levels of SB (ie, >300 min/week of MVPA) is likely to be challenging,5 particularly for stroke survivors. Evidence suggests this population group is more sedentary and engage in longer unbroken bouts of SB than other population groups7–9 and this appears to be independent of the level of functional recovery10–12 At 6 months after stroke, physical ability only has a small influence on time spent sitting among those living at home.10 Epidemiological studies indicate that stroke survivors are in the highest quartile for cardiovascular risk and increased SB adds to this rising risk.13 Thus, reducing SB has been suggested as a new target for therapeutic intervention after stroke.14
In 2016, an international group of stroke recovery and rehabilitation experts reported that inadequate theoretical intervention development may explain the lack of efficacy of many existing interventions targeting people after stroke.15 The Medical Research Council (MRC) guidelines advocate the importance of using theory and evidence in developing complex interventions.16 It has also been suggested that taking a partnership approach (eg, coproduction) can facilitate the development of feasible and context-sensitive interventions and may increase the likelihood of developing an intervention that is efficacious, due to the active involvement of all relevant stakeholders.17
RECREATE programme
Our National Institute for Health and Care Research (NIHR) funded 7-year research programme (RECREATE) seeks to develop and evaluate strategies for reducing SB after stroke to improve outcomes. The Get Set Go intervention was developed using a structured process, guided by the behaviour change wheel (BCW) which incorporates the theoretical domains framework (TDF)18 in combination with a coproduction approach19 and tested as part of a feasibility study. Get Set Go aims to decrease SB after stroke by increasing the frequency and duration of standing and moving. The intervention is a whole service intervention, designed to be implemented and embedded in routine practice. Delivery commences in the inpatient stroke unit and continues once the stroke survivor is discharged home for at least 12 weeks.
The intervention includes multiple components and focuses on:
Educating staff and stroke survivors (and their family/friends/carers where appropriate) about the importance of standing and moving after stroke;
Preparing and enabling staff to support and encourage stroke survivors to stand and move more in everyday stroke care (as part of routine practice);
Encouraging stroke survivors to monitor their own standing and moving, with assistance from family/friends/ carers where appropriate.
As Get Set Go is delivered at a service level, all clinical staff in services randomised to deliver the intervention will be invited to attend a training session (~1 hour). This will outline the intervention rationale and will provide an overview of key intervention components to prepare staff for delivering Get Set Go. Staff will participate in practical tasks aimed at ensuring they feel confident to support and encourage stroke survivors who are capable of standing independently or with the assistance of one to stand and move more as part of routine stroke care. Staff will be asked to make recommendations for how much standing and moving individuals should be doing based on their usual assessment techniques and clinical judgement. They will be asked to regularly review these recommendations and modify these in line with stroke survivors’ capabilities and circumstances.
Staff will be provided with a range of documents to record this activity. Stroke survivors will be encouraged to form habits around standing and moving as part of their day by recording and monitoring this in an information-based guide. Staff will be encouraged to include families in the intervention so they can undertake a supportive role in encouraging standing and moving in the inpatient setting and when the stroke survivor returns home. A Template for Intervention Description and Replication checklist20 will be published with trial findings.
The RECREATE multicentre cluster randomised controlled trial (cRCT) aimed to evaluate the clinical and cost effectiveness of the Get Set Go intervention. NHS stroke services randomised to the intervention group will be trained to deliver the intervention, while those randomised to the control group will continue usual practice. All patients in the stroke services randomised to the intervention will be exposed to Get Set Go. The trial originally aimed to recruit 1156 stroke survivors in 34 NHS stroke services; however, due to issues associated with the worldwide COVID-19 pandemic, a decision was made in agreement with the funder (NIHR) to reduce the trial in size and scope to become an external pilot trial. Accordingly, the recruitment target was revised to 300–400 participants from 15 NHS stroke services, and the objectives were amended as given a definitive evaluation of effectiveness was no longer be possible (protocol for the external pilot cRCT is reported separately). In view of this, a decision was also made to reduce the number of process evaluation services from 10 to 6. The primary outcome is extended activities of daily living 12 months following recruitment (Nottingham Extended Activities of Daily Living). Secondary outcomes include SB at 12 months, cost-effectiveness, disability, quality of life and reduction of cardiovascular risk factors
Process evaluation
Complex interventions consist of multiple interacting components, and generate changes within complex systems including the interactions between individuals and teams (eg, providers and recipients).21 As Get Set Go includes multiple components and targets the behaviour of health professionals, stroke survivors and their carers/family/friends (hereafter all referred to as carers in this paper) in inpatient and community settings, it is important to understand how the complexities of human behaviour and implementation across these different contexts impact outcomes. Process evaluations are integral to understanding factors which may have contributed to the trial outcomes, and to help understand and evaluate the theoretical assumptions underpinning an intervention.22
The MRC guidance16 22 recommends providing a clear description of the intervention and its causal assumptions, and Moore et al22 state that the interpretation of intervention outcomes should be informed by an investigation of three key functions: (1) implementation, (2) mechanisms of impact and (3) context.22 In our process evaluation, the MRC guidance ensured that we developed a detailed programme theory represented in a logic model and supported with a written description of how the intervention is intended to work. We also aligned our objectives with the three key functions and selected appropriate methods, according to examples provided by Moore et al.13
This paper describes the protocol for the preplanned mixed-methods process evaluation embedded in the RECREATE pilot cRCT.
Aims and objectives
The process evaluation aims to explore and understand the implementation of Get Set Go and how it is experienced and understood by providers and recipients by addressing the following objectives:
Describe and clarify causal assumptions about the intervention, and its mechanisms of impact.
Describe intervention delivery and assess intervention fidelity.
Explore views, perceptions and acceptability of the intervention to staff, stroke survivors and their carers.
Establish the contextual factors that may influence implementation, intervention mechanisms, and outcomes.
Methods and analysis
A mixed-methods process evaluation underpinned by the MRC guidance for process evaluations will be conducted by two researchers (JFJ and RS). JFJ is a senior research fellow leading the process evaluation and RS is a research fellow working on the process evaluation. Both are experienced qualitative researchers, and each has 15 years of experience in conducting a range of qualitative methods analytical approaches. This approach will combine non-participant observations of staff training sessions, non-participant observations in both inpatient and community settings; semi-structured interviews with stroke survivors, carers and staff, and documentary analysis of key intervention documents.
Patient and public involvement
Patients and/or the public are integral to the conduct of the research outlined.
Study setting
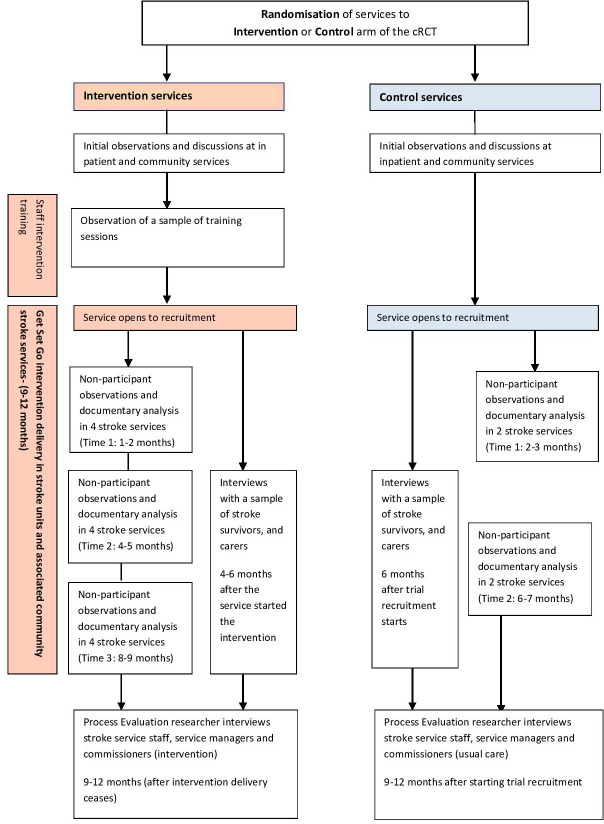
The RECREATE project will be conducted in UK stroke services comprising inpatient and community settings. The process evaluation will be undertaken in six services (four intervention, two control) that will be included in a staggered nature due to the nature of the trial set-up. We will seek to include services that vary according to geographical location and stroke service pathways. For example, some services will include a hyperacute acute and rehabilitation service in one location, whereas others will be across different locations. In terms of community service provision, some will have shorter early supported discharge services whereas others will have services that are not time limited. Data collection will begin in August 2021 and is expected to be completed in July 2023 (figure 1). Data collection activity will be shared by JFJ and RS. Each researcher will undertake activity at three of the six sites each. Where needed to manage the workload, there may be instances where JFJ or RS share activity within their allocated sites.
Figure 1.
Process evaluation flow chart. cRCT, cluster randomised controlled trial.
Theoretical approach
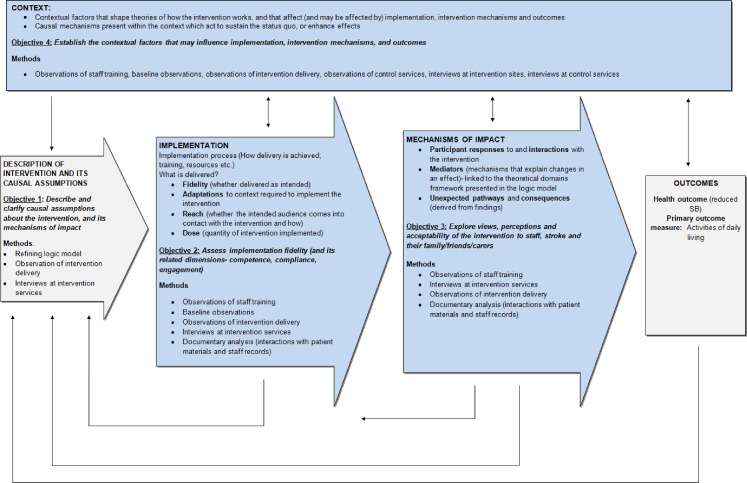
The MRC guidance for process evaluations22 guided this process evaluation to facilitate a comprehensive understanding of factors that influence whether an intervention is effective or ineffective. The guidance also provides flexibility to select relevant theories. Figure 2 shows how objectives and data collection methods fit with the MRC guidance.22
Figure 2.
Process evaluation objectives and methods mapped to the Medical Research Council guidance.22 SB, sedentary behaviour.
The Get Set Go intervention is designed to target the behaviours of staff, patients and carers, and will be implemented in complex settings; therefore, the process evaluation focuses on individual-level behaviour change, and implementation processes. During intervention development, the TDF18 was used while working through the BCW, to identify determinants of behaviour that need to be addressed with the intervention (eg, skills, knowledge and beliefs). Behaviour change techniques were then selected to address behaviours for the different individuals, for example, staff, patients and carers.19 The determinants are presented in the logic model as part of representing the intervention’s intended mechanisms of impact; one of the key functions according to Moore et al.22
To address the other two key functions (implementation and context), an implementation plan was developed based on the findings from the feasibility study. This expands the information in the logic model to outline in detail the processes that staff would ideally engage in to implement the intervention. Normalisation process theory (NPT) was used to formulate the implementation plan, based on four constructs: coherence, cognitive participation, collective action and reflexive monitoring.23
The theoretical framework of acceptability24 is another important framework in this process evaluation as part of addressing objective 3. It comprises seven constructs: affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness and self-efficacy. This framework, along with the TDF and NPT, will all be used to inform the data collection and the interpretation and analysis of findings.
Study participants
Participants (staff, patients and in some cases carers) included in the study will be recruited from intervention and control services. They will be invited to take part in observations and interviews. See table 1 for the eligibility criteria.
Table 1.
Eligibility criteria
| Inclusion criteria | Exclusion criteria | |
| Patient who had a stroke |
|
|
|
|
|
|
||
|
||
|
||
| Carer |
|
|
|
||
|
||
|
||
|
||
| Staff |
|
We aim to recruit staff for interviews across inpatient and community settings; 10 in intervention services (including 2 in a managerial position), and 6 in control services (1 in a managerial position). We aim to recruit five patients in each of the intervention and control services. Patients will be asked if they would like a carer to be present in the interview.
Participants will provide either verbal or written consent (depending on the circumstances) to take part in focused non-participant observations and semi-structured interviews. Participants are free to withdraw at any time without affecting their treatment. Participants will be made aware that if they withdraw, data collected up to that point will be included in analysis unless they request otherwise. Data will be removed on request provided it is still feasible to do so depending on the stage of write up.
Data collection methods
Qualitative data will contribute to understanding intervention mechanisms and their impacts, intervention fidelity, perceptions of the intervention and the extent to which it is acceptable and the contextual factors that may influence implementation, intervention mechanisms and outcomes. Quantitative data (documentary analysis and data relating to implementation) will provide additional insights into intervention fidelity. Table 2 provides an overview of all data to be collected.
Table 2.
An overview of data collection methods for the process evaluation
| Data collection | Setting (COVID-19 adaptation) | Timing | Quantities | Aims (objectives) | Data collection informed by | Analysis method | |
| Observations | Training at intervention services | Inpatient and community (observe via video call) | As training is delivered | Inpatient and community combined: ~1 hour each session, 2–3 sessions per service | Intervention delivery and engagement (objectives 2, 3, 4) | Observational framework listing intervention components and behaviours expected if delivered with fidelity. | Descriptive summaries, using MRC framework |
| Baseline at intervention and control services | Inpatient and community (staff telephone conversations) | Before intervention delivery | Inpatient: ~5 visits (20 hours) including ~3 therapy sessions, per service. Community: ~3 therapy sessions per service |
Understand usual practice at the service, including how staff support standing and moving (objectives 2, 4) | Researcher fieldnotes, informed by Spradley’s descriptive question matrix.25 | Thematic analysis | |
| Time points 1, 2 and 3 at intervention services | Inpatient and community (staff telephone conversations) | 1–2 months, 4–5 months and 8–9 months after starting trial recruitment |
Inpatient: ~8 visits (32 hours) including ~3 therapy sessions, per service. Community: ~3 therapy sessions per service | Fidelity of intervention delivery, and influencing factors (objectives 1, 2, 3, 4) | Observational framework listing behaviours and intervention use expected if delivered with fidelity. Researcher fieldnotes, informed by Spradley’s descriptive question matrix.25 |
Thematic analysis | |
| Time points 1 and 2 at control services | Inpatient and community (staff telephone conversations) | 2–3 months and 6–7 months after starting trial recruitment |
Inpatient: ~5 visits (20 hours) including ~3 therapy sessions, per service. Community: ~3 therapy sessions per service | Understand usual practice at the service, including how staff support standing and moving, and differences/similarities with intervention services (objective 4) | Researcher fieldnotes, informed by Spradley’s descriptive question matrix.25 | Thematic analysis | |
| Documentary analysis intervention services (time points 1, 2 and 3) | Inpatient and community (in patients home if unable to attend wards) | Alongside intervention service observations | Complete documentary analysis form observation time points 1, 2 and 3 | Capture use and delivery (adherence and compliance) of intervention components (eg, stroke patient use of intervention components) (objective 2) | Documentary analysis form informed by fidelity expectations. | Descriptive summaries | |
| Semistructured interviews | Patients who had a stroke (and carers) at intervention services | Patients’ own home (telephone or video call) | ~4–6 months after service started the intervention | Inpatient and community combined: n=5 per service | Explore patient who had a stroke and carer experiences and views of standing and moving after stroke. Explore intervention use, acceptability, impact and barriers/facilitators. (objectives 1, 2, 3, 4) | Topic guide informed by normalisation process theory23 and the intervention acceptability framework.24 | Framework analysis |
| Staff at intervention services | Inpatient and community setting (telephone or video call) | Shortly after service stops using the intervention | Inpatient and community combined: n=10 per service (including two senior) | Explore views on supporting standing and moving after stroke. Explore staff views of the intervention and barriers/ facilitators for embedding and sustaining the intervention (objectives 1, 2, 3, 4) | Topic guide informed by normalisation process theory23 and the intervention acceptability framework.24 | Framework analysis | |
| Patients who had a stroke (and carers) at control services | Community (telephone or video call) | ~6 months after trial recruitment starts | Inpatient and community combined: n=5 per service | Explore patient who had a stroke and carer experiences and views of standing and moving after stroke (objective 4). | Topic guide informed by, normalisation process theory23 and the intervention acceptability framework.24 | Framework analysis | |
| Staff at control services | Inpatient and community (telephone or video call) | ~9–12 months after starting trial recruitment | Inpatient and community combined: n=6 per service (including one senior) | Explore staff views on supporting standing and moving after stroke (objective 4) | Topic guide informed by normalisation process theory23 and the intervention acceptability framework.24 | Framework analysis |
MRC, Medical Research Council.
Qualitative data
Non-participant observations in intervention and control services: general and focused
Training observations will only be conducted in intervention services (table 2). These will focus on the fidelity of training delivery, that is, they will establish whether the training is being delivered by the implementation team as intended. They will also focus on engagement and interactions between the implementers and the staff receiving the training. We have developed an observational framework to assist the researchers in conducting these observations.
In both intervention and control services, baseline observations followed by a series of general and focused observations at different time points (three further time points in intervention services and two in control services) will be conducted (figure 1). General observations will be conducted in ward areas or community settings to gain an overall understanding of care provided and how staff members interact with each other and with patients in these general spaces. Researchers will introduce themselves to staff and patients to explain why they are undertaking the observations. No formal consent will be required for general observations but staff and patients will have the opportunity to object to being observed. For focused observations of 1:1 therapy sessions, researchers will obtain consent from both the staff members and patients who had a stroke engaging in the therapy session. We intend to include patients who had a stroke with aphasia and those who lack capacity in these focused observations where they are willing. Conversations with staff will help to identify whether patients may need the accessible information sheets and consent forms; and there is also an option for consultees to provide consent on behalf of the patient in circumstances where they lack capacity (consultee declaration).
In both intervention and control services, the baseline observations will be conducted to establish a baseline understanding of the organisations and how stroke care is provided. Observations at two further time points at control services will have a similar focus to the initial baseline observations with some additional exploration of staff and patients’ views on standing and moving after stroke. In intervention services, the observations at the three time points after baseline will be undertaken to explore the fidelity of intervention delivery (eg, whether intervention documents were evident in the inpatient and community settings, whether staff are encouraging standing and moving as part of their practice or talking to stroke survivors about Get Set Go) and the factors that influence this, including contextual factors (eg, where intervention materials are stored, how the stroke service is configured, how daily routines are managed), competence of staff delivering the intervention; and the engagement of staff, stroke survivors and carers with the intervention materials (eg, completion of documents)
During general observations, researchers will look for evidence of the intervention being used/adopted in inpatient and community environments. It will be an opportunity to identify changes to daily practice (from baseline) and whether there is evidence that the intervention is integrated into conversations and impacting on behavioural changes during day-to-day care. The focused observations will provide an opportunity to see if there are any specific changes to therapy and whether intervention language is used. For example, instances of staff encouraging stroke survivors to stand and move in the time aside from therapy sessions. In both cases, researchers would expect to see staff using or talking through intervention materials. If there are circumstances where this is not the case it would be an opportunity for the researchers to understand what factors are impacting on implementation in the context of daily practice.
In all cases, the researchers will write detailed notes during their observations and use Spradley’s descriptive question matrix25 as a guide for what to document. Researchers will interact with staff in instances where it feels appropriate to clarify what they have observed. However, they will not seek to get involved in conversations that interfere with the care being provided. Contextual features relevant to the stroke services, including relationships with social care, voluntary or community agencies, will also be considered.
Semi-structured interviews
Semi-structured interviews will be undertaken with a sample of staff, stroke survivors and their carers from the participating services (table 2). Broadly, these interviews will be conducted in addition to the observations to provide further insights into different perceptions of the intervention, its acceptability and the factors that influence whether it can be implemented. Table 1 outlines the inclusion and exclusion criteria for all participants.
Stroke survivor (and carers where appropriate)
A proportion of participants will be invited to take part in a semi-structured interview if they have already consented to the trial and/or completed a ‘consent to contact form’ which indicates they are willing to be approached about participating in an interview. At the time of signing the initial consent for the trial, it will be made clear that not all participants will be contacted regarding an interview and separate consent would be obtained if participants take part in interviews. Their details will be held securely at the Clinical Trials Research Unit and will be provided to the process evaluation researchers via a Secure File Transfer system.
The interviews will take place approximately 4–6 months after commencement of the Get Set Go intervention for each patient who had a stroke, with some flexibility. Sampling for the participants across the services (intervention n=20 across four services, control n=10 across two services) will consider severity of stroke, gender, communication difficulties, occupational status and living arrangements (alone/with a carer). Following initial contact via phone, email or post, interested participants will be provided with an information sheet via post or email. At this point JFJ and RS will check if an accessible information sheet is required.
Once they have had sufficient time to consider whether they would like to take part in an interview, potential participants will have the opportunity to ask any questions and if they are happy, an interview will be arranged. Patients who had a stroke can express if they would like a carer to be present. Interviews will take place in the participants own home or via telephone/video call if appropriate. Consent from patients who had a stroke and where relevant, their carer will be sought prior to interview (process evaluation consent is separate from trial consent). The research teams recruiting the participants for the trial will have already established capacity. JFJ and RS are experienced researchers in this population and will be able to make judgements about capacity if there are any changes in circumstances at the point of the interview. Being able to provide consent is an inclusion criteria for the interviews; however, there is an option for someone to provide consent as a witness in cases where stroke survivors have capacity but are unable to physically consent due to physical impairments post stroke (eg, difficulty writing). Table 2 provides an overview of the focus of these interviews. During interviews, patients who had a stroke will be asked to share intervention materials they received, to facilitate the documentary analysis.
We have also gained ethical approval to approach patients who have not consented to the trial and ask if they would like to take part in an interview. This increases our interviewee pool where needed and provides opportunity for participants to share their experiences of the intervention and the extent to which they think it is acceptable. To facilitate this, the individuals will be approached by a process evaluation researcher and provided with an information sheet and a ‘consent to contact’ form. Their carer (if available) will also be approached for consent to contact. They will subsequently be approached by the researcher to arrange consent and interview. All data will be held at Academic Unit of Ageing and Stroke Research.
Staff
A sample of staff from across the services (intervention n=40 across four services, control n=12 across two services) will be approached face to face at their work-place providing there are no COVID-19 restrictions in place. If COVID-19 restrictions interfere with recruitment, the researcher will liaise with a key member of staff to identify which staff may be interested in taking part in an interview. The aim is to interview a range of staff from across inpatient and community settings in different disciplines and levels of seniority. Following the initial approach, similar procedures to those outlined above for stroke survivors will be undertaken to ensure that staff are provided with an information sheet and given time to consider participation and ask questions. Staff interviews will take place as the intervention ceases at each service (approximately 9 months into intervention delivery). Table 2 outlines the focus of the interviews and how they differ between the intervention and control services. Fully informed consent will be obtained prior to the interview which will take place in a location of staffs’ choosing or via telephone/video call.
Data collection materials
Documents have been created and will be used to facilitate the data collection process during the observations (table 2). These include observational frameworks, topic guides and a documentary analysis form. The researchers will also use the existing descriptive question matrix25 to guide the focus of observations.
Training observation framework
The training observation framework was created to capture fidelity, competence and engagement in relation to training sessions delivered by the implementation team to intervention services. The framework will be used to guide the observations and score them (scale 1–5): whether the content for each slide was delivered as intended (fidelity), how well content was delivered (competence) and how engaged the facilitators and participants were during the session. Researchers will also take notes on environmental factors that might be influential, the extent to which there is staff buy-in to the intervention and any additional reflections or aspects to follow-up.
Fidelity framework (aligned with the logic model)
We have created fidelity frameworks (one for inpatient, one for community settings) to be completed during observations in the inpatient and community setting. These list all intervention components and expected behaviour if the intervention is implemented with fidelity. As with the training framework, it captures competence and engagement. The competencies are aligned with TDF components, included in the logic model.
Implementation framework
In addition to the frameworks, we will collect detailed information about the implementation of the intervention at each of the intervention services included in the process evaluation using the implementation plan described in the Theoretical approach section. We will write notes in each section of the plan and indicate what has been implemented as planned, and any additional unexpected implementation strategies. We will also highlight which constructs of NPT are being addressed and note cases where they are not being addressed as planned. This process will enhance our understandings of the implementation processes needed to successfully implement the intervention.
Topic guides
Topic guides for each of the different interviews (outlined in table 2) were developed based on feasibility study findings, and have also been informed by NPT,23 the theoretical framework of acceptability24 and the TDF.18 In line with NPT, questions focus on how staff make sense of the intervention (coherence); how they work together to build a community of practice which facilitates implementation (cognitive participation); the operational practices involved in enacting the practices (collective action) and the appraisal work to understand ways that the new practices affect those around them (reflexive monitoring). Questions to address acceptability have been included to address the seven constructs within the framework by Sekhon et al.24 Questions focused on the TDF domains in the logic model have also been included to understand more about, for example, skills, knowledge, beliefs around reducing SB from the perspectives of staff, patients and where relevant their families, friends and carers. See online supplemental file 1.
bmjopen-2023-075363supp001.pdf (177.1KB, pdf)
Interviews will be adapted to be inclusive of patients who had a stroke, for instance, by using accessible information sheets, adapting the topic guide/using appropriate images and writing down key words for people with aphasia. Interviews will be audio-recorded and a summary of contextual factors is written by the interviewer.
Quantitative data
Documentary analysis form
A documentary analysis form will be used during observations and interviews, conducted on patient-held intervention components (eg, information guide used to record standing and moving) and staff-completed records. This form will document how many documents have been checked, how many are complete up to date, and the week in which completion stopped (if incomplete). These capture the recording of delivery of intervention components and provide evidence of fidelity.
Data analysis
All data collected will be analysed to address the relevant objectives (table 2). Training observations will be summarised with a focus on fidelity, acceptability and engagement and contextual factors that may have influenced how the training was delivered or received. Relevant headings based on the MRC framework (eg, fidelity, contextual factors) will be used to organise the data.
Both observational and interview data will be subject to thematic analysis.26 Data will be analysed by a minimum of two researchers (JFJ and RS). Observational data will be coded into a thematic framework, and then related codes will be grouped together under thematic headings which convincingly capture and explain the relationship between coded elements of text. The interviews will be transcribed verbatim and anonymised. Data will be entered into NVivo V.12 software (QSR International, 2018). Interview data will separately be analysed using a thematic approach.26 To produce the thematic frameworks, a proportion of the data will be coded independently (JFJ and RS) and key themes and subthemes will be identified to form the frameworks. The same theories used to inform the topic guides (NPT23 and the theoretical framework of acceptability24) will be used to inform the thematic frameworks and themes that are produced during the analysis of the observations and interviews. The logic model, including the domains outlined in the TDF, will also be considered when developing the frameworks and throughout the analysis process.
The training summaries, fidelity frameworks that will be completed during observations, and the implementation plan that will be populated based on meetings with the implementation team, and observational and interview data will be used to support the interpretation of findings and will allow for comparisons to be made between services with regards to implementation fidelity, competency and engagement. Data from documentary analysis will be anonymised and summarised descriptively and will similarly be used to aid the interpretation of findings.
Standard approaches to demonstrating trustworthiness and quality in qualitative research will be used, including the clear documentation of the research process (methods, analysis and any problems encountered and solutions found); transparency of the development of the observational framework and interview topic guides in light of ongoing analysis; documentation of the contextual features in which the research was carried out; discussions of emerging findings among the research team; and researchers will keep a reflexive diary.27
The anticipated outputs of this evaluation include the following: recommendations for intervention refinements (both content and implementation); a revised implementation plan, and a refined logic model (and supporting written intervention description).
Ethical approval and dissemination
The study has National Health Service (NHS) permission and was approved by Yorkshire & The Humber - Bradford Leeds Research Ethics Committee (REC reference: 19/YH/0403). In light of the COVID-19 pandemic, an ethical amendment approved remote data collection where needed, for example, observations of staff training and audio-recorded interviews via zoom. Findings will be disseminated via peer review publications, and national and international conference presentations.
Discussion
Process evaluations are considered an essential part of designing and testing complex interventions.22 They allow us to understand in detail the myriad of complex factors, and complex processes that contribute to whether an intervention has an impact on outcomes. We intend to add to knowledge about: intervention theory and how interventions contribute to change; how interventions interact with their context, wider system dynamics and impacts on implementation; and how individuals experience interventions (patients, staff and carers). We also anticipate that the findings will be informative and transferable to other similar research focused on evaluating complex interventions in complex settings.
Supplementary Material
Acknowledgments
We would like to acknowledge the expert support of the RECREATE Programme Management Group who meet regularly.
Footnotes
Twitter: @mainemoreau, @MeadGillian, @Coralie_English
Collaborators: RECREATE Programme Management Group: Jennifer Airlie, Karen Birch, Gillian Carter, Bethan Copsey, Florence Day, Coralie English, Amanda Farrin, Claire Fitzsimons, Anne Forster, Jessica Faye Johansson, Rebecca Lawton, Laura Marsden, Gillian Mead, Lauren Moreau, Seline Ozer, Anita Patel, Rosie Shannon and Nahel Yaziji.
Contributors: AFo is lead grant holder and chief investigator, and will oversee the design and implementation of the trial. JFJ leads the embedded process evaluation and is responsible for planning, undertaking the research and reporting findings alongside RS. SO and LAM, assisted by JA, are responsible for managing the delivery of the trial. JA also leads on the ActivPAL and is responsible for the implementation of the intervention alongside SO and AFo. RM contributed to the planning of this process evaluation. AFa, GM, CE, CFF and DJC are coinvestigators who were all involved in the design of the trial and process evaluation, and attend regular programme meetings where advice is provided where needed. All coinvestigators and researchers contributed to the development of the protocol. JFJ drafted the manuscript which is written on behalf of the RECREATE Programme Management Group. All authors read and approved the final manuscript.
Funding: This work was supported by the National Institute for Health and Care Research (NIHR) under its Programme Grants for Applied Research Programme (grant number RP-PG-0615-20019). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Data collection, management, analysis and interpretation will remain independent of the Funder. The trial sponsor is Bradford Teaching Hospitals NHS Foundation Trust, Research Management & Support Office, Bradford Institute for Health Research, Bradford, BD9 6RJ, UK.
Competing interests: AFo, AFa, CE, CFF, GM and DJC are coinvestigators on the grant funding this work therefore are partially supported by the National Institute for Health and Social Care Research (NIHR) (grant number RP-PG-0615-20019). AFo has received additional research grant support from NIHR through the following funding streams: senior Investigator award, Health Technology Assessment (HTA) and Health and Social Care Delivery Research (HS&DR). AFo has previously received support from the Stroke Association to attend the UK stroke forum and received payment from the National Institute for Health (USA) for panel membership (2021, 2022). AFo is currently the chair/a member of programme steering committees for NIHR research programmes (grant reference numbers: NIHR 202339, NIHR 202020) and has served on the following panels: NIHR Doctoral Fellowships, NIHR senior investigators committee (2019/20), NIHR HS&DR committee (2016–2018) and Stroke Association Funding. CE has received grant funding from the Netherlands Organisation for Scientific Research (NOW) Taskforce for Applied Research (SIA RAAK) for work in a similar area (ie, sitting less and moving more after stroke) and is a non-executive director representing interests of Research and Chair of Research Advisory Committee for the Stroke Foundation of Australia (unpaid). CFF is a coinvestigator/collaborator on other grants on the topic of sedentary behaviour/physical activity and is therefore partially supported by grant funding received from the University of Edinburgh and the Irish Health Board. CE has previously been supported to conduct work in a similar area by grant funding received from the Chief Scientist Office of the Scottish Government, Medical Research Council Public Health Intervention Development award and the University of Edinburgh. JFJ, LAM, RS, RM, JA, SO and DJC report no competing interests related to the manuscript.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Collaborators: RECREATE Programme Management Group, Jennifer Airlie, Karen Birch, Gillian Carter, Bethan Copsey, Florence Day, Coralie English, Amanda Farrin, Claire Fitzsimons, Anne Forster, Jessica Faye Johansson, Rebecca Lawton, Laura Marsden, Gillian Mead, Lauren Moreau, Seline Ozer, Anita Patel, Rosie Shannon, and Nahel Yaziji
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary behavior research network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys Act 2017;14:75. 10.1186/s12966-017-0525-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owen N, Sugiyama T, Eakin EE, et al. Adults' sedentary behavior: determinants and interventions. Am J Prev Med 2011;41:189–96. 10.1016/j.amepre.2011.05.013 [DOI] [PubMed] [Google Scholar]
- 3.Rezende LFM de, Rodrigues Lopes M, Rey-López JP, et al. Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS ONE 2014;9:e105620. 10.1371/journal.pone.0105620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tremblay MS, Colley RC, Saunders TJ, et al. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab 2010;35:725–40. 10.1139/H10-079 [DOI] [PubMed] [Google Scholar]
- 5.Dempsey PC, Biddle SJH, Buman MP, et al. New global guidelines on sedentary behaviour and health for adults: broadening the behavioural targets. Int J Behav Nutr Phys Act 2020;17:151. 10.1186/s12966-020-01044-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health UDo, Services H . Physical activity guidelines advisory committee. 2018 physical activity guidelines advisory committee scientific report. Published online; 2018.
- 7.Butler EN, Evenson KR. Prevalence of physical activity and sedentary behavior among stroke survivors in the United States. Top Stroke Rehabil 2014;21:246–55. 10.1310/tsr2103-246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.English C, Healy GN, Coates A, et al. Sitting and activity time in people with stroke. Phys Ther 2016;96:193–201. 10.2522/ptj.20140522 [DOI] [PubMed] [Google Scholar]
- 9.Paul L, Brewster S, Wyke S, et al. Physical activity profiles and sedentary behaviour in people following stroke: a cross-sectional study. Disabil Rehabil 2016;38:362–7. 10.3109/09638288.2015.1041615 [DOI] [PubMed] [Google Scholar]
- 10.English C, Healy GN, Coates A, et al. Sitting time and physical activity after stroke: physical ability is only part of the story. Top Stroke Rehabil 2016;23:36–42. 10.1179/1945511915Y.0000000009 [DOI] [PubMed] [Google Scholar]
- 11.English C, Manns PJ, Tucak C, et al. Physical activity and sedentary behaviors in people with stroke living in the community: a systematic review. Phys Ther 2014;94:185–96. 10.2522/ptj.20130175 [DOI] [PubMed] [Google Scholar]
- 12.Tieges Z, Mead G, Allerhand M, et al. Sedentary behavior in the first year after stroke: a longitudinal cohort study with objective measures. Arch Phys Med Rehabil 2015;96:15–23. 10.1016/j.apmr.2014.08.015 [DOI] [PubMed] [Google Scholar]
- 13.Wullems JA, Verschueren SMP, Degens H, et al. A review of the assessment and prevalence of sedentarism in older adults, its physiology/health impact and non-exercise mobility counter-measures. Biogerontology 2016;17:547–65. 10.1007/s10522-016-9640-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morton S, Fitzsimons C, Hall J, et al. Sedentary behavior after stroke: a new target for therapeutic intervention. Int J Stroke 2019;14:9–11. 10.1177/1747493018784505 [DOI] [PubMed] [Google Scholar]
- 15.Walker MF, Hoffmann TC, Brady MC, et al. Improving the development, monitoring and reporting of stroke rehabilitation research: consensus-based core recommendations from the stroke recovery and rehabilitation Roundtable. Int J Stroke 2017;12:472–9. 10.1177/1747493017711815 [DOI] [PubMed] [Google Scholar]
- 16.Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374:n2061. 10.1136/bmj.n2061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Voorberg WH, Bekkers V, Tummers LG. A systematic review of co-creation and co-production: embarking on the social innovation journey. Public Manag Rev 2015;17:1333–57. 10.1080/14719037.2014.930505 [DOI] [Google Scholar]
- 18.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7:37. 10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall J, Morton S, Hall J, et al. A co-production approach guided by the behaviour change wheel to develop an intervention for reducing sedentary behaviour after stroke. Pilot Feasibility Stud 2020;6:115. 10.1186/s40814-020-00667-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 21.Moore GF, Evans RE, Hawkins J, et al. From complex social interventions to interventions in complex social systems: future directions and unresolved questions for intervention development and evaluation. Evaluation (Lond) 2019;25:23–45. 10.1177/1356389018803219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350:h1258. 10.1136/bmj.h1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.May C, Finch T, Rapley T. Normalization process theory. In: Handbook on implementation science. Edward Elgar Publishing, 2020. 10.4337/9781788975995 [DOI] [Google Scholar]
- 24.Sekhon M, Cartwright M, Francis JJ. Acceptability of Healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17:88.:88. 10.1186/s12913-017-2031-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spradley JP. Participant observation. Waveland Press, 2016. [Google Scholar]
- 26.Teo T. Thematic analysis: encyclopedia of critical psychology. New York, NY: Springer, 2014: 1947–52. 10.1007/978-1-4614-5583-7 [DOI] [Google Scholar]
- 27.Ritchie J, Lewis J, Nicholls CM, et al. Qualitative research practice: a guide for social science students and researchers. Sage, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-075363supp001.pdf (177.1KB, pdf)