Abstract
We prospectively studied 156 patients with a diagnosis of community-acquired pneumonia requiring admission. Several respiratory specimens were obtained for the detection of Chlamydia pneumoniae by cell culture and PCR. Three serum samples were obtained from each patient. Serological diagnosis of a C. pneumoniae infection was determined by the microimmunofluorescence (MIF) test, the complement fixation (CF) test, and recombinant lipopolysaccharide (LPS) enzyme-linked immunosorbent assay (ELISA; referred to as the rDNA LPS ELISA). Twenty-three patients (15%) had serological results compatible with acute C. pneumoniae infection; nine (39%) of these subjects were C. pneumoniae PCR positive. Twenty-two patients (14%) had positive PCR results without serological evidence of an acute C. pneumoniae infection. An attempt was made to calculate the sensitivities and specificities of the MIF test, rDNA LPS ELISA, and PCR for the diagnosis of chlamydial community-acquired pneumonia. Several “gold standards” were defined. Generally, the sensitivities of the rDNA LPS ELISA and MIF were comparable, while the sensitivity of the CF test was shown to be very low. Independent of the gold standard used, the best PCR results were obtained with nasopharyngeal specimens. However, the predictive value of a positive C. pneumoniae PCR result for patients with community-acquired pneumonia remains unknown and may be low. Although a widely accepted gold standard is still lacking, the rDNA LPS ELISA may currently be the preferred tool for diagnosing acute respiratory Chlamydia infections in routine clinical practice. However, the MIF test remains the method of choice for determining the prevalence of C. pneumoniae infections in a given community.
Most respiratory infections caused by Chlamydia pneumoniae are mild or asymptomatic (1, 9, 26, 42). Similar to Mycoplasma infections, C. pneumoniae can cause recurrent or secondary lower respiratory tract infections, even though antibody due to previous infection are detectable in serum (1). Infection with C. pneumoniae occurs worldwide, resulting in a 40 to 90% prevalence of serum antibody to the species (3, 18, 34, 48). C. pneumoniae has been associated with both epidemic and endemic occurrences of acute respiratory disease and is believed to be responsible for 6 to 20% of all community-acquired pneumonias (CAPs) (1, 13, 21, 28, 38, 41). Diagnosis of C. pneumoniae infection is preferably based on the isolation of the organism from respiratory specimens, PCR, and/or serology (20, 51). However, isolation of C. pneumoniae by cell culture remains difficult and its sensitivity is unknown. Subsequently, culture tests are not available in routine laboratories. Also, PCR requires specially trained, experienced personnel and is not yet commercially available. Therefore, serology is currently the tool most often applied for the routine diagnosis of acute C. pneumoniae infection. The commercially available serological tests include the complement fixation (CF) test, the microimmunofluorescence (MIF) test, and the enzyme-linked immunosorbent assay (ELISA). The CF test has traditionally been used to diagnose chlamydial respiratory infections (32, 39). This assay uses an enriched lipopolysaccharide (LPS) antigen derived from Chlamydia psittaci for the detection of Chlamydia genus-specific antibodies. CF assays are technically demanding, and no information is obtained about the immunoglobulin classes involved in the reaction. The “gold standard” in C. pneumoniae serology at this moment is the MIF test (12, 30, 40). Chlamydia elementary bodies, which are the infective cell forms of Chlamydia, are used as antigen in the MIF test. This test is supposed to be species specific and can differentiate between immunoglobulin G (IgG), IgM, and IgA antibodies (39, 44).
We evaluated a commercially available recombinant LPS ELISA (rDNA LPS ELISA), the MIF test, PCR, and culture for the diagnosis of CAP caused by C. pneumoniae. In addition, we sought to evaluate the usefulness of the rDNA LPS assay to determine the seroprevalence of C. pneumoniae.
MATERIALS AND METHODS
Patients.
The study population included four different groups of patients. The first group consisted of 1,104 blood donors visiting the Red Cross Blood Transfusion Center, Tilburg, The Netherlands. One serum sample from each blood donor was stored at −80°C prior to use in this study. The donors’ ages ranged from 18 to 68 years, with a median of 40 years. The second group consisted of 271 patients with chronic obstructive pulmonary diseases (COPDs) attending the outpatient clinic of pulmonary diseases from the St. Antonius Hospital, Nieuwegein, The Netherlands. The patients’ ages ranged from 43 to 88 years, with a median of 67 years. The third group consisted of 156 prospectively studied patients who were consecutively admitted to the same St. Antonius Hospital with CAP. The diagnosis was based on clinical signs and symptoms and new or progressive radiographic changes consistent with pneumonia (10). The patients’ ages ranged from 20 to 93 years, with a median of 68 years. The fourth group consisted of 40 other patients with a recent Mycoplasma pneumoniae infection, as indicated by rising CF antibody titers or by a positive IgM immunofluorescence reaction (serum samples kindly provided in part by R. J. A. Diepersloot, Diakonessen Hospital, Utrecht, The Netherlands).
Clinical specimens.
Serum samples were collected by standard procedures and were stored at −80°C prior to processing. From each patient with CAP, nasopharyngeal and throat specimens were collected with sterile cotton-tipped aluminum-shafted swabs and were suspended in 1.5 ml of Chlamydia transport medium (0.2 M sucrose phosphate [2SP]). A throat wash sample was obtained with 10 ml of phosphate-buffered saline. Sputum samples were collected by standard procedures. The first serum sample was obtained within the first 24 h of enrollment. A second (convalescent-phase) serum sample was obtained from all patients 10 days after enrollment. A third serum sample was obtained from 142 patients (91%) after 30 days.
Laboratory assays for C. pneumoniae. (i) Culture.
Culture for C. pneumoniae was done as described previously (44). Briefly, Buffalo Green Monkey (BGM) cells (St. Joseph Hospital, PAMM, Veldhoven, The Netherlands) (45) were seeded into 24-well tissue culture plates (Costar Europe Ltd.), and the plates were incubated at 35°C with 5% CO2 in a fully humidified cabinet. All cell monolayers were examined on the day of inoculation for confluent growth. For each experiment, a patient’s sample was inoculated into two wells of a 24-well cell culture plate and one flat-bottom tube. After inoculation, the cell culture plates were centrifuged at 900 × g and 25°C for 60 min and were subsequently incubated with fresh medium containing cycloheximide (0.6 mg/liter; Sigma Chemical Company, St. Louis, Mo.). After 3 days, the 24-well plates were aspirated and fixed with methanol (Merck, Darmstadt, Germany). The fixed monolayers were rinsed once with phosphate-buffered saline and stained by the fluorescent-antibody technique with Chlamydia genus-specific mouse monoclonal antibody (kindly provided by J. M. Ossewaarde, National Institute of Public Health and Environmental Protection, Bilthoven, The Netherlands). The contents of the inoculated flat-bottom tubes were passed onto fresh monolayers and were reincubated as described above. This procedure was repeated once more. In each culture series, C. pneumoniae TW-183 was included in parallel as a positive control. Positive cultures were stained with C. pneumoniae-specific mouse monoclonal antibodies (Washington Research Foundation, Seattle, Wash.). Rabbit anti-mouse immunoglobulin labeled with fluorescein isothiocyanate (Dako A/S, Glostrup, Denmark) was used as a conjugate. Evans Blue (0.05%; Sigma Chemical Company) was used as a counterstain.
(ii) PCR.
Two hundred microliters of a nasopharyngeal or a throat swab specimen or 1.0 ml of a throat wash specimen and bronchoalveolar lavage fluid were transferred to a sterile tube and centrifuged at 15,000 × g for 30 min. Sputum samples were suspended in 1.5 ml of 2SP transport medium. One hundred microliters of the suspended sputum sample was transferred to a sterile tube, and the tube was centrifuged at 15,000 × g for 30 min. The sediment was incubated with a solid carrier (Celite) and a guanidinium thiocyanate-containing lysis buffer. Nucleic acids (NA) were bound to the carrier, which was rapidly sedimented by centrifugation. The sedimented complexes were washed once with a guanidinium thiocyanate-containing washing buffer, once with 70% ethanol, and once with acetone. Complexes were dried and the NA were subsequently eluted in 55 μl of aqueous solution at 37°C for 30 min. The isolated NA were removed from the solid carrier by centrifugation (5). Amplification by PCR and analysis of the amplified products were performed as described by Campbell et al. (8). Briefly, PCR amplification was performed with 8 μl of isolated DNA in a 100-μl reaction mixture containing 20 mM (NH4)2SO4, 75 mM Tris-HCl (pH 9.0), 0.01% Tween 20, 0.2 mM deoxynucleoside triphosphates, 50 pmol of primers, and 0.2 U of Thermoperfect Taq polymerase (Integra Biosciences A. G., Wallisellen, Switzerland). A C. pneumoniae species-specific primer set was used; this primer set amplifies a 437-bp fragment and consists of the following primers: forward primer HL-1 (5′-GTTGTTCATGAAGGCCTACT-3′) and reverse primer HR-1 (5′-TGCATAACCTACGGTGTGTT-3′). The PCR products (20 μl) were analyzed by electrophoresis on a 1.5% agarose gel stained with ethidium bromide. Electrophoretic transfer transferred DNA from agarose to Hybond plus nylon filters (Amersham International plc, Amersham, United Kingdom). The PCR products were analyzed with a C. pneumoniae-specific probe, probe HM-1 (5′-GTGTCATTCGCCAAGGTTAA-3′). The ECL 3′ oligolabeling and detection system (Amersham International, plc) was used for the detection of the PCR products. A 10-fold serial dilution of a C. pneumoniae stock solution (109 target DNA copies per ml) was incorporated into each amplification. One negative control (pooled cervical specimens suspended in 2SP) was incorporated every 10 amplifications. All PCR-positive results were confirmed by repeat DNA isolation and amplification of the original specimen. Separate rooms were used for the different steps of the PCR, and the recommendations of Kwok and Higuchi (33) were used to prevent DNA carryover contamination.
(iii) MIF assay.
The MIF assay described before (44) was used to measure C. pneumoniae-specific IgG, IgM, and IgA antibodies. Briefly, purified C. pneumoniae elementary antibodies (strain AR 39; Washington Research Foundation) were used to detect IgG, IgM, and IgA antibodies to C. pneumoniae. Prior to the IgM determinations, IgG absorption was performed (44). The prevalence of C. pneumoniae-specific IgG, IgM, and IgA antibodies was based on the presence of IgG at titers of ≥1:32, IgM at titers of ≥1:16, and IgA at titers of ≥1:32, respectively. Diagnosis of an acute C. pneumoniae infection was based on the following criteria: the presence of C. pneumoniae-specific IgM in either acute- or convalescent-phase serum or a fourfold or greater increase in the C. pneumoniae-specific IgG and/or IgA antibody titer between the acute- and convalescent-phase serum samples (44).
(iv) CF test.
The CF test was used to measure Chlamydia genus-specific antibodies with C. psittaci antigen (Virion International Distribution Ltd., Chan, Switzerland). A fourfold or greater increase in titer was considered definitive etiologic evidence of infection.
(v) ELISA.
Chlamydia-specific IgG, IgM, and IgA antibodies were detected by an rDNA LPS ELISA (Medac GmbH, Hamburg, Germany). This ELISA includes a chemically pure structure of a recombinant LPS which contains a genus-specific epitope of the Chlamydia spp. pathogenic for humans (6, 7, 25). Initial serum dilutions for the detection of IgG, IgM, and IgA were 1:100, 1:50, and 1:50, respectively. Prior to the IgM determinations, IgG absorption was performed (44). Sera with optical density values exceeding 2.5 were retested with a 1:4 predilution. A twofold serially diluted standard serum sample was used to calculate the log2 titer of the patients’ samples. The IgG, IgM, and IgA cutoff values were calculated as prescribed by the manufacturer. The prevalence of Chlamydia IgG, IgM, and IgA antibodies was based on the following criteria: greater than or equal to the calculated cutoff × 1.10, greater than or equal to the calculated cutoff × 1.15, and greater than or equal to the calculated cutoff × 1.10, respectively. Serological diagnosis of an acute Chlamydia infection was based on the ELISA results by using the following criteria: a threefold or greater increase in Chlamydia-specific IgG or IgA antibody titer, a twofold or greater change in the specific IgM titer, or a twofold increase in the specific IgG antibody titer in combination with a twofold increase in the specific IgA antibody titer (47).
RESULTS
Seroprevalence.
The prevalences of Chlamydia-specific IgG antibodies in the healthy blood donor group and the COPD patient group were 29.4 and 53.1%, respectively, as determined by the rDNA LPS ELISA (P < 0.0001) (Table 1). Significantly higher seroprevalences were observed if the C. pneumoniae MIF assay was used (Table 1). The seroprevalence by the MIF assay was the same for healthy blood donors and COPD patients (71 and 72%, respectively). By using the MIF assay as the gold standard, the sensitivity and specificity of the rDNA LPS ELISA for determination of serological evidence of a C. pneumoniae infection in the past thus depended on the population tested (Table 1). For the healthy blood donor group the sensitivity and specificity were 33.5 and 80.5%, respectively, while for the patients with COPD, the sensitivity and specificity were 64.1 and 75.0%, respectively. A similar trend was observed when calculating the negative predictive value (NPV) and the positive predictive value (PPV) (Table 1).
TABLE 1.
Prevalence of chlamydia-reactive antibody determined by MIF assay and rDNA LPS ELISA
| Study population | No. of subjects | Prevalence (%) observed by the following:
|
rDNA LPS ELISAa
|
||||
|---|---|---|---|---|---|---|---|
| MIF assay | rDNA LPS ELISA | Sensitivity (%) | Specificity (%) | NPV (%) | PPV (%) | ||
| Blood donors | 1,104 | 71.2 | 29.4 | 33.5 | 80.5 | 32.9 | 80.9 |
| COPD patients | 271 | 72.0 | 53.1b | 64.1 | 75.0 | 44.9 | 86.8 |
The MIF assay was used as the gold standard.
P < 0.0001 compared to blood donors.
Acute C. pneumoniae infections.
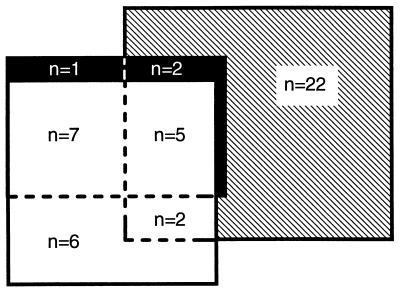
It was possible to make a diagnosis of C. pneumoniae CAP for 45 patients (29%). Twenty-three patients (15%) had serological results (MIF assay and/or rDNA LPS ELISA) indicating acute C. pneumoniae infection (seroresponders). Nine of these subjects (39%) were C. pneumoniae PCR positive. In addition, 22 (14%) patients had positive PCR results without serological evidence of acute C. pneumoniae infection (serononresponders). In 14 of 15 (93%) patients with MIF assay results indicative of acute C. pneumoniae infection, the diagnosis was supported by the rDNA LPS ELISA and/or the PCR test results. Six patients had serological results indicative of an acute infection only by the rDNA LPS ELISA (Fig. 1). Only one patient had positive C. pneumoniae culture results which were confirmed by PCR, MIF assay, and ELISA (data not shown in Fig. 1). Of those that responded serologically, only two patients had CF test results indicative of an acute chlamydial infection.
FIG. 1.
Schematic presentation of partially overlapping positive diagnostic test results for acute C. pneumoniae respiratory infection in 156 patients with CAP. ■, MIF assay positive (n = 15); □, rDNA LPS ELISA positive (n = 20); ▧, PCR positive (n = 31).
For 14 of 23 (61%) seroresponders, C. pneumoniae infection was associated with other etiologies. In six patients, Streptococcus pneumoniae infection was also diagnosed. Other frequent concomitant microorganisms were Haemophilus influenzae, M. pneumoniae, and Legionella pneumophila. Although coinfection was observed among serononresponders as well, associations with other agents were found significantly more often in seroresponders than in serononresponders (61 and 23%, respectively; P = 0.017).
No clear difference in the clinical presentation was observed between the six seroresponders with serological results indicative of an acute infection only by rDNA LPS ELISA and the other seroresponders. In addition, similar observations were found when the clinical presentations of the seroresponders and serononresponders were compared, although the severity of the disease tended to be higher among seroresponders (data not shown).
Different approaches were used to calculate the sensitivities and specificities of the MIF assay, the rDNA LPS ELISA, and PCR. When the MIF was used as the gold standard for the diagnosis of an acute C. pneumoniae infection, the sensitivity and specificity of the rDNA LPS ELISA were 80.0 and 94.3%, respectively, while the sensitivity and the specificity of the PCR were 46.7 and 83.0%, respectively (Table 2). A second gold standard was incorporated to define more liberally the true-positive patient population. A patient had true-positive results if the MIF assay results were indicative of an acute C. pneumoniae infection or one or more respiratory specimens were PCR positive. By using this expanded gold standard, the sensitivities of the MIF assay and rDNA LPS ELISA were comparable (38.5 and 35.9%, respectively). Increased sensitivity was now observed for the PCR (79.5%), but in this case all respiratory specimens had to be processed (Table 2). Two additional expanded gold standards, one more stringent and the other more liberal but both serology based, were incorporated into the evaluation to determine the impacts of the various gold standards (Table 2). Clearly, the sensitivity of the PCR assay was substandard in the latter evaluation. The PPV became clinically irrelevant.
TABLE 2.
Sensitivity, specificity, NPV, and PPV of the rDNA LPS ELISA, MIF assay, and PCR for determination of acute C. pneumoniae infections in patients with CAP requiring admission
| Gold standard | No. (%) of patients positive | Test evaluated | Sensitivity (%) | Specificity (%) | NPV (%) | PPV (%) |
|---|---|---|---|---|---|---|
| MIF assay | 15 (9.6) | ELISA | 80.0 | 94.3 | 97.8 | 60.0 |
| PCR | 46.7 | 83.0 | 93.6 | 22.6 | ||
| Expanded gold standard 1a | 39 (25.0) | MIF | 38.5 | 100.0 | 83.0 | 100.0 |
| ELISA | 35.9 | 94.9 | 81.6 | 70.0 | ||
| PCR | 79.5 | 100.0 | 93.6 | 100.0 | ||
| Expanded gold standard 2b | 12 (7.7) | MIF | 100.0 | 97.9 | 100.0 | 80.0 |
| ELISA | 100.0 | 94.4 | 100.0 | 60.0 | ||
| PCR | 41.7 | 81.9 | 94.4 | 16.1 | ||
| Expanded gold standard 3c | 23 (14.7) | MIF | 65.2 | 100.0 | 94.3 | 100.0 |
| ELISA | 87.0 | 100.0 | 97.8 | 100.0 | ||
| PCR | 39.1 | 83.5 | 88.8 | 29.0 |
PCR and culture positive and/or MIF assay results indicating acute C. pneumoniae infection.
MIF assay and rDNA LPS ELISA results indicating acute C. pneumoniae infection.
MIF assay and/or rDNA LPS ELISA results indicating acute C. pneumoniae infection.
Similar calculations were made to determine the impact of specimen type on the sensitivity, specificity, NPV, and PPV of the PCR (Table 3). Independent of the four different gold standards used, the highest PCR sensitivity and specificity could be obtained with nasopharyngeal specimens (Table 3). Surprisingly, all sputum samples tested remained negative (data not presented in Table 3).
TABLE 3.
Effect of specimen type on the performance of PCR for determination of acute C. pneumoniae infections in 156 patients with CAP requiring admission
| Gold standard | No. (%) of patients positive | Specimen evaluated | Sensitivity (%) | Specificity (%) | NPV (%) | PPV (%) |
|---|---|---|---|---|---|---|
| MIF assay | 15 (9.6) | Throat | 20.0 | 89.9 | 91.2 | 17.6 |
| Throat wash | 6.7 | 95.6 | 90.3 | 14.3 | ||
| Nasopharynx | 40.0 | 89.9 | 93.3 | 30.0 | ||
| Expanded gold standard 1a | 39 (25.0) | Throat | 43.6 | 100.0 | 83.9 | 100.0 |
| Throat wash | 17.9 | 100.0 | 77.9 | 100.0 | ||
| Nasopharynx | 51.3 | 100.0 | 85.8 | 100.0 | ||
| Expanded gold standard 2b | 12 (7.7) | Throat | 16.7 | 89.4 | 92.7 | 11.8 |
| Throat wash | 8.3 | 95.7 | 92.4 | 14.3 | ||
| Nasopharynx | 33.3 | 88.7 | 94.0 | 20.0 | ||
| Expanded gold standard 3c | 23 (14.7) | Throat | 17.4 | 90.0 | 86.1 | 23.5 |
| Throat wash | 8.7 | 96.1 | 85.5 | 28.6 | ||
| Nasopharynx | 36.4 | 90.9 | 89.6 | 40.0 |
PCR and culture positive and/or MIF assay results indicating acute C. pneumoniae infection.
MIF assay and rDNA LPS ELISA results indicating acute C. pneumoniae infection.
MIF assay and/or rDNA LPS ELISA results indicating acute C. pneumoniae infection.
The serological results for the first two serum samples were used to determine the clinical value of a third serum sample obtained after 30 days. The infections in only 67 and 75% of the patients with serological results indicative of an acute infection were diagnosed by the MIF assay and the rDNA LPS ELISA, respectively, if only the first and second serum samples were used for testing.
Since M. pneumoniae is a common agent in CAP and is a well-known polyclonal B-cell activator (4), an attempt was made to investigate the possibility of cross-reactivity in the rDNA LPS ELISA due to acute M. pneumoniae infection. Acute- and convalescent-phase serum samples from 40 patients with serological evidence of M. pneumoniae infection were used for this evaluation. None of these patients had serological results compatible with acute C. pneumoniae infection, as observed by the MIF assay and the rDNA LPS ELISA. However, high prevalences of Chlamydia-specific IgG, IgM, and IgA antibodies by rDNA LPS ELISA were found in these patients (75, 18, and 48%, respectively). Positive results for IgM were found for seven patients. However, all seven patients had an IgM titer that was rather low (optical density values ranged between 1.2 and 3.0 times the cutoff value, with a median valve of 1.5) and the titer did not change between the acute and convalescent phases of their disease. To further elucidate the nature of this IgM reactivity in these patients, their serum samples were absorbed with a highly concentrated M. pneumoniae suspension prior to their processing in the ELISA. No significant reduction in Chlamydia-specific IgM antibody titer was found after such absorption (data not shown). Furthermore, the M. pneumoniae CF antibody titers in the 156 patients with acute CAP were determined. These data, together with those for patients with M. pneumoniae infection, were analyzed. A positive correlation was found between the Mycoplasma titer and the chlamydial IgG, IgM, and IgA seroprevalence, as determined by the rDNA LPS ELISA (Table 4).
TABLE 4.
Correlation between M. pneumoniae antibody titer found by CF antibody assay and Chlamydia-specific antibodies determined by rDNA LPS ELISA
| Reciprocal M. pneumoniae CF antibody titer | No. of patients tested | No. (%) of patients seropositive by rDNA LPS ELISA
|
||
|---|---|---|---|---|
| IgGa | IgMb | IgAc | ||
| <4 | 35 | 19 (54) | 2 (6) | 18 (51) |
| 4–16 | 69 | 35 (51) | 8 (12) | 37 (54) |
| 32–128 | 69 | 43 (62) | 11 (16) | 40 (58) |
| ≥256 | 17 | 15 (88) | 5 (29) | 12 (71) |
Correlation coefficient, 0.902; P = 0.098 (by chi-square test for trend, P = 0.020).
Correlation coefficient, 0.975; P = 0.025 (by chi-square test for trend, P = 0.020).
Correlation coefficient, 0.954; P = 0.049 (by chi-square test for trend, P = 0.201).
DISCUSSION
More than 10 years after the first publication in 1986 suggesting that C. pneumoniae causes acute respiratory infection (22), the diagnosis of this infection is still difficult to make. In the early 1970s, a sensitive MIF assay was developed, and this assay proved to be suitable for routine diagnosis (49, 50). In the MIF test, purified elementary bodies are used to detect Chlamydia-specific antibodies in the IgM, IgG, and IgA serum fractions. Some researchers claim that the C. pneumoniae MIF test is highly specific (22, 23, 36). Others, however, have noted cross-reactions between C. pneumoniae and other chlamydial species (31, 35, 37). This may be explained by the fact that the elementary body of each Chlamydia species possesses both genus-specific and species-specific antigenic sites. A species-specific positive result is based on the reaction with the major outer membrane protein of the elementary body, while chlamydial LPS is responsible for a genus-specific reaction (43). Interpretation may thus be difficult. Also, rheumatoid factor can cause false-positive C. pneumoniae IgM results (44). Acute C. pneumoniae infections can also be diagnosed by culture and PCR. However, these techniques require highly trained, experienced personnel and are not yet commercially available. Recently, chemically pure chlamydial LPS has been applied in the development of a commercially available rDNA LPS ELISA (6, 7, 25). One of the disadvantages of using LPS is the inherent serological cross-reactivity among the Chlamydia species. However, a major advantage is the rapid development of anti-LPS antibodies early in the infection (29). Also, the rDNA LPS ELISA results are observer independent and can easily be standardized for routine diagnosis, while interpretation of the MIF assay results is more subjective and highly qualified personnel are required to interpret the fluorescence results. Little is known about the sensitivity and specificity of this ELISA for determination of the seroprevalence of C. pneumoniae. In this study, we found that the rDNA LPS ELISA may not be reliable for determination of the seroprevalence of C. pneumoniae, i.e., for use in searching for patients with serological evidence of a C. pneumoniae infection in the past. The seroprevalence in the two different patient populations indicates that the half-life of the anti-LPS chlamydial antibodies is much lower than that of the major outer membrane protein antibodies (this study). The chlamydial LPS antibody seroprevalence was higher in patients with a history of COPD than in blood donors. This may be partly explained by differences in exposure between the two study groups. Another explanation may be found in the coexistence of other respiratory diseases in older adults with COPD, which may, upon exposure to C. pneumoniae, predispose them to clinical disease and thus result in an increased C. pneumoniae seroprevalence (11, 24).
Another approach was to evaluate the MIF assay, CF test, rDNA LPS ELISA, PCR, and culture for the diagnosis of CAP caused by C. pneumoniae. However, the major problem in validating these tests is the definition of the gold standard. By using the MIF assay as the gold standard, the sensitivity, specificity, and, especially, the PPV of the rDNA LPS ELISA were somewhat disappointing. Even more discouraging results were observed by the CF test. The sensitivity of the CF test for the detection of chlamydial infection was shown to be very low, particularly for the elderly group of patients, in whom most C. pneumoniae infections are reinfections that may not induce complement-fixing antibodies. In the present study only two patients had CF test results indicating acute chlamydial infection. Similar results were found earlier (13). The diagnostic value of the CF test is therefore questionable, and clinicians are dissuaded from making further use of the CF test for the diagnosis of acute C. pneumoniae. Discouraging results were also observed by PCR. This finding may in part be explained by a low sensitivity of the MIF test. Only severe, deeper localized infections may induce a reaction of the immune system. This is one of the reasons that the utility of the MIF test for the etiologic diagnosis of C. pneumoniae infection has been questioned earlier by several investigators (31, 37). Another approach that can be used to search for true-positive patients has been published by Gaydos et al. (19) and Falck et al. (16). They used an expanded gold standard that was based on MIF assay serology and detection of the organism in respiratory specimens. A patient was considered to be true positive if serological evidence of an acute C. pneumoniae infection was observed by the MIF assay or respiratory specimens were positive for C. pneumoniae by PCR or culture. By using this expanded gold standard, low sensitivities were found for the MIF assay and the rDNA LPS ELISA. If all respiratory specimens were incorporated in this evaluation, the highest sensitivity was achieved by PCR. On the other hand, the use of PCR and culture for the etiologic diagnosis of CAP caused by C. pneumoniae may be questioned. Asymptomatic C. pneumoniae infections, which often have no serological response, have been reported earlier (2, 14, 20, 26, 27), and this may affect the specificity of the test. Therefore, we designed a more conservative expanded gold standard, which validated the result for a true-positive patient if the serological results obtained by the MIF assay and the rDNA LPS ELISA indicated acute chlamydial infection. This will increase the probability of true C. pneumoniae CAP. Again, the MIF assay and the rDNA LPS ELISA performed equally well and were significantly better than PCR. Either the MIF assay or the rDNA LPS ELISA based on the last expanded gold standard definition on serological results indicating acute chlamydial infection. Increased sensitivity was observed when the rDNA LPS ELISA was applied. Six patients had serological results indicative of an acute infection only by rDNA LPS ELISA. This may be explained by the difference in sensitivity which was reported earlier (47). In addition, no clear difference in the clinical presentation between these six patients and the other seroresponders was observed (data not shown).
Mixed infections in association with other agents were found significantly more often in seroresponders than in serononresponders. This may indicate that C. pneumoniae pneumonia mixed with other etiologies may enforce the increased involvement of the immune system due to more severe tissue damage. Mixed infections with S. pneumoniae were most commonly found. These findings were in accordance with the results of Kauppinen and colleagues (29, 30) and Falguera and colleagues (17).
The choice of respiratory specimen may have a major impact on the sensitivity of the C. pneumoniae PCR. Independently of the four different gold standards used, the highest sensitivity and specificity could be obtained with nasopharyngeal specimens. Surprisingly, none of the sputum samples tested became positive. These findings may indicate colonization of the organism in the upper respiratory tract rather than invasive infection of the lower respiratory tract.
Only one patient was culture positive. This may be partly explained by the cell line used. A previous investigation (45) has indicated that BGM cells are highly sensitive for the isolation and propagation of C. pneumoniae. However, the diagnostic value with patient samples was not previously evaluated. Another possibility may be the cell culture protocol. Also, an inapparent cell line contamination with Mycoplasma may confound research efforts (46).
Ekman et al. (13) demonstrated that the timing of retrieval of the convalescent-phase serum sample is of great importance, because the MIF test may not show an increase in titer until 4 weeks after infection. These results are in accordance with our data; when the results for the third serum sample were disregarded, the infection in 33 and 25% of the patients with an established C. pneumoniae etiology was not diagnosed by the MIF assay and the rDNA LPS ELISA, respectively. In other words, the use of a third serum sample, drawn after 30 days, will maximize the ability to diagnose an acute infection serologically. Also, the use of a single serum sample to diagnose an acute chlamydial infection may reduce the sensitivities and specificities of the assays. Falck et al. (15) reported high C. pneumoniae IgG antibody titers, as determined by the MIF assay, in patients with persistent C. pneumoniae infection without clinical signs of infection for periods of 6 months up to a year. Also, persistent IgM for more than a year has been found earlier (47). A chronic, asymptomatic C. pneumoniae infection may be responsible for this phenomenon.
The increased prevalence of Chlamydia-specific antibodies in patients with a recent M. pneumoniae infection found by the rDNA LPS ELISA may be explained by polyclonal B-cell activation. Polyclonal B-cell activation due to M. pneumoniae infection has been reported earlier by Biberfeld and Gronowicz (4). The positive correlation found between the Mycoplasma CF antibody titer and the Chlamydia-specific IgM prevalence may have a significant impact on the specificity of the rDNA LPS ELISA, especially when a single serum sample is used. None of these patients had significant changes in their anti-LPS IgM titers. The use of paired serum samples from each patient, taken with at least a 10-day interval, will negate this problem.
In conclusion, the study shows that the choice of the gold standard remains difficult and, as expected, has a major impact on the sensitivities and specificities of the tests validated in this study. Further studies are necessary to determine the value of the PCR with upper respiratory tract specimens to diagnose lower respiratory tract infections. In addition, the rDNA LPS ELISA may currently be the preferred serological tool for diagnosing acute respiratory Chlamydia infections in routine clinical practice. The presence of only C. pneumoniae DNA in upper respiratory tract specimens, as demonstrated by PCR, without a concomitant serological response, may indicate prolonged, harmless colonization of the respiratory tract rather than the agent causing pneumonia.
ACKNOWLEDGMENT
We thank A. F. Angulo for providing the M. pneumoniae cultures.
REFERENCES
- 1.Aldous M B, Grayston J T, Wang S P, Foy H M. Seroepidemiology of Chlamydia pneumoniae TWAR infection in Seattle families, 1966–1979. J Infect Dis. 1992;166:646–649. doi: 10.1093/infdis/166.3.646. [DOI] [PubMed] [Google Scholar]
- 2.Bauwens J E, Gibbons M S, Hubbard M M, Stamm W E. Chlamydia pneumoniae (strain TWAR) isolated from two symptom-free children during evaluation for possible sexual assault. J Pediatr. 1991;119:591–593. doi: 10.1016/s0022-3476(05)82411-4. [DOI] [PubMed] [Google Scholar]
- 3.Ben Yaakov M, Lazarovich Z, Beer S, Levin A, Shoham I, Boldur I. Prevalence of Chlamydia pneumoniae antibodies in patients with acute respiratory infections in Israel. J Clin Pathol. 1994;47:232–235. doi: 10.1136/jcp.47.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biberfeld G, Gronowicz E. Mycoplasma pneumoniae is a polyclonal B-cell activator. Nature. 1976;261:238–239. doi: 10.1038/261238a0. [DOI] [PubMed] [Google Scholar]
- 5.Boom R, Sol C J, Salimans M M, Jansen C L, Wertheim-van Dillen P M, van der Noordaa J. Rapid and simple method for purification of nucleic acids. J Clin Microbiol. 1990;28:495–503. doi: 10.1128/jcm.28.3.495-503.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brade L, Brunnemann H, Ernst M, Fu Y, Holst O, Kosma P, Naher H, Persson K, Brade H. Occurrence of antibodies against chlamydial lipopolysaccharide in human sera as measured by ELISA using an artificial glycoconjugate antigen. FEMS Immunol Med Microbiol. 1994;8:27–41. doi: 10.1111/j.1574-695X.1994.tb00422.x. [DOI] [PubMed] [Google Scholar]
- 7.Brade L, Holst O, Kosma P, Zhang Y X, Paulsen H, Krausse R, Brade H. Characterization of murine monoclonal and murine, rabbit, and human polyclonal antibodies against chlamydial lipopolysaccharide. Infect Immun. 1990;58:205–213. doi: 10.1128/iai.58.1.205-213.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell L A, Perez Melgosa M, Hamilton D J, Kuo C C, Grayston J T. Detection of Chlamydia pneumoniae by polymerase chain reaction. J Clin Microbiol. 1992;30:434–439. doi: 10.1128/jcm.30.2.434-439.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chirgwin K, Roblin P M, Gelling M, Hammerschlag M R, Schachter J. Infection with Chlamydia pneumoniae in Brooklyn. J Infect Dis. 1991;163:757–761. doi: 10.1093/infdis/163.4.757. [DOI] [PubMed] [Google Scholar]
- 10.Chow, A. W., C. B. Hall, J. O. Klein, R. B. Kammer, R. D. Meyer, and J. S. Remmington. 1992. Guidelines for the evaluation of new anti-infective drugs for the treatment of respiratory tract infections. Clin. Infect. Dis. 15(Suppl. 1):S62–S88. [DOI] [PMC free article] [PubMed]
- 11.Cohen B H, Ball W C J, Brashears S, Diamond E L, Kreiss P, Levy D A, Menkes H A, Permutt S, Tockman M S. Risk factors in chronic obstructive pulmonary disease (COPD) Am J Epidemiol. 1977;105:223–232. doi: 10.1093/oxfordjournals.aje.a112378. [DOI] [PubMed] [Google Scholar]
- 12.Cosentini R, Blasi F, Raccanelli R, Rossi S, Arosio C, Tarsia P, Randazzo A, Allegra L. Severe community-acquired pneumonia: a possible role for Chlamydia pneumoniae. Respiration. 1996;63:61–65. doi: 10.1159/000196519. [DOI] [PubMed] [Google Scholar]
- 13.Ekman M R, Leinonen M, Syrjala H, Linnanmaki E, Kujala P, Saikku P. Evaluation of serological methods in the diagnosis of Chlamydia pneumoniae pneumonia during an epidemic in Finland. Eur J Clin Microbiol Infect Dis. 1993;12:756–760. doi: 10.1007/BF02098463. [DOI] [PubMed] [Google Scholar]
- 14.Emre U, Roblin P M, Gelling M, Dumomay W, Rao M, Hammerschlag M R, Schachter J. The association of Chlamydia pneumoniae infection and reactive airway disease in children. Arch Pediatr Adolesc Med. 1994;148:727–732. doi: 10.1001/archpedi.1994.02170070065013. [DOI] [PubMed] [Google Scholar]
- 15.Falck G, Gnarpe J, Gnarpe H. Persistent Chlamydia pneumoniae infection in a Swedish family. Scand J Infect Dis. 1996;28:271–273. doi: 10.3109/00365549609027171. [DOI] [PubMed] [Google Scholar]
- 16.Falck G, Heyman L, Gnarpe J, Gnarpe H. Chlamydia pneumoniae (TWAR): a common agent in acute bronchitis. Scand J Infect Dis. 1994;26:179–187. doi: 10.3109/00365549409011782. [DOI] [PubMed] [Google Scholar]
- 17.Falguera M, Nogues A, Ruiz-Gonzalez A. Community-acquired Chlamydia pneumoniae pneumonia. Thorax. 1996;51:967. doi: 10.1136/thx.51.9.967-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freidank H M, Brauer D. Prevalence of antibodies to Chlamydia pneumoniae TWAR in a group of German medical students. J Infect. 1993;27:89–93. doi: 10.1016/0163-4453(93)94013-2. [DOI] [PubMed] [Google Scholar]
- 19.Gaydos C A, Eiden J J, Oldach D, Mundy L M, Auwaerter P, Warner M L, Vance E, Burton A A, Quinn T C. Diagnosis of Chlamydia pneumoniae infection in patients with community-acquired pneumonia by polymerase chain reaction enzyme immunoassay. Clin Infect Dis. 1994;19:157–160. doi: 10.1093/clinids/19.1.157. [DOI] [PubMed] [Google Scholar]
- 20.Gaydos C A, Roblin P M, Hammerschlag M R, Hyman C L, Eiden J J, Schachter J, Quinn T C. Diagnostic utility of PCR-enzyme immunoassay, culture, and serology for detection of Chlamydia pneumoniae in symptomatic and asymptomatic patients. J Clin Microbiol. 1994;32:903–905. doi: 10.1128/jcm.32.4.903-905.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grayston J T, Aldous M B, Easton A, Wang S P, Kuo C C, Campbell L A, Altman J. Evidence that Chlamydia pneumoniae causes pneumonia and bronchitis. J Infect Dis. 1993;168:1231–1235. doi: 10.1093/infdis/168.5.1231. [DOI] [PubMed] [Google Scholar]
- 22.Grayston J T, Kuo C C, Wang S P, Altman J. A new Chlamydia psittaci strain, TWAR, isolated in acute respiratory tract infections. N Engl J Med. 1986;315:161–168. doi: 10.1056/NEJM198607173150305. [DOI] [PubMed] [Google Scholar]
- 23.Grayston J T, Wang S P, Kuo C C, Campbell L A. Current knowledge on Chlamydia pneumoniae, strain TWAR, an important cause of pneumonia and other acute respiratory diseases. Eur J Clin Microbiol Infect Dis. 1989;8:191–202. doi: 10.1007/BF01965260. [DOI] [PubMed] [Google Scholar]
- 24.Higgings M W, Keller J B, Landis J R, Beaty T H, Burrows B, Demets D, Diem J E, Higgings I T T, Lakatos E, et al. Risk of chronic obstructive pulmonary disease. Am Rev Respir Dis. 1984;130:385. doi: 10.1164/arrd.1984.130.3.380. [DOI] [PubMed] [Google Scholar]
- 25.Holst O, Brade L, Kosma P, Brade H. Structure, serological specificity, and synthesis of artificial glycoconjugates representing the genus-specific lipopolysaccharide epitope of Chlamydia spp. J Bacteriol. 1991;173:1862–1866. doi: 10.1128/jb.173.6.1862-1866.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hyman C L, Augenbraun M H, Roblin P M, Schachter J, Hammerschlag M R. Asymptomatic respiratory tract infection with Chlamydia pneumoniae TWAR. J Clin Microbiol. 1991;29:2082–2083. doi: 10.1128/jcm.29.9.2082-2083.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hyman C L, Roblin P M, Gaydos C A, Quinn T C, Schachter J, Hammerschlag M R. Prevalence of asymptomatic nasopharyngeal carriage of Chlamydia pneumoniae in subjectively healthy adults: assessment by polymerase chain reaction-enzyme immunoassay and culture. Clin Infect Dis. 1995;20:1174–1178. doi: 10.1093/clinids/20.5.1174. [DOI] [PubMed] [Google Scholar]
- 28.Karvonen M, Tuomilehto J, Pitkaniemi J, Saikku P. The epidemic cycle of Chlamydia pneumoniae infection in eastern Finland, 1972–1987. Epidemiol Infect. 1993;110:349–360. doi: 10.1017/s0950268800068291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kauppinen M T, Saikku P. Pneumonia due to Chlamydia pneumoniae: prevalence, clinical features, diagnosis and treatment. Clin Infect Dis. 1995;21:S244–S255. doi: 10.1093/clind/21.supplement_3.s244. [DOI] [PubMed] [Google Scholar]
- 30.Kauppinen M T, Saikku P, Kujala P, Herva E, Syrjala H. Clinical picture of community-acquired Chlamydia pneumoniae pneumonia requiring hospital treatment: a comparison between chlamydial and pneumococcal pneumonia. Thorax. 1996;51:185–189. doi: 10.1136/thx.51.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kern D G, Neill M A, Schachter J. A seroepidemiologic study of Chlamydia pneumoniae in Rhode Island. Evidence of serologic cross-reactivity. Chest. 1993;104:208–213. doi: 10.1378/chest.104.1.208. [DOI] [PubMed] [Google Scholar]
- 32.Kleemola M, Saikku P, Visakorpi R, Wang S P, Grayston J T. Epidemics of pneumonia caused by TWAR, a new Chlamydia organism, in military trainees in Finland. J Infect Dis. 1988;157:230–236. doi: 10.1093/infdis/157.2.230. [DOI] [PubMed] [Google Scholar]
- 33.Kwok S K, Higuchi R. Avoiding false positives with PCR. Nature. 1989;339:237–238. doi: 10.1038/339237a0. [DOI] [PubMed] [Google Scholar]
- 34.Marton A, Karolyi A, Szalka A. Prevalence of Chlamydia pneumoniae antibodies in Hungary. Eur J Clin Microbiol Infect Dis. 1992;11:139–142. doi: 10.1007/BF01967065. [DOI] [PubMed] [Google Scholar]
- 35.Moss T R, Darougar S, Woodland R M, Nathan M, Dines R J, Cathrine V. Antibodies to Chlamydia species in patients attending a genitourinary clinic and the impact of antibodies to C. pneumoniae and C. psittaci on the sensitivity and the specificity of C. trachomatis serology tests. Sex Transm Dis. 1993;20:61–65. doi: 10.1097/00007435-199303000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Osser S, Persson K. Immune response to genital chlamydial infection and influence of Chlamydia pneumoniae (TWAR) antibodies. Eur J Clin Microbiol Infect Dis. 1989;8:532–535. doi: 10.1007/BF01967475. [DOI] [PubMed] [Google Scholar]
- 37.Ozanne G, Lefebvre J. Specificity of the microimmunofluorescence assay for the serodiagnosis of Chlamydia pneumoniae infections. Can J Microbiol. 1992;38:1185–1189. doi: 10.1139/m92-194. [DOI] [PubMed] [Google Scholar]
- 38.Pacheco A, Gonzalez Sainz J, Arocena C, Rebollar M, Antela A, Guerrero A. Community acquired pneumonia caused by Chlamydia pneumoniae strain TWAR in chronic cardiopulmonary disease in the elderly. Respiration. 1991;58:316–320. doi: 10.1159/000195952. [DOI] [PubMed] [Google Scholar]
- 39.Saikku P. Chlamydial serology. Scand J Infect Dis Suppl. 1982;32:34–37. [PubMed] [Google Scholar]
- 40.Steinhoff D, Lode H, Ruckdeschel G, Heidrich B, Rolfs A, Fehrenbach F J, Mauch H, Hoffken G, Wagner J. Chlamydia pneumoniae as a cause of community-acquired pneumonia in hospitalized patients in Berlin. Clin Infect Dis. 1996;22:958–964. doi: 10.1093/clinids/22.6.958. [DOI] [PubMed] [Google Scholar]
- 41.Sundelof B, Gnarpe J, Gnarpe H, Grillner L, Darougar S. Chlamydia pneumoniae in Swedish patients. Scand J Infect Dis. 1993;25:429–433. doi: 10.3109/00365549309008523. [DOI] [PubMed] [Google Scholar]
- 42.Tjhie H T, Kock J H, Theunissen J J, Stolz E, MacLaren D M. Successful culture of Chlamydia pneumoniae in 2 asymptomatic patients. Ned Tijdschr Geneeskd. 1994;138:1913–1916. . (In Dutch.) [PubMed] [Google Scholar]
- 43.Van Renterghem L, Van den Abeele A M, Claeys G, Plum J. Prevalence of antibodies to Chlamydia pneumoniae in a pediatric hospital population in Belgium. Eur J Clin Microbiol Infect Dis. 1990;9:347–349. doi: 10.1007/BF01973742. [DOI] [PubMed] [Google Scholar]
- 44.Verkooyen R P, Hazenberg M A, Van Haaren G H, Van Den Bosch J M, Snijder R J, Van Helden H P, Verbrugh H A. Age-related interference with Chlamydia pneumoniae microimmunofluorescence serology due to circulating rheumatoid factor. J Clin Microbiol. 1992;30:1287–1290. doi: 10.1128/jcm.30.5.1287-1290.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Verkooyen R P, Mousavi Joulandan S A, Verbrugh H A. Program and abstracts of the 32nd Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, D.C: American Society for Microbiology; 1992. Effect of cell type, test organism and DEAE-dextran on the performance of tissue culture for Chlamydia pneumoniae, abstr. 541; p. 201. [Google Scholar]
- 46.Verkooyen R P, Sijmons M, Fries E, van Belkum A, Verbrugh H A. Widely used, commercially available Chlamydia pneumoniae antigen contaminated with mycoplasma. J Med Microbiol. 1997;46:419–424. doi: 10.1099/00222615-46-5-419. [DOI] [PubMed] [Google Scholar]
- 47.Verkooyen R P, Van Lent N A, Mousavi Joulandan S A, Snijder R J, Van Den Bosch J M, Van Helden H P, Verbrugh H A. Diagnosis of Chlamydia pneumoniae infection in chronic obstructive pulmonary disease patients by using microimmunofluorescence and ELISA. J Med Microbiol. 1997;56:959–965. doi: 10.1099/00222615-46-11-959. [DOI] [PubMed] [Google Scholar]
- 48.Wang J H, Liu Y C, Cheng D L, Yeng M Y, Chen Y S, Chen B C. Seroprevalence of Chlamydia pneumoniae in Taiwan. Scand J Infect Dis. 1993;25:565–568. doi: 10.3109/00365549309008544. [DOI] [PubMed] [Google Scholar]
- 49.Wang S P, Grayston J T. Immunologic relationship between genital TRIC, lymphogranuloma venereum, and related organisms in a new microtiter indirect immunofluorescence test. Am J Ophthalmol. 1970;70:367–374. doi: 10.1016/0002-9394(70)90096-6. [DOI] [PubMed] [Google Scholar]
- 50.Wang S P, Grayston J T, Alexander E R, Holmes K K. Simplified microimmunofluorescence test with trachoma-lymphogranuloma venereum (Chlamydia trachomatis) antigens for use as a screening test for antibody. J Clin Microbiol. 1975;1:250–255. doi: 10.1128/jcm.1.3.250-255.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yamazaki T, Nakada H, Sakurai N, Kuo C C, Wang S P, Grayston J T. Transmission of Chlamydia pneumoniae in young children in a Japanese family. J Infect Dis. 1990;162:1390–1392. doi: 10.1093/infdis/162.6.1390. [DOI] [PubMed] [Google Scholar]