Abstract
Aims
In INTERSTROKE, we explored the association of anger or emotional upset and heavy physical exertion with acute stroke, to determine the importance of triggers in a large, international population.
Methods and results
INTERSTROKE was a case–control study of first stroke in 32 countries. Using 13 462 cases of acute stroke we adopted a case-crossover approach to determine whether a trigger within 1 hour of symptom onset (case period), vs. the same time on the previous day (control period), was associated with acute stroke. A total of 9.2% (n = 1233) were angry or emotional upset and 5.3% (n = 708) engaged in heavy physical exertion during the case period. Anger or emotional upset in the case period was associated with increased odds of all stroke [odds ratio (OR) 1.37, 99% confidence interval (CI), 1.15–1.64], ischaemic stroke (OR 1.22, 99% CI, 1.00–1.49), and intracerebral haemorrhage (ICH) (OR 2.05, 99% CI 1.40–2.99). Heavy physical exertion in the case period was associated with increased odds of ICH (OR 1.62, 99% CI 1.03–2.55) but not with all stroke or ischaemic stroke. There was no modifying effect by region, prior cardiovascular disease, risk factors, cardiovascular medications, time, or day of symptom onset. Compared with exposure to neither trigger during the control period, the odds of stroke associated with exposure to both triggers were not additive.
Conclusion
Acute anger or emotional upset was associated with the onset of all stroke, ischaemic stroke, and ICH, while acute heavy physical exertion was associated with ICH only.
Keywords: Stroke, Triggers, Exertion, Anger
Graphical Abstract
Introduction
As stroke is a leading global cause of death and disability, stroke prevention is a global health priority.1,2 The INTERSTROKE study reported that 10 potentially modifiable chronic risk factors are collectively associated with ∼90% of the population-attributable risk (PAR) of stroke.3 Despite multiple approaches to measuring cardiovascular risk burden, it remains difficult to predict when a stroke will occur.4 Importantly, this risk burden predominantly reflects medium- to long-term exposures (including hyperlipidaemia, obesity, and smoking) rather than acute exposures with transient effects that may act as triggers of stroke.5 This has been explored extensively for myocardial infarction, including our report on physical exertion, anger, or emotional upset as triggers of acute events.6 Although previous studies identified psychological stress,7,8 life events,9 alcohol abuse, clinical infection, anger, coffee intake, sexual activity, trauma, and surgery as potential triggers of stroke,10–12 few report on anger or emotional upset or heavy physical exertion, and those studies had small sample sizes and were completed in one country or geographical region.13 As with medium- to long-term cardiovascular risk factors, the prevalence and relative importance of triggers may also vary by geographical region, justifying the need for international studies with standardized methodologies to explore this question. The INTERSTROKE study provides an ideal opportunity to explore the association between two potential triggers and acute stroke, including important effect modifiers, in a large, international population.
Methods
Population
INTERSTROKE is a large, international, case–control study carried out in 142 centres in 32 countries, whose methods have previously been described in detail.14 In brief, cases were patients with acute first stroke (within 5 days of symptom onset and subsequently confirmed neuroimaging within 1 week of presentation) who were recruited into INTERSTROKE and completed questionnaires within 72 hours of hospital admission. Age- and sex-matched controls (community-based or hospital-based) were also recruited. In these analyses, we include only the cases of stroke, as the exposure to potential triggers was collected systematically in cases but not in controls.
Study procedures
Research study staff performed a standardized physical examination on participants and administered a structured questionnaire. Participants with acute stroke were asked dichotomous questions, ‘Were you angry or emotionally upset?’ and ‘Were you engaged in heavy physical exertion?’ in 1 hour before the onset of symptoms and during the corresponding 1 hour period on the previous day. Data were also collected for age, sex, smoking, usual physical activity, stress, education, medication use, and cardiovascular risk factors. Hypertension was defined as a self-reported history of hypertension or blood pressure ≥140/90 mmHg (including adjusted admission blood pressure, as previously reported3). Diabetes mellitus was defined as self-reported history of diabetes mellitus or glycated haemoglobin ≥6.5%. A history of atrial fibrillation prior to presentation was self-reported. Baseline physical activity, including work and leisure time, was categorized as sedentary (1–3 hours/week), mildly active (4 hours/week), moderately active (5 hours/week), or strenuous (6 hours/week). Smoking status was defined as never, former or current smoking. Baseline level of stress, including work and home time, was dichotomized as none or some periods vs. several periods or permanent stress. Depression was defined as feeling sad, blue, or depressed in the 2 weeks prior to stroke. Education was categorized as none, 1–8 years, 9–12 years, or Trade School, College or University. Countries were grouped into seven geographical regions: (i) Western Europe, North America, Australia (Canada, Australia, Germany, Denmark, Sweden, UK, and Ireland); (ii) Eastern Europe, Central Europe, Middle East (Croatia, Poland, Turkey, Iran, United Arab Emirates, Russia, and Saudi Arabia); (iii) China; (iv) South America (Argentina, Brazil, Chile, Colombia, Ecuador, and Peru); (v) Southeast Asia (Thailand, Philippines, and Malaysia); (vi) South Asia (India and Pakistan); and (vii) Africa (South Africa, Mozambique, Uganda, Sudan, and Nigeria). All data were transferred to the Population Health Research Institute, McMaster University, and Hamilton Health Sciences (Hamilton, ON, Canada). The study was approved by appropriate ethics committees in all centres and/or countries; all participants, or their proxy, provided written informed consent on study enrolment; the study was completed in line with ethical standards within each country.
Statistical analysis
Categorical variables are presented as percentage (number) and continuous variables are presented as mean (standard deviation) or median (25th–75th percentiles), as appropriate. A case-crossover approach was used in which each participant acts as his/her own control.15 The case period was defined as the 1 hour before the onset of stroke symptoms; the control period was defined as the corresponding 1 hour period on the day before symptom onset. Conditional logistic regression was used to estimate odds ratios (OR) and 99% confidence intervals (CIs) for anger or emotional upset and heavy physical exertion within the case period compared with the control period for all stroke, ischaemic stroke, and intracerebral haemorrhage (ICH). Because each participant acted as her or her own control, multivariable adjustment for baseline confounding factors was not required, but we did adjust for (i) the other triggering event because it varies with time and (ii) an interaction between both triggers, as the interaction was statistically significant (P = 0.004). PAR was calculated from the proportion of participants with exposure to the potential triggers in the case and control periods;16 99% CIs are also reported. The Breslow–Day test of homogeneity was used to explore if the conditional relationship between triggers and acute stroke was consistent by the time and day of onset of stroke.17
To explore if the associations differed significantly by conventional risk factors for stroke, analyses were stratified by the following pre-specified subgroups: age (<45, 45–65, >65 years), sex, smoking, diabetes mellitus, hypertension, atrial fibrillation, body mass index (BMI) (<25, 25–29.9, ≥30 kg/m2), angina, and myocardial infarction. For anger or emotional upset, stratified analyses were also completed by the baseline level of chronic stress, depression, and level of education to explore if the associations differed by baseline psychosocial factors. For heavy physical exertion, stratified analyses were also completed by the baseline level of physical activity to explore if the associations differed by usual level of activity, as a proxy for physical fitness. These subgroup analyses are presented for all stroke, ischaemic stroke, and ICH. For all stroke only, we also explored for differences in the observed associations by medications commonly used for the prevention of cardiovascular disease [aspirin, beta-blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACE-i/ARB), lipid-lowering therapy, and oral anticoagulant therapy], geographical region, the time, and the day of the week of symptom onset. Differential effects between stratified analyses were considered significant if the P-value for the interaction term between the stratifying variable and the trigger was <0.01; this more conservative threshold was chosen to address multiple testing. A sensitivity analysis was restricted to those participants who completed all questionnaires themselves, thus excluding those cases of acute stroke in whom questionnaires were completed by proxies. All statistical analyses were performed with Stata/MP 16.1, except for PAR, for which R version 3.3.1 for Mac was used.
Results
Of the 13 462 included participants with stroke, the mean age was 62.2 (13.6) years, 59.6% (n = 8021) were male, and there was representation from multiple ethnicities and regions (Supplementary material online, Table S1). The questionnaire was completed by the individual only in 41.4% (n = 5573), by a proxy only in 36.9% (n = 4967) and a combination of the individual and proxy in 21.7% (n = 2918).
Anger or emotional upset as a trigger
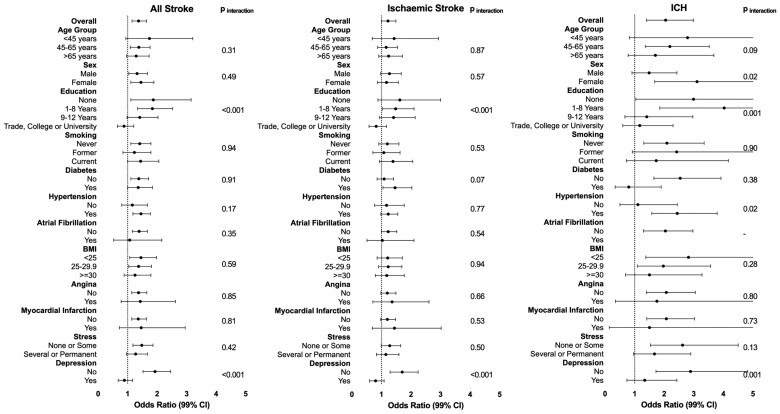
Anger or emotional upset was reported by 9.2% (n = 1233) of participants during the case period and 8.3% (n = 1111) during the control period. We had missing data for six participants (<0.1%). Those who reported anger or emotional upset in the case period were more likely to be younger and male and to have higher levels of education, BMI, and baseline stress. They were also more likely to have a history of diabetes, hypertension, angina, myocardial infarction, or depression and less likely to be taking cardiovascular prevention medications (Supplementary material online, Table S2). Compared with the control period, anger or emotional upset occurring during the case period was associated with increased odds of all stroke (OR 1.37, 99% CI 1.15–1.64 and PAR 2.5%, 99% CI 1.2–3.7), ischaemic stroke (OR 1.22, 99% CI 1.00–1.49 and PAR 1.6%, 99% CI 0.0–3.2), and ICH (OR 2.05, 99% CI 1.40–2.99 and PAR 2.5%, 99% CI 1.8–5.8) (Figure 1 and Supplementary material online, Table S3). The odds of stroke occurring in those with anger or emotional upset in the case period were greater in those without a history of depression for all stroke (Pinteraction < 0.001), ischaemic stroke (Pinteraction < 0.001), and ICH (Pinteraction = 0.012). The odds of stroke occurring in those with anger or emotional upset were greater in those with lower levels of education for all stroke (Pinteraction < 0.001) and ICH (Pinteraction = 0.001), and in those without a history of diabetes for ICH (Pinteraction = 0.002). There was no other effect modification by age group, sex, smoking, hypertension, atrial fibrillation, BMI, previous angina, previous myocardial infarction, or baseline level of stress.
Figure 1.
Association between Anger or emotional upset in case period and all stroke, ischaemic stroke and intracerebral haemorrhage (adjusted for heavy physical exertion and interaction between heavy physical exertion and anger/emotional upset in case period).
Heavy physical exertion as a trigger
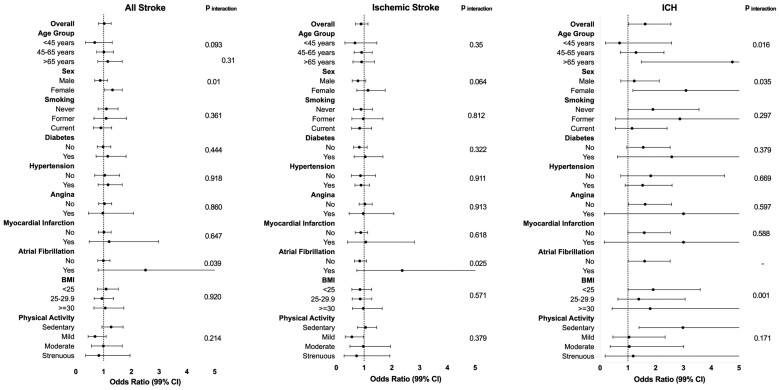
Heavy physical exertion was reported by 5.3% (n = 708) of participants during the case period and 5.4% (n = 725) during the control period. We had missing data for four participants (<0.1%). Those who reported heavy physical exertion in the case period were more likely to be younger, male, current smokers, and not diabetic. They were also more likely to have higher levels of baseline physical activity and higher adjusted systolic blood pressure at the time of admission (Supplementary material online, Table S4). Compared with the control period, heavy physical exertion occurring during the case period was not associated with all stroke (OR 1.02, 99% CI 0.82–1.27 and PAR 0.1%, 99% CI −1.0 to 1.1) or ischaemic stroke (OR 0.89, 99% CI 0.69–1.14 and PAR −0.6%, 99% CI −2.0 to 0.5) but was associated with increased odds of ICH (OR 1.62, 99% CI 1.03–2.55 and PAR −0.9%, 99% CI −4.0 to 1.3) (Figure 2 and Supplementary material online, Table S5). The odds of all stroke occurring in those with heavy physical exertion in the case period were higher in females (Pinteraction = 0.01), but there was no significant effect modification by age group, smoking, diabetes, hypertension, atrial fibrillation, previous angina, previous myocardial infarction, baseline atrial fibrillation, or baseline level of physical activity. The odds of ICH were lowest in participants with BMI 25–29.9 (Pinteraction = 0.001).
Figure 2.
Association between heavy physical exertion in case period and all stroke, ischaemic stroke and intracerebral haemorrhage (adjusted for anger/emotional upset and interaction between heavy physical exertion and anger/emotional upset in case period).
Effects of both triggers
Compared with exposure to neither trigger during the control period, the adjusted odds of stroke associated with exposure to both heavy physical exertion and anger or emotional upset occurring during the case period were not additive.
Effect modification by cardiovascular medications
There was no significant modification in the associations between either anger or emotional upset and heavy physical exertion and all stroke when analyses were stratified by the baseline use of aspirin, beta-blockers, ACE-i/ARB, lipid-lowering therapy, or oral anticoagulants (Supplementary material online, Table S6).
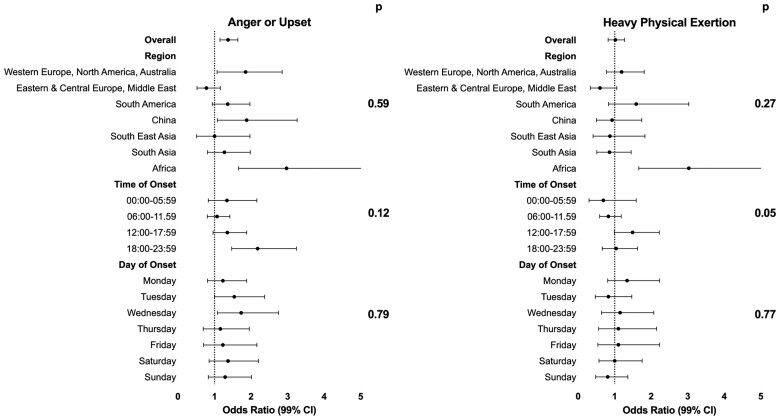
Effect modification by geographical region and timing of stroke
In analyses stratified by geographical region, there was no significant effect modification for the association between all stroke and anger or emotional upset and heavy physical exertion in the case period (Figure 3 and Supplementary material online, Table S7). The conditional relationship between each trigger and all stroke was consistent by time and day of onset (P-value for homogeneity >0.05 for each comparison).
Figure 3.
Associations between potential triggers and all stroke, stratified by geographical region, time of onset and day of onset (adjusted for anger/emotional upset and interaction between heavy physical exertion and anger/emotional upset in case period; P for interaction for analyses stratified by region; P for homogeneity for analyses stratified by time of onset and day of onset of stroke).
Ischaemic stroke subtypes
For anger or emotional upset, the greatest magnitude of association was seen for those with ‘other’ aetiological classification (OR 2.53, 99% CI 1.30–4.90) (Pinteraction < 0.001) (Table 1). There was no significant effect modification on analyses stratified by Oxfordshire Community Stroke Project (OCSP) classification (Pinteraction = 0.72). For heavy physical exertion, there was no significant effect modification on analyses stratified by aetiological classification (Pinteraction = 0.17) or OCSP classification (Pinteraction = 0.43).
Table 1.
Associations between potential triggers and ischaemic stroke, stratified by Aetiological and Oxfordshire Community Stroke Project classificationsa
| Anger or emotional upset |
Heavy physical exertion |
|||||
|---|---|---|---|---|---|---|
| Prevalence | OR (99% CI) | P int | Prevalence | OR (99% CI) | P int | |
| Overall | 9.2% (1233) | 1.22 (1.00–1.49) | – | 5.3% (708) | 0.89 (0.69–1.14) | – |
| Aetiological classification | ||||||
| Large vessel | 8.2% (174) | 0.67 (0.42–1.08) | <0.001 | 4.7% (99) | 0.62 (0.37–1.03) | 0.166 |
| Small vessel | 7.0% (278) | 1.05 (0.73–1.51) | 4.0% (162) | 0.85 (0.55–1.32) | ||
| Cardioembolic | 12.5% (150) | 1.47 (0.88–2.43) | 5.8% (69) | 1.36 (0.69–2.69) | ||
| Other | 12.5% (96) | 2.53 (1.30–4.90) | 3.2% (25) | 0.75 (0.25–2.21) | ||
| OCSP classification | ||||||
| Total anterior circulation | 9.0% (60) | 1.76 (0.79–3.93) | 0.720 | 4.5% (30) | 0.83 (0.28–2.50) | 0.427 |
| Partial anterior circulation | 8.6% (416) | 0.99 (0.73–1.34) | 4.6% (224) | 1.03 (0.71–1.50) | ||
| Posterior circulation | 10.4% (155) | 1.41 (0.87–2.29) | 5.0% (75) | 0.48 (0.26–0.89) | ||
| Lacunar | 7.7% (213) | 1.32 (0.87–2.02) | 4.0% (110) | 1.01 (0.61–1.67) | ||
CI, confidence interval; OCSP, Oxfordshire Community Stroke Project; OR, odds ratio.
Adjusted for other trigger (heavy physical exertion or anger/emotional upset) and interaction between heavy physical exertion and anger/emotional upset in case period.
Sensitivity analyses
Analyses restricted to participants who completed the questionnaires themselves showed similar results to our primary analyses. Anger or emotional upset in the case period was associated with increased odds of all stroke (OR 1.40, 99% CI 1.09–1.81), there was a weak and non-significant association with ischaemic stroke (OR 1.25, 99% CI 0.95–1.63), but a strong and increased odds of ICH (OR 3.93, 99% CI 1.62–9.56) (Pinteraction = 0.001). There was no association between heavy physical exertion in the case period and all stroke (OR 1.04, 99% CI 0.77–1.40) or ischaemic stroke (OR 0.94, 99% CI 0.68–1.29), but increased odds of ICH (OR 2.86, 99% CI 1.00–8.15) (Pinteraction = 0.009).
Discussion
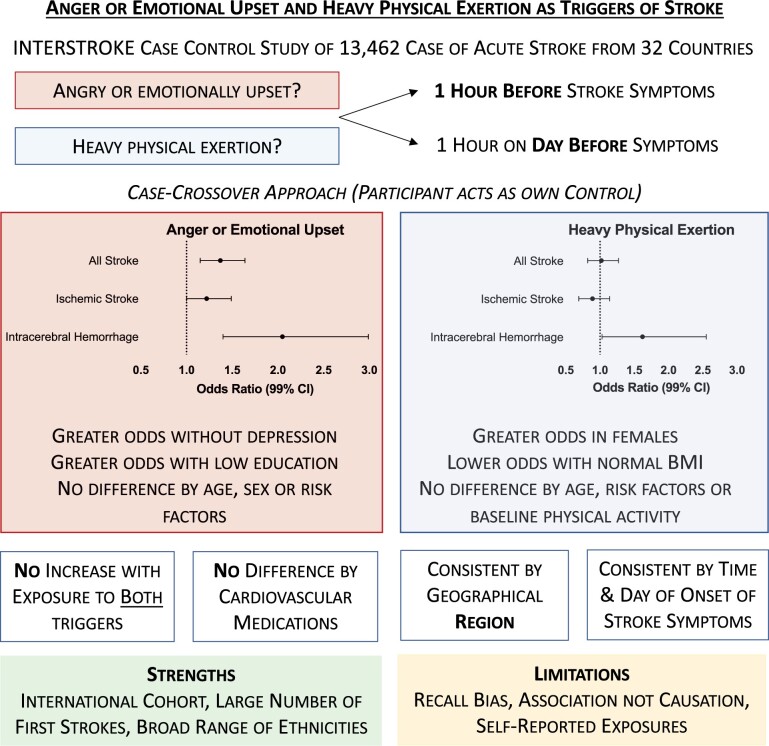
In this large, international study, we report that anger or emotional upset occurring in the 1 hour before stroke is relatively common and was associated with all stroke types, particularly for ICH. Heavy physical exertion was associated with increased odds of ICH only. No additive effects were seen in participants with both heavy physical exertion and anger or emotional upset in the 1 hour before stroke, and there were no significant differences by geographical region (Graphical Abstract). Our findings are consistent with previous, although limited, research13,18 and extend findings to an international global population.
Graphical Abstract.
Key summary of research question, study design, findings and implications.
Although long-term exposure to established cardiovascular risk factors is associated with ∼90% of the PAR of stroke (controlled for age and sex),3 they do not explain circadian or seasonal variations in stroke incidence. Although multiple studies report on the role of potential triggering events of myocardial infarction,6,19 less is known about potential triggering events of stroke. In the setting of already reduced perfusion, such as the presence of atherosclerotic plaque, exposure to a trigger may lead to a cardiovascular event.20 However, the pathogenesis of ischaemic stroke is more varied and less often due to atherosclerotic plaque, which may account for differences in the pattern and magnitude of association for stroke, compared to acute myocardial infarction. In contrast, acute increases in blood pressure are a significant risk factor for ICH12 and represent the most likely mechanism underlying the association with potential triggering events of stroke.
The case-crossover design is a powerful approach to study potential external triggers, and effect modification, as each individual serves as his or her own control, thereby controlling for many potential confounders. We did adjust for exposure to the other potential triggering event, which may vary with time within the individual, unlike common risk factors such as hypertension and diabetes. We chose 1 hour as the case period as the transient effects of external triggers decrease significantly with time after exposure, modifying the likelihood that an association between external triggers and stroke would be found. Triggers, such as acute exposure to anger or emotional upset or heavy physical exertion, are thought to lead to sympathetic activation,21 catecholamine secretion,22 vasoconstriction, and increased heart rate and blood pressure.12 Given the importance of raised blood pressure as a risk factor for stroke, and variation in PAR between ischaemic stroke and ICH,3 it is plausible that the effects of an external trigger may also differ by stroke type. While short-term increases in blood pressure may precipitate the onset of ICH,12 we speculate that short-term increases in heart rate may lead to an episode of atrial fibrillation, leading to the cardiac thrombus formation and a delayed onset of ischaemic stroke (i.e. beyond 1 hour and outside our case period). Although we had limited numbers of participants with underlying atrial fibrillation before stroke and the interaction term was not statistically significant, our stratified analyses suggest increased odds of all stroke and ischaemic stroke with heavy physical exertion in the case period, consistent with this hypothesis.
As exposure to external triggers is common and clearly does not always lead to stroke, we sought to identify those most at risk from acute exposures. We found no significant effect modification for the association between triggering events and stroke, on stratification by multiple cardiovascular risk factors (including smoking, hypertension, atrial fibrillation, previous angina, or myocardial infarction), common cardiovascular prevention medications, time, or day of onset of symptoms of stroke. Although previous studies reported circadian variation in the time of onset of stroke, with a peak in the late morning,23,24 we found no effect modification in the association between triggers and stroke by the time of symptom onset. In addition, although the greatest proportion of strokes occurred on Monday, we also found no effect modification in the association between triggers and stroke by the day of symptom onset.24 Our results from INTERSTROKE add to the literature as we remain limited in our ability to identify those most vulnerable to the effects of external triggers through risk factor stratification.
We did observe an increase in the odds of all stroke, ischaemic stroke, and ICH with anger or emotional upset during the case period in those without a history of depression and also in those with lower levels of education. Taken together, this suggests that those with higher levels of anger or psychological stress may have become acclimatized to the physiological responses to anger or emotional upset, which may blunt the physiological response to acute exposure to anger or upset.18 Therefore, our findings highlight the importance of minimizing exposure to anger or emotional upset for the majority of the population.
Regular physical activity is known to play a role in the long-term prevention of cardiovascular disease. We did not observe any association between heavy physical exertion and acute stroke and no significant effect modification on analyses stratified by the baseline level of physical activity. This contrasts against a previous study that reported moderate-to-extreme physical exertion as a potential trigger of subarachnoid haemorrhage,25 although the pathogenesis of stroke is different. Therefore, we continue to recommend regular physical activity for the prevention of cardiovascular disease, consistent with previous meta-analyses.26
The main strengths of this study include the case–control design, ideal to explore the potential impacts of triggering events, and the large international nature of the cohort with first stroke. This also provides us with the ability to explore the role of effect modifiers because of the sample size. INTERSTROKE includes large numbers of individuals from all regions of the world and multiple ethnicities, making the results broadly applicable. INTERSTROKE also includes only participants with first stroke, thereby reducing the possibility that altered lifestyles or risk factors resulting from previous stroke would affect our estimates. In addition, sensitivity analyses yielded similar associations.
The main limitation of this study is recall bias. Although the case-crossover approach, where each participant acts as her or her own control, reduces the effect of differences in perception within participants, participants who experienced stroke may differentially recall the intensity of exposure and may recall exposures as more proximate to the symptom onset. In addition, proxies completed questionnaires on behalf of some participants, who were limited by functional impairment or disability (e.g. participants with anosognosia, amnesia, or aphasia), further contributing to recall bias. However, sensitivity analyses restricted to participants who completed questionnaires themselves were similar to our primary results. Second, INTERSTROKE uses an observational design, meaning that we cannot establish causation. Third, exposure to potential triggering events was self-reported and objective scales were not used, as in some previous studies. As our comparison using the case-crossover approach is within individuals, it is unlikely that the lack of objective scales would significantly impact our findings as the participant is likely to interpret heavy physical exertion, anger, or emotional upset consistently over time. In addition, our primary findings are consistent with studies of triggers of cardiovascular events, suggesting that our measurements of the exposures are equally valid. Fourth, although standardized methodology was used in all regions, risk factors were self-reported. However, this would likely result in an underestimation of the prevalence of risk factors and bias estimates towards the null. Similarly, because INTERSTROKE only includes those patients presenting with first stroke, these data cannot be applied to the impact of triggering events in a secondary prevention population.
Conclusions
We report that anger or emotional upset is common in the 1 hour before the onset of symptoms of stroke and was associated with all stroke types. In contrast, the evidence is less convincing to support heavy physical exertion as an external trigger for stroke. There was no important effect modification by geographical region, time and day of onset of stroke, cardiovascular prevention medications, and many cardiovascular risk factors.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
The INTERSTROKE study was funded by the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, Canadian Stroke Network, Swedish Research Council, Swedish Heart and Lung Foundation, The Health & Medical Care Committee of the Regional Executive Board, and Regiona Viastra Gotaland (Sweden) and through unrestricted grants from several pharmaceutical companies with major contributions from AstraZeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), MSD, Swedish Heart and Lung Foundation, Chest, Heart and Stroke Scotland, and the Stroke Association, with support from The UK Stroke Research Network. The Department of Neurology at the University Duisburg-Essen received research grants from the German Research Council (DFG), German Ministry of Education and Research (BMBF), European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz-Nixdorf Foundation.
Conflict of interest: P.L.-J. declares honoraria from Menarini, Ely Lilly, Boehringer, and Merck. P.L. declares academic project grant support from Chest, Heart and Stroke Scotland and the Stroke Association. All other authors declare that there is no conflict of interest.
Data availability
No new data were generated or analysed in support of this research.
Supplementary Material
References
- 1. Feigin VL, Mensah GA, Norrving B, Murray CJ, Roth GA; Group GBDSPE. Atlas of the global burden of stroke (1990–2013): the GBD 2013 study. Neuroepidemiology 2015;45:230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Norrving B, Davis SM, Feigin VL, Mensah GA, Sacco RL, Varghese C.. Stroke prevention worldwide—what could make it work? Neuroepidemiology 2015;45:215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. O'Donnell MJ, Chin SL, Rangarajan Set al. ; INTERSTROKE Investigators. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016;388:761–775. [DOI] [PubMed] [Google Scholar]
- 4. Elkind MS. Why now? Moving from stroke risk factors to stroke triggers. Curr Opin Neurol 2007;20:51–57. [DOI] [PubMed] [Google Scholar]
- 5. Muller JE, Abela GS, Nesto RW, Tofler GH.. Triggers, acute risk factors and vulnerable plaques: the lexicon of a new frontier. J Am Coll Cardiol 1994;23:809–813. [DOI] [PubMed] [Google Scholar]
- 6. Smyth A, O’Donnell M, Lamelas P, Teo K, Rangarajan S, Yusuf S; INTERHEART Investigators. Physical activity and anger or emotional upset as triggers of acute myocardial infarction: the INTERHEART study. Circulation 2016;134:1059–1067. [DOI] [PubMed] [Google Scholar]
- 7. Prasad M, Khanna P, Katyal VK, Verma R.. Acute psychological stress is a trigger for stroke: a case-crossover study. J Stroke Cerebrovasc Dis 2020;29:104799. [DOI] [PubMed] [Google Scholar]
- 8. Aalbaek FS, Graff S, Vestergaard M.. Risk of stroke after bereavement—a systematic literature review. Acta Neurol Scand 2017;136:293–297. [DOI] [PubMed] [Google Scholar]
- 9. Gronewold J, Engels M, van de Velde Set al. Effects of life events and social isolation on stroke and coronary heart disease. Stroke 2021;52:735–747. [DOI] [PubMed] [Google Scholar]
- 10. Sharma A, Prasad K, Padma MVet al. Prevalence of triggering factors in acute stroke: hospital-based observational cross-sectional study. J Stroke Cerebrovasc Dis 2015;24:337–347. [DOI] [PubMed] [Google Scholar]
- 11. Guiraud V, Amor MB, Mas JL, Touze E.. Triggers of ischemic stroke: a systematic review. Stroke 2010;41:2669–2677. [DOI] [PubMed] [Google Scholar]
- 12. Vlak MH, Rinkel GJ, Greebe P, van der Bom JG, Algra A.. Trigger factors and their attributable risk for rupture of intracranial aneurysms: a case-crossover study. Stroke 2011;42:1878–1882. [DOI] [PubMed] [Google Scholar]
- 13. Koton S, Tanne D, Bornstein NM, Green MS.. Triggering risk factors for ischemic stroke: a case-crossover study. Neurology 2004;63:2006–2010. [DOI] [PubMed] [Google Scholar]
- 14. O'Donnell M, Xavier D, Diener Cet al. ; INTERSTROKE Investigators. Rationale and design of INTERSTROKE: a global case-control study of risk factors for stroke. Neuroepidemiology 2010;35:36–44. [DOI] [PubMed] [Google Scholar]
- 15. Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE.. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med 1993;329:1677–1683. [DOI] [PubMed] [Google Scholar]
- 16. Bruzzi P, Green SB, Byar DP, Brinton LA, Schairer C.. Estimating the population attributable risk for multiple risk factors using case-control data. Am J Epidemiol 1985;122:904–914. [DOI] [PubMed] [Google Scholar]
- 17. Breslow NE, Day NE.. Statistical Methods in Cancer Research Volume 1—The Analysis of Case-Control Studies. Lyon: International Agency for Research on Cancer. IARC Scientific Publications; 1980. [PubMed] [Google Scholar]
- 18. Mostofsky E, Penner EA, Mittleman MA.. Outbursts of anger as a trigger of acute cardiovascular events: a systematic review and meta-analysis. Eur Heart J 2014;35:1404–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B.. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet 2011;377:732–740. [DOI] [PubMed] [Google Scholar]
- 20. Lightbody CE, Clegg A, Patel Ket al. Systematic review and meta-analysis of psychosocial risk factors for stroke. Semin Neurol 2017;37:294–306. [DOI] [PubMed] [Google Scholar]
- 21. Mittleman MA, Maclure M, Sherwood JBet al. Triggering of acute myocardial infarction onset by episodes of anger. Determinants of Myocardial Infarction Onset Study Investigators. Circulation 1995;92:1720–1725. [DOI] [PubMed] [Google Scholar]
- 22. Mittleman MA, Mostofsky E.. Physical, psychological and chemical triggers of acute cardiovascular events: preventive strategies. Circulation 2011;124:346–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marler JR, Price TR, Clark GLet al. Morning increase in onset of ischemic stroke. Stroke 1989;20:473–476. [DOI] [PubMed] [Google Scholar]
- 24. Kelly-Hayes M, Wolf PA, Kase CS, Brand FN, McGuirk JM, D'Agostino RB.. Temporal patterns of stroke onset. The Framingham Study. Stroke 1995;26:1343–1347. [DOI] [PubMed] [Google Scholar]
- 25. Anderson C, Ni Mhurchu C, Scott D, Bennett D, Jamrozik K, Hankey G; Australasian Cooperative Research on Subarachnoid Hemorrhage Study Group. Triggers of subarachnoid hemorrhage: role of physical exertion, smoking, and alcohol in the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS). Stroke 2003;34:1771–1776. [DOI] [PubMed] [Google Scholar]
- 26. Lee CD, Folsom AR, Blair SN.. Physical activity and stroke risk: a meta-analysis. Stroke 2003;34:2475–2481. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were generated or analysed in support of this research.