Abstract
Exposure to adverse childhood experiences (ACEs), including maltreatment and family dysfunction, is a major contributor to the global burden of disease and disability. With a large body of international literature on ACEs having emerged over the past 25 years, it is timely to now synthetize the available evidence to estimate the global prevalence of ACEs and, through a series of moderator analyses, determine which populations are at higher risk. We searched studies published between January 1, 1998 and August 5, 2021 in Medline, PsycINFO and Embase. Study inclusion criteria were using the 8‐ or 10‐item ACE Questionnaire (±2 items), reporting the prevalence of ACEs in population samples of adults, and being published in English. The review protocol was registered with PROSPERO (CRD42022348429). In total, 206 studies (208 sample estimates) from 22 countries, with 546,458 adult participants, were included. The pooled prevalence of the five levels of ACEs was: 39.9% (95% CI: 29.8‐49.2) for no ACE; 22.4% (95% CI: 14.1‐30.6) for one ACE; 13.0% (95% CI: 6.5‐19.8) for two ACEs; 8.7% (95% CI: 3.4‐14.5) for three ACEs, and 16.1% (95% CI: 8.9‐23.5) for four or more ACEs. In subsequent moderation analyses, there was strong evidence that the prevalence of 4+ ACEs was higher in populations with a history of a mental health condition (47.5%; 95% CI: 34.4‐60.7) and with substance abuse or addiction (55.2%; 95% CI: 45.5‐64.8), as well as in individuals from low‐income households (40.5%; 95% CI: 32.9‐48.4) and unhoused individuals (59.7%; 95% CI: 56.8‐62.4). There was also good evidence that the prevalence of 4+ ACEs was larger in minoritized racial/ethnic groups, particularly when comparing study estimates in populations identifying as Indigenous/Native American (40.8%; 95% CI: 23.1‐59.8) to those identifying as White (12.1%; 95% CI: 10.2‐14.2) and Asian (5.6%; 95% CI: 2.4‐10.2). Thus, ACEs are common in the general population, but there are disparities in their prevalence. They are among the principal antecedent threats to individual well‐being and, as such, constitute a pressing social issue globally. Both prevention strategies and downstream interventions are needed to reduce the prevalence and mitigate the severity of the effects of ACEs and thereby reduce their deleterious health consequences on future generations.
Keywords: Adverse childhood experiences, mental health conditions, substance abuse, low‐income households, unhoused individuals, racial/ethnic minorities
Research on the impacts of child maltreatment spans over half a century. However, the publication of the Adverse Childhood Experience (ACE) Questionnaire 1 25 years ago – which is designed to document exposure to severe and stressful adversities related to maltreatment and household dysfunction experienced prior to age 18 – spurred a considerable body of research in this field.
Research has shown that ACEs have cascading life‐course effects on health‐harming behaviors (e.g., early substance use, smoking), mental health (e.g., depression, anxiety), physical health (e.g., cardiovascular disease, obesity, cancer), and relational functioning (e.g., intimate partner violence) 2 . A dose‐response association is often evident: as the number of ACEs increases, so too do the rates of the various unfavourable outcomes.
Through various mechanisms (e.g., neurodevelopmental disruption, epigenetic changes, and reprogramming of stress regulatory systems), exposure to ACEs is thus believed to increase the risk of cognitive challenges, lifelong disease and premature mortality, psychopathology, and social problems in adulthood.
In addition to the individual toll of ACEs, existing evidence also links substantial financial costs to such childhood adversity. Costs include loss of economic opportunity and productivity among individuals affected by ACEs and their families, legal and judicial costs associated with criminal offenses, as well as substantial lifetime medical costs associated with management of chronic disease and disability. The financial costs attributable to ACEs have been estimated to represent an average of 3% and as much as 6% of a country's annual gross domestic product 3 . Accordingly, ACEs have been identified by health agencies and institutions globally as one of the principal antecedent threats to individual well‐being, and an urgent social issue 3 .
The ACE Questionnaire asks respondents if they experienced any of the following events prior to the age of 18: sexual abuse, physical abuse, emotional abuse, physical or emotional neglect, growing up in a home where one or both parents were affected by mental illness or substance abuse, were incarcerated or separated, and/or were perpetrators or victims of domestic violence. Adversities that were in the original 8‐item version of the questionnaire included physical abuse, sexual abuse, emotional abuse, parent substance use, parent incarceration, parent mental health problems, and exposure to domestic violence. In 2001, an expanded 10‐item version was published that included two additional categories: physical/emotional neglect and parent divorce/separation. Otherwise, the questionnaire has remained remarkably consistent since its introduction. This consistency is critical as it allows for the development of a coherent evidence base, valid replication across time and geographical contexts, as well as comparisons between groups with different sociodemographic, economic and medical‐clinical characteristics, as well as risk profiles.
In 2018, Merrick et al 4 published the largest (N=248,934) ACE study to date, based on a representative US sample telephone survey, reporting a prevalence of 38.5% of people with no ACE, 23.5% of those with one ACE, 13.4% of those with two ACEs, 8.8% of those with three ACEs, and 15.8% of those with four or more ACEs. Research also shows that the prevalence of ACEs is higher in samples of individuals in socially and/or economically disadvantaged contexts, including groups that experience marginalization 5 , 6 , 7 . For example, in a meta‐analysis of the prevalence of ACEs in unhoused individuals, an average of 53.9% reported having 4+ ACEs 8 .
To our knowledge, no systematic review or meta‐analysis exists on the prevalence of ACEs in the general population globally, and, to date, there has been limited cross‐study moderation analysis examining whether the prevalence of ACEs differs between racial/ethnic, sex, sociodemographic and economic characteristics or profiles, or across geographical regions 5 , 6 , 7 .
With the widespread adoption of the ACE Questionnaire in public health research, and considering the individual, social and economic toll of ACEs, it is timely to synthetize the literature to establish a cross‐study and multi‐country distribution of these experiences. Systematic reviews and meta‐analyses are recognized as important resources for informing decision‐making in public health and clinical practice, because they summarize and quantify existing evidence across multiple, often heterogeneous, studies.
The objectives of the present systematic review and meta‐analysis were to estimate the distribution of ACEs across adult samples; the geographic differences in distribution of ACEs; and the differences in the distribution of ACEs among samples with different individual, social, demographic, economic and clinical characteristics.
METHODS
Search strategy
Studies published between January 1, 1998 and August 5, 2021 were searched in Medline, Embase and PsycINFO. Text word fields were searched with the phrase “adverse childhood experience or event”, as well as the acronym “ACEs”. We used both truncation symbols and adjacency operators to capture variations in phrasing. No language restrictions were applied (see also supplementary information).
This study followed the PRISMA guidelines 9 . The protocol was registered with PROSPERO (CRD42022348429).
Selection criteria
All titles/abstracts were independently double‐coded by five coders in Covidence according to the following inclusion criteria: using the 8‐ or 10‐item ACE Questionnaire (±2 items), reporting the prevalence of ACEs in population samples of adults, and being published in English. Studies were excluded if the ACE Questionnaire had <6 or >12 items.
Full‐text articles were reviewed by two independent coders (agreement probability: 84%). Discrepancies were resolved via consensus.
Data extraction
We applied a standardized protocol to extract the following study and sample characteristics: authors and publication date, country from which participants were sampled, method of data collection, sample size, counts for each category of ACEs, mean or median age, proportion of females and racially/ethnically minoritized individuals, socioeconomic profile (categorized as low, mixed or mid‐to‐high levels of household income), sociodemographic and health‐related characteristics (e.g., whether the sample included persons who were homeless, or with a history of mental health conditions or offending/criminality), and other study design and methodological characteristics to assess study quality (see also supplementary information).
Data extraction was conducted independently by two trained coders. Twenty percent of studies were randomly selected to estimate reliability among coders; intercoder agreement was 95%. Discrepancies were resolved through consensus.
Study quality assessment
Study quality was evaluated using an adapted version of the National Institutes of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies 10 . Two coders evaluated all studies for study quality (see also supplementary information). Intercoder agreement was 81%. Discrepancies were resolved through consensus.
Data preparation and analysis
Prevalence proportions for each of the five levels of ACEs (0, 1, 2, 3, 4+) were calculated by dividing the sample count for the given category of ACE by the overall study sample size. To stabilize the variances to properly weight prevalence proportions at the extreme ends of the range (e.g., where there was a 0 count for a given category of ACE), we applied the Freeman‐Tukey double arcsine transformation to each of the study estimates and standard errors prior to conducting the meta‐analysis 11 .
To estimate the prevalence proportions for each of the five levels of ACEs, a single multicategory prevalence meta‐analysis was performed in MetaXL (Version 5.3) 12 . The inverse of the average of the five levels of ACE variances was used to weigh the meta‐analysis, and between‐study heterogeneity was estimated and assessed using the tau (τ) statistic, which represents the average difference in the prevalence proportion between studies 13 .
Further subgroup and moderator analyses were conducted using the ‘regress’ command in Stata (Version 17), wherein robust (i.e., Huber‐Eicker‐White‐sandwich) error variances were applied 12 . Subgroup analysis of categorical moderators was conducted by calculating the ratio of the prevalence of a given category of ACE between different categories of the moderator (e.g., prevalence of 4+ ACEs in samples of Indigenous persons divided by the corresponding prevalence for samples of White or Asian persons). Analysis of continuous moderators was conducted by calculating the ratio between below (mean: –1 standard deviation, SD) and above (mean: +1 SD) average values for the moderator (e.g., prevalence of 4+ ACEs in studies with above average quality scores divided by the corresponding prevalence in studies with below average quality scores) 14 .
The magnitudes of the ratio representing a moderating association were interpreted using the following scale for increases in the prevalence proportion: slight: <1.11; small: 1.11‐1.43; moderate: 1.44‐2.00; large: >2.00. The inverses of these thresholds for interpreting decreases were: slight: >0.90; small: 0.90‐0.70; moderate: 0.71‐0.50; large: <0.50. The choice of such thresholds was guided by the scale of magnitudes for evaluating the effect size of a correlation coefficient devised by Cohen 15 (see also supplementary information). Thresholds for interpreting the magnitude of between‐study heterogeneity (τ) were the square root of the thresholds for ratio increases above 16 .
Sampling uncertainty was expressed as 95% confidence intervals (CI), and a precision of estimation approach was used to assess the level of evidence for or against the magnitude of a moderating association 17 , 18 , 19 . The extent of overlap of the 95% CI with slight and/or substantial (i.e., small, moderate and large) values was used to assess the level of evidence for or against the magnitude 18 (see supplementary information). Precision of estimation was deemed inadequate when the 95% CI included both substantial increases and decreases (i.e., ratios <0.90 and >1.11) 18 .
Assessment of publication bias, outliers, and influential cases
Publication bias was assessed by visually inspecting funnel plots of the double arcsine prevalence versus the standard error of the study‐estimate prevalence proportion for each category of ACE 12 . Sequential “leave‐one‐out” analysis (i.e., recalculating prevalence proportions with one study estimate omitted at a time) was conducted to identify outliers and influential cases 20 .
RESULTS
A total of 11,920 non‐duplicate records were identified by our search, of which 4,656 full‐text articles were screened for inclusion. Two hundred and six studies met the full inclusion criteria (see Figure 1), from which 208 multi‐category prevalence proportions were extracted for use in this review.
Figure 1.

PRISMA flow diagram. ACE – adverse childhood experience
The characteristics of included studies are detailed in the supplementary information. Across the 206 studies, 546,458 adults were represented. One hundred and seventy‐two studies reported data from North America (83.5%), 20 from Europe (9.7%), six from Asia (2.9%), four from Australia and New Zealand (1.9%), two from South America (1.0%), and one each from Africa (0.5%) and the Caribbean (0.5%). The average age of study samples was 33.9±11.7 years, and the average proportion of females was 35.5%. The racial/ethnic profile of the sample of included studies was as follows (as some studies allowed participants to indicate >1 category, percentages do not add to 100%): White (58.3%), Black (26.1%), Latinx (17.6%), Asian (13.3%), Indigenous/Native American (12.1%), mixed (8.3%), other unspecified (11.1%). The mean study quality score was 7.4 (range 3‐11; see also supplementary information).
Inspection of funnel plots only revealed evidence of publication bias for the category 0 ACE (see supplementary information). Sensitivity analysis of bias (i.e., “leave‐one‐out”) revealed limited evidence of influential cases; therefore, all study estimates were retained for the final meta‐analysis and moderation analyses.
The overall mean meta‐analyzed prevalence proportions for the five levels of ACEs, as well as the predicted mean prevalence proportions for ACEs at different levels of categorical and continuous moderators, are displayed in Table 1. The corresponding forest plots for each category of ACE are displayed in Figure 2 (0 ACE) and 3 (4+ ACE) and in the supplementary information.
Table 1.
Prevalence of the five levels of adverse childhood experiences (ACEs)
| Prevalence, % (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Moderators | n | 0 ACE | 1 ACE | 2 ACEs | 3 ACEs | 4+ ACEs |
| Overall mean | 208 | 39.9 (29.8‐49.2) | 22.4 (14.1‐30.6) | 13.0 (6.5‐19.8) | 8.7 (3.4‐14.5) | 16.1 (8.9‐23.5) |
| Sex at birth | ||||||
| Female | 190 | 34.6 (29.7‐39.8) | 23.6 (21.5‐25.8) | 14.1 (12.8‐15.5) | 9.1 (8.1‐10.2) | 17.5 (14.7‐20.6) |
| Male | 163 | 45.1 (34.5‐56.6) | 20.3 (16.0‐25.0) | 11.2 (8.5‐14.3) | 7.8 (6.0‐9.7) | 14.3 (12.0‐16.6) |
| Age | ||||||
| Below average (mean: –1 SD) | 170 | 33.4 (27.5‐39.6) | 21.2 (19.6‐22.9) | 14.1 (13.2‐15.1) | 10.5 (8.6‐12.6) | 18.1 (13.3‐23.5) |
| Above average (mean: +1 SD) | 170 | 38.0 (35.1‐40.9) | 23.1 (21.9‐24.3) | 13.2 (12.3‐14.2) | 9.5 (8.4‐10.6) | 14.9 (12.3‐17.7) |
| Region | ||||||
| North America | 173 | 38.7 (34.9‐42.6) | 21.8 (19.6‐24.1) | 12.8 (11.6‐14.1) | 8.7 (8.0‐9.4) | 16.9 (15.4‐18.6) |
| Europe | 21 | 46.7 (39.9‐53.7) | 25.4 (22.4‐28.5) | 12.0 (10.3‐13.7) | 7.2 (4.5‐10.6) | 5.6 (2.9‐9.0) |
| Other | 14 | 43.7 (23.2‐62.7) | 23.2 (7.1‐40.5) | 13.6 (1.5‐28.3) | 8.2 (0.0‐20.6) | 11.3 (0.5‐25.2) |
| Racial‐ethnic group | ||||||
| White | 149 | 43.4 (38.7‐48.0) | 23.7 (21.3‐26.1) | 13.2 (11.9‐14.5) | 8.1 (7.3‐9.1) | 12.1 (10.2‐14.2) |
| Black | 112 | 33.2 (25.7‐41.1) | 20.3 (17.5‐23.3) | 13.3 (11.2‐15.7) | 9.3 (7.2‐11.6) | 21.5 (16.2‐27.5) |
| Latinx | 113 | 28.6 (21.6‐36.2) | 20.3 (17.0‐23.8) | 13.3 (11.5‐15.3) | 10.7 (9.0‐12.6) | 25.6 (20.7‐30.8) |
| Asian | 73 | 51.3 (43.0‐59.6) | 24.7 (22.3‐27.3) | 11.1 (8.3‐14.2) | 6.5 (4.7‐8.5) | 5.6 (2.4‐10.2) |
| Indigenous/Native American | 61 | 20.6 (10.7‐32.7) | 11.3 (4.5‐20.8) | 13.3 (9.6‐17.7) | 12.9 (8.7‐17.9) | 40.8 (23.1‐59.8) |
| Any minoritized group | 148 | 31.2 (22.8‐40.3) | 18.5 (15.4‐22.0) | 12.2 (10.1‐14.5) | 9.60 (7.7‐11.7) | 26.6 (21.0‐32.6) |
| Household income | ||||||
| Low | 32 | 17.4 (13.3‐21.9) | 15.7 (12.6‐19.0) | 13.3 (11.9‐14.7) | 11.3 (9.9‐12.8) | 40.5 (32.9‐48.4) |
| Mid‐to‐high | 15 | 38.2 (37.6‐38.8) | 23.4 (23.1‐23.7) | 13.4 (13.4‐13.4) | 8.9 (8.8‐9.0) | 16.0 (15.4‐16.7) |
| Sociodemographic and health‐related variables | ||||||
| Unhoused | 7 | 11.6 (10.2‐13.1) | 9.1 (7.8‐10.5) | 10.0 (9.3‐10.8) | 9.6 (8.0‐11.2) | 59.7 (56.8‐62.4) |
| Substance abuse/addiction | 11 | 15.8 (13.5‐18.3) | 13.0 (11.4‐14.8) | 12.7 (1.6‐13.7) | 11.1 (10.1‐12.1) | 55.2 (45.5‐64.8) |
| History of offending/criminality | 13 | 22.1 (12.5‐33.5) | 19.7 (14.6‐25.4) | 13.3 (11.9‐14.7) | 10.2 (8.4‐12.1) | 31.8 (17.0‐48.8) |
| History of a mental health condition | 10 | 15.0 (11.0‐19.4) | 12.6 (8.4‐17.5) | 12.2 (9.4‐15.3) | 11.0 (10.0‐12.0) | 47.5 (34.4‐60.7) |
| Assessment method | ||||||
| Questionnaire | 186 | 39.9 (35.8‐43.1) | 22.1 (20.1‐24.1) | 12.8 (11.7‐14.0) | 8.6 (7.9‐9.2) | 15.8 (14.5‐17.1) |
| Other methodologies | 15 | 34.3 (21.2‐48.7) | 20.5 (18.2‐23.0) | 13.1 (11.0‐15.3) | 9.5 (7.1‐12.2) | 19.8 (11.1‐30.2) |
| Study quality | ||||||
| Below average (mean: –1 SD) | 208 | 38.5 (37.1‐39.9) | 22.9 (21.7‐24.1) | 13.1 (12.4‐13.7) | 8.6 (8.2‐9.1) | 16.3 (15.1‐17.6) |
| Above average (mean: +1 SD) | 208 | 40.5 (34.0‐47.2) | 21.0 (18.2‐24.1) | 12.4 (10.6‐14.4) | 8.5 (7.2‐9.8) | 15.3 (12.8‐17.9) |
Figure 2.
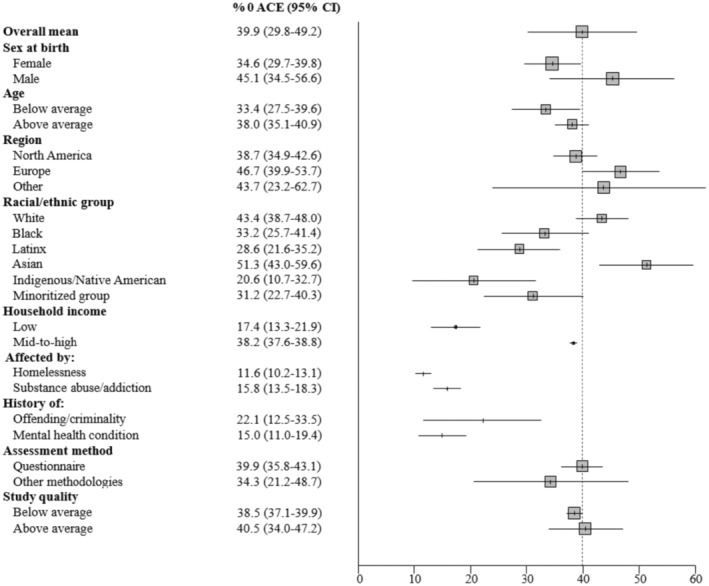
Forest plot of the prevalence of no adverse childhood experience (ACE). The overall mean prevalence of 0 ACE is displayed alongside the mean prevalence of 0 ACE for different levels of categorical moderators, and below and above average values for continuous moderators. Error bars represent 95% CIs.
Figure 3.
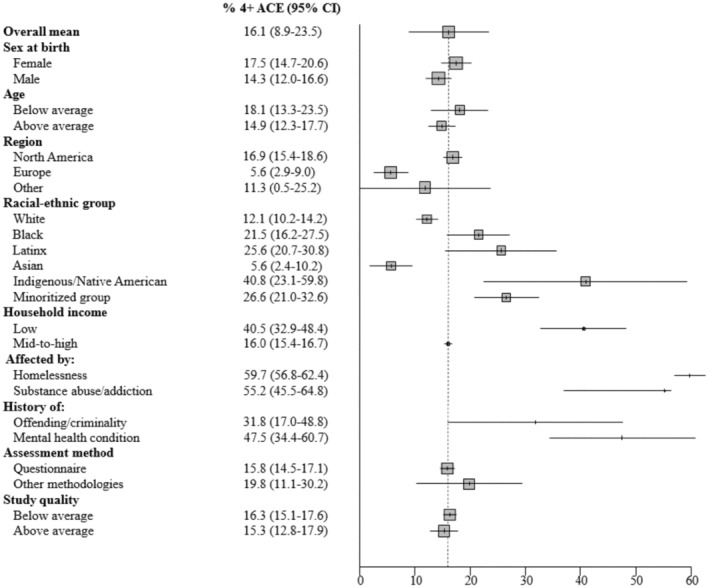
Forest plot of the prevalence of 4+ adverse childhood experiences (ACEs). The overall mean prevalence of 4+ ACEs is displayed alongside the mean prevalence of 4+ ACEs for different levels of categorical moderators, and below and above average values for continuous moderators. Error bars represent 95% CIs.
The pooled prevalence of the five levels of ACEs was derived from 208 unique samples of adults and can be summarized as follows: 39.9% (95% CI: 29.8‐49.2) for no ACE; 22.4% (95% CI: 14.1‐30.6) for one ACE; 13.0% (95% CI: 6.5‐19.8) for two ACEs; 8.7% (95% CI: 3.4‐14.5) for three ACEs; and 16.1% (95% CI: 8.9‐23.5) for four or more ACEs.
Between‐study heterogeneity was moderate in magnitude for the prevalence of no ACE (τ=24.3%; 95% CI: 21.9‐27.2) and four or more ACEs (τ=23.4%; 95% CI: 21.1‐26.2), whereas it was small in magnitude for the prevalence of one ACE (τ=10.9%; 95% CI: 9.9‐12.2), two ACEs (τ=7.8%; 95% CI: 7.1‐8.7), and three ACEs (τ=9.5%; 95% CI: 8.6‐10.6).
Ratios of prevalence proportions for the five levels of ACEs between different values of the categorical and continuous moderators are displayed in Table 2. There was strong evidence that the prevalence of 4+ ACEs was substantially larger in populations from low vs. mid‐to‐high income households (ratio: 1.21; 95% CI: 1.15‐1.28); unhoused individuals (ratio: 1.38; 95% CI: 1.35‐1.41); and people with a history of a mental health condition (ratio: 1.27; 95% CI: 1.17‐1.39), or with substance abuse or addiction (ratio: 1.34; 95% CI: 1.26‐1.43). There was also strong evidence that the prevalence of 0 ACE was substantially lower for persons from low‐income households (ratio: 0.85; 95% CI: 0.82‐0.88), unhoused individuals (ratio: 0.80; 95% CI: 0.78‐0.82), and people with a history of a mental health condition (ratio: 0.82; 95% CI: 0.79‐0.86), or with substance abuse or addiction (ratio: 0.83; 95% CI: 0.80‐0.86).
Table 2.
Moderation of prevalence of the five levels of adverse childhood experiences (ACEs)
| Ratio (95% CI) | |||||
|---|---|---|---|---|---|
| Moderators | 0 ACE | 1 ACE | 2 ACEs | 3 ACEs | 4+ ACEs |
| Sex at birth | 1.08 (0.99‐1.17) ↑ | 0.97 (0.93‐1.01) | 0.97 (0.95‐1.00) | 0.99 (0.97‐1.01) | 1.03 (1.00‐1.06) |
| Age | 1.03 (0.98‐1.09) | 1.02 (1.00‐1.03) | 0.99 (0.98‐1.00) | 0.99 (0.97‐1.01) | 0.97 (0.93‐1.02) |
| Region | |||||
| North America | 0.97 (0.91‐1.04) | 0.99 (0.96‐1.02) | 1.00 (0.98‐1.01) | 1.01 (0.99‐1.02) | 1.05 (1.02‐1.09) |
| Europe | 1.03 (0.95‐1.12) | 1.02 (0.99‐1.06) | 0.99 (0.97‐1.01) | 0.99 (0.96‐1.03) | 0.95 (0.91‐0.99) |
| Europe/North America | 1.06 (1.00‐1.12) | 1.03 (1.00‐1.06) | 0.99 (0.97‐1.01) | 0.99 (0.96‐1.02) | 0.90 (0.87‐0.93) ↓ |
| Racially/ethnically minoritized | |||||
| Black | 0.95 (0.89‐1.02) | 0.99 (0.96‐1.02) | 1.01 (0.98‐1.03) | 1.01 (0.99‐1.03) | 1.05 (1.00‐1.10) |
| Latinx | 0.91 (0.85‐0.97) ↓ | 0.99 (0.95‐1.03) | 1.01 (0.99‐1.03) | 1.02 (1.01‐1.04) | 1.09 (1.04‐1.14) ↑ |
| Asian | 1.07 (0.97‐1.18) ↑ | 1.05 (1.01‐1.09) | 1.00 (0.96‐1.03) | 0.98 (0.96‐1.01) | 0.89 (0.85‐0.94) ↓ |
| Indigenous/Native American | 0.88 (0.80‐0.96) ↓ | 0.91 (0.84‐0.98) ↓ | 1.00 (0.94‐1.04) | 1.04 (1.00‐1.08) | 1.20 (1.05‐1.37) ↑ |
| Any minoritized group | 0.92 (0.85‐0.99) ↓ | 0.96 (0.93‐0.99) | 0.99 (0.97‐1.01) | 1.01 (0.99‐1.03) | 1.13 (1.08‐1.19) ↑ |
| Household income | 0.85 (0.82‐0.88) ↓ | 0.94 (0.91‐0.96) | 1.00 (0.99‐1.01) | 1.02 (1.01‐1.04) | 1.21 (1.15‐1.28) ↑ |
| Sociodemographic and health‐related variables | |||||
| Unhoused | 0.80 (0.78‐0.82) ↓ | 0.89 (0.88‐0.91) ↓ | 0.98 (0.96‐0.99) | 1.01 (0.99‐1.03) | 1.38 (1.35‐1.41) ↑ |
| Substance abuse/addiction | 0.83 (0.80‐0.86) ↓ | 0.93 (0.91‐0.95) | 1.00 (0.99‐1.01) | 1.02 (1.01‐1.03) | 1.34 (1.26‐1.43) ↑ |
| History of offending/criminality | 0.88 (0.80‐0.96) ↓ | 0.98 (0.94‐1.03) | 1.00 (0.99‐1.02) | 1.02 (1.00‐1.03) | 1.14 (1.01‐1.28) ↑ |
| History of a mental health condition | 0.82 (0.79‐0.86) ↓ | 0.92 (0.88‐0.96) ↓ | 0.99 (0.97‐1.02) | 1.02 (1.01‐1.03) | 1.27 (1.17‐1.39) ↑ |
| Assessment method | 1.04 (0.93‐1.15) | 1.01 (0.99‐1.04) | 1.00 (0.98‐1.02) | 0.99 (0.97‐1.02) | 0.97 (0.89‐1.05) |
| Study quality | 1.01 (0.97‐1.06) | 0.99 (0.96‐1.01) | 0.99 (0.98‐1.01) | 1.00 (0.99‐1.01) | 0.99 (0.97‐1.02) |
Arrows indicate effects where the chances of a substantial and slight moderating association were respectively >25% and <95%. Bold prints indicate effects where the chances of a substantial and slight moderating association were respectively >95% and <5%. Concerning sex, the prevalence for males was divided by that for females. As to age, the prevalence for studies with above average values (mean: +1 SD) was divided by that for studies with below average values (mean: –1 SD). Concerning region, the prevalence for studies from North America or Europe was divided by that for studies from other regions, and the prevalence for studies from Europe was divided by that for studies from North America. The prevalence for each minoritized group was divided by that for people identifying as White. The prevalence for samples from low‐income households was divided by that for samples from mid‐to‐high income households. The prevalence for samples of persons with homelessness, substance abuse or addiction, or a history of a mental health condition or offending/criminality was divided by that for samples of persons without such profiles. The prevalence for studies of ACEs collected using a questionnaire was divided by that for studies using other methodologies. As to study quality, the prevalence for studies with above average values (mean: +1 SD) was divided by that for studies with below average values (mean: –1 SD).
There was good evidence that the prevalence of 4+ ACEs was higher in racially‐ethnically minoritized groups, particularly when comparing study estimates for people identifying as Indigenous/Native American to those identifying as White or Asian (ratio: 1.20; 95% CI: 1.05‐1.37). There was also good evidence that the prevalence of 0 ACE was lower for samples of individuals involved in the criminal justice system (ratio: 0.88; 95% CI: 0.80‐0.96). There was some evidence that the prevalence of 4+ ACEs was higher for Latinx persons (vs. persons of Caucasian heritage) and those with a history of offending or criminality. Finally, there was some evidence that the prevalence of 0 ACE was higher among males (vs. females), and lower in samples from Europe compared to North America.
There was weak evidence to suggest that the prevalence of 0 or 4+ ACEs differed between assessment methods. There was strong evidence that age‐ and study quality‐related differences in the prevalence of each ACE category were only slight.
DISCUSSION
In this meta‐analysis of 206 studies (208 prevalence estimates), representing 546,458 adult participants across 22 countries, the prevalence of ACEs was 39.9% for no ACE, 22.4% for one ACE, 13.0% for two ACEs, 8.7% for three ACEs, and 16.1% for four or more ACEs. Thus, six out of ten adults report having experienced at least one ACE, and one in six report exposure to four or more ACEs prior to age 18.
Although these data suggest that ACEs are common, we also found considerable disparities across the population. Specifically, there was strong evidence of differences in the prevalence of 4+ ACEs across samples with different sociodemographic, economic and health‐related profiles (in particular, racial/ethnic features, household income, and history of a mental health condition or substance abuse/addiction).
Exposure to ACEs can lead to intense and prolonged activation of the stress response, which can impact brain development, as well as cognitive, social and emotional functioning in childhood. Adoption of risky behaviours, such as substance misuse, can then occur, which can exacerbate later‐life health problems (e.g., cardiovascular, lung, liver and respiratory diseases; cancer, hypertension, diabetes), leading to premature death. In addition, research suggests that ACEs can “get under the skin” and be transmitted to the next generation, thereby perpetuating intergenerational cycles of risk 21 .
However, the occurrence of ACEs does not necessarily predict problematic outcomes for all victims, especially if they experience safe, stable and nurturing relationships at the family or community levels 22 . For example, neighbourhood collective efficacy has been shown to moderate the association between ACEs and marital discord, whereby individuals with high ACE scores had lower levels of marital discord when exposed to high levels of neighbourhood social cohesion and support 23 . Thus, protective factors can reduce or even offset the consequences of ACEs.
Our moderation analysis demonstrated that the prevalence of 4+ ACEs was greater among individuals with a history of a mental health condition, and with substance abuse or addiction. For example, we found that 55.2% of individuals with substance abuse or addiction had 4+ ACEs, whereas the prevalence of 4+ ACEs in the general population was 16.1%. The association between ACEs and risky substance use or addiction may be mediated by emotional dysregulation 24 . Further, substance abuse and addiction are known behavioural mechanisms by which ACEs precipitate involvement in the criminal justice system 25 . In general, there are both direct and indirect pathways by which early adversity can contribute to mental health and social challenges in adulthood. More research focused on these developmental pathways is critical to identify opportunities for intervention leading to better‐than‐expected outcomes.
Our moderation analysis also showed that the prevalence of 4+ ACEs was higher in samples of unhoused individuals (59.7%), which is consistent with the recent findings by Liu et al 8 . Moreover, on average, the prevalence of 4+ ACEs in samples of White persons was 12.1%, whereas the corresponding prevalence for samples of Black (21.5%), Latinx (25.6%), and Indigenous/Native American (40.8%) persons was substantially higher. Beyond ACEs, minoritized groups in Western countries have also experienced historical, structural and economic inequalities, oppression, discrimination and poverty, that could perpetuate ACEs and initiate intergenerational cycles of adversity 7 . Future research should focus on such disparities in ACEs, which could add valuable insight into population health.
Consistency of instrumentation in the measurement of ACEs was a requirement and is a strength of this systematic review and meta‐analysis. Such consistency underpinned a valid quantitative synthesis and robust estimation of the prevalence of ACEs across many studies, in addition to an extensive set of moderation analyses. However, to ensure consistency, only studies that used the 8‐ or 10‐item ACE Questionnaire (±2 items) were included in our analysis. Although the vast majority of ACE studies employed these two versions, excluding studies using <6‐ or >12‐item versions was methodologically necessary, but is still a limitation of this systematic review.
Further limitations relating to representativeness should be mentioned. Although included studies were from 22 countries across all continents, most were from North America and Europe (>90%). Thus, further studies in Asia, Australia/New Zealand, South America, the Caribbean and Africa are needed to ensure better generalizability of ACE prevalence estimates. Moreover, few studies have been conducted in low‐ and middle‐income countries, with a very high variability observed in the prevalence of 4+ ACEs (from 6.75% to 88.31%). More studies on ACEs are needed in these countries, and their consequences should be investigated in the context of global health research.
There were also too few studies with ACE prevalence estimates in samples representing the lesbian, gay, bisexual, transgender, queer, intersexual, asexual and two‐spirited (LGBTQIA2+) community. Therefore, new studies of ACEs in this community, such as the one recently published in this journal 26 , should be encouraged and welcomed to enable further exploration of gender and sexual identity as potential moderators of the impact of childhood adversity.
Efforts to mitigate the impact of ACEs are focused on screening for these experiences when interfacing with patients as part of routine care. However, there are cautions around ACE screening, especially when encounters with patients are brief and few resources are available following disclosure 27 . Specifically, it is recommended that ACE screening be optional, to give patients choice on what they discuss and disclose, and that screening only occurs in combination with trauma‐informed practice 28 .
Trauma‐informed practice requires having personnel who are sensitive to the impacts of adversity, recognize how the signs and symptoms of toxic stress manifest in individuals, integrate knowledge of ACEs and their impacts into their work practice, and can actively resist harm or re‐traumatization (e.g., having trust violated, or experiences minimized) 28 . Clinicians need to be particularly aware of the complex issues that may surround trauma‐informed care, including systemic oppression, racism, and intersecting identities 29 . A recent study 30 showed that the adoption of trauma‐informed practice in a maternity clinic was associated with fewer infant delivery complications and health risks at birth. However, future research is needed to determine the effectiveness of trauma‐informed approaches across various contexts, such as paediatric settings, schools, and justice systems.
In conclusion, ACEs are common, represent a threat to individual well‐being and societal prosperity, and should be a key public health priority. Several efforts are underway globally to mitigate ACEs and their impacts. Their prevention through universal and targeted policies that optimize early child development is critical.
It has been documented that fewer social and material resources within families are among the strongest predictors of childhood maltreatment 31 . As such, social policies that reduce income inequalities and increase social welfare, access to affordable education, higher‐paying employment opportunities, and supportive parenting policies (i.e., paid parental leave, supportive family work policies), are likely to help mitigate collective exposure to childhood adversity.
With regard to targeted prevention, the implementation and scaling up of evidence‐based interventions for preventing exposure to childhood maltreatment are needed. Home visitation programs and parent coaching interventions – particularly in families at high risk – have been identified as effective deterrents of abuse at home and child maltreatment 31 .
A multi‐pronged strategy using universal and targeted approaches to prevent maltreatment has the greatest chance to improve long‐term outcomes.
ACKNOWLEDGEMENTS
This study has been funded by the Alberta Children's Hospital Research Foundation, the Mathison Centre for Mental Health, the Owerko Centre, the Faculty of Arts and the Cumming School of Medicine at the University of Calgary, and an anonymous donor. The authors thank C. Nickel, who conducted the literature search. Supplementary information on this study is available at https://osf.io/bhcd4.
REFERENCES
- 1. Felitti VJ, Anda RF, Nordenberg D. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med 1998;14:245‐58. [DOI] [PubMed] [Google Scholar]
- 2. Hughes K, Bellis MA, Hardcastle KA et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta‐analysis. Lancet Public Health 2017;2:e356‐66. [DOI] [PubMed] [Google Scholar]
- 3. Hughes K, Ford K, Bellis MA et al. Health and financial costs of adverse childhood experiences in 28 European countries: a systematic review and meta‐analysis. Lancet Public Health 2021;6:e848‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Merrick MT, Ford DC, Ports KA et al. Prevalence of adverse childhood experiences from the 2011‐2014 Behavioral Risk Factor Surveillance System in 23 states. JAMA Pediatr 2018;172:1038‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nurius PS, Green S, Logan‐Greene P et al. Stress pathways to health inequalities: embedding ACEs within social and behavioral contexts. Int Public Health J 2016;8:241‐56. [PMC free article] [PubMed] [Google Scholar]
- 6. Mersky JP, Choi C, Plummer Lee C et al. Disparities in adverse childhood experiences by race/ethnicity, gender, and economic status: intersectional analysis of a nationally representative sample. Child Abuse Negl 2021;117:105066. [DOI] [PubMed] [Google Scholar]
- 7. Assini‐Meytin LC, Fix RL, Green KM et al. Adverse childhood experiences, mental health, and risk behaviors in adulthood: exploring sex, racial, and ethnic group differences in a nationally representative sample. J Child Adolesc Trauma 2022;15:833‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu M, Luong L, Lachaud J et al. Adverse childhood experiences and related outcomes among adults experiencing homelessness: a systematic review and meta‐analysis. Lancet Public Health 2021;6:e836‐47. [DOI] [PubMed] [Google Scholar]
- 9. Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Heart, Lung and Blood Institute . Quality assessment tool for observational cohort and cross‐sectional studies. Bethesda: National Heart, Lung and Blood Institute, 2014. [Google Scholar]
- 11. Barendregt JJ, Doi SA, Lee YY et al. Meta‐analysis of prevalence. J Epidemiol Community Health 2013;67:974. [DOI] [PubMed] [Google Scholar]
- 12. Barendregt JJ, Doi SA. MetaXL user guide: Version 5.3. Sunrise Beach: EpiGear International Pty Ltd, 2022. [Google Scholar]
- 13. Higgins JPT. Commentary: Heterogeneity in meta‐analysis should be expected and appropriately quantified. Int J Epidemiol 2008;37:1158‐60. [DOI] [PubMed] [Google Scholar]
- 14. Gelman A. Scaling regression inputs by dividing by two standard deviations. Stat Med 2008;27:2865‐73. [DOI] [PubMed] [Google Scholar]
- 15. Cohen J. Statistical power analysis for the behavioral sciences. London: Routledge, 2013. [Google Scholar]
- 16. Hopkins WG. Individual responses made easy. J Appl Physiol 2015;118:1444‐6. [DOI] [PubMed] [Google Scholar]
- 17. Cumming G. The new statistics: why and how. Psychol Sci 2013;25:7‐29. [DOI] [PubMed] [Google Scholar]
- 18. Hopkins WG. Replacing statistical significance and non‐significance with better approaches to sampling uncertainty. Front Physiol 2022;13:962132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rothman KJ. Epidemiology: an introduction. New York: Oxford University Press, 2012. [Google Scholar]
- 20. Patsopoulos NA, Evangelou E, Ioannidis JPA. Sensitivity of between‐study heterogeneity in meta‐analysis: proposed metrics and empirical evaluation. Int J Epidemiol 2008;37:1148‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Madigan S, Wade M, Plamondon A et al. Maternal adverse childhood experience and infant health: biomedical and psychosocial risks as intermediary mechanisms. J Pediatr 2017;187:282‐9.e281. [DOI] [PubMed] [Google Scholar]
- 22. Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta‐analysis. J Adolesc Health 2013;53(Suppl. 4):S32‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Madigan S, Wade M, Plamondon A et al. Neighborhood collective efficacy moderates the association between maternal adverse childhood experiences and marital conflict. Am J Community Psychol 2016;57:437‐47. [DOI] [PubMed] [Google Scholar]
- 24. Espeleta HC, Brett EI, Ridings LE et al. Childhood adversity and adult health‐risk behaviors: examining the roles of emotion dysregulation and urgency. Child Abuse Negl 2018;82:92‐101. [DOI] [PubMed] [Google Scholar]
- 25. Weber S, Lynch S. Understanding the relations among adverse childhood experiences (ACE), substance use, and reoffending among detained youth. Child Abuse Neglect 2021;120:105211. [DOI] [PubMed] [Google Scholar]
- 26. Andresen JB, Graugaard C, Andersson M et al. Adverse childhood experiences and mental health problems in a nationally representative study of heterosexual, homosexual and bisexual Danes. World Psychiatry 2022;21:427‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Racine N, Killam T, Madigan S. Trauma‐informed care as a universal precaution: beyond the Adverse Childhood Experiences Questionnaire. JAMA Pediatr 2020;174:5‐6. [DOI] [PubMed] [Google Scholar]
- 28. Substance Abuse and Mental Health Services Administration . SAMHSA's concept of trauma and guidance for a trauma‐informed approach. Rockville: Substance Abuse and Mental Health Services Administration, 2014. [Google Scholar]
- 29. Cénat JM. Complex racial trauma: evidence, theory, assessment, and treatment. Perspect Psychol Sci 2023;18:675‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Racine N, Ereyi‐Osas W, Killam T et al. Maternal‐child health outcomes from pre‐ to post‐implementation of a trauma‐informed care initiative in the prenatal care setting: a retrospective study. Children 2021;8:1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van IJzendoorn MH, Bakermans‐Kranenburg MJ, Coughlan B et al. Annual Research Review: Umbrella synthesis of meta‐analyses on child maltreatment antecedents and interventions: differential susceptibility perspective on risk and resilience. J Child Psychol Psychiatry 2020;61:272‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]


