Abstract
This study aimed to identify the 20‐year trajectories of positive and negative symptoms after the first psychotic episode in a sample of patients with an ICD‐10 diagnosis of schizophrenia spectrum disorder, and to investigate the baseline characteristics and long‐term outcomes associated with these trajectories. A total of 373 participants in the OPUS trial were included in the study. Symptoms were assessed at baseline and after 1, 2, 5, 10 and 20 years using the Scales for the Assessment of Positive and Negative Symptoms. We used latent class growth mixture modelling to identify trajectories, and multinominal regression analyses to investigate predictors of membership to identified trajectories. Five trajectories of positive symptoms were identified: early continuous remission (50.9% of the sample), stable improvement (18.0%), intermittent symptoms (10.2%), relapse with moderate symptoms (11.9%), and continuous severe symptoms (9.1%). Substance use disorder (odds ratio, OR: 2.83, 95% CI: 1.09‐7.38, p=0.033), longer duration of untreated psychosis (OR: 1.02, 95% CI: 1.00‐1.03, p=0.007) and higher level of negative symptoms (OR: 1.60, 95% CI: 1.07‐2.39, p=0.021) were predictors of the relapse with moderate symptoms trajectory, while only longer duration of untreated psychosis (OR: 1.01, 95% CI: 1.00‐1.02, p=0.030) predicted membership to the continuous severe symptoms trajectory. Two trajectories of negative symptoms were identified: symptom remission (51.0%) and continuous symptoms (49.0%). Predictors of the continuous symptoms trajectory were male sex (OR: 3.03, 95% CI: 1.48‐6.02, p=0.002) and longer duration of untreated psychosis (OR: 1.01, 95% CI: 1.00‐1.02, p=0.034). Trajectories displaying continuous positive and negative symptoms were linked to lower neurocognition, as measured by the Brief Assessment of Cognition in Schizophrenia (BACS) (z‐score: –0.78, CI: –1.39 to –0.17, for continuous positive symptoms; z‐score: –0.33, CI: –0.53 to –0.13, for continuous negative symptoms). The same trajectories were also linked to higher use of antipsychotic medication at 20‐year follow‐up (continuous positive symptoms: 78%; continuous negative symptoms: 67%). These findings suggest that the majority of patients with first‐episode schizophrenia spectrum disorder have a trajectory with early stable remission of positive symptoms. Long duration of untreated psychosis and comorbid substance abuse are modifiable predictors of poor trajectories for positive symptoms in these patients. In about half of patients, negative symptoms do not improve over time. These symptoms, in addition to being associated with poor social and neurocognitive functioning, may prevent patients from seeking help.
Keywords: First‐episode psychosis, schizophrenia spectrum disorder, positive symptoms, negative symptoms, trajectories of symptoms, predictors of symptom trajectories, social functioning, neurocognition
Schizophrenia affects roughly 1‐2% of the world's population 1 , 2 and is a leading cause of disability worldwide 3 . The disorder often has its onset early in life and is associated with long‐term impairments of social and occupational functioning 4 , and with significant adversities to both patients and their relatives.
The evolution of the disorder can vary between patients 5 . Some are affected by chronic symptoms, while others experience phases of remission or full recovery 6 , 7 , 8 . The main clinical manifestations are positive and negative symptoms, but patients may also exhibit cognitive deficits and experience a wide range of other subjective symptoms 9 , 10 . This means that the large group of patients collectively diagnosed with a schizophrenia spectrum disorder experience different patterns of illness course, some much worse than others. Latent class models and growth mixture modeling enable today the identification of clusters of individuals with specific trajectories of symptoms 11 , allowing to explore their sociodemographic, clinical and social functioning correlates.
Studies conducted in the 20st century reported great heterogeneity in the course of illness among first‐episode psychosis patients 12 , 13 . Their cross‐sectional design provided valuable knowledge on levels of psychopathology at specific timepoints, but no information on illness manifestation over time. Research collecting longitudinal data has contributed to a better understanding of the course of illness. The Suffolk County Study explored trajectories of social functioning, reporting that 75% of patients with psychotic disorders had severe and persistent social impairments 14 . Other studies have determined symptom trajectories in schizophrenia, with follow‐ups ranging from weeks to a maximum of 10 years 10 . In these studies, most patients experienced early or delayed improvement of positive symptoms followed by stable symptom levels, while a large group of patients usually experienced only minimal improvement of negative symptoms 10 , 15 . These latter symptoms are of increasing interest, since patients with a persistence of these symptoms are at high risk of poor outcomes, such as social isolation, unemployment and poor health 16 , 17 . In addition, treatment options for persistent negative symptoms are scarce 18 , 19 . Poor symptom trajectories have been previously associated with some sociodemographic and clinical variables, such as male sex, poor premorbid functioning, substance abuse, and a schizophrenia diagnosis 20 , 21 .
Determining symptom trajectories in a modern‐day treatment environment and characterizing homogeneous subgroups of patients with schizophrenia spectrum disorder based on long‐term symptom levels is a research and clinical priority, as it might help the planning of treatment and possibly the identification of biological correlates. Identifying characteristics that predict chronic illness could also help target new integrated interventions.
The aim of this study was to identify 20‐year trajectories of positive and negative symptoms after the first psychotic episode in patients with an ICD‐10 diagnosis of schizophrenia spectrum disorder. We also examined if any baseline characteristics could predict illness trajectories, and explored whether specific illness trajectories were associated with clinical and functional outcomes after 20 years.
METHODS
Study design and participants
This 20‐year follow‐up study reassessed participants from the OPUS randomized controlled trial. Five hundred seventy‐eight participants with an incident schizophrenia spectrum diagnosis (ICD‐10 classification: F20‐F25, F28‐F29) were recruited between 1998 and 2000. Inclusion criteria were a first psychotic episode, age between 18 and 45 years, and not having received more than 12 weeks of continuous antipsychotic treatment. Patients were randomized to specialized early intervention treatment (comprised of assertive community treatment, family involvement, and psychoeducation) or treatment as usual 22 . All participants were given a comprehensive description of the study and provided written consent.
Patients were assessed at baseline and after 1, 2, 5, 10 and 20 years. Each follow‐up was conducted by independent clinical staff blinded to the original treatment allocation. Participants were assessed using semi‐structured face‐to‐face interviews followed by questionnaires. Regular sessions were conducted to secure high inter‐rater reliability in the use of the assessment instruments.
For this current study, we combined the two treatment groups into one large cohort, because our main aim was to explore heterogeneity in the development of positive and negative symptoms, and allocation to either specialized early intervention treatment or treatment as usual had been found not to affect clinical outcomes at 5 years 22 . In the 20‐year trajectory analysis, we included 373 participants with complete data on symptoms at baseline and follow‐up. Of these patients, 23 participated in two interviews, 31 in three interviews, 94 in four interviews, 132 in five interviews and 93 in all six interviews (see supplementary information).
Measures of positive and negative symptoms
Symptoms were assessed at baseline and after 1, 2, 5, 10 and 20 years using the Scale for the Assessment of Positive Symptoms (SAPS) 23 and the Scale for the Assessment of Negative Symptoms (SANS) 24 . For both dimensions, we calculated composite scores ranging from 0 to 5. The “positive dimension” was the mean score of the global ratings for hallucinations and delusions. The “negative dimension” was the mean score of all four global ratings of negative domains in the SANS 25 . We regarded a symptom score of 2 or less on all global ratings of symptoms as clinical remission 26 .
Baseline risk factors
The variables examined as possible baseline predictors of trajectory membership were: age; sex; main ICD‐10 diagnosis ascertained by the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) 27 ; diagnosis of substance use disorder ascertained using the same interview; global level of functioning measured by the Global Assessment of Functioning (GAF) scale (from 0, poor to 100, good) 28 ; negative, positive and disorganized symptoms assessed using the SANS and the SAPS and rated as a continuous variable from 0 to 5; allocation to either early intervention treatment or treatment as usual; completion or not of high school; premorbid social and academic functioning assessed using the Premorbid Adjustment Scale (PAS) 29 ; duration of untreated psychosis assessed by the Interview for Retrospective Assessment of Onset of Schizophrenia (IRAOS) 30 and defined as the number of months with at least one psychotic symptom definitely present until the initiation of treatment 31 .
Distal outcomes
We examined the association between trajectories of positive and negative symptoms and distal outcomes measured at the 20‐year follow‐up. The outcomes measured were: a) rate of recovery, defined as no psychotic episode, no psychiatric hospitalization and no use of supported housing in the past two years, being engaged in studying or working, and a present GAF score ≥60; b) for positive symptom trajectories, remission of negative symptoms; for negative symptom trajectories, remission of positive symptoms; c) social functioning assessed by the Personal and Social Performance (PSP) scale 32 , which measures four domains of social functioning (useful activities, personal relationships, self‐care, aggressive and disturbing behaviour), combined and rated with a score ranging from 0 to 100; d) cognitive functioning measured by the Brief Assessment of Cognition in Schizophrenia (BACS) 33 and reported as z‐score; e) current diagnosis of schizophrenia based on the SCAN interview; and f) current treatment with antipsychotic medication.
Statistical analysis
We applied latent growth mixture modelling (LGMM) and latent class growth analysis (LCGA) to estimate trajectories of positive and negative symptom dimensions 34 . These are data‐driven, person‐centered approaches, that identify population subgroups (classes) based on prototypical patterns in intercepts and slopes. To handle missing data, we applied the full information maximum likelihood approach 35 .
We estimated LGMM and LCGA models with different growth functions (i.e., linear, quadratic or cubic) and an increasing number of classes. We examined a number of model fit estimates and model features to select the model with the best fit of the data, including Akaike information criteria (AIC), Bayesian information criteria (BIC) and sample‐size adjusted BIC (adj. BIC), entropy of the model, class size and accuracy, and test of model fit with addition of an extra class by Lo‐Mendell‐Rubin and Vuong‐Lo‐Mendell‐Rubin likelihood ratio tests.
We tested baseline variables as predictors of class membership by applying the Three‐Step approach 36 , in which covariates are not included in the modelling of trajectories but treated as auxiliary variables, so that they do not influence the formation of trajectories. Therefore, class membership is established first, and subsequently predictors for membership of identified trajectories are examined. We first tested baseline variables univariably, and then included all significant covariates in a multivariable multinomial logistic regression model. Level of significance was set at p<0.05. The results are presented as odds ratios (OR) with 95% confidence intervals (95% CI) and corresponding p values. In order to examine the association between trajectory membership and distal outcomes, we used the Lanza method 37 . All statistical analyses were conducted in Mplus statistical software version 7.
RESULTS
Dropout analysis
A total of 373 participants were included in this study. In the dropout analysis, we found that participants did not differ from non‐participants with respect to baseline psychopathological characteristics (including the proportion of those with a diagnosis of schizophrenia and of substance use disorder, and the mean scores on the positive and negative dimensions), the median duration of untreated psychosis, the employment rate, the proportion of those who completed high school education, and the mean scores for premorbid social and academic functioning. Participants were slightly younger than non‐participants (26.2±6.2 vs. 27.8±6.8 years), were less frequently male (55.1% vs. 64.0%), had higher levels of global functioning (mean GAF score: 41.0±13.7 vs. 37.7±11. 9), and had higher rates of independent living (95.5% vs. 87.6%) (see also supplementary information).
Trajectories of positive symptoms
For positive symptoms, we estimated a series of linear, quadratic and cubic term LCGA and LGMM models from one to six classes (see supplementary information). We chose the five‐class model based on likelihood ratio tests indicating that it had a superior goodness of fit compared with the four‐class model. Entropy scores were high for both the four‐ and five‐class models (0.834 vs. 0.949), but the individual class accuracy scores in the five‐class model were higher (all above 0.95), expressing a better classification accuracy (see supplementary information).
We named the five positive symptom trajectories as follows: early continuous remission (50.9% of the sample), characterized by early and continuous remission of symptoms; stable improvement (18.0%), marked by a slower decrease of symptoms in the first five years followed by stabilization; intermittent symptoms (10.2%), characterized by relapse and remission of symptoms; relapse with moderate symptoms (11.9%), marked by improvement of symptoms in the first years followed by a slow but continuous increase of symptoms subsequently; and continuous severe symptoms (9.1%), characterized by a small decrease in symptoms in the first year followed by a stable continuous course of symptoms (see Figure 1).
Figure 1.
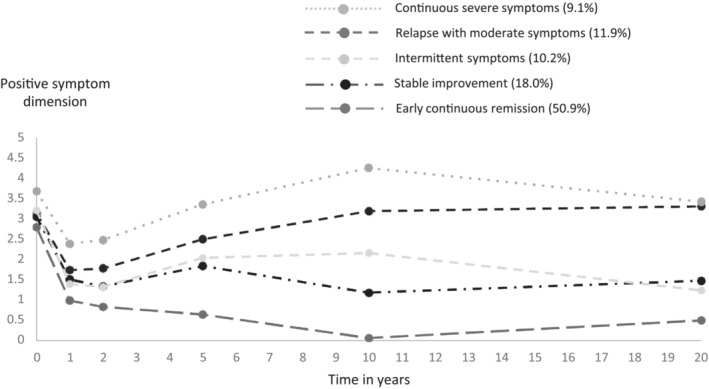
20‐year trajectories of positive symptoms after the first psychotic episode in patients with an ICD‐10 diagnosis of schizophrenia spectrum disorder
Trajectories of negative symptoms
For negative symptoms, we estimated a series of LCGA and LGMM models from one to five classes (see supplementary information). The two‐class LCGA model was chosen because it had higher entropy and class accuracies (both classes above 0.93) than models with additional classes (all class accuracies lower than 0.93). The two trajectories of negative symptoms were named symptom remission (51.0% of the sample), characterized by a low mean level of negative symptoms initially, followed by remission within the first two years, and continuous symptoms (49.0%), marked by a high mean level of negative symptoms at baseline and no changes over time (see Figure 2).
Figure 2.
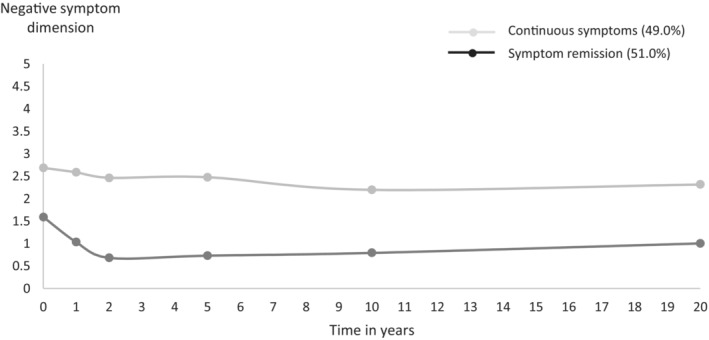
20‐year trajectories of negative symptoms after the first psychotic episode in patients with an ICD‐10 diagnosis of schizophrenia spectrum disorder
Baseline predictors of trajectory membership
Positive dimension
Using univariable multinomial logistic regression analysis, we first identified baseline characteristics associated with positive symptom trajectories using early continuous remission as a reference (see supplementary information). Significant predictors were then entered into multivariable analysis. Substance use disorder (OR: 2.83, 95% CI: 1.09‐7.38, p=0.033), longer duration of untreated psychosis (OR: 1.02, 95% CI: 1.00‐1.03, p=0.007), and higher level of negative symptoms (OR: 1.60, 95% CI: 1.07‐2.39, p=0.021) remained significant predictors of membership to the relapse with moderate symptoms trajectory, while only duration of untreated psychosis (OR: 1.01, 95% CI: 1.00‐1.02, p=0.030) predicted membership to the continuous severe symptoms trajectory. Male sex (OR: 3.69, 95% CI: 1.42‐9.58, p=0.007) predicted membership to the trajectory of intermittent symptoms (see Table 1).
Table 1.
Predictors of membership to positive symptom trajectories using patients with the early continuous remission trajectory as reference group
| Stable improvement | Intermittent symptoms | Relapse with moderate symptoms | Continuous severe symptoms | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Male | 1.01 (0.49‐2.08) | 0.977 | 3.69 (1.42‐9.58) | 0.007 | 2.47 (0.96‐6.38) | 0.061 | 0.84 (0.35‐2.03) | 0.697 |
| Completed high school | 1.24 (0.58‐2.67) | 0.575 | 0.36 (0.10‐1.25) | 0.108 | 0.51 (0.14‐1.83) | 0.301 | 0.74 (0.24‐2.29) | 0.602 |
| Employment | 1.32 (0.66‐2.66) | 0.437 | 0.67 (0.22‐2.02) | 0.483 | 0.46 (0.13‐1.73) | 0.253 | 0.49 (0.14‐1.69) | 0.257 |
| Substance use disorder | 0.90 (0.37‐2.16) | 0.806 | 0.75 (0.25‐2.28) | 0.747 | 2.83 (1.09‐7.38) | 0.033 | 2.05 (0.78‐5.40) | 0.148 |
| Poorer level of premorbid social functioning | 2.50 (0.49‐12.82) | 0.270 | 2.36 (0.17‐32.44) | 0.521 | 2.47 (0.24‐25.29) | 0.445 | 0.88 (0.04‐19.51) | 0.934 |
| Poorer level of premorbid academic functioning | 5.85 (0.67‐50.95) | 0.081 | 0.16 (0.01‐2.20) | 0.172 | 2.30 (0.11‐46.74) | 0.588 | 2.55 (0.09‐68.77) | 0.577 |
| Longer duration of untreated psychosis | 1.01 (1.00‐1.02) | 0.179 | 1.01 (1.00‐1.02) | 0.122 | 1.02 (1.00‐1.03) | 0.007 | 1.01 (1.00‐1.02) | 0.030 |
| Higher level of global functioning | 0.99 (0.96‐1.01) | 0.349 | 0.97 (0.93‐1.01) | 0.168 | 1.00 (0.96‐1.04) | 0.985 | 0.99 (0.95‐1.02) | 0.497 |
| Higher level of negative symptoms | 0.98 (0.72‐1.32) | 0.869 | 1.12 (0.69‐1.81) | 0.637 | 1.60 (1.07‐2.39) | 0.021 | 1.21 (0.80‐1.84) | 0.360 |
OR – odds ratio
Negative dimension
A similar univariable multinomial logistic regression analysis was conducted for predictors of negative symptom trajectories (see supplementary information). In multivariable analysis, male sex (OR: 3.03, 95% CI: 1.48‐6.02, p=0.002) and longer duration of untreated psychosis (OR: 1.01, 95% CI: 1.00‐1.02, p=0.034) increased the risk of belonging to the continuous symptoms trajectory compared with the symptom remission trajectory. Higher level of global functioning (OR: 0.95, 95% CI: 0.92‐0.98, p=0.001) and finishing high school (OR: 0.41, 95% CI: 0.17‐1.00, p=0.049) were associated with lower risk of belonging to the continuous symptoms trajectory (see Table 2).
Table 2.
Predictors of membership to negative symptom trajectories using patients with the symptom remission trajectory as reference group
| Continuous symptoms | ||
|---|---|---|
| OR (95% CI) | p | |
| Male | 3.03 (1.48‐6.02) | 0.002 |
| Finishing high school | 0.41 (0.17‐1.00) | 0.049 |
| Employment | 0.83 (0.36‐1.88) | 0.652 |
| Schizophrenia diagnosis at baseline | 2.09 (0.90‐4.85) | 0.085 |
| Poorer level of premorbid social function | 3.27 (0.45‐23.84) | 0.240 |
| Poorer level of premorbid academic functioning | 2.57 (0.28‐23.54) | 0.403 |
| Longer duration of untreated psychosis | 1.01 (1.00‐1.02) | 0.034 |
| Higher level of global functioning | 0.95 (0.92‐0.98) | 0.001 |
| Higher level of disorganized symptoms | 1.52 (0.94‐2.44) | 0.085 |
OR – odds ratio
Associations between trajectory membership and distal outcomes
Positive dimension
Social functioning scores at the 20‐year follow‐up were significantly higher in patients with the early continuous remission trajectory (mean PSP score: 60.7, CI: 57.6‐63.8) and the stable improvement trajectory (mean PSP score: 59.0, CI: 52.7‐65.3) compared to those with the other trajectories (mean PSP scores between 40.4 and 47.9). Patients with the early continuous remission trajectory had a significantly higher recovery rate (22%) than those with the other trajectories. Neurocognitive function was significantly more impaired in patients with the continuous severe symptoms trajectory (z‐score: –0.78, CI: –1.39 to –0.17) than in those with the early continuous remission, stable improvement and intermittent symptoms trajectories (see Table 3).
Table 3.
Associations between trajectories of positive symptoms and distal outcomes at 20‐year follow‐up
| Early continuous remission (ECR) | Stable improvement (SI) | Intermittent symptoms (IS) | Relapse with moderate symptoms (RMS) | Continuous severe symptoms (CSS) | p (interclass X2) | Significant differences between classes (p<0.05) | |
|---|---|---|---|---|---|---|---|
| Current treatment with antipsychotics | 48% | 49% | 62% | 80% | 78% | 0.040 | ECR vs. RMS and CSS |
| Current schizophrenia diagnosis | 55% | 78% | 51% | 90% | 85% | 0.002 | ECR vs. RMS, CSS and SI |
| Remission of negative symptoms | 51% | 53% | 22% | 9% | 30% | 0.003 | ECR and SI vs. RMS |
| Clinical recovery | 22% | 15% | 16% | 0 | 0 | <0.001 | ECR vs. RMS and CSS |
| Social functioning, mean PSP score (CI) | 60.7 (57.6‐63.8) | 59.0 (52.7‐65.3) | 44.8 (36.6‐53.0) | 40.4 (33.4‐48.2) | 47.9 (40.5‐55.3) | <0.001 | ECR and SI vs. RMS, CSS and IS |
| Cognitive function, BACS z‐score (CI) | −0.10 (−0.32 to 0.12) | 0.31 (−0.06 to 0.68) | 0.25 (−0.44 to 0.94) | −0.42 (−1.18 to 0.34) | −0.78 (−1.39 to −0.17) | 0.029 | CSS vs. ECR, SI and IS |
PSP – Personal and Social Performance scale, BACS – Brief Assessment of Cognition in Schizophrenia
The number of patients qualifying for a schizophrenia diagnosis at the 20‐year reassessment was significantly lower in patients with the early continuous remission trajectory (55%) than in those with the continuous severe symptoms, relapse with moderate symptoms and stable improvement trajectories. Remission of negative symptoms (all global SANS scores ≥2) was lower in patients with the relapse with moderate symptoms trajectory (9%) than in those with early continuous remission and stable improvement trajectories (51% and 53%, respectively). The probability of being on antipsychotic medication at the 20‐year follow‐up was higher for patients with the continuous severe symptoms (78%) and the relapse with moderate symptoms (80%) trajectories compared with the early continuous remission group (48%) (see Table 3).
Negative dimension
Social functioning scores at the 20‐year follow‐up were significantly higher in patients with the symptom remission trajectory (mean PSP score: 65.8, CI: 62.7‐68.9) than in those with the continuous symptoms trajectory (mean PSP score: 47.7, CI: 44.0‐51.4). Patients with the symptom remission trajectory had a significantly higher recovery rate (37%) than those with the continuous symptoms trajectory (0%). Neurocognitive function was more impaired in patients with the continuous symptoms trajectory (z‐score: –0.33, CI: –0.53 to –0.13) than in those with the symptom remission trajectory (z‐score: 0.36, CI: 0.16 to 0.56) (see Table 4).
Table 4.
Associations between trajectories of negative symptoms and distal outcomes at 20‐year follow‐up
| Symptom remission | Continuous symptoms | p (interclass X2) | |
|---|---|---|---|
| Current treatment with antipsychotics | 36% | 67% | <0.001 |
| Current schizophrenia diagnosis | 50% | 78% | <0.001 |
| Remission of negative symptoms | 84% | 41% | <0.001 |
| Clinical recovery | 37% | 0% | <0.001 |
| Social functioning, mean PSP score (CI) | 65.8 (62.7‐68.9) | 47.7 (44.0‐51.4) | <0.001 |
| Cognitive function, BACS z‐score (CI) | 0.36 (0.16‐0.56) | −0.33 (−0.53 to −0.13) | <0.001 |
PSP – Personal and Social Performance scale, BACS – Brief Assessment of Cognition in Schizophrenia
The number of patients qualifying for a schizophrenia diagnosis at the 20‐year reassessment was significantly lower in patients with the symptom remission trajectory (50%) than in those with continuous symptoms (78%). The probability of being on antipsychotic medication at the 20‐year follow‐up was significantly higher for patients with the continuous severe symptoms trajectory (67%) than in those with symptoms remission (36%) (see Table 4).
DISCUSSION
This study is the first to explore the trajectories of positive and negative symptoms over the 20‐year period following a first psychotic episode in patients with an ICD‐10 diagnosis of schizophrenia spectrum disorder.
We found five distinct trajectories of positive symptoms, characterized by early continuous remission (50.9%), stable improvement (18.0%), intermittent symptoms (10.2%), relapse with moderate symptoms (11.9%), and continuous severe symptoms (9.1%). So, about 69% of the sample did not have sustained positive symptoms. Similarly, in the AESOP 10‐year follow‐up study 38 , an improvement of positive symptoms was observed in 65% of patients. Moreover, in our study, patients with the intermittent symptoms trajectory had a mean SAPS score below 2 at the 20‐year follow‐up, suggesting that the proportion of the sample which did not experience significant positive symptoms at follow‐up was close to 80%. However, only the group with early continuous remission displayed a significantly higher recovery rate (22%) compared with patients with other trajectories. This finding supports the idea that early remission of positive symptoms is an indicator of a higher chance for recovery, as suggested by other long‐term follow‐up studies 4 , 39 .
Both patients with the relapse with moderate symptoms and the continuous severe symptoms trajectories showed a higher probability of being on antipsychotic medication at the 20‐year follow‐up than patients with other trajectories. This could be interpreted as a sign of treatment resistance. Indeed, these two trajectories accounted for about 20% of patients, similar to the rates of treatment‐resistant schizophrenia found in other studies 40 , 41 . We also found that these two trajectories were associated with lower social and neurocognitive function, and that these patients were less likely to show a remission of negative symptoms. This supports a division of schizophrenia into subgroups based on broader clinical features.
We found that longer duration of untreated psychosis, higher baseline levels of negative symptoms and a diagnosis of substance use disorder predicted membership to less favourable trajectories of positive symptoms. These baseline variables have previously been associated to poor outcome in schizophrenia 42 , 43 , 44 . It is noteworthy that they remain significant predictors of 20‐year trajectories. This emphasizes the importance of efforts to reduce the time before patients receive psychiatric treatment (promoting the development of early intervention services), and the need to address substance abuse timely and comprehensively (overcoming the current lack of integration between management of severe mental illness and substance abuse observed in several countries).
We found two trajectories of negative symptoms: symptom remission (51.0%) and continuous symptoms (49.0%). This finding differs from other studies, all with a follow‐up ranging between 1 and 10 years, which identified three or more trajectories, often including one with symptom remission 17 , 21 , 45 , 46 . In one of these studies 21 , 85% of patients achieved and maintained low levels of negative symptoms. A meta‐analysis also suggested that negative symptoms improve in the vast majority of outpatients after an initial schizophrenia spectrum diagnosis 47 . However, the Suffolk County 20‐year follow‐up study reported an average increase of negative symptoms over time 14 . So, the longer‐time perspective may explain the less favourable scenario observed in our sample. Moreover, according to the criteria suggested by Andreasen et al 26 , we regarded symptom levels above 2 on the SANS as defining a continuous negative symptoms trajectory. Other studies might have viewed such a level of symptoms as mild and categorized the relevant patients as being in remission.
Baseline predictors associated with membership to the continuous symptoms trajectory of negative symptoms were male sex, longer duration of untreated psychosis, lower level of global functioning, and not finishing high school. These baseline variables have previously been associated with poor outcomes in schizophrenia 43 , 48 , 49 . We further found the continuous symptoms trajectory to be associated with lower social and cognitive functioning at 20‐year follow‐up. This is in line with research showing that negative symptoms are associated with poor functional outcomes in schizophrenia 50 , 51 , 52 , 53 . The clinical recovery rate in the continuous symptoms trajectory was 0%, while it was 37% in the symptom remission trajectory, emphasizing the urgent need for the development of innovative multimodal interventions for this dimension of schizophrenia spectrum disorder.
The main limitation of this study is the relatively high dropout rate. Conducting long‐term follow‐up studies in this patient population is difficult, as patients with severe mental illness can be hard to reach. The European data protection law has also restricted the ways patients may be contacted, complicated the matter further. The participants in the 20‐year follow‐up did not differ from non‐participants with respect to any psychopathological variable, including the mean scores on positive and negative dimensions, but they had a slightly but significantly higher level of global functioning at baseline than those lost to follow‐up. So, our findings could potentially be biased towards a more positive direction. Moreover, some of the classes of positive symptoms were small in size, which affected power to determine predictors of class membership. Finally, the large time gap between the 10‐ and 20‐year follow‐up might have led to an oversimplification of symptom trajectories.
Our analyses are based on a sample of patients originally included in a randomized controlled trial. We know that the interventions impacted differentially on symptom levels for the first two years after inclusion, but we also know that this effect was not seen at any following assessment 22 , 54 , 55 . The inclusion of the treatment group in the analyses did not change the results, so we ruled out any significant impact of treatment on the trajectories.
In conclusion, our study is the first to identify 20‐year trajectories of positive and negative symptoms after a first psychotic episode in patients with schizophrenia spectrum disorder. We recruited participants from both inpatient and outpatient settings, making the study population representative of the real‐world schizophrenia spectrum population. Understanding the course of illness can help clinicians inform patients and their families about what can happen after the diagnosis has been made. Identifying different symptom trajectories after the initial diagnosis can improve the way we plan treatment 56 , 57 .
Our study suggests that a high proportion of patients with schizophrenia spectrum disorder recover from positive symptoms, but not from negative symptoms. These latter symptoms are associated with poor functioning and increased mortality 18 . Moreover, negative symptoms may prevent patients from seeking help. This could mean that a subgroup of patients with schizophrenia fall outside the treatment system, because they no longer require treatment for florid symptoms, and negative symptoms prevent them from seeking help for other health issues. The development of innovative multimodal treatment strategies for negative symptoms of schizophrenia spectrum disorder represents today an urgent priority.
ACKNOWLEDGEMENTS
The authors would like to thank L. Mariegaard, M. Birk and H.D. Jensen, who conducted a large number of clinical interviews in the 20‐year follow‐up. Moreover, they are grateful to the trial participants, who took time to share their stories and provided the clinical data for this study. The OPUS trial has been approved by the Regional Ethical Scientific Committee (protocol no. 17023873) and by the Danish data protection agency (RHP‐2017‐047, I‐Suite no. 05855), and registered at ClinicalTrials.gov (NCT00157313). The project was funded by unrestricted grants from the Lundbeck Foundation, Tryg Foundation and Helse Foundation. M. Starzer and H.G. Hansen are joint first authors of this paper. Supplementary information on the study can be found at https://drive.google.com/file/d/19s5TDJ0fQZ9O7I6ez6pau7m3EhRtqI7E/view.
REFERENCES
- 1. Saha S, Chant D, Welham J et al. A systematic review of the prevalence of schizophrenia. PLoS Med 2005;2:e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pedersen CB, Mors O, Bertelsen A et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry 2014;71:573‐81. [DOI] [PubMed] [Google Scholar]
- 3. James SL, Abate D, Abate KH et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990‐2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789‐858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Peritogiannis V, Gogou A, Samakouri M. Very long‐term outcome of psychotic disorders. Int J Soc Psychiatry 2020;66:633‐41. [DOI] [PubMed] [Google Scholar]
- 5. Lally J, Ajnakina O, Stubbs B et al. Remission and recovery from first‐episode psychosis in adults: systematic review and meta‐analysis of long‐term outcome studies. Br J Psychiatry 2017;211:350‐8. [DOI] [PubMed] [Google Scholar]
- 6. Jääskeläinen E, Juola P, Hirvonen N et al. A systematic review and meta‐analysis of recovery in schizophrenia. Schizophr Bull 2013;39:1296‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jobe TH, Harrow M. Long‐term outcome of patients with schizophrenia: a review. Can J Psychiatry 2005;50:892‐900. [DOI] [PubMed] [Google Scholar]
- 8. Hansen HG, Speyer H, Starzer M et al. Clinical recovery among individuals with a first‐episode schizophrenia an updated systematic review and meta‐analysis. Schizophr Bull 2023;49:297‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bottlender R, Strauß A, Möller HJ. Social disability in schizophrenic, schizoaffective and affective disorders 15 years after first admission. Schizophr Res 2010;116:9‐15. [DOI] [PubMed] [Google Scholar]
- 10. Habtewold TD, Rodijk LH, Liemburg EJ et al. A systematic review and narrative synthesis of data‐driven studies in schizophrenia symptoms and cognitive deficits. Transl Psychiatry 2020;10:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beunckens C, Molenberghs G, Verbeke G et al. A latent‐class mixture model for incomplete longitudinal Gaussian data. Biometrics 2008;64:96‐105. [DOI] [PubMed] [Google Scholar]
- 12. Sartorius N, Gulbinat W, Harrison G et al. Long‐term follow‐up of schizophrenia in 16 countries. Soc Psychiatry Psychiatr Epidemiol 1996;31:249‐58. [DOI] [PubMed] [Google Scholar]
- 13. Harrow M, Grossman LS, Jobe TH et al. Do patients with schizophrenia ever show periods of recovery? A 15‐year multi‐follow‐up study. Schizophr Bull 2005;31:723‐34. [DOI] [PubMed] [Google Scholar]
- 14. Velthorst E, Fett AKJ, Reichenberg A et al. The 20‐year longitudinal trajectories of social functioning in individuals with psychotic disorders. Am J Psychiatry 2017;174:1075‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gee B, Hodgekins J, Fowler D et al. The course of negative symptom in first episode psychosis and the relationship with social recovery. Schizophr Res 2016;174:165‐71. [DOI] [PubMed] [Google Scholar]
- 16. Abdin E, Chong SA, Vaingankar JA et al. Trajectories of positive, negative and general psychopathology symptoms in first episode psychosis and their relationship with functioning over a 2‐year follow‐up period. PLoS One 2017;12:e0187141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stiekema APM, Islam MA, Liemburg EJ et al. Long‐term course of negative symptom subdomains and relationship with outcome in patients with a psychotic disorder. Schizophr Res 2018;193:173‐81. [DOI] [PubMed] [Google Scholar]
- 18. Correll CU, Schooler NR. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr Dis Treat 2020;16:519‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fusar‐Poli P, Papanastasiou E, Stahl D et al. Treatments of negative symptoms in schizophrenia: meta‐analysis of 168 randomized placebo‐controlled trials. Schizophr Bull 2015;41:892‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Austin SF, Mors O, Budtz‐Jørgensen E et al. Long‐term trajectories of positive and negative symptoms in first episode psychosis: a 10 year follow‐up study in the OPUS cohort. Schizophr Res 2015;168:84‐91. [DOI] [PubMed] [Google Scholar]
- 21. Chan SKW, Chan HYV, Pang HH et al. Ten‐year trajectory and outcomes of negative symptoms of patients with first‐episode schizophrenia spectrum disorders. Schizophr Res 2020;220:85‐91. [DOI] [PubMed] [Google Scholar]
- 22. Bertelsen M, Jeppesen P, Petersen L et al. Five‐year follow‐up of a randomized multicenter trial of intensive early intervention vs standard treatment for patients with a first episode of psychotic illness: the OPUS trial. Arch Gen Psychiatry 2008;65:762‐71. [DOI] [PubMed] [Google Scholar]
- 23. Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS). Iowa City: University of Iowa, 1984. [Google Scholar]
- 24. Andreasen NC. Scale for the Assessment of Negative Symptoms (SANS). Iowa City: University of Iowa, 1984. [Google Scholar]
- 25. Arndt S, Andreasen NC, Flaum M et al. A longitudinal study of symptom dimensions in schizophrenia. Prediction and patterns of change. Arch Gen Psychiatry 1995;52:352‐60. [DOI] [PubMed] [Google Scholar]
- 26. Andreasen NC, Carpenter WT Jr, Kane JM et al. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 2005;162:441‐9. [DOI] [PubMed] [Google Scholar]
- 27. Bland RC. Diagnosis and clinical measurement in psychiatry: a reference manual for SCAN. J Psychiatry Neurosci 1999;24:481‐2. [Google Scholar]
- 28. Aas IM. Global Assessment of Functioning (GAF): properties and frontier of current knowledge. Ann Gen Psychiatry 2010;9:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brill N, Reichenberg A, Weiser M et al. Validity of the Premorbid Adjustment Scale. Schizophr Bull 2008;34:981‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Häfner H, Riecher‐Rössler A, Hambrecht M et al. IRAOS: an instrument for the assessment of onset and early course of schizophrenia. Schizophr Res 1992;6:209‐23. [DOI] [PubMed] [Google Scholar]
- 31. Jeppesen P, Petersen L, Thorup A et al. The association between pre‐morbid adjustment, duration of untreated psychosis and outcome in first‐episode psychosis. Psychol Med 2008;38:1157‐66. [DOI] [PubMed] [Google Scholar]
- 32. Juckel G, Schaub D, Fuchs N. Validation of the Personal and Social Performance (PSP) scale in a German sample of acutely ill patients with schizophrenia. Schizophr Res 2008;104:287‐93. [DOI] [PubMed] [Google Scholar]
- 33. Keefe RSE, Goldberg TE, Harvey PD et al. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 2004;68:283‐97. [DOI] [PubMed] [Google Scholar]
- 34. Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass 2008;2:302‐17. [Google Scholar]
- 35. Muthén LK, Muthén BO. Statistical analysis with latent variables user's guide. www.statmodel.com. [Google Scholar]
- 36. Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: three‐step approaches using Mplus. Struct Equ Model 2014;21:329‐41. [Google Scholar]
- 37. Lanza ST, Tan X, Bray BC. Latent class analysis with distal outcomes: a flexible model‐based approach. Struct Equ Model 2013;20:1‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Morgan C, Dazzan P, Lappin J et al. Rethinking the course of psychotic disorders: modelling long‐term symptom trajectories. Psychol Med 2022;52:2641‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Harrison G, Hopper K, Craig T et al. Recovery from psychotic illness: a 15‐ and 25‐year international follow‐up study. Br J Psychiatry 2001;178:506‐17. [DOI] [PubMed] [Google Scholar]
- 40. Schennach R, Meyer S, Seemüller F et al. Response trajectories in “real‐world” naturalistically treated schizophrenia patients. Schizophr Res 2012;139:218‐24. [DOI] [PubMed] [Google Scholar]
- 41. Smart SE, Keȩpińska AP, Murray RM et al. Predictors of treatment resistant schizophrenia: a systematic review of prospective observational studies. Psychol Med 2021;51:44‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Santesteban‐Echarri O, Paino M, Rice S et al. Predictors of functional recovery in first‐episode psychosis: a systematic review and meta‐analysis of longitudinal studies. Clin Psychol Rev 2017;58:59‐75. [DOI] [PubMed] [Google Scholar]
- 43. Austin SF, Mors O, Secher RG et al. Predictors of recovery in first episode psychosis: the OPUS cohort at 10 year follow‐up. Schizophr Res 2013;150:163‐8. [DOI] [PubMed] [Google Scholar]
- 44. Penttilä M, Jääskeläinen E, Hirvonen N et al. Duration of untreated psychosis as predictor of long‐term outcome in schizophrenia: systematic review and meta‐analysis. Br J Psychiatry 2014;205:88‐94. [DOI] [PubMed] [Google Scholar]
- 45. Canal‐Rivero M, Ruiz‐Veguilla M, Ortiz‐Garcìa de la Foz V et al. Longitudinal trajectories in negative symptoms and changes in brain cortical thickness: 10‐year follow‐up study. Br J Psychiatry 2023; doi: 10.1192/bjp.2022.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chang WC, Ho RWH, Tang JYM et al. Early‐stage negative symptom trajectories and relationships with 13‐year outcomes in first‐episode nonaffective psychosis. Schizophr Bull 2019;45:610‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Savill M, Banks C, Khanom H et al. Do negative symptoms of schizophrenia change over time? A meta‐analysis of longitudinal data. Psychol Med 2015;45:1613‐27. [DOI] [PubMed] [Google Scholar]
- 48. Correll CU, Howes OD. Treatment‐resistant schizophrenia: definition, predictors, and therapy options. J Clin Psychiatry 2021;82:MY20096AH1C. [DOI] [PubMed] [Google Scholar]
- 49. White C, Stirling J, Hopkins R et al. Predictors of 10‐year outcome of first‐episode psychosis. Psychol Med 2009;39:1447‐56. [DOI] [PubMed] [Google Scholar]
- 50. Ventura J, Subotnik KL, Gitlin MJ et al. Negative symptoms and functioning during the first year after a recent onset of schizophrenia and 8 years later. Schizophr Res 2015;161:407‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kaneko K. Negative symptoms and cognitive impairments in schizophrenia: two key symptoms negatively influencing social functioning. Yonago Acta Med 2018;61:91‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ventura J, Hellemann GS, Thames AD et al. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta‐analysis. Schizophr Res 2009;113:189‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lysaker PH, Vohs JL, Tsai J. Negative symptoms and concordant impairments in attention in schizophrenia: associations with social functioning, hope, self‐esteem and internalized stigma. Schizophr Res 2009;110:165‐72. [DOI] [PubMed] [Google Scholar]
- 54. Gry Secher R, Hjorthøj CR, Austin SF et al. Ten‐year follow‐up of the OPUS specialized early intervention trial for patients with a first episode of psychosis. Schizophr Bull 2015;41:617‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hansen HG, Starzer M, Nilsson SF et al. Clinical recovery and long‐term association of specialized early intervention services vs treatment as usual among individuals with first‐episode schizophrenia spectrum disorder: 20‐year follow‐up of the OPUS trial. JAMA Psychiatry 2023;80:371‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Maj M, van Os J, De Hert M et al. The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry 2021;20:4‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Killaspy H, Harvey C, Brasier C et al. Community‐based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry 2022;21:96‐123. [DOI] [PMC free article] [PubMed] [Google Scholar]


