Abstract
The methyl-α-d-glucopyranoside (MDG) test has been shown to be superior to motility testing in differentiating Enterococcus faecium from E. gallinarum. In the present study, 33 vancomycin-resistant enterococcus (VRE) isolates collected as part of a stool surveillance study were compared by using motility and MDG. Motility testing identified all 33 isolates as E. faecium, whereas MDG identified 11 of the 33 isolates as nonmotile E. gallinarum. The MDG results were confirmed by sequencing the 16S rDNA V6-to-V8 region. We conclude that the MDG test is a necessary component of routine VRE screening.
Enterococci have been shown to be the second most common cause of nosocomial infection in the United States (15). Enterococcus faecalis is responsible for the majority of enterococcal infections, whereas E. faecium, while responsible for significantly fewer infections, is more commonly associated with resistance to beta-lactams, fluoroquinones, and glycopeptides (9, 10) and is associated with greater morbidity and mortality (7). As the prevalence of infections caused by vancomycin-resistant enterococci (VRE) is presently low, the screening of stool for identification of colonizers in high-risk patients is the focus of several epidemiological studies (10, 13). It is critical in such screening studies to differentiate E. faecalis and E. faecium from other enterococcal species, such as E. gallinarum and E. casseliflavus, which do not normally cause human disease but commonly demonstrate intrinsic low-level glycopeptide resistance (1). Recent reports suggest that motility alone as the criterion for differentiating between E. gallinarum and E. faecium (3) is inadequate and may lead to the misidentification of isolates of nonmotile E. gallinarum as E. faecium (5).
Recently, Devriese and coworkers have shown the methyl-α-d-glycopyranoside (MDG) test to be reliable and accurate in differentiating E. casseliflavus and E. gallinarum from E. faecalis and E. faecium (4). We were interested in determining the impact of the MDG test using a collection of vancomycin-resistant E. faecium isolates taken from a recent stool surveillance project (10) in which 1,500 enterococcal isolates had been identified to species level with a conventional identification algorithm, not containing MDG (8). The susceptibilities to glycopeptides vancomycin and teicoplanin and the glycopeptide resistance genotypes were also determined (6, 11).
Frozen stock cultures of 33 vancomycin-resistant E. faecium isolates (MIC, 4 μg/ml) obtained in the VRE prevalence study were subcultured onto Trypticase soy–5% sheep blood agar and incubated at 37°C for 24 h for MDG testing and PCR lysate preparation. MDG testing of all VRE isolates was performed as previously described by Devriese et al. (4).
Enterococcal species identification of each isolate was confirmed by sequencing the V6-to-V8 region (12) of the 16S rDNA which corresponds to bp 929 to 1369 of the Escherichia coli 16S rRNA sequence (2). The following ATCC strains were chosen for sequence determination: E. faecalis ATCC 29212, E. faecium ATCC 35667, E. gallinarum ATCC 35038, and E. casseliflavus ATCC 12755. Thirty-two enterococcal isolates from the stool surveillance project had also been sequenced to confirm the specificity and consistency of all sequences: 9 E. faecium isolates, 10 E. faecalis isolates, 5 E. casseliflavus isolates, and 8 E. gallinarum isolates. Subsequently, sequencing of the V6-V8 region of the 16S rDNAs of all 33 VRE isolates tested for MDG was performed. DNA extracts were prepared by using one or two colonies from the 24-h subcultures. DNA was isolated by using the QIAamp tissue kit (Qiagen, Santa Clarita, Calif.) in accordance with the manufacturer’s protocol. PCR amplification was performed by using universal 16S rDNA gene primers 91E(G) (5′TCAAAGGAATTGACGGGGGC) and 13B (5′AGGCCCGGGAACGTATTCAC) (14). A 50-μl PCR mixture contained 5 μl of DNA template; 5 μl of 25 mM MgCl2–10× PCR buffer; 1.25 mM each dCTP, dGTP, dATP, and dUTP · dTTP in an 8:1 ratio; 0.5 μl of 100 mM each primer; 0.5 U of uracil DNA glycosylase (GibcoBRL, Burlington, Canada); 2.5 U of Taq DNA polymerase (Pharmacia Biotech, Baie d’Urfé, Canada); and 30 μl of sterile distilled H2O. The PCR was performed with a Perkin-Elmer GeneAmp PCR System 9600 with cycles of 37°C for 10 min and 95°C for 10 min and 30 cycles of 95, 55, and 72°C for 1 min each and incubated at 72°C for 10 min for final extension.
Sequencing reactions were performed with the ABI PRISM Dye Terminator Cycle Sequencing Ready Reaction kit (PE Applied Biosystems, Foster City, Calif.). The primer used for the sequencing reaction was 91E(G) or 13B diluted 1:100 in Tris-EDTA buffer. Cycle sequencing on the GeneAmp PCR System 9600 was performed, and sequencing analysis was performed with the PE-ABI 373 DNA sequencing system and Software 373 in accordance with the manufacturers’ instructions.
The results obtained by MDG testing for all 33 VRE isolates demonstrated that 22 isolates were MDG negative, showing concordance with prior motility-based E. faecium identification. However, 11 VRE isolates tested MDG positive, indicating that they were in fact not E. faecium as originally reported but, instead, nonmotile E. gallinarum (Table 1). These 11 strains all possessed low-level glycopeptide resistance, with vancomycin and teicoplanin MICs of 4 to 8 μg/ml and 0.25 to 0.5 μg/ml, respectively.
TABLE 1.
Comparison of MDG testing and species identification using sequencing with conventional testing of 33 VRE (E. faecium) isolates
| No. of isolates | MIC (μg/ml)
|
Genotyping result | Sequencing result | Conventionaltesta result | MDG result | |
|---|---|---|---|---|---|---|
| Vanco- mycin | Teico- planin | |||||
| 11 | 4–8 | 0.25–0.5 | vanC1 | E. cass/E. gallb | E. faeciumc | + |
| 10 | 4–8 | 0.25–0.5 | vanB | E. faecium | E. faecium | − |
| 12 | 256–512 | 4–32 | vanA | E. faecium | E. faecium | − |
Includes biochemical reactions, motility, and pigment.
E. cass, E. casseliflavus; E. gall, E. gallinarum.
Misidentification of nonmotile E. gallinarum.
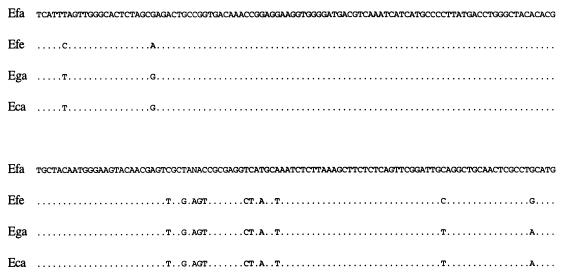
The MDG results were confirmed by sequencing the 16S rDNA V6-to-V8 regions. E. faecalis and E. faecium each showed specific and consistent sequence variability. E. gallinarum and E. casseliflavus showed a 2-bp difference from E. faecium and a 10-bp difference from E. faecalis but could not be differentiated from each other by using this area of the 16S rDNA gene (Fig. 1). Therefore, sequencing served to differentiate E. faecium from E. gallinarum and E. casseliflavus. Sequencing of the 33 VRE isolates which had previously all been identified as E. faecium confirmed that 22 isolates were E. faecium and 11 were nonmotile E. gallinarum (Table 1). E. gallinarum was differentiated from E. casseliflavus by its lack of pigment. There have been reported cases of nonpigmented E. casseliflavus (16); however, from a clinical point of view, this is not significant.
FIG. 1.
Sequence variability in the V7-V8 region of the 16S rDNA gene (bp 1130 to 1330) among E. faecalis (Efa), E. faecium (Efe), E. gallinarum (Ega), and E. casseliflavus (Eca).
The clinical significance of this work is apparent, as misidentification of vancomycin-resistant E. gallinarum as vancomycin-resistant E. faecium causes great concern. The prevalence of nonmotile E. gallinarum may be even higher due to the fact that vancomycin-sensitive nonmotile E. gallinarum can also be misidentified as vancomycin-sensitive E. faecium, although this is not a great concern.
Sequencing, which provided us with definitive identification of Enterococcus species, is not a realistic approach for routine VRE screening. Yet, it can serve as a tool for definitive identification of important pathogens or of strains of questionable identity. We conclude that the MDG test is a reliable, rapid, and cost-effective method for identification of clinically relevant Enterococcus species and that it is a necessary component for routine VRE screening.
Nucleotide sequence accession numbers.
The determined sequences comprising the V6-to-V8 regions of the 16S rDNA gene for each Enterococcus species used in this study have been submitted to GenBank with the following accession numbers: E. faecalis, AF023101; E. faecium, AF023102; E. gallinarum, AF023103; E. casseliflavus, AF023104.
REFERENCES
- 1.Arthur M, Courvalin P. Genetics and mechanisms of glycopeptide resistance in enterococci. Antimicrob Agents Chemother. 1993;37:1563–1571. doi: 10.1128/aac.37.8.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brosius J, Palmer M L, Kennedy P J, Noller H F. Complete nucleotide sequence of a 16S ribosomal RNA gene from Escherichia coli. Proc Natl Acad Sci USA. 1978;75:4801–4805. doi: 10.1073/pnas.75.10.4801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cartwright C P, Stock F, Fahle G A, Gill V J. Comparison of pigment production and motility tests with PCR for reliable identification of intrinsically vancomycin-resistant enterococci. J Clin Microbiol. 1995;33:1931–1933. doi: 10.1128/jcm.33.7.1931-1933.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devriese L A, Pot B, Karsters K, Lauwers S, Haesebrouck F. Acidification of methyl-α-d-glycopyranoside: a useful test to differentiate Enterococcus casseliflavus and Enterococcus gallinarum from Enterococcus faecium and Enterococcus faecalis. J Clin Microbiol. 1996;34:2607–2608. doi: 10.1128/jcm.34.10.2607-2608.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donabedian S, Chow J W, Shlaes D M, Green M, Zervos M. DNA hybridization and contour-clamped homogeneous electric field electrophoresis for identification of enterococci to the species level. J Clin Microbiol. 1995;33:141–145. doi: 10.1128/jcm.33.1.141-145.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dukta-Malen S, Evers S, Courvalin P. Detection of glycopeptide resistance genotypes and identification to the species level of clinically relevant enterococci by PCR. J Clin Microbiol. 1995;33:24–27. doi: 10.1128/jcm.33.1.24-27.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edmond M B, Ober J F, Dawson J D, Weinbaum D L, Wenzel R P. Vancomycin-resistant enterococcal bacteremia: natural history and attributable mortality. Clin Infect Dis. 1996;23:1234–1239. doi: 10.1093/clinids/23.6.1234. [DOI] [PubMed] [Google Scholar]
- 8.Facklam R R, Collins M D. Identification of Enterococcus species isolated from human infections by a conventional test scheme. J Clin Microbiol. 1989;27:731–734. doi: 10.1128/jcm.27.4.731-734.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gin A S, Zhanel G G. Vancomycin-resistant enterococci. Ann Pharmacother. 1996;30:615–624. doi: 10.1177/106002809603000610. [DOI] [PubMed] [Google Scholar]
- 10.Hoban D, Palatnick L, Weshnoweski B, Kabani A, Zelenitsky S, Karlowsky J, Zhanel G. Program and abstracts of the 37th Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, D.C: American Society for Microbiology; 1997. Comparative in vitro activity of LY333328, a new glycopeptide against Enterococcus gallinarum and Enterococcus casseliflavus, abstr. F-7; p. 147. [Google Scholar]
- 11.National Committee for Clinical Laboratory Standards. Methods for dilution of antimicrobial susceptibility tests for bacteria that grow aerobically. 4th ed. Publication M7-A4. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 12.Neefs J, de Peer Y V, De Rijk P, Chapelle S, De Wachter R. Compilation of small ribosomal subunit RNA structures. Nucleic Acids Res. 1993;21:3025–3049. doi: 10.1093/nar/21.13.3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ofner-Agostini M E, Conly J, Paton S, Kureishi A, Nicolle L, Mulvey M, Johnson W, Johnston L the Canadian Hospital Epidemiological Committee. Vancomycin-resistant enterococci (VRE) in Canada—results of the Canadian nosocomial infection surveillance program 1996 VRE Point Prevalence Surveillance Project. Can J Infect Dis. 1997;8:73–78. doi: 10.1155/1997/297038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Relman D A, Schmidt T M, MacDermott R P, Falkow S. Identification of the uncultured bacillus of Whipple’s disease. N Engl J Med. 1992;327:293–301. doi: 10.1056/NEJM199207303270501. [DOI] [PubMed] [Google Scholar]
- 15.Schaberg D R, Culver D H, Gaynes R P. Major trends in the microbial etiology of nosocomial infection. Am J Med. 1991;91:72S–75S. doi: 10.1016/0002-9343(91)90346-y. [DOI] [PubMed] [Google Scholar]
- 16.Vincent S, Knight R G, Green M, Sahm D F, Shlaes D M. Vancomycin susceptibility and identification of motile enterococci. J Clin Microbiol. 1991;29:2335–2337. doi: 10.1128/jcm.29.10.2335-2337.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]