Abstract
Maxillary sinus floor augmentation using lateral window and crestal technique is considered as predictable methods to increase the residual bone height; however, this surgery is commonly complicated by Schneiderian membrane perforation, which is closely related to anatomical factors. This article aimed to assess anatomical factors on successful augmentation procedures. After review of the current evidence on sinus augmentation techniques, anatomical factors related to the stretching potential of Schneiderian membrane were assessed and a decision tree for the rational choice of surgical approaches was proposed. Schneiderian membrane perforation might occur when local tension exceeds its stretching potential, which is closely related to anatomical variations of the maxillary sinus. Choice of a surgical approach and clinical outcomes are influenced by the stretching potential of Schneiderian membrane. In addition to the residual bone height, clinicians should also consider the stretching potential affected by the membrane health condition, the contours of the maxillary sinus, and the presence of antral septa when evaluating the choice of surgical approaches and clinical outcomes.
Subject terms: Surgery, Anatomy
Introduction
After tooth loss, the alveolar ridge can be compromised by atrophy and pneumatization of the maxillary sinus, which might limit the success of rehabilitation.1,2 Maxillary sinus floor augmentation (MSFA) involves Schneiderian membrane elevation to increase the residual crestal bone height (RBH) in the posterior maxilla, thereby increasing the bone volume to install dental implants in this region, including elevation through the lateral and transcrestal approaches.3 Lateral window sinus augmentation, introduced by Tatum and first published by Boyne and James,4,5 requires visualization of a bony window in the maxillary sinus lateral wall, and suffers from post-surgical complications, high cost, and complex procedures.6–8 The less invasive transcrestal approach first proposed by Tatum and adapted by Summers,5,9 is a blind technique, with advantages such as a small wound, short operation time, and high patient satisfaction.9 Evidence supports the view that MSFA through both of the above approaches is effective and safe.5,10 With the improvement of surgical techniques and equipment, the effect of anatomical factors and the choice of surgical approaches has been continuously updated.11–17
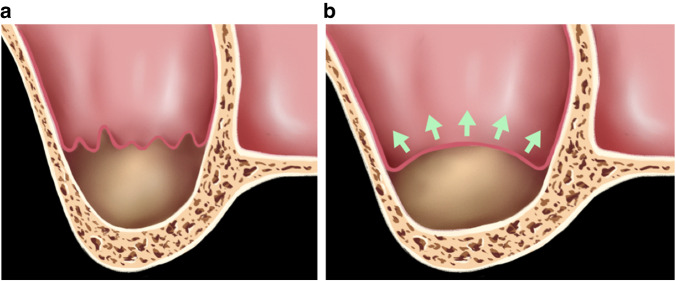
MSFA comprises the following steps: elevation of a flap, accessing the sinus cavity through a window, and Schneiderian membrane elevation above the maxillary floor and underneath the Schneider membrane to increase the alveolar bone height and create a “confined space”.18 Observation of this confined space from the coronal plane shown in Fig. 1, reveals that it consists of three walls: the maxillary sinus lateral wall, the crest of the alveolar ridge, and the stretched and lifted maxillary sinus membrane. Research suggested that an average tension of 7.3 N/mm³ caused sinus membrane perforation, and the stretching of the membrane can be achieved in one dimension up to 132.6% of its original size and in two dimensions up to 124.7%.19 In spite of the predictability of MSFA techniques, the Schneiderian membrane might be perforated when the local tension exceeds its stretching potential,20–24 which is also closely related to anatomical variations of this “confined space”.
Fig. 1.
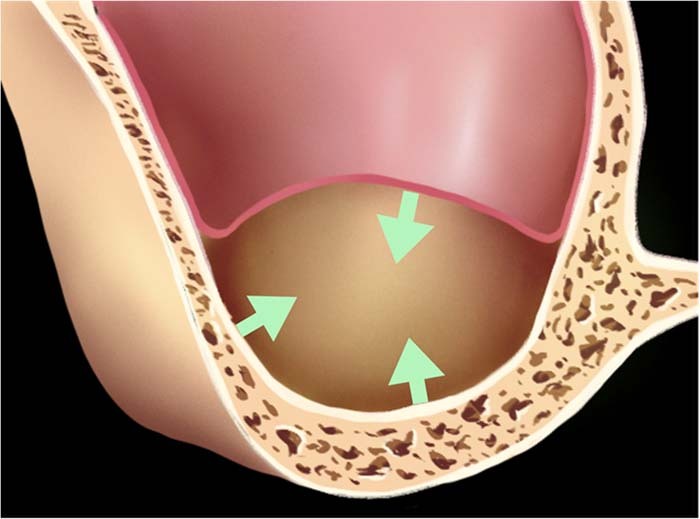
Three walls of confined space over the maxillary floor: the lateral wall of the maxillary sinus, the alveolar ridge crest, and the stretched and lifted maxillary sinus membrane
This article aims to: (1) Review the impact of the above-mentioned three walls of the confined space over the maxillary floor on sinus augmentation techniques; and (2) Propose a decision tree on the choice of surgical approaches.
Three walls of the confined space over the maxillary floor
Residual crestal bone height
The RBH is an important factor informing the choice of surgical approach. The criteria for the minimum effective implant osseointegration height of implants have been explored, along with the range of RBH to elevate the transcrestal sinus floor.
According to the academy of Osseointegration Consensus Conference on sinus grafts (1996), elevation of the MSFA can be carried out according to the category of the classification below: Category A (RBH ≥ 10 mm): classic implant procedure; Category B (RBH ≥ 7–9 mm): osteotome technique with simultaneous placement of implants ; Category C (RBH ≥ 4–6 mm): maxillary sinus elevation with lateral access and bone graft and immediate or deferred placement of implants; Category D (RBH ≥ 1–3 mm): maxillary sinus elevation with lateral access and bone graft and deferred placement of implants.25 The impact of anatomical factors and the choice of surgical approaches has been continuously updated and several studies reported that the RBH did not appear to affect osteogenesis after MSFA,12,13,26 suggesting that more emphasis should be placed on surgical difficulty and complications, rather than osteogenesis, when considering effects of the RBH on the surgical approaches.
Although the survival rate for longer (>8 mm) implants was 0.5% higher during long-term follow-up of 16–18 months, the insertion of longer dental implants into the augmented sinus is associated with biological complications, higher morbidity, increased costs, and longer surgery, and it has been suggested that alternative treatment using shorter dental implants (≤8 mm) might be preferrable.27,28 The advantages of fewer complications and disadvantages of low survival rate have been compared and discussed in different length definitions of “short implants”.29,30 For example, it is concluded that short implants (≤6 mm) are a valid option in situations of reduced bone height to avoid possible morbidity associated with augmentation procedures; however, they reveal a higher variability and lower predictability in survival rates;31 while according to Group 1 ITI Consensus Report: for atrophic posterior maxilla, short implants (≤6 mm) are a promising alternative to sinus floor elevation, with comparable survival rate, less MBL (marginal bone loss) and post-surgery reactions.32
Subsequently, it was suggested that elevation of the transcrestal sinus floor could be extended to patients with an RBH of 4–6 mm.33 The crestal approach was also considered a viable technique for us in patients with an RBH ≤ 4 mm, which merits further evaluation.34–36 Alternatively, good clinical results were observed for posterior mandibles treated using single extra-short (4 mm) implants and Pommer et al., using multifactorial analysis of the maxillae of human cadavers, reported no significant influence of RBH on the stability of the primary implant in atrophic sinus floor.37,38 but initial RBH of less than 4 mm was reported to influence the success rates of implants inserted in combination with sinus floor elevation using osteotomes.39 Although elevation of the sinus using the transcrestal window technique in a patient with residual alveolar bone in the posterior maxilla of 1–2 mm was reported recently11,25 and new bone formation differences were non-significant for residual bone height ≤2 and >2 mm,12 the evidence was insufficient and further long-term follow-up studies were needed and data reviewed from literature suggested a higher implant survival predictability as available residual bone increases.40
Lateral wall
Besides the RBH, evaluation of the lateral wall thickness should also be carried out when choosing the lateral approach. The mean maxillary lateral wall thickness has been reported as (1.98 ± 1.87) mm at the first molar and (1.21 ± 1.07) mm at the second molar.41 A retrospective study reported that the overall mean lateral wall thickness was (1.59 ± 0.84) mm at 4 mm coronal to the sinus floor and (1.58 ± 0.83) mm at 6 mm.21 Also, A. Monje et al. reported mean sinus lateral wall thickness for partial edentulous atrophic maxilla was (1.71 ± 0.12) mm, and for complete edentulous atrophic maxilla, (1.57 ± 0.07) mm.42
Firstly, membrane elevation requires good access and vision; however, a thick lateral wall can hinder instrument maneuverability during the lateral window sinus augmentation.43 Secondly, vascularization of cancellous bone is more extensive than that of cortical bone, and increased bleeding might obstruct visibility, thus prolonging surgery.44,45 Thirdly, membrane perforation is affected by maxillary sinus lateral wall thickness.21,46 At a lateral wall thickness of ≥2 mm at 4 mm coronal to the sinus floor, a perforation rate of 56.4% was observed, which decreased to 12.1% if the lateral wall thickness was ≤1 mm.21 And the alteration of the lateral approach sinus elevation technique is recommended if complications such as membrane perforation or bleeding are expected.47 Meanwhile, when accessing the antral cavity from a lateral wall of more than 2 mm, considering the vision, bleeding, and membrane perforation risk, a transcrestal approach might be a favorable alternative.
Maxillary sinus membrane
Schneiderian membrane perforation is the most frequently reported surgical complication.48,49 An intact Schneiderian membrane is crucial to maintain the postoperative osteogenic space. Multiple studies reported associations between Schneiderian membrane perforation and postoperative sinusitis, bone graft infection, and implant osseointegration failure.50–54 Perforation might occur when the local tension exceeds the stretching potential of the Schneiderian membrane (for example, a mean perforation tension of 7.3 N·mm−3),19 which is closely related to membrane health and thickness, and anatomical characteristics, such as the maxillary sinus width and contours.55
Sinus health
Given the maxillary sinus diseases present in some patients, the application of sinus floor elevation is restricted.25,56,57
The presence of sinus diseases might affect the tensile potential of the Schneiderian membrane and increase the difficulty of surgery and the risk of postoperative complications.58 Besides, Schneiderian membrane thickened caused by inflammation might decrease elasticity and thus a reduced stretching potential. Sinusitis, polypoid (cystic) lesions, and mucosal thickening are the most frequently noted radiographical indications of sinus diseases.59 Small antral pseudocysts lacking clinical symptoms and slight flat thickening (>2 mm and <5 mm) are not considered as contraindications for osteotome sinus floor elevation surgery.55 However, pre-existing conditions that might abrogate drainage patency must be addressed.60
Schneiderian membrane thickness
An appropriate membrane thickness has an important and beneficial effects on the tensile potential of the Schneiderian membrane.61,62
The sinus membrane comprises a ciliated pseudostratified columnar epithelium and an average thickness = 0.5 mm.63 Studies of the risk factors for membrane perforation, identified that perforation was more frequent for thinner membranes.64,65 In a retrospective study reviewing the records of 551 patients, a thinner membrane was observed in patients who suffered membrane perforation compared with those that did not.49 In those that suffered perforation, the average membrane thickness was (0.84 ± 0.67) mm, whereas it was (2.65 ± 4.02) mm in the patients that did not suffer perforation.49
By contrast, a Schneiderian membrane thickened because of inflammation, such as from odontogenic infections, particularly apical infections,63 and smoking66 might have decreased elasticity and thus a reduced stretching potential.67,68 And thicker maxillary sinus membrane was indeed observed in smokers compared to non-smokers,69,70 and smokers (46.2%) versus nonsmokers (23.4%) presented with at least a 10% difference in rates of perforations.71 Certain types of irritation, e.g., allergies, are associated with mucosal thickening.59 Park et al. reported that perforation occurrence and preoperative sinus lesions correlated significantly,51 possibly because of the gelatinous structures of the pathologically thickened membranes.72,73
Sinus width
Perforation might occur when the local tension exceeds the stretching potential of Schneider’s membrane,55 which is closely related membrane health and thickness, and anatomical characteristics, such as the width and contours of the maxillary sinus.74–78
Chan et al. defined sinuses as narrow (<8 mm), average (8–10 mm), and wide (>10 mm) on the basis of a mean distance of 2.3 mm from the sinus floor, and as narrow (<14 mm), average (14–17 mm), and wide (>17 mm) on the basis of a mean distance of 15 mm from the alveolar crest.79 Histological analysis indicated that a narrower maxillary sinus, a sinus floor with a tapered morphology, and a higher proportion of native mineralized bone would lead to a higher level of osteogenesis after MSFA.13 Similarly, Stacchi C al. represented newly formed bone after transcrestal sinus floor elevation was strongly influenced by sinus width and occurred consistently only in narrow sinus cavities (sinus width <12 mm).80 And graft bone resorption in elevated sinus showed a positive correlation with the sinus width.81
Surgically, the chance of membrane perforation during elevation and the difficulty of surgery are increased by the presence of a maxillary sinus cavity with a narrow-tapered shape.33,82 This surgical difficulty might result from the acute angles encountered. However, the local tension increases with wider maxillary sinus floors when lifting the maxillary sinus membrane.
Sinus contours
Sinus contours have a vital function in procedures to elevate the sinus floor,74–76 and special structures such as a maxillary sinus septum and tooth roots, might increase the membrane perforation risk.24,83,84 Notably, when the Schneiderian membrane is raised to the same height, its different contours affect its the stretching percentage. The maxilla sinus floor could have a complicated morphology, in which the width and contours of the sinus are closely related.85
Sinus contours were classified into five categories by Niu et al. in 2018: Narrow tapered, tapering, ovoid, square, and irregular. Niu et al. recommended a modified lateral sinus for a narrow-tapered sinus; both lateral and transcrestal approaches for tapering and ovoid sinuses; and for irregular sinuses, a lateral sinus with a wider window or a lateral sinus with double-window floor elevation were proposed.33 Compared with that for a U-shaped sinus, the risk of perforation is higher for an acute angled sinus because it is more difficult to angulate the instruments.22 Similarly, in a review of 407 augmentation procedures, anatomical variations, including a V-shaped sinus cavity and the presence of underwood septa, were identified as potential risk factors for membrane perforation because they limit access to the antral space and obscure the surgeon’s view.24
Sinus septum
Membrane perforation risk and surgical difficulty during elevation might be increased by special structures.24,83 Studies have reported much higher perforation rates of MSFA in the presence of septa.86,87
About 20–35% of maxillary sinuses contain an antral septum.88 A single septum is more commonly observed than multiple septa. Shih-Cheng et al. proposed that septa could be classified as easy (E), moderate (M), or difficult (D) according to the size, orientation, number, and location of antral septa.86 Treatment approaches for each category have been suggested; however, antral septa complicate sinus elevation surgery.
Assessment of membrane stretching potential: stretch-favorable type (SFT) and stretching-unfavorable type (SUT)
Perforation might occur when the local tension exceeds the intrinsic or stretching potential of the Schneiderian membrane, which is also closely related anatomical factors, such as membrane health and the width of the maxillary sinus. The stretching potential of the Schneiderian membrane, involving the sinus width, sinus contours, sinus/membrane health, and membrane thickness, allows sinuses to be classified as the following two types (Fig. 2):
Fig. 2.
Anatomical illustrations of maxillary sinus: a Type A-Stretch-favorable type (SFT); b Type B-Stretching-unfavorable type (SUT)
Type A: Stretch-favorable type (SFT). An SFT occurs when the maxillary sinus/membrane is in a healthy state; the membrane thickness is within the normal range, the maxillary contours tend to be oval; and there is no special structure, such as a maxillary sinus septum. Under these conditions, the stretching potential of the maxillary sinus membrane is relatively favorable, with relatively low surgical difficulty and risk (Fig. 2a).
Type B: Stretching-unfavorable type (SUT). By contrast, an SUT presents when the maxillary sinus/membrane is in a diseased state; the maxillary membrane is too thin or thickened because of inflammation; the maxillary contour tends to be wide, sharp, or angular; or there are special structures, such as a maxillary sinus septum. Under these circumstances, the stretch potential of the maxillary sinus mucosa is relatively poor, and the surgical difficulty and risks are relatively high. Table 1 lists the effects of anatomical variations on the stretching potential of Schneiderian membrane, based on the combined consideration of the sinus width, sinus contours, sinus/membrane health, and membrane thickness, which can be used to assess surgical risk and guide surgical approaches (Fig. 2b).
Table 1.
Impact of anatomical variations on the stretching potential of the Schneiderian membrane
| Stretch-favorable type (SFT) | Stretching-unfavorable type (SUT) | |||
|---|---|---|---|---|
| Anatomic variable | Anatomical features | Advice | Anatomical features | Advice |
| Sinus health condition | Health sinus | Lower perforation risk96 | Sinus diseases | Managed with care before sinus lift procedure59,96 |
| pseudocysts in a small size without clinical symptoms | Not contraindications to surgery55 | |||
| Membrane thickness | Appropriate membrane thickness between 1–2 mm | Predictable sinus augmentation procedure65 | Thinner membrane thickness of (0.84 ± 0.67) mm | Higher perforation risk compared with (2.65 ± 4.02) mm group49 |
| Thicken due to inflammation | Significant correlation between preoperative sinus lesions and perforation51 | |||
| Sinus width and contours | Tapering or ovoid | Both lateral and transcrestal approaches are recommended33,87 | V-shape, | Obscured visibility and limitd access to the antral space22,24 |
| Irregular | Higher perforation risk87 | |||
| Square | Lateral approach with a wider window33 | |||
| Septa | Absence of septa | Lower perforation risk86 | One or multiple septa | Higher perforation risk24,86 |
Decision tree and clinical cases
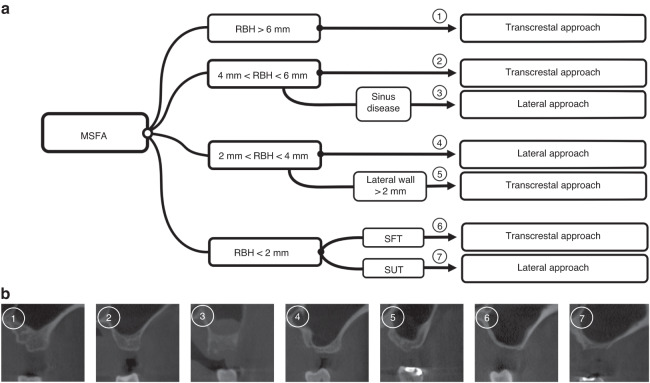
Decision tree
Ultimately, the goal of sinus elevation is to augment the available bone height to place implants, meanwhile lowering the risk of surgery. However, the success of the procedure depends on the technique chosen and treatment indications must be strictly adhered to. The RBH, lateral wall thickness, maxillary sinus contours, and the health of the Schneiderian membrane and sinus should be assessed when considering the choice of surgical approach and clinical outcomes. After a review of the literature concerning anatomical factors, and considering clinical findings, we propose the following decision tree for choosing the optimal surgical approach (Fig. 3):
If the RBH exceeds 6 mm: the transcrestal approach is the more favorable alternative because it is minimally invasive, and its morbidity, duration, and cost are limited.
If the RBH is between 4 and 6 mm, the transcrestal approach is the more favorable alternative when the sinus and membrane are in a relatively healthy state, which is the most common situations, whereas the lateral approach is preferred when the sinus and membrane are in an unhealthy state. The RBH does not appear to affect osteogenesis, indicating that surgical difficulty and complications should be considered rather than osteogenesis in this situation. The presence of sinus diseases might have an important effect on the tensile potential of Schneiderian membrane, thus increasing the difficulty of surgery and the risk of postoperative complications.
If the RBH is between 2 and 4 mm, the lateral approach is the more favorable alternative when the sinus wall is less than 2 mm, which is the most common situations, otherwise, the transcrestal approach should be chosen. Membrane elevation requires good vision and access, and the incidence of membrane perforation correlates with the thickness of the maxillary sinus lateral wall. Thus, when accessing the antral cavity from a lateral wall more than 2 mm away, the transcrestal approach is more favorable alternative. Health state of Schneiderian membrane and sinus should also be considered when necessary.
If the RBH is less than 2 mm, we suggest that the stretching potential of Schneiderian membrane and risk of the surgery should be assessed comprehensively (Table 1). Histologically, the smaller the width of the maxillary sinus, the higher the level of osteogenesis can be anticipated after MSFA. Surgically, during elevation, the membrane perforation risk is increased by the presence of a narrow and tapered maxillary sinus cavity; however, the wider the floor of the maxillary sinus floor, the greater local tension stretches when lifting the maxillary sinus membrane. If a patient has a healthy maxillary sinus, and the maxillary contours tends to be oval and no septa are present in the lifting region, the stretching potential of the maxillary sinus membrane is relatively favorable (Type A: SFT). For a stretch-favorable case, the transcrestal approach is the more favorable alternative. If a patient has an unhealthy maxillary sinus, or the maxillary contours tend to be wide (or too sharp) and there is a septum within the lifting region, the stretching potential of the maxillary sinus membrane is relatively unfavorable (Type B: SUT), and the surgical difficulty and risks are relatively high. For a stretch-unfavorable cases, the lateral approach is recommended.
Fig. 3.
Decision tree and CBCT classification: a A decision tree for choice of surgical approaches; b Relevant 3D CBCT Classification
Clinical cases
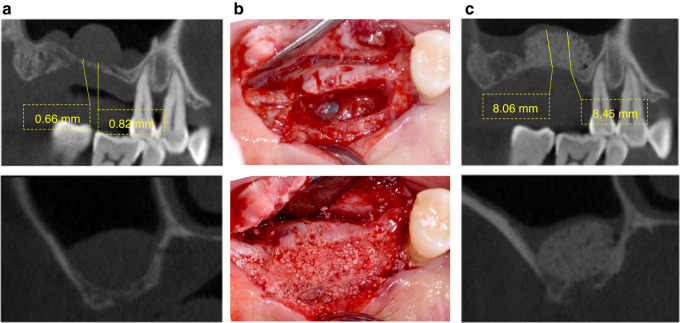
Case 1
This case comprised a 67-year-old male patient with a pseudocyst on the right maxillary sinus antral floor. Clinical examination revealed an edentulous maxilla encompassing the region from right first molar to the second molar. Assessment using pre-operative Cone Beam Computed Tomography (CBCT) revealed an atrophied edentulous ridge with an RBH < 1–2 mm (Fig. 4a). The maxillary contours tended to be oval and a homogeneous radiopaque mass without clinical symptoms was observed on the antral floor. The stretching potential of the maxillary sinus membrane was assessed as relatively favorable (SFT). Intentional perforation of the sinus membrane was carried out and a fine needle was used to aspirate the fluid to reduce the volume of the pseudocyst. Following saline irrigation, the transcrestal approach was used to elevate the sinus membrane. Subsequently, anorganic bone graft (Bio-Oss, Geistlich Pharma, Switzerland) was inserted (Fig. 4b). Post-operative CBCT showed that the sinus membrane was elevated and the bone graft material was successfully emplaced (Fig. 4c).
Fig. 4.
Case 1: a Pre-operative CBCT assessment, b surgical procedure, and c post-operative CBCT assessment of patient in case 1
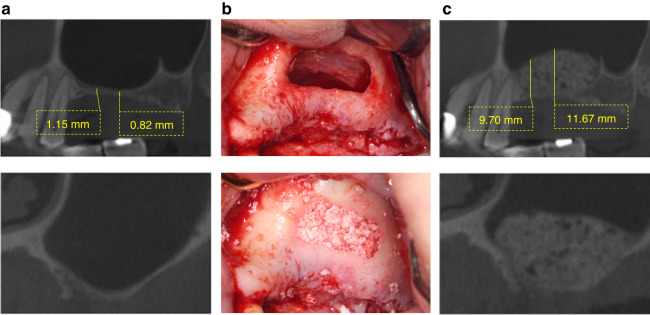
Case 2
This case was a 49-year-old female without sinus pathology. Clinical examination revealed an edentulous maxilla encompassing the region from the left first molar to the second molar. Assessment using pre-operative Cone Beam Computed Tomography (CBCT) revealed an atrophied edentulous ridge with an RBH < 1–2 mm (Fig. 5a). The maxillary sinus of the patient was in a healthy state, while the maxillary contours tended to be wide and there was a maxillary sinus septum in the distal part. The stretching potential of the maxillary sinus membrane was assessed as relatively unfavorable (SUT), and the surgical difficulty and risks were relatively high. The lateral wall approach was used to elevate the sinus membrane (Fig. 5b). Subsequently, the sinus cavity was compacted using an anorganic bone graft (Bio-Oss, Geistlich Pharma, Switzerland). Post-operative CBCT showed that the sinus membrane was elevated and the bone graft material was successfully emplaced (Fig. 5c).
Fig. 5.
Case 2: a Pre-operative CBCT assessment, b surgical procedure, and c post-operative CBCT assessment of patient in case 2
Discussion
Sinus pneumatization and ridge atrophy represent challenges to the successful rehabilitation of patients with posterior maxilla endosseous implants. Elevating the sinus comprises forming a “mucoperiosteal-alveolar pocket” above the maxillary floor and underneath the Schneiderian membrane to increase alveolar bone height and create a “confined space”.18
Although both osteotome and lateral window procedures are safe and effective in atrophic posterior maxilla, residual bone height is crucial in determining the survival of these implants,89 and sinus graft surgical decisions are majorly influenced by the RBH.90–92 With the improvement of implant surface modification and surgical equipment, the choice of MSFA approaches has been continuously updated and whether to choose immediate deferred placement of implants with anatomical variations is still controversial. No significant influence of RBH on the stability of the primary implant in atrophic sinus floor were reported, while initial RBH of less than 4 mm was reported to influence the success rates of implants inserted in combination with sinus floor elevation using osteotomes.37–39 Sinus elevation through the transcrestal window approach for a patient whose posterior maxilla had only 1–2 mm of residual alveolar bone was reported recently, and the incisions used in transcrestal window approach were shorter, compared with the lateral window approach, which could reduce discomfort of the patient after sinus elevation surgery.11,93 The evidence is insufficient and further long-term follow-up studies were needed. Meanwhile the transcrestal window approach requires a thorough assessment of the anatomy of sinus, elasticity, and deformation capacity of the Schneiderian membrane, the location of the intraosseous artery(which could be undetectable in CT/CBCT images), precise surgical approach, and so on.93 In addition, the crestal approach was used to elevate the sinus floor of 27 patients with residual bone heights of 2–3 mm.94 Moreover, a recent study revealed that the RBH and vital bone formation were not statistically correlated.13 No significant differences in the amount of osteogenesis in sinuses classified as having an RBH ≤ 2 mm or >2 mm were observed.13 When choosing the surgical technique, clinicians should assess the lateral wall thickness. A difference in the perforation rate was noted for a wall thickness measured at 6 mm coronal to the sinus floor.21 While other researchers also reported that lateral wall thickness had no effect on the perforation rate.95
Despite the predictability of sinus lift procedures, intra-operative complications are common,96,97 especially Schneiderian membrane perforation.24,98–100 Sinus compliance comprises the intrinsic potential of the sinus mucosa to resume its homeostatic status after the surgical trauma caused by sinus lifting.18 A higher rate of perforation is associated with a thinner membrane, possibly because the tensile capacity of a thicker membrane is significantly higher.19 Sinus augmentation surgery can be carried out on a 1–2 mm thick healthy and resilient membrane; however, for a thin membrane (<1 mm), a more cautious approach should be adopted.65 The Schneiderian membrane has the potential to thicken during inflammation, such as during odontogenic infections, especially apical infections.63 Irritations, such as allergies, can also thicken the mucosa.59 However, sinus augmentation is not contraindicated by the presence of mild mucosal thickening or pseudocysts in the absence of coexisting sinonasal symptoms.101 However, with a deeper understanding of the maxillary sinus disease, some researchers formed different opinions,23 and diseases of the maxillary sinus should be diagnosed and managed carefully prior to sinus elevating surgery.96
The stretching potential of Schneider’s membrane should be considered surgically and histologically.13,33 After lateral sinus floor elevation surgery, transient swelling of sinus membrane is observed, which reaching a peak value 7 days after surgery and completely resolves over months.62 The widths and contours of the sinus are closely related. For example, Wang et al. described the palate-nasal-recess (PNR) as the intersection point of the two imaginary lines following the lower part of the lateral nasal wall and the palatal wall in the maxillary sinus,102 which would make elevation of the sinus membrane more complicated and enhance the risk of membrane perforation. Niu et al. considered the sinus width, sinus depth, the PNR, and angle A simultaneously.33 A flat or irregular maxillary sinus stretches more when lifted to the same height, which requires a better stretch potential of the Schneider membrane. For example, the presence of irregular bone walls, exostosis, and septa might contribute to the occurrence of sinus perforations.87 Perforation rates of MSFA when septa were present were much higher than in those without septa.86,87 However, at 6–9 months post-surgery, wider sinuses added with deproteinized bovine bone mineral (DBBM) alone showed a lower percentage of newly formed bone, while the sinus contours and the RBH and sinus contours did not appear to influence post-MSFA osteogenesis.13
Conclusion
Anatomical factors, including the remaining alveolar bone, maxillary sinus characteristics, the health condition of the Schneiderian membrane, and the lateral wall thickness, crucially affect successful lifting. The stretching potential affected by maxillary sinus characteristics and the health condition of Schneiderian membrane/sinus, as well as the residual bone height, influence clinical outcomes and the choice of surgical techniques, which should be taken into account by clinicians.
Acknowledgements
This work was supported by grants from: 1. Young Clinical Research Fund of the Chinese Stomatological Association [grant number CSA-SIS2022-19]. 2. Sichuan Science and Technology Program: [grant number 2023NSFSC0567].
Author contributions
Q.Y. and M.L. conceived the study; Q.Y. helped in study design; D.X. and X.Z. collected the images and generated the figures; M.L. wrote the manuscript; Q.Y., M.L., D.X. and X.Z. reviewed the manuscript. All authors read and approved the final version of manuscript.
Funding
This work was supported by grants from: 1. Young Clinical Research Fund of the Chinese Stomatological Association [grant number CSA-SIS2022-19]. 2. Sichuan Science and Technology Program: [grant number 2023NSFSC0567].
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This is a review in which data was collected from the patients’ data base in the university affiliated hospital. The policy of the institution includes patients consent to participate in any trial and approve the use of their data with full explanation of the benefits and risks of any procedure. Informed consent was obtained from all subjects before the study. Moreover, all methods were carried out in accordance with the principles of the declaration of Helsinki.
References
- 1.Janner SF, et al. Characteristics and dimensions of the Schneiderian membrane: a radiographic analysis using cone beam computed tomography in patients referred for dental implant surgery in the posterior maxilla. Clin. Oral. Implants Res. 2011;22:1446–1453. doi: 10.1111/j.1600-0501.2010.02140.x. [DOI] [PubMed] [Google Scholar]
- 2.Mohan N, Wolf J, Dym H. Maxillary sinus augmentation. Dent. Clin. North Am. 2015;59:375–388. doi: 10.1016/j.cden.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int. J. Oral. Maxillofac. Implants. 2007;22:49–70. [PubMed] [Google Scholar]
- 4.Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral. Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 5.Tatum H., Jr Maxillary and sinus implant reconstructions. Dent. Clin. North Am. 1986;30:207–229. [PubMed] [Google Scholar]
- 6.Woo I, Le BT. Maxillary sinus floor elevation: review of anatomy and two techniques. Implant Dent. 2004;13:28–32. doi: 10.1097/01.id.0000116369.66716.12. [DOI] [PubMed] [Google Scholar]
- 7.Wallace SS, et al. Maxillary sinus elevation by lateral window approach: evolution of technology and technique. J. Evid.-based Dent. Pract. 2012;12:161–171. doi: 10.1016/S1532-3382(12)70030-1. [DOI] [PubMed] [Google Scholar]
- 8.Testori T, Weinstein T, Taschieri S, Wallace SS. Risk factors in lateral window sinus elevation surgery. Periodontology 2000. 2019;81:91–123. doi: 10.1111/prd.12286. [DOI] [PubMed] [Google Scholar]
- 9.Summers, R. B. A new concept in maxillary implant surgery: the osteotome technique. Compendium (Newtown, Pa.) 15, 154–156, 158 passim; quiz 162 (1994). [PubMed]
- 10.Del Fabbro M, Wallace SS, Testori T. Long-term implant survival in the grafted maxillary sinus: a systematic review. Int. J. Periodontics Restor. Dent. 2013;33:773–783. doi: 10.11607/prd.1288. [DOI] [PubMed] [Google Scholar]
- 11.Liu, Y., Ji, P., Fu, G. & Huang, H. Transcrestal sinus augmentation with simultaneous implant placement in 1 to 2 mm residual alveolar bone: a case report. J. Oral Implantol.10.1563/aaid-joi-D-20-00303 (2021). [DOI] [PubMed]
- 12.Pignaton TB, et al. Influence of residual bone height and sinus width on the outcome of maxillary sinus bone augmentation using anorganic bovine bone. Clin. Oral. Implants Res. 2019;30:315–323. doi: 10.1111/clr.13417. [DOI] [PubMed] [Google Scholar]
- 13.Zhou W, et al. The effect of anatomy on osteogenesis after maxillary sinus floor augmentation: a radiographic and histological analysis. Clin. Oral. Investig. 2021;25:5197–5204. doi: 10.1007/s00784-021-03827-6. [DOI] [PubMed] [Google Scholar]
- 14.Kim YK, Lee JY, Park JW, Kim SG, Oh JS. Sinus membrane elevation by the crestal approach using a novel drilling system. Implant Dent. 2017;26:351–356. doi: 10.1097/ID.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 15.Isidori M, Genty C, David-Tchouda S, Fortin T. Sinus floor elevation with a crestal approach using a press-fit bone block: a case series. Int. J. Oral. Maxillofac. Surg. 2015;44:1152–1159. doi: 10.1016/j.ijom.2015.01.028. [DOI] [PubMed] [Google Scholar]
- 16.Trombelli L, Franceschetti G, Trisi P, Farina R. Incremental, transcrestal sinus floor elevation with a minimally invasive technique in the rehabilitation of severe maxillary atrophy. Clinical and histological findings from a proof-of-concept case series. J. Oral. Maxillofac. Surg. 2015;73:861–888. doi: 10.1016/j.joms.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Danesh-Sani SA, Loomer PM, Wallace SS. A comprehensive clinical review of maxillary sinus floor elevation: anatomy, techniques, biomaterials and complications. Br. J. Oral. Maxillofac. Surg. 2016;54:724–730. doi: 10.1016/j.bjoms.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 18.Pignataro L, Mantovani M, Torretta S, Felisati G, Sambataro G. ENT assessment in the integrated management of candidate for (maxillary) sinus lift. Acta otorhinolaryngologica Italica : organo ufficiale della Soc. Ital. di otorinolaringologia e chirurgia cervico-facciale. 2008;28:110–119. [PMC free article] [PubMed] [Google Scholar]
- 19.Pommer B, Unger E, Sütö D, Hack N, Watzek G. Mechanical properties of the Schneiderian membrane in vitro. Clin. Oral. Implants Res. 2009;20:633–637. doi: 10.1111/j.1600-0501.2008.01686.x. [DOI] [PubMed] [Google Scholar]
- 20.Wen SC, Lin YH, Yang YC, Wang HL. The influence of sinus membrane thickness upon membrane perforation during transcrestal sinus lift procedure. Clin. Oral. Implants Res. 2015;26:1158–1164. doi: 10.1111/clr.12429. [DOI] [PubMed] [Google Scholar]
- 21.Basma H, et al. Association between lateral wall thickness and sinus membrane perforation during lateral sinus elevation: A retrospective study. Int. J. Oral. Implantol. 2021;14:77–85. [PubMed] [Google Scholar]
- 22.Cho SC, Wallace SS, Froum SJ, Tarnow DP. Influence of anatomy on Schneiderian membrane perforations during sinus elevation surgery: three-dimensional analysis. Practical Proced. Aesthetic Dent. 2001;13:160–163. [PubMed] [Google Scholar]
- 23.Baykul T, Fındık Y. Maxillary sinus perforation with presence of an antral pseudocyst, repaired with platelet rich fibrin. Ann. Maxillofac. Surg. 2014;4:205–207. doi: 10.4103/2231-0746.147144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwarz L, et al. Risk factors of membrane perforation and postoperative complications in sinus floor elevation surgery: review of 407 augmentation procedures. J. Oral. Maxillofac. Surg. 2015;73:1275–1282. doi: 10.1016/j.joms.2015.01.039. [DOI] [PubMed] [Google Scholar]
- 25.Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int. J. Oral. Maxillofac. Implants. 1998;13:11–45. [PubMed] [Google Scholar]
- 26.Avila-Ortiz G, et al. Analysis of the influence of residual alveolar bone height on sinus augmentation outcomes. Clin. Oral. Implants Res. 2012;23:1082–1088. doi: 10.1111/j.1600-0501.2011.02270.x. [DOI] [PubMed] [Google Scholar]
- 27.Thoma DS, Zeltner M, Hüsler J, Hämmerle CH, Jung RE. EAO Supplement Working Group 4 - EAO CC 2015 Short implants versus sinus lifting with longer implants to restore the posterior maxilla: a systematic review. Clin. Oral. Implants Res. 2015;26:154–169. doi: 10.1111/clr.12615. [DOI] [PubMed] [Google Scholar]
- 28.Esposito M, et al. Posterior atrophic jaws rehabilitated with prostheses supported by 6 mm-long, 4 mm-wide implants or by longer implants in augmented bone. Preliminary results from a pilot randomised controlled trial. Eur. J. Oral. Implantol. 2012;5:19–33. [PubMed] [Google Scholar]
- 29.Bechara S, et al. Short (6-mm) dental implants versus sinus floor elevation and placement of longer (≥10-mm) dental implants: a randomized controlled trial with a 3-year follow-up. Clin. Oral. Implants Res. 2017;28:1097–1107. doi: 10.1111/clr.12923. [DOI] [PubMed] [Google Scholar]
- 30.Pohl V, et al. Short dental implants (6 mm) versus long dental implants (11-15 mm) in combination with sinus floor elevation procedures: 3-year results from a multicentre, randomized, controlled clinical trial. J. Clin. Periodontol. 2017;44:438–445. doi: 10.1111/jcpe.12694. [DOI] [PubMed] [Google Scholar]
- 31.Yan Q, Wu X, Su M, Hua F, Shi B. Short implants (≤6 mm) versus longer implants with sinus floor elevation in atrophic posterior maxilla: a systematic review and meta-analysis. BMJ open. 2019;9:e029826. doi: 10.1136/bmjopen-2019-029826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jung RE, et al. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin. Oral. Implants Res. 2018;29:69–77. doi: 10.1111/clr.13342. [DOI] [PubMed] [Google Scholar]
- 33.Niu L, Wang J, Yu H, Qiu L. New classification of maxillary sinus contours and its relation to sinus floor elevation surgery. Clin. Implant Dent. Relat. Res. 2018;20:493–500. doi: 10.1111/cid.12606. [DOI] [PubMed] [Google Scholar]
- 34.Gonzalez S, Tuan MC, Ahn KM, Nowzari H. Crestal approach for maxillary sinus augmentation in patients with ≤4 mm of residual alveolar bone. Clin. Implant Dent. Relat. Res. 2014;16:827–835. doi: 10.1111/cid.12067. [DOI] [PubMed] [Google Scholar]
- 35.Ramos AH, et al. Extra short 4mm implants used to rehabilitation of atrophic posterior mandible. A serial case reports. J. Clin. Exp. Dent. 2020;12:e519–e522. doi: 10.4317/jced.56654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jang JW, Chang HY, Pi SH, Kim YS, You HK. Alveolar crestal approach for maxillary sinus membrane elevation with <4 mm of residual bone height: a case report. Int. J. Dent. 2018;2018:1063459. doi: 10.1155/2018/1063459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pommer B, et al. Primary implant stability in the atrophic sinus floor of human cadaver maxillae: impact of residual ridge height, bone density, and implant diameter. Clin. Oral. Implants Res. 2014;25:e109–e113. doi: 10.1111/clr.12071. [DOI] [PubMed] [Google Scholar]
- 38.Leighton Y, Carpio L, Weber B, Dias FJ, Borie E. Clinical evaluation of single 4-mm implants in the posterior mandible: A 3-year follow-up pilot study. J. Prosthet. Dent. 2022;127:80–85. doi: 10.1016/j.prosdent.2020.06.039. [DOI] [PubMed] [Google Scholar]
- 39.Călin C, Petre A, Drafta S. Osteotome-mediated sinus floor elevation: a systematic review and meta-analysis. Int. J. Oral. Maxillofac. Implants. 2014;29:558–576. doi: 10.11607/jomi.3206. [DOI] [PubMed] [Google Scholar]
- 40.Rios HF, Avila G, Galindo P, Bratu E, Wang HL. The influence of remaining alveolar bone upon lateral window sinus augmentation implant survival. Implant Dent. 2009;18:402–412. doi: 10.1097/ID.0b013e3181b4af93. [DOI] [PubMed] [Google Scholar]
- 41.Danesh-Sani SA, Movahed A, ElChaar ES, Chong Chan K, Amintavakoli N. Radiographic evaluation of maxillary sinus lateral wall and posterior superior alveolar artery anatomy: a cone-beam computed tomographic study. Clin. Implant Dent. Relat. Res. 2017;19:151–160. doi: 10.1111/cid.12426. [DOI] [PubMed] [Google Scholar]
- 42.Monje A, et al. Maxillary sinus lateral wall thickness and morphologic patterns in the atrophic posterior maxilla. J. Periodontol. 2014;85:676–682. doi: 10.1902/jop.2013.130392. [DOI] [PubMed] [Google Scholar]
- 43.Boreak N, Maketone P, Mourlaas J, Wang W, Yu Y. Decision tree to minimize intra-operative complications during maxillary sinus augmentation procedures. J Oral Biol. 2018;5:8. [Google Scholar]
- 44.Ella B, et al. Vascular connections of the lateral wall of the sinus: surgical effect in sinus augmentation. Int. J. Oral. Maxillofac. Implants. 2008;23:1047–1052. [PubMed] [Google Scholar]
- 45.Rosano G, Taschieri S, Gaudy JF, Weinstein T, Del Fabbro M. Maxillary sinus vascular anatomy and its relation to sinus lift surgery. Clin. Oral. Implants Res. 2011;22:711–715. doi: 10.1111/j.1600-0501.2010.02045.x. [DOI] [PubMed] [Google Scholar]
- 46.Stacchi C, et al. Intraoperative complications during sinus floor elevation with lateral approach: a systematic review. Int. J. oral. Maxillofac. Implants. 2017;32:e107–e118. doi: 10.11607/jomi.4884. [DOI] [PubMed] [Google Scholar]
- 47.Kang SJ, et al. Anatomical structures in the maxillary sinus related to lateral sinus elevation: a cone beam computed tomographic analysis. Clin. Oral. Implants Res. 2013;24:75–81. doi: 10.1111/j.1600-0501.2011.02378.x. [DOI] [PubMed] [Google Scholar]
- 48.Zijderveld SA, van den Bergh JP, Schulten EA, ten Bruggenkate CM. Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J. Oral. Maxillofac. Surg. 2008;66:1426–1438. doi: 10.1016/j.joms.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 49.Lum AG, Ogata Y, Pagni SE, Hur Y. Association between sinus membrane thickness and membrane perforation in lateral window sinus augmentation: a retrospective study. J. Periodontol. 2017;88:543–549. doi: 10.1902/jop.2017.160694. [DOI] [PubMed] [Google Scholar]
- 50.Pikos MA. Maxillary sinus membrane repair: update on technique for large and complete perforations. Implant Dent. 2008;17:24–31. doi: 10.1097/ID.0b013e318166d934. [DOI] [PubMed] [Google Scholar]
- 51.Park WB, Han JY, Kang P, Momen-Heravi F. The clinical and radiographic outcomes of Schneiderian membrane perforation without repair in sinus elevation surgery. Clin. implant Dent. Relat. Res. 2019;21:931–937. doi: 10.1111/cid.12752. [DOI] [PubMed] [Google Scholar]
- 52.Oh E, Kraut RA. Effect of sinus membrane perforation on dental implant integration: a retrospective study on 128 patients. Implant Dent. 2011;20:13–19. doi: 10.1097/ID.0b013e3182061a73. [DOI] [PubMed] [Google Scholar]
- 53.Hernández-Alfaro F, Torradeflot MM, Marti C. Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin. Oral. Implants Res. 2008;19:91–98. doi: 10.1111/j.1600-0501.2007.01372.x. [DOI] [PubMed] [Google Scholar]
- 54.Nolan PJ, Freeman K, Kraut RA. Correlation between Schneiderian membrane perforation and sinus lift graft outcome: a retrospective evaluation of 359 augmented sinus. J. Oral. Maxillofac. Surg. 2014;72:47–52. doi: 10.1016/j.joms.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 55.Qin L, et al. Influences of Schneiderian membrane conditions on the early outcomes of osteotome sinus floor elevation technique: a prospective cohort study in the healing period. Clin. Oral. Implants Res. 2017;28:1074–1081. doi: 10.1111/clr.12920. [DOI] [PubMed] [Google Scholar]
- 56.Friedland B, Metson R. A guide to recognizing maxillary sinus pathology and for deciding on further preoperative assessment prior to maxillary sinus augmentation. Int. J. Periodontics Restor. Dent. 2014;34:807–815. doi: 10.11607/prd.2043. [DOI] [PubMed] [Google Scholar]
- 57.Timmenga NM, Raghoebar GM, Boering G, van Weissenbruch R. Maxillary sinus function after sinus lifts for the insertion of dental implants. J. Oral. Maxillofac. Surg. 1997;55:936–939. doi: 10.1016/s0278-2391(97)90063-x. [DOI] [PubMed] [Google Scholar]
- 58.Kozuma A, et al. Preoperative chronic sinusitis as significant cause of postoperative infection and implant loss after sinus augmentation from a lateral approach. Oral. Maxillofac. Surg. 2017;21:193–200. doi: 10.1007/s10006-017-0611-8. [DOI] [PubMed] [Google Scholar]
- 59.Rege IC, Sousa TO, Leles CR, Mendonça EF. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral. Health. 2012;12:30. doi: 10.1186/1472-6831-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stacchi C, et al. Minimally Invasive Management of Implant-Supported Rehabilitation in the Posterior Maxilla, Part II. Surgical Techniques and Decision Tree. Int. J. Periodontics Restor. Dent. 2020;40:e95–e102. doi: 10.11607/prd.4498. [DOI] [PubMed] [Google Scholar]
- 61.Insua A, et al. Mechanical characteristics of the maxillary sinus Schneiderian membrane ex vivo. Clin. Oral. Investig. 2018;22:1139–1145. doi: 10.1007/s00784-017-2201-4. [DOI] [PubMed] [Google Scholar]
- 62.Makary C, Rebaudi A, Menhall A, Naaman N. Changes in sinus membrane thickness after lateral sinus floor elevation: a radiographic study. Int. J. Oral. Maxillofac. Implants. 2016;31:331–337. doi: 10.11607/jomi.4108. [DOI] [PubMed] [Google Scholar]
- 63.Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral. Surg., Oral. Med., Oral. Pathol., oral. Radiol., Endod. 2010;109:e80–e87. doi: 10.1016/j.tripleo.2009.10.031. [DOI] [PubMed] [Google Scholar]
- 64.Rapani M, Rapani C, Ricci L. Schneider membrane thickness classification evaluated by cone-beam computed tomography and its importance in the predictability of perforation. Retrospective analysis of 200 patients. Br. J. Oral. Maxillofac. Surg. 2016;54:1106–1110. doi: 10.1016/j.bjoms.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 65.Lin YH, Yang YC, Wen SC, Wang HL. The influence of sinus membrane thickness upon membrane perforation during lateral window sinus augmentation. Clin. Oral. Implants Res. 2016;27:612–617. doi: 10.1111/clr.12646. [DOI] [PubMed] [Google Scholar]
- 66.Testori T, Weinstein RL, Taschieri S, Del Fabbro M. Risk factor analysis following maxillary sinus augmentation: a retrospective multicenter study. Int. J. Oral. Maxillofac. Implants. 2012;27:1170–1176. [PubMed] [Google Scholar]
- 67.Guo ZZ, et al. Longitudinal response of membrane thickness and ostium patency following sinus floor elevation: a prospective cohort study. Clin. Oral. Implants Res. 2016;27:724–729. doi: 10.1111/clr.12655. [DOI] [PubMed] [Google Scholar]
- 68.Anduze-Acher G, et al. Change in sinus membrane dimension following sinus floor elevation: a retrospective cohort study. Clin. Oral. Implants Res. 2013;24:1123–1129. doi: 10.1111/j.1600-0501.2012.02520.x. [DOI] [PubMed] [Google Scholar]
- 69.Ghasemi S, et al. Intra- and postoperative complications of lateral maxillary sinus augmentation in smokers vs nonsmokers: a systematic review and meta-analysis. Int. J. Oral. Maxillofac. Implants. 2017;32:759–767. doi: 10.11607/jomi.5364. [DOI] [PubMed] [Google Scholar]
- 70.Pommer B, et al. Effect of maxillary sinus floor augmentation on sinus membrane thickness in computed tomography. J. Periodontol. 2012;83:551–556. doi: 10.1902/jop.2011.110345. [DOI] [PubMed] [Google Scholar]
- 71.von Arx T, Fodich I, Bornstein MM, Jensen SS. Perforation of the sinus membrane during sinus floor elevation: a retrospective study of frequency and possible risk factors. Int. J. Oral. Maxillofac. Implants. 2014;29:718–726. doi: 10.11607/jomi.3657. [DOI] [PubMed] [Google Scholar]
- 72.Anavi Y, Allon DM, Avishai G, Calderon S. Complications of maxillary sinus augmentations in a selective series of patients. Oral. Surg., Oral. Med., Oral. Pathol., Oral. Radiol., Endod. 2008;106:34–38. doi: 10.1016/j.tripleo.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 73.Shanbhag S, Karnik P, Shirke P, Shanbhag V. Cone-beam computed tomographic analysis of sinus membrane thickness, ostium patency, and residual ridge heights in the posterior maxilla: implications for sinus floor elevation. Clin. Oral. Implants Res. 2014;25:755–760. doi: 10.1111/clr.12168. [DOI] [PubMed] [Google Scholar]
- 74.Nunes LS, Bornstein MM, Sendi P, Buser D. Anatomical characteristics and dimensions of edentulous sites in the posterior maxillae of patients referred for implant therapy. Int. J. Periodontics Restor. Dent. 2013;33:337–345. doi: 10.11607/prd.1475. [DOI] [PubMed] [Google Scholar]
- 75.Lundgren S, et al. Sinus floor elevation procedures to enable implant placement and integration: techniques, biological aspects and clinical outcomes. Periodontology 2000. 2017;73:103–120. doi: 10.1111/prd.12165. [DOI] [PubMed] [Google Scholar]
- 76.Busenlechner D, et al. Sinus augmentation analysis revised: the gradient of graft consolidation. Clin. Oral. Implants Res. 2009;20:1078–1083. doi: 10.1111/j.1600-0501.2009.01733.x. [DOI] [PubMed] [Google Scholar]
- 77.Lombardi T, et al. Influence of maxillary sinus width on new bone formation after transcrestal sinus floor elevation: a proof-of-concept prospective cohort study. Implant Dent. 2017;26:209–216. doi: 10.1097/ID.0000000000000554. [DOI] [PubMed] [Google Scholar]
- 78.Teng M, et al. Sinus width analysis and new classification with clinical implications for augmentation. Clin. Implant Dent. Relat. Res. 2016;18:89–96. doi: 10.1111/cid.12247. [DOI] [PubMed] [Google Scholar]
- 79.Chan HL, Suarez F, Monje A, Benavides E, Wang HL. Evaluation of maxillary sinus width on cone-beam computed tomography for sinus augmentation and new sinus classification based on sinus width. Clin. Oral. Implants Res. 2014;25:647–652. doi: 10.1111/clr.12055. [DOI] [PubMed] [Google Scholar]
- 80.Stacchi C, et al. New bone formation after transcrestal sinus floor elevation was influenced by sinus cavity dimensions: a prospective histologic and histomorphometric study. Clin. Oral. Implants Res. 2018;29:465–479. doi: 10.1111/clr.13144. [DOI] [PubMed] [Google Scholar]
- 81.Zheng X, et al. Influence of maxillary sinus width on transcrestal sinus augmentation outcomes: radiographic evaluation based on cone beam CT. Clin. Implant Dent. Relat. Res. 2016;18:292–300. doi: 10.1111/cid.12298. [DOI] [PubMed] [Google Scholar]
- 82.Spinato S, Bernardello F, Galindo-Moreno P, Zaffe D. Maxillary sinus augmentation by crestal access: a retrospective study on cavity size and outcome correlation. Clin. Oral. Implants Res. 2015;26:1375–1382. doi: 10.1111/clr.12477. [DOI] [PubMed] [Google Scholar]
- 83.Gurler G, Delilbasi C. Relationship between preoperative cone beam computed tomography and intraoperative findings in sinus augmentation. Int. J. Oral. Maxillofac. Implants. 2015;30:1244–1248. doi: 10.11607/jomi.3797. [DOI] [PubMed] [Google Scholar]
- 84.Kirkham-Ali K, La M, Sher J, Sholapurkar A. Comparison of cone-beam computed tomography and panoramic imaging in assessing the relationship between posterior maxillary tooth roots and the maxillary sinus: a systematic review. J. Investigative Clin. Dent. 2019;10:e12402. doi: 10.1111/jicd.12402. [DOI] [PubMed] [Google Scholar]
- 85.Wagner F, et al. Morphometric analysis of sinus depth in the posterior maxilla and proposal of a novel classification. Sci. Rep. 2017;7:45397. doi: 10.1038/srep45397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wen SC, Chan HL, Wang HL. Classification and management of antral septa for maxillary sinus augmentation. Int. J. Periodontics Restor. Dent. 2013;33:509–517. doi: 10.11607/prd.1609. [DOI] [PubMed] [Google Scholar]
- 87.Shao Q, et al. Risk factors for sinus membrane perforation during lateral window maxillary sinus floor elevation surgery: a retrospective study. Clin. implant Dent. Relat. Res. 2021;23:812–820. doi: 10.1111/cid.13052. [DOI] [PubMed] [Google Scholar]
- 88.Shen EC, et al. Prevalence and location of maxillary sinus septa in the Taiwanese population and relationship to the absence of molars. Clin. Oral. Implants Res. 2012;23:741–745. doi: 10.1111/j.1600-0501.2011.02195.x. [DOI] [PubMed] [Google Scholar]
- 89.Al-Dajani M. Recent trends in sinus lift surgery and their clinical implications. Clin. Implant Dent. Relat. Res. 2016;18:204–212. doi: 10.1111/cid.12275. [DOI] [PubMed] [Google Scholar]
- 90.Fugazzotto PA. Augmentation of the posterior maxilla: a proposed hierarchy of treatment selection. J. Periodontol. 2003;74:1682–1691. doi: 10.1902/jop.2003.74.11.1682. [DOI] [PubMed] [Google Scholar]
- 91.Tan WC, Lang NP, Zwahlen M, Pjetursson BE. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. Part II: transalveolar technique. J. Clin. Periodontol. 2008;35:241–254. doi: 10.1111/j.1600-051X.2008.01273.x. [DOI] [PubMed] [Google Scholar]
- 92.Rosen PS, et al. The bone-added osteotome sinus floor elevation technique: multicenter retrospective report of consecutively treated patients. Int. J. Oral. Maxillofac. Implants. 1999;14:853–858. [PubMed] [Google Scholar]
- 93.Wang M, Yan M, Xia H, Zhao Y. Sinus elevation through transcrestal window approach and delayed implant placement in 1- to 2-mm residual alveolar bone: a case report. Implant Dent. 2016;25:866–869. doi: 10.1097/ID.0000000000000503. [DOI] [PubMed] [Google Scholar]
- 94.Kanayama T, Horii K, Senga Y, Shibuya Y. Crestal approach to sinus floor elevation for atrophic maxilla using platelet-rich fibrin as the only grafting material: a 1-year prospective study. Implant Dent. 2016;25:32–38. doi: 10.1097/ID.0000000000000327. [DOI] [PubMed] [Google Scholar]
- 95.Marin S, Kirnbauer B, Rugani P, Payer M, Jakse N. Potential risk factors for maxillary sinus membrane perforation and treatment outcome analysis. Clin. Implant Dent. Relat. Res. 2019;21:66–72. doi: 10.1111/cid.12699. [DOI] [PubMed] [Google Scholar]
- 96.Chan HL, Wang HL. Sinus pathology and anatomy in relation to complications in lateral window sinus augmentation. Implant Dent. 2011;20:406–412. doi: 10.1097/ID.0b013e3182341f79. [DOI] [PubMed] [Google Scholar]
- 97.Shiffler K, Lee D, Aghaloo T, Moy PK, Pi-Anfruns J. Sinus membrane perforations and the incidence of complications: a retrospective study from a residency program. Oral. Surg., Oral. Med., Oral. Pathol. Oral. Radiol. 2015;120:10–14. doi: 10.1016/j.oooo.2015.02.477. [DOI] [PubMed] [Google Scholar]
- 98.Yilmaz HG, Tözüm TF. Are gingival phenotype, residual ridge height, and membrane thickness critical for the perforation of maxillary sinus? J. Periodontol. 2012;83:420–425. doi: 10.1902/jop.2011.110110. [DOI] [PubMed] [Google Scholar]
- 99.Cortes AR, Cortes DN, Arita ES. Effectiveness of piezoelectric surgery in preparing the lateral window for maxillary sinus augmentation in patients with sinus anatomical variations: a case series. Int. J. Oral. Maxillofac. Implants. 2012;27:1211–1215. [PubMed] [Google Scholar]
- 100.Cortes AR, Pinheiro LR, Cavalcanti MG, Arita ES, Tamimi F. Sinus floor bone failures in maxillary sinus floor augmentation: a case-control study. Clin. Implant Dent. Relat. Res. 2015;17:335–342. doi: 10.1111/cid.12113. [DOI] [PubMed] [Google Scholar]
- 101.Feng Y, Tang Y, Liu Y, Chen F, Li D. Maxillary sinus floor elevation using the osteotome technique in the presence of antral pseudocysts: a retrospective study with an average follow-up of 27 months. Int. J. Oral. Maxillofac. Implants. 2014;29:408–413. doi: 10.11607/jomi.2644. [DOI] [PubMed] [Google Scholar]
- 102.Chan HL, Monje A, Suarez F, Benavides E, Wang HL. Palatonasal recess on medial wall of the maxillary sinus and clinical implications for sinus augmentation via lateral window approach. J. Periodontol. 2013;84:1087–1093. doi: 10.1902/jop.2012.120371. [DOI] [PubMed] [Google Scholar]