Abstract
This review aimed to summarise the relative risk (RR) of the main symptoms of long COVID in people infected with SARS-CoV-2 compared to uninfected controls, as well as the difference in health-related quality of life (HRQoL) after infection. MEDLINE, EMBASE, PubMed, NLM-LitCovid, WHO-COVID-19, arXiv and Europe-PMC were searched up to 23rd March 2022. Studies reporting risk (four or more weeks after infection) of fatigue, shortness of breath, and cognitive dysfunction, as well as comparative HRQoL outcomes, were included. Pairwise random-effects meta-analyses were performed to pool risks of individual symptoms. Thirty-three studies were identified; twenty studies reporting symptom risks were included in the meta-analyses. Overall, infection with SARS-CoV-2 carried significantly higher risk of fatigue (RR 1.72, 95% confidence intervals [CIs] 1.41, 2.10), shortness of breath (RR 2.60, 95% CIs 1.96, 3.44), memory difficulties (RR 2.53, 95% CIs 1.30, 4.93), and concentration difficulties (RR 2.14, 95% CIs 1.25, 3.67). Quality of life findings were varied and comparisons between studies were challenging due to different HRQoL instruments used and study heterogeneity, although studies indicated that severe hospitalised COVID is associated with a significantly poorer HRQoL after infection. These risks are likely to constantly change as vaccines, reinfections, and new variants alter global immunity.
Subject terms: Infectious diseases, Signs and symptoms
Introduction
Background
A growing body of evidence has shown that a significant proportion of COVID-19 survivors experience persistent symptoms after the acute phase of SARS-CoV-2 infection, also known as long COVID1. Several terms have been proposed to describe long COVID, however there is a lack of standardised nomenclature or diagnostic criteria. The National Institute for Health and Care Excellence (NICE) in the UK defines ‘long COVID’ as "signs and symptoms that develop during or after an infection consistent with COVID‑19, continue for more than 4 weeks and are not explained by an alternative diagnosis1." Under this definition, long COVID consists of two categories, ongoing symptomatic COVID-19, where symptoms last for 4–12 weeks, and post-COVID-19 syndrome, where symptoms persist beyond 12 weeks2. According to the World Health Organization (WHO), “post-COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis”3, 4.
The number of people globally with long COVID is currently unknown, and so far attempts to estimate prevalence have resulted in heterogenous findings5. A recent systematic review and meta-analysis has estimated that there are around 200 million individuals affected by post-COVID-19 syndrome6. Three recent meta-analyses have found that fatigue is the most common post-COVID-19 sequelae, while also finding cognitive dysfunction to be common6–8. These reviews assessed different length of time post COVID investigating 4+ weeks6, 12+ weeks8, and 12+ months7, respectively. In addition, a recent synthesis of ten longitudinal study samples from the UK found the proportions of presumed COVID-19 cases reporting any symptoms for 12+ weeks after infection ranged from 7.8 to 17%, while 1.2% to 4.8% reported debilitating symptoms9.
The risk of developing long COVID, and of its specific symptoms remains unclear. This is further complicated by the fact that many of the symptoms associated with long COVID are also common in the general population. A recent systematic review attempted to assess the risk of post-COVID-19 fatigue and estimated the risk of fatigue to be 3.7 times higher in post-COVID patients than in healthy controls 76–97 days after infection10. However, this review only included three studies in the meta-analyses, due to relatively early date that the review searches were performed (February 2021).
Aim of this review
While a number of systematic reviews and meta-analyses on long COVID symptoms exist, including those characterizing persisting post-COVID-19 symptoms and impact on quality of life11–13, these reviews do not assess the risk of these symptoms after infection compared with uninfected people, and therefore the excess risk of post-COVID-19 syndrome is poorly understood.
This review aims to systematically investigate the relative risk of three major long COVID symptoms (fatigue, shortness of breath/dyspnoea, and cognitive dysfunction) and quality of life ≥ 4 weeks from SARS-CoV-2 infection compared to non-infected controls. These three symptoms were selected for study as they are often the most prevalent symptoms of long COVID reported in the literature, and are the three named symptoms in the December 2021 WHO Delphi consensus on the definition of post COVID-19 condition14.
Results
Literature search
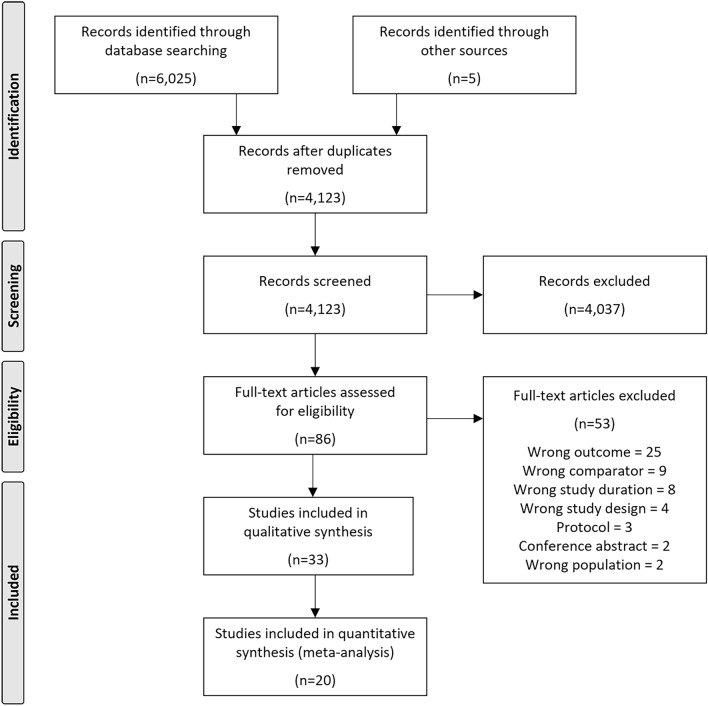
The searches identified 6025 records from electronic databases and five records from hand searching. After removing duplicates, 4123 records were title/abstract screened, of which 86 full-text articles were retrieved and assessed for eligibility. Studies excluded at full-text screening, with reasons for exclusion, are listed in Supplementary Table S3. A total of 33 studies were identified for inclusion in the systematic review (Fig. 1).
Figure 1.
Flow diagram of study selection67.
Study and patient characteristics
The characteristics of the 33 included studies are summarised in Table 1, with further details available in Supplementary Table S4. Studies were performed in a total of 15 countries, with the majority from Europe and North America. Outcomes reported by the studies were risk of fatigue15–34, shortness of breath/dyspnoea15–17, 19, 22–25, 27–31, 35, 36, cognitive dysfunction15, 17–20, 22–25, 27, 29–31, 33, 37, 38, and comparisons of quality of life23, 36, 39–47.
Table 1.
Characteristics of included studies.
| Study | Country | Data source | Study design | COVID-19 test | COVID + population | N cases/controls |
|---|---|---|---|---|---|---|
| Al-Aly16 | USA | Veterans’ Health Administration database | Cohort | NR | Adults; military veterans | 73,435/4,990,835 |
| Al-Aly15 | USA | Veterans’ Health Administration database | Cohort | NR | Adults; military veterans | 113,474/4,983,491 (COVID) 5,785,273 (influenza) |
| Amin-Chowdhury17 | UK | Public Health England database | Cohort | Antibody test | Adults; healthcare workers | 140/1160 |
| Borch18 | Denmark | Danish Health Data Authority and other national registries | Cohort | PCR | Children (0–17 yrs) | 15,041/47,780 |
| Carazo37 | Canada | Provincial COVID-19 and SARS-CoV-2 laboratory databases | Case–control | PCR | Adults; healthcare workers | 6052/4390 |
| Caspersen19 | Norway | Norwegian Mother, Father and Child Cohort Study and linked registries | Cohort | PCR | Adults; participants in MoBa cohort study | 774/72,953 |
| Castro20 | USA | Electronic hospital records | Case–control | PCR | Adults; hospitalised; emergency inpatients | 6619/6342 |
| Chevinsky21 | USA | Premier Healthcare Database Special COVID-19 Release | Matched cohort | NR | Adults; outpatients | 44,489/44,489 |
| Desgranges22 | Switzerland | Hospital patients | Cohort | PCR | Outpatients | 418/89 |
| Elkan39 | Israel | Hospital patients | Case–control | PCR | Adults; hospitalised | 66/42 |
| Huang40 | China | Hospital patients | Cohort | PCR | Hospitalised | 1164/1164 |
| Kikkenborg Berg23 | Denmark | Danish COVID-19 database | Matched cross-sectional | PCR | Adolescents (15–18 yrs) | 6630/21,640 |
| Kuodi24 | Israel | Hospital testing laboratory | Cross-sectional (from cohort study) | PCR | Adults; tested in hospital | 951/2437 |
| Liu38 | China | Hospital patients | Cohort | NR | Adults (≥ 60 yrs); hospitalised | 1438/438 |
| Matta25 | France | French CONSTANCES cohort | Cross-sectional (from cohort study) | Antibody test | Adults (18–69 yrs) | 1091/25,732 |
| Nielsen35 | Denmark | Hospital healthcare workers | Cohort | PCR | Adults, healthcare workers; non-hospitalised | 210/630 |
| Niyatiwatchanchai41 | Thailand | Hospital patients | Matched cross-sectional | PCR | Adults; hospitalised | 105/25 |
| Noviello26 | Italy | Hospital testing laboratory | Cohort | PCR | Adult (18–60 yrs); tested in hospital | 164/183 |
| Petersen36 | Germany | Medical centre clinical information system and community participants | Matched cross-sectional | PCR | Adults (45–74 yrs) | 443/1328 |
| Radtke47 | Switzerland | Proxy-reported questionnaires | Cross-sectional (from cohort study) | Antibody test | Children and adolescents (6–16 yrs) | 109/1246 |
| Raman 202042 | UK | Hospital patients | Matched cohort | PCR | Adults | 58/30 |
| Rivera-Izquierdo27 | Spain | Hospital patients | Cohort | PCR | Hospitalised | 453/453 |
| Roessler28 | Germany | Health insurance database | Matched cohort | Laboratory virus detection | Adults and children; hospitalised/outpatient | 678,965/3,394,825 |
| Roge29 | Latvia | Hospital patients | Cohort | Rapid antigen test | Children (1 mth-18 yrs), hospitalised/outpatient | 236/142 |
| Søras44 | Norway | Laboratory records | Cohort | PCR | Adults | 794/7978 |
| Søras45 | Norway | Laboratory records | Cohort | PCR | Adults | 794/7992 |
| Sørenson30 | Denmark | National COVID-19 surveillance system | Cross-sectional | PCR | Adults (≥ 15 yrs) | 61,002/91,878 |
| Spotnitz31 | USA | Health insurance database | Cohort | NR | Adults and children; hospitalised | 448,176/803,870 |
| Stephenson46 | UK | Public Health England database | Cohort | PCR | Adolescents (11–17 yrs) | 3065/3739 |
| Strahm32 | Switzerland | Hospital employees | Cohort | PCR/rapid antigen test | Adults; healthcare workers | 784/2550 |
| Taquet33 | USA | TriNetX Analytics | Cohort | PCR | Adolescents and adults (≥ 10 yrs); hospitalised | 106,578/106,578 |
| Vlake43 | Netherlands | ISARIC database and Franciscus Corona Registry | Cohort | PCR | Adults; hospitalised | 1446/148 |
| Xie34 | USA | US Department of Veterans Affairs | Cohort | NR | Adults | 181,384/4,397,509 |
mth, months; NR, not reported; PCR, polymerase chain reaction; yrs, years.
Participants or records in the studies were retrieved or recruited from healthcare databases or registries, COVID-19 databases, hospitals (including inpatients and outpatients, healthcare workers, and hospital employees), COVID-19 laboratory records, questionnaires, existing study cohorts, and schools. Case populations included people with a positive COVID-19 test, users of healthcare facilities with a positive test, volunteers or survey respondents, and hospitalized patients or outpatients of hospitals. Studies were classed by this review as either those including hospitalized patients, hospital outpatients, or those more representative of the general population (all SARS-CoV2 infections). Two studies included individuals who were tested for SARS-CoV-2 infection in hospital but did not clarify whether these were hospitalized patients24, 26; these were therefore considered representative of a general population by this review. Control populations included those testing negative for SARS-CoV-2 infection (31 studies) or a historical influenza cohort to compare COVID-19 with a well-characterized respiratory viral illness (four studies). Nearly all studies included controls from the same population as the cases; of the 13 studies including outpatients and hospitalized patients, three studies included non-hospitalized individuals as controls38, 41, 42.
Most included studies enrolled adults only. The reported ages of COVID-positive participants in studies that included adults ranged from a median of 39.8 to 70.8 years, and a mean of 35.6 to 60.7 years. Five studies enrolled children or adolescents18, 23, 29, 46, 47. The reported percentage of female participants ranged from 5.4 to 84.3%.
SARS-CoV-2 infection was assessed by PCR (22 studies), antibody test (3 studies) or rapid antigen test (2 studies); the remaining studies did not report the diagnostic test used. Only one study reported details concerning the main circulating variant during the time period for SARS-CoV-2 infection46. The original wild-type COVID-19 strain was estimated to be in circulation during the infection period in most studies.
Risks of fatigue, shortness of breath, and cognitive dysfunction after SARS-CoV-2 infection
Risk of post-COVID symptoms ≥ 4 weeks after infection was reported by 20 studies for fatigue (Supplementary Table S5), 15 studies for shortness of breath (Supplementary Table S6), and 16 studies for cognitive dysfunction (Supplementary Table S7). COVID-19 cases were compared to COVID-19-negative controls in most studies; four studies compared risks in hospitalised COVID-19 patients to hospitalised historical influenza cohorts. While outcome descriptions were similar across fatigue and shortness of breath, cognitive dysfunction outcome descriptions were more varied, and included general cognition outcomes (e.g., cognitive impairment), memory-related problems, concentration-related problems and language disturbances.
At least one significantly higher outcome risk was reported by 15 studies for fatigue, by 11 studies for shortness of breath, and by nine studies for cognitive dysfunction.
Compared to historical hospitalised influenza cohorts, risks of long COVID-19 symptoms ranged from 1.30 (95% CIs not reported) to 2.65 (95% CIs 2.22, 3.08) for fatigue, 1.14 (95% Cis 0.94, 1.40) to 2.28 (95% CIs not reported) for shortness of breath, and from 1.18 (95% Cis 0.89, 1.48) to 1.47 (95% Cis 1.15, 1.87) for cognition.
Meta-analyses of risks of fatigue, shortness of breath, and cognitive dysfunction after SARS-CoV-2 infection
Meta-analyses (random-effects) of risks of fatigue, shortness of breath, and cognitive dysfunction after SARS-CoV-2 infection included all studies of adolescents and/or adults comparing COVID-19-positive cases with COVID-19-negative controls and reporting a comparable risk outcome. Comparisons of historical influenza cohorts were not included as of the four studies, two were additional sub-analyses of hospitalised patients, one did not report a comparable risk ratio, and one did not report 95% CIs. Fourteen studies were eligible for inclusion in the meta-analysis for fatigue and 12 for shortness of breath. Cognitive dysfunction outcomes were classified into those reporting general cognition problems (three studies), memory-related problems (seven studies), and concentration-related problems (six studies).
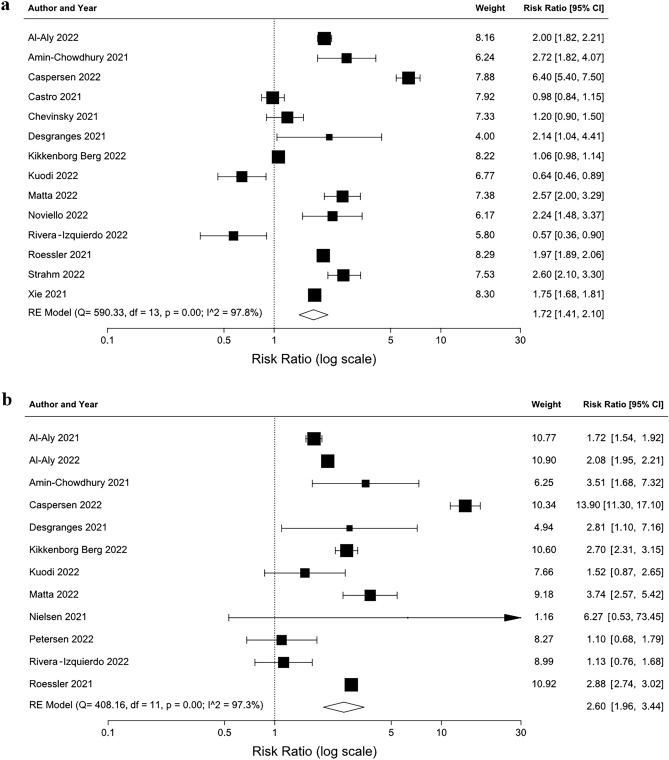
Compared to non-infected controls, SARS-CoV-2 infection was associated with a significantly higher risk of fatigue (RR 1.72 [95% CIs 1.41, 2.10]) and shortness of breath (RR 2.60 [95% CIs 1.96, 3.44]) ≥ 4 weeks after the infection (Fig. 2). Analyses of studies or subgroups only reporting risks for hospitalised patients/outpatients found a risk ratio of 1.59 (95% CIs 1.20, 2.11) for fatigue (seven studies) and 2.78 (95% CIs 2.31, 3.34) for shortness of breath (five studies).
Figure 2.
Meta-analyses results (random-effects) of risk of fatigue (a) and shortness of breath (b) after SARS-CoV-2 infection. Arrow indicates upper 95% CI is greater than risk ratio scale range shown. df, degrees of freedom; RE, random-effects.
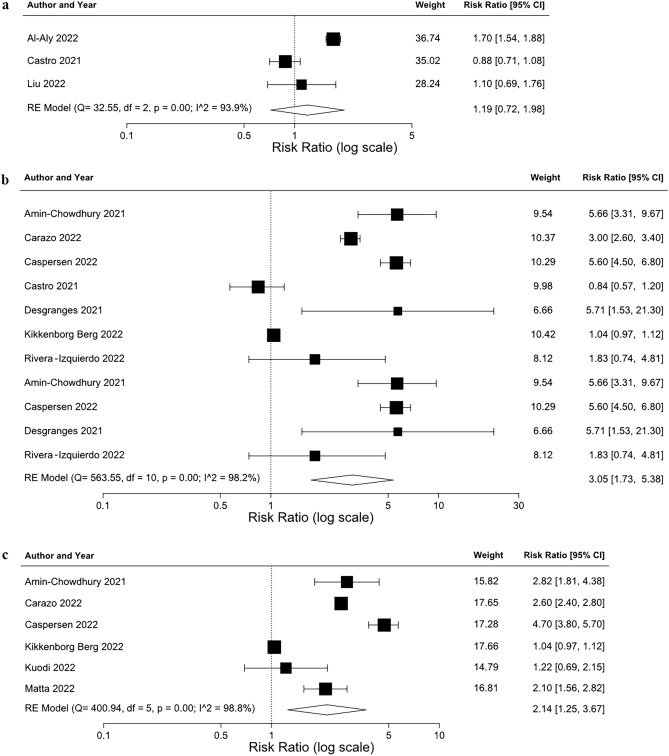
Both memory and concentration-related problems had a significantly higher risk in COVID-positive participants (memory: RR 2.53 [95% CIs 1.30, 4.93]; concentration: RR 2.14 [95% CIs 1.25, 3.67]) ≥ 4 weeks after infection; while there was an increased risk of cognition problems (RR 1.44 [95% CIs 0.59, 3.56]), this was not statistically significant (Fig. 3).
Figure 3.
Meta-analyses results (random-effects) of risk of cognitive problems (a), memory problems (b), and concentration problems (c) after SARS-CoV-2 infection. df, degrees of freedom; RE, random-effects.
Sensitivity analyses, heterogeneity, leave-1-out analyses, and publication bias
Sensitivity analyses were performed for all four symptoms, where three or more studies could be included in the analysis (Table 2). All fatigue and shortness of breath sensitivity analyses showed a similar result to the main analyses with no loss of statistical significance, indicating that the results were generally robust. Removal of preprints from the memory and concentration analyses, and removal of post-vaccination studies from the concentration analysis, resulted in a loss of significance, however these analyses included a small number of studies.
Table 2.
Sensitivity analyses.
| Sensitivity analysis | Risk ratio (95% CIs) | Q | df | Q P-value | I2 (%) |
|---|---|---|---|---|---|
| Fatigue | |||||
| ≥ 12 weeks after infection | 1.75 (1.49, 2.04) | 154.71 | 9 | < 0.01 | 94.2 |
| Included population overlap study | 1.73 (1.44, 2.07) | 590.45 | 14 | < 0.01 | 97.6 |
| Included children-only study | 1.78 (1.46, 2.17) | 596.68 | 14 | < 0.01 | 97.7 |
| Pre-vaccination studies only | 2.05 (1.53, 2.74) | 250.41 | 8 | < 0.01 | 96.8 |
| Adjusted risks only | 1.69 (1.30, 2.21) | 553.17 | 12 | < 0.01 | 97.8 |
| Peer-reviewed publications only | 1.89 (1.41, 2.54) | 468.10 | 9 | < 0.01 | 98.1 |
| Shortness of breath | |||||
| ≥ 12 weeks after infection | 2.45 (1.86, 3.22) | 125.51 | 6 | < 0.01 | 95.2 |
| Included children-only study | 2.59 (1.96, 3.42) | 408.19 | 12 | < 0.01 | 97.1 |
| Pre-vaccination studies only | 2.83 (1.77, 4.52) | 343.65 | 8 | < 0.01 | 97.7 |
| Adjusted risks only | 2.56 (1.73, 3.80) | 362.22 | 10 | < 0.01 | 97.2 |
| Peer-reviewed publications only | 2.63 (1.70, 4.08) | 358.85 | 8 | < 0.01 | 97.8 |
| Memory problems | |||||
| ≥ 12 weeks after infection | 3.02 (1.15, 7.94) | 81.45 | 4 | < 0.01 | 95.1 |
| Included children-only study | 2.69 (1.41, 5.15) | 397.96 | 7 | < 0.01 | 98.2 |
| Pre-vaccination studies only | 4.84 (3.28, 7.15) | 5.29 | 3 | 0.15 | 43.3 |
| Peer-reviewed publications only | 2.70 (0.82, 8.92) | 233.63 | 3 | < 0.01 | 98.7 |
| Concentration problems | |||||
| Pre-vaccinated studies only | 2.39 (0.76, 7.47) | 202.11 | 2 | < 0.01 | 99.0 |
| Peer-reviewed publications only | 2.17 (0.77, 6.10) | 200.78 | 2 | < 0.01 | 99.0 |
df, degrees of freedom.
Heterogeneity between the studies in all analyses was high, with an I2 value ranging from to 97.1% to 98.8% in the five main analyses. This reflects the highly variable study designs included in the analysis due to the disparate nature of the available data or the heterogeneity of COVID-19 disease and long COVID itself.
Leave-1-out analyses found the main analyses did not lose statistical significance when each study was individually removed, with the exception of the removal of Carazo 202237 from the concentration analysis, indicating that the results were generally robust.
For all analyses, no evidence of publication bias was found when using the Egger’s test (fatigue P-value = 0.53; shortness of breath P-value = 0.99; cognition P-value = 0.58; memory P-value = 0.57; concentration P-value = 0.87), and funnel plots generally showed symmetry, indicating publication bias is unlikely.
Health-related quality of life after SARS-CoV-2 infection
Health-related quality of life was reported in 11 studies (Supplementary Table S8) by validated instruments including the RAND-36, EuroQol-5D (EQ-5D), and 36-Item Short Form Survey (SF-36), and three paediatric instruments: Health Behaviour in School-aged Children (HBSC), Paediatric Quality of Life Inventory (PedsQL), and Children’s Somatic Symptoms Inventory-24 (CSSI-24).
Hospitalised COVID-19 patients’ quality of life was significantly lower in most or all instrument domains when compared to healthy, non-hospitalised uninfected controls40–42 but similar to controls hospitalised for pneumonia or other non-COVID-19 reasons39, 43. Quality of life comparisons for all SARS-CoV-2 infections were overall inconclusive; two studies reported no differences between cases and controls for adults using the EQ-5D36, while two studies found that more COVID-19-positive adults self-reported poorer health compared to the previous year at 3 and 8 months post-infection compared to non-infected controls44, 45. In children and/or adolescents, one study reported no significant difference between groups47, one found quality of life and sleep significantly better in the SARS-CoV-2-infected adolescents23, and one study reported that younger teenagers were more likely to report physical concerns while older teenagers more likely to report mental concerns46.
Methodological quality
Study quality assessed by the modified Newcastle–Ottawa scale found that 21 studies were of low risk of bias/high quality and 12 of medium risk of bias/medium quality. Scores for each study are presented in Supplementary Table S9.
Discussion
Our systematic review and meta-analyses found that COVID-19 infection results in a significantly raised risk of fatigue (1.72-fold) and shortness of breath (2.60-fold) at four or more weeks post-onset of infection when compared to an uninfected control group. There was also an increased risk of neurological symptoms found in this post-infection period; memory problems had a 1.44-fold increased risk, and concentration problems a 2.53-fold increased risk. Although analyses of only hospitalised or outpatient populations showed a similar risk of fatigue (RR 1.59) or shortness of breath (RR 2.78) to the analyses of all COVID-19 infections, those studies included in the SLR that reported risks from different COVID-19 populations consistently found a higher relative risk of symptoms in intensive care unit (ICU) patients compared to all hospitalised patients15. A higher relative risk was also observed in patients with severe infection compared to non-severe infection, and in and non-hospitalised subgroups compared to all COVID-19 infections (adjusted for prior healthcare use and comorbidities)15, 16, 38. These studies indicate that severity of infection may have a significant impact on the likelihood of developing long COVID.
While previous systematic reviews of long COVID have aimed to characterise its symptoms, prevalence, and risk factors, reviews and quantitative analyses of risks of common symptoms after infection reported studies with uninfected controls are still limited. A clear understanding of post-COVID symptom risk and prevalence is important for informing healthcare providers and healthcare systems to improve access to resources and investigate new therapeutic strategies. However, many long COVID symptoms are commonly found in the general population and can be caused by other illnesses and infections, while it is also possible that some symptoms, such as fatigue and headache, may have been worsened by other stresses or disruptions associated with the pandemic48. This review therefore confirms that SARS-CoV-2 infection, including non-severe infection, is associated with substantially increased risks of developing mid- and long-term symptoms after adjustments for factors such as demographic characteristics and comorbidities.
Some definitions of long COVID require infection to have occurred at least 12 weeks before symptoms. As we included all studies with a minimum follow-up of 4 weeks to enable us to capture a larger number of studies to perform meta-analyses for as many symptoms as possible, we also performed sensitivity analyses that included only those studies with outcomes reported 12 weeks after infection. Relative risks for these were similar to that of the main analyses for fatigue and shortness of breath; while the risk of memory problems was higher than the main analysis (RR 3.02 vs. RR 2.53), this increase was not significantly different and only three studies could be included in the sensitivity analysis.
Sensitivity analyses confirmed that the main analyses of risk of fatigue, shortness of breath, and cognition outcomes were robust, as only two sensitivity analyses resulted in a loss of statistical significance, and these analyses only included a small number of studies. Interestingly, sensitivity analyses including only studies estimated to include a pre-vaccination population found a higher risk ratio than the main analyses for fatigue, shortness of breath, and memory problems which may indicate that vaccination lowers risk of long COVID; however, this increase was not significant.
Health-related quality of life of people after COVID-19 infection compared to uninfected controls was also significantly lower in many or all domains when compared to non-hospitalised controls, but not compared to controls hospitalised for other non-COVID causes, and QoL differences between all COVID-19 infections and their controls were varied, with no statistical analysis of QoL outcomes performed in some studies. However, there is evidence from a number of studies that people with long COVID symptoms report an overall deterioration in quality of life. A recent meta-analysis reported the pooled prevalence of poor quality of life to be 59%49. In addition to having a decreased quality of life, patients with long COVID are also likely to report reduced mobility (36%), self-care (8%), and usual activities (28%), increased pain/discomfort (42%), and deteriorated psychological health (38%)49–51.
There is evidence that increasing age, female sex, socioeconomic deprivation, smoking, obesity, asthma, and poor pre-pandemic physical and mental health are some of the major risk factors for development of long COVID comorbidities9, 52, although we were unable to assess the impact of these on relative risk of long COVID symptoms due to a lack of comparable subpopulations between the included studies. While long COVID can develop regardless of the severity of the initial infection, the severity of the initial COVID-19 infection53, as well as the number of symptoms during acute illness, have been indicated as risk factors for long COVID54. Studies included in our review that stratified symptom risks by severity support this association, as subgroups of hospitalised patients had a higher risk of fatigue, shortness of breath, and neurocognitive decline than all COVID-19 patients, with an even higher risk for ICU patients15. Patients hospitalised with severe COVID-19 illness had a greater risk of cognitive impairment than those hospitalised with non-severe illness38.
There is increasing evidence that vaccination against SARS-CoV-2 may decrease the risk of long COVID development after infection. Two studies included in our review reported significantly lowered risks of fatigue and concentration in vaccinated infected cases compared to unvaccinated infected controls15, 24. Moreover, a recent systematic review identified 17 studies investigating the impact of COVID-19 vaccines before infection on risk or odds of long COVID, or on changes to long COVID symptoms. The six studies investigating the impact of vaccines before infection found that vaccination is associated with reduced risks, with preliminary evidence indicating that two vaccine doses are more effective than a single dose. Of the 11 studies investigating changes in long COVID symptoms after vaccination, seven studies showed improvements in symptoms at least one dose post-vaccination, while four studies reported either no change or worsening of symptoms55.
The variant of SARS-CoV-2 may also influence risk of long COVID. A case–control observational study of vaccinated participants using self-reported data from the UK COVID Symptom Study app found a significant reduction in risk of long COVID at least 4 weeks after infection with the Omicron variant compared to the Delta variant; adjusted odds ratios ranged from 0.24 to 0.50, depending on time since vaccination56. Data from the UK’s Office for National Statistics as of 27 May 2022 also show the unadjusted prevalence in triple-vaccinated adults of self-reported long COVID 12 to 16 weeks after infection was 4.5%, 4.2%, and 5.0% for infections compatible with Omicron BA.1, Omicron BA.2, or Delta variants, respectively, although there was no statistical evidence of differences between the three variants. Among double-vaccinated adults, the odds of reporting long COVID of any severity was 48.2% lower for the Omicron variant than Delta variant57.
Altogether, the immunity that has been globally built up following multiple infections, vaccinations and boosters, and evolving COVID-19 variants may mean that the risk of long COVID not only varies by country and continent, but is constantly changing as reinfections occur, new variants emerge and improved vaccines are introduced.
This study has a number of limitations. Firstly, it only focuses on a few of the most frequently occurring long COVID symptoms, while a wide range of symptoms associated with long COVID have been reported, including headache, chest pain, loss of smell, dizziness, depression and anxiety, sleep disruption, gastrointestinal issues, and joint, muscle and back pain48, 58. Secondly, a large amount of heterogeneity in study design, population and outcomes between studies was present. The different study designs of the studies in this review included retrospective, prospective and ambidirectional cohort studies, case–control studies and cross-sectional studies. Additionally, methods of comparing the infected population with the non-infected controls varied across studies. While we stratified patient populations into those that included all infected people and those from hospitals, some studies with hospital patients did not make it clear whether their population was exclusively people hospitalised for COVID-19 illness or for any reason. Two studies included records from hospital testing laboratories, and these were considered not representative of hospitalised patients or outpatients as they may have included regular testing for healthcare workers or visitors24, 26.
While some of the included studies reported outcomes for various subgroups, including age, sex, and infection severity, it was not possible to perform informative subgroup analyses due to lack of comparability and the low number of included studies reporting comparable subgroup data. COVID-19 variants at the time of the study were also poorly reported, and therefore a comparison of risks from different variants was not possible. Multiple time points and different outcome descriptions (particularly for cognition outcomes) were also reported by some studies, and although a feasibility assessment was performed in order to select the most comparable outcomes, this process still carries the risk of subjectivity. A need for standardised and validated COVID-19 research tools to improve the quality and reduce reporting variability has been highlighted by a previous review of long COVID59, and standardised symptom outcome descriptions may greatly improve future comparisons between studies. Finally, meta-analyses to determine the pooled reported impact of SARS-CoV-2 on quality of life could not be performed, due to the different HRQoL instruments used by the studies.
This review comprehensively summaries the evidence that COVID-19 infection is followed by a significant risk of fatigue, shortness of breath, and cognitive dysfunction, in both hospitalised and non-hospitalised populations, and hospitalised COVID-19 infections are associated with a lower quality of life in the months after illness. Further research is still necessary to clearly understand the impact of vaccination and acquired immunity on the development of long COVID, as well as the risk of long COVID associated with newer COVID-19 variants. However, the widespread extent of COVID-19 infection and reinfection in the global population will make future studies with confirmed uninfected controls difficult to perform.
Now that the wide breadth of COVID-19 symptoms is gradually becoming clearer, further research into their long-term prevalence is required. While our review identified some studies that reported risk of symptoms at multiple time points, the number of studies were sparse and the overall findings from these were inconclusive. Large cohort studies are necessary to fully understand the potential long-term effects of infection and persistence of symptoms in the years after infection, while the need for clinical trials to address the hypothesized underlying mechanisms of long COVID symptoms has also been acknowledged60.
Methods
Search strategy
This study was conducted in accordance with the Meta-analysis Of Observational Studies in Epidemiology61 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for conducting and reporting systematic reviews62. The study protocol was published via PROSPERO: International Prospective Register of Systematic Reviews (#CRD42022331682) and is available at the following link: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022331682.
MEDLINE (Ovid), MEDLINE, In-Process Citations, Daily Update & Epubs Ahead-of-Print (Ovid), EMBASE (Ovid), PubMed, National Library of Medicine LitCovid, WHO COVID-19, arXiv (https://arxiv.org/) and Europe PMC (https://europepmc.org/) were searched from January 2020 to March 2022, with no language restrictions. Searches were not limited by publication status (unpublished, published, in press, and in progress). The detailed search strategy is available in Supplementary Table S1. Hand-searching, including searching reference lists of relevant articles, was also performed.
Eligibility criteria, screening and abstraction
We included full publications meeting the following criteria: (1) non-interventional studies with a control group (including retrospective, prospective, and ambidirectional cohort studies, case–control studies, and cross-sectional studies; (2) conducted in people with SARS-CoV-2 infection diagnosed by testing or clinician-suspected; (3) uninfected controls (including those with COVID-19 symptoms but testing negative, and those with other respiratory infections); (4) reporting the relative risk of fatigue, shortness of breath, or cognitive dysfunction or health-related quality of life measured using validated questionnaires in the case populations compared to control populations; (5) reporting outcomes 4 weeks or more after SARS-CoV-2 infection (6) published from 2020 to the date of the search; and (7) full text in English.
Excluded publication types were editorials, letters, case reports or conference abstracts/proceedings. There was no limit on countries included.
Two reviewers (ZM and MG) independently performed two-stage screening (title/abstract and full text screening), with disagreement resolved by discussion. Data extraction and risk of bias assessment were performed by one reviewer, and a second independent reviewer conducted data checking. Data on study characteristics and the outcomes of interest were extracted.
Data were collected using a standardised data extraction form. Extracted data included the name of the geographical location of the study, data source or study setting, SARS-CoV-2 infection period, population characteristics (including size, age, sex, disease severity, and vaccination status), SARS-CoV-2 test, time between infection and outcomes, and symptom (fatigue, shortness of breath, cognitive dysfunction) risk or QoL outcomes. Risk outcomes extracted included hazard ratio, rate ratio, risk ratio, odds ratio, incidence rate ratio, standardised incidence rate, absolute risk increase, or risk difference measures with 95% confidence intervals (CIs), and the risk description used and adjustments performed. QoL outcomes extracted included the instrument and domains used, and QoL scores or descriptions.
Where the SARS-CoV-2 variant or variants in the study were not reported, circulating variants at the time of the studies’ SARS-CoV-2 infection period were estimated by reviewers using global and national COVID-19 variant surveillance data sources for the included countries.
Quality assessment
Risk of bias was assessed by a modified Newcastle–Ottawa scale, which assessed study quality in three domains: (1) selection of the study groups; (2) comparability of cohorts on the basis of the design or analysis; and (3) ascertainment of outcomes of interest (Supplementary Table S2). Studies were classified as low risk of bias if they scored 7–9 overall, 4–6 for medium risk of bias, and 0–3 for high risk of bias.
Statistical analysis
Pairwise meta-analyses were performed for the risk of fatigue, shortness of breath, and cognitive dysfunction outcomes. A feasibility assessment was performed to determine whether it was recommended to combine identified studies in a pairwise meta-analysis, based on study population source, cases and controls, participant characteristics (including age, vaccination status, and disease severity), SARS-CoV-2 infection periods, and outcome reporting. Timepoints reported in the studies were assessed, and the risks from the most comparable timepoints across studies included in the analysis. Where multiple outcome descriptions were reported, the broadest description was used in the analysis. Odds ratios, hazard ratios, rate ratios, and prevalence ratios were considered equal estimates63. All are referred to in this paper as ‘risk ratios’ (RR), and the most adjusted RR were log transformed and used in analysis. Absolute risk increases and risk differences were not included in any analyses. Weights were calculated using the inverse variance method (weight = 1/variance). Random-effects DerSimonian and Laird models64 were fitted to calculate pooled RR and 95% CI for all outcomes.
Heterogeneity was measured using the Cochran’s Q statistic with statistical significance set at P < 0.10 (due to a limitation of the Q test that it may be underpowered when the number of studies is low, a higher P-value threshold for statistical significance is recommended in these situations) and quantified by the I2 test. Publication bias was assessed with funnel plots and the Egger’s test65.
The robustness of the results was evaluated using the leave-1-out method66 to assess the effect on pooled estimates of removing individual studies. Subgroup analyses of hospitalised or outpatient studies were also performed where possible. A range of sensitivity analyses were conducted where possible, and included (1) only studies that had a minimum of 12 weeks between infection and the reporting of symptoms; (2) addition of a single study removed for potential population overlap; (3) inclusion of children-only studies; (4) only studies where SARS-CoV-2 infection occurred before introduction of COVID-19 vaccination; (5) removal of non-adjusted risks; and (6) exclusion of pre-print studies. Sensitivity analyses were performed if three or more studies could be included in the analysis.
All statistical analyses were conducted using R version 3.5.1, using the packages metafor and forestplot.
Supplementary Information
Acknowledgements
We acknowledge the support from Valentine Delore in the design, and Lorenzo Bertizzolo and Rebecca C Harris in the conceptualisation of this review.
Author contributions
N.S., C.E.G.S., S.L., C.T., K.M. and Z.M. conceived and designed this study. K.M. devised the search strategies and performed the literature searching. Z.M. and M.G. performed initial screening, a review of full texts for eligibility, and extracted the data. Z.M. conducted the data analysis. N.S., C.E.G.S., S.L., C.T. and Z.M.: conducted the data interpretation. Z.M. drafted the final manuscript and prepared the tables and figures. S.L., C.T., N.S., and C.E.G.S. provided critical analysis and made revisions of the manuscript and important intellectual contributions. All authors reviewed the manuscript before final submission.
Funding
Funding was provided by Sanofi.
Data availability
All data analysed in this work were extracted from published materials. Additional extracted data can be obtained upon reasonable request from the corresponding author, Z.M.
Competing interests
Review funded by Sanofi. Sean Leng and Carlo Tascini have no conflicts to declare. Nabila Shaikh and Clotilde El Guerche Seblain are employees of Sanofi and hold stock and/or stock options in the company. Zoe Marjenberg, Megha Garg and Kate Misso are employees of Maverex Ltd and received funding for their role in conducting the SLR.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-42321-9.
References
- 1.NICE. Overview|COVID-19 rapid guideline: managing the long-term effects of COVID-19 | Guidance|NICE. 1–111 https://www.nice.org.uk/guidance/ng188 (2021).
- 2.Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 3.Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022;22:e102–e107. doi: 10.1016/S1473-3099(21)00703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. 27 file:///C:/Users/pbradley/Downloads/WHO-2019-nCoV-Post-COVID-19-condition-Clinical-case-definition-2021.1-eng.pdf (2021).
- 5.Michelen M, et al. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021;6:e005427. doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen C, et al. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. J. Infect. Dis. 2022 doi: 10.1093/INFDIS/JIAC136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han Q, Zheng B, Daines L, Sheikh A. Long-term sequelae of COVID-19: A systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens. 2022;11:269. doi: 10.3390/pathogens11020269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ceban F, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav. Immun. 2022;101:93–135. doi: 10.1016/j.bbi.2021.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson EJ, et al. Long COVID burden and risk factors in 10 UK longitudinal studies and electronic health records. Nat. Commun. 2022;13(1):1–11. doi: 10.1038/s41467-022-30836-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rao S, et al. Fatigue symptoms associated with COVID-19 in convalescent or recovered COVID-19 patients; a systematic review and meta-analysis. Ann. Behav. Med. 2022;56:219–234. doi: 10.1093/abm/kaab081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopez-Leon S, et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021;11:16144. doi: 10.1038/s41598-021-95565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernández-de-las-Peñas C, et al. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur. J. Intern. Med. 2021;92:55–70. doi: 10.1016/j.ejim.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michelen M, et al. Characterising long COVID: A living systematic review. BMJ Glob. Health. 2021;6:5427. doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Organization, W. H. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (2021).
- 15.Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. 2022;28:1461–1467. doi: 10.1038/s41591-022-01840-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594:259–264. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]
- 17.Amin-Chowdhury Z, et al. Characterising long COVID more than 6 months after acute infection in adults; prospective longitudinal cohort study, England. medRxiv. 2021 doi: 10.1101/2021.03.18.21253633. [DOI] [Google Scholar]
- 18.Borch L, Holm M, Knudsen M, Ellermann-Eriksen S, Hagstroem S. Long COVID symptoms and duration in SARS-CoV-2 positive children—A nationwide cohort study. Eur. J. Pediatr. 2022;181:1597–1607. doi: 10.1007/s00431-021-04345-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Caspersen IH, Magnus P, Trogstad L. Excess risk and clusters of symptoms after COVID-19 in a large Norwegian cohort. Eur. J. Epidemiol. 2022;37:539. doi: 10.1007/s10654-022-00847-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castro VM, Rosand J, Giacino JT, McCoy TH, Perlis RH. Case-control study of neuropsychiatric symptoms in electronic health records following COVID-19 hospitalization in 2 academic health systems. Mol. Psychiatry. 2022 doi: 10.1038/s41380-022-01646-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chevinsky JR, et al. Late conditions diagnosed 1–4 months following an initial coronavirus disease 2019 (COVID-19) encounter: A matched-cohort study using inpatient and outpatient administrative data-United States, 1 March-30 June 2020. Clin. Infect. Dis. 2021;73:S5–S16. doi: 10.1093/cid/ciab338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desgranges F, et al. Post-COVID-19 syndrome in outpatients: A cohort study. J. Gen. Intern. Med. 2022;37:1943–1952. doi: 10.1007/s11606-021-07242-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kikkenborg Berg S, et al. Long COVID symptoms in SARS-CoV-2-positive adolescents and matched controls (LongCOVIDKidsDK): A national, cross-sectional study. Lancet Child Adolesc. Health. 2022;6:240–248. doi: 10.1016/S2352-4642(22)00004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuodi P, et al. Association between vaccination status and reported incidence of post-acute COVID-19 symptoms in Israel: A cross-sectional study of patients tested between March 2020 and November 2021. medRxiv. 2022 doi: 10.1101/2022.01.05.22268800. [DOI] [Google Scholar]
- 25.Matta J, et al. Association of self-reported COVID-19 infection and SARS-CoV-2 serology test results with persistent physical symptoms among french adults during the COVID-19 pandemic. JAMA Intern. Med. 2022;182:19–25. doi: 10.1001/jamainternmed.2021.6454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noviello D, et al. Functional gastrointestinal and somatoform symptoms five months after SARS-CoV-2 infection: A controlled cohort study. Neurogastroenterol. Motil. 2022;34:e14187. doi: 10.1111/nmo.14187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rivera-Izquierdo M, et al. Long COVID 12 months after discharge: persistent symptoms in patients hospitalised due to COVID-19 and patients hospitalised due to other causes—A multicentre cohort study. BMC Med. 2022;20:92. doi: 10.1186/s12916-022-02292-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roessler M, et al. Post COVID-19 in children, adolescents, and adults: Results of a matched cohort study including more than 150,000 individuals with COVID-19. medRxiv. 2021 doi: 10.1101/2021.10.21.21265133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roge I, et al. Comparison of persistent symptoms after COVID-19 and other non-SARS-CoV-2 infections in children. Front. Pediatr. 2021;9:752385. doi: 10.3389/fped.2021.752385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sørensen AIV, et al. A nationwide questionnaire study of post-acute symptoms and health problems after SARS-CoV-2 infection in Denmark. Nat. Commun. 2022;13(1):1–8. doi: 10.1038/s41467-022-31897-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spotnitz, M., Hripcsak, G., Ryan, P., medRxiv, K. N.- & 2021, undefined. Characterizing post-acute sequelae of SARS-CoV-2 infection across claims and electronic health record databases. medrxiv.org10.1101/2021.03.19.21253756.
- 32.Strahm C, et al. Symptoms compatible with long coronavirus disease (COVID) in healthcare workers with and without severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection—Results of a prospective multicenter cohort. Clin. Infect. Dis. 2022 doi: 10.1093/cid/ciac054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taquet M, et al. Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18:e1003773. doi: 10.1371/journal.pmed.1003773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xie Y, Bowe B, Al-Aly Z. Burdens of post-acute sequelae of COVID-19 by severity of acute infection, demographics and health status. Nat. Commun. 2021;12:6571. doi: 10.1038/s41467-021-26513-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nielsen KJ, et al. Day-by-day symptoms following positive and negative PCR tests for SARS-CoV-2 in non-hospitalized healthcare workers: A 90-day follow-up study. Int. J. Infect. Dis. 2021;108:382–390. doi: 10.1016/j.ijid.2021.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petersen EL, et al. Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme. Eur. Heart J. 2022;43:1124–1137. doi: 10.1093/eurheartj/ehab914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carazo S, et al. Physical, psychological and cognitive profile of post-COVID condition in healthcare workers, Quebec, Canada. medRxiv. 2022 doi: 10.1101/2022.03.08.22272057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu YH, et al. One-year trajectory of cognitive changes in older survivors of COVID-19 in Wuhan, China: A longitudinal cohort study. JAMA Neurol. 2022;79:509–517. doi: 10.1001/jamaneurol.2022.0461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elkan M, et al. Patient-reported outcome measures after hospitalization during the covid-19 pandemic: A survey among covid-19 and non-COVID-19 patients. Int. J. Gen. Med. 2021;14:4829–4836. doi: 10.2147/IJGM.S323316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang C, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Niyatiwatchanchai N, et al. Comparative study of early impacts of post-COVID-19 pneumonia on clinical manifestations, pulmonary function, and chest radiographs. Medicina. 2022;58:216. doi: 10.3390/medicina58020216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Raman B, et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine. 2021;31:100683. doi: 10.1016/j.eclinm.2020.100683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vlake JH, et al. Psychological distress and health-related quality of life in patients after hospitalization during the COVID-19 pandemic: A single center, observational study. PLoS ONE. 2021;16:e0255774. doi: 10.1371/journal.pone.0255774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Søraas A, et al. Persisting symptoms three to eight months after non-hospitalized COVID-19, a prospective cohort study. PLoS ONE. 2021;16:e0256142. doi: 10.1371/journal.pone.0256142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Søraas A, et al. Self-reported memory problems 8 months after COVID-19 infection. JAMA Netw. Open. 2021;4:e2118717–e2118717. doi: 10.1001/jamanetworkopen.2021.18717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stephenson T, et al. Physical and mental health 3 months after SARS-CoV-2 infection (long COVID) among adolescents in England (CLoCk): A national matched cohort study. Lancet Child Adolesc. Health. 2022;6:230–239. doi: 10.1016/S2352-4642(22)00022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Radtke T, Ulyte A, Puhan MA, Kriemler S. Long-term symptoms after SARS-CoV-2 infection in children and adolescents. JAMA. 2021;326:869–871. doi: 10.1001/jama.2021.11880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ballering AV, van Zon SKR, olde Hartman TC, Rosmalen JGM. Persistence of somatic symptoms after COVID-19 in the Netherlands: An observational cohort study. Lancet. 2022;400:452–461. doi: 10.1016/S0140-6736(22)01214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Malik P, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)—A systematic review and meta-analysis. J. Med. Virol. 2022;94:253. doi: 10.1002/jmv.27309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Halpin SJ, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J. Med. Virol. 2021;93:1013–1022. doi: 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
- 51.Han JH, et al. Associations between persistent symptoms after mild COVID-19 and long-term health status, quality of life, and psychological distress. Influenza Respir. Viruses. 2022;16:680–689. doi: 10.1111/irv.12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Subramanian A, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat. Med. 2022;28:1706–1714. doi: 10.1038/s41591-022-01909-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Prevalence of post COVID-19 condition symptoms: a systematic review and meta-analysis of cohort study data, stratified by recruitment setting. European Centre for Disease Prevention and Controlhttps://www.ecdc.europa.eu/en/publications-data/prevalence-post-covid-19-condition-symptoms-systematic-review-and-meta-analysis (2022).
- 54.Augustin M, et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: A longitudinal prospective cohort study. Lancet Reg. Health Eur. 2021;6:100122. doi: 10.1016/j.lanepe.2021.100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Notarte KI, et al. Impact of COVID-19 vaccination on the risk of developing long-COVID and on existing long-COVID symptoms: A systematic review. EClinicalMedicine. 2022;53:101624. doi: 10.1016/j.eclinm.2022.101624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Antonelli M, Pujol JC, Spector TD, Ourselin S, Steves CJ. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet. 2022;399:2263–2264. doi: 10.1016/S0140-6736(22)00941-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ayoubkhani, D. & Bosworth, M. Self-reported long COVID after infection with the Omicron variant in the UK - Office for National Statistics. UK Office for National Statisticshttps://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidafterinfectionwiththeomicronvariant/18july2022 (2022).
- 58.Perlis RH, et al. Prevalence and correlates of long COVID symptoms among US adults. JAMA Netw Open. 2022;5:e2238804. doi: 10.1001/jamanetworkopen.2022.38804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Michelen M, et al. Characterising long COVID: A living systematic review. BMJ Glob. Health. 2021 doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023 doi: 10.1038/s41579-022-00846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brooke B, Shwartz T, Pawlik T. MOOSE reporting guidelines for meta-analyse of observational studies. JAMA Surg. 2021;156:787–788. doi: 10.1001/jamasurg.2021.0522. [DOI] [PubMed] [Google Scholar]
- 62.Page MJ, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol. Rev. 1987;9:1–30. doi: 10.1093/oxfordjournals.epirev.a036298. [DOI] [PubMed] [Google Scholar]
- 64.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 65.Stuck AE, Rubenstein LZ, Wieland D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. BMJ. 1998;316:469–469. [PMC free article] [PubMed] [Google Scholar]
- 66.Viechtbauer W. Conducting meta-analyses in R with the metafor. J. Stat. Softw. 2010;36:1–48. [Google Scholar]
- 67.Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med.151, 264–9, W64 (2009) [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data analysed in this work were extracted from published materials. Additional extracted data can be obtained upon reasonable request from the corresponding author, Z.M.