Abstract
Background:
Differences in social and environmental factors can contribute to disparities in fatal injury rates. The purpose of this study was to examine the relationship between social and environmental factors and unintentional fatal injury across counties in the United States and how this relationship varies by geography.
Methods:
County-level vital statistics on age-adjusted unintentional fatal injury rates for 2015–2019 were linked with county-level data from the 2018 Social Vulnerability Index (SVI), a dataset identifying socially vulnerable communities. We conducted linear regression to examine the association between SVI and unintentional fatal injury, overall and by Census region/division. We mapped county-level data for SVI and unintentional fatal injury rates in bivariate choropleth maps using quartiles.
Results:
SVI was positively associated with unintentional fatal injury (β = 18.29, p < 0.001) across U.S. counties. The geographic distribution of SVI and unintentional fatal injury rates varied spatially and substantially for U.S. counties, with counties in the South and West regions having the greatest levels of SVI and rates of unintentional fatal injury.
Conclusions:
Our findings demonstrate that the social vulnerability of counties is associated with unintentional fatal injury rates. Modification of the SVI for injury research could include additional social determinants and exclude variables not applicable to injuries. A modified SVI could inform unintentional injury prevention strategies by prioritizing efforts in areas with high levels of social vulnerability.
Practical Applications:
This study is the first step in combining the SVI and injury mortality data to provide researchers with an index to investigate upstream factors related to injury.
Keywords: Social vulnerability Disparities, Health equity, Injury prevention, Social determinants of health
1. Background
Unintentional injury (e.g., motor vehicle crashes, drownings, falls) is the leading cause of death for children and adults between one and 45 years of age in the United States (U.S.) (CDC, 2021). Identifying the social and environmental risk factors for fatal injury may be critical in decreasing the public health burden of these injuries.
Risk factors for unintentional fatal injuries differ by injury type and mechanism, sociodemographic characteristics, and geographic location (Burns & Kakara, 2018; Clemens, 2021; Henning-Smith & Kozhimannil, 2018). Many injuries disproportionately affect subgroups of the U.S. population. For instance, American Indian/Alaska Native persons have an unintentional injury mortality rate that is 2.4 times higher than that of White non-Hispanic persons for years 2005–2009 (Murphy et al., 2014). Additionally, unintentional injury death rates differ across the U.S., with generally higher rates in the Southeast and lower rates in Northeast, illustrating the role of geography in influencing injury risk (Ballesteros et al., 2018).
Research indicates social and environmental factors are strong contributors to unintentional injury risk (Mercy et al., 2008). Differences in social and environmental factors, such as housing conditions and socioeconomic status, can contribute to disparities in injury (Roberts & Meddings, 2010). Identifying social and environmental determinants can provide researchers and public health professionals with a better understanding of upstream factors influencing injury outcomes to address health inequities in injuries. Injury prevention programs can focus on individual-level factors impacting injury risk and community-level prevention strategies. Focusing on community-level factors can improve our knowledge of underlying and upstream causes and possible shared risk and protective factors for injury and may improve community-level public health prevention efforts.
The purpose of our ecological study was to address the broad category of unintentional fatal injury rates, recognizing there are significant similarities and differences among risk factors, as a first step to assessing the influence of social vulnerability on injuries. Using the Centers for Disease Control and Prevention’s (CDC) 2018 Social Vulnerability Index (SVI),1 we examined the relationship between unintentional fatal injury outcomes and social vulnerability (i.e., demographic and socioeconomic factors that contribute to risk for being adversely affected by community-level stressors that cause disease and injury) and assessed this relationship by geography. Based on a literature review, we hypothesized higher levels of social vulnerability are associated with higher unintentional injury death rates, and the strength of these associations varies by region.
2. Methods
2.1. Measures
County-level data on age-adjusted unintentional fatal injury rates for 2015–2019 were obtained from the National Vital Statistics System through a data use agreement from the National Center for Health Statistics (NCHS).2
Fatal injury was defined based on the underlying cause of death, following definitions established in the NCHS injury intent by injury mechanism matrix applicable to the International Classification for Diseases 10th edition (ICD-10) (World Health Organization, 2004). Unintentional fatal injury was defined by ICD-10 codes V01-X59 and Y85-Y86 (e.g., falls, motor vehicle traffic crashes, poisonings, drownings). All rates were age-adjusted using the direct method (Clayton & Hills, 1993) and the year 2000 U.S. standard population.
County-level data on social vulnerability were obtained from the CDC’s 2018 SVI, a publicly available dataset that identifies the most socially vulnerable communities in the U.S. based on social determinants of health (Flanagan et al., 2011). The SVI ranks all U.S. counties and census tracts on a scale of 0 to 1 regarding social vulnerability, with 1 representing the highest level of social vulnerability and ranked within the U.S. (Flanagan et al., 2018). The SVI was originally developed to assist communities with preparing for and responding to public health emergencies (Flanagan et al., 2011, 2018) and continues to be applied for such purposes, such as the COVID-19 pandemic (Amram et al., 2020; Hughes et al., 2021; Karaye & Horney, 2020; Nayak et al., 2020). Recently, researchers have applied the SVI to various health outcomes (An & Xiang, 2015a; Gay et al., 2016; Yee et al., 2019), but there are few applications of injury-related outcomes (Morgan et al., 2020). For the analysis, we included data for overall SVI, the four SVI domains,3 and the 15 SVI indicators.
Census geographic regions and divisions (United States Census Bureau, 2018) were defined by the four U.S. Census regions (Northeast, Midwest, South, and West) and the nine U.S. Census divisions (New England, Middle Atlantic, East North Central, West North Central, South Atlantic, East South Central, West South Central, Mountain, and Pacific) in accordance with the U.S. Census Bureau, respectively. Due to the nature of this study, it was not appropriate or possible to involve patients or the public in the design, conduct, reporting, or dissemination plans of this study.
2.2. Data analysis
Descriptive statistics were calculated to obtain mean age-adjusted rates and 95% confidence intervals for unintentional fatal injury rates by SVI metrics (overall SVI, the four SVI domains, and the 15 SVI indicators). SVI scores for each metric were categorized into quartiles as follows: low (0.0–0.2500), mid-low (0.2501–0.5000), mid-high (0.5001–0.7500), and high (0.7501–1.0) social vulnerability, based on previous studies (An & Xiang, 2015b; Dasgupta et al., 2020; Yee et al., 2019).
To examine the relationship between SVI and unintentional fatal injury rates, we conducted linear regression models with SVI coded as a continuous variable on the 0–1 scale. We evaluated scatterplots and linear fit tests to confirm linear regression was appropriate. Our analysis was stratified by Census region and division. Pearson’s bivariate correlation analysis was performed between each SVI domain to ensure no strong correlation occurred between domains. A sensitivity analysis was performed using a negative binomial regression.
To visualize the relationship between SVI and unintentional injury, we mapped county-level data for overall SVI and unintentional fatal injury rates in a bivariate choropleth map using quartile classification.4 All statistical analyses were conducted in STATA 16.0 MP-Parallel Edition, and all mapping was conducted using ArcMap version 10.8 (Esri, Redlands, CA).
3. Results
3.1. Descriptive analysis
Of the 3,142 total U.S. counties, we analyzed 3,141 counties based on available data. One county was missing data for SVI due to data collection errors reported by the U.S. Census Bureau that prohibited the inclusion of income and poverty data. All other data were accounted for in the model estimates and quartile derivation. However, only counties that met NCHS data suppression rules5 were included in the figures, so ultimately 2,983 (94.9%) counties were included in the mapping.
Counties with higher overall SVI had higher mean age-adjusted rates for unintentional fatal injury (Table 1). The Socioeconomic Status domain and Household Composition and Disability domain had similar patterns with unintentional fatal injury, with increasing injury rates as social vulnerability in these domains increased (Socioeconomic Status domain: 49.25 per 100,000 population for the low SVI quartile vs. 68.45 per 100,000 population for the high SVI quartile; Household Composition and Disability domain: 48.74 per 100,000 population for the low SVI quartile vs. 66.06 per 100,000 population for the high SVI quartile). Counties with low SVI had higher overall unintentional rates (62.04 per 100,000 population) in the Minority Status and Language domain than counties with high SVI (54.98 per 100,000 population). Unintentional injury rates in the Housing Type and Transportation domain were similar across SVI levels (55.72 per 100,000 population for the low SVI quartile vs. 59.73 per 100,000 population for the high SVI quartile). There was variation among the 15 SVI indicators, with most indicators following the same pattern as the overall domain. For example, within the Socioeconomic Status domain, for the Below Poverty Line indicator, unintentional fatal injury rates increased as social vulnerability in this indicator increased.
Table 1.
Mean age-adjusted ratesa per 100,000 population for unintentional fatal injury (CI) by Social Vulnerability Index (SVI) quartileb,c,d – United States.
| Mean age-adjusted rate for unintentional fatal injury | ||||
|---|---|---|---|---|
| SVI metric | Low SVI | Mid-low SVI | Mid-high SVI | High SVI |
| Overall SVI | 50.97 (49.64, 52.31) | 56.34 (55.06, 57.62) | 62.04 (60.73, 63.35) | 65.01 (63.40, 66.62) |
| Socioeconomic status | ||||
| Overall domain | 49.25 (47.97, 50.54) | 55.82 (54.64, 57.00) | 60.84 (59.53, 62.14) | 68.45 (66.84, 70.05) |
| Below poverty level | 50.23 (48.93, 51.54) | 56.50 (55.27, 57.73) | 60.92 (59.64, 62.20) | 66.95 (65.30, 68.60) |
| Unemployment | 52.13 (50.77, 53.50) | 56.18 (54.92, 57.43) | 59.04 (57.88, 60.20) | 67.46 (65.74, 69.18) |
| Per capita income | 49.59 (48.37, 50.81) | 55.40 (54.17, 56.62) | 62.24 (60.86, 63.61) | 67.14 (65.55, 68.74) |
| No high school diploma | 50.31 (49.05, 51.57) | 57.12 (55.89, 58.36) | 62.12 (60.68, 63.57) | 65.24 (63.67, 66.81) |
| Household composition and disability | ||||
| Overall domain | 48.74 (47.50, 49.99) | 55.80 (54.66, 56.93) | 60.39 (59.18, 61.60) | 66.06 (64.62, 67.51) |
| Age ≥ 65 years | 53.64 (52.01, 55.27) | 58.75 (57.44, 60.06) | 60.37 (59.12, 61.62) | 61.64 (60.15, 63.13) |
| Age ≤ 17 years | 58.91 (57.49, 60.32) | 59.51 (58.13, 60.89) | 57.93 (56.68, 59.17) | 58.00 (56.31, 59.69) |
| Disability status | 49.19 (47.85, 50.52) | 56.59 (55.18, 58.00) | 60.58 (59.32, 61.85) | 68.26 (66.85, 69.67) |
| Single-parent household | 56.58 (55.05, 58.11) | 57.58 (56.27, 58.89) | 58.93 (57.67, 60.19) | 61.39 (59.77, 63.01) |
| Minority status and language | ||||
| Overall domain | 62.04 (60.55, 63.53) | 51.40 (50.37, 52.43) | 53.20 (52.19, 54.21) | 54.98 (53.55, 56.41) |
| Racial/ethnic minority | 60.54 (59.04, 62.04) | 57.52 (56.21, 58.83) | 57.56 (56.37, 58.75) | 58.73 (57.03, 60.43) |
| Limited English | 63.98 (62.48, 65.48) | 58.30 (56.88, 59.71) | 57.05 (55.77, 58.33) | 53.74 (52.36, 55.11) |
| Housing type and transportation | ||||
| Overall domain | 55.72 (54.26, 57.19) | 52.16 (51.14, 53.18) | 54.85 (53.71, 55.98) | 59.73 (58.15, 61.30) |
| Multi-unit housing | 65.64 (64.02, 67.27) | 61.68 (60.28, 63.08) | 57.29 (56.02, 58.55) | 49.48 (48.34, 50.61) |
| Mobile homes | 50.75 (49.37, 52.14) | 55.52 (54.24, 56.80) | 60.64 (59.26, 62.03) | 67.54 (66.11, 68.98) |
| Crowded housing | 56.16 (54.73, 57.59) | 58.14 (56.89, 59.39) | 59.94 (58.65, 61.23) | 60.35 (58.60, 62.10) |
| No vehicle | 54.58 (53.16, 55.99) | 57.47 (56.22, 58.71) | 58.68 (57.51, 59.86) | 63.87 (62.07, 65.68) |
| Group quarters | 59.51 (57.96, 61.07) | 58.70 (57.43, 59.96) | 60.26 (58.78, 61.74) | 56.01 (54.58, 57.44) |
Notes: CI: 95% confidence intervals.
Age-adjusted rates per 100,000 population were calculated using the direct method and the 2000 U.S. standard population.
SVI scores were categorized into quartiles: Low (0–0.2500); Mid-low (0.2501–0.5000); Mid-high (0.5001–0.7500); High (0.7501–1.0).
Data for SVI from 2018; Data for fatal injury from 2015–2019.
Overall SVI, the four SVI domains, and the 15 SVI indicators were defined and calculated by Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
3.2. Associations between social vulnerability and unintentional fatal injury
In the linear regression analyses, social vulnerability was associated with unintentional fatal injury rates (Table 2). Overall SVI was positively associated with unintentional fatal injury rates across 3,141 U.S. counties (β = 18.29, SE = 1.22, p < 0.001); therefore for each quartile increase in overall SVI, there was an additional 4.57 unintentional fatal injuries per 100,000 population.
Table 2.
Association between Social Vulnerability Index (SVI) metricsa and age-adjusted unintentional fatal injury ratesb (per 100,000 population)c– United States.
| SVI metric | β | SE | 95% CI |
|---|---|---|---|
| Overall SVI | 18.29** | 1.22 | (15.89, 20.69) |
| Domain 1 Socioeconomic Status | 24.96** | 1.74 | (21.55, 28.37) |
| Domain 2 Household Composition and Disability | 7.83** | 1.51 | (4.88, 10.79) |
| Domain 3 Minority Status and Language | −13.28** | 1.27 | (−15.77, −10.79) |
| Domain 4 Housing Type and Transportation | −3.70* | 1.47 | (−6.59, −0.82) |
p < 0.05;
p < 0.001.
Notes: CI: confidence intervals; SE: standard error.
Overall SVI and the four SVI domains were defined and calculated by Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
Age-adjusted rates per 100,000 population were calculated using the direct method and the 2000 U.S. standard population.
Data for SVI from 2018; Data for fatal injury from 2015 to 2019.
Among the four SVI domains, the Socioeconomic Status domain (β = 24.96, SE = 1.74, p < 0.001) and Household Composition and Disability domain (β = 7.83, SE = 1.51, p < 0.001) were positively associated with unintentional fatal injury rates. The Minority and Language Status domain (β = −13.28, SE = 1.27, p < 0.001) and Housing Type and Transportation domain (β = −3.70, SE = 1.47, p < 0.05) were negatively associated with unintentional fatal injury rates.
The results of the negative binomial regression were consistent with the main specification. Due to the scatterplot showing a linear relationship, the linear regression results were presented.
3.3. Geographic distribution
In linear regression analyses, social vulnerability was also associated with unintentional fatal injury rates by Census region/division (Table 3). The strongest association occurred in the Midwest (β = 28.17, SE = 2.47, p < 0.001) and West (β = 24.38, SE = 3.96, p < 0.001) regions. Specifically, the Pacific (β = 33.38, SE = 8.74, p < 0.001), West North Central (b = 31.61, SE = 3.51, p < 0.001), and Mountain (β = 26.54, SE = 4.19, p < 0.001) divisions had the strongest associations between unintentional fatal injury and social vulnerability. No association between unintentional fatal injury and social vulnerability was found in the Northeast region or its respective divisions as well as in the East South Central and West South Central divisions in the South.
Table 3.
Association between Social Vulnerability Index (SVI)a and age-adjusted unintentional fatal injury ratesb (per 100,000 population) by Census regionc and divisiond,e– United States.
| Counties | Unintentional fatal injury | |||
|---|---|---|---|---|
| Census region and division | n (%) | β | SE | 95% CI |
| Northeast | 217 (6.9) | −4.52 | 5.17 | (−14.70, 5.66) |
| Division 1: New England | 67 (2.1) | 13.61 | 7.17 | (−0.71, 27.94) |
| Division 2: Middle Atlantic | 150 (4.8) | −4.33 | 6.95 | (−18.07, 9.41) |
| Midwest | 1055 (33.6) | 28.17 *** | 2.47 | (23.33, 33.02) |
| Division 3: East North Central | 437 (13.9) | 21.61*** | 3.29 | (15.14, 28.08) |
| Division 4: West North Central | 618 (19.7) | 31.61*** | 3.51 | (24.73, 38.50) |
| South | 1422 (45.3) | 10.25 *** | 2.01 | (6.32, 14.19) |
| Division 5: South Atlantic | 588 (18.7) | 14.52*** | 2.66 | (9.30, 19.75) |
| Division 6: East South Central | 364 (11.6) | 7.22 | 4.36 | (−1.36, 15.80) |
| Division 7: West South Central | 470 (14.9) | 4.41 | 3.91 | (−3.27, 12.10) |
| West | 447 (14.2) | 24.38 *** | 3.96 | (16.60, 32.17) |
| Division 8: Mountain | 280 (8.9) | 26.54*** | 4.19 | (18.30, 34.79) |
| Division 9: Pacific | 167 (5.3) | 33.38*** | 8.74 | (16.13, 50.64) |
p < 0.001.
Notes: CI: confidence intervals; SE: standard error.
Overall SVI was defined and calculated by Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
Age-adjusted rates per 100,000 population were calculated using the direct method and the 2000 U.S. standard population.
U.S. Census Bureau defines geographic Census regions as follows: Northeast—CT, ME, MA, NH, NJ, NY, PA, RI, VT; Midwest—IL, IN, IA, KS, MI, MN, MO, NE, ND, OH, SD, WI; South—AL, AR, DE, DC, FL, GA, KY, LA, MD, MS, NC, OK, SC, TN, TX, VA, WV; West— AK, AZ, CA, CO, HI, ID, MT, NV, NM, OR, UT, WA, WY.
U.S. Census Bureau defines geographic Census divisions as follows: New England—ME, NH, VT, MA, RI; Middle Atlantic—NY, PA, CT, NJ; East North Central—WI, IL, MI, IN, OH; West North Central—ND, SD, NE, KS, MN, IA, MO; South Atlantic—DE, MD, DC, WV, VA, NC, SC, GA, FL; East South Central—KY, TN, MS, AL; West South Central—TX, OK, AR, LA; Mountain—MT, ID, WY, NV, UT, AZ, CO, NM; Pacific—WA, OR, CA, AK, HI.
Data for SVI from 2018; Data for fatal injury from 2015–2019.
The geographic distribution between overall SVI and unintentional fatal injury rates varies by U.S. county (Fig. 1). The blue shades indicate counties with higher levels of overall social vulnerability, and the gold shades indicate counties with higher rates of unintentional fatal injury, with the black shade indicating counties with both high levels of overall social vulnerability and unintentional fatal injury rates. Approximately 9.1% (271/2,983) of counties with complete data had both high levels of overall social vulnerability and unintentional fatal injury rates, with most of these counties located in the southern and western states of New Mexico (39.4%; 13/33 counties), Oklahoma (33.8%; 26/77), Kentucky (28.3%; 34/120), Mississippi (28.0%; 23/82), Louisiana (17.2%; 11/64), North Carolina (17.0%; 17/100), and Georgia (10.7%; 17/159).
Fig. 1.
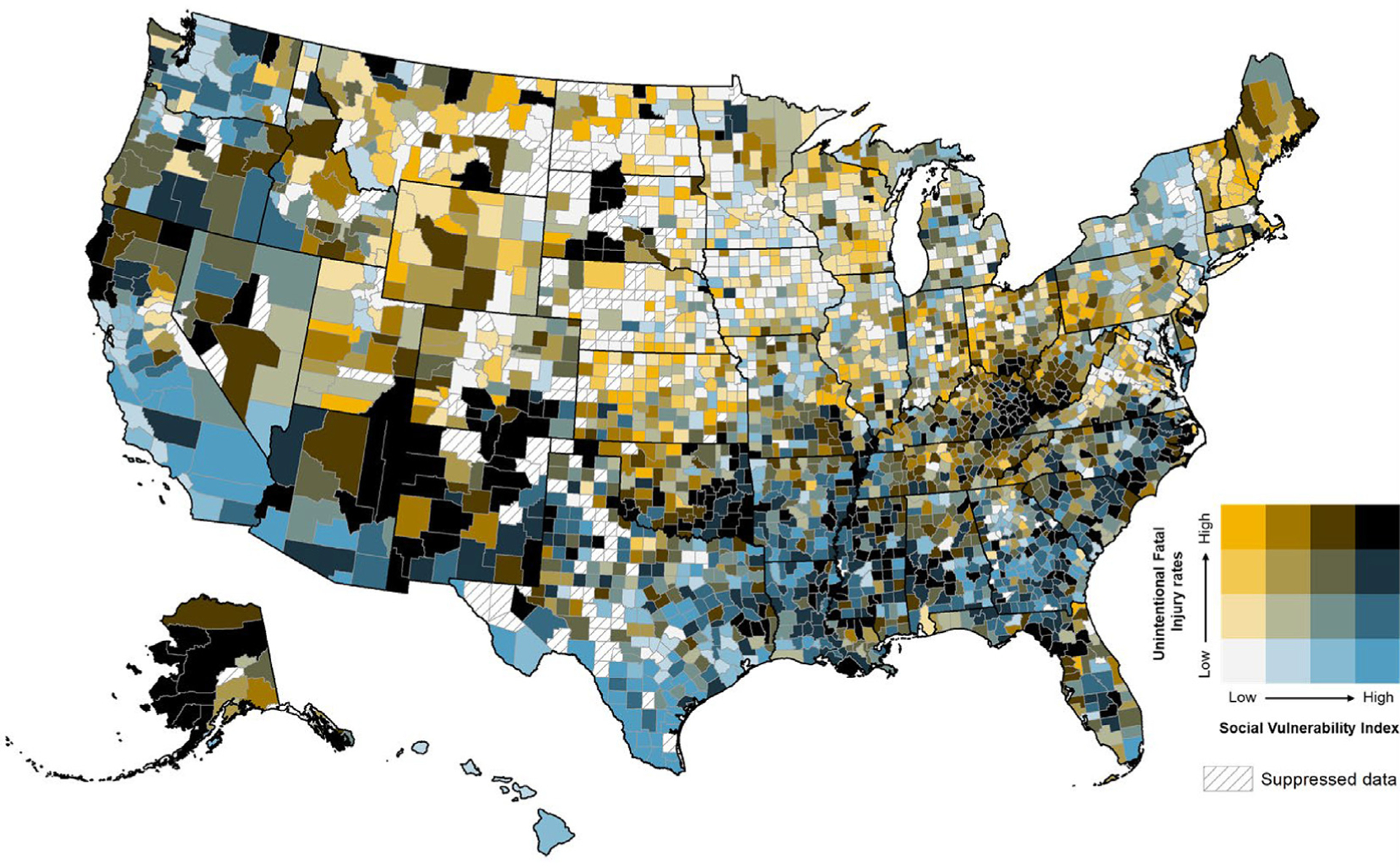
Bivariate geographic distribution of unintentional fatal injury ratesa (per 100,000 population) and the 2018 CDC/ATSDR Social Vulnerability Index (SVI)bc– United States. aUnintentional injury rates (per 100,000 population) were categorized into quartiles: quartile 1 (0–45.3); quartile 2 (45.3–56.2); quartile 3 (56.2–68.3); quartile 4 (68.3–200.7). bSVI scores were categorized into quartiles: Low (0–0.2500); Mid-low (0.2501–0.5000); Mid-high (0.5001–0.7500); High (0.7501–1.0).cData for SVI from 2018; Data for fatal injury from 2015–2019.
4. Discussion
Our findings demonstrate that SVI is associated with unintentional fatal injury rates. Our ecological study shows a significant positive association between county-level social vulnerability and unintentional fatal injury rates illustrating the critical role social and environmental factors may play in impacting the public health burden of injuries. This study provides the first step in combining the SVI and injury mortality data to provide researchers with a promising index to investigate social and environmental factors related to injury. By utilizing indexes, such as the SVI, researchers and injury prevention professionals are provided with information to help identify communities that may need to target specific social and environmental factors to prevent fatal injuries.
Overall SVI, the Socioeconomic Status domain, and the Household Composition and Disability domain had significant positive associations with unintentional fatal injury. Our findings are aligned with previous literature that identified poverty as a risk factor for unintentional fatal injury (Karb et al., 2016) and disability as a risk factor for unintentional injury in children (Shi et al., 2015), illustrating the important influence these factors can have on unintentional injury outcomes. Reducing poverty (Karb et al., 2016) and implementing multidisciplinary injury prevention strategies for people with disabilities (Xiang et al., 2014) may help reduce disparities in unintentional injury for these groups.
The Minority Status and Language domain and Housing Type and Transportation domain had negative associations with unintentional fatal injury rates. A study on firearm injuries and SVI found similar results, though not significant, for the Limited English variable (Van Dyke et al., 2022). Additionally, previous literature suggests injury risk is lower among children of immigrant parents than children of U.S.-born parents which, may be explained by assistance with parenting and differences in cultural factors (Schwebel et al., 2005). Our findings may also be driven by the way racial/ethnic minority is defined in the SVI for this domain. The racial/ethnic minority indicator is defined as the percentage of all racial and ethnic minority individuals in a county, or all persons who are not non-Hispanic White in a county. Grouping all persons who are not non-Hispanic White together in a single indicator may mask any variation by racial/ethnic minority group. The inability to compare between different racial/ethnic minority groups using the racial/ethnic minority SVI indicator may be contributing to the unexpected negative association given the literature demonstrates that there are differences in unintentional fatal injury by race/ethnicity (Clemens, 2021; Daugherty et al., 2019). Because the SVI combines all racial/ethnic minority groups together, relationships between injuries and specific minority groups may not be identified. Further, the use of the large categories of unintentional fatal injuries reduces the opportunity to identify indicators that function differently by specific injury intent and mechanism, such as the racial/ethnic differences for falls and drowning. Additionally, multi-unit housing is more likely to be located in urban areas (Fletcher et al., 2021), while unintentional injury is higher in non-urban areas (Olaisen et al., 2019), which could explain the inverse relationship found in this study. Due to the variation in associations across themes, future research should further investigate these relationships by SVI themes and individual variables.
We found substantial spatial variation in the geographic distribution of overall social vulnerability and unintentional injury rates for U.S. counties. Notably, counties in the South and West regions of the United States had the greatest levels of social vulnerability and greatest rates of unintentional fatal injury, which aligns with previous research that found the Southeast had the highest rates of unintentional fatal injury (Ballesteros et al., 2018; Kegler et al., 2021). However, the reasons for higher unintentional injury death rates in these areas are not fully understood but could be related to complex social factors, such as the concentration of rural communities in the South and limited access to preventive services in certain geographic areas (Baker et al., 1992). Such counties may consider tailored injury prevention interventions to address social and structural conditions that disproportionately disadvantage communities in these counties.
Future studies could examine the social conditions contributing to counties with the highest levels of social vulnerability and rates of unintentional fatal injury to better tailor injury prevention strategies for these communities. More research could focus on identifying risk and protective factors by specific fatal injury mechanisms since the unintentional fatal injury types examined in our study included numerous injury types with different risk factors, such as falls, poisoning, motor vehicle crashes, and drowning. In addition, these data only represent those who died by injuries; it is possible that the injury incidence may be higher in lower SVI counties, but due to differences in injury-related characteristics (e.g., the ability to receive timely trauma/emergency care or differences in injury mechanism) based on SVI level, the effects of SVI on injury mortality may differ from its effect on injury incidence. Future studies may investigate the association between social vulnerability and intentional injury. The field of injury prevention may benefit from the development of a vulnerability index specific to injury since the SVI was developed for use in emergency management and public health preparedness (Burse et al., 2020; Flanagan et al., 2011). This study may inform future work for unintentional fatal injury prevention that could modify the SVI to include additional social determinants of unintentional injuries and exclude variables that are not applicable to unintentional injuries.
5. Limitations
Our findings are subject to several limitations. First, given the ecological nature of this study, counties were represented by one SVI score and one unintentional fatal injury rate. Nevertheless, counties are diverse, containing different communities with varying sociodemographic characteristics living within one county. The results cannot identify the differences at the community level and within counties; conclusions are limited to county level. Since each county was treated the same regardless of population size, with each quartile having an equal number of counties, the results may not accurately represent the population being studied. The counties were not weighted in the statistical modeling; therefore, each county regardless of population size were treated equally. Second, this analysis uses the broad category of unintentional fatal injury. Based on previous literature, sociodemographic factors have varying associations with different types of unintentional injury within this broad category, and these associations may be masked due to analyzing different types of unintentional injury collectively. Additionally, while all data were used for model estimates and quartile derivations, suppressed data were not shown in the figure. Approximately 5.1% (159/3,142) of counties with data on unintentional fatal injury were suppressed according to NCHS suppression rules, limiting the interpretation of our map. In addition, we included the most recent SVI data available from 2018. These data may not account for current trends in social vulnerability, thus we only included unintentional fatal injury data up until 2019 to align with the SVI data. Finally, fatal injury rates were determined based on county of residence and may not reflect the county or SVI score of where the injury occurred.
6. Conclusion
These findings demonstrate that the social vulnerability of counties is associated with unintentional fatal injury rates illustrating the critical role social and environmental factors may play in impacting the public health burden of injuries. Modification of the SVI for unintentional injury research could include additional social determinants of injuries and exclude variables that are not applicable to unintentional injuries. A modified SVI could inform unintentional injury prevention strategies by prioritizing efforts in areas with high levels of social vulnerability.
7. Practical Applications
This study is the first step in combining the SVI and injury mortality data to provide researchers with a promising index to investigate upstream factors related to injury.
Biographies
Avital Wulz, MPH, LMSW, MSPP, is a health scientist within the Office of the Director in National Center for Injury Prevention and Control (NCIPC) in the Division of Injury Prevention (DIP) at the Centers for Disease Control and Prevention. Avital leads and advances health equity related research and initiatives within DIP. Avital received her Master of Public Health, Master of Social Work, and Bachelors of Science in psychology from the University of Georgia and her Masters of Science in Positive Psychology from Life University.
J. Danielle Sharpe, PhD, MS is a Geospatial Epidemiologist at the Centers for Disease Control and Prevention where she has led the Social Vulnerability Index (SVI) project, an effort to measure and map the social vulnerability of communities to public health crises. In this role, Dr. Sharpe has overseen the development of new SVI databases and managed a diverse portfolio of research examining the relationships between social vulnerability and health outcomes related to environmental health, infectious diseases, chronic diseases, injury epidemiology, and emergency response. Her research focuses on spatial epidemiology, social vulnerability, health equity, and social determinants of health.
Gabrielle Ferro Miller, PhD, is a Health Economist in the National Center for Injury Prevention and Control (NCIPC) in the Division of Injury Prevention. Dr. Miller’s research focuses on traumatic brain injury, suicide, and drug overdose. Her research has been published in journals such as American Journal of Public Health, Injury Prevention, and Journal of Public Health Management and Practice. She graduated from the University of Florida in 2008 with her Bachelors of Science in Economics. In 2010 and 2014, respectively, she received her Masters of Science and Doctorate in Food and Resource Economics, also from the University of Florida.
Dr. Amy Wolkin is the Chief of the Data Analytics Branch, Division of Injury Prevention at the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Dr. Wolkin received her Doctorate of Public Health from the University of North Carolina and her Masters of Science in Public Health from Emory University. Dr. Wolkin joined the CDC in 2002. Her research experience includes data analytics, surveillance, injury research and prevention, environmental epidemiology, and emergency preparedness and response.
Appendix A.
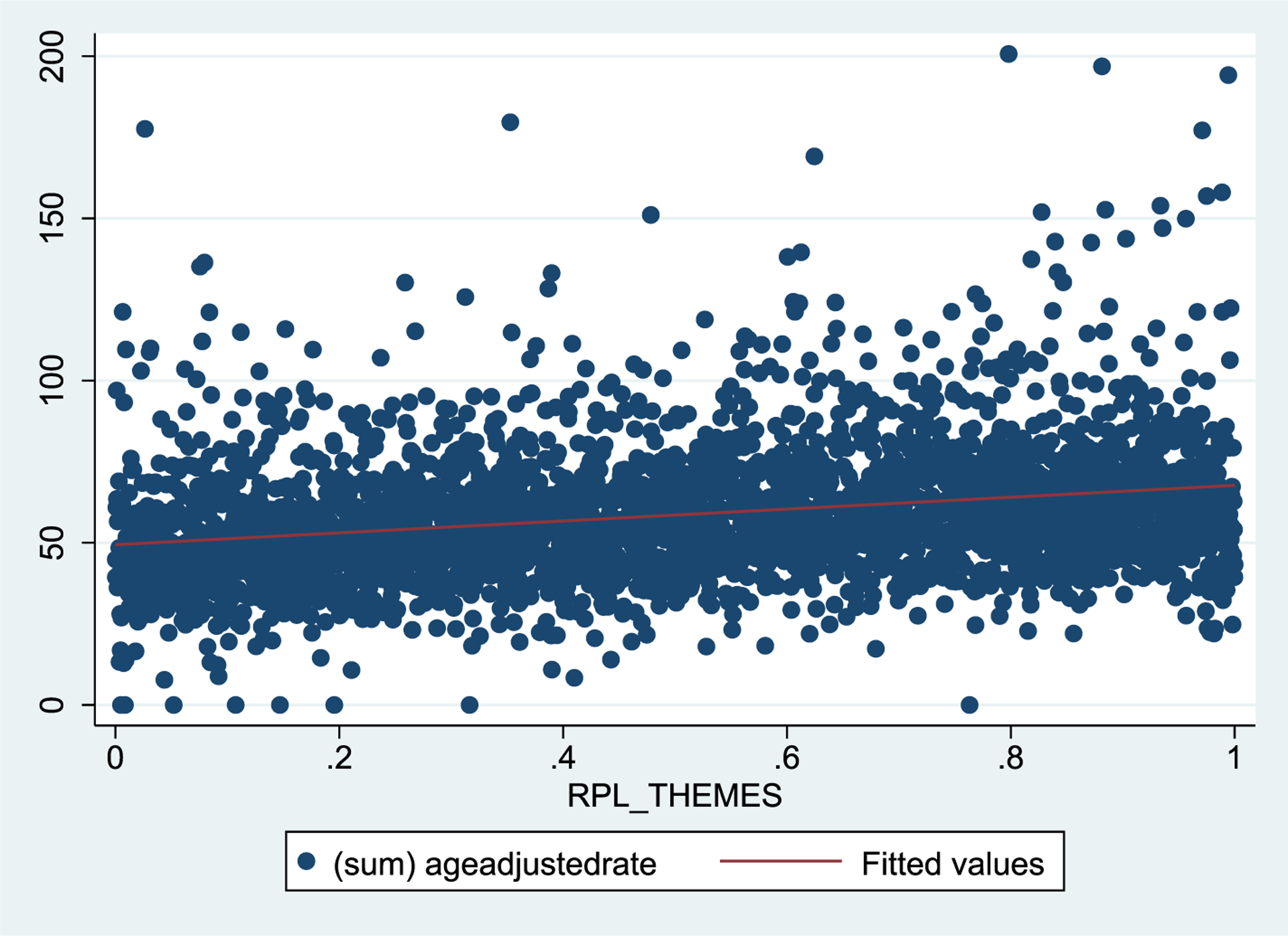
Scatterplot of linearity for fatal unintentional injury rates by overall social vulnerability index
Appendix B.
Negative binomial regression Models: Association between social vulnerability index (SVI) metricsa and age-adjusted unintentional fatal injury ratesb (per 100,000 population)c– United States
| SVI metric | IRR | SE | 95% CI |
|---|---|---|---|
| Overall SVI | 1.37* | 0.28 | (1.32, 1.43) |
| Domain 1 Socioeconomic Status | 1.52* | 0.04 | (1.43, 1.60) |
| Domain 2 Household Composition and Disability | 1.16* | 0.03 | (1.11, 1.22) |
| Domain 3 Minority Status and Language | 0.80* | 0.02 | (0.77, 0.84) |
| Domain 4 Housing Type and Transportation | 0.93 | 0.02 | (0.89, 0.98) |
p < 0.001.
Notes: IRR: incidence rate ratio; CI: confidence intervals; SE: standard error.
Overall SVI and the four SVI domains were defined and calculated by Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
Age-adjusted rates per 100,000 population were calculated using the direct method and the 2000 U.S. standard population.
Data for SVI from 2018; Data for fatal injury from 2015–2019.
Appendix C.
Negative binomial regression Models: Association between social vulnerability index (SVI)a and age-adjusted unintentional fatal injury ratesb (per 100,000 population) by Census regionc and divisionde– United States
| Counties | Unintentional fatal injury | |||
|---|---|---|---|---|
| Census region and division | n (%) | IRR | SE | 95% CI |
| Northeast | 217 (6.9) | −0.08 | 0.10 | (−0.27, 0.11) |
| Division 1: New England | 67 (2.1) | 0.23 | 0.12 | (−0.00, 0.46) |
| Division 2: Middle Atlantic | 150 (4.8) | −0.08 | 0.13 | (−0.35, 0.18) |
| Midwest | 1055 (33.6) | 0.48 * | 0.04 | (0.40, 0.56) |
| Division 3: East North Central | 437 (13.9) | 0.38* | 0.06 | (0.27, 0.49) |
| Division 4: West North Central | 618 (19.7) | 0.53* | 0.06 | (0.41, 0.65) |
| South | 1422 (45.3) | 0.18 * | 0.03 | (0.11, 0.24) |
| Division 5: South Atlantic | 588 (18.7) | 0.26* | 0.04 | (0.17, 0.34) |
| Division 6: East South Central | 364 (11.6) | 0.11 | 0.06 | (−0.01, 0.23) |
| Division 7: West South Central | 470 (14.9) | 0.08 | 0.07 | (−0.06, 0.22) |
| West | 447 (14.2) | 0.39 * | 0.06 | (0.27, 0.51) |
| Division 8: Mountain | 280 (8.9) | 0.41* | 0.06 | (0.28, 0.54) |
| Division 9: Pacific | 167 (5.3) | 0.59* | 0.13 | (0.33, 0.84) |
p < 0.001.
Notes: IRR: incidence rate ratio; CI: confidence intervals; SE: standard error.
Overall SVI was defined and calculated by Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
Age-adjusted rates per 100,000 population were calculated using the direct method and the 2000 U.S. standard population.
U.S. Census Bureau defines geographic Census regions as follows: Northeast—CT, ME, MA, NH, NJ, NY, PA, RI, VT; Midwest—IL, IN, IA, KS, MI, MN, MO, NE, ND, OH, SD, WI; South—AL, AR, DE, DC, FL, GA, KY, LA, MD, MS, NC, OK, SC, TN, TX, VA, WV; West— AK, AZ, CA, CO, HI, ID, MT, NV, NM, OR, UT, WA, WY.
U.S. Census Bureau defines geographic Census divisions as follows: New England—ME, NH, VT, MA, RI; Middle Atlantic—NY, PA, CT, NJ; East North Central—WI, IL, MI, IN, OH; West North Central—ND, SD, NE, KS, MN, IA, MO; South Atlantic—DE, MD, DC, WV, VA, NC, SC, GA, FL; East South Central—KY, TN, MS, AL; West South Central—TX, OK, AR, LA; Mountain—MT, ID, WY, NV, UT, AZ, CO, NM; Pacific—WA, OR, CA, AK, HI.
Data for SVI from 2018; Data for fatal injury from 2015–2019.
Footnotes
CDC Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Ethics statement
This study was exempt from institutional review board approval due to the nature of the study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Domain 1: Socioeconomic Status (indicators: percentage of persons living below the poverty line, percentage of civilians aged 16 years and older who are unemployed, per capita income, percentage of persons aged 25 years and older with no high school diploma)Domain 2: Household Composition and Disability (indicators: percentage of persons aged 65 years and older, percentage of persons aged 17 years and younger, percentage of the civilian noninstitutionalized population with a disability, percentage of single-parent households with children under 18 years)Domain 3: Minority Status and Language (indicators: percentage of racial/ethnic minority persons (all persons except non-Hispanic White persons), percentage of persons aged five years and older who speak English “less than well”)Domain 4: Housing Type and Transportation (indicators: percentage of multi-unit housing or housing in structures with 10 or more units, percentage of mobile homes, percentage of crowded housing or households with more people than rooms, percentage of households with no vehicle available, percentage of persons living in group quarters).
Unintentional injury rates (per 100,000 population) were categorized into quartiles: quartile 1 (0–45.3); quartile 2 (45.3–56.2); quartile 3 (56.2–68.3); quartile 4 (68.3–200.7). SVI scores were categorized into quartiles: Low (0–0.2500); Mid-low (0.2501–0.5000); Mid-high (0.5001–0.7500); High (0.7501–1.0).
Fatal injury counts <10 were suppressed.
References
- Amram O, Amiri S, Lutz RB, et al. (2020). Development of a vulnerability index for diagnosis with the novel coronavirus, COVID-19, in Washington State, USA. Health & Place. 10.1016/j.healthplace.2020.102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An R, & Xiang X (2015a). Social vulnerability and leisure-time physical inactivity among US adults. American Journal of Health Behavior, 39(6), 751–760. 10.5993/AJHB.39.6.2. [DOI] [PubMed] [Google Scholar]
- An R, & Xiang X (2015b). Social vulnerability and obesity among US adults. International Journal of Health Sciences, 3(3), 7–21. 10.15640/ijhs.v3n3a2. [DOI] [Google Scholar]
- Baker SP, O’Neill B, Li GG, & Ginsburg MJ (1992). The injury fact book (pp. 54–57). USA: Oxford University Press. [Google Scholar]
- Ballesteros MF, Williams DD, Mack KA, et al. (2018). The epidemiology of unintentional and violence-related injury morbidity and mortality among children and adolescents in the United States. International Journal of Environmental Research and Public Health, 15(4), 616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns E, & Kakara R (2018). Deaths from falls among persons aged 65 years—United States, 2007–2016. MMWR. Morbidity and Mortality Weekly Report, 67 (18), 509. 10.15585/mmwr.mm6718a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burse N, Thompson E, & Monger M (2020). The role of public health in COVID-19 emergency response efforts from a rural health perspective. Preventing Chronic Disease, 17, E70. 10.5888/pcd17.200256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Web-based Injury Statistics Query and Reporting System (WISQARS) US Department of Health and Human Services, CDC; 2021. [Available from: https://www.cdc.gov/injury/wisqars/index.htm accessed April 5 2021. [Google Scholar]
- Clayton D, & Hills M (1993). Statistical models in epidemiology (pp. 136–138). New York: Oxford University Press. [Google Scholar]
- Clemens T (2021). Persistent racial/ethnic disparities in fatal unintentional drowning rates among persons aged 29 years—United States, 1999–2019. MMWR. Morbidity and Mortality Weekly Report, 70(24), 869–874. 10.15585/mmwr.mm7024a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta S, Bowen VB, Leidner A, et al. (2020). Association between social vulnerability and a county’s risk for becoming a COVID-19 hotspot—United States, June 1–July 25, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(42), 1535. 10.15585/mmwr.mm6942a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daugherty J, Waltzman D, Sarmiento K, et al. (2019). Traumatic brain injury– related deaths by race/ethnicity, sex, intent, and mechanism of injury—United States, 2000–2017. MMWR. Morbidity and Mortality Weekly Report, 68(46), 1050. 10.15585/mmwr.mm6846a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan BE, Gregory EW, Hallisey EJ, et al. (2011). A social vulnerability index for disaster management. Journal of Homeland Security and Emergency Management, 8(1). 10.2202/1547-7355.1792. [DOI] [Google Scholar]
- Flanagan BE, Hallisey EJ, Adams E, et al. (2018). Measuring community vulnerability to natural and anthropogenic hazards: The Centers for Disease Control and Prevention’s Social Vulnerability Index. Journal of Environmental Health, 80(10), 34–36. [PMC free article] [PubMed] [Google Scholar]
- Fletcher KM, Espey J, Grossman MK, et al. (2021). Social vulnerability and county stay-at-home behavior during COVID-19 stay-at-home orders, United States, April 7–April 20, 2020. Annals of Epidemiology, 64, 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay JL, Robb SW, Benson KM, et al. (2016). Can the social vulnerability index be used for more than emergency preparedness? An examination using youth physical fitness data. Journal of Physical Activity & Health, 13(2), 121–130. 10.1123/jpah.2015-0042. [DOI] [PubMed] [Google Scholar]
- Henning-Smith C, & Kozhimannil KB (2018). Rural–urban differences in risk factors for motor vehicle fatalities. Health Equity, 2(1), 260–323. 10.1089/heq.2018.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes MM, Wang A, Grossman MK, et al. (2021). County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. MMWR. Morbidity and Mortality Weekly Report, 70(12), 431. 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaye IM, & Horney JA (2020). The impact of social vulnerability on COVID-19 in the US: An analysis of spatially varying relationships. American Journal of Preventive Medicine, 59(3), 317–325. 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karb RA, Subramanian S, & Fleegler EW (2016). County poverty concentration and disparities in unintentional injury deaths: A fourteen-year analysis of 1.6 million US fatalities. PLoS One, 11(5), e0153516. 10.1371/journal.pone.0153516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kegler SR, Dahlberg LL, & Vivolo-Kantor AM (2021). A descriptive exploration of the geographic and sociodemographic concentration of firearm homicide in the United States, 2004–2018. Preventive Medicine, 153 106767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercy JA, Mack KA, & Steenkamp M (2008). Changing the social environment to prevent injuries. Handbook of injury and violence prevention. Springer. [Google Scholar]
- Morgan ME, Horst MA, Vernon TM, et al. (2020). An analysis of pediatric social vulnerability in the Pennsylvania trauma system. Journal of Pediatric Surgery, 55(12), 2746–2751. 10.1016/j.jpedsurg.2020.05.024. [DOI] [PubMed] [Google Scholar]
- Murphy T, Pokhrel P, Worthington A, et al. (2014). Unintentional injury mortality among American Indians and Alaska natives in the United States, 1990–2009. American Journal of Public Health, 104(S3), S470–S480. 10.2105/AJPH.2013.301854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayak A, Islam SJ, Mehta A, et al. (2020). Impact of social vulnerability on COVID-19 incidence and outcomes in the United States. medRxiv. 10.1101/2020.04.10.20060962. [DOI] [Google Scholar]
- Olaisen RH, Rossen LM, Warner M, et al. (2019). Unintentional injury death rates in rural and urban areas: United States, 1999–2017. [PubMed]
- Roberts H, & Meddings D (2010). Violence and unintentional injury: Equity and social determinants. In Blas E, Kurup A, (Eds.) Equity, Social Determinants and Public Health Programmes (pp. 244–254). [Google Scholar]
- Schwebel DC, Brezausek CM, Ramey CT, et al. (2005). Injury risk among children of low-income US-born and immigrant mothers. Health Psychology, 24(5), 501. [DOI] [PubMed] [Google Scholar]
- Shi X, Shi J, Wheeler KK, et al. (2015). Unintentional injuries in children with disabilities: A systematic review and meta-analysis. Inj Epidemiol, 2(1), 1–13. 10.1186/s40621-015-0053-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2018). Census regions and divisions of the United States.
- Van Dyke ME, Chen MS, Sheppard M, et al. (2022). County-level social vulnerability and emergency department visits for firearm injuries—10 US Jurisdictions, January 1, 2018–December 31, 2021. Morbidity and Mortality Weekly Report, 71(27), 873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2004). ICD-10: International statistical classification of diseases and related health problems (2ns ed.). World Health Organization. [Google Scholar]
- Xiang H, Wheeler KK, & Stallones L (2014). Disability status: A risk factor in injury epidemiologic research. Annals of Epidemiology, 24(1), 8–16. 10.1016/j.annepidem.2013.10.014. [DOI] [PubMed] [Google Scholar]
- Yee CW, Cunningham SD, & Ickovics JR (2019). Application of the Social Vulnerability Index for identifying teen pregnancy intervention need in the United States. Maternal and Child Health Journal, 23(11), 1516–1524. 10.1007/s10995-019-02792-7. [DOI] [PubMed] [Google Scholar]


