Abstract
Purpose
Delay in performance of hip fracture surgery can be caused by medical and/or administrative reasons. Although early surgery is recommended, it is unclear what constitutes a delayed surgery and whether the impact of delayed surgery can differ depending on the reason for the delay.
Materials and Methods
A total of 269 consecutive hip fracture patients over 50 years of age who underwent surgery were prospectively enrolled. They were divided into two groups: early and delayed (time from reaching the hospital to surgery less than or more than 48 hours). Patients were also categorized as fit or unfit based on anesthetic fitness. One-year mortality was recorded, and regression analyses were performed to assess the impact of delay on mortality.
Results
A total of 153 patients (56.9%) had delayed surgery with a mean time to surgery of 87±70 hours. A total of 115 patients (42.8%) were considered medically fit to undergo surgery. No difference in one-year mortality was observed between patients with early surgery and those with delayed surgery (P=0.854). However, when assessment of the time to surgery was performed in a continuous manner, mortality increased with prolonged time to surgery, particularly in unfit patients, and higher mortality was observed when the delay exceeded six days (fit: P=0.117; unfit: P=0.035).
Conclusion
The effect of delay on mortality was predominantly observed in patients who were not considered medically fit, suggesting that surgical delays might have a greater impact on patients with medical reasons for delay.
Keywords: Hip fractures, Mortality, Time factors, Preoperative care, Delay
INTRODUCTION
High mortality has been reported for patients with hip fracture, which can be attributed at least in part to the prolonged bed stay following fracture, leading to complications such as pulmonary embolism, pneumonia, infections, and heart failure1,2,3,4,5). Therefore, early surgery is recommended in treatment of hip fractures in order to minimize morbidity and mortality following hip fractures6,7,8). Multiple studies have demonstrated that early surgery results in improved outcomes, and according to consensus among various guidelines, surgery for treatment of hip fractures should be performed on an urgent basis9,10,11,12,13). The guidelines established by the American Academy of Orthopaedic Surgeons (AAOS) recommend surgery within 48 hours while the National Institute of Healthcare and Excellence (NICE) guidelines recommend surgery within 36 hours11,12,14).
Surgical delays may occur as a result of limited hospital resources or inefficient care pathways for patients with hip fracture. Surgical delays may also occur as a result of certain medical conditions requiring preoperative optimization. Because medical reasons for delay of surgery are a major confounder, there is still controversy regarding the association between early surgery and better outcomes9,10). Although many studies reported that the surgical delay resulted in increased mortality, even after adjusting for medical conditions, some studies including a large randomized trial failed to demonstrate that early surgery provided a survival benefit13). This possible discrepancy can mainly be attributed to variations in the definition of delay and difficulty in accurately accounting for comorbidities. Analysis of time as a continuous variable allows for a better delineation of the effect of timing on surgery. In addition, stratifying patients based on the reason for delay facilitates the analysis of independent effects of delay on outcomes. Understanding the association between timing and outcomes is particularly important in resource-limited settings like India where hospitals must prioritize the patients who require emergency surgery15).
Therefore, a prospective study on elderly patients with hip fractures in India was conducted in order to examine the effect of timing of surgery on mortality. The objectives of this study were: (1) to evaluate the effect of delayed surgery on one-year mortality based on the reason for the delay (stratified based on medical fitness) and (2) to examine the effect of time to surgery on mortality on a continuous spectrum.
MATERIALS AND METHODS
This was a prospective observational study of all hip fracture patients (proximal femur fractures: neck, intertrochanteric, or subtrochanteric) over 50 years of age who were admitted to a single tertiary level trauma center (Jai Prakash Narayan Apex Trauma Center [JPNATC], All India Institute of Medical Sciences [AIIMS]) from February to December 2019. This study was approved by the Institutional Review Board at AIIMS (No. IECPG-631/19.12.2018, RT-29/23.01.2019). All patients agreed to participate in the study and provided written informed consent. An in-person interview of the patient and/or relatives was conducted during admission along with a review of medical records for collection of data.
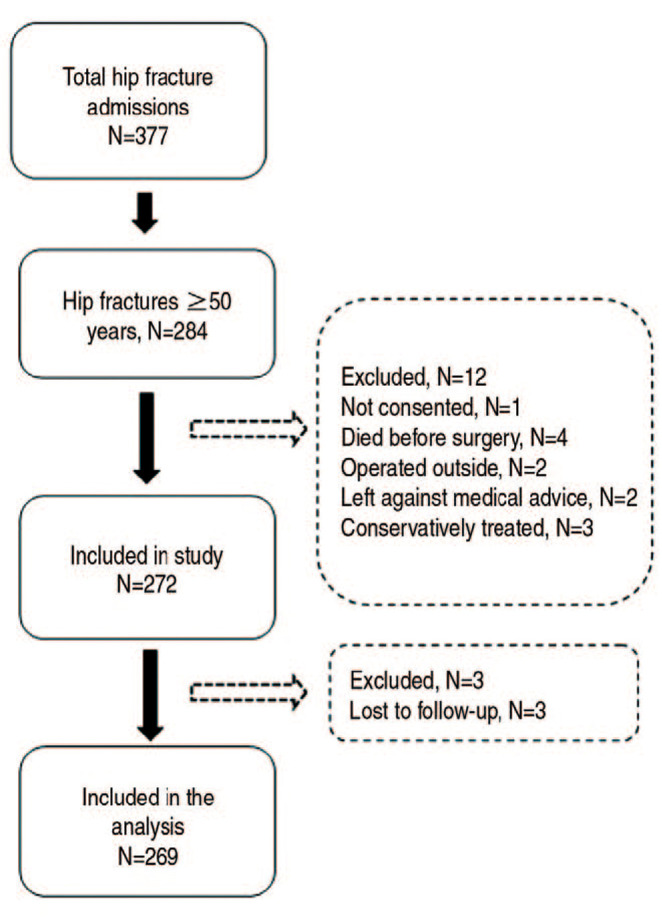
During the study period, there were 377 admissions for hip fracture, and 93 of these patients were under the age of 50. One patient did not provide consent. Among the 283 patients who provided consent, four patients died before surgery, three patients received conservative management due to poor health, two patients decided to undergo surgery outside our institution, and two patients refused surgery. Among the remaining 272 patients, one-year follow-up data was available for 269 patients (98.9%) who were included in this study (Fig. 1). All patients were of Indian origin.
Fig. 1. Flowchart showing the inclusion of patients in the study.
All patients initially presented to the emergency department and were admitted to the orthopedic ward after routine assessments and preliminary medical examination by the orthopedic resident. All patients were reviewed for fitness by the emergency anesthetic team. The preoperative evaluation included the following assessments: chest X-ray, electrocardiogram, complete blood count, serum electrolytes, renal function test, prothrombin time/international normalized ratio, and serum bilirubin. Additional assessments were performed if necessary. Based on the evaluation by the anesthetic team patients were included in either the fit or unfit group16). Any patient who required an additional assessment or intervention other than the previously mentioned assessments was considered unfit (Table 1). These patients underwent surgery after pre-operative optimization and/or further evaluations as advised by the anesthetic team or other concerned specialty. In cases where unfit patients had a delay, it was assumed to be due to medical reasons that prevented performance of an otherwise early surgery. Patients who did not require an additional examination or intervention before surgery were regarded as fit, and surgery was performed at the earliest available time slot. Any delay in performance of surgery on these patients was assumed to be due to administrative reasons such as lack of theatre time, inability to arrange implants, etc.17). The type of surgery was decided by the attending orthopedic physician on call.
Table 1. Reasons for Considering Patients Unfit for Surgery (n=154).
| Reason | Value |
|---|---|
| Poor chest condition | 24 (15.6) |
| Cardiac evaluation | 31 (20.1) |
| Correction of anemia or electrolyte imbalance | 24 (15.6) |
| Uncontrolled sugars | 24 (15.6) |
| Uncontrolled hypertension | 12 (7.8) |
| Antiplatelet therapy | 9 (5.8) |
| Renal disease | 6 (3.9) |
| Multiple issues/others | 24 (15.6) |
Values are presented as number (%).
According to the AAOS guidelines, delayed surgery was defined as the time from reaching the hospital to surgery more than 48 hours14). In addition, the total time to surgery, defined as the duration from the time of injury (as reported by the patient/relative) to surgery, was also recorded. The total time to surgery was the sum of time to reach the hospital and time from hospital to surgery. Assessment of one-year mortality was based on chart review and/or telephonic interview. In addition to mortality, the following in-hospital complications were recorded: cardiac, renal, pulmonary, venous thromboembolism, re-operation.
Comparison of categorical variables was performed using a chi-squared or Fisher exact test. Student’s t-test was used for comparison of continuous variables. Kaplan–Meier failure curves were used to represent the mortality of patients following hip fracture. Comparison of Kaplan–Meier curves between patients with and without a delay was performed using the log-rank test. A Cox proportional hazards model was used to determine whether delayed surgery was associated with increased mortality. Age, sex, and Charlson comorbidity score were included as covariates in multivariable analysis to adjust for possible confounding factors. Time to surgery was included as a spline term with 3° of freedom in the proportional hazards model in order to examine the pattern of relationship between time to surgery and mortality. Predictive plots of the spline regression models were created in order to perform a graphic assessment of the relationship between time to surgery and mortality. Inflection points (or points where the slope of the graph changed) were estimated from the predictive plots. These points represented possible cut-offs for change in the influence of timing on mortality. The results of the tests for non-linearity were analysed from the spline regression model to determine whether the changes in the slope (or the estimated cut-offs) were statistically significant. The predictive plots demonstrate the hazard ratio (HR) for each time point compared with 48 hours as the reference. Spline regression analysis was performed using the ‘smoothHR’ package provided with R software18). The level of significance for the analysis was also set at P<0.05. Kaplan–Meier curves were plotted using Stata statistical software (ver. 12; Stata Corp.).
RESULTS
Overall, of 153 patients (56.9%) who had delayed surgery, the number of patients who had delayed surgery was greater in the unfit group (P<0.001). The mean time to surgery was 87±70 hours. Out of the 269 patients with hip fractures, 115 patients (42.8%) were considered medically fit for surgery. The reasons for determining that a patient was unfit are shown in Table 1, and the characteristics of patients according to surgical fitness are shown in Table 2. Unfit patients were older (P<0.001) and had a higher Charlson comorbidity score (P<0.001). The mean time to surgery was higher for unfit patients (P<0.001); however, the time from injury to the hospital was similar (P=0.877). Overall, 44 patients (16.4%) died within one year. The mean time to surgery was higher for patients who died (110±93 hours vs. 82±64 hours, P=0.014). The Kaplan–Meier survival curve for patients with and without delay (defined as surgery within 48 hours of admission) is plotted in Fig. 2. No difference in one year mortality was observed between the two groups (18.3% vs. 13.8%, unadjusted HR=1.36 [0.74-2.52], P=0.322; adjusted HR=1.06 [0.57-1.99], P=0.854). No difference in mortality was observed between patients with and without delay based on fitness (fit: unadjusted HR=0.61 [0.17-2.18], P=0.444; unfit: unadjusted HR=2.32 [0.69-7.81], P=0.172) (Fig. 3). In addition, no difference in mortality was observed between the fit and unfit groups (unadjusted HR=1.23 [0.64-2.34], P=0.538). Five patients (8.2%) died during the hospital stay, and 11 patients (4.1%) had one or more in-hospital complications (cardaic, 3; deep vein thrombosis, 1; pulmonary, 2; renal, 2; reoperation, 1; multiple, 2).
Table 2. Characteristics of Patients Based on Medical Fitness for Surgery.
| Variable | Medically fit (n=115) | Medically unfit (n=154) | P-value | |
|---|---|---|---|---|
| Age (yr) | 66.9±12.4 | 71.9±11.2 | <0.001 | |
| Sex | 0.379 | |||
| Male | 57 (49.6) | 68 (44.2) | ||
| Female | 58 (50.4) | 86 (55.8) | ||
| Mean Charlson comorbidity score | 0.25±0.75 | 0.99±1.03 | <0.001 | |
| Mode of injury | 0.133 | |||
| Fall | 82 (71.3) | 122 (79.2) | ||
| Others | 33 (28.7) | 32 (20.8) | ||
| Ambulatory status | 0.085 | |||
| Community | 104 (90.4) | 128 (83.1) | ||
| Home | 11 (9.6) | 26 (16.9) | ||
| Type of fracture | 0.589 | |||
| Neck | 28 (24.3) | 42 (27.3) | ||
| Pertrochanteric | 87 (75.7) | 112 (72.7) | ||
| Type of surgery | 0.061 | |||
| Arthroplasty | 17 (14.8) | 37 (24.0) | ||
| Fixation | 98 (85.2) | 117 (76.0) | ||
| Delay in surgery | 31 (27.0) | 122 (79.2) | <0.001 | |
| No. of days of delay | <0.001 | |||
| Within 2 days | 84 (73.0) | 32 (20.8) | ||
| 3-4 days | 27 (23.5) | 52 (33.8) | ||
| 5-6 days | 2 (1.7) | 43 (27.9) | ||
| >6 days | 2 (1.7) | 27 (17.5) | ||
| Time to surgery (hr) | 34.6±33.0 | 104.6±73.5 | <0.001 | |
| Time to hospital (hr) | 26.6±64.5 | 23.4±53.7 | 0.877 | |
| Total time to surgery (hr) | 72.1±78.4 | 141.0±88.4 | <0.001 | |
Values are presented as mean±standard deviation or number (%).
Fig. 2. Kaplan–Meier analysis showing the cumulative mortality of patients with and without delay.

Fig. 3. Kaplan–Meier analysis showing the cumulative mortality of patients with and without delay stratified by fitness (A: fit patients, B: unfit patients).

Assessment of the association between mortality and time to surgery was performed using time as a continuous variable. According to our results, time to surgery (P=0.117), time to hospital (P=0.536), and total time to surgery (P=0.098) showed no association with mortality (Table 3). The detailed regression model is shown in the Appendix Tables 1-3. Among fit patients, time to surgery (P=0.644), time to hospital (P=0.904), and total time to surgery (P=0.937) showed no association with mortality. However, in unfit patients, time to surgery (P=0.035) and total time to surgery (P=0.016) showed an association with mortality, but not time to hospital (P=0.342). A spline regression was used to determine whether the association between time to surgery and mortality was non-linear. Assessment of inflection points in the predictive plots suggested that a change in trend occurred when the time to surgery was approximately 150 hours, which may indicate a steady rise in mortality after the delay had exceeded six days, although the test for non-linearity did not show significance (P=0.242) (Fig. 4). In the group of medically fit patients, a minor decrease in mortality was observed over the first two days followed by an increase in mortality with delay longer than four days, and a sharp rise was observed when the delay was longer than six days, even though the wide confidence intervals with the test for non-linearity were not significant (P=0.264). In the group of unfit patients, a minor increase in mortality was observed over the first two days followed by similar mortality until approximately six days, followed by a steady rise in mortality, though not signifcant (P=0.397) (Fig. 5).
Table 3. The Effect of Different Components of Total Time to Surgery on Mortality.
| Variable | All patients | Fit patients | Unfit patients | |||
|---|---|---|---|---|---|---|
| Adjusted HR (95% CI) | P-value | Adjusted HR (95% CI) | P-value | Adjusted HR (95% CI) | P-value | |
| Time to surgery | 1.00 (1.00-1.01) | 0.117 | 1.00 (0.99-1.02) | 0.644 | 1.01 (1.00-1.01) | 0.035 |
| Total time to surgery | 1.00 (1.00-1.01) | 0.098 | 1.00 (1.00-1.01) | 0.937 | 1.01 (1.00-1.01) | 0.016 |
| Injury to hospital | 1.00 (1.00-1.01) | 0.536 | 1.01 (1.00-1.01) | 0.904 | 1.01 (1.00-1.01) | 0.342 |
HR: hazard ratio, CI: confidence interval.
Fig. 4. Spline regression analysis showing the changes in mortality (as expressed by adjusted hazard ratio) with time to surgery. Dashed lines indicate 95% confidence intervals.
Fig. 5. Spline regression analysis showing the changes in mortality (as expressed by adjusted hazard ratio) with time to surgery, stratified by fitness (A: fit patients, B: unfit patients). Dashed lines indicate 95% confidence intervals.
DISCUSSION
The principle finding of this study is that a significant association was observed between mortality and time to surgery for patients who had a delay due to medical reasons. However, this association was not observed in patients who were medically fit. Although previous studies have reported on the benefits of early surgery, the current study contributes to the literature by identifying patients who might benefit most from a timely surgery. We also observed that mortality rates showed an apparent increase when the delay was longer than six days; however, conduct of additional studies including larger numbers of patients will be required in order to perform a detailed examination of these relationships.
There are a few limitations to this study. The sample size is moderate; therefore, the study might have been underpowered for detection of minor associations. However, we included a consecutive series of patients, which strengthens the reliability of the data. Surgery was defined as surgery beyond 48 hours from reaching the hospital. However, there are no current guidelines for delayed surgery in India, and many patients tend to experience significant delays even before reaching the hospital. Nevertheless, we assessed the impact of timing of surgery as a continuous variable, as well as the impact of delayed presentation to the hospital. While the Charlson comorbidity score was included in the regression analysis and subgroup analysis based on medical fitness was performed as an attempt to adjust for medical comorbidities, there might have been other medical reasons that influenced the time to surgery. In addition, the current study did not include an evaluation to determine whether the delay due to medical reasons could have been avoided as well as the safety of the surgery performed in non-optimized/partially optimized patients. Furthermore, in the current study patients were included in the fit or unfit group based on the requirement for any examination/test other than the routine tests. Although this criterion was used in previous studies, the decision to order an additional test may be dependent on the respective anesthetist16,19). Finally, the study included patients from a single trauma hospital. Although hip fractures are common in females, the current study included a higher proportion of males, similar to other studies conducted in India and could be related to the incidence or due to fewer elderly females seeking attention at a hospital20,21,22). In addition, the guidelines for hip fracture and care pathways may differ in other hospitals, thus the findings of this study may be less applicable to other hospitals.
No significant association was observed between one-year mortality and delayed surgery defined as surgery beyond 48 hours. No change in the findings was observed when subgroup analysis based on medical fitness was performed. In a registry-based analysis of more than 15,000 hips, Schoeneberg et al.23) reported that early surgery showed no association with a decreased rate of in-hospital mortality even after adjusting for comorbidities. Similar findings were reported by Orosz et al.6), who observed no difference between early and late surgery (≤24 hours vs. >24 hours) in a prospective cohort study of 1,206 hip fractures from the New York metropolitan area, and by Smektala et al.24), who found no association between one-year mortality and time to surgery in a study of 2,916 hip fracture patients treated in 268 hospitals in Germany. By contrast, Novack et al.25) reported that lower one-year mortality (17.4% vs. 26.2%) was observed for patients who underwent surgery within 48 hours, while Siegmeth et al.26) also reported a lower one-year mortality rate for patients who underwent surgery within 48 hours (6.9% vs. 13.8%). These discrepancies among studies suggest that variations in the definition of delay as well as unidentified confounding factors can affect the conclusions of the study.
In the current study, the association between the timing of surgery and mortality was more evident when assessment of the timing was performed continuously. The more pronounced effect of delaying surgery on patients who were unfit suggests that deterioration or decompensation of their acute medical conditions might occur (which was the reason for the delay in the first place) leading to increased mortality. Because elderly patients are often in a physiologically compromised state, the normal physiology can easily be disrupted by an acute event such as a hip fracture27). While strategies for optimization should be implemented as early as possible in these patients, waiting for total correction of various anomalies may be counterproductive as complete correction may not be possible without definitive treatment for fractures28). It is also important to note that optimization may not be possible for many patients who are considered unfit and some of them even die before undergoing surgery. According to the results of our analysis, a substantial increase in mortality was observed when the delay was longer than six days and the association was more significant in medically unfit patients. While most guidelines recommend surgery within 36-48 hours, these guidelines may not apply to countries like India where substantial delays in both reaching the hospital and undergoing surgery are possible17,20,29). The findings of our study may be helpful in establishing guidelines in resource-limited settings where hospital resources can be optimally distributed between hip fracture patients and other patients in need of urgent surgical intervention.
CONCLUSION
In summary, we observed that there was no significant difference between patients who underwent surgery within two days and those who underwent surgery after two days. However, according to our findings, a substantial increase in mortality was observed when the delay was longer than six days, suggesting a possible effect of longer delays on mortality. The effect of timing on mortality was predominantly observed in patients who were not considered medically fit, suggesting that avoiding unnecessary surgical delays may be beneficial to patients with medical conditions who might be more vulnerable to surgical delays. Conduct of additional studies will be required in order to determine whether aggressive optimization is necessary and whether unnecessary pre-operative examinations can be avoided in order to limit delay of surgery in patients who are not considered fit to undergo surgery.
Appendix
Appendix Table 1
A list of participating centers
Appendix Table 2
Cox Proportional Hazards Model Showing the Effect of Total Time to Surgery on Mortality
Appendix Table 3
Cox Proportional Hazards Model Showing the Effect of Time from Injury to Hospital on Mortality
Footnotes
FUNDING: No funding to declare.
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractured neck of femur in an English population, 1968-98: database study. BMJ. 2003;327:771–775. doi: 10.1136/bmj.327.7418.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panula J, Pihlajamäki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord. 2011;12:105. doi: 10.1186/1471-2474-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Groff H, Kheir MM, George J, Azboy I, Higuera CA, Parvizi J. Causes of in-hospital mortality after hip fractures in the elderly. Hip Int. 2020;30:204–209. doi: 10.1177/1120700019835160. [DOI] [PubMed] [Google Scholar]
- 4.Carpintero P, Caeiro JR, Carpintero R, Morales A, Silva S, Mesa M. Complications of hip fractures: a review. World J Orthop. 2014;5:402–411. doi: 10.5312/wjo.v5.i4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Handoll HH, Farrar MJ, McBirnie J, Tytherleigh-Strong G, Milne AA, Gillespie WJ. Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database Syst Rev. 2002;(4):CD000305. doi: 10.1002/14651858.CD000305. [DOI] [PubMed] [Google Scholar]
- 6.Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291:1738–1743. doi: 10.1001/jama.291.14.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nyholm AM, Gromov K, Palm H, Brix M, Kallemose T, Troelsen A. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish Fracture Database collaborators. J Bone Joint Surg Am. 2015;97:1333–1339. doi: 10.2106/JBJS.O.00029. [DOI] [PubMed] [Google Scholar]
- 8.Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40:692–697. doi: 10.1016/j.injury.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Maheshwari K, Planchard J, You J, et al. Early surgery confers 1-year mortality benefit in hip-fracture patients. J Orthop Trauma. 2018;32:105–110. doi: 10.1097/BOT.0000000000001043. [DOI] [PubMed] [Google Scholar]
- 10.Simunovic N, Devereaux PJ, Bhandari M. Surgery for hip fractures: does surgical delay affect outcomes? Indian J Orthop. 2011;45:27–32. doi: 10.4103/0019-5413.73660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Voeten SC, Krijnen P, Voeten DM, Hegeman JH, Wouters MWJM, Schipper IB. Quality indicators for hip fracture care, a systematic review. Osteoporos Int. 2018;29:1963–1985. doi: 10.1007/s00198-018-4558-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhandari M, Sprague S, Schemitsch EH International Hip Fracture Research Collaborative. Resolving controversies in hip fracture care: the need for large collaborative trials in hip fractures. J Orthop Trauma. 2009;23:479–484. doi: 10.1097/BOT.0b013e3181a772e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.HIP ATTACK Investigators. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet. 2020;395:698–708. doi: 10.1016/S0140-6736(20)30058-1. Erratum in: Lancet 2023;401:1078. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Orthopaedic Surgeons (AAOS) Management of hip fractures in the elderly: evidence-based clinical practice guideline [Internet] Rosemont: AAOS; 2014. Sep 05, [cited 2022 Mar 3]. Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/hip-fractures-in-the-elderly/management_of_hip_fractures_in_the_elderly-7-24-19.pdf . [Google Scholar]
- 15.Rath S, Yadav L, Tewari A, et al. Management of older adults with hip fractures in India: a mixed methods study of current practice, barriers and facilitators, with recommendations to improve care pathways. Arch Osteoporos. 2017;12:55. doi: 10.1007/s11657-017-0344-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87:483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 17.George J, Sharma V, Farooque K, Mittal S, Trikha V, Malhotra R. Factors associated with delayed surgery in elderly hip fractures in India. Arch Osteoporos. 2021;16:7. doi: 10.1007/s11657-020-00858-6. [DOI] [PubMed] [Google Scholar]
- 18.Meira-Machado L, Cadarso-Suárez C, Gude F, Araújo A. smoothHR: an R package for pointwise nonparametric estimation of hazard ratio curves of continuous predictors. Comput Math Methods Med. 2013;2013:745742. doi: 10.1155/2013/745742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ftouh S, Morga A, Swift C Guideline Development Group. Management of hip fracture in adults: summary of NICE guidance. BMJ. 2011;342:d3304. doi: 10.1136/bmj.d3304. [DOI] [PubMed] [Google Scholar]
- 20.Dash SK, Panigrahi R, Palo N, Priyadarshi A, Biswal M. Fragility hip fractures in elderly patients in Bhubaneswar, India (2012-2014): a prospective multicenter study of 1031 elderly patients. Geriatr Orthop Surg Rehabil. 2015;6:11–15. doi: 10.1177/2151458514555570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dhanwal DK, Siwach R, Dixit V, Mithal A, Jameson K, Cooper C. Incidence of hip fracture in Rohtak district, North India. Arch Osteoporos. 2013;8:135. doi: 10.1007/s11657-013-0135-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skirbekk V, James KS. Abuse against elderly in India--the role of education. BMC Public Health. 2014;14:336. doi: 10.1186/1471-2458-14-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schoeneberg C, Aigner R, Pass B, et al. Effect of time-to-surgery on in-house mortality during orthogeriatric treatment following hip fracture: a retrospective analysis of prospectively collected data from 16,236 patients of the AltersTraumaRegister DGU®. Injury. 2021;52:554–561. doi: 10.1016/j.injury.2020.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Smektala R, Endres HG, Dasch B, et al. The effect of time-tosurgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet Disord. 2008;9:171. doi: 10.1186/1471-2474-9-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Novack V, Jotkowitz A, Etzion O, Porath A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19:170–176. doi: 10.1093/intqhc/mzm003. [DOI] [PubMed] [Google Scholar]
- 26.Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87:1123–1126. doi: 10.1302/0301-620X.87B8.16357. [DOI] [PubMed] [Google Scholar]
- 27.Beloosesky Y, Hendel D, Weiss A, et al. Cytokines and C-reactive protein production in hip-fracture-operated elderly patients. J Gerontol A Biol Sci Med Sci. 2007;62:420–426. doi: 10.1093/gerona/62.4.420. [DOI] [PubMed] [Google Scholar]
- 28.Brauer C, Morrison RS, Silberzweig SB, Siu AL. The cause of delirium in patients with hip fracture. Arch Intern Med. 2000;160:1856–1860. doi: 10.1001/archinte.160.12.1856. [DOI] [PubMed] [Google Scholar]
- 29.George J, Sharma V, Farooque K, Mittal S, Trikha V, Malhotra R. Injury mechanisms of hip fractures in India. Hip Pelvis. 2021;33:62–70. doi: 10.5371/hp.2021.33.2.62. [DOI] [PMC free article] [PubMed] [Google Scholar]







