Abstract
Aim
Out-of-hospital cardiac arrest (OHCA) with an initial non-shockable rhythm is the predominant form of OHCA in adults. We evaluated its 10-year trends in epidemiology and management in Singapore.
Methods
Using the national OHCA registry we studied the trends of 20,844 Emergency Medical Services-attended adult OHCA from April 2010 to December 2019. Survival to hospital discharge was the primary outcome. Trends and outcomes were analyzed using linear and logistic regression, respectively.
Results
Incidence rates of adult OHCAs increased during the study period, driven by non-shockable OHCA. Compared to shockable OHCA, non-shockable OHCAs were significantly older, had more co-morbidities, unwitnessed and residential arrests, longer no-flow time, and received less bystander cardiopulmonary resuscitation (CPR) and in-hospital interventions (p < 0.001). Amongst non-shockable OHCA, age, co-morbidities, residential arrests, no-flow time, time to patient, bystander CPR and epinephrine administration increased during the study period, while presumed cardiac etiology decreased (p < 0.05). Unlike shockable OHCA, survival for non-shockable OHCA did not improve (p < 0.001 for trend difference). The likelihood of survival for non-shockable OHCA significantly increased with witnessed arrest (adjusted odds ratio (aOR) 2.02) and bystander CPR (aOR 3.25), but decreased with presumed cardiac etiology (aOR 0.65), epinephrine administration (aOR 0.66), time to patient (aOR 0.93) and age (aOR 0.98). Significant two-way interactions were observed for no-flow time and residential arrest with bystander CPR (aOR 0.96 and 0.40 respectively).
Conclusion
The incidence of non-shockable OHCA increased between 2010 and 2019. Despite increased interventions, survival did not improve for non-shockable OHCA, in contrast to the improved survival for shockable OHCA.
Keywords: Out-of-hospital cardiac arrest, Non-shockable rhythms, Trends, Survival
Introduction
Successful resuscitation after out-of-hospital cardiac arrest (OHCA) is highly dependent on the first recorded rhythm, with shockable rhythms (ventricular tachycardia and fibrillation) linked to better clinical outcomes compared to non-shockable rhythms (pulseless electrical activity (PEA) and asystole).1, 2 The past four decades have seen an increasing incidence of OHCA presenting with an initial non-shockable rhythm and it is now the predominant form of OHCA in adults globally.3, 4, 5, 6, 7 Despite accompanying advances in resuscitation science, outcomes of OHCAs with non-shockable rhythms have remained dismal globally with limited improvement over the years.7
The overall survival rates from OHCA have improved over the years in Singapore,1 but little is known about the incidence and outcomes of non-shockable OHCAs in adults, that is, those presenting with an initial non-shockable rhythm. Singapore’s population is rapidly aging,8 increasing in medical co-morbidities,9 and mostly lives in high-rise buildings which are challenging to access during emergencies, all of which are factors associated with non-shockable OHCAs.10, 11, 12 Singapore has systematically introduced a series of public health bystander-focused interventions over the years to improve OHCA outcomes.13 A recent study by Lin et al demonstrated improvements in clinical outcomes of non-traumatic OHCA with initial non-shockable rhythms in Taipei city, through multi-faceted initiatives on the community chain of survival over a 10-year period.14 Knowledge of the epidemiology of adult, non-shockable OHCAs in Singapore, a similarly urbanized city state, may help design policies and interventions to improve their outcomes.
Using the national OHCA database, Singapore Pan-Asian Resuscitation Outcomes Study (PAROS), we aimed to evaluate the temporal trends in incidence, management and outcomes of adult non-shockable OHCA in Singapore. We hypothesized the incidence of non-shockable OHCA would increase with the aging population of Singapore, and survival of non-shockable OHCA would increase given the improvements in pre-hospital (Emergency Medical Service [EMS] response and bystander interventions), and in-hospital care over the past decade.
Methods
Study design and setting
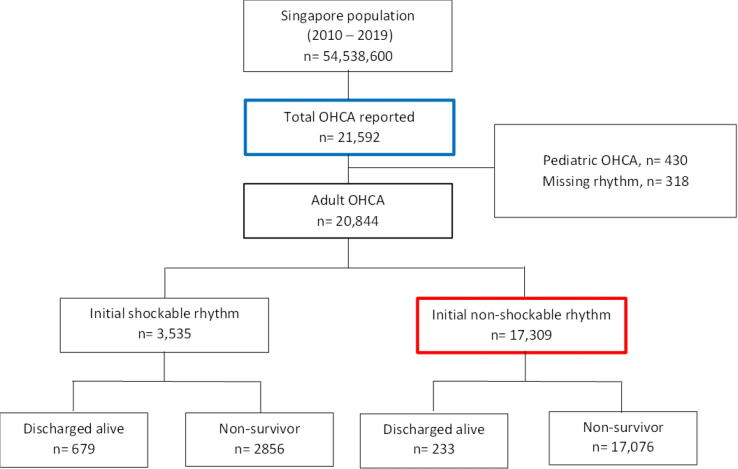
This was a secondary analysis from PAROS performed in Singapore, a densely-populated, multi-ethnic city-state in Southeast Asia. We included adult (defined as ≥20 years of age), EMS-attended OHCA patients presenting between 1 April 2010 to 31 December 2019 (Fig. 1).
Fig. 1.
Patient selection. Selection of adult, EMS-attended OHCA in Singapore from April 2010 to December 2019. Blue box indicates OHCA patients captured by the national OHCA registry. Red box indicates final study population. Abbreviation: OHCA, out-of-hospital cardiac arrest.
EMS
The Singapore Civil Defence Force (SCDF) is the sole EMS provider in Singapore.1 It is activated via a centralized “995” dispatch system.1 Each OHCA case is attended by an SCDF ambulance comprising of three Emergency Medical Technicians (EMT)-one EMT-Intermediate (EMT-I) equivalent and two EMT-Basic (EMT-B) equivalent; the ambulance driver is one of the EMT-Bs. Motorcycle-based EMTs or fire bikers, equipped with automated external defibrillators (AED) are dispatched ahead of ambulances when available. During the study period, dispatcher-assisted cardiopulmonary resuscitation (DA-CPR), community CPR and AED training, and mobile community first-responder scheme were introduced, in 2012, 2014 and 2015 respectively.13 The Registry for AED Integration initiative was developed in 2015 to improve the management and utilization of the 9880 public AEDs across Singapore.15, 16
Data source and definitions
Data for this study were imported from the PAROS database. Only data from Singapore were utilized for the study. PAROS is an ongoing clinical research network for OHCA in the Asia-Pacific providing baseline information on OHCA epidemiology, management and outcomes, with data definitions in accordance with Utstein definitions.17, 18 Data are extracted from emergency dispatch records, ambulance case notes, and emergency department (ED) and in-hospital records. Quality assurance data checks are built into the data entry system and data verification checks are implemented to ensure data integrity.
The Charlson Co-morbidity Index (CCI) was applied to measure and ascertain the patients’ disease burden succinctly.19 Disease conditions not systematically collected by the database were assumed to be absent in all the patients. These included peripheral vascular disease, dementia, connective tissue disease, peptic ulcer disease, liver disease, lymphoma, leukemia and acquired immunodeficiency syndrome. Although the computation might not be complete, it was the relative impact that mattered in comparing the odds of survival and neurological outcomes at hospital discharge.
Study outcomes
The primary outcome was survival to hospital discharge, defined as discharge from acute hospital care. Secondary outcomes included: (1) transport to acute hospital, (2) survival to hospital admission, defined as admission to hospital intensive care unit after successful resuscitation in the ED, and (3) neurological status at time of hospital discharge, based on the Cerebral Performance Category (CPC) scale,20 where CPC 1 or 2 denoted a positive neurological outcome and CPC 3 or 4 denoted a poor neurological outcome. Inpatient mortality was designated CPC 5.
Statistical analysis
The data were presented with median (inter-quartile range, [IQR]) and frequencies (%), and the exploratory analyses were performed with Mann-Whitney test and Chi-square test. Direct age-adjustment of the shockable and non-shockable OHCA incidence rates was carried out with the World Health Organization population.21 The analysis was prepared in two aspects. First, the monthly trends of crude and age-adjusted incidence rates of shockable and non-shockable OHCA, and the proportions of patient characteristics, event characteristics, pre-hospital and in-hospital management, and outcomes were estimated and tested with seemingly unrelated regression.22 Second, using data only from non-shockable adult OHCA, the binary clinical outcomes of survival to and neurological outcomes at discharge were analyzed with logistic regression. The two-way interactions between bystander CPR and arrest location and no flow time were considered. The final models were selected based on backward elimination (p-value threshold of 0.05), with the Akaike Information Criterion (AIC) taken into consideration.23 When an interaction effect was featured both in the model building and in the final model, their independent components were included mandatorily. Should CCI turn out to be non-significant in the model-building process then age would be included for further scrutiny. The analysis was further stratified by age (<65 and ≥65 years) and type of non-shockable rhythm (PEA and asystole). The Hosmer-Lemeshow test was applied for ascertaining model goodness of fit. Analyzed with Stata MP v16 (Stata Corp, Texas, USA), all statistical tests were performed at 5% level of significance.
Ethical consideration
The Centralized Institutional Review Board (2010/270/C, 2013/604/C and 2018/2937) and Domain Specific Review Board (C/10/545 and 2013/00929) granted approval for Singapore PAROS registry. Waiver of patient consent was granted and all data were de-identified.
Results
Overall characteristics
The baseline characteristics of 20,844 EMS-attended adult OHCA patients are summarized in Table 1. The median age was 69 years old (IQR: 57–81), and the majority were males (64.2%). The ethnic distribution (Chinese: 68.3%, Malay: 15.6%, Indian: 11.1%) was reflective of the nation’s racial mix. The majority of OHCAs occurred at residences (73.0%), were presumed cardiac in etiology (68.6%) and witnessed (58.1%). A total of 912 (4.4%) patients survived to hospital discharge.
Table 1.
Baseline characteristics of adult EMS-attended OHCA.
| Non-Shockable n = 17,309 |
Shockable n = 3,535 |
P-value | |
|---|---|---|---|
| Demographics | |||
| Age in years, median (IQR) | 71 (59, 82) | 61 (52,70) | <0.001 |
| Male sex, n (%) | 10,447 (60.4%) | 2936 (83.1%) | <0.001 |
| Race, n (%) | <0.001 | ||
| Chinese | 11,933 (68.9%) | 2,311 (65.4%) | |
| Malay | 2,653 (15.3%) | 593 (16.8%) | |
| Indian | 1,905 (11.0%) | 414 (11.7%) | |
| Other | 818 (4.7%) | 217 (6.1%) | |
| Event information | |||
| Arrest location, n (%) | <0.001 | ||
| Private residence | 13,3461 (77.1%) | 1,870 (52.9%) | |
| Healthcare facility | 1,635 (9.5%) | 369 (10.4%) | |
| Public area | 2,328 (13.5%) | 1,296 (36.7%) | |
| Presumed cardiac aetiology, n (%) | 11,025 (63.7%) | 3,265 (92.4%) | <0.001 |
| Witnessed arrest, n (%) | <0.001 | ||
| Unwitnessed | 7,879 (45.5%) | 861 (24.4%) | |
| Bystander witnessed | 7,864 (45.4%) | 2,372 (67.1%) | |
| EMS witnessed | 1,566 (9.1%) | 302 (8.5%) | |
| Medical history, n (%) | |||
| Heart disease | 5,855 (33.8%) | 1,491 (42.2%) | <0.001 |
| Diabetes | 5,723 (33.1%) | 966 (27.3%) | <0.001 |
| Cancer | 1,969 (11.4%) | 150 (4.2%) | <0.001 |
| Hypertension | 9,379 (54.2%) | 1,719 (48.6%) | <0.001 |
| Renal disease | 2,527 (14.6%) | 423 (12.0%) | <0.001 |
| Respiratory disease | 2,200 (12.7%) | 231 (6.5%) | <0.001 |
| Hyperlipidaemia | 6,702 (38.7%) | 1,353 (38.3%) | 0.620 |
| Stroke | 2,380 (13.8%) | 307 (8.7%) | <0.001 |
| CCI, median (IQR) | 4 (2,5) | 3 (1,4) | <0.001 |
| Pre-hospital management | |||
| Bystander CPR, n (%) | 8,449 (48.8%) | 2,139 (60.5%) | <0.001 |
| DA CPR, n (%) | 5,041 (29.1%) | 827 (23.4%) | <0.001 |
| Bystander AED application, n (%) | 690 (4.0%) | 415 (11.7%) | <0.001 |
| Pre-Hospital defibrillation, n (%) | 1,718 (9.9%) | 3,422 (96.8%) | <0.001 |
| Epinephrine, n (%) | 9,219 (53.3%) | 2,095 (59.4%) | <0.001 |
| Times in minutes, median (IQR) | |||
| No-flow time in min, median (IQR)* | 16 (10,25) | 13 (8.6,18.5) | <0.001 |
| Time to Dispatch | 1.7 (1,2.5) | 1.6 (0.9,2.4) | <0.001 |
| Time to Scene | 8∙3 (6.6,10.5) | 8 (6.3,10.2) | <0.001 |
| Time to Patient | 11∙3 (9.2,14.0) | 10∙5 (8.4,13.1) | <0.001 |
| Time at Scene | 19∙8 (15.8,23.8) | 18∙0 (13.9,22.5) | <0.001 |
| Hospital Management, n (%)** | |||
| TTM | 433 (18.3%) | 507 (39.1%) | <0.001 |
| PCI | 217 (9.2%) | 624 (48.1%) | <0.001 |
| Patient Outcomes, n (%) | |||
| Transported | 17,028 (98.4%) | 3,533 (99.9%) | <0.001 |
| Pre-hospital ROSC | 1,051 (6.1%) | 900 (25.5%) | <0.001 |
| Survived to admission | 2,368 (13.7%) | 1,297 (36.7%) | <0.001 |
| Survived to discharge | 233 (1.4%) | 679 (19.2%) | <0.001 |
| CPC 1 or 2 at discharge | 107 (0.6%) | 529 (15.0%) | <0.001 |
Abbreviations: EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest; IQR, inter-quartile range; CCI, Charlson Co-morbidity Index; CPR, cardiopulmonary resuscitation; AED, automated external defibrillator; TTM, targeted temperature management; PCI, percutaneous coronary intervention; ROSC, return of spontaneous circulation; CPC, Cerebral Performance Category.
Numbers are n (%) for categorical variables and median (Q1–Q3) for continuous variables.
Charlson Co-morbidity Index was calculated based on available medical history. Where details were not available, they were assumed to be absent.
Good neurological outcome was defined as CPC 1 or 2.
Time to scene is the interval, in minutes, between the time the call was received by the dispatch center and the time of arrival at scene of either the ambulance or a rapid responder dispatched via the same dispatch center.
Time to patient refers to the interval, in minutes, between time call received by the dispatch center and the time of patient contact by either the ambulance or rapid responder dispatched via the same dispatch center.
No-flow time was unavailable for 164 patients.
The proportions of patient receiving these interventions were based on those who survived to hospital admission, as only these patients were eligible.
Compared to shockable OHCA, adult non-shockable OHCAs were older and had more co-morbidities. Non-shockable OHCAs were more often residential arrests, unwitnessed, of non-cardiac etiology and experienced longer no-flow time; they received less bystander and in-hospital interventions. Significantly fewer non-shockable OHCAs survived to hospital discharge and were discharged with good neurological outcomes, compared to shockable OHCAs.
Temporal trends in OHCA incidence, management and outcomes
The study period saw a significant increase in the monthly incidence of adult OHCA, regardless of rhythm. The increase in incidence was significantly greater for non-shockable OHCA, when compared with shockable OHCA, with or without age adjustment (Supplemental Table 1, Fig. 2a and b).
Fig. 2.
Temporal trends of adult, EMS-attended OHCA. This figure shows the temporal trends of adult EMS-attended OHCA in Singapore, stratified by rhythm type where (a) and (b) show incidence and outcomes, (c) and (d) show patient and event characteristics, and (e) and (f) show interventions. Incidence was calculated per 100,000 population and adjustment for age was performed using direct method, based on World Health Organisation population data. TTM and PCI are expressed as proportions of OHCA subgroup (adult, EMS-attended OHCA who survived to hospital admission). Abbreviation: EMS, Emergency Medical Services; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation; CCI, Charlson Comorbidity Index; CPR, cardiopulmonary resuscitation; TTM, targeted temperature management; PCI, percutaneous coronary intervention.
Compared to shockable OHCA, non-shockable OHCA reported significantly steeper growing monthly trends in median age, certain co-morbidities (hyperlipidemia and renal disease), and arrests which were unwitnessed and of non-cardiac etiology (Fig. 2c and d).
Both non-shockable and shockable OHCA saw increases in bystander CPR and targeted temperature management (TTM) use, with the increase in TTM use significantly higher in shockable OHCA (Fig. 2e and f). Shockable OHCA saw a growing trend of percutaneous coronary intervention (PCI). Time to patient increased significantly for both shockable and non-shockable OHCA; no-flow time increased significantly only for non-shockable OHCA.
The study period witnessed significant improvements in outcomes for shockable OHCA, with rising trends in the proportions of pre-hospital ROSC, survival to hospital admission, survival to hospital discharge and discharge with good neurological outcomes (Fig. 2a and b). In contrast, non-shockable OHCA reported a downward trend in the proportions of survival to admission and no change in the proportion of survival to discharge. The proportions of non-shockable OHCA discharged with good neurological outcomes were below 1% throughout the study period.
Predictors of survival & neurological outcomes at discharge
The analysis began with a bivariate examination on all relevant predictors. The subsequent logistic regression analysis revealed that younger patients, PEA, non-cardiac etiology, bystander CPR, witnessed arrests, no epinephrine administration and shorter time to patient were jointly significant in raising the odds of survival to discharge (Table 2 and Fig. 3). While no-flow time and residential arrest were not significant as independent predictors, their effects were manifested though their interactions with bystander CPR. More specifically, bystander CPR coupled with a longer no-flow time or residential arrest had the effect of reducing the odds of survival to discharge. Among patients who survived to hospital admission, there was significant evidence suggesting that PCI could almost triple the odds of survival to discharge (Supplemental Table 2).
Table 2.
Significant predictors of non-shockable OHCA outcomes by logistic regression.
| Predictor | Survived to discharge |
CPC 1 or 2 at discharge |
||
|---|---|---|---|---|
| Adjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value | |
| Age (continuous)* | 0.98 (0.97–0.99) | 0.001 | 0.98 (0.96–0.99) | 0.009 |
| Presumed cardiac etiology (yes vs no) | 0.65 (0.45–0.93) | 0.018 | NS | |
| Witnessed arrest (bystander vs unwitnessed) | 2.02 (1.35–3.02) | 0.001 | 1.96 (0.10–3.84) | 0.051 |
| Rhythm type (PEA vs asystole) | 6.04 (3.94–9.26) | <0.001 | 11.47 (4.83–27.26) | <0.001 |
| Bystander CPR (yes vs no) | 3.25 (1.46–7.24) | 0.004 | 8.30 (1.81–38.07) | 0.006 |
| Epinephrine administration (yes vs no) | 0.66 (0.46–0.95) | 0.024 | 0.29 (0.15–0.55) | <0.001 |
| Time to patient (continuous) | 0.93 (0.89–0.98) | 0.006 | NS | |
| Bystander CPR and arrest location (residential vs non-residential)** | 0.40 (0.17–0.91) | 0.028 | 0∙14 (0.03–0.65) | 0.012 |
| Bystander CPR and no-flow time*** | 0.96 (0.93–0.99) | 0.012 | 0.92 (0.86–0.99) | 0.037 |
Abbreviations: OHCA, out-of-hospital cardiac arrest; PEA, pulseless electrical activity; CPR, cardiopulmonary resuscitation; OR, odds ratio; CI, confidence interval; CPC, Cerebral Performance Category; NS, non-significant; CCI, Charlson Comorbidity Index.
EMS-witnessed OHCA and non-shockable OHCA with no subtype (PEA vs asystole) were excluded from the analysis. Final population included 14,888 patients. This model included clinically relevant and statistically significant interaction terms such as bystander CPR and arrest location, bystander CPR and no-flow time. Time to patient refers to the interval, in minutes, between time call received by the dispatch center and the time of patient contact by either the ambulance or rapid responder dispatched via the same dispatch center.
Age was included in the model where CCI was non-significant. Increasing age decreased the likelihood of survival to discharge and discharge with good neurological outcome.
Arrest location was dichotomized into residential and non-residential (public and healthcare facility). On its own, arrest location did not significantly predict survival to discharge or discharge with good neurological outcome.
No-flow time was not a significant predictor of survival to discharge or discharge with good neurological outcome, on its own.
Fig. 3.
Predictors of survival and neurological outcome for non-shockable OHCA. This figure shows the predictors of survival to hospital discharge for non-shockable OHCA. EMS-witnessed OHCA and non-shockable OHCA with no subtype (PEA vs asystole) were excluded from the analysis. This model included clinically relevant and statistically significant interaction terms such as bystander CPR and arrest location, bystander CPR and no-flow time. Time to patient refers to the interval, in minutes, between time call received by the dispatch center and the time of patient contact by either the ambulance or rapid responder dispatched via the same dispatch center. * indicates significant predictors of discharge with good neurological outcomes (CPC 1 or 2) for non-shockable OHCA. Abbreviations: OHCA, out-of-hospital cardiac arrest; BCPR, bystander cardiopulmonary resuscitation; PCI, percutaneous coronary intervention; OR, odds ratio; CI, confidence interval; CPC, Cerebral Performance Category.
Similarly, younger age, PEA, bystander CPR and no epinephrine administration were jointly significant in explaining a good neurological outcome at discharge. The interactions between bystander CPR with no-flow time and arrest location (residential) were significant.
The final models presented in Table 2 could offer a satisfactory fit to the data, according to the Hosmer-Lemershow test (p > 0.05).
Exploratory analyses stratified by age and rhythm type
Amongst non-shockable OHCA patients, the above-mentioned analyses were further stratified by age (<65 and ≥65 years) and rhythm type (PEA vs asystole) for exploratory purposes.
Compared to their younger counterparts, older non-shockable OHCAs (≥65-years old) were more likely females, and had more co-morbidities and residential arrests. Older non-shockable OHCAs received more bystander CPR, less in-hospital interventions (for those who survived to hospital admission) and had worse outcomes (Supplemental Table 3).
Temporal trends in incidence, characteristics, management and outcomes of older and younger non-shockable OHCA are summarized in Supplemental Table 4 and Supplemental Fig. 1. The study period saw significant increases in the monthly incidence of non-shockable OHCA and bystander CPR, which were significantly greater for older non-shockable OHCA. Outcomes improved for younger non-shockable OHCA, but not for older, non-shockable OHCA.
Among younger non-shockable OHCAs, an initial rhythm of PEA, bystander CPR, witnessed arrests and shorter time to patient independently improved the odds of survival to discharge. While an initial rhythm of PEA improved the odds of discharge with good neurological outcomes, diabetes and longer no-flow time reduced the odds of discharge with good neurological outcomes. Bystander CPR interacted significantly with no-flow time and residential arrest to reduce the odds of survival and discharge with good neurological outcomes respectively (Supplemental Table 5).
Unwitnessed arrests, asystole and epinephrine administration were the common independent factors contributing to lower odds of survival to and good neurological outcomes at discharge among the older non-shockable OHCAs. The interaction between bystander CPR and residential arrest was also significantly associated with the lower odds of survival to discharge.
The exploratory analyses stratified by rhythm type (PEA vs asystole) are summarized in Supplemental Tables 6–8 and Supplemental Fig. 2.
Discussion
In this large multi-ethnic nationwide study, we observed increasing incidence of adult EMS-attended OHCA over the past decade, driven mainly by non-shockable OHCA. The same period saw increases in pre-hospital and in-hospital interventions of adult OHCA regardless of rhythm. Amongst non-shockable OHCA, there were significant increases in median age, co-morbidities, residential arrests and that of non-cardiac etiology. In contrast with shockable OHCA, there was limited progress in improving survival of non-shockable OHCA. Witnessed arrests, bystander CPR and having PEA as the initial non-shockable rhythm increased the odds of survival from non-shockable OHCA, while increasing age, presumed cardiac etiology, epinephrine administration and time taken for EMS to arrive at patients’ side decreased the odds of survival. Bystander CPR interacted significantly with location of arrest and duration of no-flow time. Our study extends the findings of prior studies by providing more granular information on the temporal trends and the interplay of factors affecting the outcomes of non-shockable OHCA.
The increasing incidence of non-shockable OHCA in Singapore mirrors the global situation. Fuelled by the rapidly aging population in Singapore8 and increasing disease burden of cardiovascular and non-cardiovascular co-morbidities,9 we observed increasingly older and sicker non-shockable OHCA patients, and predominance of residential OHCA which tend to be unwitnessed. Unsurprisingly, the proportion of non-shockable OHCA attributed to non-cardiac etiology increased. The improved rates of bystander CPR, in-hospital interventions and pre-hospital ROSC for non-shockable OHCA did not translate into improved survival to hospital discharge, which ran contrary to our hypothesis and contrasted with the improved outcomes for shockable OHCA. We offer a few explanations for our findings: (1) pre-hospital ROSC in our registry was defined as any ROSC, whether sustained or not, and a proportion of these patients with pre-hospital ROSC may not have sustained it and survived to hospital admission,24 (2) the increasingly older and sicker non-shockable OHCAs with longer ischemic duration may have had injuries too severe to salvage, hence nullifying the improvements in pre-hospital and in-hospital interventions, and (3) there were few effective in-hospital therapies (PCI and TTM); while the use of these therapies increased over time, they were not applied sufficiently for non-shockable OHCA.
Singapore systematically introduced a bundle of three public health bystander-focused interventions between 2012 and 2016, which greatly improved bystander CPR rates over the study period.13 While bystander CPR increased the odds of survival to discharge and good neurological outcomes for non-shockable OHCA in our study, the interactions between bystander CPR with residential arrests and no-flow time are worth mentioning. Bystander CPR reduced the odds of survival and good neurological outcomes for residential arrests and longer no-flow time. Taken together, the interactions suggested a counter-benefit of bystander CPR on sicker patients (older, more co-morbidities) with longer duration of primary injury (no-flow time), presumably due to worse ischemic-reperfusion response (secondary injury). Furthermore, little is known about the quality of bystander CPR, which may have been suboptimal in OHCAs occurring at home, depending on the bystander characteristics (demographics and prior training in CPR) and home condition (ease of finding a flat hard surface etc). In heavily-urbanized Singapore, CPR performed by EMS personnel may have been compromised in quality if performed during vertical transportation. Information on CPR performance metrics and bystander characteristics should be further investigated.
We observed increasing duration of no-flow time for non-shockable OHCA over the study period, despite systematic introduction of DA-CPR, community CPR and AED training, and mobile community first-responder scheme. This was specifically observed in older non-shockable OHCA. Our data offered a few possible explanations for this: (1) Older, non-shockable OHCA occurred more often at home, hence they were more likely to be unwitnessed, (2) Even if these residential arrests were witnessed, the bystanders were probably older spouses likely to display some initial hesitation in performing bystander CPR, and required coaxing and coaching by the dispatchers, and (3) Time to patient increased significantly over the study period, reflecting the challenges faced by EMS personnel and first responders (including community first responders) in reaching the victims in our heavily-urbanized country.
Prior studies have suggested that PEA and asystole, while frequently grouped together as non-shockable rhythms, are different entities with different pre-arrest and intra-arrest characteristics, and portend different outcomes.25, 26, 27 Despite less bystander CPR and similar rates of in-hospital interventions throughout the study period, clinical outcomes were consistently better in PEA compared to asystole. Asystole, being the final endpoint of all rhythms of arrest, may represent PEA which degenerated without effective intervention, reflecting the duration of no-flow and low-flow time. The etiologies of OHCA may account for different initial rhythms and it is conceivable that PEA reflects reversible etiologies amenable to therapy. Detailed information on the etiologies of OHCA would have been good to have but was not available for the study.
Presumed cardiac etiology was associated with poorer outcomes in our study, running contrary to existing literature.1, 28 As prior studies included both shockable and non-shockable OHCA, it is plausible the improved outcomes seen with OHCA of presumed cardiac etiology were driven by shockable OHCAs, which are more likely due to acute coronary occlusion amenable to coronary revascularization.29 Non-shockable OHCAs of presumed cardiac etiology may have been associated with end-stage heart diseases or acute coronary syndromes that started out with shockable rhythms before degenerating into non-shockable rhythms, conditions which are less reversible and portend worse prognosis. Furthermore, misclassification of etiology in our registry could not be excluded despite best efforts.30
The strengths of our study include the population-based registry with data collection based on Utstein definitions for reporting cardiac arrest and the capture of all EMS-attended OHCA cases. The registry has in-built quality control measures and regular data audits to ensure data quality and integrity. Nonetheless, our study should be interpreted in the context of the following limitations. The observational nature of the study precluded causality. The registry collected mainly pre-hospital and essential hospital data variables, and we lacked granular information on socioeconomic factors, vertical location of arrest, hospital-based management, etiologies of arrest and long-term functional outcomes. There were varying amounts of missing data for all OHCA cases, albeit a small proportion (<2%). Finally, as with all epidemiological studies, ascertainment bias and misclassifications were other potential limitations.
Our findings have important clinical implications. The incidence of non-shockable OHCA, in particular older (≥65 years) non-shockable OHCA, is likely to continue to increase in Singapore and other parts of the world with ageing populations, putting a strain on EMS, hospital and community resources. We need to improve our practice of patient selection in order to rationalize limited resources. Termination of resuscitation protocol was implemented by the SCDF in January 201927; a before-after comparison would allow us to evaluate if better rationalization of resources (i.e. transport to acute hospitals and definitive hospital care) translates into improved outcomes. Leveraging on validated risk scores to select patients for intensive care at the hospital level would similarly allow us to focus our efforts on those with higher likelihood of survival with good neurological outcomes and should be considered. Our study also highlights the complex interplay of variables contributing to the poorer outcomes for OHCAs happening in residential settings and the need for focused public health interventions.
Conclusion
Singapore saw increasing incidence of and interventions for OHCA with non-shockable rhythms between 2010 and 2019, but limited gains in survival, partly explained by the ageing population with increasing comorbidities and residential arrests. This contrasts with the improvement in survival for shockable OHCA. Our findings highlight the need for more research in optimizing patient selection for pre-hospital termination of resuscitation and in-hospital advanced interventions.
CRediT authorship contribution statement
Shir Lynn Lim: Conceptualization. Marcus Eng Hock Ong: Conceptualization, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank Ms Pek Pin Pin and the late Ms Susan Yap from Department of Emergency Medicine, Singapore General Hospital; Ms Nurul Asyikin, Ms Noor Azuin and Ms Joann Poh from Unit for Prehospital Emergency Care, Singapore General Hospital; Ms Woo Kai Lee from Department of Cardiology, National University Heart Centre Singapore and Ms Charlene Ong previously from Accident & Emergency, Changi General Hospital for their contributions and support to the Singapore OHCA registry.
Singapore PAROS Investigators:
Michael YC Chia (Tan Tock Seng Hospital, Singapore); Yih Yng Ng (Tan Tock Seng Hospital, Singapore); Han Nee Gan (Changi General Hospital, Singapore); Ling Tiah (Changi General Hospital, Singapore); Wei Ming Ng (Ng Teng Fong General Hospital, Singapore); Wei Ling Tay (Ng Teng Fong General Hospital, Singapore); Si Oon Cheah (Urgent Care Clinic International, Singapore); Desmond R Mao (Khoo Teck Puat Hospital, Singapore); Nausheen Edwin Doctor (Sengkang General Hospital, Singapore); Lai Peng Tham (KK Women’s and Children’s Hospital, Singapore).
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100473.
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Lim S.L., Smith K., Dyson K., et al. Incidence and outcomes of out-of-hospital cardiac arrest in Singapore and Victoria: a collaborative study. J Am Heart Assoc. 2020;9:e015981. doi: 10.1161/JAHA.119.015981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajan S., Folke F., Hansen S.M., et al. Incidence and survival outcome according to heart rhythm during resuscitation attempt in out-of-hospital cardiac arrest patients with presumed cardiac etiology. Resuscitation. 2017;114:157–163. doi: 10.1016/j.resuscitation.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 3.Berdowski J., Berg R.A., Tijssen J.G., Koster R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Bunch T.J., White R.D., Friedman P.A., Kottke T.E., Wu L.A., Packer D.L. Trends in treated ventricular fibrillation out-of-hospital cardiac arrest: a 17-year population-based study. Heart Rhythm. 2004;1:255–259. doi: 10.1016/j.hrthm.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Cobb L.A., Fahrenbruch C.E., Olsufka M., Copass M.K. Changing incidence of out-of-hospital ventricular fibrillation, 1980–2000. JAMA. 2002;288:3008–3013. doi: 10.1001/jama.288.23.3008. [DOI] [PubMed] [Google Scholar]
- 6.Oving I., de Graaf C., Karlsson L., et al. Occurrence of shockable rhythm in out-of-hospital cardiac arrest over time: a report from the COSTA group. Resuscitation. 2020;151:67–74. doi: 10.1016/j.resuscitation.2020.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Daya M.R., Schmicker R.H., Zive D.M., et al. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC) Resuscitation. 2015;91:108–115. doi: 10.1016/j.resuscitation.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Population and Talent Division SG, Prime Minister’s Office. Population in Brief; 2021. [Accessed 13 September 2022, at https://www.population.gov.sg/files/media-centre/publications/population-in-brief-2021.pdf].
- 9.Singapore Health Facts – Disease Burden; 2020 [Accessed 13 September 2022, at https://www.moh.gov.sg/resources-statistics/singapore-health-facts/disease-burden].
- 10.Engdahl J., Bång A., Lindqvist J., Herlitz J. Factors affecting short- and long-term prognosis among 1069 patients with out-of-hospital cardiac arrest and pulseless electrical activity. Resuscitation. 2001;51:17–25. doi: 10.1016/s0300-9572(01)00377-x. [DOI] [PubMed] [Google Scholar]
- 11.Folke F., Gislason G.H., Lippert F.K., et al. Differences between out-of-hospital cardiac arrest in residential and public locations and implications for public-access defibrillation. Circulation. 2010;122:623–630. doi: 10.1161/CIRCULATIONAHA.109.924423. [DOI] [PubMed] [Google Scholar]
- 12.Granfeldt A., Wissenberg M., Hansen S.M., et al. Clinical predictors of shockable versus non-shockable rhythms in patients with out-of-hospital cardiac arrest. Resuscitation. 2016;108:40–47. doi: 10.1016/j.resuscitation.2016.08.024. [DOI] [PubMed] [Google Scholar]
- 13.Blewer A.L., Ho A.F.W., Shahidah N., et al. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: a cohort study. Lancet Public Health. 2020;5:e428–e436. doi: 10.1016/S2468-2667(20)30140-7. [DOI] [PubMed] [Google Scholar]
- 14.Lin H.Y., Chien Y.C., Lee B.C., et al. Outcomes of out-of-hospital cardiac arrests after a decade of system-wide initiatives optimising community chain of survival in Taipei city. Resuscitation. 2022;172:149–158. doi: 10.1016/j.resuscitation.2021.12.027. [DOI] [PubMed] [Google Scholar]
- 15.Chua S.Y.I., Ng Y.Y., Ong M.E.H. Getting R-AEDI to save lives in Singapore. Singapore Med J. 2020;61:60–62. doi: 10.11622/smedj.2020013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pourghaderi A.R., Kogtikov N., Lees M.H., et al. Maximum expected survival rate model for public access defibrillator placement. Resuscitation. 2022;170:213–221. doi: 10.1016/j.resuscitation.2021.11.039. [DOI] [PubMed] [Google Scholar]
- 17.Ong M.E., Shin S.D., Tanaka H., et al. Pan-Asian Resuscitation Outcomes Study (PAROS): rationale, methodology, and implementation. Acad Emerg Med. 2011;18:890–897. doi: 10.1111/j.1553-2712.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 18.Perkins G.D., Jacobs I.G., Nadkarni V.M., et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest. Circulation. 2015;132:1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 19.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.Edgren E., Hedstrand U., Kelsey S., Sutton-Tyrrell K., Safar P. Assessment of neurological prognosis in comatose survivors of cardiac arrest. BRCT I Study Group. Lancet. 1994;343:1055–1059. doi: 10.1016/s0140-6736(94)90179-1. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organisation. Age Standardization of Rates: A New WHO Standard; 2001. [Accessed 13 September 2022, at https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf].
- 22.Zellner A. An efficient method of estimating seemingly unrelated regressions and tests for aggregation bias. J Am Stats Assoc. 1962;57:348–368. [Google Scholar]
- 23.Akaike H. In: Selected papers of Hirotugu Akaike. Parzen E., Tanabe K., Kitagawa G., editors. Springer New York; New York: 1998. A new look at the statistical model identification. [Google Scholar]
- 24.Salcido D.D., Stephenson A.M., Condle J.P., Callaway C.W., Menegazzi J.J. Incidence of rearrest after return of spontaneous circulation in out-of-hospital cardiac arrest. Prehosp Emerg Care. 2010;14:413–418. doi: 10.3109/10903127.2010.497902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fukuda T., Ohashi-Fukuda N., Matsubara T., et al. Association of initial rhythm with neurologically favorable survival in non-shockable out-of-hospital cardiac arrest without a bystander witness or bystander cardiopulmonary resuscitation. Eur J Intern Med. 2016;30:61–67. doi: 10.1016/j.ejim.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 26.Ko D.T., Qiu F., Koh M., et al. Factors associated with out-of-hospital cardiac arrest with pulseless electric activity: a population-based study. Am Heart J. 2016;177:129–137. doi: 10.1016/j.ahj.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 27.Myerburg R.J., Halperin H., Egan D.A., et al. Pulseless Electric Activity: definition, causes, mechanisms, management, and research priorities for the next decade: report from a National Heart, Lung, and Blood Institute workshop. Circulation. 2013;128:2532–2541. doi: 10.1161/CIRCULATIONAHA.113.004490. [DOI] [PubMed] [Google Scholar]
- 28.Wittwer M.R., Zeitz C., Beltrame J.F., Arstall M.A. Aetiology of resuscitated out-of-hospital cardiac arrest treated at hospital. Resuscitation. 2022;170:178–183. doi: 10.1016/j.resuscitation.2021.11.035. [DOI] [PubMed] [Google Scholar]
- 29.Spirito A., Vaisnora L., Papadis A., et al. Acute coronary occlusion in patients with non-ST-segment elevation out-of-hospital cardiac arrest. J Am Coll Cardiol. 2023;81:446–456. doi: 10.1016/j.jacc.2022.10.039. [DOI] [PubMed] [Google Scholar]
- 30.Kürkciyan I., Meron G., Behringer W., et al. Accuracy and impact of presumed cause in patients with cardiac arrest. Circulation. 1998;98:766–771. doi: 10.1161/01.cir.98.8.766. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.