Abstract
Objectives:
The purpose of this study was to: [1] Assess inter-rater reliability of a novel technique for measurement of NSA; [2] Use pelvic anteroposterior (AP) radiographs of unaffected hips to assess variability of NSA; [3] Evaluate the side-to-side variability of NSA to determine reliability of using the contralateral hip as a template.
Design:
Retrospective cohort study
Setting:
Academic Level 1 regional trauma center
Patients/Participants:
406 femora (203 patients) with standing AP pelvis radiographs were selected. Exclusions included lack of acceptable imaging, congenital abnormalities, or prior hip surgery.
Intervention:
An anteroposterior pelvis radiograph in the standing position.
Main Outcome Measurements:
Bilateral NSA measurements obtained in a blinded fashion between two reviewers. Pearson coefficients and coefficient of determination assessed correlations and variability between left and right NSA. Concordance correlation coefficients assessed the inter-rater reliability between measurements performed by the two reviewers.
Results:
203 patients (406 femora) were assessed. Male patients had a lower overall NSA mean of 131.56° ± 4.74 than females with 133.61° ± 5.17. There was no significant difference in NSA side to side in females (p=0.18, 0.3° (95% CI [−0.15, 0.75)) or males (p=0.68, 0.19° (95% CI [−0.74, 1.12)). There was a strong linear relationship between left and right femora (r2=0.70). 41% of patients fell within the 131-135° range bilaterally. 88% of patients had <5° difference in NSA bilaterally and 0% had >10° difference.
Conclusions:
There is no significant variability between bilateral femora in males and females. Use of this measurement method and contralateral NSA for proximal femur fracture planning is supported.
Levels of Evidence:
Level III, Retrospective Cohort Study
Introduction
Proximal femur fractures are common and debilitating injuries (2-6) which include femoral neck, intertrochanteric, and subtrochanteric femur fractures. The latter can include a proximal extension that may include combined intertrochanteric and femoral neck fracture patterns (7). Varying degrees of technical skill are required depending on fracture pattern, patient factors, and availability of required implants and reduction tools (7). Appropriate management of proximal femur fractures is critical for both young and old patients, as suboptimal management of these injuries can result in fracture nonunion or malunion, avascular necrosis, and fixation failure (8, 9). Restoration of the patient’s native anatomy is a critical aspect of reduction during fracture repair and requires insight into the reliability of native femoral neck shaft angle (NSA).
Treatment of a proximal femoral fracture includes optimal restoration of the normal anatomy using various implants, with fixed angle implants being a commonly chosen device. Proximal femur fractures are often discussed in terms of their stability and implants are chosen for similar reasons: Intramedullary nail (IMN) has become the most common choice for unstable fracture patterns (10), while stable patterns may be managed with an IMN, dynamic hip screw (DHS), or blade plate (6, 10, 11). Intramedullary devices have been found to bear greater load than extramedullary devices (2). Studies on implant loading confirm that varus malreduction causes increased implant loading and decreased fracture stability (2), leading to higher likelihood of complication and underscoring the need for restoration of native NSA.
Understanding of the patient’s native NSA, also known as the caput-collum-diaphyseal (CCD) angle, is crucial to avoid varus malreduction (12). In the frequent absence of pre-injury radiographs of the injured hip, the NSA of the contralateral side is most frequently used as a surrogate. Further, NSA measurement methodology varies widely in the literature (12). Boese CK, et al performed a systematic review of 26 publications measuring NSA on conventional radiographs, discovering that many authors failed to define or only partially described how they performed measurements. Inter-rater reliability ranged widely from ICC of 0.58 to 0.89 (12, 13). Others have found that NSA measurement error range is between ±2 to 6°, which could result in iatrogenic varus malreduction and subsequent fixation failure (14, 15).
Multiple variables that may influence the femoral NSA have been documented. Femoral NSA generally falls between 120-140°, with coxa vara defined as NSA<120° and coxa valga defined as NSA>140°. Gilligan et al studied human skeletons and compared left and right femurs in the same specimens, finding a mean NSA of 126.4° in 8,271 femora, a significant difference of 1.3° between left and right femur, but no sex-based differences (1). Other studies have had similar results and noted variability in NSA (13, 16-18). However, these studies compared large, combined cohort data sets rather than between individual patients. Croom et al compared side-to-side variability of femoral rotational profile, and surprisingly showed a greater than 10° difference between sides in 17% of uninjured patients (19).
Restoration of native proximal femoral anatomy requires the best possible reduction and selection of an implant that the surgeon feels will maintain that reduction and mitigate the risk of screw cut-out from the femoral head (20, 21). Fixed angle implants range between a 120 and 150° NSA, in addition to a dynamic condylar screw (DCS) or angled blade plate with a 95° angle. The 125° CMN is the most commonly used implant angle cited in limited research, despite controversy regarding the most common native NSA (22).
Fixed angle implants are often selected to match the patient’s natural anatomy by utilizing the morphology and NSA of the contralateral uninjured proximal femur. Minimal evidence exists, however, regarding the appropriateness of utilizing this approach due to the aforementioned evidence of bilateral asymmetry and gender differences. The variability in measuring and reproducing NSA further complicates the applicability of this technique. Therefore, the aims of this study were the following: [1] Assess inter-rater reliability in a specific technique measurement of NSA; [2] Assess the variability and range of NSA within our patient population using plain radiographs of bilateral, unaffected hips; [3] Evaluate the side-to-side variability in NSA of bilateral femora to assess the adequacy of utilizing the contralateral, uninjured hip as a template in the setting of proximal femur fractures.
Materials and Methods
A total of 214 patient radiographs were obtained from a database maintained by the senior author (TGM). Inclusion criteria were adults ≥ 18-year-old and presence of acceptable standing pelvis radiographs that capture the pelvis and bilateral proximal femora. Imaging was performed at our institution’s surgical center with well-defined protocol for radiographical imaging that required patients to stand with extremities parallel in a neutral position with toes pointed directly forward (23). Exclusion criteria included patients without acceptable imaging (incomplete AP pelvis radiograph not including the entire pelvis and bilateral proximal femora), post-traumatic proximal femoral deformities or congenital abnormalities, and history of prior trauma or proximal femoral surgery. Review of imaging was performed in a blinded fashion by two study authors. Eleven patients were removed during the review due to exclusion criteria, leaving a total of 203 patients (406 femora) who underwent measurement on Philips Intellispace PACS Enterprise (© Koninklijke Philips N.V., 2004 - 2020).
NSA Measurement
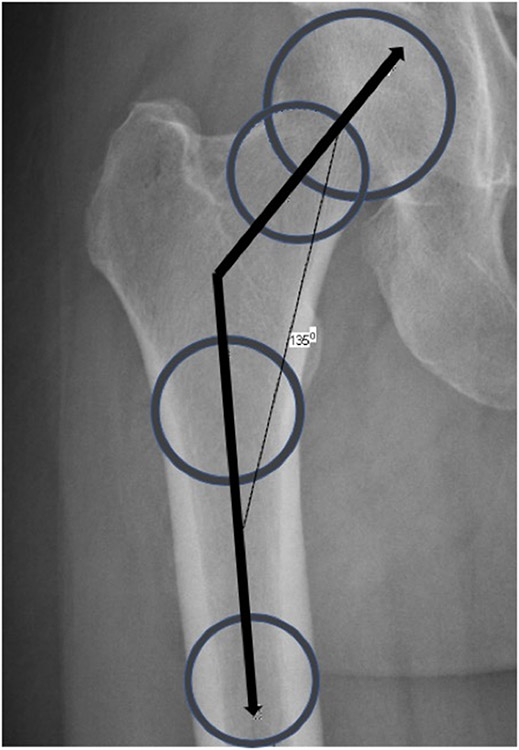
Individual patient pelvic radiographs underwent measurement of bilateral NSA by two blinded reviewers specialized in orthopaedic surgery using identical imaging software. The NSA was defined in the method espoused by Boese et al (12): [1] The femoral neck axis was calculated by drawing a line connecting two circles located at the center of the femoral head and the center of the femoral neck (12). [2] The femoral long axis was measured by placing two circles in the diaphyseal femur (12). The proximal circle was placed at the lower margin of the lesser trochanter and the distal circle was placed at the furthest aspect of the femur available on the radiograph. The circle was drawn until it reached the edge of the cortex. A line was drawn connecting both circles. [3] The NSA was calculated between the line of the femoral neck axis and the femoral long axis (Figure 1). This technique was performed bilaterally for each patient and labeled by laterality.
Figure 1.
Femoral neck shaft angle calculation performed by identifying the angle between the femoral neck axis and the femoral long axis.
Statistics
Data was summarized with mean, standard deviation (SD) and percentage of the cohort. The mean NSA by sex was compared with the t-test and box plot. Given numeric data within a parametric distribution, paired T-test was used to compare difference means between NSA of the right and left femur. Pearson correlation coefficient (r) and the coefficient of determination (r2) were used to measure correlations and variabilities between inter-patient (overall cohort, male and female cohorts) left and right NSA. The coefficient of determination provided insight into the amount of observed variance in one femur that is predicted by the contralateral femur and denotes the strength of the linear association between the two. Intra-patient variation was assessed using the coefficient of variation (CV), in order to describe the relative variability of femora in individual patients. This is calculated as the ratio of the standard deviation to the mean (24). Concordance correlation coefficients were calculated to assess the inter-rater reliability between first measure and second measure performed by two reviewers. Bland-Altman plots were used to visualize the agreement.
Results
A total of 203 patients (406 femora) were assessed for NSA variability as a group. The data set included 53 (26.1%) males and 150 (73.9%) females. The entire cohort NSA mean ± SD was 133.07° ± 5.13 and when separated by laterality, the cohort’s right femur NSA was 133.21° ± 5.18 and the left femur NSA was 132.94° ± 5.11. However, there was no significant difference between NSA of right and left femur in the entire cohort (p=0.59, −0.27° (95% CI [−1.27, 0.73)) (Table 1).
Table 1:
Patient Demographic and Neck-Shaft Angle Characteristics
| Patient Demographics and Neck-Shaft Angle Characteristics | ||
|---|---|---|
| Variable | N* | |
| Total Number of Patients | 203 patients (406 femora) | |
| Sex | Male | 53 |
| Female | 150 | |
| NSA | Cohort | 133.07° ± 5.13 |
| (mean ± SD) | ||
| Cohort L v R NSA | −0.27° (95% CI [−1.27, 0.73]) p=0.59 |
|
| Male NSA | 131.56° ± 4.74 | |
| Female NSA | 133.61° ± 5.17 | |
| (mean ± SD) | ||
| Male v Female NSA | 2.04° (95% CI [0.92, 3.17]) p=0.01 |
|
| Male L v R NSA | 0.19° (95% CI [−0.74, 1.12]) p=0.68 |
|
| Female L v R NSA | 0.3° (95% CI [−0.15, 0.75] p=0.18 |
|
| Inter-patient Assessment | ||
| Pearson Correlation Coefficient (r) | Cohort | r=0.84 |
| (between L and R femora) | Male | r=0.75 |
| Female | r=0.86 | |
| Coefficient of Determination (r2) | Cohort | r2=0.70 (p<0.01) |
| Male | r2=0.56 (p<0.01) | |
| Female | r2=0.74 (p<0.01) | |
| Intra-patient Assessment | ||
| Coefficient of Variation (CV) | Intra-patient CV | 84.3% |
NSA = Neck-Shaft Angle, L = left, R = Right, SD = Standard Deviation, CI = Confidence Interval
The data set was then separated by sex. Male patients had a significantly lower overall NSA mean of 131.56° ± 4.74 compared to the overall NSA mean in female patients of 133.61° ± 5.17 (p=0.01, 2.04° (95% CI [0.92, 3.17]). When looking specifically at left and right femora by sex, male patients had a mean NSA of 131.47° ± 4.82 on the left and 131.66° ± 4.71 on the right versus female patient mean NSA of 133.46 ± 5.11 on the left and 133.76° ± 5.25 on the right. There were no significant differences in NSA between right and left femora in males (p=0.68, 0.19° (95% CI [−0.74, 1.12])) or in females (p=0.18, 0.3° (95% CI [−0.15, 0.75])). The data was also assessed by two standard deviations from the mean. This is represented in Table 2A and Table 2B.
Table 2A.
Mean Neck-Shaft Angle Degree ± 2 Standard Deviations by Laterality in Male Patients
| Laterality | 2 SD below | 1 SD below | Mean | 1 SD above | 2 SD above |
|---|---|---|---|---|---|
| Left | 121.83 | 126.95 | 131.47 | 136.29 | 141.11 |
| Right | 122.24 | 126.95 | 131.66 | 136.37 | 141.08 |
SD = Standard Deviation
Table 2B.
Mean Neck-Shaft Angle Degree ± 2 Standard Deviations by Laterality in Female Patients
| Laterality | 2 SD below | 1 SD below | Mean | 1 SD above | 2 SD above |
|---|---|---|---|---|---|
| Left | 123.24 | 128.35 | 133.46 | 138.57 | 143.68 |
| Right | 123.26 | 128.51 | 133.76 | 139.01 | 144.26 |
SD = Standard Deviation
The magnitude of the correlation between the NSA of right and left femora was assessed in several ways: inter-patient correlation was performed by assessing the NSA on both sides in the larger cohort as well as by sex versus the intra-patient correlation, which was performed by assessing the NSA bilaterally in each individual (Table 1). The inter-patient correlation between left and right femoral NSA was isolated with Pearson correlation coefficients (r) to assess correlation between the variable of NSA between left and right femurs. The entire cohort of patients had a high positive correlation (r=0.84). When further separated by sex, the correlation coefficients comparing left and right femora in males was 0.75, and 0.86 when comparing left and right femora in females. The amount of observed variance in one femur that can be predicted from the other femur was further assessed with the coefficient of determination (r2), as seen in Table 1. The overall r2 of the entire cohort was 0.70, meaning that 70% of observed variance in one femur is predicted by the anatomy and morphology of the other side, denoting a strong linear relationship between left and right femora. The intra-patient variation between left and right femora utilized the differences between NSA in individual patients and was assessed with CV and found to be 84.3%. Furthermore, patients were separated in groups depending on how many degrees of variation were found between NSA in individual patients (Table 3).
Table 3.
Intra-patient Variation in Neck-Shaft Angle
| Difference in NSA | Cohort (%) | Female (%) | Male (%) |
|---|---|---|---|
| <5° | 87.68 | 88 | 86.79 |
| 5-10° | 12.32 | 12 | 13.21 |
| >10° | 0 | 0 | 0 |
NSA = Neck-Shaft Angle
Two members of the study team performed the NSA measurements in every patient. Inter-rater reliability of NSA was calculated with concordance correlation coefficients in order to assess the reproducibility of the measurements. The overall correlation coefficient was 0.91 for both left and right femora,
Patients were separated into groups based on the NSA angle in the following ranges: 115-119, 120-125, 126-130, 131-135, 136-140, 141-145, 146-150, and 151-155° (Table 4). Almost half of the patients fell within the 131-135° range on both the left and right side. Approximately 25% of patients fell into the 126-130° range bilaterally and approximately 20% into the 136-140° range bilaterally. The number of patients meeting the definition of coxa vara (<120°) on one or both sides was 1 (0.5%) and the number of patients meeting the definition of coxa valga (>140°) on one or both sides was 23 (11.3%).
Table 4.
Neck-Shaft Angle Groups by Laterality
| Right NSA | Left NSA | ||||
|---|---|---|---|---|---|
| Degrees | Number | % | Degrees | Number | % |
| 115-119 | 0 | 0 | 115-119 | 1 | 0.49 |
| 120-125 | 12 | 5.91 | 120-125 | 11 | 5.42 |
| 126-130 | 49 | 24.14 | 126-130 | 52 | 25.62 |
| 131-135 | 83 | 40.89 | 131-135 | 83 | 40.89 |
| 136-140 | 43 | 21.18 | 136-140 | 40 | 19.7 |
| 141-145 | 11 | 5.42 | 141-145 | 12 | 5.91 |
| 146-150 | 4 | 1.97 | 146-150 | 3 | 1.48 |
| 151-155 | 1 | 0.49 | 151-155 | 1 | 0.49 |
| Total | 203 | 100 | Total | 203 | 100 |
Neck-Shaft Angle
Discussion
The aims of this study were to improve the understanding of this NSA measurement technique accuracy, assess the baseline variations in proximal femur morphology, and evaluate how these variations could influence fracture fixation. This method of measuring femoral NSA was reproducible between observers and temporally between repeated observations. Female patients had a larger NSA than males, and the 41% of patients’ NSA ranged within 131-135° bilaterally. There was a strong linear correlation between bilateral femora NSA and the majority of patients (88%) had <5° difference between their NSA bilaterally, allowing the contralateral femur to be a suitable surrogate when restoring NSA in the setting of a proximal femur fracture. Only 12% of patients had between 5-10° difference between their NSA bilaterally and none had a >10° difference.
This approach to measuring NSA had reassuring inter-rater reliability with a concordance correlation coefficient of 0.91, particularly given the historical methodological differences and inaccuracies in NSA measurement (14, 15, 25-27). The method proposed by Boese, et al that has been utilized here appears to be a reproducible way to obtain NSA between multiple reviewers and should be considered for use in future studies focused on femoral NSA (12). Moreover, when calculating femoral NSA for surgical planning, this technique may be used to accurately determine this angle. Anyone who has attempted to measure NSA using lines on a plain film can attest to the subjectivity of placing these lines. The described technique appears to remove some of this subjectivity by using multiple circles to define axes. Establishing a gold standard for NSA measurement would be helpful in the setting of both future research efforts (15) and surgical planning.
It should be noted that our study found an average femoral NSA of 133.07°, significantly higher than historical findings which have a documented a range between 125-131° (18, 22, 28-31). Methods of femoral NSA measurement notoriously vary between studies, without an established and transparent manner of measurement (12). Additionally, many studies have been performed on cadaveric femora (1, 18, 26) and these studies did not necessarily account for the femoral anteversion (26). All of these factors could, at least in part, explain the differences in femoral NSA and speak to the importance of standardizing the measurement method for imaging modalities.
Current approaches to proximal femur fracture fixation can utilize the contralateral femur as a surrogate (32). Identifying and understanding the inherent variability in bilateral femora of individual patients is crucial for deciding if one can utilize the contralateral femoral NSA in the setting of proximal femur fixation. The current study data support the use of the contralateral femur as a reasonable surrogate during fracture fixation, with both female and male patients having a strong positive correlation between the femoral NSA of bilateral femora. The coefficient of determination supports this conclusion, demonstrating that the majority of individual femoral anatomy can be predicted by the same individual’s contralateral anatomy with a strong, linear correlation between the two (entire cohort r2=0.7, p<0.01). Additionally, 88% of patients had less than 5° difference between their femoral NSA.
Implant selection is complex in that the surgical goal is to not only restore anatomic NSA but optimize the reduction and subsequent healing (32, 33). Within our large cohort, female patients had a slightly larger NSA than males by two degrees. Moreover, coxa valga was significantly more common than coxa vara in both sexes. This information is useful when selecting the appropriately angled implant from a selection that can vary depending on hospital availability and surgeon preference. These data may also be helpful in the setting of managing bilateral proximal femur fractures, or if a patient has a contralateral femur with significant deformity that makes the measurement of the contralateral NSA inadequate. The gaussian curve generated by the data demonstrated that 68% of female NSAs occurred within 128-139° bilaterally and male NSAs within 127-136°. Refined further, 41% of our patients fell within the 131-135° range. Implant NSA angle options are typically 120, 125, 130, 135, 145 and 150°, and the available angles vary depending on the brand of implant. Given the aforementioned data, it may be reasonable to utilize a fixed angle implant that mirrors native anatomy. A femoral NSA in the range of 131-135° can be used as the default in the setting of bilateral fractures, congenital deformities or if limited by implant availability. Moreover, the demonstration of slightly increased NSA in females and the propensity for coxa valga may be helpful in the absence of reliable comparison data.
The importance of accurate proximal femoral reduction is supported by prior research on varus malreduction of proximal femoral fractures. Varus malreduction has been shown to increase the risk for lag screw cut out through the anterior superior femoral head with resultant varus collapse (21, 30, 34, 35). For this reason, fracture fixation in slight valgus is recommended, as both CMN and SHS fixation may experience 4° of varus collapse in the first 6 weeks after fixation (30, 34). Parry et al assessed a group of 83 patients and found that post-operative NSA was significantly less than native NSA (127±5° post-operatively versus 129±6° pre-operatively, p=0.0002), with the average NSA produced by the reduction and implantation differing from the native angle by −4±5° and with 80% of patients ultimately having a NSA less than their native angle based on contralateral femur (30). Varus malreduction was associated with the use of a nail with an NSA less than the native NSA (30). The utilization of contralateral NSA from pre-operative radiographs may ensure selection of an impact with an NSA that matches or is greater than native NSA.
Limitations
While the current study utilized a large patient cohort and a very reproducible measurement methodology, it nevertheless had limitations. While the sample size was large (n=203, 406 femora), we had a higher proportion of female (n=150) than male (n=53) patients, which could affect the application of these data to male patients. However, we utilized robust statistical analyses in which the number of male patients included was more than sufficient and thus should not affect these results. All patients included in the current study were seen within one hospital system and thus may be subject to regional ethnic sampling biases. Prior studies have suggested that femoral NSA varies in different ethnic groups and regions around the world (1, 36). Our patient population may be more homogenous than international studies.
Acquisition of pelvic radiographs could have affected femoral NSA measurement as hip rotation has been identified as a factor affecting the measurement of NSA on plain film (26, 37, 38). In order to correct for femoral rotation and version, bi-planar radiographic methods have been developed (39, 40). Our plain anteroposterior pelvic films were standardized such that each film was obtained with the patient in a standing position and positioned to include the iliac crest and an extended femoral shaft view to allow improved angle calculations. Extremities were kept parallel and in a neutral position with toes pointed directly forward (23). This positioning was consistently maintained by our musculoskeletal radiology technicians in order to minimize rotational variation. While we did not utilize biplanar imaging, our technique has been previously evaluated (15) and found to be adequate. Utilizing standing, weight bearing AP pelvic radiographs may affect the extrapolation of our results to imaging obtained in a supine position, the typical position of patients with a femoral fracture. The patient is also not in a weight- bearing posture intra-operatively at the time of hip fracture repair.
Conclusion
This large cohort of patients had a mean NSA of 133.07° without a significant difference between left and right femora. The NSA is notably higher than in prior studies. Female patients have a higher mean NSA than males and neither sex had significant differences between left and right femora. 41% of patients fall within the NSA range of 131-135°. There is a strong linear correlation between bilateral femoral NSA in both sexes. The majority of patients have <5° difference between bilateral NSA. NSA measurement can be reliably reproduced using the method described in this manuscript.
References
- 1.Gilligan I, Chandraphak S, Mahakkanukrauh P. Femoral neck-shaft angle in humans: variation relating to climate, clothing, lifestyle, sex, age and side. J Anat. 2013;223:133–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Socci AR, Casemyr NE, Leslie MP, et al. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. 2017;99-B:128–133. [DOI] [PubMed] [Google Scholar]
- 3.Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458–1460. [DOI] [PubMed] [Google Scholar]
- 4.Heckmann N, Hill JR, Vakhshori V, et al. Increased Pulmonary Complications Associated with Intramedullary Fixation of Intertrochanteric Fractures: An Analysis of 13,276 Hips. J Am Acad Orthop Surg. 2019;27:690–695. [DOI] [PubMed] [Google Scholar]
- 5.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413. [DOI] [PubMed] [Google Scholar]
- 6.Kim JT, Jung CH, Shen QH, et al. Mechanical effect of different implant caput-collum-diaphyseal angles on the fracture surface after fixation of an unstable intertrochanteric fracture: A finite element analysis. Asian J Surg. 2019;42:947–956. [DOI] [PubMed] [Google Scholar]
- 7.Lundy DW. Subtrochanteric femoral fractures. J Am Acad Orthop Surg. 2007;15:663–671. [DOI] [PubMed] [Google Scholar]
- 8.Goudie EB, Duckworth AD, White TO. Femoral Neck Fractures in the Young. Proximal Femur Fractures: Springer, Cham; 2017:47–58. [Google Scholar]
- 9.Sheehan SE, Shyu JY, Weaver MJ, et al. Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know. Radiographics. 2015;35:1563–1584. [DOI] [PubMed] [Google Scholar]
- 10.Kovalak E, Ermutlu C, Atay T, et al. Management of unstable pertrochanteric fractures with proximal femoral locking compression plates and affect of neck-shaft angle on functional outcomes. J Clin Orthop Trauma. 2017;8:209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brox WT, Roberts KC, Taksali S, et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on Management of Hip Fractures in the Elderly. J Bone Joint Surg Am. 2015;19:1196–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boese CK, Dargel J, Oppermann J, et al. The femoral neck-shaft angle on plain radiographs: a systematic review. Skeletal Radiol. 2016;45:19–28. [DOI] [PubMed] [Google Scholar]
- 13.Doherty M, Courtney P, Doherty S, et al. Nonspherical femoral head shape (pistol grip deformity), neck shaft angle, and risk of hip osteoarthritis: a case-control study. Arthritis Rheum. 2008;58:3172–3182. [DOI] [PubMed] [Google Scholar]
- 14.Mast NH, Impellizzeri F, Keller S, et al. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson JD, Eardley W, Odak S, et al. To what degree is digital imaging reliable? Validation of femoral neck shaft angle measurement in the era of picture archiving and communication systems. Br J Radiol. 2011;84:375–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Isaac B, Vettivel S, Prasad R, et al. Prediction of the femoral neck-shaft angle from the length of the femoral neck. Clin Anat. 1997;10:318–323. [DOI] [PubMed] [Google Scholar]
- 17.Jiang N, Peng L, Al-Qwbani M, et al. Femoral version, neck-shaft angle, and acetabular anteversion in Chinese Han population: a retrospective analysis of 466 healthy adults. Medicine (Baltimore). 2015;94:e891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am. 1987;69:873–880. [PubMed] [Google Scholar]
- 19.Croom WP, Lorenzana DJ, Auran RL, et al. Is Contralateral Templating Reliable for Establishing Rotational Alignment During Intramedullary Stabilization of Femoral Shaft Fractures? A Study of Individual Bilateral Differences in Femoral Version. J Orthop Trauma. 2018;32:61–66. [DOI] [PubMed] [Google Scholar]
- 20.Baumgaertner MR, Curtin SL, Lindskog DM, et al. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. [DOI] [PubMed] [Google Scholar]
- 21.De Bruijn K, den Hartog D, Tuinebreijer W, et al. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J Bone Joint Surg Am. 2012;94:1266–1272. [DOI] [PubMed] [Google Scholar]
- 22.Walton NP, Wynn-Jones H, Ward MS, et al. Femoral neck-shaft angle in extra-capsular proximal femoral fracture fixation; does it make a TAD of difference? Injury. 2005;36:1361–1364. [DOI] [PubMed] [Google Scholar]
- 23.Marchand LS, Todd DC, Kellam P, et al. Is the Lesser Trochanter Profile a Reliable Means of Restoring Anatomic Rotation After Femur Fracture Fixation? Clin Orthop Relat Res. 2018;476:1253–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rousseaux CG, Gad SC. Statistical Assessment of Toxicologic Pathology Studies. Haschek and Rousseaux’s Handbook of Toxicologic Pathology; 2013:893–988. [Google Scholar]
- 25.Bhashyam AR, Rodriguez EK, Appleton P, et al. The Effect of Hip Positioning on the Projected Femoral Neck-Shaft Angle: A Modeling Study. J Orthop Trauma. 2018;32:e258–e262. [DOI] [PubMed] [Google Scholar]
- 26.Liu RW, Toogood P, Hart DE, et al. The effect of varus and valgus osteotomies on femoral version. J Pediatr Orthop. 2009;29:666–675. [DOI] [PubMed] [Google Scholar]
- 27.Olsen M, Davis ET, Gallie PA, et al. The reliability of radiographic assessment of femoral neck-shaft and implant angulation in hip resurfacing arthroplasty. J Arthroplasty. 2009;24:333–340. [DOI] [PubMed] [Google Scholar]
- 28.Kapandji IA. The physiology of the joints. Ed. 2. New York: Churchill Linvingstone; 1970. [Google Scholar]
- 29.Kelley DL. Kinesiology; fundamentals of motion description. New Jersey: Eaglewood Cliffs, Prentice-Hall; 1971. [Google Scholar]
- 30.Parry JA, Barrett I, Schoch B, et al. Does the Angle of the Nail Matter for Pertrochanteric Fracture Reduction? Matching Nail Angle and Native Neck-Shaft Angle. J Orthop Trauma. 2018;32:174–177. [DOI] [PubMed] [Google Scholar]
- 31.Williams PL, Warwick R. Gray’s Anatomy. New York: Churchill Livingstone; 1980. [Google Scholar]
- 32.Parry JA, Barrett I, Schoch B, et al. Validation of Neck-Shaft Angle Correction After Cephalomedullary Nail Fixation. J Orthop Trauma. 2018;32:505–507. [DOI] [PubMed] [Google Scholar]
- 33.Min BW, Lee KJ, Oh JK, et al. The Treatment Strategies for Failed Fixation of Intertrochanteric Fractures. Injury. 2019;50:1339–1346. [DOI] [PubMed] [Google Scholar]
- 34.Pajarinen J, Lindahl J, Savolainen V, et al. Femoral shaft medialisation and neck-shaft angle in unstable pertrochanteric femoral fractures. Int Orthop. 2004;28:347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parker MJ. Valgus reduction of trochanteric fractures. Injury. 1993;24:313–316. [DOI] [PubMed] [Google Scholar]
- 36.Tang ZH, Yeoh CS, Tan GM. Radiographic study of the proximal femur morphology of elderly patients with femoral neck fractures: is there a difference among ethnic groups? Singapore Med J. 2017;58:717–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rippstein J [Determination of the antetorsion of the femur neck by means of two x-ray pictures]. Z Orthop Ihre Grenzgeb. 1955;86:345–360. [PubMed] [Google Scholar]
- 38.Tonnis D Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976:39–47. [PubMed] [Google Scholar]
- 39.Grunert S, Bruckl R, Rosemeyer B. [Rippstein and Muller roentgenologic determination of the actual femoral neck-shaft and antetorsion angle. 1: Correction of the conversion table and study of the effects of positioning errors]. Radiologe. 1986;26:293–304. [PubMed] [Google Scholar]
- 40.Miller F, Liang Y, Merlo M, et al. Measuring anteversion and femoral neck-shaft angle in cerebral palsy. Dev Med Child Neurol. 1997;39:113–118. [DOI] [PubMed] [Google Scholar]