Summary
Traumatic inferior rectus muscle rupture secondary to blunt injury in the absence of associated orbital or ocular fractures or injury is rarely encountered, and there are limited published reports on subsequent surgical repair. We present the case of a 74-year-old man with complete inferior rectus transection following a fall with facial strike. A computed tomography scan of the face was unremarkable. Surgical exploration and repair of the muscle was performed by hooking the inferior oblique muscle to identify the inferior rectus muscle. Subsequent strabismus surgery was performed for residual binocular diplopia, resulting in excellent anatomic and visual outcomes and postoperative ocular alignment.
Introduction
Extraocular muscle rupture secondary to trauma is usually accompanied by other significant orbital injury, such as orbital fractures or globe rupture.1–5 Isolated inferior rectus muscle (IR) rupture following blunt trauma in the absence of associated globe damage or fracture is a rarely encountered clinical entity.6,7 Of the reported cases, none reported subsequent strabismus surgery following initial surgical repair of the ruptured IR. We present a case of isolated IR rupture following a fall and describe clinical findings and surgical management of this case. The current literature is also reviewed.
Case Report
A 74-year-old man presented to Massachusetts Eye and Ear following a mechanical fall that resulted in a facial strike on a fireplace brick. On presentation, the left eye had a visual acuity of 20/150 and a mid-dilated and minimally reactive pupil. Intraocular pressure was 27 mm Hg, and ptosis of the left upper eyelid was noted. There was left hypertropia and complete loss of infraduction on the left, with preservation of other eye movements (Figure 1). Slit-lamp evaluation of the anterior chamber of the left eye showed 2+ red blood cells with hemorrhage noted at the nasal and temporal iris margin, and there was a large inferior conjunctival laceration with associated subconjunctival hemorrhage. A 9 mm portion of the anterior IR muscle was still attached to the globe at its anatomical insertion and protruding through the conjunctival laceration and over the lower lid margin (Figure 2). The posterior chamber intraocular lens was in good position. Dilated fundus examination showed normal macula, vessels, and periphery. The right eye was normal. A computed tomography scan of the face confirmed an intact globe and no orbital fractures. Past ocular history included bilateral pseudophakia.
Figure 1.
Preoperative photographs in nine cardinal directions of gaze.
Figure 2.
Inferior rectus muscle (arrow) protruding through the conjunctival laceration and sitting on the inferior eyelid.
Operative exploration revealed a completely transected IR muscle. A 9 mm anterior IR muscle was inserted 6.5 mm posterior to the inferior limbus. The posterior portion of the IR muscle was not immediately identified as it was retracted into the orbit. Surgical exploration of the inferior quadrants revealed no posterior eye trauma or open-globe injury. The inferior oblique (IO) muscle was subsequently hooked using muscle hooks temporally and nasally and was used as a landmark to locate the posterior portion of the IR muscle, to which it was still attached. A full-thickness, central pass of the suture was used to secure the posterior IR muscle. This was followed by partial thickness, imbricating passes laterally, which were locked at the edges of the muscle. A horizontal mattress suture was used to attach the anterior and posterior IR muscle ends (Figure 3). The lateral edge of the proximal IR muscle was again secured with a full-thickness pass of the suture and attached to the IO muscle for increased security. The conjunctiva was closed, and subconjunctival cefazoline 50 mg / 0.5 mL and dexamethasone 4 mg / 1.0 mL injections were administered.
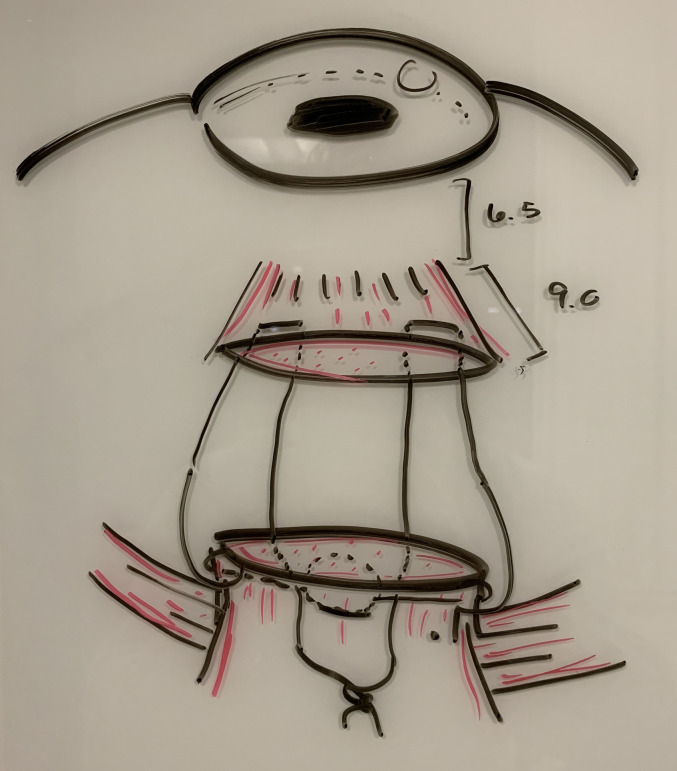
Figure 3.
6-0 Mersilene suture was used to reconnect the two muscle bellies of the inferior rectus muscle.
Postoperatively, the patient regained visual acuity of 20/30, with a fixed, mid-dilated left pupil and persistent oblique binocular diplopia. There was a residual left hypertropia of 16Δ at in primary gaze at distance and a left hypertropia of 4Δ and exotropia of 2Δ at near. There was also persistent limitation in infraduction of the left globe. He underwent strabismus surgery 1 year postoperatively, with right inferior rectus muscle and left superior rectus muscle recessions, resulting in improved postoperative alignment, measuring orthotropia in primary gaze and in downgaze at distance, and subjective resolution of diplopia (Figure 4). He had full ductions of the left eye after the second surgery. Persistent left upper eyelid ptosis was corrected via external levator advancement.
Figure 4.
Postoperative photographs in nine cardinal directions of gaze.
Discussion
The IR muscle is the second most injured muscle in ocular trauma, the first being the medial rectus.3,6 However, IR muscle rupture following blunt trauma without associated orbital fractures or significant ocular injury is rarely encountered (Table 1).6,7 We present a patient with traumatic IR muscle rupture that was primarily anastomosed and who underwent subsequent strabismus surgery, resulting in good ocular alignment. Compared with other reported cases, this case is unique in that the IR muscle was injured in the absence of other orbital injuries or fractures, and secondary strabismus surgery yielded excellent ocular alignment. We discuss a useful surgical approach for IR muscle repair after trauma that allows complete return of muscle function, postoperatively.
Table 1.
Literature review of cases of inferior rectus rupture following blunt trauma in the absence of other associated injuries
In patients with extraocular muscle rupture, muscle repair is the only way to fully regain muscle function. Surgical repair of such injuries is difficult, because the posterior orbital muscle stump immediately retracts into the orbit and becomes difficult to localize. Fortunately, the IR muscle has a unique anatomic association with the IO muscle: the IR and IO muscle sheaths share attachments, as the two muscles cross. This means that the IO muscle can serve as a landmark for retrieval of the posterior portion of the IR muscle during surgical repair. Such association of extraocular muscles with adjacent muscle tissues is not seen with other extraocular muscles. In our patient, the IO muscle, to which the IR muscle was still attached, was identified and hooked intraoperatively. Subsequently, the posterior IR muscle belly was secured and attached to the anterior portion of the IR muscle.
A more difficult, alternative technique, known as generated muscle force duction testing (GDT), can be employed to identify the posterior portion of the IR muscle.7 In GDT, the patient is asked to look in the direction opposite of the action of the muscle of interest. The surgeon explores within the orbit and grasps the suspected Tenon’s capsule of the ruptured extraocular muscle. The patient is then asked to look in the direction of action of the muscle slowly. With purchase on the muscle, the force generated as the patient attempts to look in the direction of action of the muscle may be felt to confirm the location of the proximal muscle. This test may only be performed if the patient is awake or under lighter sedation; it cannot be employed for those under general anesthesia.
In the event of an unidentifiable posterior portion of the IR muscle, management options that provide some restoration of muscle function include transposition of the IO muscle and adjacent rectus muscles and superior rectus muscle recession.8,9 Reattaching muscle fibers of the IO muscle anteriorly changes its vector force and function from elevating and intorting the eye to depression of the globe.10 In addition, initial closure of the conjunctival wounds and reassessment in 1–3 months is also possible with late recovery of the muscle using magnetic resonance imaging guidance as most of these severed muscles will reattach to the globe at some location posteriorly with time.
Eye misalignment secondary to trauma could resolve spontaneously without surgical intervention. Although strabismus surgery following initial IR muscle rupture repair has not been previously reported, it was offered to our patient, who had persistent binocular diplopia. The surgery involved right IR muscle and left superior rectus muscle recessions. Postoperatively, he was orthotropic in primary gaze and in downgaze and maintained full ductions of the left eye. An alternative approach is the Hummelsheim technique, which is traditionally used to treat abducens nerve palsy and involves the transposition of two adjacent rectus muscles to improve ocular alignment and enhance mobility. In Batra et al,11 it was performed for residual ocular misalignment following IR muscle rupture. In that case, the IR muscle was not initially repaired; therefore, it could not be retrieved subsequently during strabismus surgery 5 months after injury. One advantage of the Hummelsheim technique over other transposition techniques is that it prevents anterior segment ischemia, because it spares the ciliary vessel in the nontransposed half of each rectus muscle.12 It also serves as an approach in the case of unidentifiable IR muscle stump. However, the outcome of such approach can be discouraging, with nonoptimal postoperative alignment reported in Batra et al.11 Our patient’s excellent postoperative ocular alignment highlights the possibility of successful immediate IR muscle repair with subsequent strabismus surgery if necessary in patients with extraocular muscle rupture.
Notably, on presentation, our patient displayed a left-sided fixed and dilated pupil. This might have been the result of direct, blunt damage to the ciliary muscle or iris sphincter muscles, or it might have resulted indirectly from interrupted parasympathetic innervation. The parasympathetic fibers that supply the constrictor pupillae and ciliary muscles accompany the oculomotor nerve fibers and terminate in the ciliary ganglion, where they synapse to become part of the short ciliary nerves. Due to its anatomic association with those fibers, IR muscle injury interrupts pupillary parasympathetic innervation, leading to pupillary dilation and lack of pupillary reactivity. In our case, left-sided pupil function did not return, though this was not visually significant for the patient.
Rupture of the IR muscle in the event of trauma to the eye is rarely an isolated injury. IR muscle trauma is more commonly encountered with associated orbital fractures or injury to the globe. The IO muscle is an important landmark that can and should be used to facilitate identification of the posterior portion of the IR muscle, whose fibers run directly through it. Subsequent strabismus surgery can result in excellent ocular alignment and should be considered for resolution of residual binocular diplopia.
Literature Search
PubMed was searched on September 8, 2022, using the following terms: inferior rectus muscle and rupture.
References
- 1.Akiyama K, Karaki M, Hoshikawaa H, Mori N. Retrieval of ruptured medial rectus muscle with an endoscopic endonasal orbital approach: a case report and indication for surgical technique. Auris Nasus Larynx. 2015;42:241–4. doi: 10.1016/j.anl.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Chen J, Kang Y, Deng D, Shen T, Yan J. Isolated total rupture of extraocular muscles. Medicine (Baltimore) 2015;94:e1351. doi: 10.1097/MD.0000000000001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tomasetti P, Metzler P, Jacobsen C. Isolated inferior rectus muscle rupture after blunt orbital trauma. J Surg Case Rep. 20132013 doi: 10.1093/jscr/rjt076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tynan D, Dunn H, Roberts T. Complete inferior rectus transection following blunt trauma: a case report and novel approach to surgical repair. Ophthalmic Plast Reconstr Surg. 2019;35:e69–e72. doi: 10.1097/IOP.0000000000001352. [DOI] [PubMed] [Google Scholar]
- 5.Flanders M, Chaudhry Z, Mercer G. Traumatic rupture of the inferior rectus muscle: clinical presentation and surgical management. Can J Ophthalmol. 2022:S0008-4182(21)00421-X. doi: 10.1016/j.jcjo.2021.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Batra R, Gao A, Shun-Shin GA. The management of traumatic isolated inferior rectus rupture. Strabismus. 2012;20:105–8. doi: 10.3109/09273972.2012.680228. [DOI] [PubMed] [Google Scholar]
- 7.Zuo X, Gao L, Bao L, Chunyan L. Surgical repair of traumatic isolated inferior rectus muscle avulsion. Eur J Ophthalmol. 2019;29:106–9. doi: 10.1177/1120672118769780. [DOI] [PubMed] [Google Scholar]
- 8.Guardana GG. Satisfied result of modified Knapp procedure for a rare case of isolated superior rectus muscle rupture: a case report. Ophthalmol Ina. 2021;47:3–8. [Google Scholar]
- 9.Singh A, Pandey PK, Agrawal A, Rana KM, Mittal SK, Kumar B. Simultaneous superior rectus recession and anterior transposition of inferior oblique muscle as a surgical option for traumatically lost inferior rectus muscle. Strabismus. 2018;26:90–5. doi: 10.1080/09273972.2018.1444066. [DOI] [PubMed] [Google Scholar]
- 10.Beauchamp C, Mitchell PR. Inferior oblique muscle surgery. In: Duane TD, Tasman W, Jaeger EA, editors. Duane’s Clinical Ophthalmology. Revised ed. Philadelphia: Lippencott-Raven; 1995. chapter 87. [Google Scholar]
- 11.Batra R, Gao A, Shun-Shin GA. The management of traumatic isolated inferior rectus rupture. Strabismus. 2012;20:105–8. doi: 10.3109/09273972.2012.680228. [DOI] [PubMed] [Google Scholar]
- 12.Couser NL, Lenhart PD, Hutchinson AK. Augmented Hummelsheim procedure to treat complete abducens nerve palsy. J AAPOS. 2012;16:331–5. doi: 10.1016/j.jaapos.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]