Abstract
BACKGROUND:
The Critical Care Societies Collaborative included not ordering diagnostic tests at regular intervals as one of their Choosing Wisely initiatives. A reduction in unnecessary chest radiographs (CXRs) can help reduce exposure to radiation and eliminate health care waste. We aimed to reduce daily screening CXRs in a pediatric ICU (PICU) by 20% from baseline within 4 months of implementation of CXR criteria.
METHODS:
All intubated patients in the PICU were included in this quality improvement project. Patients with tracheostomies were excluded. We developed criteria delineating which patients were most likely to benefit from a daily screening CXR, and these criteria were discussed for each patient on rounds. Patients on extracorporeal membrane oxygenation, on high-frequency oscillatory ventilation, or on high support on conventional mechanical ventilation were included as needing a daily screening CXR. We tracked the percentage of intubated subjects receiving a screening CXR as an outcome measure. Unplanned extubations and the number of non-screening CXRs per intubated subject were followed as balancing measures.
RESULTS:
The percentage of intubated subjects receiving a daily screening CXR was reduced from 79% to 31%. There was no increase in frequency of unplanned extubations or number of non-screening CXRs. With an estimated subject charge of roughly $270 and hospital cost of $54 per CXR, this project led to an estimated $300,000 in patient charge savings and $60,000 in hospital cost savings.
CONCLUSIONS:
Adopting criteria to delineate which patients are most likely to benefit from screening CXRs can lead to a reduction in the percentage of intubated patients receiving screening CXRs without appearing to increase harm.
Keywords: chest radiographs, waste, unplanned extubations, quality, radiology, intubated, pediatric
Introduction
An increasing body of literature in critically ill adult patients indicates that reducing the number of daily chest radiographs (CXRs) does not equate to increased patient harm.1–4 Past studies in the pediatric ICU (PICU) have aimed to identify subject populations in which routine CXRs may be more beneficial than others.5,6 Obtaining screening CXRs has been justified to identify pathology or malpositioned devices that could not be identified otherwise and would lead to poor patient outcomes.5 They are not without cost, however, as unnecessary CXRs lead to additional health care expenditures and avoidable radiation exposure to patients.3,7–9
The Choosing Wisely campaign was created with the goal of promoting patient care that is supported by evidence and is truly necessary (https://www.choosingwisely.org. Accessed June 10, 2022). In 2014, the Critical Care Societies Collaborative identified routinely scheduled CXRs as one of their Choosing Wisely initiatives (https://www.choosingwisely.org/societies/critical-care-societies-collaborative-critical-care. Accessed June 10, 2022). In 2015, the Section of Perinatal Medicine of the American Academy of Pediatrics followed the same trend and added avoiding daily CXRs to their Choosing Wisely initiatives (https://www.choosingwisely.org/societies/american-academy-of-pediatrics-section-on-perinatal-pediatrics. Accessed June 10, 2022). The Section of Critical Care for the American Academy of Pediatrics does not have any Choosing Wisely initiatives. Additionally, there are no explicit guidelines to help determine how frequently screening CXRs should be obtained in the PICU and who should receive them.
Historically, nearly all of the intubated patients in our PICU received daily screening CXRs to evaluate for pathology and device location. Some of these screening CXRs likely did not have a meaningful impact on patient care and contributed to health care waste.10 The cardiovascular ICU at our institution had recently instituted a CXR reduction quality improvement project and demonstrated that CXRs could be safely reduced in that unit.10 We hypothesized that daily screening CXRs could be safely reduced in our PICU, but it was unclear to what degree given the more diverse reasons for patients to be intubated and on mechanical ventilation in the PICU. Our SMART aim was to reduce the number of daily screening CXRs for intubated patients in the PICU by 20% from baseline within 4 months of implementation of the CXR criteria.
QUICK LOOK.
Current knowledge
Our group had previously published data in the pediatric cardiovascular ICU that chest radiographs (CXRs) could be safely reduced without an increase in adverse events. It is unclear how this translates to a pediatric ICU (PICU) where respiratory indications for intubation are more diverse.
What this paper contributes to our knowledge
Daily screening CXRs were safely reduced for intubated patients in a PICU. This was achieved without increasing unplanned extubations, duration of mechanical ventilation, patient mortality, or ICU or hospital stay. This reduces costs and unnecessary radiation exposure.
Methods
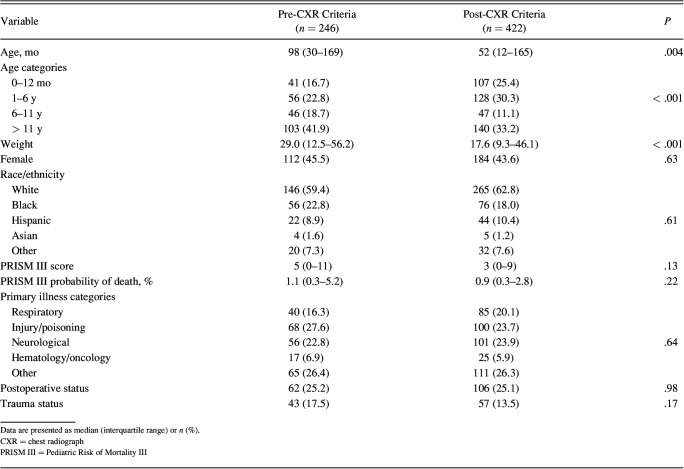
The Standards for Quality Improvement Reporting Excellence 2.0 guidelines for publishing quality improvement studies were followed in the preparation of this manuscript.11 The PICU at Riley Hospital for Children at Indiana University Health is an urban, quaternary, academic, 42-bed ICU. It is staffed by 18 intensivists, who care for approximately 2,500 admissions annually. The patients in the PICU are cared for during the day by 2 resident teams (4–5 residents and 1 pediatric critical care fellow per team) and 1 nurse practitioner team. There are 2 residents, a nurse practitioner, and an intensivist or critical care fellow present to care for the patients at night. This project did not meet the criteria for human subject study, and institutional review board approval was exempted. To achieve our SMART aim, we identified key drivers to target, including engaging radiology staff, standardizing respiratory status assessment and documentation, and standardizing CXR criteria (Fig. 1).
Fig. 1.
The key driver diagram for the reduction in daily screening chest radiograph project. PICU = pediatric ICU; CXR = chest radiograph; RT = respiratory therapist; RN = registered nurse.
Intervention one was to change the endotracheal tube (ETT) depth and securement assessment and documentation to every 4 h (April 2020). In an effort to improve patient monitoring and care, the respiratory therapy department changed their practice around the evaluation and documentation of device location and securement from every 12 h to every 4 h in April 2020. This intervention occurred 2 months before data collection. This was discussed with the critical care group during the planning stage to assuage fears that we would be missing device migration without screening CXRs. The ETTs at our facility are secured with tape if they are < 5.0 and secured with a Hollister ETT fastener (Hollister, Libertyville, Illinois) if ≥ 5.0.
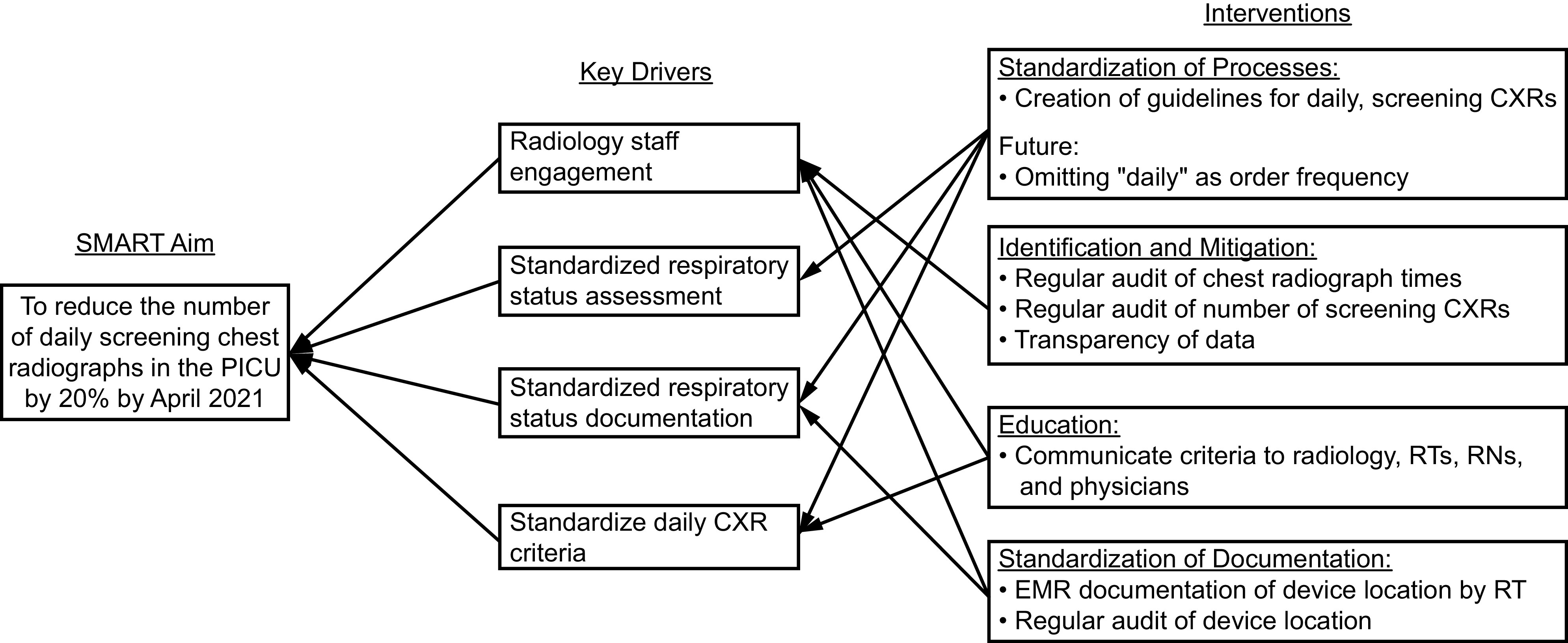
Intervention 2 was to develop criteria for which subjects were most likely to benefit from a daily screening CXR (September 2020–week 16). The criteria were created with the goal of identifying subjects who were most likely to benefit from a daily screening CXR (Table 1). The criteria were agreed upon by the pediatric critical care division in September 2020 and were shared with the pediatric surgeons and surgical subspecialties.
Table 1.
Daily Screening Chest Radiograph Criteria
Intervention 3 was to add the CXR criteria to the daily rounding checklist (January 2021–week 31). The CXR criteria were added to the daily rounding checklist in January 2021. The daily rounding checklist is used by the rounding teams to ensure we talk day to day patient care issues, such as central line utilization, lab frequency, etc. The delay from development of the criteria to the date it was added to the rounding checklist was due to the education required for the various stakeholders (nursing, respiratory therapy, critical care providers, etc).
Intervention 4 was a division update (March 2021–week 40). The pediatric critical care division was updated with the initial progress of the project in March of 2021. This was to provide reassurance through data transparency that unplanned extubations didn't increase as a result of having fewer CXRs. This helped alleviate some of the initial concerns the group had that fewer screening CXRs would result in ETT migration.
Data were collected retrospectively by chart review between June 2020–December 2020, whereas prospective data were collected between January 2021–October 2021. Unplanned extubations have been followed at our institution since June 2019 and were followed prospectively throughout this project. The primary outcome measure was the percentage of intubated subjects who received a daily screening CXR. Data were organized by weeks for ease of visualization. All intubated patients were included in this study. Patients with a tracheostomy were excluded as screening CXRs are infrequently obtained on these patients. Intubated subjects with continuous renal replacement catheters were included in the study, and a CXR was ordered or not based on the same criteria.
Process measures included adherence with the CXR criteria. Adherence was defined as the percentage of intubated subjects who correctly had a CXR ordered or not ordered based upon the CXR criteria. This was retrospectively evaluated from chart review, with a set goal of 80%. Similar CXR criteria were retrospectively applied to subjects in the PICU throughout the project.
Two balancing measures were followed throughout the project. The first was the rate of unplanned extubations, calculated as the number of unplanned extubations per 100 ventilator days. The rate of unplanned extubations is tracked regularly and reported to our division monthly. The second was the number of non-routine CXRs per intubated subject. Non-routine CXRs were defined as CXRs ordered at any time for a specific indication (ie, not for screening purposes). CXRs obtained for central venous line placement (including peripherally inserted central catheters), intubation, extracorporeal membrane oxygenation cannulation, and chest tube placement were excluded from counts as these CXRs would be obtained regardless of this project. PICU stay, hospital stay, duration of mechanical ventilation, extubation failure (defined as re-intubation within 48 h of first extubation attempt), severity of illness (Pediatric Risk of Mortality III [PRISM III]), and mortality were also evaluated as balancing measures.12
Statistical process control charts, p-charts, and u-charts were created using QI Macros (KnowWare International, Denver, Colorado). The percentage of intubated subjects who received a daily screening CXR and the percentage of non-routine screening CXRs per intubated subject were shown with p-charts. A run chart was used to show adherence with the CXR criteria. Data analyses were performed using Stata 17 (StataCorp, College Station, Texas). Clinical and demographic data were summarized and compared between groups. Non-normally distributed continuous variables were compared using Wilcoxon rank-sum, and categorical variables were compared using the chi-square test or Fisher exact as appropriate.
Results
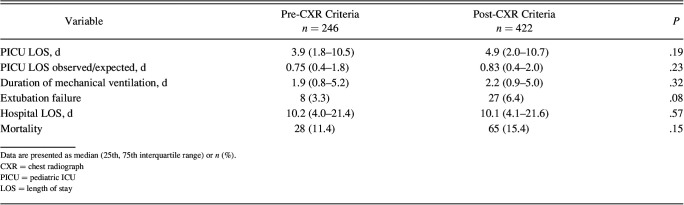
There were 246 subjects pre-CXR criteria implementation group and 422 subjects in the post-CXR criteria implementation group (Table 2). The post-CXR criteria group was younger, with a median age of 52 months (interquartile range 12–165) compared to 98 months (interquartile range of 30–169) in the pre-CXR criteria group (P = .004). The post-CXR criteria group also weighed less than the pre-CXR criteria group (P < .001). There was no statistically significant difference in severity of illness as measured by PRISM III score between the pre- and post-intervention 3 groups. There was no statistically significant difference in any of the other evaluated demographic data (Table 2).
Table 2.
Comparison of Demographic and Clinical Variables Between the Pre– and Post–Chest Radiograph Criteria Groups
During the pre-CXR criteria implementation period, intensivists would have been compliant with the criteria for 42% of the intubated subjects. Between development of the criteria (intervention 2) and implementation of the criteria (intervention 3), adherence improved to a median of 71%, which was below our 80% goal (Fig. 2).
Fig. 2.
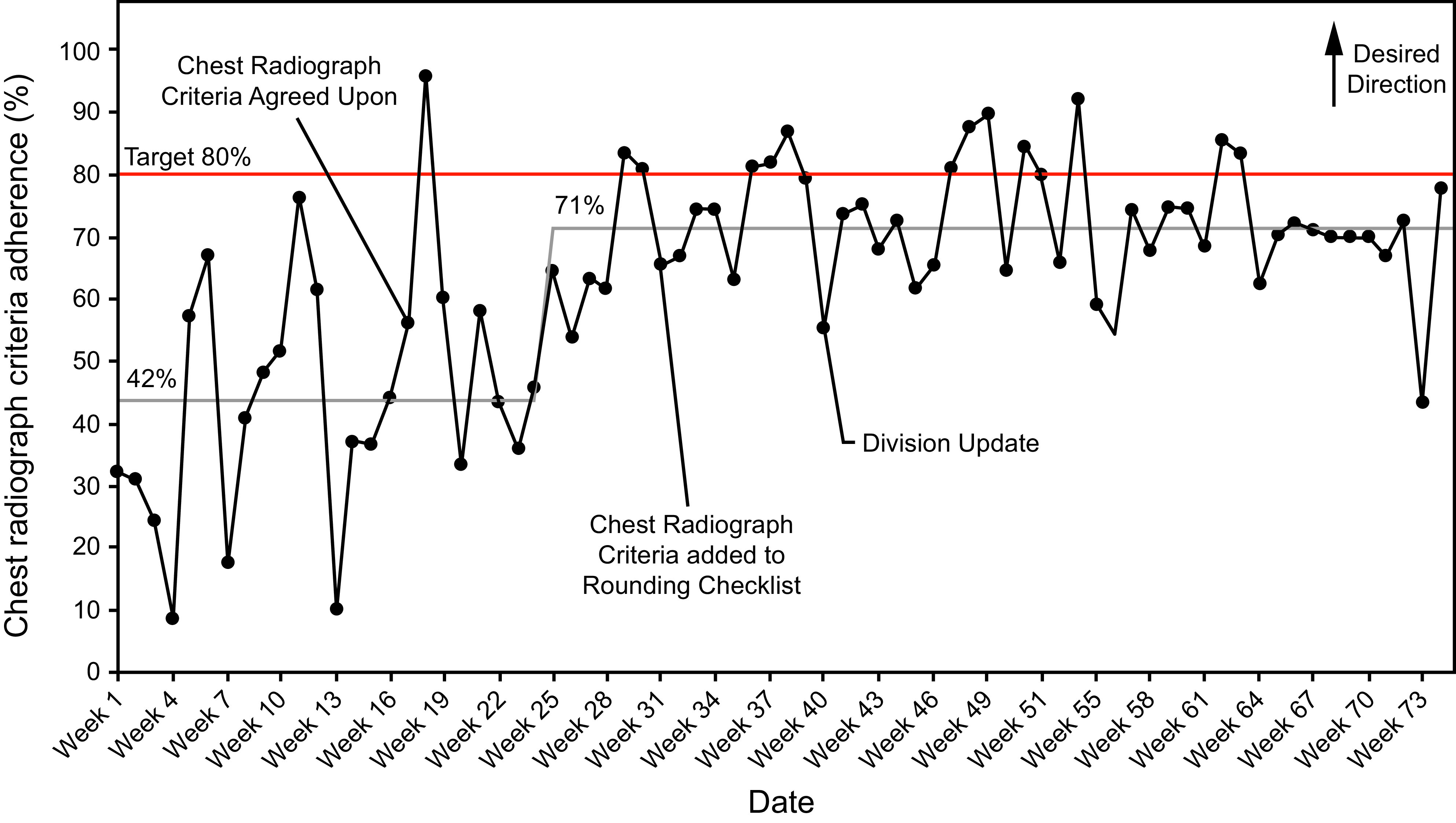
Adherence with the chest radiograph criteria.
Our baseline data showed that 79% of the ventilated subjects in the PICU received a daily screening CXR (Fig. 3). After the criteria were discussed and agreed upon (intervention 2), a shift to 69% was noted. The percentage of subjects receiving a daily screening CXR shifted to 51% after the CXR criteria were added to the daily rounding sheet for discussion for each subject (intervention 3). A further baseline shift to 31% was noted in March of 2021 when the critical care division was updated with regard to project progress and lack of an increase in balancing measures (intervention 4).
Fig. 3.

A p-chart showing the percentage of intubated subjects in the pediatric ICU who received a daily screening chest radiograph. LCL = lower control limit; CL = control limit; LCL = lower control limit.
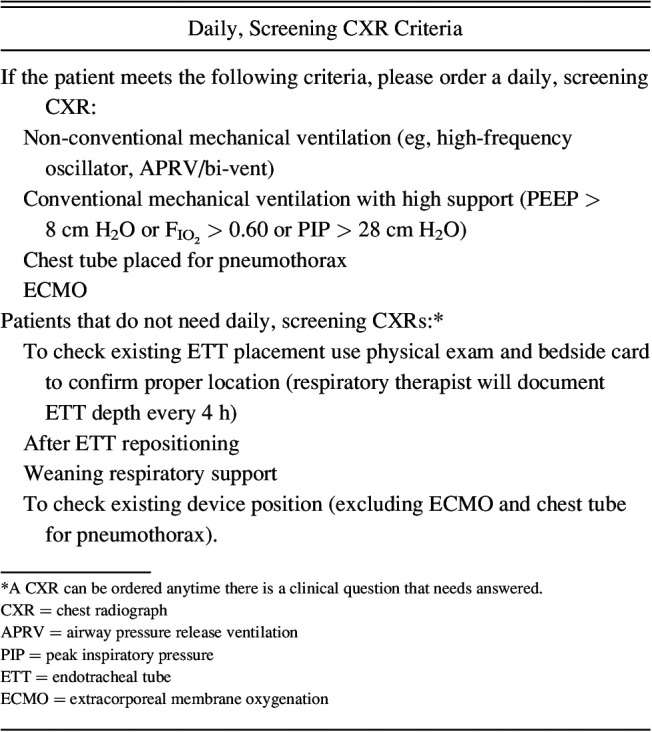
During the study period, there was no increase in the rate of unplanned extubations (Fig. 4). The percentage of non-screening CXRs per intubated subject did not change over the course of this study (Fig. 5). The PICU stay, PICU observed/expected stay, hospital stay, duration of mechanical ventilation, extubation failure, and mortality were similar between the 2 groups (Table 3).
Fig. 4.
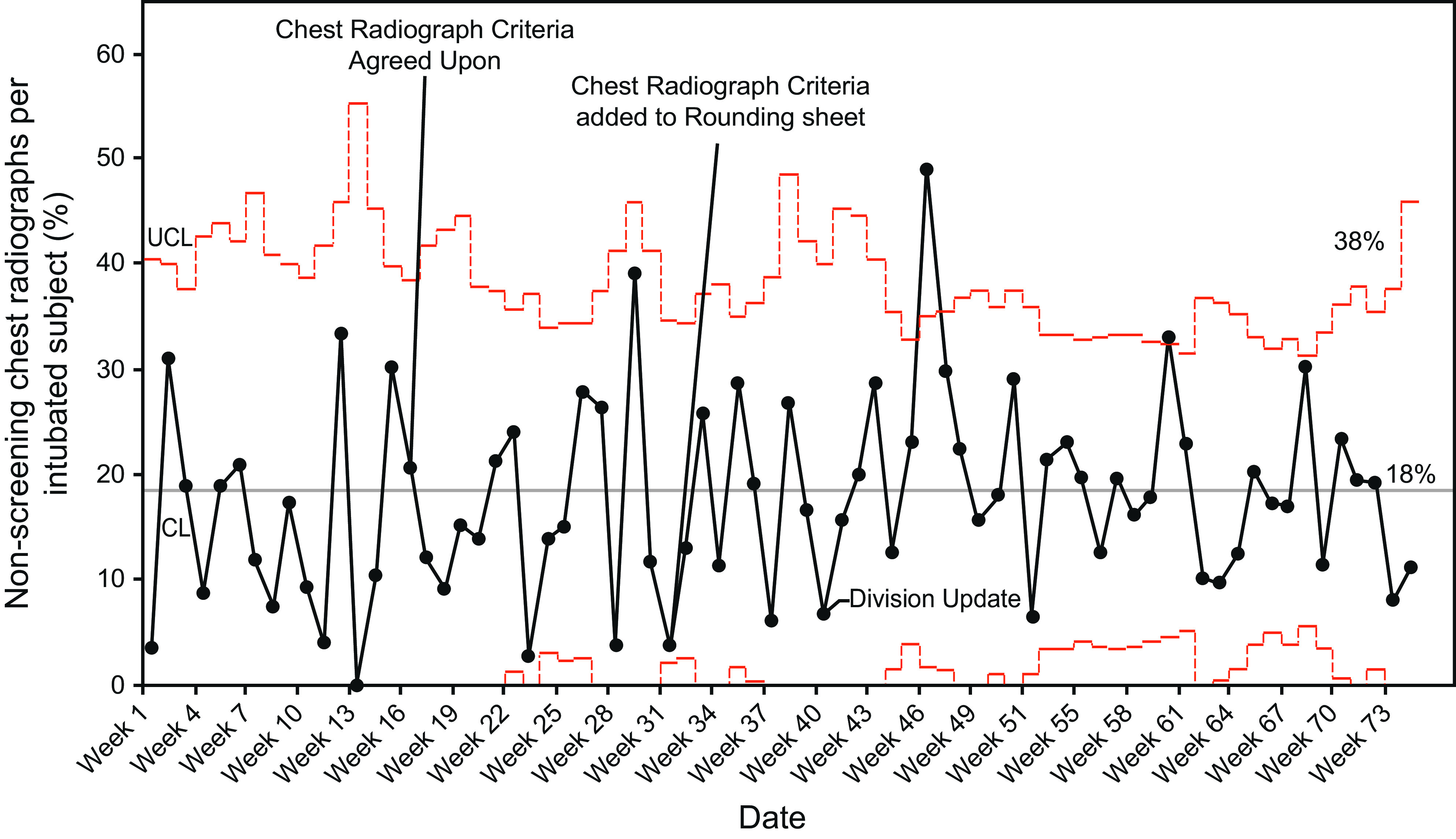
A p-chart showing the percentage of non-screening chest radiographs per intubated subject. UCL = upper control limit; CL = control limit.
Fig. 5.
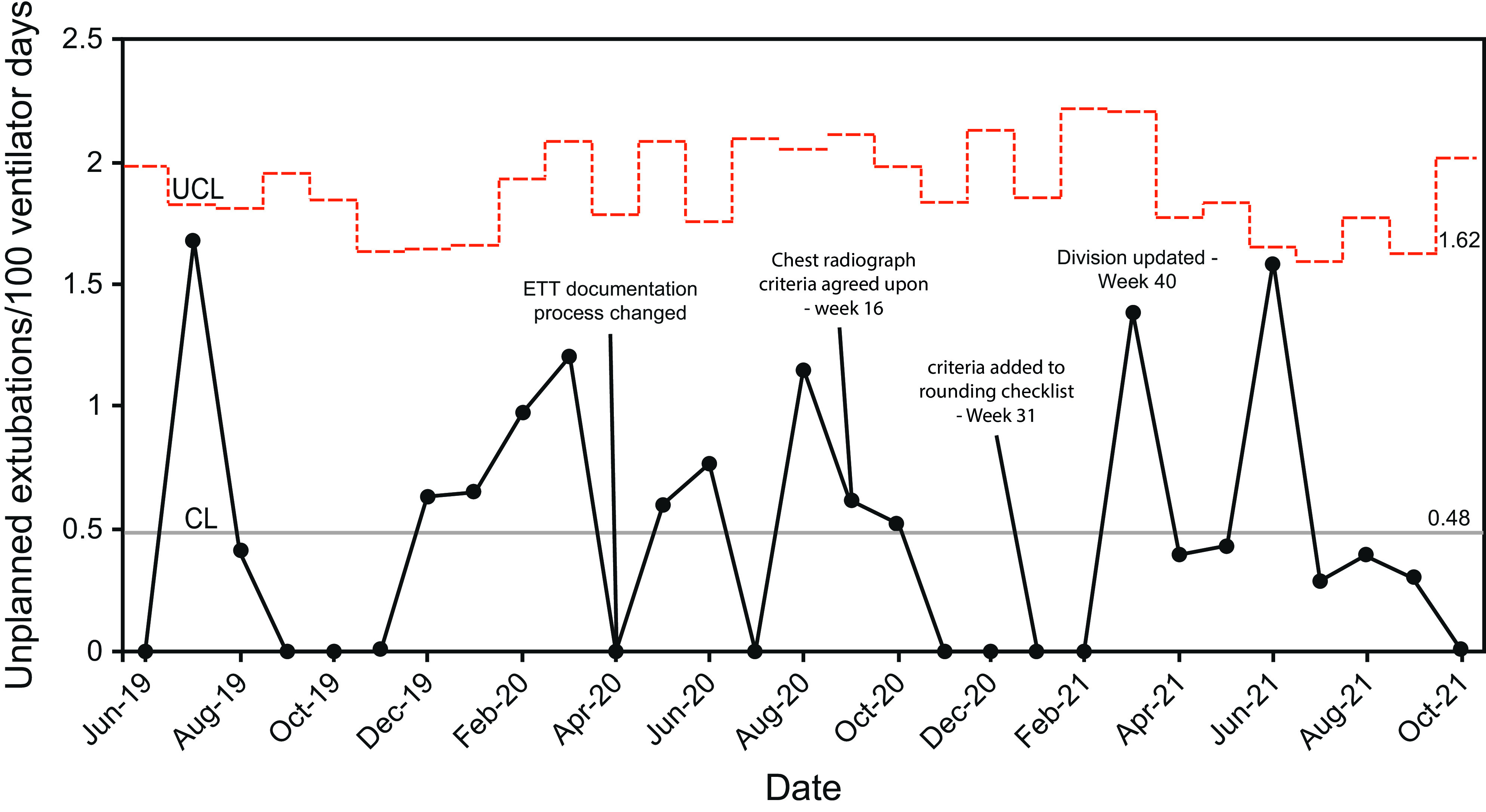
A u-chart showing the frequency of unplanned extubations per 100 ventilator days. UCL = upper control limit; ETT = endotracheal tube; CL = control limit.
Table 3.
Comparison of Clinical Outcomes Between the Pre– and Post–Chest Radiograph Criteria Groups
CXRs have an estimated patient charge of approximately $270 and hospital cost of $54 per CXR. This does not include the radiologist fee for interpretation. This project led to an estimated $300,000 in patient charge savings and $60,000 in hospital cost savings.
Discussion
Quality improvement methodology was used to reduce the percentage of intubated subjects in the PICU who received a daily screening CXR from 79% to 31%. This exceeded our SMART aim goal of 20%, and this reduction was able to be sustained over time without an increase in unplanned extubations, which was a major point of concern initially. Historically, our practice had been to order a daily, screening CXR for each intubated patient. This order was usually entered on admission or after intubation with a frequency of daily until the patient extubated, despite lack of a formal policy requiring this practice. Currently, individualized and daily assessment of the need for CXR has become our new practice. To ensure sustainability, we plan to continue to track screening CXR utilization over time.
Increasing amounts of literature support an on-demand approach to CXRs.6,13 The evidence for this is more robust in adults. There is concern that these data aren't applicable to pediatrics as tracheal length is shorter and tracheal diameter is smaller and consequently the risk of device malposition is higher.3,6 When the CXR criteria were first discussed among our division, there was concern that a lack of daily screening CXRs would increase the risk of malpositioned devices (for example, ETTs above the thoracic inlet that put patients at risk of unplanned extubations). The increased frequency of ETT depth assessment and documentation (intervention one) as well as data transparency and regular reporting of unplanned extubations assuaged some of this concern and allowed for agreement with the criteria. Intervention one occurred several months prior to the development of the criteria; however, we included it because we felt it allowed the criteria to be more restrictive and is important for reproducibility at other institutions.
Additionally, our institution has had success with other respiratory quality improvement projects, which facilitated buy-in from the stakeholders and success of implementing this project.14–16 Since having fewer screening CXRs did not result in an increase in CXRs obtained at other points throughout the day, we feel that the majority of the CXRs eliminated were a source of health care waste and unnecessary radiation exposure. Whereas an individual CXR may not contribute to a substantial amount to radiation exposure, the cumulative effect of repeated screening CXRs could contribute to increased exposure.8 The Section of Perinatal Medicine of the American Academy of Pediatrics lists reduced radiation exposure as a reason to eliminate CXRs without a clear indication in their Choosing Wisely initiative (https://www.choosingwisely.org/societies/american-academy-of-pediatrics-section-on-perinatal-pediatrics. Accessed June 10, 2022).
We chose to compare subject characteristics prior to and after the addition of the CXR criteria to the daily rounding sheet as this was the novel intervention for our institution and a novel intervention for PICUs. The post-CXR criteria group had younger subjects and fewer daily screening CXRs. Patients < 2 y of age are the group that providers are more concerned about not obtaining a daily screening CXR due to having a higher risk for unplanned extubations.17 The difference in age between the pre- and post-CXR criteria implementation groups is consistent with the change in seasonality of respiratory viruses reported throughout the world in response to the SARS-CoV2 pandemic.18–21 At our institution, we had a delayed outbreak in respiratory syncytial virus into the spring and summer months of 2021 that likely contributed to the age difference seen in Table 2.18 Despite that, our unplanned extubation rate was stable at 0.45/100 ventilator days, which is lower the national target rate of 1/100 ventilator days.22
One of the limitations of this study was that we were never able to achieve our goal of 80% adherence with the CXR criteria. Whereas some subjects who did not meet the criteria had a daily screening CXR ordered, there were also subjects who met criteria who did not have a daily screening CXR ordered. Even without achieving the adherence goal, we were able to reduce the percentage of intubated subjects receiving a daily screening CXR. Future plan-do-study-act (PDSA) cycles will aim to explore barriers for protocol adherence and solutions to improve adherence to achieve this goal. This may include modifying the current screening CXR criteria.
Another limitation is that this was a single-center quality improvement project. Differences in patient populations and clinical practice may limit the generalizability of this project. Whereas restricting daily screening CXRs has become standard practice at our institution, we plan to evaluate generalizability through a multi-center quality improvement project. Other institutions considering implementing a similar project should consider proactively evaluating the additional time required by the respiratory therapists (RTs) to increase the frequency of ETT assessment and documentation. We ask our RTs to be present during CXRs to protect the tube though, so the decrease in daily screening CXRs likely offset some of this.
Further outlining which patients would be most likely to benefit from a daily screening CXR can be the target of future PDSA cycles through a multi-center collaborative project. Daily, screening CXRs are often obtained early in the morning to ensure they are available for rounds. This likely awakens a patient when they would ideally be sleeping. A reduction in daily screening CXRs may reduce the incidence of delirium and decrease sedation/analgesia needs, but more research is needed to prove this hypothesis.
Conclusions
The percentage of intubated patients in a PICU receiving a daily screening CXR can be safely reduced through the development and implementation of criteria delineating which patients are most likely to benefit them. This elimination of waste can be achieved without having an increase in unplanned extubations, PICU and hospital stay, and duration of mechanical ventilation.
Footnotes
The authors have disclosed no conflicts of interest.
Dr Malin presented the abstract at the Pediatric Academic Societies Conference in April 2022.
REFERENCES
- 1. Amorosa JK, Bramwit MP, Mohammed TL, Reddy GP, Brown K, Dyer DS, et al. ACR appropriateness criteria routine chest radiographs in intensive care unit patients. J Am Coll Radiol 2013;10(3):170–174. [DOI] [PubMed] [Google Scholar]
- 2. Ganapathy A, Adhikari NK, Spiegelman J, Scales DC. Routine chest x-rays in intensive care units: a systematic review and meta-analysis. Crit Care 2012;16(2):R68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Resnick S, Inaba K, Karamanos E, Skiada D, Dollahite JA, Okoye O, et al. Clinical relevance of the routine daily chest x-ray in the surgical intensive care unit. Am J Surg 2017;214(1):19–23. [DOI] [PubMed] [Google Scholar]
- 4. Gershengorn HB, Wunsch H, Scales DC, Rubenfeld GD. Trends in use of daily chest radiographs among US adults receiving mechanical ventilation. JAMA Netw Open 2018;1(4):e181119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Quasney MW, Goodman DM, Billow M, Chiu H, Easterling L, Frankel L, et al. Routine chest radiographs in pediatric intensive care units. Pediatrics 2001;107(2):241–248. [DOI] [PubMed] [Google Scholar]
- 6. Drummond N, Laizner AM. Exploring the necessity of routine daily chest x-rays for mechanically ventilated patients in the pediatric intensive care unit: an integrative review. J Pediatr Nurs 2021;61:176–184. [DOI] [PubMed] [Google Scholar]
- 7. Kapileshwarkar YS, Smith LT, Szpunar SM, Anne P. Radiation exposure in pediatric intensive care unit patients: how much is too much? Clin Pediatr (Phila) 2018;57(12):1391–1397. [DOI] [PubMed] [Google Scholar]
- 8. Strawbridge H, Kurland G, Watson RS, Sheetz M, Wilkinson S, Weiner DJ. Radiation exposure from diagnostic imaging in the pediatric intensive care unit. Pediatr Crit Care Med 2012;13(4):e245–e248. [DOI] [PubMed] [Google Scholar]
- 9. Price MB, Grant MJ, Welkie K. Financial impact of elimination of routine chest radiographs in a pediatric intensive care unit. Crit Care Med 1999;27(8):1588–1593. [DOI] [PubMed] [Google Scholar]
- 10. Malin SW, Maue DK, Cater DT, Ealy AR, McCallister AE, Valentine KM, Abu-Sultaneh SM. A quality improvement initiative to reduce unneeded screening chest x-rays in a pediatric cardiovascular intensive care unit. Respir Care 2023;68(3):392–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. Am J Crit Care 2015;24(6):466–473. [DOI] [PubMed] [Google Scholar]
- 12. Kaur A, Kaur G, Dhir SK, Rai S, Sethi A, Brar A, Singh P. Pediatric Risk of Mortality III score - predictor of mortality and hospital stay in pediatric intensive care unit. J Emerg Trauma Shock 2020;13(2):146–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bafaqih H, Almohaimeed S, Thabet F, Alhejaili A, Alarabi R, Zolaly M, et al. Utility of daily routine portable chest x-ray in mechanically ventilated patients in the pediatric intensive care unit. J Pediatr Intensive Care 2014;3(1):29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rogerson CM, Tori AJ, Hole AJ, Summitt E, Allen JD, Abu-Sultaneh S, et al. Reducing unnecessary nitric oxide use: a hospital-wide, respiratory therapist-driven quality improvement project. Respir Care 2021;66(1):18–24. [DOI] [PubMed] [Google Scholar]
- 15. Abu-Sultaneh S, Hole AJ, Tori AJ, Benneyworth BD, Lutfi R, Mastropietro CW. An interprofessional quality improvement initiative to standardize pediatric extubation readiness assessment. Pediatr Crit Care Med 2017;18(10):e463–e471. [DOI] [PubMed] [Google Scholar]
- 16. Peterson RJ, Hassumani DO, Hole AJ, Slaven JE, Tori AJ, Abu-Sultaneh S. implementation of a high-flow nasal cannula management protocol in the pediatric ICU. Respir Care 2021;66(4):591–599. [DOI] [PubMed] [Google Scholar]
- 17. Lucas da Silva PS, de Carvalho WB. Unplanned extubation in pediatric critically ill patients: a systematic review and best practice recommendations. Pediatr Crit Care Med 2010;11(2):287–294. [DOI] [PubMed] [Google Scholar]
- 18. Agha R, Avner JR. Delayed seasonal RSV surge observed during the COVID-19 pandemic. Pediatrics 2021;148(3). [DOI] [PubMed] [Google Scholar]
- 19. Mameli C, Picca M, Buzzetti R, Pace ME, Badolato R, Cravidi C, et al. ; Italian Society of Paediatrics Lombardy Section. Incidence of acute respiratory infections in preschool children in an outpatient setting before and during COVID-19 pandemic in Lombardy Region, Italy. Ital J Pediatr 2022;48(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Diesner-Treiber SC, Voitl P, Voitl JJM, Langer K, Kuzio U, Riepl A, et al. Respiratory Infections in children during a COVID-19 pandemic winter. Front Pediatr 2021;9:740785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Taylor A, Whittaker E. The changing epidemiology of respiratory viruses in children during the COVID-19 pandemic: a canary in a COVID time. Pediatr Infect Dis J 2022;41(2):e46–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Klugman D, Melton K, Maynord PO, Dawson A, Madhavan G, Montgomery VL, et al. Assessment of an unplanned extubation bundle to reduce unplanned extubations in critically ill neonates, infants, and children. JAMA Pediatr 2020;174(6):e200268. [DOI] [PMC free article] [PubMed] [Google Scholar]