Abstract
BACKGROUND:
Aggressive behavior of psychiatric inpatients causes severe complications during treatment; nursing staff needs to understand the factors associated with aggression in inpatient units to prevent aggression.
AIM:
This study aimed to examine the level of aggression and its associated factors.
MATERIALS AND METHODS:
A descriptive observational design was conducted among aggressive patients. An aggressive behavior event was observed during the aggression episode. Data were collected from 55 patients with aggressive behavior using the Staff Observation Aggression Scale-Revised (SOAS-R) and Brief Psychiatric Rating Scale (BPRS). Patient-, staff-, and ward-related factors were assessed using a structured questionnaire.
RESULTS:
About 69% of patients had a severe level of aggressive behavior. There was a significant association between gender, the severity of symptoms, staff-to-patient ratio, ward milieu, and the number of caregivers with levels of aggression.
CONCLUSION:
The majority of the persons with mental illness exhibited severe aggression in a psychiatric setting. Being male, the presence of psychotic symptoms, ward milieu, staff-to-patient ratio, and availability of caregivers were significantly associated with aggression. This study adds to the existing literature by focusing on managing ward-related factors (avoiding noise and overcrowding) to prevent aggressive behavior among mentally ill patients.
Keywords: Aggression, incidence, mentally ill patients, patient factor, staff factor, ward factor
Introduction
Mental illness and violence are often seen in today's society as being inseparably connected, creating a harsh negative perception for patients and, at times, an uncomfortable environment for mental health professionals.[1] Physical aggression can be a major problem among patients admitted to acute psychiatric wards,[2] and aggressive behavior by psychiatric patients is a serious issue in clinical practice, and adequate management of such behavior is required with careful evaluation of the factors causing it.[3]
Violent patients are not a homogenous group, and their violence reflects various biological, psychodynamic, and social factors. Most researchers and clinicians agree that a combination of factors plays a role in violence and aggression, although there are differing opinions regarding the importance of individual factors.[4,5] The problem of violence and aggressive behavior among patients with psychiatric disorder has centralized the attention of researchers as aggression is a serious problem in psychiatric wards and has a major consequence for patients and also for staff working in mental healthcare settings as well.[6]
There is a general agreement among clinicians and researchers that aggression and violence in inpatient psychiatric units are associated with ward-related factors, which put healthcare workers at significant risk for injury.[5] Furthermore, a study conducted among nurses on patients’ aggression revealed that a higher number of nurses working in psychiatric settings had both poor self-rated health and reduced work ability due to patients’ ward-related aggressive events.[7] Therefore, nursing staff needs to understand the factors associated with aggression and violence in inpatient units.[6]
Several studies have shown that violent incidents occur relatively frequently in inpatient psychiatric units and are associated with specific socio-demographic and clinical variables such as young age, unmarried status, and unemployment stand out as more reliable predictors of aggressiveness.[5,6] Studies conducted to assess the aggression among psychiatric inpatients by the Staff Observation Aggression Scale-Revised (SOAS-R) had reported that patients with substance use, psychoses, and non-adherent to treatment were quite aggressive and people with younger age, ethnicity, and serious mental illnesses such as schizophrenia or bipolar disorders were two to three times as likely to be violent and assaultive compared with their counterparts.[8,9]
Aggression in an acute psychiatric care setting is generally explained as multifactorial including environmental factors such as ward design, privacy, doors, ambiance, noise, and stimulation; system-related factors such as hospital, ward, and regional policies, attitude toward patients and cultural factors; patient-related factors such as demographics, cognitive and emotional states, diagnosis, and pathology; and few clinically related factors such as the degree of communication, attitude toward aggression, and their stress level.[6]
Although there is a significant body of research on the subject of aggression and violence in inpatient psychiatric settings, the question of which factors are associated with an increased risk of assaulting others remains elusive. Knowing these factors at the ward level would assist in the interpretation of reported violence in particular wards.[2]
Earlier literature studies were majorly limited to only patient-related or demographic factors associated with reported aggression but were not concerned about the environmental (ward) and staff-related factors, which suggest the researchers undertake further research into this area to understand the missing literature with regard to the ward- and staff-related factors associated with psychiatric inpatients’ aggression.
The conceptual framework for this study was based on a tentative model of inpatient aggression developed by Nijman et al. (1999). This model attempts to account for inpatient aggression in terms of psychopathology, as well as situational factors relevant to a psychiatric ward. There are four main components in the tentative model of inpatient aggression model: psychopathology (patient variables), environmental stress (ward variables), communication stress (staff variables), and cognitive stress (patient variables).[10,11]
Patient, ward, and staff variables may interact to cause or exacerbate aggression in persons with mental illness. In the present study, this assumption is selected as a hypothesis to test the model. The conceptual model of this study is presented in [Figure 1].
Figure 1.
Tentative model of inpatient aggression (Nijman et al., 1999)
Although previous studies have focused on aggressive episodes and their characteristics, very few studies have been conducted on factors influencing aggressive behavior. There is a paucity of literature conducted in Indian psychiatric wards to assess the various factors such as patient factors, staff factors, and ward factors influencing aggressive behavior among mentally ill patients. Thus, the researcher felt the importance of understanding various factors causing aggressive behavior in persons with mental illness in the Indian context, to prevent and manage aggressive behavior in emergency wards of a psychiatric hospital.
Materials and Methods
Study design and setting
The descriptive observational study was conducted among aggressive patients. An aggressive behavior event was observed during the aggression episode. The study was conducted from December 2017 to June 2018. The study aimed to estimate the level of aggression and its association with various factors such as patient factors, staff factors, and ward factors. Permission was obtained from the Institutional Ethics Committee (IEC), Dharwad Institute of Mental Health & Neurosciences, Karnataka, to carry out the study with Registration No. DIMHANS/I.E.R.B/004/2016-17. Anonymity and confidentiality of information were maintained and informed about their freedom of choice. Informed consent was obtained from the caregivers. This study was prepared and reported as per the guidelines/checklist of Strengthening The Reporting of Observational Studies in Epidemiology (STROBE).
This study was conducted at an emergency psychiatry ward of a selected mental health care setting, in India. It is a state government mental healthcare setting with a 20-bed emergency psychiatry ward. In the emergency unit, the length of stay usually will be 7 to 10 days.
Study participants and sampling
During the six-month study period, 666 patients were admitted to the emergency unit. Of these, 55 patients who met inclusion criteria were purposively selected for the study. An aggressive behavior event was observed during the aggression episode. Inclusion criteria were persons with mental illness admitted to the emergency ward of a selected psychiatric hospital, who had at least one incidence of aggressive behavior during the present treatment period as recorded in the patient's file.
Procedure and data collection
The data were collected through direct structured participant observation with the event sampling method. All the aggressive incidents that occurred in the emergency ward during the period were assessed using SOAS-R. After the aggressive behavior subsided, the first investigator/author interacted with the patient and caregivers and collected information on socio-demographic details and the clinical profile of the patient using structured questionnaires. Patient-related information was collected using the Brief Psychiatric Rating Scale (BPRS) and case files, staff-related information was collected using a structured questionnaire by interview method from the staff nurses working in the ward during the incidence, and ward-related factors were assessed using a structured questionnaire by observing the ward environment.
Data collection tools and technique
Socio-demographic datasheet: The items included in the socio-demographic data sheet were divided into four parts of a structured questionnaire: Patients’ basic information, clinical characteristics, staff-related variables, and ward-related variables.
Patient factors: It includes patient's age, gender, education, occupation, family monthly income, religion, marital status, area of residence, age of onset of illness, duration of present illness, psychiatric diagnosis, number of previous hospitalizations, type of admission, history of substance use, history of attempted suicide, drug compliance, and BPRS score.
Staff factors: It includes age, gender, staff qualification, staff-to-patient ratio, number of years of experience in psychiatric wards, and number of staff nurses working in that ward during the incident.
Ward factors: It includes noise, crowd, time of the day of the incidence (morning: 8 am–2 pm, evening: 2 pm–8 pm, and night: 8 pm–8 am), location of incidence (bedside, nurse's station, corridor), and a number of caregivers present at the time of incidence.
BPRS[12]
The BPRS is a widely used instrument for assessing the positive, negative, and affective symptoms of individuals who have psychotic disorders, especially schizophrenia. The BPRS consists of 18 symptom constructs and takes 20–30 minutes for the interview and scoring. It is a 7-point Likert scale ranging from not present to extremely severe.
SOAS-R[13]
The SOAS-R is a tool for measuring the frequency and severity of aggressive acts of patients in psychiatric wards, which was developed by Nijman et al. (1999). It consists of five columns, and the score of the severity of incidents is calculated by adding the scores in each column. The theoretical range of total SOAS-R scores is from 0 to 22 points, with higher scores indicating greater incident severity, scores of 0–7 indicating mild aggression severity, scores of 8–15 indicating moderate severity, and scores of 16–22 indicating severe severity.
Psychometric properties
Validity: The content validity of the socio-demographic datasheet and appropriateness of the SOAS-R were established by obtaining suggestions and approval from experts.
Reliability: SOAS—This scale is widely used to document aggressive events and has adequate validity and reliability. Concurrent validity of the SOAS-R with staff estimates on Visual Analog Scale correlations ranged from r = 0.49 to 0.62, while the comparison to the Modified Overt Aggression Scale, the Violence Scale, and the Social Dysfunction and Aggression Scale ranged from 0.62 to 0.81. Inter-rater reliability is not available; however, for the original SOAS, the kappa value ranged from 0.61 to 0.74.[13]
Data analysis
Statistical Package for Social Sciences (SPSS) version 16.0 was used. The data were analyzed using descriptive statistics (frequency, percentage, mean, and standard deviation) and inferential statistics (Chi-square test).
Results
Of 666 admissions, the incidence of violence or aggression was noted among 55 patients from an emergency psychiatric setting who were study participants. A total of 55 incidences (one incidence per patient) were reported among the chosen population for 6 months and analyzed accordingly.
Level of aggression among participants
The largest proportion (n = 38, 69%) of participants had a severe level of aggressive behavior, while eighteen percent (n = 10) of them had a moderate level of aggressive behavior, and the remaining patients (n = 7, 13%) demonstrated a mild level of aggressive behavior. Furthermore, the mean severity score of aggression was 15.92 (SD 5.40) [Figure 2].
Figure 2.
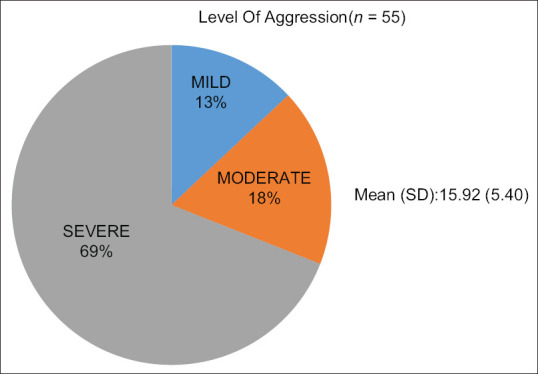
Level of aggression
Personal and clinical profile of participants
Nearly 82% (n = 45) of the patients belong to 18–40 years of age with a mean age of 32 (SD 10.01) years. There was a clear preponderance of males (60%) and Hindus (82%) among the study population. Nearly half of them were married (51%), and about 62% of them belong to a rural region. Only half of the participants were (51%) employed, and 43.64% had completed secondary education [Table 1].
Table 1.
Socio-demographics of the sample and their association with the level of aggression (n=55)
| Socio-demographic variables | Categories | n (%) | Level of aggression | X 2 | P | |
|---|---|---|---|---|---|---|
|
| ||||||
| Mild–moderate | Severe | |||||
| Age in years mean (SD) | 32 (10.01) | 2.0859 | 0.1487 | |||
| 18–40 | 45 (81.82) | 12 | 33 | |||
| 41–60 | 10 (18.18) | 5 | 5 | |||
| Gender | Male | 33 (60) | 6 | 27 | 6.2577 | 0.0124* |
| Female | 22 (40) | 11 | 11 | |||
| Marital status | Single | 21 (38.18) | 4 | 18 | 3.167 | 0.205 |
| Married | 28 (50.91) | 10 | 17 | |||
| Widowed/divorced | 6 (10.91) | 3 | 3 | |||
| Education | Illiterate | 15 (27.27) | 5 | 10 | 0.076 | 0.963 |
| Primary and secondary | 24 (43.64) | 7 | 17 | |||
| PUC and above | 16 (29.09) | 5 | 11 | |||
| Religion | Hindu | 45 (81.82) | 14 | 31 | 0.005 | 0.632 |
| Muslim | 10 (18.18) | 3 | 7 | |||
| Monthly income mean (SD) | 11972.73 (9253.84) | 2.554 | 0.095 | |||
| <=9000 | 24 (43.64) | 5 | 20 | |||
| >=9001 | 31 (56.36) | 12 | 18 | |||
| Occupation | Unemployed | 21 (38.18) | 9 | 12 | 4.160 | 0.125 |
| Student | 6 (10.91) | 0 | 6 | |||
| Employed | 28 (50.91) | 8 | 20 | |||
*P<0.05
The mean age of onset of illness was 27.47 (SD 9.68) years. The mean duration of the present illness was 121.85 (SD 417.18) days. The majority of the patients (n = 24, 44%) were suffering from schizophrenia and other psychotic disorder. Twenty-five (45%) of them had a history of substance use. Ten participants (18%) had a history of attempted suicide. More than half (n = 29, 53%) of them had poor drug compliance. Nearly 40% (n = 22) of the participants had the 1st episode of illness. Further, the mean BPRS score was 62.58 (SD 15.75) [Table 2].
Table 2.
Clinical profile of the sample and their association with the level of aggression (n=55)
| Clinical variables | Categories | n (%) | Level of aggression | X 2 | P | |
|---|---|---|---|---|---|---|
|
| ||||||
| Mild–moderate | Severe | |||||
| Diagnosis | Mood disorder | 20 (36.36) | 6 | 14 | 1.33 | 0.5142 |
| Schizophrenia and other psychotic disorders | 24 (43.64) | 9 | 15 | |||
| Substance use disorder | 11 (20.0) | 2 | 9 | |||
| History of substance use | Yes | 25 (45.45) | 5 | 20 | 2.55 | 0.6640 |
| No | 30 (54.55) | 12 | 18 | |||
| History of suicide attempts | Yes | 10 (18.18) | 2 | 8 | 0.68 | 0.1100 |
| No | 45 (81.82) | 15 | 30 | |||
| Drug compliance | Poor | 29 (52.73) | 9 | 20 | 0.81 | 0.4092 |
| Good | 4 (7.27) | 2 | 2 | |||
| 1st episode | 22 (40.0) | 6 | 16 | |||
| Mean BPRS score (SD) | 62.58 (15.75) | 51.18 (10.82) | 67.68 (15) | -4.0776# | 0.0002* | |
| Age of onset of illness mean (SD) 27.47 (9.68) | ||||||
| Duration of present illness mean (SD) 121.85 (417.18) | ||||||
*P<0.05, #-independent t-test
Nurses profile
The variables related to nurses who were working in the ward during the time of aggressive incidences were also evaluated. The mean age of nurses was 34.49 (SD 7.27) years. Most of the time (n = 32, 58%) female nurses were on duty. A majority (n = 39, 71%) of them were graduate nurses, and the mean number of years of experience in psychiatric wards was 4.09 (SD 3.35). During the incidences of aggressive behavior, for the majority of the time (n = 49, 89%) there was only one staff working in the ward. More than half of the incidences (51%) took place when there was a 1:5 staff-to-patient ratio [Table 3].
Table 3.
Nurses’ profile and their association with patients’ level of aggression (n=55)
| Nurses profile | Categories | n (%) | Level of aggression | X 2 | P | |
|---|---|---|---|---|---|---|
|
| ||||||
| Mild–moderate | Severe | |||||
| Age in years mean (SD): 34.49 (7.27) | ||||||
| Gender | Male | 23 (41.82) | 9 | 14 | 1.2512 | 0.2633 |
| Female | 32 (58.18) | 8 | 24 | |||
| No. of years of experience in psychiatric ward mean (SD): 4.09 (3.35) | ||||||
| 1–2 yrs | 2 | 8 | 1.5816 | 0.4535 | ||
| 3–5 yrs | 14 | 25 | ||||
| >=6 yrs | 1 | 5 | ||||
| Staff-to-patient ratio during the incidence | 1:5 | 28 (50.91) | 13 | 15 | 6.461 | 0.040* |
| 1:10 | 19 (34.55) | 3 | 16 | |||
| 1:20 | 8 (14.55) | 1 | 7 | |||
*P<0.05
Ward environment profile
It was found that with regard to the incidence of aggressive behavior, the majority of the incidences (n = 35, 64%) took place when the ward was noisy, and more than half of (n = 32, 58%) incidences occurred when the ward was overcrowded. Incidences were more frequently reported during the morning shift (n = 20, 36%) between 8 am and 2 pm and the evening shift (n = 19, 35%) between 2 pm and 8 pm and less often occurred at the night shift (n = 16, 29%) between 8 pm and 8 am. The largest proportion (n = 42, 76%) of incidences occurred at the bedside, while one (2%) incidence occurred at the nurses’ station and the remaining (n = 12, 22%) incidences occurred in the corridor. Almost 40 (73%) of incidences occurred when there was two or more caregiver present with the patient [Table 4].
Table 4.
Ward profile and their association with patients’ level of aggression (n=55)
| Ward profile | Categories | n (%) | Level of aggression | X 2 | P | |
|---|---|---|---|---|---|---|
|
| ||||||
| Mild–moderate | severe | |||||
| Noisy ward | No | 20 (36.36) | 2 | 18 | 6.434 | 0.015* |
| Yes | 35 (63.64) | 15 | 20 | |||
| Overcrowded | No | 23 (41.82) | 3 | 20 | 5.908 | 0.019* |
| Yes | 32 (58.18) | 14 | 18 | |||
| Time of incidence | Morning | 20 (36.36) | 6 | 14 | 0.5209 | 0.7707 |
| Evening | 19 (34.55) | 5 | 14 | |||
| Night | 16 (29.09) | 6 | 10 | |||
| Caregivers of specific patients’ availability during the incidence | One | 15 (27.27) | 8 | 7 | 4.856 | 0.047* |
| >=2 | 40 (72.73) | 9 | 31 | |||
*P<0.05
Association between the level of aggression and selected patient characteristics
The gender of the patient was significantly associated with severe aggression scores. The male gender had a higher aggression score compared with females (x2 = 6.25, P < 0.05) [Table 1]. Likewise, patients with higher BPRS scores and severe aggression scores are significantly associated (t = 4.0776, p < 0.05). This suggests that there is a link between psychopathology and the level of aggression [Table 2].
Association between the level of aggression and nurses and ward profile
There was a significant association found between staff-related variables such as the staff-to-patient ratio (x2 = 6.461) and the level of aggressive behavior. Furthermore, it was noted that there was a significant association of ward-related factors such as noisy ward (x2 = 6.434), overcrowded ward (x2 = 5.908), and a number of caregivers (x2 = 4.856) with the level of aggressive behavior among persons with mental illness at p < 0.05 [Tables 3 and 4].
Discussion
Inpatients’ violent and aggressive behavior in mental hospitals exists worldwide and is a severe and persistent clinical and nursing problem. The present study estimated the level of aggression and its correlates among persons with mental illness for a 6-month period.
The present study revealed that the total mean severity score of aggressive behavior is 15.92 (SD 5.40) with majority (69%) reported severe aggression, which was supported by the other study where results with a mean severity score was 10.12 (SD 4.84) of reported incidents, with a severity score ≥9, symbolizing more severe aggression.[9] However, caregivers of patients with mental illness from North India revealed that one-third of their patients (33%) demonstrated severe or extreme levels of aggressive behavior, while 53% had moderate aggression.[14]
The major proportion of patients (82%) in the present study belongs to young adults (18–40 years). Several researchers also proved that younger patients (those in their 20s and 30s) were more aggressive than older patients.[9,15] Another study revealed that severely agitated patients were younger compared with non-agitated patients.[16] In the present study, there was a significant association found between the male gender and aggressive behavior (x2 = 6.25, P < 0.05). Likewise, with regard to gender, males (N = 605) have exhibited more aggression than their counterparts[14] and male patients may feel bored easily, especially when they are not involved in indoor activities such as arts and crafts.[17] In the other study, it was reported that males were highly aggressive (33.6%) compared with their counterparts (23.9%).[18]
In the present study, 51% of the participants were married and employed, while others were single (38%) and widowed/divorced/separated (11%). About 38% of the patients were unemployed, and the remaining 11% were students. Other studies also showed regarding patient demographics that 65% were single, 11% were separated or divorced, and 24% were married. Almost two of five patients (41%) were unemployed, with 39% in full-time employment, 11% in full-time education, and 9% working at home.[19]
With regard to patient-related variables, the diagnoses/psychopathology of current study patients were schizophrenia and other psychotic disorder (44%), mood disorder (36%), and substance use disorder (20%). These findings were consistent with an Indian study, which reported that patients with schizophrenia committed 60.8% to 77.4% of assaults.[14] Another study reported that patients diagnosed with psychotic disorders such as schizophrenia,[20] bipolar disorders in combination with cannabis and other substance abuse,[21] and one systematic review stated, a psychotic disorder (or schizophrenia), a manic episode or bipolar disorder, and personality disorder were at increased risk of becoming aggressive in the psychiatric ward.[6]
With regard to staff-related variables, the results revealed that the staff-to-patient ratio during the incidence had a significant association with psychiatric inpatient aggression (p = 0.04). These findings were partially consistent with the study from Southeast Asia, which reviewed that staff-related factors such as educational level, work experience, unfamiliarity with the staff, rigid routines, and lack of training in assault control could contribute to aggression among psychiatric inpatients.[22,23] It is also suggested that violence in the ward may have a detrimental effect on not only patients but also on staff health and organization.[24]
With regard to ward-related variables, the incidences were reported more during the morning shift (36%) and evening shift (35%). The largest proportion (76%) of incidences occurred at the bedside and others (22%) in the corridor. Almost 40 (73%) incidences occurred when there were two or more caregivers present with the patient. These findings were consistent with other studies where it revealed all the incidences; most of them were reported during the day shift (54.3%) and 57% and 40% during the morning and night shifts, respectively,[25,26] and most of the incidences were reported in hallways (14%–67%), the activity room (13%–28%), bedside (8.5%–21.9%), dining room (7%– 17%), staff office (6.1–19%), and courtyard of the unit 3.3%.[6] Other studies found an association between hospital environments such as time of day and excessive stimuli with the level of aggression[22,23]
The current study revealed that noisy (p = 0.015) and crowded (p = 0.019) wards had a significant association with the level of aggression. A possible explanation for these findings is that in more crowded wards there are more patients and fewer staff available to handle the assault. In several studies of violent behavior in psychiatric wards, crowding is the only ward atmosphere-associated variable to receive attention.[17]
Conclusion
The study proved that aggression is a measurable construct in psychiatric inpatients, which requires psychiatric nurses to identify the predictors of aggressive behavior and should be able to apply a humanistic approach in dealing with aggression in persons with mental illness. The majority of the persons with mental illness exhibited severe aggression in an Indian psychiatric setting. Being male, the presence of psychotic symptoms, ward milieu (noisy ward, crowded ward), staff-to-patient ratio, and availability of caregivers were significantly associated with aggression. It suggests investigating phenomenological causes of aggression in persons with mental illness.
Ethical statement
Administrative and ethical approval was obtained from Institutional Ethics Committee (IEC), Dharwad Institute of Mental Health & Neurosciences, Karnataka (DIMHANS/I.E.R.B/004/2016-17). Informed consent was obtained from the caregivers. The purpose of carrying out the research project was explained and a participant information sheet was provided with detailed information regarding participation, and assurance of confidentiality was given to the participants. The study was carried out by the guidelines laid by the Indian Council of Medical Research (2017).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Varshney M, Mahapatra A, Krishnan V, Gupta R, Deb KS. Violence and mental illness: What is the true story? J Epidemiol Community Health. 2015;70:223–5. doi: 10.1136/jech-2015-205546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iozzino L, Ferrari C, Large M, Nielssen O, De Girolamo G. Prevalence and risk factors of violence by psychiatric acute inpatients: A systematic review and meta-analysis. PLoS One. 2015;10:e0128536. doi: 10.1371/journal.pone.0128536. doi: 10.1371/journal.pone.0128536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sato M, Noda T, Sugiyama N, Yoshihama F, Miyake M, Ito H. Characteristics of aggression among psychiatric inpatients by ward type in Japan: Using the Staff observation aggression scale – Revised (SOAS-R) Int J Ment Health Nurs. 2017;26:602–11. doi: 10.1111/inm.12228. [DOI] [PubMed] [Google Scholar]
- 4.Beaudoin M, Potvin S, Dellazizzo L, Luigi M, Giguère CE, Dumais A. Trajectories of dynamic risk factors as predictors of violence and criminality in patients discharged from mental health services: A longitudinal study using growth mixture modeling. Front Psychiatry. 2019;10:301. doi: 10.3389/fpsyt.2019.00301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caruso R, Antenora F, Riba M, Belvederi Murri M, Biancosino B, Zerbinati L, et al. Aggressive behavior and psychiatric inpatients: A narrative review of the literature with a focus on the European Experience. Curr Psychiatry Rep. 2021;23:29. doi: 10.1007/s11920-021-01233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weltens I, Bak M, Verhagen S, Vandenberk E, Domen P, van Amelsvoort T, et al. Aggression on the psychiatric ward: Prevalence and risk factors. A systematic review of the literature. PLoS One. 2021;16:e0258346. doi: 10.1371/journal.pone.0258346. doi: 10.1371/journal.pone.0258346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pekurinen V, Willman L, Virtanen M, Kivimäki M, Vahtera J, Välimäki M. Patient aggression and the wellbeing of nurses: A cross-sectional survey study in psychiatric and non-psychiatric settings. Int J Environ Res Public Health. 2017;14:1245. doi: 10.3390/ijerph14101245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Araya T, Ebnemelek E, Getachew R. Prevalence and associated factors of aggressive behavior among patients with schizophrenia at ayder comprehensive specialized hospital, Ethiopia. Biomed Res Int. 2020;2020:7571939. doi: 10.1155/2020/7571939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hansen NW, Reinhardt SM. 1385 – Characteristics of the aggressive in-patient in a forensic psychiatric hospital in denmark: Using the staff observation aggression scale – revised (SOAS-R) Eur Psychiatry. 2013;28:1. [Google Scholar]
- 10.Nijman HLI. A model of aggression in psychiatric hospitals. Acta Psychiatr Scand. 2002;106(SUPPL.S412):142–3. doi: 10.1034/j.1600-0447.106.s412.30.x. [DOI] [PubMed] [Google Scholar]
- 11.Nijman HLI, À Campo JMLG, Ravelli DP, Merckelbach HLGJ. A tentative model of aggression on inpatient psychiatric wards. Psychiatr Serv. 1999;50:832–4. doi: 10.1176/ps.50.6.832. [DOI] [PubMed] [Google Scholar]
- 12.Overall JE, Gorham DR. The Brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 13.Nijman HLI, Palmstierna T, Almvik R, Stolker JJ. Fifteen years of research with the staff observation aggression scale: A review. Acta Psychiatr Scand. 2005;111:12–21. doi: 10.1111/j.1600-0447.2004.00417.x. [DOI] [PubMed] [Google Scholar]
- 14.Varghese A, Khakha DC, Chadda RK. Pattern and type of aggressive behavior in patients with severe mental illness as perceived by the caregivers and the coping strategies used by them in a tertiary care hospital. Arch Psychiatr Nurs. 2016;30:62–9. doi: 10.1016/j.apnu.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Suchting R, Green CE, Glazier SM, Lane SD. A data science approach to predicting patient aggressive events in a psychiatric hospital. Psychiatry Res. 2018;268:217–22. doi: 10.1016/j.psychres.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 16.Sacchetti E, Valsecchi P, Tamussi E, Paulli L, Morigi R, Vita A. Psychomotor agitation in subjects hospitalized for an acute exacerbation of Schizophrenia. Psychiatry Res. 2018;270:357–64. doi: 10.1016/j.psychres.2018.09.058. [DOI] [PubMed] [Google Scholar]
- 17.Antonysamy A. How can we reduce violence and aggression in psychiatric inpatient units? BMJ Qual Improv Rep. 2013;2:u201366.w834. doi: 10.1136/bmjquality.u201366.w834. doi: 10.1136/bmjquality.u201366.w834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cho UJ, Lee JY, Kim HW, Lee JS, Joo YH, Kim SY, et al. Age structure at diagnosis affects aggression in a psychiatric inpatient population: Age structure affecting inpatient aggression. Psychiatry Res. 2014;220:1059–63. doi: 10.1016/j.psychres.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 19.Cohen DP, Akhtar MS, Siddiqui A, Shelley C, Larkin C, Kinsella A, et al. Aggressive incidents on a psychiatric intensive care unit. Psychiatr Bull. 2008;32:455–8. [Google Scholar]
- 20.Schaefer R, Broadbent M, Bruce M. Violent typologies among women inpatients with severe mental illness. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1615–22. doi: 10.1007/s00127-016-1280-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson JM, Wu CY, Winder GS, Casher MI, Marshall VD, Bostwick JR. The Effects of cannabis on inpatient agitation, aggression, and length of stay. J Dual Diagn. 2016;12:244–51. doi: 10.1080/15504263.2016.1245457. [DOI] [PubMed] [Google Scholar]
- 22.Papoulias C, Csipke E, Rose D, McKellar S, Wykes T. The psychiatric ward as a therapeutic space: Systematic review. Br J Psychiatry. 2014;205:171–6. doi: 10.1192/bjp.bp.114.144873. [DOI] [PubMed] [Google Scholar]
- 23.Ulrich RS, Bogren L, Gardiner SK, Lundin S. Psychiatric ward design can reduce aggressive behavior. J Environ Psychol. 2018;57:53–66. [Google Scholar]
- 24.Bhat S, Rentala S, Nanjegowda RB, Chellappan XB. Effectiveness of Milieu therapy in reducing conflicts and containment rates among schizophrenia patients? Invest Educ Enferm. 2020;38:e06. doi: 10.17533/udea.iee.v38n1e06. doi: 10.17533/udea.iee.v38n1e06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giarelli E, Nocera R, Jobes M, Boylan C, Lopez J, Knerr J. Exploration of aggression/violence among adult patients admitted for short-term, acute-care mental health services. Arch Psychiatr Nurs. 2018;32:215–23. doi: 10.1016/j.apnu.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Yang BX, Stone TE, Petrini MA, Morris DL. Incidence, type, related factors, and effect of workplace violence on mental health nurses: A cross-sectional survey. Arch Psychiatr Nurs. 2018;32:31–8. doi: 10.1016/j.apnu.2017.09.013. [DOI] [PubMed] [Google Scholar]



