Abstract
BACKGROUND:
Irritable bowel syndrome (IBS) is a functional bowel disorder that psychological interventions are effective on it. The present study aimed to compare the effect of internet-delivered short-term PMR (iPMR) and psychoeducation on mindful ability (MA), visceral hypersensitivity (VH), and symptoms of patients with IBS.
MATERIALS AND METHODS:
This randomized clinical trial was performed on individuals with IBS in 2020, recruiting a total of 60 patients fulfilling the inclusion criteria. Prior to the intervention, the Freiburg Questionnaire- Short Form (FMI-SF), the Visceral Sensitivity Questionnaire (VSI), and the Gastrointestinal Symptoms Rating Scale (GSRS) were filled out for the patients. Patients were divided into iPMR and psychoeducation groups randomly. All training in both groups was accomplished via WhatsApp social network. FMI-SF, VSI, and GSRS questionnaires for patients were completed 1 month (post-test) and 2 months later (follow-up). The data was analyzed by SPSS-23 software and one-way analysis of variance (ANOVA).
RESULTS:
Compared to the psychoeducation group, the MA of the iPMR group increased significantly in post-test and follow-up (43.06 ± 7.12 and 42.88 ± 6.28 vs 51.23 ± 11.7 and 56.74 ± 12.36 and P < 0.001) and their VH decreased significantly (37.85 ± 11.6 and 38.03 ± 11.8 vs 26.9 ± 6.45 and 22.46 ± 5.32 and P < 0.001). Also, their GSRS had significant decreases (43.27 ± 10.73 and 41.18 ± 9.31 vs 32.33 ± 8.21 and 25.79 ± 6.30 and P < 0.001).
CONCLUSION:
The findings showed iPMR in patients with IBS, in spite of a few sessions and internet-delivered approach, increased MA and decreased VH and gastrointestinal symptoms of them.
Keywords: Irritable bowel syndrome, muscle relaxation, visceral
Introduction
Irritable bowel syndrome (IBS) is a type of bowel dysfunction characterized by chronic abdominal pain, discomfort, bloating, and changes in bowel habits in the absence of an underlying structural or organic cause, which also happens to be well-known as a psychosomatic disorder associated with the gastrointestinal tract affecting bowel motility and producing cramps.[1] The prevalence of this disease in society is high and estimated to be 1.7-20%.[2]
Several underlying mechanisms have been assumed in the pathophysiology of IBS as a multifactorial disease. They included Inflammatory reactions, a history of childhood infections, gastrointestinal dysmotility, changes in gut microflora, food intolerance, genetic factors, psychological factors, and hypersensitivity in visceral perception.[3]
Visceral hypersensitivity (VH) is defined as an enhanced perception of mechanical triggers applied to the bowel which seems as pain and discomfort.[4] VH is known as decreased thresholds of stimuli perception generated from the gastrointestinal tract. The prevalence of VH in patients with IBS was reported between 33% to 90%.[4]
A variety of psychological interventions have been introduced in addition to pharmacological treatments to help resolve IBS symptoms. Progressive muscle relaxation (PMR) is a simple yet oldest form of relaxation technique that has been proven to be effective. PMR is an intervention that embodies the principles of psychoneuroimmunology to achieve physiological equilibrium in different systems of the body.[5] Uncontrollability and social-evaluation threat (e.g., judgment or evaluation) are the two main stressors that activate the sympathetic nervous system (SNS).[6] Therefore, having the ability to being nonjudgmental and tolerance of ambiguity (contrasting needs to control)-named mindful ability- can improve symptoms of diseases with SNS involvement such as IBS.
Mindfulness is the awareness that arises from paying attention on purpose, in the present moment, non-judgmentally.[7] Mindfulness practices help to bring focus to a specific “object of awareness” happening in the present moment. These “objects” can include various internal or external sensory experiences such as the breath, body sensations, thoughts, or sounds. A key element of mindfulness practices is noticing experiences with openness and curiosity, without trying to change or suppress them.[6] Some studies showed PMR focusing on internal senses especially the breath and body sensations can increase mindful ability (MA).[6,8]
Numerous studies portrayed relaxation techniques as effective for many illnesses and problems such as generalized anxiety disorder,[9] sleep disorders,[10] headache,[11] hypertension[12], and cardiovascular diseases.[13] Although various studies have shown the effectiveness of PMR and similar techniques such as mindfulness-based treatments (MBT) in reducing IBS symptoms,[14,15] the literature lacks studies that examine the benefits of short-term training. Especially given the current pandemic of COVID-19, social media and virtual platforms have gained more fame in terms of communication and access than ever before. So, this study aimed to compare the effect of internet-delivered and short-term PMR coincidently and psychoeducation on mindful ability, visceral hypersensitivity, and symptoms of patients with IBS.
Materials and Methods
Study design and setting
In this randomized clinical trial with 3 stages of pre-test, post-test and follow-up, participants were selected from the patients with IBS that were referred to Hakim Poursina Digestive Research Center in Isfahan for treatment.
Study participants and sampling
The participants were selected by a simple randomized sampling method. The study sample size obtained 60 patients according to the formula below:
N = (Z1-α/2 + Z1-β) 2* (σ1 2+ σ2 2)/d2
Counting the possible dropout of the sample, 80 patients were enrolled in the study. Inclusion criteria were as follows: age between 18-50 years, IBS diagnosis based on Rome III criteria, diagnosis by a gastroenterologist or internal medicine specialist, no known major psychiatric illness, Absence of substance-related disorders, literacy, failure to receive psychological treatment during the last six months, and consent to participation. Exclusion criteria included: reluctance to participate in the study at any time, manifestations of new symptoms such as gastrointestinal bleeding, bloody stools, fever, etc., during the study, not attending iPMR sessions and not doing homework, and those diagnosed with a psychiatric illness and requiring medications.
Data collection tool and technique
The two groups filled out the study questionnaire including demographic characteristics and history of GI disease, the Freiburg Short Form Mindfulness Questionnaire (FMI-SF), Visceral Sensitivity Inventory (VSI), and Gastrointestinal Symptoms Rating Scale (GSRS) in the pre-test, 1 month and 2 months later.
The FMI-SF was designed to measure mindfulness as a multidimensional construct. It initially consisted of 30 questions, which were later replaced with a shorter form with 14 items, more suitable for the general population. The 13 questions based on a 4-point Likert scale (rarely = 1 to almost always = 4) were filled out by the patients. The minimum score for this questionnaire is 14 and the maximum is 56, while a higher score indicates greater levels of mindfulness.[16]
The VSI comprising 15 questions, presents to be a great tool for assessing gastrointestinal anxiety in patients with irritable bowel syndrome. The validity of this tool based on the focus group method has been reported as appropriate and reliability was calculated as 0.93 with alpha Cronbach.[17]
The GSRS questionnaire is another useful tool to evaluate GI disorders based on symptoms and clinical relevance. This questionnaire is composed of 13 questions, each given a score of no discomfort (0) to severe discomfort (7) based on a 7-point Likert scale and measures 5 important domains related to digestion. These include heartburn, reflux, diarrhea, constipation, and indigestion. The final score is the sum of the scores from each subscale. A high score denotes the exacerbation of symptoms. In Our study Cronbach's alpha obtained 0.84 after assessing the reliability of this tool on 40 patients, indicating its appropriateness.
The iPMR group received short-term psychoeducation, which included a brief description of the disorder, and nutritional and psychological factors affecting it and taught PMR (based on 12 big muscles groups of Öst et al.,[18]. For this purpose, the patients received the audio file of this technique with the voice of the therapist, and for 4 weeks, the patients were being followed through WhatsApp in terms of implementation of the technique and to address other possible problems that would arise with the internet-delivered sessions.
The psychoeducation group received the file that only contained a description of the disorder, psychological factors, and nutrition affecting it without the relaxation technique. At the end of the program, all the topics presented to the iPMR group were given to this group for ethical purposes. Two groups received their medical drugs based on physician prescriptions.
For data analysis, Chi-square was used to evaluating of the differences of patients in demographic variables, and an independent t-test was used to compare the mean scores of patients in the questionnaires (FMI-SF, VSI, and GSRS) in psychoeducation and iPMR groups. Mean scores of patients in the questionnaires in 3 phases of the study (pre-test, post-test, and follow-up) in each group were compared using repeated measures analysis of variance (RM-ANOVA). All analyzes were performed using SPSS software version 24 and a value of 0.05 was considered statistically significant.
Ethical consideration
The research was conducted in accordance with the tents of the Declaration of Helsinki. The Ethics Committee of Isfahan University of Medical Sciences (IUMS) approved this study (IR.MUI.MED.REC.1399.575). The trial protocol was approved in the Iranian registry of clinical trials IRCT20180909040974N4; https://en.irct.ir/trial/51756).
Results
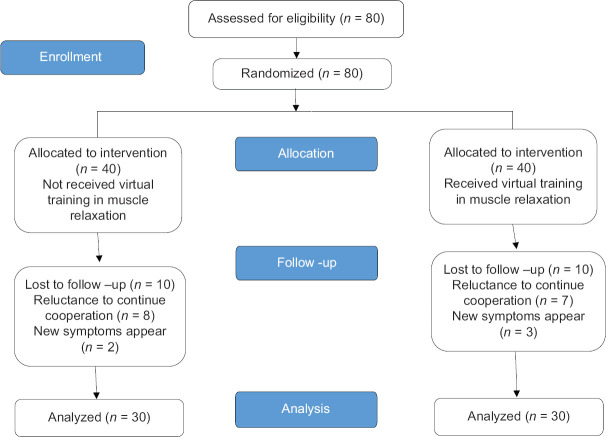
Initially, 80 patients were enrolled in the study and were randomly divided into two groups of 40 patients (psychoeducation and iPMR). Finally, after the interventions and during the follow-up, 20 of the participants were eliminated and the data from 60 patients were analyzed as depicted in Figure 1.
Figure 1.
CONSORT diagram
The results related to the demographic characteristics of the patients studied were displayed in Table 1.
Table 1.
Demographic characteristics of the subjects in psychoeducation and iPMR groups
| Variable | Psychoeducation Number (percentage) | iPMR Number (percentage) | P |
|---|---|---|---|
| Age (Mean±SD) | 32.61±4.52 | 33.56±4.83 | 0.91** |
| Gender | 0.35* | ||
| Male | 12 (40%) | 14 (46.7%) | |
| Female | 18 (60%) | 16 (53.3%) | |
| Occupation | 0.26* | ||
| Unoccupied | 2 (6.6%) | 0 | |
| Worker | 12 (40%) | 12 (40%) | |
| Private sector | 8 (26.7%) | 8 (26.7%) | |
| Employee | 8 (26.7%) | 10 (33.3%) | |
| Education status | 0.34 | ||
| High school | 4 (13.3%) | 6 (20%) | |
| Diploma and advanced-diploma | 6 (20%) | 4 (13.3%) | |
| Undergraduate | 12 (40%) | 8 (26.7%) | |
| Masters | 4 (13.3%) | 6 (20%) | |
| Doctorate | 4 (13.3%) | 6 (20%) |
*Chi-square test. **Independent t-test. The results with a significance level of 0.05% were evaluated
According to Table 1, no significant difference was observed in demographic variables of age, gender, occupation, and level of education between the psychoeducation and iPMR groups (P > 0.05).
Table 2 demonstrates the effect of short-term iPMR and psychoeducation on the mindfulness of patients in pre-test, post-test, and follow-up.
Table 2.
The effect of iPMR and psychoeducation on MA in the pre-test, post-test and follow-up
| Variables | Psychoeducation (Mean±SD) | iPMR (Mean±SD) | P** | |
|---|---|---|---|---|
| Mindful ability | Pre-test | 44.3±8.9 | 43.64±8.6 | 0.9 |
| Post-test | 43.06±7.12 | 51.23±11.7 | 0.001 | |
| follow-up | 42.88±6.28 | 56.74±12.36 | 0.001 | |
| P* | 0.7 | 0.001 | - | |
*RM-ANOVA. **Independent t-test. The results with a significance level of 0.05% were evaluated
According to Table 2, the mean scores of patients’ mindful ability in the iPMR group were significantly higher than psychoeducation group (P < 0.05).
Table 3 denotes the effect of short-term iPMR and psychoeducation on visceral hypersensitivity in 3 phases of the study. According to the and Table 3, patients in the iPMR group significantly had lower scores in VH (P < 0.05).
Table 3.
The effect of iPMR and psychoeducation on VH in the pre-test, post-test and follow-up
| Variables | Psychoeducation (Mean±SD) | iPMR (Mean±SD) | P** | |
|---|---|---|---|---|
| Visceral Sensitivity | Pre-test | 36.3±10.7 | 38.12±11.09 | 0.56 |
| Post-test | 37.85±11.6 | 26.9±6.45 | 0.001 | |
| follow-up | 38.03±11.8 | 22.46±5.32 | 0.001 | |
| P* | 0.67 | 0.001 | - | |
*RM-ANOVA. **Independent t-test. The results with a significance level of 0.05% were evaluated
Table 4 represents the effect of short-term iPMR and psychoeducation on gastrointestinal symptoms and their related domains including indigestion, abdominal pain, constipation, diarrhea, and the total score of the GSRS. According to Table 4, the rate of indigestion, abdominal pain, and diarrhea of patients in the iPMR group decreased significantly compared to the psychoeducation group (P < 0.05). Moreover, the overall mean score of the GSRS after iPMR decreased significantly (P < 0.05). However, no significant change in the rate of constipation in patients after iPMR was observed.
Table 4.
The effect of iPMR and psychoeducation on gastrointestinal symptoms in the pre-test, post-test and follow-up
| GI symptoms | Psychoeducation (Mean±SD) | iPMR (Mean±SD) | P** | |
|---|---|---|---|---|
| Indigestion/dyspepsia | Pre-test | 7.95±1.6 | 7.85±1.2 | 0.12 |
| Post-test | 7.83±0.9 | 5.54±0.62 | 0.001 | |
| Follow-up | 7.72±0.7 | 4.24±0.42 | 0.001 | |
| P* | 0.23 | 0.001 | - | |
| Abdominal pain | Pre-test | 17.5±3.6 | 18.03±4.72 | 0.37 |
| Post-test | 16.64±2.37 | 9.14±1.57 | 0.001 | |
| Follow-up | 15.67±2.12 | 6.44±1.03 | 0.001 | |
| P* | 0.33 | 0.001 | - | |
| Constipation | Pre-test | 9.5±2.67 | 8.36±4.71 | 0.08 |
| Post-test | 8.42±2.23 | 6.37±1.6 | 0.06 | |
| Follow-up | 8.10±2.18 | 6.19±1.1 | 0.06 | |
| P* | 0.36 | 0.07 | - | |
| Diarrhea | Pre-test | 13.5±2.36 | 12.75±2.45 | 0.67 |
| Post-test | 11.30±1.51 | 6.91±0.88 | 0.001 | |
| Follow-up | 10.18±1.22 | 4.32±0.48 | 0.001 | |
| P* | 0.06 | 0.001 | - | |
| Total score of GSRS | Pre-test | 45.71±11.09 | 48.6±12.95 | 0.26 |
| Post-test | 43.27±10.73 | 32.33±8.21 | 0.001 | |
| Follow-up | 41.18±9.31 | 25.79±6.30 | 0.001 | |
| P* | 0.07 | 0.001 | - | |
*RM-ANOVA. **Independent t-test. The results with a significance level of 0.05% were evaluated
Discussion
The current study compared the effect of short-term iPMR and psychoeducation on MA, VH, and symptoms of patients with IBS. The findings revealed that iPMR followed by psychoeducation significantly raised the level of MA in patients with IBS compared to those who received psychoeducation only. This finding is consistent with other research.[8,19] Although a few researches have shown similarities between PMR and MBT,[6,8] the issue remains controversial among researchers. This finding of our study shows the similarity of the two therapies because PMR has been able to increase the MA that is claimed to be specific to MBT. PMR through mechanisms related to MBT works in people with IBS. The two mechanisms are recognizing the dysfunctional triggers/irrational fear of the disease and changes in self-awareness.[19] On the other hand, in our study, FMI measures MA includes two fundamental facets: (a) focus on the present moment including bodily awareness, and (b) nonreactivity to the inner experience, thus an accepting attitude.[16] So, it can be said PMR through enhancing these facets has increased MA.
Furthermore, PMR similar to MBT improves quality of life by diminishing IBS symptoms. The sole purpose of the MBT is to achieve a state of alert, focused relaxation by deliberately paying attention to thoughts and emotions and understanding them as transient with a non-judgmental approach in an attempt to avoid rumination (repetitive negative thoughts), thereby preventing mental catastrophe, stress and other dysfunctional coping mechanisms. Overall, this makes IBS more tolerable.[20]
Our study also noted that the VH in iPMR was reported significantly lower compared to the psychoeducation group. Although a systematic review on psychotherapy for IBS published by Cochrane Research Centre has claimed PMR evaluated only two outcomes, including IBS symptom relief and quality of life,[21] but our study showed the efficacy of PMR in the underling mechanisms of IBS such as VH and MA in patients with IBS. This finding is consistent with other studies especially examining the effect of psychological therapies similar to PMR on VH.[22,23] One of them[23] was a recent meta-analysis that evaluated 6 studies about the effect of mindfulness on IBS.
The neurological mechanism of VH in patients with IBS has been described in this way that they show altered responses in both the emotional arousal circuits (including the anterior cingulate cortex and the amygdala) and the cortex-modulating circuit (which includes the internal and external prefrontal cortex), which may be responsible for the arousal and cognitive aspects of VH.[24] PMR could help the acceptance of internal experiences[25,26] such as VH and improve them as well as bowel dysfunction through sending signals to the limbic system. This system inhibits the within-brain axes, including the hypothalamic-pituitary-adrenal axis which is responsible for the production of stress hormones[27,28] that has an important role in VH and overall the symptoms of IBS.
Another finding of the present study was that the rate of IBS symptoms including indigestion, abdominal pain, and diarrhea of patients diminished significantly in the iPMR group. Our results demonstrated that the overall mean score of the GSRS in the PMR group decreased significantly. This finding is consistent with other studies that showed the effect of PMR on IBS symptoms such as indigestion, diarrhea, constipation, and abdominal pain.[15,22]
It seems all dependent variables in the present study are related together. Because an effecting factor on VH and the symptoms of IBS is pain catastrophizing (PC). A study showed PC directly predicted VH and VH predicted IBS symptoms.[29] Having an accepting and non-judgmental view of the pain (or mindfulness of pain) could decrease exaggerated negative “mental set” toward pain and its consequences (that is named PC). It has been shown that PC has a negative relationship with MA and MBT could diminish PC.[30] Since PMR like MBT could increase MA, it could decrease VH and the symptoms of IBS. So, it can be concluded the underlying mechanism for the effect of PMR on IBS is MA.
Although a study declared that psychoeducation had healing effects in the long-term,[20] but in line with previous studies that stated short-term training had favorable effects,[24,31] our study also found that short-term PMR (4 sessions) did improve IBS symptoms.
The strength of the present study is using of short-term and internet-delivered PMR which leads to high accessibility and ease of application for a common clinical sample.
Limitation and recommendation
The limitation of this study were no comparison with a gold standard treatment such as Cognitive Behavior Therapy. Another limitation was the selection of participants from one treatment center. It is recommended that PMR compare with other treatments. Also, a study comparing this treatment in two short-term and long-term forms is recommended. In addition, other studies are recommended by selecting a sample group from multiple centers.
Conclusion
Our study showed it is reasonable and cost-effective to use short-term and internet-delivered PMR to improve symptoms of IBS in conjunction with medications. So, it should be considered as one of the interventions that should be considered by doctors, other health staff, and treatment centers involved in the treatment of IBS patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This research has been carried out of a general physician dissertation that was approved by Isfahan University of Medical Sciences (Code No: 399490).
References
- 1.Ng QX, Soh AYS, Loke W, Venkatanarayanan N, Lim DY, Yeo W-S. A meta-analysis of the clinical use of curcumin for irritable bowel syndrome (IBS) J Clin Med. 2018;7:298. doi: 10.3390/jcm7100298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: A systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:908–17. doi: 10.1016/S2468-1253(20)30217-X. [DOI] [PubMed] [Google Scholar]
- 3.Ludidi S, Mujagic Z, Jonkers D, Keszthelyi D, Hesselink M, Kruimel J, et al. Markers for visceral hypersensitivity in patients with irritable bowel syndrome. Neurogastroenterol Motil. 2014;26:1104–11. doi: 10.1111/nmo.12365. [DOI] [PubMed] [Google Scholar]
- 4.Deiteren A, de Wit A, van der Linden L, De Man JG, Pelckmans PA, De Winter BY. Irritable bowel syndrome and visceral hypersensitivity: Risk factors and pathophysiological mechanisms. Acta Gastro-enterologica Belgica. 2016;79:29–38. [PubMed] [Google Scholar]
- 5.Ford AC, Lacy BE, Harris LA, Quigley EM, Moayyedi P. Effect of antidepressants and psychological therapies in irritable bowel syndrome: An updated systematic review and meta-analysis. Am J Gastroenterol. 2019;114:21–39. doi: 10.1038/s41395-018-0222-5. [DOI] [PubMed] [Google Scholar]
- 6.Luberto CM, Hall DL, Park ER, Haramati A, Cotton S. A perspective on the similarities and differences between mindfulness and relaxation. Glob Adv Health Med. 2020;9:2164956120905597. doi: 10.1177/2164956120905597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quaglia JT, Braun SE, Freeman SP, McDaniel MA, Brown KW. Meta-analytic evidence for effects of mindfulness training on dimensions of self-reported dispositional mindfulness. Psychol Assess. 2016;28:803–18. doi: 10.1037/pas0000268. [DOI] [PubMed] [Google Scholar]
- 8.Mander J, Blanck P, Neubauer AB, Kröger P, Flückiger C, Lutz W, et al. Mindfulness and progressive muscle relaxation as standardized session-introduction in individual therapy: A randomized controlled trial. J Clin Psychol. 2019;75:21–45. doi: 10.1002/jclp.22695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zargar F, Farid AAA, Atef-Vahid M-K, Maroof M, Afshar H, Omranifard V. Effect of acceptance-based behavior therapy on severity of symptoms, worry and quality of life in women with generalized anxiety disorder. Iran J Psychiatry Behav Sci. 2012;6:23–32. [PMC free article] [PubMed] [Google Scholar]
- 10.Bacaro V, Benz F, Pappaccogli A, De Bartolo P, Johann AF, Palagini L, et al. Interventions for sleep problems during pregnancy: A systematic review. Sleep Med Rev. 2020;50:101234. doi: 10.1016/j.smrv.2019.101234. [DOI] [PubMed] [Google Scholar]
- 11.Minen MT, Adhikari S, Padikkala J, Tasneem S, Bagheri A, Goldberg E, et al. Smartphone-delivered progressive muscle relaxation for the treatment of migraine in primary care: A randomized controlled trial. Headache. 2020;60:2232–46. doi: 10.1111/head.14010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ermayani M, Prabawati D, Susilo WH. The effect of progressive muscle relaxation on anxiety and blood pressure among hypertension patients in east Kalimantan, Indonesia. Enferm Clí. 2020;30:121–5. [Google Scholar]
- 13.Cahyati A, Herliana L, Februanti S, editors Progressive muscle relaxation (PMR) enhances oxygen saturation in patients of coronary heart disease. Journal of Physics: Conference Series. 2020:IOP Publishing. [Google Scholar]
- 14.Potter GK, Hunter PV, Morrison TG. Dispositional mindfulness in irritable bowel syndrome: The mediating role of symptom interference and self-compassion. Mindfulness. 2020;11:462–71. [Google Scholar]
- 15.Naliboff BD, Smith SR, Serpa JG, Laird KT, Stains J, Connolly LS, et al. Mindfulness-based stress reduction improves irritable bowel syndrome (IBS) symptoms via specific aspects of mindfulness. Neurogastroenterol Motil. 2020;32:e13828. doi: 10.1111/nmo.13828. [DOI] [PubMed] [Google Scholar]
- 16.Karatepe HT, Yavuz KF. Reliability, validity, and factorial structure of the Turkish version of the Freiburg Mindfulness Inventory (Turkish FMI) Psychiatry Clin Psychopharmacol. 2019;29:472–8. [Google Scholar]
- 17.Brown TA, Reilly EE, Murray HB, Perry TR, Kaye WH, Wierenga CE. Validating the visceral sensitivity index in an eating disorder sample. Int J Eat Disord. 2021;54:986–94. doi: 10.1002/eat.23471. [DOI] [PubMed] [Google Scholar]
- 18.Öst L-G. Applied relaxation: Description of a coping technique and review of controlled studies. Behav Res Ther. 1987;25:397–409. doi: 10.1016/0005-7967(87)90017-9. [DOI] [PubMed] [Google Scholar]
- 19.Park S-H, Han KS, Kang C-B. Relaxation therapy for irritable bowel syndrome: A systematic review. Asian Nurs Res. 2014;8:182–92. [Google Scholar]
- 20.Ljótsson B, Hedman E, Lindfors P, Hursti T, Lindefors N, Andersson G, et al. Long-term follow-up of internet-delivered exposure and mindfulness based treatment for irritable bowel syndrome. Behav Res Ther. 2011;49:58–61. doi: 10.1016/j.brat.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Zijdenbos IL, de Wit NJ, van der Heijden GJ, Rubin G, Quartero AO. Psychological treatments for the management of irritable bowel syndrome. Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD006442.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Garland EL, Gaylord SA, Palsson O, Faurot K, Mann JD, Whitehead WE. Therapeutic mechanisms of a mindfulness-based treatment for IBS: Effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. J Behav Med. 2012;35:591–602. doi: 10.1007/s10865-011-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baboş C-I, Leucuţa D-C, Dumitraşcu DL. Meditation and irritable bowel syndrome, a systematic review and meta-analysis. J Clin Med. 2022;11:6516. doi: 10.3390/jcm11216516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolitzky-Taylor K, Craske MG, Labus JS, Mayer EA, Naliboff BD. Visceral sensitivity as a mediator of outcome in the treatment of irritable bowel syndrome. Behav Res Ther. 2012;50:647–50. doi: 10.1016/j.brat.2012.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zargar F, Farid AA, Atef-Vahid MK, Afshar H, Omidi A. Comparing the effectiveness of acceptance-based behavior therapy and applied relaxation on acceptance of internal experiences, engagement in valued actions and quality of life in generalized anxiety disorder. J Res Med Sci. 2013;18:118–22. [PMC free article] [PubMed] [Google Scholar]
- 26.Mohammadi MM, Parandin S. Effect of the combination of Benson's relaxation technique and brief psychoeducational intervention on multidimensional pain and negative psychological symptoms of pregnant women: A randomized controlled trial. J Educ Health Promot. 2019;8:91. doi: 10.4103/jehp.jehp_286_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ismail AA, Saad A, Abd-Elrahman NF, Elfahl AA. Effect of Benson's relaxation therapy alone or combined with aerobic exercise on cortisol, sleeping quality, estrogen, and severity of dyspeptic symptoms in perimenopausal women with functional dyspepsia. Eur Rev Med Pharmacol Sci. 2022;26:8342–50. doi: 10.26355/eurrev_202211_30367. [DOI] [PubMed] [Google Scholar]
- 28.Soheili M, Nazari F, Shaygannejad V, Valiani M. A comparison the effects of reflexology and relaxation on the psychological symptoms in women with multiple sclerosis. J Educ Health Promot. 2017;6:11. doi: 10.4103/jehp.jehp_166_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cassar G, Knowles S, Youssef GJ, Moulding R, Uiterwijk D, Waters L, et al. Examining the mediational role of psychological flexibility, pain catastrophizing, and visceral sensitivity in the relationship between psychological distress, irritable bowel symptom frequency, and quality of life. Psychol Health Med. 2018;23:1168–81. doi: 10.1080/13548506.2018.1476722. [DOI] [PubMed] [Google Scholar]
- 30.Erfan A, Aghaei A, Golparvar M. Comparison of the effect of mindfulness based cognitive therapy and Iranian-Islamic positive therapy on pain catastrophizing and severity symptoms in women with irritable bowel syndrome. Daneshvar Med. 2021;29:42–56. [Google Scholar]
- 31.Recabarren RE, Gaillard C, Guillod M, Martin-Soelch C. Short-term effects of a multidimensional stress prevention program on quality of life, well-being and psychological resources. A randomized controlled trial. Front Psychiatry. 2019;10:88. doi: 10.3389/fpsyt.2019.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]