Abstract
Micropigmentation and microblading is a popular technique now a days which is used as a semi permanent method for camoflaging various dermatological indications. This article will elaborate upon various indications of micropigmenation. Micropigmentation is used in variety of dermatological conditions like semi permanent make up and vitiligo (stable forms). In this technique, a thorough knowledge of the indication and colour theory is crucial to achieve near to natural output. Micropigmentation or medical tattooing is a novel and easy to learn technique to camouflage various dermatological conditions like stable vitiligo, alopecia (androgenetic alopecia or stable alopecia areata) as well as for semi permanent make up.
Keywords: Make up, medical tattooing, micropigmentaion
Introduction
‘Micropigmentation’ also known as ‘dermatography’ denotes the aesthetic use of tattooing in dermatology for camouflaging of various skin conditions with a cosmetic importance like vitiligo, alopecia, etc.[1,2] Tattooing, first introduced by Captain Cook in 1976, literally means implantation of black pigment into the skin.[3,4]
Definition
Micropigmentation is defined as uniform implantation of minute and metabolically inert pigment granules into the dermis using electrically driven needles.[1,2] The pigments are deposited intradermally between superficial and mid dermis, where they are permanently fixed intracellularly within dermal mononuclear cells and extracellularly among collagen fibres, blood vessels, and hair follicles. After few years, a small amount of pigment is taken up by the regional lymph nodes which may cause color fading at the treated site. Since the pigments used are metabolically inert and nontoxic, nonallergenic, chances of foreign body reaction are low.[5]
Instruments
Various machines are used for micropigmentation ranging from conventional tattoo machines which are used by tattoo artists and specialized medical tattoo machine which is used by medical professionals [Table 1].
Table 1.
Type of tattoo machines
| Conventional tattoo machine[6] | Specialized medical tattoo device[5] |
|---|---|
| Heavy | Light weight |
| Needle depth has to be set manually by rough estimation by adjusting the needle chamber and locking it on the handle using a screw | Precision of accurate needle depth insertion (0.8 to 1 mm deep) |
| Painful | Less painful |
| Has multiple parts like handpiece, power adaptor, primary unit with display, plug | Single handpiece which is connected to power supply |
| Has a provision for attaching reusable cartridge which can be sterilized after every use |
Pigment[8,9]
The pigment which is used for micropigmentation is nontoxic, metabolically inert, noncarcinogenic, and tissue-stable with a particle size of approximately 6 microns. The tattoo inks are available in gel base and alcohol base. The alcohol-based dye is the one commonly used and in patients with oily scalp the gel-based dye can be used. There are various inks available in the market which have a wide range in their quality and cost. In author’s experience, the good quality dyes are superior as they cause less diffusion after deposition into the skin.
Different shades are built up of different constituents- [Figure 1]
Figure 1.

Pigments used in micropigmentation
White- titanium dioxide
Red- cinnabar, mercuric sulfate (cadmium sulfide is added to make red darker)
Yellow- cadmium sulfide
Ochre yellow – iron oxide
Brown- iron oxide
Black- iron oxide
Colour theory
Color theory is one of the most important aspect of micropigmentation training. There are three important basic colors shades: red, yellow, and blue.[10] The way these color shades are merged to produce secondary and tertiary colors determines the end results of how the healed lesions will look like. Now-a-days, a wide array of color shades are available in market. The colors mostly used for permanent make-up (eyeliners, eyebrows), for areola in darker individuals, and scalp micropigmentation are mostly shades of brown. Shades of red/pink are used for lips and areola in fair individuals. Choosing the right shade is essential as every color component undergoes various chemical changes after few weeks owing to sun exposure. Touch-up sessions at regular intervals are also important to maintain the results for a longer duration of time.
Patients’ eyebrows may heal with bluish, greenish, grayish, or reddish tone after chronic exposure to sunlight or in case of an old tattoo. In such cases, we need to select complimentary colors to correct the color mismatch. Use of iron oxide containing pigments leads to undesirable tones (reddish or bluish) after few weeks.
Indications- Table 2 enlists the various indications of micropigmentation in dermatology.
Table 2.
Indications of micropigmentation[7]
| Serial No | Indications of micropigmentation |
|---|---|
| 1 | Stable vitiligo |
| 2 | Nevus depigmentosus, idiopathic guttate hypomelanosis |
| 3 | Permanent make-up |
| 4 | Madarosis |
| 5 | Scalp micropigmentation in alopecia |
| 6 | Camouflaging scars due to burns, surgical defects, striae distensae |
|
| |
| Contraindication for micropigmentation | |
|
| |
| 1 | Unrealistic expectations |
| 2 | History of allergies |
| 3 | Patient who is seropositive for HIV, HBsAg, HCV |
| 4 | Any major illnesses like bleeding diasthesis, cardiac disorders, autoimmune diseases, uncontrolled diabetes mellitus, CNS (central nervous system) disoders |
| 5 | Pregnancy and lactation |
| 7 | Age less than 18 years |
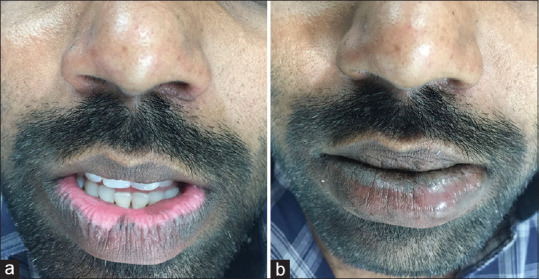
Stable vitiligo [Figure 2-5]- Micropigmentation is useful in camouflaging any residual color defects in patients of stable and recalcitrant local forms of vitiligo who are not responding to medical treatment after a certain extent. It is highly used in body sites like areola, lips, and genitals but can be used in other localized patches at other body sites.[9]
Figure 2.

(a and b) Before and after images of micropigmentation of stable lip vitiligo
Figure 5.

(a and b) Before and after images of micropigmentation in stable acral vitiligo
Figure 4.
(a) Before image (stable vitiligo) (b) After micropigmentation (stable vitiligo)
Permanent make-up [Figure 6a and b]-.Micropigmentation with appropriate color matching and shading helps to enhance the beauty of lips and eyebrows for patients who have a busy work culture and for individuals who are in beauty industry, corporate industry, airhostesses, cabin crew, etc., It is also used to create artificial moles or beauty spots.[10]
Figure 6.

(a) Eyebrows before microblading and micropigmentation, (b) Eyebrows after microblading and micropigmentation
Madarosis- Patients of madarosis due to hypothyroidism, leprosy, erythroderma, alopecia areata, and severe atopic dermatitis can be managed with micropigmentation but only when there disease activity is nullified by medical treatment.[10]
Alopecia- Androgenic alopecia and various types of cicatricial alopecias like pseudopelade of Brocq can be subjected to micropigmentation once disease activity is nulled. It certainly helps to the quality of life by improving the cosmetic outcome.[11]
Scars- Striae distensae, small scars due to burns, or any surgical defect at any body site of aesthetic importance can be camouflaged with micropigmentation.[5]
Preprocedural work-up
A detailed medical history to rule any contraindications is necessary.
Counselling and an informed consent is mandatory.
Complete blood count, bleeding and clotting time, prothrombin time, and blood glucose levels.
HIV enzyme-linked immunosorbent assay and hepatis B and hepatitis C virus screening.
COVID-19 RT-PCR.
Patch test to rule out any allergy to pigment.
Avoid consumption of alcohol, tobacco, and drugs like aspirin (antiplatelet drugs, anticoagulant drugs) 4 days before procedure.
Avoid excessive sun exposure and tanning.
Preparation of pigment
Prepare the pigment in a sterile container.
While preparing pigment, lighter shade is used as base and darker shade is added drop by drop till desired color match is achieved.
For color matching, the prepared mixture is applied on the boundary of the lesion and compared with surrounding skin.
Steps
Clinical baseline photography.
Preliminary preparation- Maintain asepsis throughout the procedure. Cleanse the desired site with spirit and betadine. Mark the border of site with a sterile skin-marking pen. Use a new and sterile cartridge for every patient.
Anesthesia- Topical EMLA (Eutactic mixture of local anesthetic) cream under occlusion must be applied 45 minutes to 60 minutes before starting the procedure. In vascular areas like lips, injection lignocaine 2% with adrenaline (1:10,000) should be used.
-
Procedure- Apply a thick paste of the pigment on the desired site and spread uniformly. If area is larger, treat the area in parts. But ensure that all the parts are covered in the same session. Make sure that the desired area is in a horizontal plane. Start the machine at around 1,500 rpm to 4,500 rpm and keep needle length to 1.2 to 1.5 mm (needle length can be kept at 1 mm for facial lesions; it can be increased for thicker areas like back). Hold the machine in a pen holding fashion with needle perpendicular to the skin surface. Stretch the area to be treated with thumb and index finger firmly and steadily. With circular movements, spread the pigment onto the skin surface with the needle. Avoid big loops. Pinpoint bleeding may be visible. After completion, wipe out the area with white petrolatum and look for any skip areas. Repeat the same procedure for the skip areas.
If bleeding is more, then try to stop the bleeding by steady compression with gauze piece soaked in white petrolatum and resume the pigmentation process after bleeding stops.
Postprocedure care- A pressure dressing and oral antibiotics and nonsteroidal anti-inflammatory drugs are prescribed to the patient postoperatively. Patient is advised to avoid contact with water for 3 to 7 days. The crust and scab falls off after 7 days. Patient is reviewed after 4 weeks to check if any touch-up micropigmentation is needed.
Adverse effects and complications[12]
Immediate side effects like edema, ecchymosis, reactivation of herpes simplex, secondary bacterial infection, and allergy to pigment can be noticeable within first week postoperatively. Delayed hypersensitivity reactions in the form of foreign body granulomas and foreign body reactions can occur after 2 to 4 weeks of micropigmentation.[13,14,15,16]
Late side effects like photo-allergic reaction especially with cadmium sulfate and blurring of pigment due to color leaks from original site can be encountered on rare occasions after 3 to 6 weeks.
Delayed complications like mycobacterial infections and deep fungal infections can occur in case of breach of aseptic measures.[12,13] Allergic reactions are common with mercury salts, cadmium, cobalt, and dichromate-based pigments. Koebnerization can occur in vitiligo or concomitant lichen planus or psoriasis if disease activity was not stabilized by medical management before planning the procedure. Sarcoidal granulomas, foreign body granulomas, milia, seborrhoeic keratosis, and epidermal cysts are other rare cutaneous side effects.[13,14,15,16]
Under extremely rare circumstances, skin cancers like melanoma, squamous cell carcinoma, dermatofibrosarcoma, and keratoacanthomas can occur especially with pigments of carcinogenic potential, for example, black pigment with benzopyrene is carcinogenic.[12]
Recent updates
In past recent years, there has been a lot of upgradation in the type of equipment used for micropigmentation. Also, newer colors in various shades are introduced in the market. Various other indications have been explored especially for permanent make-up or permanent cosmetic camouflage.
This is not only used as a camouflage for conventional dermatological conditions like vitiligo, alopecia (scalp micropigmentation), burn scars, and nipple-areola complex reconstruction but also for cosmetic indications like eyelash pigmentation (blepharopigmentation), permanent eyeliner, permanent lipsticks, reshaping of eyebrows (microblading), and so on. It is estimated to save up to 5,000 hours of make-up in a lifetime! Newer advances in the field include roller hair simulation, tattoo removal, scar camouflage, microfeathering, dedicated lip services, etc. There have been changes apart from the indications, such as principle, equipment, procedures, variables, and pigments as well.
Variables
In recent times, various variables have been delineated, to make the crossover from a cosmetic procedure done by tattoo artists to a scientific intervention performed by trained dermatologists. These include the needle angle, sharpness, depth, shape, number, caliber, the resistance of skin, time of contact, rotor torque and speed, colour combinations and palette – all in all, an in-depth amalgamation of mathematics, art, and science.
Equipment
The equipment used has undergone a paradigm shift, beginning at the assessment part. Nowadays, usage of Vernier’s calipers has been replaced by the Golden Mean Calipers and other Fibonacci number-evaluated assessment tools, like brow calipers, brow stencils, etc. Assessment includes measuring the patients’ Fitzpatrick skin type, vein tests, white fabric, and gold/silver testing to ascertain the skin undertone. The machine itself has taken a leap from manual syringes to coil machines (used by decorative tattoo artists), to pen-grip oscillators, and to fully electronic machines that can control torque, depth, and time digitally. Manual pens are routinely employed for microblading. Needles used also come in prongs of 3 (scalp), 5 (nipple-areolae, vitiligo), and 7 (brow reconstruction). Various needle types are now available, viz., round, flat, magnum, shader, and stacked. Corneal loupes are employed for improving attention to detail.
Pigments
Traditionally, pigments used were oxides (iron and titanium) and sulphates (cadmium and mercury). Newer pigments are organic fruit or vegetable-based botanical pigments, considered safer to use than its inorganic predecessors. Pigment preparation is done by making a pigment paste using 1–2 drops of normal saline/water/80% alcohol/glycerin to get proper consistency. Longer-lasting pigments are now in use, stretching the permanency from 2 years to 10 years. The pigment palette has also widened extraordinarily to include hundreds of shades to match brows, lashes, lips, mucosae, nipple/areolae, and vitiliginous skin. Specific ‘color correctors’ are also now in use.
Newer interventions
Microblading[10]
Microblading is a semi-permanent cosmetic tattooing treatment that fills in sparse eyebrows. The technique uses a hand-held tool like a superfine pen with needles (12 to 15) or tiny blades (microblading) to apply pigments that simulate additional hairs. The color fades over time and yearly touch-ups are recommended to maintain optimal results. This is because the pigments deposited here are superficial compared to the other permanent make-up techniques.
Microfeathering is a variant of microblading which is used when only a small amount of filling is required in already existing eyebrows.[10]
Microshading on the other hand uses deposition of pigment dots instead of pigment strokes used in microblading or microfeathering that imparts a powdered appearance to the eyebrows.[10]
Semi-permanent make up
This technique uses digital technology with more precise blades, needles, and better shades of the inks which gives a natural color to the patient. These pigments last for nearly 2 years, thus giving freedom to the patient to change as per the latest trends, and especially useful for people who vacillate and are indecisive.
Lip coloring
This service gives a natural color to the lips which makes them fuller, sometimes extending beyond the existing margin and shape of the lips. A digital pen is used which gives precise control over the speed and depth of pigment deposition. Just after the procedure, the patient may find the color bolder than he/she desired; in such a case, the patient should be reassured as the color fades over the next three days giving the desired shade.[5]
Lash line enhancement
This technique involves use of a digital pen which deposits pigments filling gaps in eye-lash line giving an illusion of naturally set eyelashes. This revolutionary technique has made false eyelashes and lash extensions a thing of the past.[17]
Nipple-areola reconstruction [Figure 3a and b]
Figure 3.

(a and b) Before and after images of stable vitiligo in nipple areolar complex
Breast cancer has the highest mortality and morbidity globally. A sequalae to mastectomy remains radical removal of the nipple-areola complex. Since the 1940s, composite grafts, surgical flaps, autologous augmentation with cartilage, or muscle and synthetic augmentation has been in practice. Micropigmentation is being extended to this field too, as the least invasive modality with excellent results, even lending a ‘simulated’ three-dimensional look to the nipple-areola complex.[18]
Hair simulation
This is a newer advancement in the field of scalp micropigmentation, wherein, instead of the classic 3-pronged needle, a microneedling device is used (manually or attached to a rotor) to smear pigment over the bald scalp. This imparts a ‘uniform shaded look’ as opposed to simulation of each follicular unit (in scalp micropigmentation) and is easier to perform as a procedure, reducing the contrast between hair and the scalp.[11]
Tattoo removal
Touted as ‘Non-LASER’ tattoo removal systems, these employ microneedling devices with more than 500 microneedles and deliver agents like lactic acid or hydrocyanic acid, which act as bleaching agents and disintegrate the tattoo for the desired effect. They come as attachments to existing micropigmentation pens or as a separate apparatus.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Singh AK, Karki D. Micropigmentation tattooing for the treatment of lip vitiligo. J Plast Reconstr Aesthet Surg. 2010;63:988–91. doi: 10.1016/j.bjps.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Traquina AC. Micropigmentation as an adjuvant in cosmetic surgery of the scalp. Dermatol Surg. 2001;27:123–8. [PubMed] [Google Scholar]
- 3.Kaliyadan F, Kumar A. Camouflage for patients with vitiligo. Indian J Dermatol Venereol Leprol. 2012;78:8–15. doi: 10.4103/0378-6323.90940. [DOI] [PubMed] [Google Scholar]
- 4.Earley MJ. Basal cell carcinoma arising in tattoos: A clinical report of two cases. Br J Plast Surg. 1983;36:258–9. doi: 10.1016/0007-1226(83)90103-0. [DOI] [PubMed] [Google Scholar]
- 5.Garg G, Thami GP. Micropigmentation: Tattooing for medical purposes. Dermatol Surg. 2005;31:928–31. [PubMed] [Google Scholar]
- 6.Serup J, Carlsen KH, Sepehri M. Tattoo complaints and complications: diagnosis and clinical spectrum. Curr Probl Dermatol. 2015;48:48–60. doi: 10.1159/000369645. [DOI] [PubMed] [Google Scholar]
- 7.De Cuyper C. Permanent makeup: Indications and complications. Clin Dermatol. 2008;26:30–4. doi: 10.1016/j.clindermatol.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 8.Tiziano JP. Dermography: A complement to esthetic surgery. Ann Chir Plast Esthet. 1990;35:489–95. [PubMed] [Google Scholar]
- 9.Halder RM, Pham HN, Breadon JY, Johnson BA. Micropigmentation for the treatment of vitiligo. J Dermatol Surg Oncol. 1989;15:1092–8. doi: 10.1111/j.1524-4725.1989.tb03129.x. [DOI] [PubMed] [Google Scholar]
- 10.Marwah MK, Kerure AS, Marwah GS. Microblading and the science behind it. Indian Dermatol Online J. 2021;12:6–11. doi: 10.4103/idoj.IDOJ_230_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dhurat RS, Shanshanwal SJS, Dandale AL. Standardization of SMP procedure and its impact on outcome. J Cutan Aesthet Surg. 2017;10:145–9. doi: 10.4103/JCAS.JCAS_116_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khunger N, Molpariya A, Khunger A. Complications of tattoos and tattoo removal: Stop and think before you ink. J Cutan Aesthet Surg. 2015;8:30–6. doi: 10.4103/0974-2077.155072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hypolite T, Grant-Kels JM, Chirch LM. Nontuberculous mycobacterial infections: A potential complication of cosmetic procedures. Int J Womens Dermatol. 2015;1:51–4. doi: 10.1016/j.ijwd.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valbuena MC, Franco VE, Sánchez L, Jiménez HD. Sarcoidal granulomatous reaction due to tattoos: Report of two cases. An Bras Dermatol. 2017;92:138–41. doi: 10.1590/abd1806-4841.20175860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wollina U. Nodular skin reactions in eyebrow permanent makeup: Two case reports and an infection by mycobacterium haemophilum. J Cosmet Dermatol. 2011;10:235–9. doi: 10.1111/j.1473-2165.2011.00564.x. [DOI] [PubMed] [Google Scholar]
- 16.Koh MJA, Teo RYL, Liu TT. Multiple epidermal cysts occurring in a tattoo. Singapore Med J. 2009;50:e376–7. [PubMed] [Google Scholar]
- 17.Patipa M, Jakobiec FA, Krebs W. Light and electron microscopic findings with permanent eyeliner. Ophthalmology. 1986;93:1361–5. doi: 10.1016/s0161-6420(86)33565-6. [DOI] [PubMed] [Google Scholar]
- 18.de Pinho Pessoa SG, Matos JRF, Dias IS, de Pinho Pessoa BBG, de Alencar JCG. Simple and safe technique for nipple-areola reconstruction with intradermal tattoo. Rev Bras Cir Plást. 2012;27:415–20. [Google Scholar]


