Abstract
Background
The coronavirus 2019 (COVID-19) pandemic resulted in rapid implementation of telemedicine. Little is known about the impact of telemedicine on both no-show rates and healthcare disparities on the general primary care population during the pandemic.
Objective
To compare no-show rates between telemedicine and office visits in the primary care setting, while controlling for the burden of COVID-19 cases, with focus on underserved populations.
Design
Retrospective cohort study.
Setting
Multi-center urban network of primary care clinics between April 2021 and December 2021.
Participants
A total of 311,517 completed primary care physician visits across 164,647 patients.
Main Measures
The primary outcome was risk ratio of no-show incidences (i.e., no-show rates) between telemedicine and office visits across demographic sub-groups including age, ethnicity, race, and payor type.
Results
Compared to in-office visits, the overall risk of no-showing favored telemedicine, adjusted risk ratio of 0.68 (95% CI 0.65 to 0.71), absolute risk reduction (ARR) 4.0%. This favorability was most profound in several cohorts with racial/ethnic and socioeconomic differences with risk ratios in Black/African American 0.47 (95% CI 0.41 to 0.53), ARR 9.0%; Hispanic/Latino 0.63 (95% CI 0.58 to 0.68), ARR 4.6%; Medicaid 0.58 (95% CI 0.54 to 0.62) ARR 7.3%; Self-Pay 0.64 (95% CI 0.58 to 0.70) ARR 11.3%.
Limitation
The analysis was limited to physician-only visits in a single setting and did not examine the reasons for visits.
Conclusion
As compared to office visits, patients using telemedicine have a lower risk of no-showing to primary care appointments. This is one step towards improved access to care.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-023-08236-x.
Introduction
The coronavirus 2019 (COVID-19) pandemic served as a stark reminder of the systematic healthcare inequities that exist in the USA. The Centers of Disease Control and Prevention (CDC) reported 146 million total infections and 921,000 deaths as of October 2021, with underserved populations disproportionately affected. These patient populations generally are from minority groups and are prone to facing healthcare care inequities due to their racial/ethnic background or physical/mental disabilities.[1–3] Underserved populations suffer worse health outcomes due to a variety of factors, such as logistical and economic barriers, racism, and low representation of healthcare providers from the marginalized communities.[4–6]
The demand for telemedicine, which refers to remote delivery of medical care, during the COVID-19 pandemic irreversibly changed our healthcare system, ushering a technological revolution. Even before COVID, telemedicine was introduced as a potential solution for reducing disparities.[6,7] Telemedicine helps to save fuel, reduce costs, and prevent patients from missing days at work, especially those who live in rural areas.[8] Over the last few decades, Human Resources and Services Administration (HRSA) and Medicaid allowed state programs to provide reimbursement of telemedicine visits; however, widespread telemedicine use has remained limited due to need of in-person visits based on acuity or of physical examinations, and lack of comfort with technology.[9,10]. Then, in March of 2020, as COVID forced healthcare systems to find alternative methods of care delivery, Congress enacted the Coronavirus Aid, Relief, and Economic Security (CARES) Act to allow provision of widespread telemedicine care during the pandemic.[10]
Telemedicine refers to delivery of digital care via telephone and video visits.[11] It comes with its own challenges. For example, video-based visits are dependent on access to quality internet, and poor broadband coverage, lack of digital access, and inadequate digital literacy can limit the delivery of virtual care which creates problems for patients of lower socioeconomic class who lack access to technology.[11–14] Telemedicine can hinder the interpretation of physical exam findings such as assessment of skin rashes, signs of cardiac diseases murmurs, and limb swelling. It can affect patient-physician relationships particularly in first time or complex encounters, can create language barriers for less proficient in English language, and perhaps is less personable compared to in-office visits.[15–17] Apart from lack of familiarity with technology, older patients and those with disabilities may suffer from chronic medical conditions such as reduced hearing and vision as well as cognitive and motor decline which impair telehealth use.[12,15,17] Given such challenges of telemedicine, the implications on access to care remain uncertain, but several steps have been taken to ensure proper integration of telemedicine into healthcare systems which would improve access to care.[18] For example, Health Insurance Portability and Accountability Act (HIPPA) compliant virtual platforms promote privacy and interpersonal connection between the patient and physician.[19] In addition, as part of the emergency use authorization (EUA), patients can get assistance for their internet coverage.[20]
One important marker of access to care to a certain degree is when appointments in the primary care setting are missed, in other words, when patients “no-show” to their appointments. No-shows create interference in a patient’s care plan such as reduced age-appropriate preventative screening and delayed disease detection, contributing to poor control and outcomes of chronic conditions. Simply put, any interaction with the patient is an opportunity to provide care and thus address potential healthcare disparities and outcomes, but only if the interaction happens.[21,22] In addition, no-shows cause missed opportunities for other patients who could have filled the spot.[23] Before the pandemic, no-show rates were higher in socio-economically underprivileged patient populations (17.5%)[21] (i.e., Black, Hispanic), and patients on Medicaid due to unaffordability of healthcare, lack of transport and health insurance, etc.[22,24] Much of the available literature on telemedicine utilization during the pandemic has been limited by narrow time intervals and small samples of convenience, or otherwise are less generalizable to non-specialty clinic populations.[25–30] Furthermore, while telemedicine was a prominent healthcare delivery method early in the pandemic, by late 2020, many patients were provided the opportunity to complete either virtual or in-office visits.[31] This serves as an opportunity to compare differences in the no-show rates between the two encounter types.
Given the impact of telemedicine on our healthcare system, despite its challenges and initial barriers to uptake in historically underserved and underserved patient populations, a key question remains: can widespread implementation of telemedicine affect healthcare disparities by improving access to care? In this study, we aim to assess this impact by examining the risk of no-showing to appointments with telemedicine as compared to office visits in these patient populations.
METHODS
Study Setting
This retrospective cohort study was approved by the HonorHealth Institutional Review Board [1710381–1] and grant funding was supported by the Federation of State Medical Boards Foundation.
We examined visits conducted between January 2019 through December 2021 at both HonorHealth Medical Group (HHMG) primary care clinics and Neighborhood Outreach Access to Health (NOAH) primary care clinics. HonorHealth Medical Group (HHMG) comprised 27 primary care clinics with > 150 primary care providers serving the greater Scottsdale/Phoenix, Arizona, area. There are 8 NOAH clinics affiliated with HonorHealth that are Federally Qualified Health Centers (FQHC). Both HHMG and NOAH are non-profitable organizations. Both networks send out telephone reminders to patients about the time, date, and provider names at least 24 h before the actual appointment. Medical assistants also provide easy to follow instructions to operate telemedicine services to patients with virtual appointments.
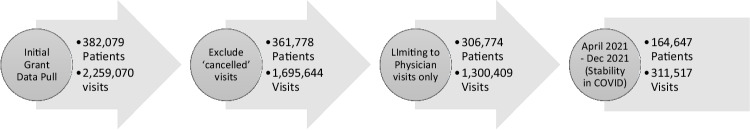
Study Population
All outpatient primary care adult (age 18 +) visits record from within HHMG and NOAH were queried on January 4, 2022, from our shared Electronic Health Record, EPIC™ (Epic Systems Corporation; Verona, Wisconsin). In total, 2.2 million visits were initially extracted and de-identified to include variables of interest: ethnicity/race, payer type, age, sex, visit type (telehealth vs. office), and no-show data. Ethnicity/race included White, Hispanic/Latino, Black, Other (Pacific Islander, Native Hawaiian, American Indian), and Asian. Data on payor types included Medicaid, Medicare, managed care (private managed care), and self-pay (surrogate for uninsured patients) which primarily represents the underprivileged patient population. Telemedicine appointments included video and phone visits, with video visits being conducted using HIPPA-compliant software. We excluded “Cancelled visits” (comprising appointments that were rescheduled or otherwise cancelled ahead of time), such that the only visit statuses were “completed” or “no-show.” Pre-COVID data was excluded since there were minimal to no telemedicine visits. Additionally, visits from non-physicians (i.e., advanced practice practitioners) were excluded because in our organization they generally have lower rates of continuity of care and higher rates of same day add-ons or sick visits, and we felt this would skew the results. Finally, our result showed a final inclusion of 311,517 visits across 164,647 patients. Out of 311,517 visits, 56,725 were telemedicine visits with 5.2% no-show rate while 254.792 were office visits with 7.3% no-show rate. This progression is depicted in Fig. 1.
Fig. 1.
Inclusion criteria from initial grant-funded data pull down to steady-state statistical process control (SPC) analysis. The first arrow shows the initial data pull from January 2019 to December 2021. Data were refined by removing cancelled visits and visits conducted by non-MD/DO providers. The final timeline analyzed in this study was the steady state from April 2021 to December 2021 as shown in the last arrow.
Statistical Analysis: Controlling for Effects of COVID-19 with Stability in Time Trends
To account for the variable impact of COVID-19 upon no-show rate behaviors, we used Statistical Process Control (SPC) software (QI Macros version 2018.01) to analyze monthly no-show time-trends to identify periods of stability/steady state (April 2021 through December 2021) in rate ratios against background variations. This steady state was less affected by the wide no-show fluctuations seen related to COVID-19 surges over time, refining any subsequent statistical analysis.
Statistical Analysis
Counts, incidence rates, and relative risk ratios were calculated, along with 95% confidence intervals, where appropriate. Relative risks were calculated using a Poisson distribution with robust confidence intervals,[32] and an exchangeable working correlation matrix.
Incidence rates for no-shows were calculated for demographic predictor sub-categories (e.g., self-pay, Medicare, Medicaid, Managed care within payor type), stratified by telemedicine and office visits. Then, relative risk ratios for no-shows were estimated for telemedicine vs. office visits for each of these categories.
Finally, a multivariable analysis, including age, sex, race, ethnicity, and financial class, along with visit type (i.e., office visit or telemedicine visit), was used to estimate the overall impact of visit type on no-show rates, while controlling for demographic attributes.
p-values are not reported in this manuscript because the sample size is so large that even very small effect sizes reflecting no meaningful differences yield statistically significant results. Further, the many statistical tests performed increase the probability of type I error (falsely rejecting a null hypothesis based on p < 0.05). Instead, we have relied on 95% confidence intervals to communicate the precision of our statistical estimates. Analyses were conducted using SPSS v. 28 (IBM Corp., Armonk, NY, USA).
RESULTS
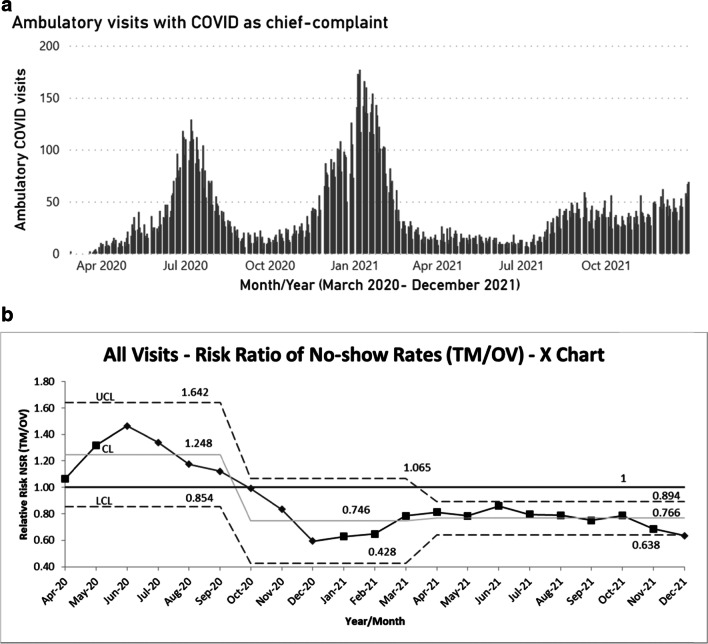
Examination of monthly no-show time-trends identified two process change points (October 2020 and April 2021), corresponding to the nadirs of COVID-19 cases in our community (Fig. 2a).
Fig. 2.
a Daily ambulatory visits (HHMG and NOAH) with COVID as chief complaint over time. b Risk ratios over time (X-chart) for all visits (points of special cause variation identified with diamond markers). Upper and lower control limits (UCL/LCL) set at 3 standard deviations (99% CI). The two figures are used to compare the trend of the overall risk ratio of no-showing between telehealth and office visits superimposed with the burden of COVID cases during that time. The risk of no-showing via telehealth was higher immediately after the implementation of telehealth, but eventually declined and reached a statistically significant steady state by April 2021.
The time-period from April of 2021 through December of 2021 displayed substantial stability with narrow control limits (3 Sigma or 3 standard deviations), indicating that this period of 8 months displayed consistent relative risk in all relevant subgroups despite meaningful increases in Delta-variant COVID-19 cases during fall of 2021 (Fig. 2b).
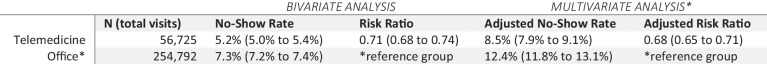
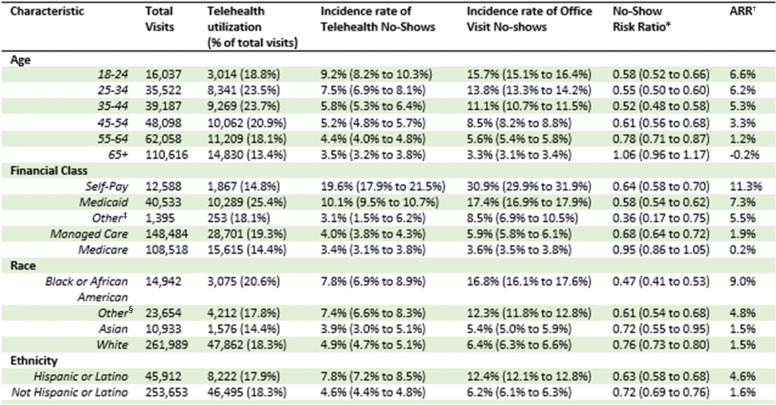
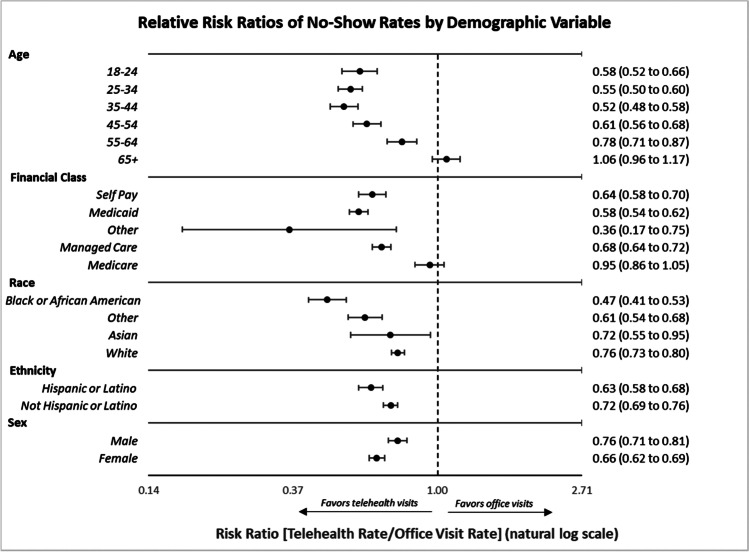
Bivariate modeling of relative risk ratios of no-show incidence from April 2021 to December 2021 revealed significant differences between telemedicine no-show risk and office visit no-show risk (risk ratio 0.71 [95% CI 0.68 to 0.74], as seen in Table 1. The adjusted risk ratio which adjusted for all variables and visit types again confirmed lower no-show risk as shown in Table 1 with telemedicine compared to office visits (0.68 [95% CI 0.65 to 0.71]), i.e., 32% relative risk reduction, 4% absolute risk reduction (ARR). Relative risk ratios universally favored telemedicine in most subgroups analyzed (see Table 2, Fig. 3). Table 2 displays the no-show incidence rates of both telemedicine and office visits for each demographic variable with further distinction of risk ratios, and absolute risk reduction. There was significant benefit of telehealth on no-show risk with respect to socioeconomic status, age, and race/ ethnicity. For example, Self-pay was associated with the greatest benefits (risk ratio 0.64 [95%CI 0.58 to 0.70]; ARR 11.3%) followed by Blacks/African Americans (risk ratio 0.47 [95% CI 0.41 to 0.53]; ARR 9.0%). The third group that benefitted from telemedicine was patients with Medicaid (risk ratios of 0.58 [95% CI 0.54 to 0.62]; ARR 7.3%). Younger age overall was associated with net positive effects of telemedicine on no-show risk, with the greatest benefits within 35–44 cohort (risk ratio 0.52 [95%CI 0.48 to 0.58]; ARR 5.2%).
Table 1.
Transition from Bivariate to Multivariate Analysis for No-Show Rates
The adjusted risk ratio represents the “true” effect of telehealth (when controlling for the other variables in Table 2)
*Adjusted for age, sex, race, ethnicity, and financial class
Table 2.
Bivariate Analyses with Interaction of Telehealth on Characteristics Affecting No-Showing
The total number of visits, telehealth utilization, incidence rates of no-shows with telehealth and office visits, and relative risk ratio, absolute reduction risk, and the number needed to treat, stratified by age, financial/payor type, race, and ethnicity, as well sex. Except for patients older than 65 or those with Medicare where risk was equivalent, the no-show rate was lower with telehealth than office visits in all other cohorts
*Risk ratio defined as ratio of telehealth no-show incidence rate/office visit no-show incidence rate
†Absolute risk reduction (ARR) defined as raw difference between office visit and telehealth no-show incidence rates
‡Other includes payers which could not be classified into available categories by EMR
§Other includes Pacific Islander, Native Hawaiian, and American Indian/Alaska Native
Fig. 3.
Forest plot of relative risk ratios (telehealth NSR/office visit NSR) by variable of interest. A forest plot of the primary outcome (relative risk ratio of no-show rates between telehealth and office visits). The effect measure used was RR, where values less than 1 favor telehealth and values greater than 1 favor office visits. The dotted vertical line at RR= 1 indicates equivalent risk of no-show between visit types. Dot represents point estimates; bars represent 95% confidence intervals.
All remaining cohorts examined also showed lower risk of no-showing with telemedicine except for those patients who were 65 + (risk ratio 1.06 [95%CI 0.96 to 1.17] − 0.2%). Those with Medicare had equivalent no-show risk between telehealth and office visits (risk ratio 0.95 [95%CI 0.86 to 1.05]). These patients had parity of no-show risk between telehealth and office visits.
DISCUSSION
This large, longitudinal, retrospective study addresses an important gap which is scarcity of available literature on the effects of telemedicine on adult ambulatory primary care no-show rates. From April to December 2021, we found lower no-show rates with telemedicine than office visits in all racial/ethnic groups, patients younger than 65, and those with Managed Cared, Medicaid, or Self-pay. There was not a difference in the no-show risk for telemedicine or office visits for those 65 and older and those with Medicare. To the best of our knowledge, this is the first paper that uses a longitudinal approach to review a large dataset on the risk or incidence of no-showing in adult primary care settings to identify a mid-pandemic steady state.
Prior studies during the initial months of the pandemic showed reduced telemedicine utilization in similar groups to those analyzed in our study, such as older/Medicare patients or those of lower socioeconomic status due to lower literacy rate, high cost and unavailability of broadband services, lack of skills, assistance and comfort with telehealth services, etc.[28,33,34] Although there was an initial rise of no-showing with telemedicine visits, we start to see a gradual decline from late 2020 onwards (see Appendix) in the risk of no-showing which suggests that patients and providers may have experienced a learning curve as mentioned above in acquiring the skills necessary to operate telemedicine visits. Over time, we found parity of telemedicine to in-office visits in all subgroups, and superiority in most cohorts. Thus, with appropriate time and training, telemedicine visits can be successfully implemented and completed.
As shown in Fig. 3, there was a significant reduction in the risk of no-showing with telemedicine in historically underserved patient groups such as African American, Hispanic/Latino, and Asian patients. There is conflicting evidence on these racial/ethnic groups in the literature. For example, some studies noted minimal benefits of telemedicine in underserved patients when compared to in-office or emergency visits[26,35–37] or White patients.[37,38] Some of the potential barriers to telemedicine usage include lack of already established primary care providers, economic vulnerability, linguistic barriers, and lack of access, skills, or digital education.[39–42] Despite such barriers, other studies have shown comparable[43,44] or superior rates of telemedicine usage compared to White patients[45], or overall increase in visit completion in underserved patients compared to before the pandemic.[46] As these groups have previously been shown to suffer worse healthcare outcomes,[26,35,37] our results support the assertion that telemedicine should be seen as an important method for reducing barriers to care in such potentially underserved populations.
Other underserved populations benefitted from the availability of telemedicine, as shown by the significant no-show risk reduction in Medicaid and Self-pay patients (used as a surrogate for patients from lower socioeconomic status). Prior early research has also been conflicting in these populations, with some studies showing favorability of telemedicine which overcomes barriers of long distance and costly commute, finding transportation, challenging parking, spending long in waiting room, and time away from work and home[46,47], and others showing less favorability, particularly with video visits due to challenges with technology.[35,47,48] Therefore, telemedicine may be of particular benefit in this population with respect to cost and time savings.
Unsurprisingly, younger patients had less risk of no-showing with telemedicine, as this population may be more facile with technology and prefer visits that limit time away from home and work. However, an important finding from our work is that there was no significant difference in the no-show rate with telemedicine compared to in-office visits in those older than 65 or with Medicare—in other words, that the two visit types were equivalent with respect to visit completion. This contrasts with prior work in this population which has shown unfavorability towards telemedicine during the early pandemic[14,15,49,50], possibly due to lack of access to technology or skills to manage virtual visits.[51] Telemedicine improves medication adherence and alleviates logistical barriers in elderly patients with chronic medical conditions and restricted physical mobility.[46,52–55] While the decision to offer telemedicine visits to such patients needs to be individualized, our results suggest that telemedicine is an important option for this patient population.
This study has important policy and financial implications. First, the CARES Act, instituted during the pandemic, increased Medicare reimbursement to medical providers and allowed provision of telehealth services to patients across different state lines if permitted by the state or interstate policies.[56,57] Such conveniences may facilitate telemedicine usage for all patient groups but particularly in the underserved patient population during and after the pandemic. As coverage and continued expansion of telemedicine services is currently in flux as the pandemic lessens, our results should offer support to policymakers to at minimum continue current practices. Second the US healthcare system loses $150 billion on missed appointments every year, with a loss of $150,000 annually per physician.[23] In the era of severe shortage of primary care physicians and higher cost of healthcare, telemedicine may help to mitigate the financial waste caused by no-show visits and has the potential to reduce overhead expenses. Further study is needed to explore the benefits of telemedicine based on chief complaint/visit type, patient location (i.e., rural vs. urban), provider type, and the ways in which baseline patient characteristics interact (i.e., multivariable analyses) to contribute to risk of no-showing.
Limitations
This study has several limitations. First, we conducted the study within two networks of clinics, in one medical system, and did not account for nuances in workflows among individual clinics, but largely these were similar among all clinics. Similarly, we did not examine specialty clinic visits or primary care visits with an advanced practice practitioner (APP). It is possible that our trends in telemedicine usage which is limited to the urban setting do not reflect the trends of the larger US population, rural population, or those seeking care from specialty clinics or from an APP. Second, we performed our analysis prior to the Omicron wave of COVID cases. Third, we aggregated three ethnic groups in “Other” due to the small sample size. It is possible that larger trends in these groups do not mirror the trends we describe in our study populations. Fourth, we did not examine visits by chief complaint. It is possible that certain types of visits (i.e., sick versus preventative care visits) lend themselves better to telemedicine, and this might then impact the likelihood of no-showing to a telemedicine visit. Lastly, we did not analyze phone visits and video visits separately as this data was not reliably available. Thus, it remains unclear whether one particular modality lends itself better to visit completion.
CONCLUSIONS
Our study supports continued use of telemedicine in an urban primary care setting. Although initially introduced as a disruptive innovation, our study suggests telemedicine helps to improve access to care in primary care settings through increased appointment attendance. It is a viable step to addressing healthcare disparities, recognizing that a provider-patient interaction is only one of many factors relating to healthcare outcomes.
Supplementary Information
Below is the link to the electronic supplementary material.
(DOCX 744 kb)
Funding
This work was supported by the Federation of State Medical Boards (FSMB).
Declarations:
Conflict of Interest:
Consultancies: Dr Curt Bay received a consulting fee to assist in data analysis.
Advisory Board: Dr Alethea Turner received payment for her participation on the editorial board for the Association of Family Medicine Residency Directors (AFMRD) and Family Medicine Residency Curriculum Resource as an associate editor. Drs Alethea Turner and Dmitry Bisk received payment as the members of Innovation Care partners (ICP) and Clinical Integration Committee (CIC).
Leadership/Fiduciary role: Dr Priya Radhakrishnan is the Governor of the Arizona Chapter of the American College of Physicians (ACP). She is also the Chair Elect of the ACP Board of Governors and Principal Investigator of the Improving Health Equity via Telemedicine (IHET) grant. Dr Radhakrishnan did not receive any payment.
Footnotes
Dania A. Shah, MD, and Rustan Sharer, MD, are co-first authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CDC Covid Data tracker [Internet]. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. Available at: https://covid.cdc.gov/covid-data-tracker. Accessed 10 Jul 2022.
- 2.Andraska EA, Alabi O, Dorsey C, et al. Health care disparities during the COVID-19 pandemic. Semin Vasc Surg. 2021;34(3):82–8. [DOI] [PMC free article] [PubMed]
- 3.Thebault R, Tran AB, Williams V. The coronavirus is infecting and killing Black Americans at an alarmingly high rate [Internet]. The Washington Post. WP Company; 2020. Available at: https://www.washingtonpost.com/nation/2020/04/07/coronavirus-is-infecting-killing-black-americans-an-alarmingly-high-rate-post-analysis-shows/. Accessed 10 Jul 2022.
- 4.Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. 2012;123:167-174. [PMC free article] [PubMed]
- 5.LaVeist TA, Gaskin D, Richard P. Estimating the economic burden of Racial Health Inequalities in the United States. Int J Health Serv. 2011;41(2):231–8. [DOI] [PubMed]
- 6.Bove AA, Homko CJ, Santamore WP, et al. Managing hypertension in urban underserved subjects using telemedicine—a clinical trial. Am Heart J. 2013;165(4):615–21. [DOI] [PubMed]
- 7.Battineni G, Nittari G, Sirignano A, et al. Are telemedicine systems effective healthcare solutions during the COVID-19 pandemic? J Taibah Univ Med Sci. 2021;16(3):305-306. [DOI] [PMC free article] [PubMed]
- 8.Bynum AB, Irwin CA, Cranford CO et al. The impact of telemedicine on patients' cost savings: Some preliminary findings. Telemed J e-Health. 2003;9(4):361–7. [DOI] [PubMed]
- 9.Telemedicine [Internet]. Medicaid. Available at: https://www.medicaid.gov/medicaid/benefits/telemedicine/index.html. Accessed 10 Jul 2022.
- 10.Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic — United States, January–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1595–9. [DOI] [PMC free article] [PubMed]
- 11.Huang J, Gopalan A, Muelly E, et al. Primary care video and telephone telemedicine during the COVID-19 pandemic: treatment and follow-up health care utilization. Am J Manag Care. 2023;29(1):e13-e17. Published 2023 Jan 1. [DOI] [PMC free article] [PubMed]
- 12.Scott Kruse C, Karem P, Shifflett K, et al. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2016;24(1):4–12. [DOI] [PMC free article] [PubMed]
- 13.Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11(2):60–70. [DOI] [PubMed]
- 14.Vogels EA. Digital divide persists even as Americans with lower incomes make gains in tech adoption [Internet]. Pew Research Center. Pew Research Center; 2021. Available at: https://www.pewresearch.org/fact-tank/2021/06/22/digital-divide-persists-even-as-americans-with-lower-incomes-make-gains-in-tech-adoption/. Accessed 10 Jul 2022.
- 15.Segrelles-Calvo G, López-Padilla D, de Granda-Orive JI. Pros and cons of telemedicine in the management of patients with chronic respiratory diseases. Arch Bronconeumol (English Edition). 2016;52(12):575–6. [DOI] [PubMed]
- 16.Moghaddamjou A, Salaheen Z, Fehlings MG. A New Era of Practice: COVID 19 and Neurosurgical Care via Telemedicine [Internet]. AANS Neurosurgeon. 2021. Available at: https://www.aansneurosurgeon.org/feature/a-new-era-of-practice-covid-19-and-neurosurgical-care-via-telemedicine/. Accessed 10 Jul 2022.
- 17.Mira-Solves JJ, Orozco-Beltrán D, Sánchez-Molla M, et al. Evaluation of satisfaction with telemedicine devices and with the results of the care received among chronic patients. Aten Primaria. 2014;46:16–23. [DOI] [PMC free article] [PubMed]
- 18.Daniel H, Sulmasy LS; Health and Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med. 2015;163(10):787–9. [DOI] [PubMed]
- 19.Baker J, Stanley A. Telemedicine Technology: A review of services, equipment, and other aspects. Curr Allergy Asthma Rep. 2018;18(11). [DOI] [PubMed]
- 20.Burke BL Jr, Hall RW; Section on Telehealth Care. Telemedicine: Pediatric Applications. Pediatrics. 2015;136(1):e293-e308. [DOI] [PMC free article] [PubMed]
- 21.Chou EY, Moore K, Zhao Y, et al. Neighborhood effects on missed appointments in a large urban academic multispecialty practice. J Gen Intern Med. 2021;37(4):785–92. [DOI] [PMC free article] [PubMed]
- 22.Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments. J Prim Care Commun Health. 2013;4(4):251–5. [DOI] [PubMed]
- 23.No show appointments: Why they happen and how to reduce them - MGMA [Internet]. Available at: https://www.mgma.com/getattachment/Resources/Resources/Business-Strategy/No-Show-Appointments-Why-They-Happen-and-How-to-R/No-Show-Appointment-Paper.pdf.aspx?lang=en-US&ext=.pdf. Accessed 10 Jul 2022.
- 24.Zhang D, Shi L, Han X, et al. Disparities in telehealth utilization during the COVID-19 pandemic: Findings from a nationally representative survey in the United States [published online ahead of print, 2021 Oct 11]. J Telemed Telecare. 2021;1357633X211051677. [DOI] [PubMed]
- 25.Fuerst ML. Black & Hispanic patients used telehealth less during pandemic. Oncology Times. 2021;43(1):35–.
- 26.Wray CM, Tang J, Shah S, et al. Sociodemographics, Social Vulnerabilities, and Health Factors Associated with Telemedicine Unreadiness Among US Adults. J Gen Intern Med. 2022;37:1811–1813. [DOI] [PMC free article] [PubMed]
- 27.Drerup B, Espenschied J, Wiedemer J, et al. Reduced no-show rates and sustained patient satisfaction of telehealth during the COVID-19 pandemic. Telemed e-Health. 2021;27(12):1409–15. [DOI] [PubMed]
- 28.Darrat I, Tam S, Boulis M, et al. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg. 2021;147(3):287. [DOI] [PMC free article] [PubMed]
- 29.Alkilany R, Tarabichi Y, Hong R. Telemedicine visits during covid ‐19 improved clinic show rates. ACR Open Rheumatol. 2021;4(2):136–41. [DOI] [PMC free article] [PubMed]
- 30.Kemp MT, Liesman DR, Brown CS, et al. Factors associated with increased risk of patient no-show in telehealth and traditional surgery clinics. J Am Coll Surg. 2020;231(6):695–702. [DOI] [PMC free article] [PubMed]
- 31.Mafi JN, Craff M, Vangala S, et al. Trends in US ambulatory care patterns during the COVID-19 pandemic, 2019-2021. JAMA. 2022;327(3):237. [DOI] [PMC free article] [PubMed]
- 32.Zou G. A modified Poisson regression approach to prospective studies with Binary Data. American J Epidemiol. 2004;159(7):702–6. [DOI] [PubMed]
- 33.Branson S. Telehealth: Improving care of chronic conditions [Internet]. Assisted Home Health and Hospice. Available at: https://assistedcares.com/telehealth-improving-care-of-chronic-conditions/. Accessed 10 Jul 2022.
- 34.Witten B. [Internet]. Home Dialysis Central. Available at: https://homedialysis.org/news-and-research/blog/288telehealth-for-home-dialysis. Accessed 10 Jul 2022.
- 35.Hsiao V, Chandereng T, Lankton RL, et al. Disparities in telemedicine access: A cross-sectional study of a newly established infrastructure during the COVID-19 pandemic. Appl Clin Inform. 2021;12(03):445–58. [DOI] [PMC free article] [PubMed]
- 36.Rodriguez JA, Betancourt JR, Sequist TD, et al. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021 Jan;27(1):21-26. [DOI] [PMC free article] [PubMed]
- 37.Alishahi ML, Sevick C, Mathieu S, Everhart R, Gritz M. No-Show Rates for Telemedicine Versus In-Person Appointments During the COVID-19 Pandemic: Implications for Medicaid Populations. J Ambul Care Manage. 2022;45(4):332-340. [DOI] [PubMed]
- 38.Meno M, Abe J, Fukui J, et al. Telehealth amid the covid-19 pandemic: Perception among Asian, Native Hawaiian and pacific islander cancer patients. Future Oncol. 2021;17(23):3077–85. [DOI] [PMC free article] [PubMed]
- 39.Johnson PJ, Ghildayal N, Ward AC, et al. Disparities in potentially avoidable emergency department (ED) care. Med Care. 2012;50(12):1020–8. [DOI] [PubMed]
- 40.Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res. 2014;16(7):e172. [DOI] [PMC free article] [PubMed]
- 41.Anthony DL, Campos-Castillo C, Lim PS. Who isn’t using patient portals and why? evidence and implications from a national sample of US adults. Health Affairs. 2018;37(12):1948–54. [DOI] [PubMed]
- 42.Nouri S, Khoong EC, Lyles CR, et al. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal. 2020;1(3):1-13.
- 43.Siow MY, Walker JT, Britt E, et al. What Was the Change in Telehealth Usage and Proportion of No-show Visits for an Orthopaedic Trauma Clinic During the COVID-19 Pandemic?. Clin Orthop Relat Res. 2020;478(10):2257-2263. [DOI] [PMC free article] [PubMed]
- 44.Eberly LA, Khatana SA, Nathan AS, et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic. Circulation. 2020;142(5):510–2. [DOI] [PMC free article] [PubMed]
- 45.Campos-Castillo C, Anthony D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: A secondary analysis of a US survey of internet users from late March. J Am Med Inform Assoc. 2020;28(1):119–25. [DOI] [PMC free article] [PubMed]
- 46.Shah DA, Sall D, Peng W, Sharer R, Essary AC, Radhakrishnan P. Exploring the role of telehealth in providing equitable healthcare to the vulnerable patient population during COVID-19 [published online ahead of print, 2022 Jul 14]. J Telemed Telecare. 2022;1357633X221113711. [DOI] [PMC free article] [PubMed]
- 47.Pierce RP, Stevermer JJ. Disparities in the use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2023;29(1):3-9. [DOI] [PMC free article] [PubMed]
- 48.Ray KN, Chari AV, Engberg J, et al. Opportunity costs of ambulatory medical care in the United States. Am J Manag Care. 2015;21(8):567-574. [PMC free article] [PubMed]
- 49.Drake C, Lian T, Cameron B, et al. Understanding telemedicine's “New normal”: Variations in telemedicine use by Specialty Line and patient demographics. Telemed e-Health. 2022;28(1):51–9. [DOI] [PMC free article] [PubMed]
- 50.Frydman JL, Li W, Gelfman LP, et al. Telemedicine Uptake Among Older Adults During the COVID-19 Pandemic. Ann Intern Med. 2022;175(1):145-148. [DOI] [PMC free article] [PubMed]
- 51.Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med. 2020;180(10):1386. [DOI] [PMC free article] [PubMed]
- 52.Albritton J, Ortiz A, Wines R, et al. Video Teleconferencing for Disease Prevention, Diagnosis, and Treatment : A Rapid Review. Ann Intern Med. 2022;175(2):256-266. [DOI] [PubMed]
- 53.Telehealth interventions to improve chronic disease [Internet]. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; 2020. Available at: https://www.cdc.gov/dhdsp/pubs/telehealth.htm. Accessed 10 Jul 2022.
- 54.Reed ME, Huang J, Parikh R, et al. Patient-Provider Video Telemedicine Integrated With Clinical Care: Patient Experiences. Ann Intern Med. 2019;171(3):222-224. [DOI] [PubMed]
- 55.Reed ME, Huang J, Graetz I, et al. Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians. JAMA Netw Open. 2020;3(6):e205873. [DOI] [PMC free article] [PubMed]
- 56.Goodrich K. How the CARES Act supports America’s Healthcare System in the Fight against COVID 19. JW News; 2020. Available at: https://www.jdsupra.com/legalnews/how-the-cares-act-supports-america-s-59894/. Accessed 28 Jul 2022.
- 57.Medicare and Medicaid policies. Telehealth.hhs.gov;2021. Available at: https://telehealth.hhs.gov/providers/telehealth-policy/medicare-and-medicaid-policies. Accessed 28 Jul 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 744 kb)