Abstract
Digital technologies change the healthcare environment, with several studies suggesting barriers and facilitators to using digital interventions by healthcare professionals (HPs). We consolidated the evidence from existing systematic reviews mentioning barriers and facilitators for the use of digital health technologies by HP. Electronic searches were performed in five databases (Cochrane Database of Systematic Reviews, Embase®, Epistemonikos, MEDLINE®, and Scopus) from inception to March 2023. We included reviews that reported barriers or facilitators factors to use technology solutions among HP. We performed data abstraction, methodological assessment, and certainty of the evidence appraisal by at least two authors. Overall, we included 108 reviews involving physicians, pharmacists, and nurses were included. High-quality evidence suggested that infrastructure and technical barriers (Relative Frequency Occurrence [RFO] 6.4% [95% CI 2.9–14.1]), psychological and personal issues (RFO 5.3% [95% CI 2.2–12.7]), and concerns of increasing working hours or workload (RFO 3.9% [95% CI 1.5–10.1]) were common concerns reported by HPs. Likewise, high-quality evidence supports that training/educational programs, multisector incentives, and the perception of technology effectiveness facilitate the adoption of digital technologies by HPs (RFO 3.8% [95% CI 1.8–7.9]). Our findings showed that infrastructure and technical issues, psychological barriers, and workload-related concerns are relevant barriers to comprehensively and holistically adopting digital health technologies by HPs. Conversely, deploying training, evaluating HP’s perception of usefulness and willingness to use, and multi-stakeholders incentives are vital enablers to enhance the HP adoption of digital interventions.
Subject terms: Health occupations, Public health
Introduction
Recent developments in health technology have positively affected multiple and essential sectors of the economy, especially the healthcare sector, by providing solutions that guarantee the exchange of medical knowledge and information and establish long-lasting health outcomes1,2. Digital health technologies, such as wearables devices, computerized decision support systems, and telemedicine improve the technical performance and satisfaction of healthcare employees, demonstrate potential to decrease direct and indirect costs of medical services, and enhance the quality of delivered care3. Worldwide, using digital solutions in practice seems inevitable, with modality-specific prevalence (e.g., 50.8% for telemedicine, 89.9% for electronic health records, and 91.9% for social media platforms)4–6. However, the prevalence of use might be even higher, as no previous study has collated and assessed the overall prevalence of using digital health technologies by healthcare providers. Likewise, several studies have suggested that ethnicity, race, geographic location, age, and medical specialty directly interfere in the adoption of technology use, evidencing the importance of understanding variables accounting for the digital divide and disparity of access7–9.
Several barriers to healthcare’s overall quality, transparency, and efficiency naturally arise during or following the creation, implementation, and maintenance of digital health technologies. Therefore, during the design of any health-related project, it is essential to identify and quanti-qualitatively analyze its risks and facilitators, enhancing the likelihood of obtaining favorable outcomes and optimizing the chances of success. The efficient implementation of digital technologies, characterized by proper implementation of a systematic management approach, including strategic planning, resource allocation, and control and evaluation processes, is fundamental to refining healthcare services, equipment, and technologies10–12. In reaction to these aforementioned elements, multiple efforts have strengthened healthcare systems through employing DHTs for healthcare professionals and stakeholders from low-, middle-, and high-income countries. For instance, the World Health Organization (WHO) endorsed in the 73rd World Health Assembly the institution of the Global Strategy on Digital Health 2020–2025, in which four guiding principles rely on the acknowledgment that the institutionalization of digital health in a national system requires a decision and commitment by countries, recognition that successful digital technologies require an integrated strategy, promotion of the appropriate use of digital interventions for health, and recognition of the urgent need to address the major impediments faced by least-developed countries implementing digital health technologies13. Furthermore, the Regional Digital Health Action Plan for the WHO European Region 2023–2030 has a critical regional focus area on strengthening digital literacy skills and capacity-building in the general population, with particular attention to the health workforce, for the use of digital health services and disease prevention and management14. Due to these global actions, numerous studies have focused on assessing barriers to and facilitators for many technologies15–17.
To date, hundreds of clinical trials based on specific technologies applied to the healthcare professionals’ environments have assessed the implementation of digital interventions in the healthcare system, while several systematic reviews have combined these publications, evidencing their effectiveness, safety, and feasibility. However, a summary of enablers and restraints to healthcare professionals’ coordinated and integrated use of digital health technologies has not been published yet, making the current evidence dispersed, misused, and overlooked. Therefore, in this overview of systematic reviews and semantic-based occurrence meta-analysis, we report all published evidence from existing systematic reviews covering and mentioning barriers and facilitators to the solid use of digital health technologies by healthcare providers.
Results
Study selection and characteristics
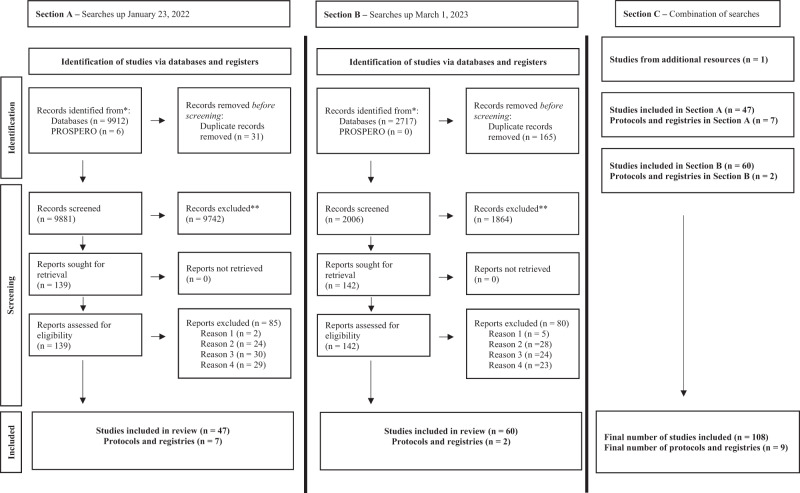
Our database and PROSPERO search are shown in Fig. 1. Our January 21, 2022 search retrieved 9,912 records, of which 139 underwent full-text review (Fig. 1, section A). Based on the inclusion and exclusion criteria, 47 studies and seven ongoing studies were included. On March 1, 2023, 2,717 new publications were identified through an additional database search (Fig. 1, section B). Of those, 142 studies were shortlisted for full-text assessment, and 60 reviews were added to our umbrella review. Two additional ongoing studies or protocols were identified. In total, this overview of systematic reviews included 108 primary systematic reviews and nine ongoing studies (Fig. 1, section C).18–125 One study was identified from alternative resources.64 Justification for the exclusion of 165 studies is presented in Supplementary Information 1 (pp 2–7). Included study characteristics are characterized in Table 1 and Table 2. One study is pending classification as it required translation. No additional data needed to be requested from the corresponding authors.
Fig. 1. PRISMA flow chart diagram.
Reason 1—wrong intervention or platform was unclear. Reason 2—the study did not provide any relevant outcome influencing healthcare providers. Reason 3—targeted population was not healthcare providers. Reason 4—study design used did not match our inclusion criteria.
Table 1.
Main characteristics of included studies evaluating the impact of digital health solutions on health workers (n = 108).
| Study ID | Publication Year | Journal | Number of Included Databases | Which Databases | Study Objective | Number of Included Studies |
|---|---|---|---|---|---|---|
| Adepoju 2017 | 2017 | JMIR mHealth uHealth | 5 | PubMed, CINAHL, Web of Science, Cochrane Library of Systematic Reviews, and Grey Literature | To synthesize evidence on the use of mHealth for point-of-care decision support and improved quality of care by health care workers in Africa | 22 |
| Addotey-Delove 2023 | 2023 | Int J Env. Res. and Public Health | 2 | PubMed and Scopus | To identify and examine empirical evidence to answer the research question “what factors have impacted (enabled or impeded) adoption of mHealth by healthcare workers in developing countries?” | 85 |
| Alkhaldi 2023 | 2023 | JMIR mHealth and uHealth | 4 | MEDLINE, Scopus, CINAHL, and PsycINFO | To classify and evaluate interventions aimed at encouraging HCPs to prescribe mHealth apps | 11 |
| Al Bawashdeh 2022 | 2022 | Sensors | 9 | Google Scholar, Science Direct, Emerald, Wiley, PubMed, Springer, MDPI, IEEE, and Scopus | To accumulate existing knowledge about the factors that influence medical professionals to adopt IoT applications in the healthcare sector | 22 |
| Agarwal 2015 | 2015 | Trop Med Int Health | 5 | MEDLINE, Embase, Global Health, Google Scholar, and Scopus | To review and synthesize the evidence on the feasibility and effectiveness of mobile-based services for healthcare delivery by front line health workers | 42 |
| Amoakoh-Coleman 2016 | 2016 | J Med Internet Res | 5 | Cochrane Library of Systematic Reviews, PubMed, Embase, Global Health Library, and PopLine | To evaluate the effectiveness of mHealth interventions targeting health care workers to improve maternal and neonatal outcomes in LMIC | 19 |
| Arsad 2023 | 2023 | J of Health Research | 5 | Ovid, Web Of Science, PubMed, SAGE and EBSCOhost | To identify and review the impact of eHealth applications (apps) on healthcare interventions | 10 |
| Aslani 2022 | 2022 | Int Cardiovascular Research Journal | 3 | PubMed, Scopus, and Web of Science | To identify the advantages and disadvantages of using telecardiology and to provide solutions for its successful implementation based on the obtained results | 30 |
| Avoka 2022 | 2022 | Trop Med Int Health | 4 | PubMed, Embase, Cochrane Register and CINAHL Plus | To review the evidence on interventions to improve obstetric emergency referral decision making, communication and feedback between health facilities in sub-Saharan Africa | 14 |
| Balusxkek 2022 | 2022 | BMC Health Services Research | 4 | MEDLINE, Embase, APA PsycINFO, and CINAHL | To identify and categorize challenges experienced and/or perceived by practitioners | 5 |
| Bervell 2019 | 2019 | Soc Sci Med | 6 | Google Scholar, Springer, Global Health, PubMed, IEEE Xplore, Science Direct | To provide an in-depth look at e-health and m-health utilization in SSA countries, together with the opportunities they offer and the challenges in their trends of usage | 61 |
| Boonstra 2010 | 2010 | BMC Heal Serv Res | 4 | Science, EBSCO, PubMed, and Cochrane Library of Systematic Reviews | To identify, categorize, and analyze barriers perceived by physicians to the adoption of EMRs in order to provide implementers with beneficial intervention options | 22 |
| Brommeyer 2023 | 2023 | Int J of Medical Informatics | 8 | Scopus, ProQuest, Web of Science, ACM Digital Library, CINAHL, PubMed, Google Scholar and ProQuest Dissertations | To present and discuss the findings from a scoping review identifying: 1) competencies required for health service managers leading the implementation and transformation of informatics and digital technology in the health sector; and 2) factors that are critical to building the management workforce capacity in the era of health informatics and digital health | 19 |
| Braun 2013 | 2013 | PLoS ONE | 7 | PubMed/MEDLINE, CAB Global Health, Web of Science, INSPEC, WHO publication database, Health UnBound Content Library, and Royal Tropical Institute Resource Database | To review the evidence for the use of mobile technology by community health workers to identify opportunities and challenges for strengthening health systems in resource-constrained settings | 25 |
| Brewster 2014 | 2014 | J Adv Nurs | 7 | Assia, AMED, British Nursing Index, CINAHL, Embase, MEDLINE, and Web of Knowledge | To synthesize qualitative and quantitative evidence of front-line staff acceptance of the use of telehealth technologies for the management of Chronic Obstructive Pulmonary Disease and Chronic Heart Failure | 10 |
| Brown 2020 | 2020 | J Clin Nurs | 5 | CINAHL, Embase, PsychINFO, MEDLINE, and PubMed | To evaluate and synthesize the evidence regarding the development of digital capability in nurses and the strategies that support effective integration of digital skills into the workplace | 17 |
| Calleja 2022 | 2022 | Rural and Remote Health | 6 | CINAHL, MEDLINE, Nursing & Allied Health (Proquest), PubMed, Joanna Briggs Institute Evidence Based Practice, and Embase | To determine the existence and characteristics of telehealth education in rural and remote setting; evaluate current telehealth education models and resources; establish the quality of education provided through telehealth along with the facilitators or enablers of a successful service; and develop recommendations for supporting and developing an education model for rural and remote health practitioners through telehealth | 60 |
| Cansdale 2022 | 2022 | BMJ Open | 3 | PubMed, CINAHL and Global Health | To evaluate which mHealth tools have been reported to birth outcomes in the delivering room in LMICs and document their reported advantages and drawbacks | 21 |
| Cartolovni 2022 | 2022 | Int J Med Inform | 6 | PubMed, Web of science, Ovid, Scopus, IEEE Xplore, EBSCO Search (Academic Search Premier, CINAHL, PSYCINFO, APA PsycArticles, ERIC) | To surface the underlying ethical and legal but also social implications (ELSI) that have been overlooked in recent reviews while deserving equal attention in the development stage, and certainly ahead of implementation in healthcare | 94 |
| Celes 2018 | 2018 | Pan American J of Public Health | 3 | Virtual Health Library, PubMed, and Google Scholar | To identify telehealth initiatives described in the literature as a strategy for national health policies | 21 |
| Cen 2022 | 2022 | BMJ Open | 6 | PubMed, Scopus, MEDLINE, Web of Science, ScienceDirect, and China National Knowledge Infrastructure | To determine how eHealth was adopted in pharmaceutical care (PC), the outcome reported and the contextual factors | 43 |
| Chan 2018 | 2018 | J. Med. Internet Res. | 4 | MEDLINE, Embase, CINAHL, and InfoSci Journals | To examine the utilization of SNSs for communication among health professionals in frontline clinical practice, professional networks, and education and training to identify areas for future health communication research | 33 |
| Chen 2022 | 2022 | Frontiers in Medicine | 4 | PubMed, Embase, IEEE Xplore, and Web of Science | To investigate clinical AI acceptance among physicians and medical students around the world to provide implementation guidance | 60 |
| Christensen 2020 | 2020 | J Psychiatr Ment Health Nurs | 8 | PubMed, Academic Search Premiere, CINHAL, Scopus, PyscINFO, Web of Science, Sociological Abstracts, and Embase | To conduct a systematic review of the existing research literature, focusing on patients’ and providers’ experiences of VCs used in the treatment of patients 60+ years with unipolar depression | 21 |
| da Costa 2020 | 2020 | Telemedicine. e-Health | 5 | PubMed/MEDLINE, Virtual Health Library, CINAHL, Scopus, and Web of Science | To collect information regarding the inclusion of the application of TD tools in the public dental health services | 24 |
| Davis 2014 | 2014 | Telemedicine. e-Health | 3 | MEDLINE, IEEE Xplore, and Compendex | To explore the acceptability and feasibility of RMT use in routine adult patient care, from the perspectives of primary care clinicians, administrators, and clinic staff | 15 |
| de Grood 2016 | 2016 | J Multidisc Healthcare | 3 | MEDLINE, Embase, and PsycINFO | To summarize the current literature identifying barriers and opportunities that facilitate adoption of e-health technology by physicians. | 74 |
| Drissi 2021 | 2021 | Telemedicine. e-Health | 5 | IEEE Xplore, ACM, ScienceDirect, Scopus, and PubMed | To identify available e-mental health interventions, reported in the literature, that are developed for HCWs during the COVID-19 pandemic | 11 |
| Dutta 2020 | 2020 | Medicine | 5 | PubMed, Web of Science, Scopus, Cochrane Library of Systematic Reviews, and ProQuest | To explore and identify the potential barriers perceived by physicians in the adoption of EMR | 26 |
| Early 2019 | 2019 | Health Promot Pract | 7 | Web of Science, CINAHL, PubMed, MEDLINE, Academic Search Complete, Cochrane Library of Systematic Reviews, and Google Scholar | To identify and describe over ten years of studies on the use, effectiveness, and potential of mHealth involving Community Health Workers | 64 |
| Ebneter 2022 | 2022 | Swiss Med Wkly | 4 | PubMed, MEDLINE, Cochrane Library of Systematic Reviews, and Scopus | To analyze the needs, elements of feasibility, and reasons for acceptance or possible barriers before the implementation of a telemedicine intervention in Switzerland | 31 |
| Emmett 2022 | 2022 | Journal of Clin Nursing | 7 | TRIP, CINAHL, EMCARE, MEDLINE, Scopus, PsychINFO, and EMBASE | To identify and explore the experiences of health professionals towards using mobile electrocardiogram (ECG) technology | 6 |
| Ferdousi 2021 | 2021 | Int Nurs Rev | 7 | MEDLINE, Embase, Cochrane Library of Systematic Reviews, CINAHL, Scopus, Web of Science and Farsi Databases | To evaluate the attitudes of Iranian nurses towards clinical information systems in nursing practice | 17 |
| Fletcher 2023 | 2023 | BMC Primary Care | 3 | MEDLINE, HMIC, and Web of Science | To identify the available evidence on the use of eCDS tools by health professionals in general practice in relation to their impact on workload and workflow | 95 |
| Ftouni 2022 | 2022 | BMC Med Inform Decis Mak | 7 | PubMed, Scopus, Web of Science, Academic Search Complete, CINAHL, Embase, and Science Direct | To explore the barriers and challenges of telemedicine use during the pandemic and to propose solutions for improving future use | |
| Gagnon 2012 | 2012 | J Med Syst | 14 | MEDLINE, Embase, CINAHL, Cochrane Library of Systematic Reviews, DARE, Biosis Previews, PsycINFO, Current Content, HSTAT, Dissertation Abstracts, ERIC, ProQuest, ISI Web of Knowledge, Latin American and Caribbean Health Sciences, Ingenta, and ISI Science Citation Index | To review factors that are positively or negatively associated with ICT adoption by healthcare professionals in clinical settings | 101 |
| Gagnon 2016 | 2016 | JAMIA | 4 | PubMed, Embase, CINHAL, and PsychInfo | To synthesize current knowledge of the factors influencing healthcare professional adoption of mobile health (m-health) applications. | 33 |
| Garvey 2022 | 2022 | JMIR Medical Informatics | 3 | MEDLINE, CINAHL, and the Cochrane Library of Systematic Reviews | To systematically identify research on provider competencies needed for the use of AI in clinical settings | 4 |
| Garavand 2022 | 2022 | Informatics in Medicine Unlocked | 4 | Web of Science, PubMed, Scopus, and Embase | To identify the behavioral factors influencing the acceptance of telemedicine technology among physicians in different contexts | 37 |
| Ghimire 2023 | 2023 | Int J Med Inform | 4 | PubMed, Scopus, Cochrane Library of Systematic Reviews, and Web of Science | To assess the practical implications of virtual prenatal care and identify the needs and experiences associated with it | 23 |
| Gonçalves R 2023 | 2023 | J Med Internet Res | 7 | MEDLINE, Embase, BIREME, IEEE Xplore, BVS, Google Scholar, and Grey literature | To assess evidence on health professionals’ perceptions of the usability of telehealth systems in primary care of individuals with hypertension and diabetes from the COVID-19 pandemic onward | 11 |
| Grant 2022 | 2022 | Australian J of Rural Health | 7 | Scopus, CINAHL, MEDLINE, PEDro, Speechbite, OTseeker and ScienceDirect | To identify the attitudes and perspectives of speech pathologists, occupational therapists and physiotherapists on using telehealth videoconferencing for service delivery to children with developmental delays | 14 |
| Hagstram 2022 | 2022 | J Med Internet Res | 3 | PubMed, CINAHL, and PsycINFO | To identify, categorize, and summarize knowledge about different stakeholders’ (e.g., children and adolescents, parents, HCPs, policy makers, and designers of patient portals or PAEHRs) views, use, and experiences of EHR access for children, adolescents, and parents. | 74 |
| Huang 2023 | 2023 | J Med Internet Res | 5 | PubMed, Scopus, PsycINFO, Embase, and CINAHL | To provide an overview of the research on the use of intelligent physical robots in health care through a systematic literature review, especially to identify its antecedents and consequences | 94 |
| Ionescu 2022 | 2022 | JAMIA | 8 | Embase, MEDLINE, Web of Science Core Collection, WHO GHL, SCIELO, CINAHL EBSCOhost, ERIC Ovid | To create an overview of what is currently known in the literature about the use and implementation of e-consultation and e-learning by HCWs in LMICs and whether there is evidence of complementarity in the joint use of these 2 tools | 96 |
| Isidori 2022 | 2022 | JMIR nursing | 3 | PubMed, Google Scholar, and Web of Science | To review and define the role of nurses and the skills they are asked to master in terms of new methodological approaches and digital knowledge that have emerged before and during the COVID-19 pandemic (2011-2021) | 60 |
| Ismatullaev 2022 | 2022 | Human Factors | 3 | IEEE Xplore, Springer Link and Google Scholar | To provide a comprehensive overview of the factors impacting technology adoption, to predict the acceptance of artificial intelligence (AI)-based technologies | 85 |
| Jacob 2020 | 2020 | JMIR mHealth and uHealth | 4 | MEDLINE, PubMed, Cochrane Library of Systematic Reviews, and the SAGE database | To systematically explore relevant published literature to synthesize the current understanding of the factors impacting clinicians’ adoption of mHealth tools, not only from a technological perspective but also from social and organizational perspectives | 171 |
| Jimenez 2020 | 2020 | Int J Med Inform | 4 | MEDLINE, Embase, CINAHL, and Cochrane Library of Systematic Reviews | To examine the broad literature on DHCs as it applies to Primary Care (PC) settings | 28 |
| Jimma 2022 | 2022 | Informatics in medicine unlocked | 4 | PubMed, Scopus, ProQuest, and Science Direct | To show the best available evidence associated with the obstacles to the acceptance of the electronic medical record system. | 21 |
| Joo 2022 | 2022 | Computers, Informatics, Nursing | 5 | CINAHL, Ovid, PubMed, PsycINFO, and Web of Science | To identify the strengths and weaknesses of nurse-led telehealth interventions for the care of community-dwelling outpatients during the COVID-19 pandemic. | 23 |
| Jonasdottir 2022 | 2022 | Int J Med Inform | 4 | Scopus, PubMed, ProQuest, and EBSCOhost | To answer the research question, “what is known in the literature about challenges and opportunities of telehealth service provision from the perspective of health professionals?“ | 22 |
| Jose 2023 | 2023 | Int J Environmental Research and Public Health | 3 | PubMed, Scopus, and Web of Science | To analyse the previous research related to the competence requirements when adopting Healthcare 4.0 technologies | 44 |
| Kane 2022 | 2022 | JMIR human factors | 3 | PubMed, Cairn, Ascodocpsy | To describe the uses of digital technologies at the time of COVID-19 and their impact on professional practices in psychiatry and mental health and to understand the place of digital technologies in the organizational adaptations linked to the COVID-19 epidemic, but also to identify how this specific context questions the modalities of care. | 61 |
| K Zhang 2022 | 2022 | J of Interprofessional Care | 6 | CIPE. PubMed, CINAHL, ERIC, PsycINFO, Cochrane Library of Systematic Reviews, and Google/Google Scholar | To identify the program features and areas of behavior change in healthcare professionals using e-learning | 32 |
| Keyworth 2018 | 2018 | BMC Med Inform Decis Mak | 6 | MEDLINE, Embase, CINAHL, PsycINFO, Web of Science, and Cochrane Library of Systematic Reviews | To identify interventions with a technological component that are successful at changing professional practice, to determine if and how such interventions are theory-based, and to examine barriers and facilitators to successful implementation | 69 |
| Koivunen 2018 | 2018 | Scand J Caring Sci | 6 | PubMed/MEDLINE, CINAHL, ProQuest, Web of Science, Scopus, Finnish Medic, and Ohtanen | To synthesize the best available research evidence on nursing professionals’ experiences of the facilitators and barriers to the use of online telehealth services in nursing practice | 25 |
| Kolla 2021 | 2021 | J Public Health Manage Pract | 2 | PubMed and Google Scholar | To conduct a scoping review on health informatics-based strategies for CHW-provider communication that aim to improve integration of CHWs into clinical settings; discuss their advantages, limitations, and future directions to maximize these strategies in the context of clinical care | 31 |
| Konnyu 2023 | 2023 | Obstetrics and gynecology | 6 | Medline (through PubMed), the Cochrane Register of Clinical T1ials, the Cochrane Database of Systematic Reviews, EMBASE, CINAHL, and Clinica!Ttials.gov | To systematically review patient, partner or family, and clinician perspectives, preferences, and experiences related to prenatal care visit schedules and televisits for routine prenatal care | 9 |
| Kruse 2022 | 2022 | J Med Internet Res | 4 | PubMed, CINAHL, Web of Science, and ScienceDirect | To examine physician burnout issues incident to the EHR prior to and during the first year of the COVID-19 pandemic by analyzing the literature from the last 5 years | 25 |
| Laar 2022 | 2022 | BMC Health Services Research | 6 | Medline, Scopus, PsychINFO, CINAHL and Cochrane Library, Google | To identify HCPs perspectives on barriers to, and facilitators of, mobile phone based SRH services and information in rural areas of LMICs from current literature. | 12 |
| Lam 2022 | 2022 | npj Nature | 4 | MEDLINE, Embase, Web of Science, and IEEE Xplore | To systematically review the literature and determine the ML techniques used for technical surgical skill assessment and identify challenges and barriers in the field | 66 |
| Lampickien˙e 2022 | 2022 | Life (Basel, Switzerland) | 3 | PubMed, Web of Science, and IEEE Xplore | To explore the existing literature concerning the user experience of digital care visits (telemedicine) from different healthcare professionals’ points of view | 28 |
| Li 2013 | 2013 | Interac J Med Res | 8 | MEDLINE, Cinahl, Web of Science, PubMed, PsychInfo, ERIC, ProQuest Science Journals, and Embase. | To identify and synthesize the factors influential to health care providers’ acceptance of various eHealth applications. | 93 |
| Li 2019 | 2019 | Telemedicine. e-Health | 11 | Cochrane Library of Systematic Reviews, Academic Search Premier, CINAHL, British Education Index, CDAS, CMMC, EA, LISTA, MEDLINE, MLA International Bibliography, and Web of Science | To critique and summarize existing research on ICU nurses’ perspectives toward the telemedicine intensive care unit (Tele-ICU). In addition to this, find evidence to support implementation of Tele-ICU program in China | 14 |
| Lluch 2011 | 2011 | Intl J Med Inform | 25 | Cochrane Library of Systematic Reviews, CSA Illumina, EBSCOHOST, JSTOR, Collections, ACM, ProQuest, Emerald Journals, Ingenta, PubMed, Science Direct, Google Scholar, EPPI Centre, CDR, Rand Corportation, Joanna Briggs Institute, NICE, SCIE, The Commonwealth Fund, CHSRF, Government sources, and think tanks | To identify and categorize, from an organizational management perspective, barriers to use of or ICT adoption for health and future policy interventions | 79 |
| Longhini 2022 | 2022 | J Med Internet Res | 4 | MEDLINE, CINAHL, PsycINFO, and Scopus | To summarize digital health competencies investigated to date and the tools used to assess them among health care professionals | 26 |
| Martin 2019 | 2019 | JAMIA | 7 | MEDLINE, PsycINFO, Embase, CINAHL Plus, HMIC, Cochrane Library of Systematic Reviews, and National Institute of Health Research HTA | To summarize the quality and breadth of evidence for the impact of mobile technologies on communication and teamwork in hospitals | 30 |
| Marvaso 2022 | 2022 | Applied Sciences (Switzerland) | 4 | Dimensions database, Embase, PubMed, and Web of Science | To provide a glance at the recent developments in augmented reality/virtual reality to support students’ education, personnel training and patients’ empowerment in this clinical setting | 41 |
| Meunier 2023 | 2023 | Annals of Family Medicine | 5 | PubMed, PsycInfo, Embase, CINAHL, and Cochrane Library of Systematic Reviews | To identify and quantify the barriers and facilitators to the use of CDSSs by primary care professionals | 48 |
| Moore 2020 | 2020 | JAMIA | 6 | Embase, MEDLINE, CINAHL, Scopus, PsycInfo, and Web of Science | To study the impact of health information technology on nurses’ time and to address the knowledge gap | 33 |
| Muhiyaddin 2020 | 2020 | Stud Health Technol Inform | 3 | CINAHL, PubMed, and Google Scholar | To explore the impact of the CDSS on physicians as reported through the literature | 14 |
| Mulita 2022 | 2022 | Sensors (Basel, Switzerland) | 2 | PubMed and Web of Science | To summarize the most important studies evaluating the internet of things concept within surgical practice, focusing on Telesurgery and surgical telementoring | 48 |
| Namasivayam 2022 | 2022 | PloS one | 7 | MEDLINE, CINAHL, Scopus, Web of Science Core Collection, Embase, PsycINFO, and Emcare | To review and map the available evidence on the use of telehealth in providing after-hours palliative care services in rural and remote Australia. | 12 |
| Nezamdoust 2022 | 2022 | Journal of Research in Nursing: JRN | 6 | Google Scholar, Scopus, Cochrane Library of Systematic Reviews, Embase, Ovid, and PubMed | To study the utilization of mobile health applications by nurses and presenting a scenario of how and why they are utilized | 25 |
| Nguyen 2021 | 2021 | JAMIA | 6 | MEDLINE, Embase, CINAHL, PsycINFO, ProQuest, and Web of Science | To assess the multilevel (organizational, physician, and information technology [IT]) factors associated with EHR-related impacts on physician well-being and burnout and to identify promising potential EHR improvements, as recommended by physicians | 35 |
| Niazkhani 2020 | 2020 | BMC Med Inform Decis Mak | 6 | MEDLINE, PubMed, Science Direct, CINAHL, CENTRAL, and IEEE | To identify the types of barriers to a patient, provider, and caregiver adoption/use of ePHRs and to analyze their extent in chronic disease care | 60 |
| Nizeyimana 2022 | 2022 | Digital health | 7 | PubMed, Scopus, PEDro, Cochrane library, EBSCOhost (Academic search premier, Africa-wide information, CINAHL, Eric, MEDLINE, Health sources - Nursing/Academic edition), Africa online, and ProQuest databases | To scope all published information reporting on the feasibility, cost, access to rehabilitation services, implementation processes including barriers and facilitators of telerehabilitation (TR) in low- and middle-income countries (LMICs) and high-income countries (HICs). | 29 |
| O’Connor 2022 | 2022 | Journal of Clinical Nursing | 4 | CINAHL, Embase, PubMed, and Scopus | To identify and summarize the scientific literature on AI in nursing and midwifery, to identify the extent of nurses and midwives’ involvement in the development, delivery, or use of AI in healthcare, to identify methods AI being employed across the nursing and midwifery professions in terms of clinical practice, education, research, and policy, to identify the benefits, limitations, and risks of AI in nursing and midwifery? | 140 |
| Odendaal 2020 | 2020 | Cochrane Database of Syst Rev | 13 | MEDLINE, Embase, CINAHL, SSCI, Global health, Eldis, Google Scholar, mHealth database, mHealth Evidence, mHealth Knowledge, mPowering, OpenGrey, and Grey Literature | To synthesize qualitative research evidence on health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services, and to develop hypotheses about why some technologies are more effective than others | 53 |
| Osman 2019 | 2019 | BMC Glob Health | 8 | MEDLINE, Embase, Cochrane Library of Systematic Reviews, CINAHL, PsycINFO, ProQuest, Conference Proceedings Citation Index, and Google search | To investigate factors (barriers and facilitators) influencing the adoption and implementation of electronic consultation (eConsult services) to enhance access to speacialist care | 130 |
| Papadopoulos 2018 | 2018 | Contemporary Nurse | 7 | MEDLINE, PubMed, CINHAL, Embase, PsycInfo, Web of Science, and IEEE Xplore | To provide an overview of the existing evidence related to the views of nurses and other health and social care workers about the use of assistive humanoid and animal-like robots | 19 |
| Police 2011 | 2011 | Inform Prim Care | 3 | MEDLINE, Embase, and Grey Literature | To better understand current utilization rates along with benefits and barriers to HIT adoption in physician practice organizations | 119 |
| Prakash 2022 | 2022 | J of Personalized Medicine | 2 | PubMed and Google Scholar | To scrutinize the ethical complications associated with the application of artificial intelligence in the healthcare field | 16 |
| Rahal 2021 | 2021 | BMC Med Inform Decis Mak | 4 | MEDLINE, PsycINFO, Embase, and PROSPERO | To explore and identify the factors that impact Primary Care Physcians’ mature use of EMR | 14 |
| Ramachandran 2023 | 2023 | Heart and Lung | 9 | PubMed, Embase, CINAHL, Cochrane Library of Systematic Reviews, Scopus, PsycINFO, Web of Science, ERIC, and Proquest Dissertations and Theses Global | To summarize patient- and healthcare provider-level barriers and facil- itators in the adoption of DHIs for COPD management | 27 |
| Ratshidi 2022 | 2022 | Sustainability | 7 | Scopus, PubMed, Web of Science, Science direct, Google, Google scholar, CHW Central website | To conceptualise the social factors to consider when implementing a bespoke ICT solution suited to the specific demands of CHWs in primary healthcare in developing contexts, with a particular focus on the South African context | 59 |
| Rukavina 2021 | 2021 | J. Med. Internet Res. | 3 | PubMed, CINAHL, and Scopus | The purpose of this scoping review is to characterize the recent original peer-reviewed research studies on the e-professionalism of HCPs; to assess the quality of the methodologies and approaches used; to explore the impact of SM on e-professionalism of HCPs; to recognize the benefits and dangers of SM; and to provide insights to guide future research in this area | 88 |
| Saigí-Rubió 2022 | 2022 | J Med Internet Res | 5 | PubMed, Embase, Web of Science, Cochrane Library of Systematic Reviews, and Scopus | To summarize findings regarding the use of telemedicine across the 53 member states of the WHO European Region and to identify the medical fields and levels of care in and at which the effectiveness, feasibility, and applicability of telemedicine have been demonstrated | 33 |
| Sipanoun 2022 | 2022 | Int J of Med Inform | 8 | Embase, EMCARE, MEDLINE, Cochrane Library, Web of Science, Scopus, CINAHL and PsycINFO | To understand the experiences and perceptions of all relevant stakeholders using an EMR system in the pediatric hospital setting, including the use of an EMR-linked patient portal | 36 |
| Sullivan 2022 | 2022 | Social Work in Public Health | 5 | Google Scholar, VA Library Network, JSTOR, PubMed, ERIC via EBSCOhost | To assess the current responses from the field of social work during the COVID-19 pandemic, leveraging telemedicine, social work, self-care, and the fluidity of VA services | 10 |
| Tabaeeian 2022 | 2022 | J of Science and Technology Policy Management | 2 | Scopus and PubMed | To identify barriers to the use of telemedicine systems in primary health-care individual level among professionals | 37 |
| Tegegne 2023 | 2023 | Interactive J of Medical Research | 6 | PubMed, Web of science, African journals OnLine, EMBASE, Medline, Scopus | To determine the pooled estimate of EMR use and success determinants among health professionals in Ethiopia. | 5 |
| Tickner 2023 | 2023 | Social work in health care | 7 | CINAHL, Embase, Medline, PsycINFO, Scopus, Social Work Abstracts and Sociological Source Ultimate | To explore what is known about the use of eHealth technologies in health social work practice | 25 |
| Torres-Castaño 2023 | 2023 | Int J Environmental Research and Public Health | 2 | MEDLINE and Embase | To identify the impact of the ELSI dimensions and other dimensions, such as the organizational and environmental, to analyze in depth the challenges of the implementation of teleneurology as a complement to face-to-face neurology care | 53 |
| Poissant 2005 | 2005 | JAMIA | 4 | MEDLINE, CINAHL, HealthSTAR, and Current Health | To estimate the extent to which an Electronic Health Records affects clinicians’ documentation time and to identify factors that may explain efficiency differences observed across studies | 23 |
| Thomas-Craig 2021 | 2021 | JAMIA | 4 | MEDLINE, Embase, Cochrane Library of Systematic Reviews, and ACM | To identify and summarize interventions used to address the burden of digital tools and their impact on workflow inefficiencies | 81 |
| Vejdani 2022 | 2022 | BMC Med Inform Decis Mak | 4 | Web of Science, PubMed, Scopus, and ProQuest | To identify the requirements of the electronic prescribing system | 13 |
| Verma 2022 | 2022 | BJGP Open | 2 | PubMed and PsychInfo | To synthesize data on patients’ and PCPs’ experiences with remote consultations in the primary care setting to inform future research and policy in this area | 24 |
| von Wedel 2020 | 2020 | J Med Internet Res | 2 | PubMed and Google Scholar | To provide a comprehensive overview including a variety of technologies beyond computer-based patient records | 50 |
| Walle 2023 | 2023 | Informatics in Medicine Unlocked | 8 | MedLine, PubMed, Scopus, EMBASE, African Journal Online, HINARI, Science Direct, Web of science | To identify the pooled levels of readiness to use EMRs and associated factors among health professionals in Ethiopia | 3 |
| Walsh 2021 | 2021 | Clinical Ophthalmology | 5 | Embase, PubMed, Web of Science, Google Scholar, Google | To conduct a systematic review identifying, describing and contrasting teleophthalmology services in NZ with the comparable countries of Australia, USA, Canada and the United Kingdom | 132 |
| Wisner 2019 | 2019 | Int J Nurs Stud | 5 | MEDLINE/PubMed, CINAHL, Embase, Web of Science, and PsycINFO | To synthesize the literature on the electronic health record’s impact on nurses’ cognitive work | 18 |
| Xyrichis 2021 | 2021 | Cochrane Database of Syst Rev | 4 | MEDLINE, Embase, CINAHL, and Web of Science | To identify, appraise and synthesize qualitative research evidence on healthcare stakeholders’ perceptions and experiences of factors affecting the implementation of CCT, and to identify factors that are more likely to ensure successful implementation of CCT for subsequent consideration and assessment in telemedicine effectiveness reviews | 13 |
| Young 2011 | 2011 | Chest | 5 | PubMed, CINAHL, Global Health, Web of Science, and Cochrane Library of Systematic Reviews | To systematically evaluate the published and unpublished literature addressing the acceptance of tele-ICU coverage by ICU staff with a focus on benefits and challenges seen by frontline providers in adopting this new technology | 23 |
| Zakerabasali 2021 | 2021 | Healthc Informatics Res | 4 | PubMed, Embase, Web of Science, and Google Scholar | To conduct a systematic review of more recent literature on barriers associated with mHealth reported by healthcare professionals and identify the most important barriers | 18 |
| Zhang J 2023 | 2023 | Int Orthopaedics | 3 | PubMed MEDLINE, Ovid EMBASE and Scopus. | To identify the type of XR most frequently used in various surgical specialties and phases of surgical intervention, identify key outcome measures and trends for the use of XR in surgery, determine if XR has been a promising addition to surgery, and which aspect of surgical practice has benefited the most, and to identify opportunities and challenges for XR development and usage in the future | 168 |
| Zhang Z 2023 | 2023 | JMIR Medical Informatics | 6 | ACM Digital Library, Cochrane Library, IEEE Xplore, Ovid MEDLINE, Embase, and Web of Science | To synthesize the knowledge and experiences of smart glasses, understand the benefits and limitations regarding adopting smart glasses as a telemedicine tool, and inform the design of future smart glass applications to better support remote care coordination | 21 |
| Protocols registered and identified | Protocol objective | |||||
| Abreu 2018 | 2018 | PROSPERO | N/A | To understand the use and impact of mHealth by community health workers in developing and least developed countries | N/A | |
| Bajgain 2023 | 2023 | BMJ open | 6 | To map and synthesize determinants (barriers and facilitators) to implementing AI-based CDS tools in healthcare. | N/A | |
| Cherifi 2021 | 2021 | PROSPERO | N/A | To evaluate what are the barriers and enablers to implementing TD with dental healthcare professionals | N/A | |
| Jacques 2019 | 2019 | PROSPERO | N/A | To answer the question: “Does the scientific evidence available in the literature demonstrate the effectiveness of the use of web applications to promote the mental health of health workers?” | N/A | |
| Luangphituck 2023 | 2023 | JMIR research protocols | N/A | To synthesize the best available evidence concerning the preventive effect of internet-based cognitive behavior therapy on employees | N/A | |
| Mahmood 2018 | 2018 | PROSPERO | N/A | To answer the question: “What are the various community health worker-based mobile health approaches to improve the management and knowledge/perception of caregivers regarding common childhood infections?” | N/A | |
| Mbuthia 2018 | 2018 | PROSPERO | N/A | To understand how m-Health communication strengthen postnatal care in rural areas | N/A | |
| Park 2020 | 2020 | PROSPERO | N/A | To analyze how effective is m-Health intervention in reducing the burden of caregivers of dementia patients | N/A | |
| Wootton 2011 | 2011 | BMC Health Ser. Res. | N/A | Estimate the travel reduction associated with the use of telemedicine by patients and healthcare professionals | N/A | |
ACM Association for Computing Machinery, AHRQ Agency for Healthcare Research and Quality, AMED Allied and Complementary Medicine Database, ASSIA Applied Social Sciences Index and Abstracts, CCT Critical Care Telemedicine, CDAS Child Development & Adolescent Studies, CDR York Centre for Reviews and Dissemination, CDSS Clinical Decision Support System, CENTRAL Cochrane Central Register of Controlled Trials, CHF Chronic Heart Failure, CHSRF Canadian Health Services Research Foundation, CHW Community Health Worker, CINAHL Cumulative Index to Nursing and Allied Health Literature, CMMC Communication & Mass Media Complete, COPD Chronic Obstructive Pulmonary Disease, DARE Database of Abstract of Reviews of Effectiveness, EA Education Abstracts [H.W. Wilson], EHI Electronic Health Information, EMR Electronic medical record, HCP Health Care Professionals, HCW Health Care Worker, HMIC Healthcare Management Information Consortium, HSRProj Health Services Research Projects in Progress, HSTAT Health Services, Technology, Assessment Text, HTA Health Technology Assessment, ICT Information Communication Technology, ICTRP International Clinical Trials Registry Platform, ICU Intensive Care Unit, INSPEC Database for Engineering Researchers, LISA Library and Information Science Abstracts, LISTA Library, Information Science, & Technology Abstracts, LMIC Low- and middle-income countries, NHS National Health System, NICE National Institute for Health and Clinical Excellence, PopLine Database Database from the University of London, RMT Remote Monitoring Technology, SCIE Social Care Institute for Excellence, SNS Social Network Sites, SSCIE Social Sciences Citation Index Expanded, SSSCI Science and Social Science Citation Indices, TD Teledentistry, UK United Kingdom, VC Video Consultations, WHO World Health Organization.
*In the abstract of the referred review it is stated the inclusion of 15 databases; however, there is a description of only 13 databases (value considered correct).
Table 2.
Population being evaluated, studies’ methodologies and technologies being evaluated.
| Study ID | Targeted health workers | Number of health workers | Study Designs Included | Technology under investigation | Geographic region | Disease or Condition Considered (Based on the ICD-10) |
|---|---|---|---|---|---|---|
| Addotey-Delove 2023 | Healthcare professionals in general | N/A | Quantitative studies | 1. m-Health technologies | African, Asian, and Latin American regions | N/A |
| Adepoju 2017 | Community health workers, nurses, clinicians, clinical officers, and healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. CDSS | African region | Maternal and prenatal health, childhood illness, tuberculosis, HIV, and Hypertension |
| Alkhaldi 2023 | Healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. m-Health technologies | European and North American regions, and Australia | N/A |
| Al-Rawashdeh 2022 | Healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. Internet of things | Asian, European, and Latin American regions | N/A |
| Agarwal 2015 | Frontline health workers, midwives, nurses, and outpatient health care workers | N/A | Qualitative studies | 1. m-Health technologies | African, Asian, and Latin American regions | Anemia, tuberculosis, drug-dosing, pre- and post-natal care, family planning, postpartum hemorrhage, and HIV |
| Amoakoh-Coleman 2016 | Healthcare professionals in general, community health workers, health surveillance assistants, and midwives | N/A | Qualitative and quantitative studies | 1. m-Health technologies | African and Asian regions | Maternal health, HIV, post-natal depression, and malaria in pregnancy |
| Arsad 2023 | General practitioners and healthcare professionals in general | 1130 | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. eHealth technologies | Asian and European regions | N/A |
| Aslani 2022 | Physicians and nurses | N/A | Quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | Asian, European, and Latin and North American regions | Cardiovascular diseases |
| Avoka 2022 | Healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. m-Health technologies | African region | Maternal health |
| Baluszek 2022 | Healthcare professionals in general | N/A | Qualitative and mixed methods study | 1. Telehealth, telemedicine, telemonitoring and remote monitoring technologies | European region | N/A |
| Bervell 2019 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1. m-Health technologies 2. Electronic medical records and clinical information systems 3. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 4. e-Health technologies |
African region | Infectious, cardiovascular, and oral diseases |
| Boonstra 2010 | Physicians | 25624 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Electronic medical records and clinical information systems | European region | N/A |
| Brommeyer 2023 | Healthcare professionals in general | N/A | Qualitative and quantitative studies | 1. Electronic medical records and clinical information systems | Asian, European, and Latin and North American regions, and Australia | N/A |
| Braun 2013 | Community health workers | N/A | Qualitative and quantitative studies | 1. m-Health technologies | African, Asian, and Latin American regions | Sexual, reproductive, maternal illnesses, child health, HIV, tuberculosis, and malaria |
| Brewster 2014 | Front-line professionals | 228 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | European region and Australia | COPD and CHF |
| Brown 2020 | Nurses | 41176 | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1. Electronic medical records and clinical information systems 2. m-Health technologies |
African, Asian, European, and Latin and North American regions, and Australia | N/A |
| Calleja 2022 | Healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | African, Asian, European, Latin and North American regions, and Australia | N/A |
| Cansdale 2022 | Nurses, birth attendants, and community health workers | 1486 | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. m-Health technologies | African, Asian, and Latin American regions | Neonatology |
| Cartolovni 2022 | Healthcare professionals in general | N/A | Original research | 1. eHealth technologies | Asian, European, and North American regions, and Australia | N/A |
| Celes 2018 | Healthcare profesionals in general | N/A | Quantitative studies | 1. Telehealth, telemedicine, telemonitoring and remote monitoring technologies | African, Asian, European, Latin and North American regions, and Australia | N/A |
| Cen 2022 | Pharmacists | N/A | Quantitative and qualitative studies | 1. eHealth technologies | Asian, European, and North American regions, and Australia | N/A |
| Chan 2018 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Social media network platforms | N/A | N/A |
| Chen 2022 | Physicians and healthcare professionals in general | 14049* | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. Artificial intelligence | Asian, European, Latin and North American regions, and Australia and New Zealand | N/A |
| Christensen 2020 | Mental health practitioners | N/A | Quantitative and qualitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | Asian and European regions, and Australia | Unipolar depression |
| Da Costa 2020 | Dental health services providers | N/A | Quantitative, qualitative, mixed qualitative-quantitative studies, and economic analysis | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | Asian, European, and Latin and North America regions, and Australia | Dental health conditions |
| Davis 2014 | Primary care professionals, medical assistants, clinicians, consultants, and healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | Asian, European, and North American regions | Diabetes, cardiac diseases, lung diseases, and cancers |
| de Grood 2016 | Physicians | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1. Electronic medical records and clinical information systems 2. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies |
North American region | N/A |
| Drissi 2021 | Healthcare professionals in general | N/A | N/A |
1. Social media network platforms 2. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 3. m-Health technologies |
Asian, European, and North American regions | Post-traumatic stress disorder, anxiety, and stress |
| Dutta 2020 | Physicians | N/A | N/A | 1. Electronic medical records and clinical information systems | African, Asian, and North American regions | N/A |
| Early 2019 | Community health workers | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. m-Health technologies | African and Latin and North American regions, and Australia | Maternal, child, and reproductive health, tuberculosis, and HIV |
| Ebneter 2022 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | European region | Palliative care |
| Emmett 2022 | Healthcare professionals in general | 111 | Qualitative and mixed qualitative-quantitative studies studies | 1. m-Health technologies | Australia | Cardiovascular diseases |
| Ferdousi 2021 | Nurses | 3989 | Quantitative and qualitative studies | 1. Electronic medical records and clinical information systems | Asian region | N/A |
| Fletcher 2023 | Healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. CDSS | African, Asian, European, North American regions, and Australia | Miscellaneous (oncology, cardiology, infectious diseases, and others) |
| Ftouni 2022 | Healthcare professionals in general | N/A | Quantitative and qualitative studies | 1.Telehealth, telemedicine, telemonitoring and remote monitoring technologies | African, Asian, European, Latin and North American regions | N/A |
| Gagnon 2012 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1. Electronic medical records and clinical information systems 2. m-Health technologies 3. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 4. CDSS 5. Clinical reminder and alert systems 6. Laboratory reporting system 7. Personal Digital Assistant 8. Clinical information systems 9. E-learning |
European and North American regions, and Australia | N/A |
| Gagnon 2016 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1. m-Health technologies 2. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies |
African, Asian, and European regions, and Australia | N/A |
| Garavand 2022 | Physicians | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. Telemedicine, telehealth, telemonitoring and remote monitoring technologies | African, Asian, European, and North and Latin American regions | N/A |
| Garvey 2022 | Healthcare professionals in general | 22 | Quantitative studies | 1. Artificial intelligence | North American region | N/A |
| Ghimire 2023 | Healthcare professionals in general | 51 | Quantitative and Qualitative | 1. Telemedicine, telehealth, telemonitoring and remote monitoring technologies | Asian, European, and North American regions | Pregnancy and maternal health |
| Gonçalves R 2023 | Healthcare professionals in general | 248 | Quantitative and qualitative studies | 1. Telemedicine, telehealth, telemonitoring and remote monitoring technologies | Asian, European, and Latin and North American regions, and Australia | Chronic diseases (including DM and hypertension) |
| Grant 2022 | Speech pathologists, Occupational therapists and Physiotherapists | N/A | Quantitative, Qualitative, and mixed qualitative-quantitative studies | Telemedicine, telehealth, telemonitoring and remote monitoring technologies | North American and Australian region | Children with Developmental delays |
| Hagstram 2022 | Healthcare professionals in general | 496 | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. Electronic medical records and clinical information systems | European and North American regions, and Australia | Pediatrics |
| Huang 2023 | Healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies | 1. Intelligent Physical Robots | N/A | N/A |
| Ionescu 2022 | Healthcare professionals in general | N/A | Qualitative, quantitative, and mixed qualitative-quantitative studies |
1. E-learning 2. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 3. Electronic medical records and clinical information systems |
African, Asian, and Latin American regions | Maternal health, infectious diseases, such as HIV/AIDs, and tuberculosis |
| Isidori 2022 | Nurses | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | N/A | N/A |
| Ismatullaev 2022 | Healthcare professionals in general | N/A | N/A | 1. Artificial intelligence | N/A | N/A |
| Jacob 2020 | Physicians | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. mHealth technologies | African, Asian, European, North and Latin America, and Australia and New Zealand | Miscellaneous (acute diseases, diabetes, mental disorders, and others) |
| Jimenez 2020 | Primary healthcare professionals | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1.Electronic medical records and clinical information systems 2.Telehealth, telemedicine, telemonitoring and remote monitoring technologies 3. mHealth technologies 4. Personal Digital assisstant |
African, European, North American regions, and Australian region | N/A |
| Jimma 2022 | Physicians and nurses | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Electronic medical records and clinical ainformation systems | African, Asian, European and North American regions | N/A |
| Joo 2022 | Nurses | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | Asian, European, and North American regions, and Australia and New Zealand | Cardiovascular disease and oncology |
| Jonasdottir 2022 | Healthcare professionals in general | N/A | Qualitative, Quantitative and mixed qualitative - quantitative studies | 1. Telehealth, telemedicine, telemonitoring and remote monitoring technologies | African, Asian, European, North American regions, and Australia | N/A |
| Jose 2023 | Healthcare professionals in general | N/A | Quantitative and qualitative studies |
1. mHealth technologies 2. Telehealth, telemedicine, telemonitoring and remote monitoring technologies 3. Electronics medical records and clinical information systems |
N/A | N/A |
| Kane 2022 | Health care professionals, Psychiatrist, Community Health | N/A | Qualitative and Quantitative studies |
1. Telehealth, telemedicine, telemonitoring and remote monitoring technologies 2. mHealth technologies 3. Social media network platforms 4. Artificial intelligence |
African, Asian, European, North American regions, and Australian region | Psychiatry and Mental health |
| K. Zhang 2022 | Healthcare professionals in general | 35542 | Qualitative, Quantitative and mixed qualitative - quantitative studies |
1. E-Learning 2. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 3. Social media network platforms 4. mHealth technologies |
North American region and Australian region | N/A |
| Keyworth 2018 | Healthcare professionals in general | N/A | Quantitative, qualitative, mixed qualitative-quantitative studies | 1. e-Health technologies | European and North American regions, and Australia | N/A |
| Koivunen 2018 | Healthcare professionals in general | 364 | Qualitative and mixed methods studies |
1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 2. m-Health technologies |
N/A | N/A |
| Kolla 2021 | Community health workers | N/A | Quantitative, qualitative, mixed qualitative-quantitative studies |
1. Electronic medical records and clinical information systems 2. m-Health technologies 3. Cloud- and web-based systems |
North American region | N/A |
| Konnyu 2023 | Healthcare professionals in general | 674 | Qualitative studies | Telehealth, telemedicine, telemonitoring and remote monitoring technologies | European and North American region | N/A |
| Kruse 2022 | Physicians | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Electronic medical record and clinical information systems | N/A | Mental Health |
| Laar 2022 | Health workers, Community health workers, Health care providers in general, Nurses | N/A | Qualitative studies | 1. mHealth technologies | Asian regions | Sexual and reproductive health |
| Lam 2022 | Surgeons | 1603 | Quantitative studies | 1. Artificial intelligence | African, Asian, European, North American regions, and Australia | N/A |
| Lampickienė 2022 | Mental health professionals, physicians, surgeons, Nurses | N/A | Quantitative, qualitative, mixed qualitative-quantitative studies, and review | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | European and North American regions, and Australia | N/A |
| Li 2013 | Healthcare professionals in general | N/A | Qualitative and quantitative studies |
1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 2. Electronic medical records and clinical information systems |
Australia | N/A |
| Li 2019 | Nurses | 2106 | Qualitative and quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | Asian region | Critical care conditions |
| Lluch 2011 | Healthcare professionals in general | N/A | Quantitative, qualitative, mixed qualitative-quantitative studies |
1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 2. Electronic medical records and clinical information systems |
N/A | N/A |
| Longhini 2022 | Healthcare professionals in general | 17143 | Quantitative, qualitative, mixed qualitative-quantitative studies | 1. e-Health technologies | African, Asian, European, and North American regions | N/A |
| Martin 2019 | Physicians and nurses | > 3705 | Qualitative and quantitative studies | 1. m-Health technologies | Asian, European, and North American regions, and Australia/New Zealand | N/A |
| Marvaso 2022 | Radiotherapy, RT students, Medical Physics | N/A | Survey | 1. Virtual reality or augmentative Reality | N/A | Radiotherapy |
| Meunier 2023 | Primary Care physicians and nurses | 59 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. CDSS | African, Asian, European, and Latin and North American regions, and Australia | N/A |
| Moore 2020 | Nurses | N/A | Qualitative and quantitative studies | 1. Electronic medical records and clinical information systems | Asian, European, and Latin and North American regions, and Australia | N/A |
| Muhiyaddin 2020 | Physicians | N/A | N/A | 1. CDSS | N/A | N/A |
| Mulita 2022 | Healthcare professionals in general | 757 | Quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | N/A | Surgical field |
| Namasivayam 2022 | Healthcare professionals in general | 46 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | Australian region | Palliative care |
| Nezamdoust 2022 | Nurses | N/A | N/A | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | African, Asian, European, Latin and North American regions, and Australia | N/A |
| Nguyen 2021 | Physicians | 30182 | Quantitative, qualitative, mixed qualitative-quantitative studies | 1. Electronic medical records and clinical information systems | North American region | N/A |
| Niazkhani 2020 | Healthcare professionals in general | Quantitative, qualitative, mixed qualitative-quantitative studies | 1. Electronic medical records and clinical information systems | European and Latin and North American regions, and Australia/New Zealand | Chronic conditions (such as diabetes, cystic fibrosis, arthritis, hypertension, multiple sclerosis, asthma, and CHF) | |
| Nizeyimana 2022 | Health professionals in general | N/A | Quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | African, Asian, European, North American regions, and Australia | N/A |
| O’Connor 2022 | Nurses, and midwives | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1. CDSS 2. Artificial intelligence |
Asian, European and Latin and North American regions, and Australia | Maternal and child Health, mental diseases |
| Odendaal 2020 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. m-Health technologies | African, Asian, European, and Latin and North American regions, and Australia | NA |
| Osman 2019 | Physicians | 82420 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | European and Latin and North American regions | N/A |
| Papadopoulos 2018 | Nurses and social care workers | >1545 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Assistive humanoid and animal-like robots | Asian, European, and North American regions, and Australia and New Zealand | Mostly neurological conditions (including dementia) |
| Police 2011 | Physician | 28217 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Electronic medical record and clinical information systems | North American region | N/A |
| Poissant 2005 | Nurses and physicians | 328 | Quantitative and qualitative studies | 1. Electronic medical records and clinical information systems | Countries were not reported | N/A |
| Prakash 2022 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Artificial intelligence | N/A | N/A |
| Rahal 2021 | Physicians | 106876 | Quantitative and qualitative studies | 1. Electronic medical records and clinical information systems | European and North American regions, and Australia/New Zealand | N/A |
| Ramachandran 2023 | Healthcare professionals in general and patients | 390 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | European region | COPD |
| Ratshidi 2022 | Community healthcare professionals | N/A | Quantitative, Qualitative and mixed qualitative-quantitative studies | 1. mHealth technologies | Asian, African, Latin and North American region | N/A |
| Rukavina 2021 | Healthcare professionals in general | 98 | N/A | 1. Social media network platforms | N/A | N/A |
| Saigí-Rubió 2022 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | European Region | N/A |
| Sipanoun 2022 | Overall users, including health professionals | 1638 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Electronic medical records and clinical information systems | Asian, European, and North American regions, and Australia | Pediatrics |
| Sullivan 2022 | Healthcare professionals in general | N/A | Qualitative and quantitative methods | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | North American region | N/A |
| Tabaeeian 2022 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | European, North American regions, Latin American and Australia | N/A |
| Tegegne 2023 | Health professionals in general | 2439 | Quantitative and qualitative studies | 1. Electronic medical records and clinical information systems | African region | N/A |
| Thomas Craig 2021 | Physicians | 9791 | Quantitative and qualitative studies |
1. CDSS 2. Electronic medical records and clinical information systems |
European and North American regions | Burnout |
| Tickner 2023 | Healthcare social workers | 2599 | Qualitative and quantitative studies |
m-Health technologies 2. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies |
European and North American regions, and Australia | N/A |
| Torres-Castaño 2023 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | African, European, and North American regions, and Australia | Neurology |
| Vejdani 2022 | Healthcare professionals in general | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Electronic medical records and clinical information systems | Asian, European, and North American regions | N/A |
| Verma 2022 | Patients and Physicians | N/A | Quantitative, qualitative studies | 1. Telehealth, telemedicine, telemonitoring and remote monitoring technologies | Asia, Europe, North American and Australia | N/A |
| von Wedel 2020 | Physicians | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies |
1. Electronic medical records and clinical information systems 2. CDSS 3. Advanced and business analytics 4. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies |
Asian, European, and Latin and North American regions, and Australia | N/A |
| Walle 2023 | Healthcare professionals in general | 1786 | Quantitative studies | 1. Electronic medical records and clinical information systems | African region | N/A |
| Walsh 2021 | Ophthalmologists | N/A | N/A | 1. Telehealth, Telemedicine, telemonitoring and remote monitoring technologies | European, and North American regions, and Australia and New Zealand | |
| Wisner 2019 | Nurses and physicians | N/A | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Electronic medical records and clinical information systems | European and North American regions, and Australia | N/A |
| Xyrichis 2021 | Healthcare professionals in general | 268 | Quantitative and qualitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | North American region | N/A |
| Young 2011 | ICU staff | > 1325 | Quantitative, qualitative, and mixed qualitative-quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | N/A | N/A |
| Zakerabasali 2021 | Healthcare professionals in general | N/A | Qualitative and quantitative studies | 1. m-Health technologies | African, European, and North American regions, and Australia and New Zealand | N/A |
| Zhang J 2023 | Surgical trainees or qualified surgeons of any surgical specialty | N/A | Quantitative studies | 1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies | N/A | Surgical field |
| Zhang Z 2023 | Healthcare professionals in general | N/A | N/A |
1. Telehealth, telemedicine, telemonitoring, and remote monitoring technologies 2. e-Health technologies |
N/A | N/A |
CDSS Computerized Decision Support Systems, HIV Human Immunodeficiency Virus, ICD-10 International Classification of Diseases, 10th version, ICU Intensive Care Unit, m-Health mobile health technologies, N/A Not applicable or not available.
Few studies (n = 20; 18.5%) initially targeted evaluating the creation, implementation, long-lasting use, and self-reported barriers and facilitators to using digital health technologies by healthcare professionals25,27,29,43,45,51,66,68,70,72–74,82,86,93,96,98,101,107,120. Thus, the remaining reviews were cautiously evaluated in order to identify a report of any barrier or facilitator to using digital health technologies by healthcare workers. Included reviews were heterogeneous in terms of the digital health technologies being assessed (e.g., alert systems, clinical reminders applications, computerized clinical decision support systems, electronic documentation systems, mobile health applications, social media platforms, and telemedicine tools) and enrolling different healthcare professionals (e.g., general practitioners and specialists, nurses, pharmacists, community healthcare workers) at several levels of care (primary, secondary, and tertiary health facilities).
Most reviews (n = 63; 58.3%) were executed in North America, Europe (n = 61; 56.4%), and Asia (n = 50; 46.2%). Thirty-three reviews suggested barriers and facilitators in the African territory (30.5%), while 28 reported data from Latin American and Caribbean regions (25.9%). Our study involved reviews from low- (e.g., Kenya, Rwanda, Uganda, and Ghana), middle- (e.g., Brazil, China, Russia, South Africa, and India), and high-income countries (e.g., Japan, the Czech Republic, United States of America, and Australia).
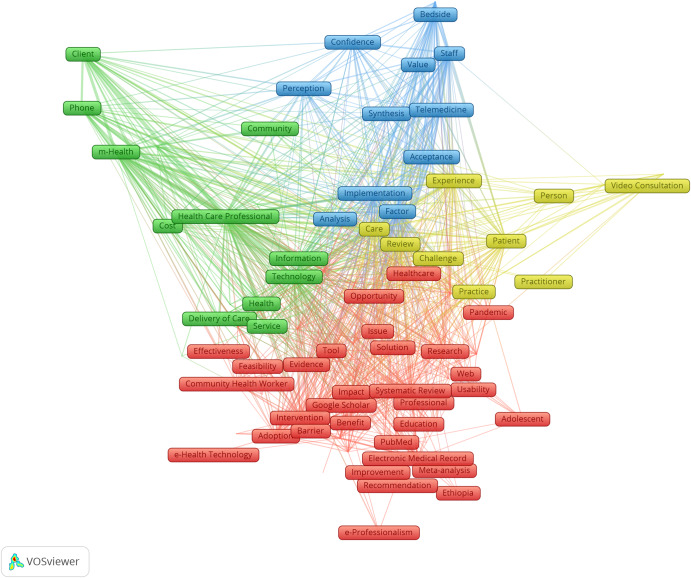
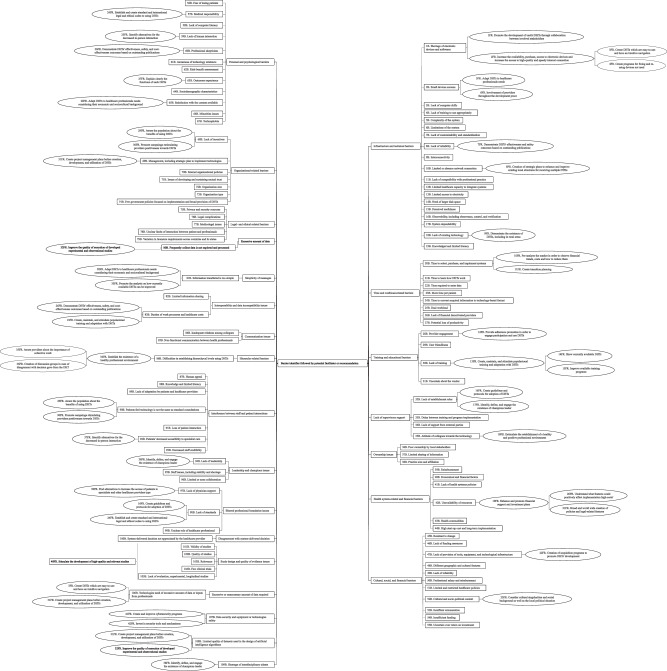
According to our bibliometric analysis, our data were classified into five clusters based on identifier clustering assessment, and recorded keywords by co-occurrence frequency are shown in Table 3 and Fig. 2. The ten most common identifiers were “healthcare professionals,” “technology,” “review,” “barrier,” “care,” “systematic review,” “factor,” “patient,” and “implementation”.
Table 3.
Top author-provided identifiers among included reviews.
| Label | Cluster | Weight links | Weight as total link strength | Weight as occurrences |
|---|---|---|---|---|
| Acceptance | 3 | 90 | 3216 | 48 |
| Adolescent | 1 | 20 | 516 | 12 |
| Adoption | 1 | 95 | 3044 | 88 |
| Advantage | 3 | 90 | 2076 | 24 |
| Analysis | 3 | 94 | 2448 | 43 |
| Attitude | 1 | 89 | 1086 | 22 |
| Barrier | 1 | 99 | 4539 | 125 |
| Bedside | 3 | 53 | 2785 | 15 |
| Benefit | 1 | 98 | 2203 | 48 |
| Care | 4 | 99 | 7425 | 125 |
| Clinical Decision Support Systems | 1 | 34 | 312 | 10 |
| Challenge | 4 | 100 | 3608 | 68 |
| CINAHL | 1 | 98 | 1507 | 29 |
| Client | 2 | 50 | 4947 | 25 |
| Cochrane Library | 1 | 81 | 422 | 11 |
| Communication | 1 | 96 | 2266 | 47 |
| Community | 2 | 84 | 1566 | 15 |
| Community Health Worker | 1 | 50 | 1296 | 36 |
| Concern | 3 | 91 | 1762 | 29 |
| Confidence | 3 | 83 | 2745 | 19 |
| Cost | 2 | 93 | 2524 | 28 |
| COVID-19 | 1 | 89 | 1685 | 46 |
| Data Collection | 2 | 92 | 1555 | 22 |
| Electronic Database | 1 | 98 | 1684 | 44 |
| Delivery of Care | 2 | 93 | 1923 | 35 |
| Depression | 4 | 32 | 759 | 12 |
| e-Health Technology | 1 | 31 | 345 | 10 |
| e-Professionalism | 1 | 26 | 520 | 10 |
| Education | 1 | 88 | 1241 | 36 |
| Effectiveness | 1 | 91 | 924 | 19 |
| Efficiency | 1 | 83 | 542 | 15 |
| Electronic Medical Record | 1 | 89 | 2787 | 78 |
| Embase | 1 | 100 | 1618 | 33 |
| Ethiopia | 1 | 26 | 342 | 10 |
| Evidence | 1 | 100 | 2745 | 61 |
| Experience | 4 | 95 | 5895 | 71 |
| Facilitator | 1 | 90 | 1574 | 40 |
| Factor | 3 | 97 | 7144 | 112 |
| Feasibility | 1 | 76 | 489 | 15 |
| Google Scholar | 1 | 87 | 519 | 15 |
| Health | 2 | 96 | 2766 | 52 |
| Health Care Professional | 2 | 102 | 14681 | 176 |
| Health Information Technology | 1 | 68 | 669 | 23 |
| Health Professional | 1 | 84 | 1394 | 27 |
| Healthcare | 1 | 96 | 2149 | 45 |
| Healthcare Professional | 1 | 87 | 896 | 25 |
| Healthcare Service | 2 | 89 | 2888 | 26 |
| Hospital Staff | 3 | 49 | 2544 | 12 |
| Impact | 1 | 96 | 2566 | 66 |
| Implementation | 3 | 99 | 5893 | 95 |
| Improvement | 1 | 90 | 658 | 18 |
| Information | 2 | 100 | 3655 | 54 |
| Integration | 1 | 83 | 689 | 17 |
| Intervention | 1 | 89 | 3018 | 85 |
| Issue | 1 | 100 | 2654 | 49 |
| Knowledge | 1 | 101 | 2358 | 43 |
| Literature Search | 1 | 87 | 778 | 16 |
| LMICs | 2 | 61 | 609 | 16 |
| Clinical Management | 1 | 96 | 1486 | 31 |
| MEDLINE | 1 | 99 | 1914 | 41 |
| Meta-analysis | 1 | 85 | 862 | 24 |
| m-Health | 2 | 84 | 7650 | 76 |
| Nurse | 1 | 84 | 1350 | 46 |
| Nursing | 1 | 71 | 360 | 12 |
| Opportunity | 1 | 95 | 1470 | 26 |
| Overview | 1 | 74 | 510 | 15 |
| Pandemic | 1 | 90 | 1335 | 31 |
| Patient | 4 | 97 | 5055 | 97 |
| Patient Care | 1 | 82 | 592 | 20 |
| Perception | 3 | 88 | 3076 | 27 |
| Person | 4 | 85 | 1329 | 19 |
| Phone | 2 | 61 | 3817 | 24 |
| Physician | 1 | 94 | 2097 | 60 |
| Practice | 4 | 98 | 2898 | 66 |
| Practitioner | 4 | 77 | 664 | 16 |
| PRISMA | 1 | 87 | 566 | 16 |
| Professional | 1 | 85 | 962 | 25 |
| PsycINFO | 1 | 80 | 476 | 12 |
| PubMed | 1 | 98 | 1487 | 40 |
| Recommendation | 1 | 83 | 595 | 14 |
| Research | 1 | 100 | 2902 | 60 |
| Review | 4 | 100 | 8315 | 143 |
| Science Direct | 1 | 92 | 1110 | 25 |
| Scoping Review | 1 | 94 | 2050 | 60 |
| Scopus | 1 | 96 | 1142 | 31 |
| Service | 2 | 94 | 3020 | 62 |
| Solution | 1 | 79 | 630 | 17 |
| Staff | 3 | 87 | 5860 | 42 |
| Strategy | 1 | 94 | 1782 | 34 |
| Synthesis | 3 | 92 | 2154 | 21 |
| Systematic Literature Review | 1 | 75 | 596 | 17 |
| Systematic Review | 1 | 101 | 4086 | 116 |
| Technology | 2 | 99 | 7989 | 157 |
| Telehealth | 1 | 77 | 1237 | 31 |
| Telemedicine | 3 | 86 | 3127 | 34 |
| Tool | 1 | 97 | 2712 | 69 |
| Training | 1 | 99 | 3032 | 50 |
| Treatment | 4 | 82 | 860 | 15 |
| Usability | 1 | 77 | 798 | 18 |
| Value | 3 | 71 | 1494 | 14 |
| Video Consultation | 4 | 27 | 1202 | 22 |
| Web | 1 | 95 | 1320 | 30 |
| Workflow | 2 | 86 | 1055 | 18 |
Fig. 2. Overview of the network map of the most frequently identified terms among included studies.
Please note that in the network visualization, items are represented by their label and by default also by a rectangles. The size of the label and the circle of an item is determined by the weight of the item. The higher the weight of an item, the larger the label and the circle of the item. The color of an item is determined by the cluster to which the item belongs.
Taking into account the 37 (34.2%) records providing data regarding the number of healthcare professionals considered in primary studies, sample sizes ranged from 22 to 106,876 (totaling approximately 345,000 healthcare workers), with a mean of 3,197 (SD 12,364), and a median of 1,545 (IQR 258 to 9,016). Most studies did not precisely consider one medical specialty, disease, or condition. However, some reviews focused on diseases of the respiratory system (e.g., tuberculosis, asthma, and chronic pulmonary obstructive disease)19,22,31,32,46,93,101,123, pregnancy, childbirth, or puerperium (e.g., maternal health, postpartum hemorrhage, and reproductive health)19,22,23,26,31,35,46,56,61,77,94, certain infectious or parasitic diseases (e.g., malaria, human immunodeficiency virus infection, and influenza)19,22,23,28,31,46,50,61, endocrine, nutritional, or metabolic diseases (e.g., diabetes mellitus)57,64,76,93,123, mental and behavioral disorders (e.g., post-traumatic disorder syndrome, stress, depression, and burnout)23,41,44,64,70,76,94,125, neoplasms50,67,85,123, diseases of the circulatory system (e.g., hypertension)19,25,48,50,57,67,93,123, diseases of the blood or blood-forming organs (e.g., anemia)22, and diseases or disorders of orofacial complex (e.g., oral lesions)28,42. Identified reviews mostly included quantitative (randomized and non-randomized trials, surveys, economic analysis, structured questionnaires, and experimental studies), qualitative (e.g., non-structured interviews, literature reviews, focus groups, observation, and cultural reports), and mixed-method reviews (sequential exploratory and concurrent transformative studies). An additional description of included reviews is shown in Table 2.
Barriers and facilitators identified in included reviews and potential recommendations
The final domains created based on the thematic analysis can be accessed in Figs. 3, 4, and the summary of findings of the top seven barriers and facilitators can be accessed in Table 4. Our linguistic and semantic-based analysis stratified the data into 21 barriers and 19 recommendations. Predominant barriers were associated with infrastructure and technical (RFO of 6.4% [95% CI 2.9–14.1]), personal and psychological barriers (RFO of 5.3% [95% CI 2.2–12.7]), time and workload-related (RFO of 3.9% [95% CI 1.5–10.1]), training and educational (RFO of 3.4% [95% CI 1.3–8.9]), and legal- and ethical-related factors (RFO of 3.6% [95% CI 1.3–9.6]). Most predominant enablers related to the offer of training and educational activities (RFO of 3.8% [95% CI 1.6–9.0]), healthcare provider perception of digital health technologies usefulness and willingness to use (RFO of 3.8 % [95% CI 1.8–7.9]), the existence of government and multisector incentives (RFO of 3.0% [95% CI 1.4–6.6]), adherence promotion campaigns (RFO of 2.2% [95% CI 1.1–4.3]), involvement of healthcare providers in the process of digital health technologies development and implementation (RFO of 2.0% [95% CI 0.8–4.9]), and intuitive navigation in healthcare technology systems (RFO of 1.9% [95% CI 0.7–5.2]).
Fig. 3. Relative frequency meta-analysis of most reported barriers for the use of digital health technologies by healthcare professionals.
Frequencies (expressed as % and their confidence interval) are distributed among each categorized barriers as well as by healthcare technology modality.
Fig. 4. Relative frequency meta-analysis of most reported facilitators for the use of digital health technologies by healthcare professionals.
Frequencies (expressed as % and their confidence interval) are distributed among each categorized facilitators as well as by healthcare technology modality.
Table 4.
Summary of qualitative findings.
| Summary of review findings | RFO expressed as % (95% CI) | GRADE-CERQual components | ||||
|---|---|---|---|---|---|---|
| Methodological Limitationsa | Coherenceb | Adequacyc | Relevanced | Overall assessmente | ||
| Top 7 identified barriers | ||||||
| 1. Healthcare professionals perceived that infrastructure and technical barriers were significantly crucial to using DHTs | 6.4 % (95% CI 2.9–14.1) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 2. Healthcare professionals perceived that psychological and personal issues directly affect the utilization of DHTs | 5.3% (95% CI 2.2–12.7) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 3. Fear of increased working hours and workload hinder the adoption and broad use of DHTs | 3.9% (95% CI 1.5–10.1) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 4. Healthcare professionals are aware and alert to legal and ethical features of using DHTs, factors that interfere with the success rate of any DHT | 3.6% (95% CI 1.3–9.6) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 5. Lack of training and educational programs causes a negative experience for healthcare professionals using DHTs, decreasing their use | 3.4% (95% CI 1.3–8.9) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 6. The structure of the healthcare system and lack of financial support limit the use of DHTs | 2.9% (95% CI 1.0–8.3) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 7. Interoperability and data incompatibility are conflicting elements in using DHTs | 2.2% (95% CI 1.0–5.0) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| Top 7 identified facilitators | ||||||
| 1. Offering training and educational activities increase the positive experience and facilitate the adoption of DHTs by healthcare providers | 3.8% (95% CI 1.6–9.0) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 2. Those healthcare professionals who perceived the full usefulness of DHTs and were willing and opened to the new technology are more likely to use them in a long-term period | 3.8% (95% CI 1.8–7.9) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 3. Government and multisector incentives increase the use of DHTs by healthcare professionals | 3.0% (95% CI 1.4–6.6) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 4. Adherence promotion campaigns facilitate and increase the use of DHTs by healthcare providers | 2.2% (95% CI 1.1–4.3) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 5. Involvement of healthcare professionals in the process of development and implementation of DHTs facilitates their experience with the technology and increases their acceptance | 2.0% (95% CI 0.8–4.9) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 6. Easy-to-use and intuitive navigation systems facilitate the use of DHTs by healthcare providers | 1.9% (95% CI 0.7–5.2) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
| 7. The existence of solid leadership and local champion facilitate the creation, implementation, and long-term adoption of DHTs by healthcare professionalsFeeling of reliability in utilized equipment and technologies improve the implementation and the adoption of DHTs by healthcare providers | 1.7% (95% CI 0.7–3.8) | Moderate concerns | No or very minor concerns | No or very minor concerns | No or very minor concerns | High confidence |
CI Confidence Interval, DHTs Digital Health Technologies, RFO Relative Frequency of Occurrence.
aWe downgraded one level of confidence in the evidence based on the methodological quality of included systematic reviews and not based on the methodological limitations of primarily included studies. The rationale is that the AMSTAR-2 tool has seven strict critical domains, which, if occurred at least once, decreases overall confidence by two levels. Nevertheless, since several experts have already suggested that the reporting of many items in the PRISMA statement is suboptimal, we believe that this lack of reporting or evaluation might be associated with a “mass effect”, where researchers simply follow an inadequate pattern. Therefore, we decreased one level in the certainty of evidence instead of two levels on reviews’ methodological limitations.
bCoherence was rated as no or very minor concerns because the reviews’ findings appropriately described the data’s complexity, variation, and interconnectedness. Therefore, the available qualitative evidence provided no signs of contradictory, ambiguous, or incomplete data and competing theories or theoretical elements.
cWe found the obtained data rich enough considering the complex and vast amount of data, the number of studies included, and their associated number of participants.
dBased on the review questions expressed in each included review, we judged the body of data from these reviews to be fully integrated with each research question.
eAlthough most of our included reviews were classified as “very low methodological quality” using the AMSTAR 2 tool, we believe that the reported data is significant enough not to decrease the confidence level primarily based on the methodological quality. We analyzed a group of phenomena that could hinder or enable the use of DHTs by healthcare providers, and we did find any signs of unbalanced or one-sided. Data underlying the reviews’ findings were sufficiently rich in terms of the number of studies and number of healthcare professionals.
As represented in Figs. 3, 4, several semantic clusters were described throughout included reviews. Herein, we outline and exemplify the five most common barriers and facilitators to the design, implementation, longitudinal maintenance, and evaluation of digital health technologies by healthcare professionals. The remaining barriers and facilitators are explained in detail in Supplementary Information 2 (pp 8). Infrastructure and technical barriers were the most frequently described barriers among included reviews, relating to issues with a limited or insufficient network, lack of existing technologies, lack of devices, compatibility with daily workflow, connectivity speed, healthcare capacity of technology integration, interconnectedness, absence of standardized/harmonized systems at different facilities, limited access to electricity, and requirement of a functional database system or large disk space. Notably, technical issues seem to be the worst in rural and countryside regions. Firstly, counteracting connectivity-related barriers involves ensuring availability (especially in rural areas) and affordability, guaranteeing high-speed fiber connectivity, and increasing the number of reliable local networks. In addition, we found reviews suggesting that to overcome infrastructure and technical barriers, the involvement of healthcare professionals in developing and implementing any health technology tools is fundamental, enhancing their capacity to manage such applications and increase their independence from co-workers and support centers. Remarkably, all reviews stated that user engagement and collaboration with system developers or associated stakeholders is crucial in all design and development stages, deployment, and continued utilization, as created applications are fit for purpose, based on understanding and addressing healthcare providers’ needs and expectations.
Personal and psychological barriers involved complex thematic components, including the healthcare professionals’ resistance to change, difficulty understanding the technology, perception of less human interaction, technophobia, ages, education levels, professional experience, low literacy, poor writing skills, linguistic features, adherence behavior, and fear of using particular health technology. Moreover, unwillingness, low expectations, skepticism from healthcare providers, and low motivation for compliance were also associated with personal barriers. For counterbalancing these barriers, healthcare professionals’ perception of usefulness and willingness was a highly cited facilitator, characterized by the degree to which the employees believe that using specific digital health technologies would enhance their performance and the proportion of participants intending to utilize that technology. Furthermore, personal and psychological barriers could be addressed by using and adopting training programs and educational activities appropriately tailored to healthcare professionals’ needs and coverage of deficient abilities. High-quality, real-time technical support and coaching also appeared as a component that increased healthcare providers’ efficiency, decreased implementation fear, and potentially could reduce internal conflicts during system adoption. Importantly, training programs may be developed with the ongoing involvement of the intended community to understand their needs and knowledge gaps. Moreover, evidence shows that user-friendly design, intuitive system navigation, and easy-to-use interfaces are critical to improving overall product performance and facilitating data collection and input, data processing, and further analysis.
Some reviews suggested that the limiting factors for the broad use of digital health technologies are associated with healthcare workers’ concerns about increased workload and altered workflow, which could hinder the sustainability of the digital health technologies. Additionally, these newly implemented technologies would require additional purchase time and increased set-up, implementation, training, access, adaptation, and establishment stages. In addition, healthcare professionals commonly stressed that digital health technologies would impact the quality of delivered care, as recently trained professionals would need a longer time to convert acquired data into the implemented system. However, although time might be required to acquire the right skills and operating competencies, with adequate training, continuous technical support, and peer-to-peer collaboration, threats associated with increased time to complete a specific task are significantly reduced. Useful written guidelines, instructions, and handouts appear to be important facilitators that could be easily implemented73. Likewise, incentives from government agencies and multisectoral organizations were shown to significantly improve digital health technologies’ effectiveness and chances of success in large-scale healthcare systems. Therefore, this conceptual perspective should be shown to healthcare providers, as increased effectiveness is directly related to the appropriate use of time and less wasteful processes.
Fourth, legal- and ethical-related barriers were shown to be a relevant factor for healthcare providers, as privacy and security concerns, national legislation, jurisdiction, and the existence of unclear legal liability regarding response protocols would directly affect healthcare professionals. Possible interventions for these barriers are associated with the development of safer data storage systems, the establishment of requirements on safety and security in cooperation with healthcare professionals and patients, or the creation of an international legal framework and legislative norm, which would clarify security regulation policies that could help ensure patients’ privacy and confidentiality, as well as define healthcare professionals’ liabilities.
Lastly, deficient or inexistent training and educational activities were evidenced to significantly impact the success and efficiency of digital health technologies in the healthcare environment . Some reviews highlighted that without training, healthcare providers tend to feel low self-efficacy when utilizing any digital health technologies, resulting in negative attitudes toward these technologies. In addition, as evidenced by healthcare workers, prior technology introduction, vendor training, in-depth seminars, workshops, or correlated training activities are unusual, and regular quality process assessment following implementation to ensure efficiency are also rare. Interestingly, reviews not only highlighted that training was fundamental to the success of using digital health technologies but also suggested that training per se would also be delivered through certain digital health technologies, such as mobile technologies and computers. Thus, the training offer positively affects healthcare professionals’ experience with digital health technologies, especially when monetary incentives are added to this variable, given the time invested in obtaining the proper abilities to operate any digital health technologies.
Using the AMSTAR 2 methodological quality assessment tool, most reviews had a very critically low overall methodological quality, as shown in Table 5. Nine-nine reviews were classified as very low quality, six as low quality, and only three were rated to have a high methodological quality. Two top-ranked reporting inadequacies related to the lack of evaluating the presence and likely impact of publication bias (95.2%), and the disregard of the risk of bias when interpreting the results of the review (95.2%). Where judgment was lost, this generally associated with the lack of prior protocol (50.9%), absence of justification for excluding individual studies (88.8%), lack of risk of bias assessment from individual studies being included in the review (63.8%).
Table 5.
Quality assessment rating of systematic reviews included in the digital health solutions applied to healthcare workers environment overview.
| Study ID | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | Overall Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Addotey-Delove 2023 | Y | N | N | PY | Y | Y | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Adepoju 2017 | Y | N | Y | PY | Y | Y | N | PY | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Agarwal 2015 | Y | N | Y | N | N | N | N | N | N | N | NA | NA | N | N | NA | N | Critically Low |
| Alkhaldi 2023 | Y | N | Y | N | Y | Y | N | Y | Y | N | NM | NM | Y | Y | NM | Y | Critically Low |
| Al-Rawashdeh 2022 | Y | Y | Y | Y | Y | Y | N | PY | Y | Y | NM | NM | Y | Y | NM | Y | Low |
| Amoakoh-Coleman 2016 | Y | PY | Y | N | Y | Y | N | PY | PY | Y | NA | NA | Y | Y | NA | Y | Critically Low |
| Arsad 2023 | Y | N | Y | N | N | N | N | Y | Y | N | NM | NM | N | N | NM | Y | Critically Low |
| Aslani 2022 | Y | N | Y | N | N | Y | N | Y | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Avoka 2022 | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | NM | NM | Y | Y | NM | Y | Low |
| Baluszek 2022 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NM | NM | Y | Y | NM | Y | High |
| Bervell 2019 | Y | N | N | Y | Y | N | N | PY | PY | N | NA | NA | N | N | NA | N | Critically Low |
| Boonstra 2010 | Y | N | Y | N | Y | N | N | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Bommeyer 2023 | Y | Y | Y | PY | Y | Y | N | PY | N | N | NA | NA | N | N | NM | Y | Critically Low |
| Braun 2013 | Y | N | Y | N | Y | Y | N | N | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Brewster 2014 | Y | N | Y | N | Y | N | N | Y | Y | N | NA | NA | N | N | NA | Y | Critically Low |
| Brown 2020 | Y | PY | Y | N | N | N | N | PY | Y | N | NA | NA | Y | N | NA | N | Critically Low |
| Calleja 2022 | Y | N | Y | N | Y | Y | N | Y | N | N | NM | NM | N | N | NM | N | Critically Low |
| Cansdale 2022 | Y | N | Y | Y | Y | Y | N | Y | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Cartolovni 2022 | Y | N | Y | Y | Y | N | N | Y | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Celes 2018 | Y | PY | Y | PY | Y | Y | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Cen 2022 | Y | Y | Y | PY | Y | Y | N | Y | N | N | NM | NM | N | Y | NM | Y | Critically Low |
| Chen 2022 | Y | N | Y | PY | N | N | Y | Y | Y | N | NM | NM | N | N | NM | Y | Critically Low |
| Chan 2018 | Y | N | Y | N | Y | N | Y | Y | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Christensen 2020 | Y | N | Y | PY | Y | N | N | PY | Y | N | NA | NA | Y | N | NA | Y | Critically Low |
| Da Costa 2020 | Y | PY | Y | N | Y | Y | N | PY | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Davis 2014 | Y | N | Y | N | Y | N | N | PY | N | N | NA | NA | N | N | NA | Y | Critically Low |
| de Grood 2016 | Y | N | Y | PY | Y | Y | N | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Drissi 2021 | Y | N | N | N | N | N | N | PY | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Dutta 2020 | Y | N | Y | N | N | N | N | N | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Early 2019 | Y | N | Y | N | Y | Y | N | N | N | N | NA | NA | N | Y | NA | N | Critically Low |
| Ebneter 2022 | Y | N | Y | N | Y | Y | N | PY | N | N | NM | NM | N | Y | NM | Y | Critically Low |
| Emmett 2022 | Y | PY | Y | N | Y | Y | N | PY | PY | N | NM | NM | Y | N | NM | Y | Critically Low |
| Ferdousi 2021 | Y | Y | Y | N | Y | N | N | N | Y | N | Y | Y | Y | Y | Y | Y | Critically Low |
| Fletcher 2023 | Y | N | Y | PY | Y | Y | N | Y | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Ftouni 2022 | Y | Y | Y | N | Y | Y | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Gagnon 2012 | Y | Y | Y | N | Y | Y | N | PY | Y | N | NA | NA | Y | Y | NA | N | Critically Low |
| Gagnon 2016 | Y | N | Y | N | N | Y | Y | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Garavand 2022 | Y | N | N | Y | N | Y | N | PY | Y | Y | NM | NM | N | N | NM | Y | Critically Low |
| Garvey 2021 | Y | N | N | PY | N | N | N | Y | Y | Y | NM | NM | Y | Y | NM | Y | Critically Low |
| Ghimire 2023 | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | NM | NM | Y | Y | NM | Y | Low |
| Gonçalves R 2023 | Y | PY | Y | Y | Y | Y | Y | Y | Y | N | NM | NM | Y | N | NM | Y | Critically Low |
| Grant 2022 | Y | Y | Y | Y | Y | Y | N | Y | Y | N | NM | NM | Y | N | NM | Y | Critically Low |
| Hagstram 2022 | Y | Y | Y | PY | Y | Y | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Huang 2023 | Y | PY | Y | N | Y | Y | N | PY | Y | N | NM | NM | Y | N | NM | Y | Critically Low |
| Ionescu 2022 | Y | N | Y | N | Y | N | N | PY | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Isidori 2022 | Y | N | Y | N | N | N | N | PY | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Ismatullaev 2022 | Y | N | Y | N | Y | Y | N | N | N | N | NM | NM | N | N | NM | N | Critically Low |
| Jacob 2020 | Y | PY | Y | PY | Y | N | N | N | Y | N | NM | NM | N | N | NM | Y | Critically Low |
| Jimenez 2022 | Y | Y | Y | N | Y | Y | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Jimma 2022 | Y | Y | Y | PY | Y | Y | Y | PY | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Joo 2022 | Y | N | Y | N | N | N | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Jonasdottir 2022 | Y | Y | Y | Y | Y | Y | N | PY | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Jose 2023 | Y | N | N | PY | Y | N | N | N | N | Y | NM | NM | Y | Y | NM | Y | Critically Low |
| K. Zhang 2022 | Y | N | Y | N | N | N | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Kane 2022 | Y | N | Y | N | Y | N | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Keyworth 2018 | Y | PY | Y | PY | Y | N | N | PY | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Koivunen 2018 | Y | Y | N | Y | N | N | N | PY | Y | N | NM | NM | N | Y | NM | Y | Critically Low |
| Kolla 2021 | Y | N | Y | PY | N | N | N | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Konnyu 2023 | Y | Y | Y | PY | Y | Y | N | PY | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Kruse 2022 | Y | PY | N | Y | Y | Y | N | PY | Y | N | NM | NM | Y | N | NM | Y | Critically Low |
| Laar 2022 | Y | Y | Y | Y | Y | Y | N | PY | Y | N | NM | NM | N | N | NM | Y | Critically Low |
| Lam 2022 | Y | N | N | N | N | N | N | PY | N | Y | NM | NM | Y | Y | NM | Y | Critically Low |
| Lampickien 2022 | Y | N | Y | N | N | N | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Li 2013 | Y | N | Y | N | N | N | N | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Li 2019 | Y | PY | Y | Y | N | N | N | Y | Y | N | NA | NA | Y | N | NA | Y | Low |
| Lluch 2020 | Y | N | Y | PY | N | N | N | N | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Longhini 2022 | Y | Y | Y | Y | Y | Y | N | Y | Y | N | NM | NM | N | N | NM | Y | Critically Low |
| Martin 2019 | Y | Y | Y | Y | Y | Y | N | Y | Y | N | NA | NA | N | Y | NA | Y | Critically Low |
| Marvaso 2022 | Y | PY | N | PY | N | N | N | PY | N | Y | NM | NM | N | N | NM | Y | Critically Low |
| Meunier 2023 | Y | Y | Y | PY | Y | Y | N | PY | Y | Y | NM | NM | Y | Y | NM | Y | Low |
| Moore 2020 | Y | N | Y | PY | Y | Y | N | Y | Y | N | NM | NM | Y | N | NM | Y | Critically Low |
| Muhiyaddin 2020 | Y | N | N | PY | Y | Y | N | N | N | N | NA | NA | N | N | NA | N | Critically Low |
| Mulita 2022 | Y | N | N | PY | N | N | N | N | N | Y | NM | NM | N | Y | NM | Y | Critically Low |
| Namasivayam 2022 | Y | Y | Y | PY | Y | Y | N | Y | N | Y | NM | NM | N | Y | NM | Y | Critically Low |
| Nezamdoust 2022 | Y | N | Y | PY | N | N | N | N | N | Y | NM | NM | N | Y | NM | Y | Critically Low |
| Nguyen 2021 | Y | Y | Y | N | Y | Y | N | Y | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Niazkhani 2020 | Y | N | Y | N | Y | Y | N | Y | Y | N | NA | NA | N | N | NA | Y | Critically Low |
| Nizeyimana 2022 | Y | Y | Y | Y | Y | Y | N | N | N | N | NA | NA | N | N | NA | Y | Critically Low |
| O’Connor 2022 | Y | N | Y | N | Y | N | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Odendaal 2020 | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | NA | NA | Y | Y | NA | Y | High |
| Osman 2019 | Y | Y | Y | N | Y | N | N | Y | Y | N | NA | NA | N | N | NA | Y | Critically Low |
| Papadopoulos 2018 | Y | N | Y | N | Y | Y | N | PY | N | N | NM | NM | N | Y | NM | N | Critically Low |
| Police 2011 | Y | N | N | Y | N | N | N | PY | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Prakash 2022 | Y | Y | Y | Y | Y | Y | N | N | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Rahal 2021 | Y | Y | Y | N | Y | Y | N | Y | Y | N | NA | NA | Y | N | NA | Y | Critically Low |
| Ramachandran 2023 | Y | Y | Y | Y | Y | Y | N | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Ratshidi 2022 | Y | Y | Y | PY | N | N | N | N | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Rukavina 2021 | Y | Y | Y | N | Y | Y | Y | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Saigi-Rubio 2022 | Y | Y | Y | N | Y | Y | N | Y | Y | Y | NM | NM | Y | N | NM | Y | Critically Low |
| Sipanoun 2022 | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | NM | NM | Y | Y | NM | Y | Low |
| Sullivan 2022 | Y | N | N | N | N | N | N | PY | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Poissant 2005 | Y | N | Y | Y | Y | N | N | Y | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Tabaeeian 2022 | Y | N | Y | N | Y | Y | N | N | N | N | NM | NM | N | N | NM | N | Critically Low |
| Tegegne 2023 | Y | PY | N | PY | N | Y | N | Y | N | Y | Y | N | N | Y | Y | Y | Critically Low |
| Thomas Craig 2021 | Y | Y | Y | Y | Y | Y | N | Y | Y | N | NA | NA | N | Y | NA | Y | Critically Low |
| Tickner 2023 | Y | N | Y | Y | N | N | N | Y | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Torres-Castano 2023 | Y | Y | Y | Y | Y | N | Y | Y | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Vejdani 2022 | Y | PY | Y | PY | Y | N | N | Y | N | N | NM | NM | N | Y | NM | Y | Critically Low |
| Verma 2022 | Y | Y | Y | N | Y | N | N | Y | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Von Wedel 2020 | Y | PY | N | Y | Y | N | Y | Y | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Walle 2023 | Y | PY | Y | PY | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Critically Low |
| Walsh 2021 | Y | N | Y | PY | N | N | N | Y | N | Y | NM | NM | N | Y | NM | Y | Critically Low |
| Wisner 2019 | Y | PY | Y | Y | N | N | N | PY | Y | N | NA | NA | N | N | NA | N | Critically Low |
| Xyrichis 2021 | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | NA | NA | Y | Y | NA | Y | High |
| Young 2011 | Y | N | N | Y | Y | N | N | Y | N | N | NA | NA | N | Y | NA | Y | Critically Low |
| Zakerabasali 2021 | Y | N | Y | N | Y | Y | N | Y | N | N | NA | NA | N | N | NA | Y | Critically Low |
| Zhang J 2023 | Y | N | N | N | Y | N | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
| Zhang Z 2023 | Y | N | Y | N | Y | Y | N | N | N | N | NM | NM | N | N | NM | Y | Critically Low |
Judgement was performed by two reviews authors and based on the AMSTAR-2 approach.
Domain 1—Did the research questions and inclusion criteria for the review include the components of PICO?
Domain 2—Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review and did the report justify any significant deviations from the protocol?
Domain 3—Did the review authors explain their selection of the study designs for inclusion in the review?
Domain 4—Did the review authors use a comprehensive literature search strategy?
Domain 5—Did the review authors perform study selection in duplicate?
Domain 6—Did the review authors perform data extraction in duplicate?
Domain 7—Did the review authors provide a list of excluded studies and justify the exclusions?
Domain 8—Did the review authors describe the included studies in adequate detail?
Domain 9—Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review?
Domain 10—Did the review authors report on the sources of funding for the studies included in the review?
Domain 11—If meta-analysis was performed did the review authors use appropriate methods for statistical combination of results?
Domain 12—If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis?
Domain 13—Did the review authors account for RoB in individual studies when interpreting/ discussing the results of the review?
Domain 14—Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review?
Domain 15—If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review?
Domain 16—Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review.
We mapped the aforementioned data and complementary results, as shown in Fig. 5 (also available for virtual access through the GitMind platform).126 As evidenced in supplementary information 3 (pp 9), we found several terms with similar semantic structures. Thus, we coded each barrier or facilitator and identified recommendations, suggesting the possibility of a complex and broad linguistic connection and relationship amongst codes. These thematic relationships are not limited in our analysis and can be explored and exhausted.
Fig. 5.
Conceptual map of reported barriers and potential facilitators and recommendations to overcome these barriers.
Discussion
To our knowledge, this is the first overview of systematic reviews to collate, cluster, and synthesize the quantitative, qualitative, and mixed methods body of literature associated with barriers and facilitators to and use of several digital health technologies by healthcare professionals at all levels of care. The decision for carrying out this valuable, but complex study, relies on the noticeable detachment of research data and investigation groups in the field of Medical Informatics, who usually inadvertently duplicate technical and financial resources given the existing gaps in the literature. Here we report 21 overarching barriers and 19 facilitators, mostly interconnected, containing a complex sequence of thematic describers and identifiers. Understanding and overcoming identified barriers to the fully integrated and coordinated use of DHTs by any class of healthcare providers and evaluating its facilitators could positively impact successful creation, implementation, adoption, training, and long-term services or product utilization.
The evidence suggests that healthcare providers and managers predominantly face infrastructure, technical-, training-, legal-, ethics-, time-, and workload-related barriers to using digital health technologies, regardless of the level of care or digital technology. In the second level of semantic occurrence, several restraining factors to the wide use of digital health technologies were combined and reported, including psychological and personal barriers, lack of supervisory support, ownership issues, and healthcare system-cultural-, social-, and financial-related limiting features. Nevertheless, we are aware that some of the classified items are interconnected, meaning that the prevalence of occurrence ranking should not be used as a priority guide for policymakers and health organizations when addressing these barriers. For instance, the highlighted barrier “81B” (regarding the simplicity of contents usually transferred in mobile applications or clinical alert systems) might be directly related (or potentially caused due to) to the technical limitations per se (considering devices screen’s reduced size (“2B”), the complexity of the systems themselves and the information they carry (“5B”), or even because the lack of standardization and customizability of such systems and technologies (“7B”). Therefore, the creation of artificial intelligence-based mind mapping representing these interconnections is of utmost relevance126.
Creating and applying digital health technologies to healthcare environments must be driven by a regime of comprehensive assumptions instead of empirical models and processes. Our results corroborate with published systematic reviews that have already evidenced patient-reported barriers and facilitators to utilizing digital health solutions for self-care127–129. For instance, self-management of low-back pain using mobile health applications was mainly challenging due to information technology, usability-accessibility, quality-quantity of content, tailoring-personalization, and motivation-support barriers127. In contrast, flexibly structured and intuitive navigation, trustworthy content and sources, content accounting for individual needs and priorities, and the opportunity to influence the application design appeared as relevant facilitators affecting the uptake and utilization of digital health interventions for self-management of lower back pain127. Likewise, Powell and colleagues suggested that a lack of awareness, self-motivation, training, privacy, and security concerns are the most common patient-derived barriers to using electronic portals128. Emphasized facilitators correlated with use engagement by a leader (i.e., physician), free access and control over health information, and an adequate communication profile. Therefore, as the relationships between our identified barriers and facilitators and existing patient-related evidence highlight, the development of digital healthcare solutions should consider multiple factors, which can facilitate or deteriorate broad goals of high-quality use of information technology in the healthcare environment.
During protocol modeling, our research group discussed the possibility of including reviews that summarize evidence on barriers and facilitators involving students in health fields. The decision was not to include these reviews because these students are not yet legally considered professionals or critically necessary workforce, and they are not considered essential in healthcare settings130,131. However, one aspect found in these excluded reviews was revealed in our overview with significant frequent and relevant findings: the use of digital health technologies for training and educational purposes. Although distance education dates from 1728132,133, e-learning or virtual learning started during the early 1980s at the University of Toronto134 and has been developing ever since, particularly during the COVID-19 pandemic135,136. Currently, several high-income countries, such as New Zealand and the United States of America, have already integrated and implemented the Information and Communication Technology constructivist learning model in their national or statewide policies, ensuring that students have the chance to become digitally competent citizens137,138. These actions effectively decrease multiple barriers observed related to limited or no computer skills, restricted knowledge and technology literacy, and lack of reliability in technological tools. However, it has been suggested that numerous low- and middle-income countries still struggle with device acquisition, connectivity issues, tutors’ level of expertise and lack of motivation, absence of basic infrastructure, and the unwillingness of the government to implement such solutions129.
Foremost, we chose only six health solutions as systematic and feasible choices for comprehensive data processing. Nevertheless, we observed additional modalities of health solutions being implemented worldwide (e.g., laboratory and radiology automatic reporting systems, picture archiving and communication systems, cloud-based systems, and advanced and business analytics), and our synthesis may miss emerging or recent technologies52,74,114. For instance, studies have suggested that electronic laboratory reporting systems not only improve surveillance for notifiable conditions but can also be helpful in real-time laboratory testing in emergency departments and significantly improve organizational framework and efficiency139,140. Correspondingly, cloud-based computing systems have been increasingly applied in the healthcare system to ensure secure storage, handling, and processing of medical information141. Regardless of the digital health solution being implemented and utilized, healthcare workers and patients benefit from it. By improving real-time patient access to their results and providing better patient involvement with care, the incidence of unwanted tests or extra prescriptions decreases, and the overall quality of care is subsequently enhanced142,143.
We observed a limited number of reviews assessing the potential challenges and enablers for artificial intelligence models, machine learning algorithms, and platforms utilizing features such as augmented reality40,54,63,70,78,85,94,99. However, although the restricted number of studies assessing these subgroups in the field of digital technologies, core barriers and facilitators remained like other subgroups. Nevertheless, we highlight the need for further research with these technologies, as alternative barriers and facilitators would arise.
Due to the wide variety of digital health technologies currently being used in several medical specialties and levels of care, we had to restrict our report in different ways, limiting our certainty of evidence. Similarly, our series of analyses did not consider the existence of subgroup singularities by type of healthcare professional. As suggested in our map based on bibliometric data, only physicians, community health workers, and nurses appeared as recurrent keywords among all studies within the 42 systematic reviews eligible for inclusion. Therefore, studies analyzing impeding and enabling factors to the general use of digital health technologies in other healthcare providers (e.g., pharmacists, physiotherapists, physical educators, speech therapists, healthcare governmental agents, biologists, social services agents, healthcare managers, dentists, and psychologists) cause a “professional class bias” event that should be addressed in future studies. Likewise, factors like age, racial group, gender, country income index, or geographic location could affect a different subgroup (e.g., potential higher reporting of barriers of professionals practicing in low- or middle-income countries would focus more on technical and infrastructure features). Moreover, we neglected that digital health technologies utilized in the healthcare environment are usually concomitant and integrated. Thus, we may have considered the reported health solution independently instead of using a translational and adapted assignment methodology. Therefore, the provided RFO represented only the tendency of domain observance and reporting and not the identical picture of healthcare professionals’ reality. To conclude, we are aware that some highlighted barriers and facilitators could be assigned to a broader subtheme (e.g., lack of supervisory support in training and educational skills). However, during the overall execution, we observed that some terminologies and coding were commonly reported separately, so we decided to maintain them as individual elements to ensure the representativeness of the findings. Interestingly, the use of the AMSTAR 2 tool for evaluating the methodological quality of all included reviews should also be stated as a limitation, as the approach was primarily intended to systematic reviews of randomized controlled trials. Nevertheless, as most AMSTAR domains are on the elements that any review is structured (e.g., search strategy, protocol, extraction, combing studies, and publication bias), we believe that applying this methodology to our include reviews do not hinder the observed results. Likewise, although we Apart from these minor methodological limitations, the major strength of our study is the strict adhesion to international guidelines for reporting of systematic reviews (e.g., Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement and the Cochrane Handbook of Systematic Reviews and Meta-Analyses) and the execution of the entire study with international and blinded collaboration. We acknowledge that more than one methodology for evaluating the certainty of the evidence in qualitative research exists. We applied the GRADE CERQual method to check the overall quality of evidence for the seven most-reported barriers and facilitators. Generally, the evidence quality is high, with all considered domains without major concerns but with methodological limitations. We judged this domain as a moderate concern based on the phenomena of interest, adequate data collection and extraction, and quality in reporting observed data. In addition, expert groups have been discussing.
Although digital health technologies and their numerous types of technologies positively affect the healthcare environment, barriers impacting the successful creation, adoption, implementation, and sustainability of digital interventions are commonly reported by healthcare workers. Notwithstanding, the identification and deployment of different enabling factors allow the utilization of digital technologies in a holistic and integrated way. This overview of reviews emphasizes remarkable limiting features that should be considered by all stakeholders and provides advice to overcome these issues, with the expectation of increasing professional satisfaction and, perhaps, the quality of delivered care.
Methods
This overview of systematic and scoping review (herein referred to as “overview”) protocol was registered on PROSPERO (CRD42022304372, supplementary information 4, pp 10–20) and it was part of a broader study conducted by the Data and Digital Health Unit of the Division of Country Health Policies and Systems of the World Health Organization, Regional Office for Europe3. This initiative provides strategic direction, technical assistance, and tailored support to countries and policymakers to strengthen their capacity to generate timely, credible, reliable, and actionable health-related data. The scientific community is currently defining an explicit, systematic, and transparent methodology to create evidence- and agreement-based reporting guidelines for overviews of reviews144. Therefore, we used the Preferred Reporting Items for Systematic Reviews and Meta-Analysis reporting recommendations145, the Cochrane Handbook guidelines146, and reports published by Fusar-Poli et al.147 and Cornell et al.148 guiding the practice on how to effectively conduct an umbrella review. As our study relies upon secondary data, ethics approval was waived. It is worthwhile mentioning that although in our protocol we initially stated that a standard meta-analysis would not be carried out, we decided to mathematically evaluate the obtained results. The technique utilized for the word- and sentence-based assessment (particularly associated with discourse analysis) is a well-known summarizing strategy used in the field of Human Sciences and was systematically presented and implemented in our research team after the protocol preparation. Therefore, in consonance with the requirements of continuous scientific evolvement and improvement, we decided to apply this newly introduced technique. However, this deviation does not alter the core of this project.
Data sources and searches
We searched five databases (Cochrane Database of Systematic Reviews, Embase®, Epistemonikos, MEDLINE®, and Scopus) and the PROSPERO protocol registration platform from inception to Jan 23, 2022, for systematic and scoping reviews evaluating barriers and facilitators to using digital health technologies by healthcare professionals worldwide. We also performed a manual search of reference lists of reviews shortlisted for full-text review and planned to contact the authors of included review to retrieve additional data.
An experienced information specialist and the expert team tailored search strategies to each database using Medical Subject Headings (MeSH) and free-text identifiers associated with the research topic149–152. The search included three main categories of key terms. Digital health technologies search identifiers included terms such as “telemedicine,” “telehealth,” “mobile health,” “mHealth,” “artificial intelligence,” “machine learning,” “social media,” “natural language processing,” and “computer decision support systems,” healthcare professional-related terms included “healthcare worker,” “healthcare provider,” and “healthcare support worker,” and systematic review filters used were “systematic review,” “meta-analysis,” and “scoping review.” Our terms are defined in recently published studies in the World Health Organization guidelines on digital health technologies for strengthening health systems, the World Assembly Resolution on Digital Health, and The Lancet Digital Health. In supplementary information 5 (pp 21-28), we present the detailed search strategy for the databases.
Study selection
Eligibility was evaluated by two independent investigators who primarily screened titles and abstracts and subsequently reviewed the full texts using Covidence® (Veritas Health Innovation, Melbourne, Australia)153. Systematic and scoping reviews deemed eligible must have used at least two databases for their assessment, should have described the search methods, and evidenced the use of a transparent methodology for study selection and data extraction. Moreover, these reviews were only included if a qualitative analysis of barriers and facilitators to using digital health technologies by healthcare providers was clearly noted. We did not place limits on targeted healthcare professionals, medical specialty, level of care, language, and publication date. However, in order to avoid bias and results inflation, those studies strictly prioritizing the assessment of digital technologies for students and education in the field of health sciences were excluded.
Data extraction and quality assessment
Two independent researchers appraised the methodological quality of included systematic reviews using the AMSTAR-2 tool154. Following the initial evaluation, a third researcher cross-checked rated domains. The methodological quality of reviews was classified as “critically low,” “low,” “moderate,” and “high.” Our research team is aware that the AMSTAR 2 tool is not intended to generate an overall score of the review’s quality. Thus, we emphasize that we considered the appraisal methodology holistically, mostly related to the provision of an extensive evaluation of quality, particularly weaknesses associated with poor conduct of the review or word counting limitation endorsed by a determined journal.
Relevant data (first author identification, publication year, published journal, number of included databases, review objectives, primary study design, type of healthcare professional, type of digital technologies being analyzed, number of included primary studies, and barriers, facilitators, and recommendations for using digital health technologies) was extracted from included reviews by two independent researchers using Microsoft Excel (Microsoft Corporation, Redmond, USA)155. In the second stage, four independent volunteer collaborators reassessed extracted data to resolve inconsistencies.
Data synthesis and analysis
We used VOSviewer to assess research hotspots associated with digital health technologies based on the principle of co-occurrence analysis156. The minimum number of co-occurrences was set as 3, normalization method as an association, random starts as 1, random seed as 0, resolution as 1, and we merged small clusters. We attempted to clean the network map as much as possible, as some keywords were not meaningful. Thus, we extracted data from the top 100 author-provided keywords and mapped them into a single keyword co-existing network. Representative and frequent terms are expressed as larger nodes, and the thickness of the link between two or more nodes represents the strength of the relationships between them.
Our findings were evaluated and collated using an adapted version of a thematic synthesis developed by Thomas and Harden157. The 21 domains prioritized in the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) statement were followed158. First, qualitative data of included reviews on the main barriers and facilitators identified were coded line-by-line using QSR’s NVivo software (QSR International, Burlington, USA)159. In addition, primary highlighted concepts were re-evaluated by four volunteer collaborators who double-checked selected data and evaluated extraction errors or missing information. If needed, they also created new in-text selections. Furthermore, we organized free selections into similar themes to combine the preliminary results into descriptive themes. Lastly, we developed analytical themes that summarized barriers and facilitators closely related to the original remarks reported in included reviews. The explanatory delineation of thematic barriers and facilitators was a dynamic, deductive, and intuitive process, as different review authors had their peculiarities in academic and text writing. The alignment of thematic barriers and facilitators was discussed by all authors, resulting in the development of recommendations. In the result section, we have identified only the five most frequent barriers and facilitators. Recommendations were also emphasized for these five features. However, a complete list of barriers, facilitators, and recommendations can be accessed in supplementary information 2 (2.1 and 2.2). Where homogenous barriers were recognized (e.g., lack of leadership and local champions), guidance to overcome these barriers were prepared by the group of specialists (e.g., identification of processes weaknesses, implementation of improved strategies, and adjustment of progress based on stakeholder feedback). Similarly, the recommendations also considered the identified facilitators. Systematic reviews with similar research questions were expected to be included in our umbrella review. Consequently, the likelihood of two or more reviews including the same primary study in their analysis was meaningful160. Therefore, we carefully extracted and evaluated all references mentioned in the results section of each included review to exclude overlapping studies.
After establishing analytical themes, the frequency of occurrence for each categorized barrier and facilitator was aggregated into a standard meta-analysis of proportions. Certainty of the evidence was based on the GRADE-Cer-Qual approach161. Nominally identified results are indicated as the relative frequency of occurrence (RFO) and 95% confidence interval (CI). Analysis was executed using R software (version 4.1.1), using the metaprop function package. This study is deemed exempt as it does not assess data or intervene in humans.
Supplementary information
Acknowledgements
This project is a result of an international task force to provide high-quality evidence in Medicine. Authors and contributors are mostly active Cochrane members. We are highly grateful for the research collaborators involved in the data extraction phase of this project, including Dr. Kusum Singal (Scientist Medical Doctor, ICMR—Evidence Based Center for Child Health, Post Graduate Institute of Medical Education and Research, Chandigarh, India), Anirudha Agnihoty (Biomedical Sciences, Arthur A Dugoni School of Dentistry, University of the Pacific, San Francisco, United States), Muhammad Ayyan (King Edward Medical University, Pakistan), and Atiya Karim (London School of Hygiene and Tropical Medicine, University of London, London, United Kingdom). We thank Anneliese Arno (University College London, England) for granting complimentary access to Covidence. Lasse Østengaard also represents the University Library of Southern Denmark, University of Southern Denmark, Odense, Denmark. Israel Júnior Borges do Nascimento is affiliated with the School of Medicine and University Hospital at the Federal University of Minas Gerais, Belo Horizonte, Minas Gerais, Brazil. We thank Prf. Dr. Érika Amâncio Caetano (Department of Applied Linguistics at the Federal University of Minas Gerais, Brazil) for supporting and providing insights on the thematic analysis assessment. There was no funding for this project. D.N.-O., N.A.-M., and T.Z. are staff members of the WHO. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy, or views of the WHO.
Author contributions
All authors involved in this study participated in the conception of the work, analysis, or interpretation of data, drafting the manuscript and revising it, and approving its final version. In addition, all authors ensured that features related to the accuracy and integrity of reported information and knowledge were appropriately addressed in the final version. All authors guarantee the integrity of the work.
Data availability
The authors hereby declare that all pertinent data has already been displayed within the article. Additional data can be accessed upon request to Dr. Israel Júnior Borges do Nascimento (borgesi@who.int) or Dr. David Novillo-Ortiz (dnovillo@who.int).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41746-023-00899-4.
References
- 1.Beer P, Mulder RH. The effects of technological developments on work and their implications for continuous vocational education and training: a systematic review. Front. Psychol. 2020;11:918. doi: 10.3389/fpsyg.2020.00918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bronsoler, A., Doyle, J. & Van Reenen J. The Impact of New Technology on the Healthcare Workforce. 60. Available at https://workofthefuture.mit.edu/wp-content/uploads/2020/10/2020-Research-Brief-Bronsoler-Doyle-VanReenen.pdf.
- 3.Borges do Nascimento IJ, et al. The global effect of digital health technologies on health workers’ competencies and health workplace: an umbrella review of systematic reviews and lexical-based and sentence-based meta-analysis. Lancet Digit Health. 2023;5:e534–e544. doi: 10.1016/S2589-7500(23)00092-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Electronic Health Records Survey public use file national weighted estimates—NEHRS Survey Results and Products (2019). https://www.cdc.gov/nchs/data/nehrs/2019NEHRS-PUF-weighted-estimates-508.pdf.
- 5.Fischer SH, Ray KN, Mehrotra A, Bloom EL, Uscher-Pines L. Prevalence and Characteristics of Telehealth Utilization in the United States. JAMA Netw. Open. 2020;3:e2022302. doi: 10.1001/jamanetworkopen.2020.22302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan, M. N. et al. A Study to See the Effect of Social Media Usage Among Healthcare Providers. Cureus13, e16350. [DOI] [PMC free article] [PubMed]
- 7.Christopher Gibbons M. Use of health information technology among racial and ethnic underserved communities. Perspect. Health Inf. Manag. 2011;8:1f. [PMC free article] [PubMed] [Google Scholar]
- 8.Liu C, et al. Academia-industry digital health collaborations: a cross-cultural analysis of barriers and facilitators. Digit Health. 2019;5:2055207619878627. doi: 10.1177/2055207619878627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samarasekera U. The rise of racial minority health apps. Lancet Digit Health. 2022;4:e218–e219. doi: 10.1016/S2589-7500(22)00043-7. [DOI] [PubMed] [Google Scholar]
- 10.Vinzant DH, Vinzant JC. Strategy and organizational capacity: finding a fit. Public Product. Manag. Rev. 1996;20:139–157. [Google Scholar]
- 11.Lavoie-Tremblay M, Aubry M, Richer M-C, Cyr G. A health care project management office’s strategies for continual change and continuous improvement. Health Care Manag (Frederick) 2018;37:4–10. doi: 10.1097/HCM.0000000000000185. [DOI] [PubMed] [Google Scholar]
- 12.Pickens S, Solak J. Successful healthcare programs and projects: organization portfolio management essentials. J. Health. Inf. Manag. 2005;19:19–27. [PubMed] [Google Scholar]
- 13.World Health Organization. Global Strategy on Digital Health (WHO, 2020–2025). [DOI] [PMC free article] [PubMed]
- 14.Regional Committee for Europe, 72nd session. Seventy-second Regional Committee for Europe: Tel Aviv, 12–14 September 2022: Regional digital health action plan for the WHO European Region 2023–2030. World Health Organization. Regional Office for Europe (2022).
- 15.Schreiweis B, et al. Barriers and facilitators to the implementation of ehealth services: systematic literature analysis. J. Med. Internet Res. 2019;21:e14197. doi: 10.2196/14197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weißenfeld MM, Goetz K, Steinhäuser J. Facilitators and barriers for the implementation of telemedicine from a local government point of view - a cross-sectional survey in Germany. BMC Health Serv. Res. 2021;21:919. doi: 10.1186/s12913-021-06929-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jimbo M, et al. Perceived barriers and facilitators of using a Web-based interactive decision aid for colorectal cancer screening in community practice settings: findings from focus groups with primary care clinicians and medical office staff. J. Med. Internet Res. 2013;15:e286. doi: 10.2196/jmir.2914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Addotey-Delove M, Scott RE, Mars M. Healthcare workers’ perspectives of mHealth adoption factors in the developing world: scoping review. Int. J. Environ. Res. Public health. 2023;20:1244. doi: 10.3390/ijerph20021244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adepoju I-OO, Albersen BJA, De Brouwere V, van Roosmalen J, Zweekhorst M. mHealth for clinical decision-making in Sub-Saharan Africa: a scoping review. JMIR Mhealth Uhealth. 2017;5:e38. doi: 10.2196/mhealth.7185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alkhaldi O, McMillan B, Maddah N, Ainsworth J. Interventions aimed at enhancing health care providers’ behavior toward the prescription of mobile health apps: systematic review. JMIR mHealth uHealth. 2023;11:e43561. doi: 10.2196/43561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Rawashdeh, M., Keikhosrokiani, P., Belaton, B., Alawida, M. & Zwiri, A. IoT Adoption and application for smart healthcare: a systematic review. Sensors (Basel, Switzerland)22 (2022). [DOI] [PMC free article] [PubMed]
- 22.Agarwal S, Perry HB, Long L-A, Labrique AB. Evidence on feasibility and effective use of mHealth strategies by frontline health workers in developing countries: systematic review. Trop. Med. Int. Health. 2015;20:1003–1014. doi: 10.1111/tmi.12525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amoakoh-Coleman M, et al. Effectiveness of mHealth interventions targeting health care workers to improve pregnancy outcomes in low- and middle-income countries: a systematic review. J. Med. Internet Res. 2016;18:e226. doi: 10.2196/jmir.5533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arsad, F. S. et al. The impact of eHealth applications in healthcare intervention: a systematic review. J. Health Res.37 (2023).
- 25.Aslani, N. et al. Advantages and challenges of telecardiology and providing solutions for its successful implementation: a scoping review. Int. Cardiovascular Res. J.16 (2022).
- 26.Avoka, C. K., McArthur, E. & Banke-Thomas, A. Interventions to improve obstetric emergency referral decision making, communication, and feedback between health facilities in sub-Saharan Africa: a systematic review. Tropical Med. Int. Health10.1111/tmi.13747 (2022). [DOI] [PMC free article] [PubMed]
- 27.Baluszek JB, Wiig S, Myrnes-Hansen KV, Bronnick KK. Specialized healthcare practitioners’ challenges in performing video consultations to patients in Nordic Countries—a systematic review and narrative synthesis. BMC Health Serv. Res. 2022;22:1432. doi: 10.1186/s12913-022-08837-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bervell B, Al-Samarraie H. A comparative review of mobile health and electronic health utilization in sub-Saharan African countries. Soc. Sci. Med. 2019;232:1–16. doi: 10.1016/j.socscimed.2019.04.024. [DOI] [PubMed] [Google Scholar]
- 29.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv. Res. 2010;10:231. doi: 10.1186/1472-6963-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brommeyer M, Whittaker M, Mackay M, Ng F, Liang Z. Building health service management workforce capacity in the era of health informatics and digital health—a scoping review. Int. J. Med. Inform. 2023;169:104909. doi: 10.1016/j.ijmedinf.2022.104909. [DOI] [PubMed] [Google Scholar]
- 31.Braun R, Catalani C, Wimbush J, Israelski D. Community health workers and mobile technology: a systematic review of the literature. PLoS ONE. 2013;8:e65772. doi: 10.1371/journal.pone.0065772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brewster L, Mountain G, Wessels B, Kelly C, Hawley M. Factors affecting front line staff acceptance of telehealth technologies: a mixed-method systematic review. J. Adv. Nurs. 2014;70:21–33. doi: 10.1111/jan.12196. [DOI] [PubMed] [Google Scholar]
- 33.Brown J, Pope N, Bosco AM, Mason J, Morgan A. Issues affecting nurses’ capability to use digital technology at work: an integrative review. J. Clin. Nurs. 2020;29:2801–2819. doi: 10.1111/jocn.15321. [DOI] [PubMed] [Google Scholar]
- 34.Calleja, P., Wilkes, S., Spencer, M. & Woodbridge, S. Telehealth use in rural and remote health practitioner education: an integrative review. Rural Remote Health22 (2022). [DOI] [PubMed]
- 35.Cansdale LG, et al. Can mHealth improve recording of birth outcomes in LMICs—a scoping review. BJOG: Int. J. Obstet. Gynaecol. 2022;129:98–99. [Google Scholar]
- 36.Cartolovni A, Tomicic A, Lazic Mosler E. Ethical, legal, and social considerations of AI-based medical decision-support tools: a scoping review. Int. J. Med. Inform. 2022;161:104738. doi: 10.1016/j.ijmedinf.2022.104738. [DOI] [PubMed] [Google Scholar]
- 37.Celes, R. S., Rossi, T. R. A., De Barros, S. G., Santos, C. M. L. & Cardoso, C. Telehealth as state response strategy: systematic review. Rev. Panam. Salud Publica Pan Am. J. Public Health42 (2018). [DOI] [PMC free article] [PubMed]
- 38.Cen ZF, et al. Systematic literature review of adopting eHealth in pharmaceutical care during COVID-19 pandemic: recommendations for strengthening pharmacy services. BMJ Open. 2022;12:e066246. doi: 10.1136/bmjopen-2022-066246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chan WS, Leung AY. Use of social network sites for communication among health professionals: systematic review. J. Med. Internet Res. 2018;20:e117. doi: 10.2196/jmir.8382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen M, et al. Acceptance of clinical artificial intelligence among physicians and medical students: a systematic review with cross-sectional survey. Front. Med. 2022;9:990604. doi: 10.3389/fmed.2022.990604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Christensen LF, Moller AM, Hansen JP, Nielsen CT, Gildberg FA. Patients’ and providers’ experiences with video consultations used in the treatment of older patients with unipolar depression: a systematic review. J. Psychiatr. Ment. Health Nurs. 2020;27:258–271. doi: 10.1111/jpm.12574. [DOI] [PubMed] [Google Scholar]
- 42.da Costa CB, Peralta FDS, Ferreira de Mello ALS. How has teledentistry been applied in public dental health services? An integrative review. Telemed. J. E Health. 2020;26:945–954. doi: 10.1089/tmj.2019.0122. [DOI] [PubMed] [Google Scholar]
- 43.de Grood C, Raissi A, Kwon Y, Santana MJ. Adoption of e-health technology by physicians: a scoping review. J. Multidiscip. Health. 2016;9:335–344. doi: 10.2147/JMDH.S103881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Drissi N, et al. A systematic literature review on e-mental health solutions to assist health care workers during COVID-19. Telemed. J. E Health. 2021;27:594–602. doi: 10.1089/tmj.2020.0287. [DOI] [PubMed] [Google Scholar]
- 45.Dutta B, Hwang H-G. The adoption of electronic medical record by physicians: a PRISMA-compliant systematic review. Medicine (Baltimore) 2020;99:e19290. doi: 10.1097/MD.0000000000019290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Early J, Gonzalez C, Gordon-Dseagu V, Robles-Calderon L. Use of mobile health (mHealth) technologies and interventions among community health workers globally: a scoping review. Health Promot Pr. 2019;20:805–817. doi: 10.1177/1524839919855391. [DOI] [PubMed] [Google Scholar]
- 47.Ebneter AS, Sauter TC, Christen A, Eychmueller S. Feasibility, acceptability and needs in telemedicine for palliative care. Swiss Med. Wkly. 2022;152:w30148. doi: 10.4414/SMW.2022.w30148. [DOI] [PubMed] [Google Scholar]
- 48.Emmett, A., Kent, B., James, A. & March-McDonald, J. Experiences of health professionals towards using mobile electrocardiogram (ECG) technology: a qualitative systematic review. J. Clini. Nursing10.1111/jocn.16434 (2022). [DOI] [PubMed]
- 49.Ferdousi R, Arab-Zozani M, Tahamtan I, Rezaei-Hachesu P, Dehghani M. Attitudes of nurses towards clinical information systems: a systematic review and meta-analysis. Int Nurs. Rev. 2021;68:59–66. doi: 10.1111/inr.12603. [DOI] [PubMed] [Google Scholar]
- 50.Fletcher E, et al. Workload and workflow implications associated with the use of electronic clinical decision support tools used by health professionals in general practice: a scoping review. BMC Prim. Care. 2023;24:23. doi: 10.1186/s12875-023-01973-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ftouni R, AlJardali B, Hamdanieh M, Ftouni L, Salem N. Challenges of telemedicine during the COVID-19 pandemic: a systematic review. BMC Med. Inform. Decis. Mak. 2022;22:207. doi: 10.1186/s12911-022-01952-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gagnon M-P, et al. Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. J. Med Syst. 2012;36:241–277. doi: 10.1007/s10916-010-9473-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gagnon M-P, Ngangue P, Payne-Gagnon J, Desmartis M. m-Health adoption by healthcare professionals: a systematic review. J. Am. Med Inf. Assoc. 2016;23:212–220. doi: 10.1093/jamia/ocv052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Garvey, K. V. et al. Considering clinician competencies for the implementation of artificial intelligence–based tools in health care: findings from a scoping review. JMIR Med. Informatics10 (2022). [DOI] [PMC free article] [PubMed]
- 55.Garavand, A., Aslani, N., Nadri, H., Abedini, S. & Dehghan, S. Acceptance of telemedicine technology among physicians: a systematic review. Informatics Med. Unlocked30 (2022).
- 56.Ghimire, S., Martinez, S., Hartvigsen, G. & Gerdes, M. Virtual prenatal care: a systematic review of pregnant women’s and healthcare professionals’ experiences, needs, and preferences for quality care. Int. J. Med. Informatics170 (2023). [DOI] [PubMed]
- 57.Gonçalves, R. L. et al. Usability in telehealth systems for non-communicable diseases attention in primary care, from the COVID-19 pandemic onwards: a systematic review. J. Med. Internet Res.10.2196/44209 (2023). [DOI] [PMC free article] [PubMed]
- 58.Grant C, Jones A, Land H. What are the perspectives of speech pathologists, occupational therapists and physiotherapists on using telehealth videoconferencing for service delivery to children with developmental delays? A systematic review of the literature. Aust. J. Rural Health. 2022;30:321–336. doi: 10.1111/ajr.12843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hagström, J. et al. Views, use, and experiences of web-based access to pediatric electronic health records for children, adolescents, and parents: scoping review. J. Med. Internet Res.24 (2022). [DOI] [PMC free article] [PubMed]
- 60.Huang, R., Li, H., Suomi, R., Li, C. & Peltoniemi, T. Intelligent physical robots in health care: systematic literature review. J. Med. Internet Res.25 (2023). [DOI] [PMC free article] [PubMed]
- 61.Ionescu A, De Jong PGM, Drop SLS, Van Kampen SC. A scoping review of the use of e-learning and e-consultation for healthcare workers in low- and middle-income countries and their potential complementarity. J. Am. Med. Inform. Assoc. 2022;29:713–722. doi: 10.1093/jamia/ocab271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Isidori V, et al. Digital technologies and the role of health care professionals: scoping review exploring nurses’ skills in the digital era and in the light of the COVID-19 pandemic. JMIR Nurs. 2022;5:e37631. doi: 10.2196/37631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ismatullaev, U. V. U. & Kim, S. H. Review of the factors affecting acceptance of AI-infused systems. Human Factors. 10.1177/00187208211064707 (2022). [DOI] [PubMed]
- 64.Jacob C, Sanchez-Vazquez A, Ivory C. Social, organizational, and technological factors impacting clinicians’ adoption of mobile health tools: systematic literature review. JMIR Mhealth Uhealth. 2020;8:e15935. doi: 10.2196/15935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jimenez, G. et al. Digital health competencies for primary healthcare professionals: a scoping review. Int. J. Med. Informatics143 (2020). [DOI] [PubMed]
- 66.Jimma BL, Enyew DB. Barriers to the acceptance of electronic medical records from the perspective of physicians and nurses: a scoping review. Inform. Med. unlocked. 2022;31:100991. doi: 10.1016/j.imu.2022.100991. [DOI] [Google Scholar]
- 67.Joo JY. Nurse-led telehealth interventions during COVID-19: a scoping review. Comput. Inform. Nurs. 2022;40:804–813. doi: 10.1097/CIN.0000000000000962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jonasdottir, S. K., Thordardottir, I. & Jonsdottir, T. Health professionals? Perspective towards challenges and opportunities of telehealth service provision: a scoping review. Int. J. Med. Informatics167 (2022). [DOI] [PubMed]
- 69.Jose A, Tortorella GL, Vassolo R, Kumar M, Mac Cawley AF. Professional competence and its effect on the implementation of healthcare 4.0 technologies: scoping review and future research directions. Int. J. Environ. Res. Public Health. 2023;20:478. doi: 10.3390/ijerph20010478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kane, H. et al. Opportunities and challenges for professionals in psychiatry and mental health care using digital technologies during the COVID-19 pandemic: systematic review. JMIR Human Factors9 (2022). [DOI] [PMC free article] [PubMed]
- 71.Zhang, K. K. & Thompson, A. W. Effectiveness of electronic learning for continuing interprofessional education on behavior change of healthcare professionals: a scoping review. J. Interprofessional Care 1–11. 10.1080/13561820.2022.2071850 (2022) [DOI] [PubMed]
- 72.Keyworth C, Hart J, Armitage CJ, Tully MP. What maximizes the effectiveness and implementation of technology-based interventions to support healthcare professional practice? A systematic literature review. BMC Med. Inf. Decis. Mak. 2018;18:93. doi: 10.1186/s12911-018-0661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Koivunen M, Saranto K. Nursing professionals’ experiences of the facilitators and barriers to the use of telehealth applications: a systematic review of qualitative studies. Scand. J. Caring Sci. 2018;32:24–44. doi: 10.1111/scs.12445. [DOI] [PubMed] [Google Scholar]
- 74.Kolla A, Lim S, Zanowiak J, Islam N. The role of health informatics in facilitating communication strategies for community health workers in clinical settings: a scoping review. J. Public Health Manag Pr. 2021;27:E107–E118. doi: 10.1097/PHH.0000000000001092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Konnyu KJ, et al. Changes to prenatal care visit frequency and telehealth: a systematic review of qualitative evidence. Obstet. Gynecol. 2023;141:299–323. doi: 10.1097/AOG.0000000000005046. [DOI] [PubMed] [Google Scholar]
- 76.Kruse, C. S. et al. Physician burnout and the electronic health record leading up to and during the first year of Covid-19: systematic review. J. Med. Internet Res.24 (2022). [DOI] [PMC free article] [PubMed]
- 77.Laar, A. S., Harris, M. L., Shifti, D. M. & Loxton, D. Perspectives of health care professionals’ on delivering mHealth sexual and reproductive health services in rural settings in low-and-middle-income countries: a qualitative systematic review. BMC Health Services Research22 (2022). [DOI] [PMC free article] [PubMed]
- 78.Lam K, et al. Machine learning for technical skill assessment in surgery: a systematic review. NPJ digital Med. 2022;5:24. doi: 10.1038/s41746-022-00566-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lampickienė, I. & Davoody, N. Healthcare professionals’ experience of performing digital care visits—a scoping review. Life (Basel, Switzerland)12 (2022). [DOI] [PMC free article] [PubMed]
- 80.Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre CR. Health care provider adoption of ehealth: systematic literature review. Interact. J. Med. Res. 2013;2:e7. doi: 10.2196/ijmr.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li L, Cotton A. A systematic review of nurses’ perspectives toward the telemedicine intensive care unit: a basis for supporting its future implementation in China? Telemed. J. E Health. 2019;25:343–350. doi: 10.1089/tmj.2018.0006. [DOI] [PubMed] [Google Scholar]
- 82.Lluch M. Healthcare professionals’ organisational barriers to health information technologies-a literature review. Int. J. Med. Inf. 2011;80:849–862. doi: 10.1016/j.ijmedinf.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 83.Longhini J, Rossettini G, Palese A. Correction: digital health competencies among health care professionals: systematic review. J. Med. Internet Res. 2022;24:e43721. doi: 10.2196/43721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martin G, et al. The impact of mobile technology on teamwork and communication in hospitals: a systematic review. J. Am. Med. Inf. Assoc. 2019;26:339–355. doi: 10.1093/jamia/ocy175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Marvaso, G. et al. Virtual and augmented reality as a novel opportunity to unleash the power of radiotherapy in the digital era: a scoping review. Appl. Sci. (Switzerland)12 (2022).
- 86.Meunier PY, Raynaud C, Guimaraes E, Gueyffier F, Letrilliart L. Barriers and facilitators to the use of clinical decision support systems in primary care: a mixed-methods systematic review. Ann. Fam. Med. 2023;21:57–69. doi: 10.1370/afm.2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Moore EC, Tolley CL, Bates DW, Slight SP. A systematic review of the impact of health information technology on nurses’ time. J. Am. Med Inf. Assoc. 2020;27:798–807. doi: 10.1093/jamia/ocz231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Muhiyaddin R, Abd-Alrazaq AA, Househ M, Alam T, Shah Z. The Impact of Clinical Decision Support Systems (CDSS) on physicians: a scoping review. Stud. Health Technol. Inf. 2020;272:470–473. doi: 10.3233/SHTI200597. [DOI] [PubMed] [Google Scholar]
- 89.Mulita, F., Verras, G. I., Anagnostopoulos, C. N. & Kotis, K. A Smarter health through the internet of surgical things. Sensors (Basel, Switzerland)22 (2022). [DOI] [PMC free article] [PubMed]
- 90.Namasivayam P, et al. The use of telehealth in the provision of after-hours palliative care services in rural and remote Australia: A scoping review. PLoS ONE. 2022;17:e0274861. doi: 10.1371/journal.pone.0274861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nezamdoust S, Abdekhoda M, Ranjbaran F, Azami-Aghdash S. Adopting mobile health applications by nurses: a scoping review. J. Res. Nurs. 2022;27:480–491. doi: 10.1177/17449871221077080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nguyen OT, et al. A systematic review of contributing factors of and solutions to electronic health record-related impacts on physician well-being. J. Am. Med Inf. Assoc. 2021;28:974–984. doi: 10.1093/jamia/ocaa339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Niazkhani Z, Toni E, Cheshmekaboodi M, Georgiou A, Pirnejad H. Barriers to patient, provider, and caregiver adoption and use of electronic personal health records in chronic care: a systematic review. BMC Med Inf. Decis. Mak. 2020;20:153. doi: 10.1186/s12911-020-01159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.O’Connor, S. et al. Artificial intelligence in nursing and midwifery: a systematic review. J. Clinical Nursing. 10.1111/jocn.16478 (2022). [DOI] [PubMed]
- 95.Odendaal, W. et al. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database Syst. Rev. 10.1002/14651858.CD011942.pub2 (2020). [DOI] [PMC free article] [PubMed]
- 96.Osman MA, et al. Barriers and facilitators for implementation of electronic consultations (eConsult) to enhance access to specialist care: a scoping review. BMJ Glob. Health. 2019;4:e001629. doi: 10.1136/bmjgh-2019-001629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Papadopoulos I, Koulouglioti C, Ali S. Views of nurses and other health and social care workers on the use of assistive humanoid and animal-like robots in health and social care: a scoping review. Contemp. Nurse. 2018;54:425–442. doi: 10.1080/10376178.2018.1519374. [DOI] [PubMed] [Google Scholar]
- 98.Police RL, Foster T, Wong KS. Adoption and use of health information technology in physician practice organisations: systematic review. Inf. Prim. Care. 2010;18:245–258. doi: 10.14236/jhi.v18i4.780. [DOI] [PubMed] [Google Scholar]
- 99.Prakash, S., Balaji, J. N., Joshi, A. & Surapaneni, K. M. Ethical conundrums in the application of Artificial Intelligence (AI) in healthcare—a scoping review of reviews. J. Personalized Med.12 (2022). [DOI] [PMC free article] [PubMed]
- 100.Rahal RM, Mercer J, Kuziemsky C, Yaya S. Factors affecting the mature use of electronic medical records by primary care physicians: a systematic review. BMC Med Inf. Decis. Mak. 2021;21:67. doi: 10.1186/s12911-021-01434-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ramachandran HJ, et al. Barriers and facilitators to the adoption of digital health interventions for COPD management: a scoping review. Heart Lung: J. Crit. Care. 2023;59:117–127. doi: 10.1016/j.hrtlng.2023.02.004. [DOI] [PubMed] [Google Scholar]
- 102.Ratshidi, L., Grobbelaar, S. & Botha, A. Conceptualising the factors influencing community health workers’ preparedness for ICT implementation: a systematised scoping review. Sustainability (Switzerland)14 (2022).
- 103.Vukušić Rukavina T, et al. Dangers and benefits of social media on e-professionalism of health care professionals: scoping review. J. Med. Internet Res. 2021;23:e25770. doi: 10.2196/25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Saigí-Rubió F, et al. The current status of telemedicine technology use across the World Health Organization European Region: an overview of systematic reviews. J. Med. Internet Res. 2022;24:e40877. doi: 10.2196/40877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sipanoun, P., Oulton, K., Gibson, F. & Wray, J. The experiences and perceptions of users of an electronic patient record system in a pediatric hospital setting: a systematc review. Int. J. Med. Informatics160, (2022). [DOI] [PubMed]
- 106.Sullivan-Tibbs MA, et al. Social work’s response during the COVID-19 pandemic: a systematic literature review—balancing telemedicine with social work self-care during a pandemic. Soc. Work Public Health. 2022;37:499–509. doi: 10.1080/19371918.2022.2032904. [DOI] [PubMed] [Google Scholar]
- 107.Tabaeeian, R. A., Hajrahimi, B. & Khoshfetrat, A. A systematic review of telemedicine systems use barriers: primary health care providers’ perspective. J. Sci. Technol. Policy Manag. 10.1108/JSTPM-07-2021-0106 (2022).
- 108.Tegegne MD, et al. Electronic medical record system use and determinants in ethiopia: systematic review and meta-analysis. Interact. J. Med. Res. 2023;12:e40721. doi: 10.2196/40721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tickner C, Heinsch M, Brosnan C, Kay-Lambkin F. “Another tool in our toolbox”: a scoping review of the use of eHealth technologies in health social work practice. Soc. Work Health Care. 2023;62:1–18. doi: 10.1080/00981389.2022.2163450. [DOI] [PubMed] [Google Scholar]
- 110.Torres-Castano, A. et al. Ethical, legal, organisational and social issues of teleneurology: a scoping review. Int. J. Environ. Res. Public Health20 (2023). [DOI] [PMC free article] [PubMed]
- 111.Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J. Am. Med Inf. Assoc. 2005;12:505–516. doi: 10.1197/jamia.M1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Vejdani M, et al. Electronic prescription system requirements: a scoping review. BMC Med. Inform. Decis. Mak. 2022;22:231. doi: 10.1186/s12911-022-01948-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Verma P, Kerrison R. Patients’ and physicians’ experiences with remote consultations in primary care during the COVID-19 pandemic: a multi-method rapid review of the literature. BJGP Open. 2022;6:BJGPO.2021.0192. doi: 10.3399/BJGPO.2021.0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.von Wedel, P. & Hagist, C. Economic value of data and analytics for health care providers: Hermeneutic systematic literature review. J. Med. Internet Res. 22, (2020). [DOI] [PMC free article] [PubMed]
- 115.Walle AD, et al. Readiness to use electronic medical record systems and its associated factors among health care professionals in Ethiopia: A systematic review and meta-analysis. Inform. Med. Unlocked. 2023;36:101140. doi: 10.1016/j.imu.2022.101140. [DOI] [Google Scholar]
- 116.Walsh L, Hong SC, Chalakkal RJ, Ogbuehi KC. A systematic review of current teleophthalmology services in new zealand compared to the four comparable countries of the United Kingdom, Australia, united states of America (USA) and Canada. Clin. Ophthalmol. 2021;15:4015–4027. doi: 10.2147/OPTH.S294428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wisner K, Lyndon A, Chesla CA. The electronic health record’s impact on nurses’ cognitive work: An integrative review. Int J. Nurs. Stud. 2019;94:74–84. doi: 10.1016/j.ijnurstu.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 118.Xyrichis A, et al. Healthcare stakeholders’ perceptions and experiences of factors affecting the implementation of critical care telemedicine (CCT): qualitative evidence synthesis. Cochrane Database Syst. Rev. 2021;2:CD012876. doi: 10.1002/14651858.CD012876.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Young LB, Chan PS, Cram P. Staff acceptance of tele-ICU coverage: a systematic review. Chest. 2011;139:279–288. doi: 10.1378/chest.10-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zakerabasali S, Ayyoubzadeh SM, Baniasadi T, Yazdani A, Abhari S. Mobile health technology and healthcare providers: systemic barriers to adoption. Health. Inf. Res. 2021;27:267–278. doi: 10.4258/hir.2021.27.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang J, Lu V, Khanduja V. The impact of extended reality on surgery: a scoping review. Int. Orthop. 2023;47:611–621. doi: 10.1007/s00264-022-05663-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang Z, et al. Smart glasses for supporting distributed care work: systematic review. JMIR Med. Inform. 2023;11:e44161. doi: 10.2196/44161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Davis MM, Freeman M, Kaye J, Vuckovic N, Buckley DI. A systematic review of clinician and staff views on the acceptability of incorporating remote monitoring technology into primary care. Telemed. J. E Health. 2014;20:428–438. doi: 10.1089/tmj.2013.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nizeyimana, E., Joseph, C., Plastow, N., Dawood, G. & Louw, Q. A. A scoping review of feasibility, cost, access to rehabilitation services and implementation of telerehabilitation: Implications for low- and middle-income countries. Digital Health8 (2022). [DOI] [PMC free article] [PubMed]
- 125.Thomas Craig KJ, Willis VC, Gruen D, Rhee K, Jackson GP. The burden of the digital environment: a systematic review on organization-directed workplace interventions to mitigate physician burnout. J. Am. Med Inf. Assoc. 2021;28:985–997. doi: 10.1093/jamia/ocaa301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Borges do Nascimento, I. J. Barriers, facilitators, and recommendations visual mind mapping. https://gitmind.com/app/docs/mv5g6b6x.
- 127.Svendsen, M. T., Tiedemann, S. N. & Andersen, K. E. Pros and cons of eHealth: a systematic review of the literature and observations in Denmark. SAGE Open Med. 9 (2021). [DOI] [PMC free article] [PubMed]
- 128.Powell KR. Patient-perceived facilitators of and barriers to electronic portal use: a systematic review. Comput. Inf. Nurs. 2017;35:565–573. doi: 10.1097/CIN.0000000000000377. [DOI] [PubMed] [Google Scholar]
- 129.O’Connor S, et al. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies. BMC Med. Inf. Decis. Mak. 2016;16:120. doi: 10.1186/s12911-016-0359-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Miller DG, Pierson L, Doernberg S. The role of medical students during the COVID-19 pandemic. Ann. Intern. Med. 2020;173:145–146. doi: 10.7326/M20-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Menon, A., Klein, E. J., Kollars, K. & Kleinhenz, A. L. W. Medical students are not essential workers: examining institutional responsibility during the COVID-19 pandemic. Acad. Med.10.1097/ACM.0000000000003478 (2020) [DOI] [PMC free article] [PubMed]
- 132.Bower BL, Hardy KP. From correspondence to cyberspace: changes and challenges in distance education. N. Directions Community Coll. 2004;2004:5–12. doi: 10.1002/cc.169. [DOI] [Google Scholar]
- 133.Bethany D. W., Gattenberg R. W., & Freed K. ‘Societal Issues in Distance Learning’, September 2001, University of South Florida and ‘Technological Rug down the Hallways of Distance Education’. Wikipedia (2001).
- 134.Soumik Sarka. A. Brief History of Online Education. Adamas Universityhttps://adamasuniversity.ac.in/a-brief-history-of-online-education/ (2020).
- 135.Deepika V, Soundariya K, Karthikeyan K, Kalaiselvan G. ‘Learning from home’: role of e-learning methodologies and tools during novel coronavirus pandemic outbreak. Postgrad. Med. J. 2021;97:590–597. doi: 10.1136/postgradmedj-2020-137989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Grafton-Clarke C, et al. Pivot to online learning for adapting or continuing workplace-based clinical learning in medical education following the COVID-19 pandemic: A BEME systematic review: BEME Guide No. 70. Med. Teach. 2022;44:227–243. doi: 10.1080/0142159X.2021.1992372. [DOI] [PubMed] [Google Scholar]
- 137.Jhurree, V. Technology integration in education in developing countries: Guidelines to policy makers. Int. Educ. J.6, 467–483.
- 138.Hipkins, C. New digital technologies for schools and kura. The Beehivehttps://www.beehive.govt.nz/release/new-digital-technologies-schools-and-kura.
- 139.Chang J, et al. Real-time display of laboratory testing status improves satisfaction levels in an emergency department: A pilot study. J. Clin. Lab Anal. 2020;34:e23290. doi: 10.1002/jcla.23290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Overhage JM, Suico J, McDonald CJ. Electronic laboratory reporting: barriers, solutions and findings. J. Public Health Manag. Pr. 2001;7:60–66. doi: 10.1097/00124784-200107060-00007. [DOI] [PubMed] [Google Scholar]
- 141.EUROSTAT - Statistics Explained. Cloud computing—statistics on the use by enterprises. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Cloud_computing_-_statistics_on_the_use_by_enterprises (2021).
- 142.Cismondi F, et al. Reducing unnecessary lab testing in the ICU with artificial intelligence. Int J. Med. Inf. 2013;82:345–358. doi: 10.1016/j.ijmedinf.2012.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Noblin A, Cortelyou-Ward K, Servan RM. Cloud computing and patient engagement: leveraging available technology. J. Med. Pr. Manag. 2014;30:89–93. [PubMed] [Google Scholar]
- 144.Pollock M, et al. Preferred Reporting Items for Overviews of Reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst. Rev. 2019;8:335. doi: 10.1186/s13643-019-1252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Higgins J. P. T. et al. (eds) Cochrane Handbook for Systematic Reviews of Interventions version 6.3. (Cochrane, 2022). Available from www.training.cochrane.org/handbook.
- 147.Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid. Based Ment. Health. 2018;21:95–100. doi: 10.1136/ebmental-2018-300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cornell JE, Laine C. The science and art of deduction: complex systematic overviews. Ann. Intern. Med. 2008;148:786–788. doi: 10.7326/0003-4819-148-10-200805200-00012. [DOI] [PubMed] [Google Scholar]
- 149.World Health Organization. Digital Health—draft Resolution Proposed by Algeria, Australia, Brazil, Estonia, Ethiopia, Germany, India, Indonesia, Israel, Italy, Luxembourg, Mauritius, Morocco, Panama, Philippines and South Africa (WHO, 2018).
- 150.World Health Organization. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening (WHO, 2019). [PubMed]
- 151.Jiang Y, et al. Predicting peritoneal recurrence and disease-free survival from CT images in gastric cancer with multitask deep learning: a retrospective study. Lancet Digit Health. 2022;4:e340–e350. doi: 10.1016/S2589-7500(22)00040-1. [DOI] [PubMed] [Google Scholar]
- 152.Venkateswaran M, et al. A digital health registry with clinical decision support for improving quality of antenatal care in Palestine (eRegQual): a pragmatic, cluster-randomised, controlled, superiority trial. Lancet Digit Health. 2022;4:e126–e136. doi: 10.1016/S2589-7500(21)00269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Covidence systematic review software. Melbourne, Australia: Veritas Health Innovation. www.covidence.org. Covidence.
- 154.Shea BJ, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Microsoft Corporation. (2018). Microsoft Excel. Retrieved from https://office.microsoft.com/excel.
- 156.van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523–538. doi: 10.1007/s11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12:181. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Jackson, K. & Bazeley, P. Qualitative Data Analysis with NVivo. (3rd Edition) (Sage Publications, 2019).
- 160.Borges do Nascimento IJ, et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect. Dis. 2021;21:525. doi: 10.1186/s12879-021-06214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lewin S, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13:2. doi: 10.1186/s13012-017-0688-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors hereby declare that all pertinent data has already been displayed within the article. Additional data can be accessed upon request to Dr. Israel Júnior Borges do Nascimento (borgesi@who.int) or Dr. David Novillo-Ortiz (dnovillo@who.int).