Highlights
-
•
Few studies have examined the effects of public health funding on COVID-19 outcomes.
-
•
We linked national survey datasets with county-level COVID-19 surveillance data.
-
•
Public health expenditures varied widely across U.S. counties, even within states.
-
•
County public health expenditures were associated with decreased COVID-19 burden.
-
•
Community health planning activities had weaker associations with COVID-19 burden.
Keywords: Public Health Finance, Social Determinants of Health, Data Linkage, Public Health Infrastructure, Local Health Departments, COVID-19
Abstract
The COVID-19 pandemic has revealed consequences of past defunding of the U.S. public health system, but the extent to which public health infrastructure is associated with COVID-19 burden is unknown. We aimed to determine whether previous county-level public health expenditures and community health planning activities are associated with COVID-19 cases and deaths. We examined 3050 of 3143 U.S. counties and county equivalents from March 1, 2020 to February 28, 2022. Multivariable-adjusted linear regression and generalized additive models were used to estimate associations between county-level public health expenditures and completion of community health planning activities by a county health department with outcomes of county-level COVID-19 cases and deaths per 100,000 population. After adjusting for county-level covariates, counties in the highest tertile of public health expenditures per capita had on average 542 fewer COVID-19 cases per 100,000 population (95% CI, −1004 to −81) and 21 fewer deaths per 100,000 population (95% CI, –32 to −10) than counties in the lowest tertile. For analyses of community health planning activities, adjusted estimates of association remained negative for COVID-19 deaths, but confidence intervals included negative and positive values. In conclusion, higher levels of local public health expenditures and community health planning activities were associated with fewer county-level COVID-19 deaths, and to a lesser extent, cases. Future public health funding should be aligned with evidence for the value of county health departments programs and explore further which types of spending are most cost effective.
1. Introduction
From the beginning of the coronavirus disease 2019 (COVID-19) pandemic and into 2022, the United States (U.S.) consistently experienced higher COVID-19 and all-cause mortality as compared to other peer countries in the Organisation for Economic Co-operation and Development (OECD). (Bilinski and Emanuel, 2020, Bilinski et al., 2023) This increase in deaths has further widened the long-standing mortality and life expectancy gaps between the U.S. and other developed countries. (Heuveline and Lanza Queiroz, 2023, Bor et al., 20232023, Woolf, 2023) Therefore, examining what worked and what did not work to prevent cases and deaths from COVID-19 offers opportunities for learning how future funding and programs can best be spent to prevent future cases and deaths from COVID-19 as well as other emerging infectious diseases and public health threats. (Freeman, 2021) As emphasized in a 2021 report by the National Academy of Medicine (formerly the Institute of Medicine), the future of public health post-COVID-19-pandemic requires adequate funding resources and community partnerships. (DeSalvo et al.,) Thus, there is a need to understand the understudied roles of public health expenditures and community health planning.
Despite extensive literature on hospital medical expenditures, less research has examined the impact of non-hospital or public health expenditures. (Edwards et al., 2013) Public health expenditures per capita vary widely across U.S. counties, and increases in public health expenditures are associated with decreased all-cause mortality, improved county-level health rankings, and numerous other health outcomes. (Leider et al., 2018, McCullough and Leider, 2016, Singh, 2014) However, public health has been underfunded over several decades in the U.S., leaving populations potentially more vulnerable to COVID-19. (Maani and Galea, 2020, Alfonso et al., 2021) The U.S. spends less on prevention and public health services relative to overall health expenditures as compared to other OECD countries such as Canada, Italy, and South Korea, (Gmeinder et al., 2017) while median per-capita spending among U.S. local health departments decreased by 25% from 2008 to 2016. (Hoornbeek et al., 2019) Public health expenditures may provide a proxy measure of public health infrastructure, preparedness, and disposition for handling impacts of the pandemic.
In the landmark 1988 Institute of Medicine report The Future of Public Health, local assessments of health and subsequent actions are deemed core functions of public health. (Institute of Medicine (US) Committee for the Study of the Future of Public Health) Local health departments can voluntarily apply for accreditation by the Public Health Accreditation Board if they complete a community health assessment and improvement plan every five years, among other requirements. (Shah et al., 2015) Completion of these community health planning activities by local health departments is associated with increased delivery of chronic disease prevention programs: a proxy of a public health system’s decision-making capacity and ability to act. (Rabarison et al., 2015) Local health departments with such activities may have greater understanding and trust of the community whom they serve, and therefore better positioned to mitigate the effects of COVID-19 within their jurisdictions.
Our study aimed to provide evidence on potential areas to bolster U.S. public health infrastructure by examining relationships between public health expenditures, community health planning activities, and COVID-19 burden. We hypothesized that increased prior county-level public health expenditures and implementation of community health planning activities by respective county health departments are associated with decreased county-level COVID-19 cases and deaths. By examining both expenditures and community health activities, instead of either one alone, we can study their independent effects.
2. Methods
2.1. Data sources & variables
We linked national surveys with COVID-19 surveillance data to conduct a series of cross-sectional studies on associations between county-level public health expenditures per capita and community health planning activities with COVID-19 incidence and mortality. The Stanford University Institutional Review Board approved this study.
Our outcome variables were county-level COVID-19 cases and deaths per 100,000 population from March 1, 2020 to February 28, 2022. These public data come from Johns Hopkins University Center for Systems Science and Engineering and USAFacts. (Dong et al., 2020, USAFacts) Because the state of Nebraska discontinued their daily COVID-19 dashboard in June 2021 leading to underreported numbers, we excluded Nebraskan counties from our analyses. Our final analyses on public health expenditures included 3050 out of 3143 U.S. counties and county equivalents. To adjust for other sources of variation, we included county-level variables previously identified as key risk factors for COVID-19 infection and mortality, (Chin et al., 2020) including: percentages of population over 70 years old; living under poverty line; living in group quarters; with race alone or in combination (American Indian and Alaska Native, Asian, Black or African American, Native Hawaiian and Other Pacific Islander) and Hispanic ethnicity; living alone over 65 years old; with broadband internet; and between 18 and 64 years old without health insurance; as well as median household income; total county expenditures per capita; in-patient costs per capita; prevalence of diabetes; coronary heart disease and hypertension-related hospitalizations; average household size; percentage of households with grandparents living with grandchildren; percentage of households that are renter-occupied; population size; population density; number of hospital and ICU beds; premature mortality (years of potential life lost before age 75); and U.S. Census Region. Missing data were imputed via random forest imputation.
Our first exposure variable was county-level public health expenditures per capita. Data on public health expenditures were derived from the U.S. Census Bureau’s 2017 Census of Governments, a survey conducted every 5 years collecting detailed finance data from all 87,000 + units of local government across the U.S. (U.S. Census Bureau. Census of Governments) Throughout this paper, “public health expenditures” will refer to public health expenditures per capita.
Our second exposure variable was implementation of community health planning activities (community health assessment and improvement plan) by the respective county health department within three years prior to 2019, similar to previous research. (Rabarison et al., 2015) These data come from the 2019 National Profile of Local Health Departments Study (2019 Profile Study) conducted by the National Association of County and City Health Officials (NACCHO) (National Association of County and City Health Officials). After excluding counties in Nebraska, our final study sample included 1728 counties. We included covariates previously identified as local health department characteristics related to public health service delivery. (Rabarison et al., 2015) Additional details on variable definitions, selection, and missingness are described in the online supplement (Supplemental Methods).
2.2. Analytic strategy
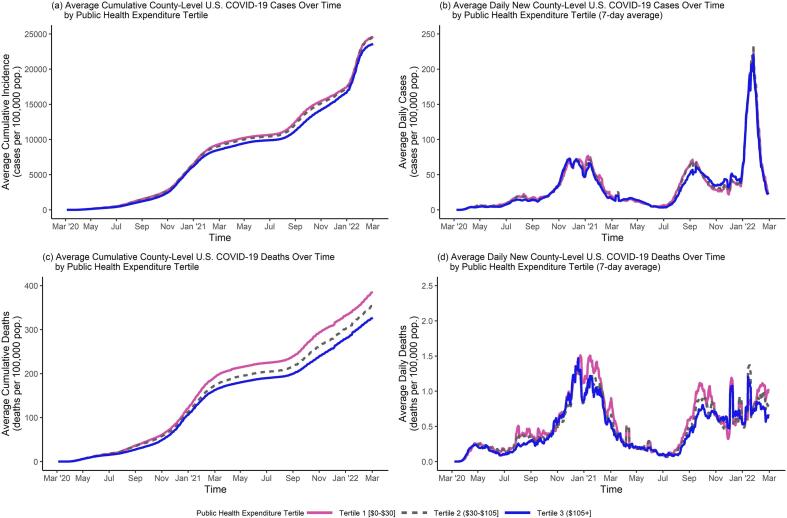
We divided counties into tertiles of public health expenditures (cut-points: $30 and $105) and calculated descriptive statistics. To assess for geographic variations, we mapped intersections of public health expenditures and COVID-19 measures. We also plotted time series of average daily COVID-19 measures by public health expenditure tertile and community health assessment implementation.
To estimate associations between public health expenditure tertile and COVID-19 measures, we conducted unadjusted and multivariable-adjusted regression models. We estimated linear models by regressing cumulative COVID-19 measures on public health expenditure tertile (Tertile 1, lowest, as reference) using the dataset of 3050 counties and controlled for aforementioned covariates. With confounding variables defined as variables that affect both exposure and outcome, (Lash et al., 2020) we did not control for COVID-19 policies or vaccination rates because those occurred after the advent of COVID-19 and therefore cannot affect pre-pandemic public health expenditures (Supplemental Fig. 1). As sensitivity analyses to assess whether associations between public health expenditure tertiles and COVID-19 differed over time, we examined COVID-19 measures in 2-month periods, resulting in 12 time periods spanning from March 2020 to February 2022. Given there may be non-linear relationships between public health expenditures and COVID-19 measures, we also used generalized additive models to regress overall COVID-19 outcomes on a continuous measure of public health expenditures. (Wood, 2017) To estimate associations between community health planning activities with COVID-19 burden, we adopted a similar linear regression approach using the sample of 1728 counties from NACCHO’s 2019 Profile Study. All analyses were performed using R. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
3. Results
3.1. Descriptive analyses
County characteristics are summarized by public health expenditure tertile in Table 1. The overall mean (SD) of public health expenditure per capita was $133 ($375) and for lowest, middle, and highest tertiles were $11 ($9), $63 ($22), and $317 ($599), respectively. Density plots of public health expenditure are shown in Supplemental Fig. 2. Geographic distributions are found in Supplemental Table 2. Many county-level covariates differed across tertiles. For example, mean (SD) proportions (%) of population living under the poverty line (Tertile 1: 16.9 (6.8); Tertile 2: 15.9 (6.2); Tertile 3: 15.3 (5.8)), hospitalization rates for hypertension per 1,000 Medicare beneficiaries (Tertile 1: 141.6 (37.3); Tertile 2: 132.3 (39.4); Tertile 3: 126.4 (40.4)), and number of intensive care unit beds per 100,000 population (Tertile 1: 9.7 (18.2); Tertile 2: 12.3 (23.8); Tertile 3: 13.0 (41.1)). The overall mean (SD) cumulative number of COVID-19 cases was 24,202 (5700) per 100,000 population and for deaths was 355 (155) per 100,000 population, while the number of average cases and deaths decreased from lowest to highest public health expenditure tertiles.
Table 1.
Descriptive Statistics for U.S. Counties by Public Health Expenditure Tertile from March 1, 2020 to February 28, 2022.
| Characteristics | Overall n = 3050Mean (SD) |
Tertile 1 (Lowest) n = 976Mean (SD) |
Tertile 2 n = 1029 Mean (SD) |
Tertile 3 (Highest) n = 1045 Mean (SD) |
|---|---|---|---|---|
| County-level Characteristics | ||||
| Public health expenditures,a 2017 ($ per capita) | 133 (375) | 11 (9) | 63 (22) | 317 (599) |
| In-patient hospital expenditures, all CMS beneficiaries,b 2019 ($ per capita) | 3213 (640) | 3231 (652) | 3165 (581) | 3242 (681) |
| Population over 70 years old,c 2018 (%) | 13.1 (3.5) | 13.0 (3.5) | 12.9 (3.4) | 13.2 (3.5) |
| Population living under poverty line,d 2016 (%) | 16.0 (6.3) | 16.9 (6.8) | 15.9 (6.2) | 15.3 (5.8) |
| Living in group quarters,a 2018 (%) | 3.6 (4.6) | 3.7 (5.1) | 3.5 (4.7) | 3.4 (4) |
| Median household income,a 2016 ($) | 49,479 (13021) | 47,725 (13403) | 49,613 (12705) | 50,986 (12780) |
| Total county expenditures,a 2017 ($ per capita) | 25669.6 (33523.7) | 19679.1 (19323.5) | 25629.9 (39800.2) | 31303.6 (36171.1) |
| Proportion American Indian and Alaska Native race,a 2018 (%) | 3.3 (8.4) | 3.9 (10.9) | 3.3 (8.1) | 2.8 (5.3) |
| Proportion Asian race,a 2018 (%) | 2.1 (3.6) | 1.7 (3.5) | 2.0 (3.3) | 2.4 (3.8) |
| Proportion Black or African American race,a 2018 (%) | 10.5 (14.7) | 11.8 (15.3) | 11.0 (15.5) | 8.7 (13.3) |
| Proportion Native Hawaiian and Other Pacific Islander race,a 2018 (%) | 0.3 (1.4) | 0.3 (2.4) | 0.2 (0.8) | 0.2 (0.3) |
| Proportion Hispanic ethnicity,a 2018 (%) | 9.7 (14) | 9.9 (15) | 9.1 (13.3) | 10.1 (13.7) |
| Diabetes prevalence,d 2016 (%) | 10.4 (3.8) | 11.1 (4) | 10.5 (3.8) | 9.7 (3.5) |
| Medicare CHD hospitalization rate,d 2014–2016 (per 1,000 capita) | 70.9 (23.5) | 75.7 (22) | 69.9 (23.2) | 67.5 (24.4) |
| Medicare hypertension hospitalization rate,d 2014–2016 (per 1,000 capita) | 133.3 (39.6) | 141.6 (37.2) | 132.3 (39.4) | 126.4 (40.5) |
| Average household size,a 2018 (n) | 2.5 (0.3) | 2.6 (0.3) | 2.5 (0.3) | 2.5 (0.3) |
| Living alone and over 65 years old,a 2018 (%) | 12.5 (3.1) | 12.5 (3) | 12.4 (3.1) | 12.7 (3.1) |
| Households with grandparents living with own grandchildren,a 2018 (%) | 5.7 (3.2) | 6.3 (3.7) | 5.8 (3) | 5.0 (2.7) |
| Renter-occupied household,a 2018 (%) | 28.6 (8.3) | 27.9 (8.3) | 28.3 (7.8) | 29.6 (8.7) |
| Total population size,a,h 2019 | 106,985 (337916) | 59,030 (140030) | 112,146 (311752) | 146,693 (464453) |
| Log(Population),a 2019 | 4.5 (0.6) | 4.4 (0.6) | 4.5 (0.6) | 4.5 (0.7) |
| Population density,a 2010 (per sq. mi.) | 266 (1750) | 164 (704) | 186 (487) | 439 (2863) |
| Population with broadband internet,a 2018 (%) | 72.6 (9.3) | 70.5 (9.7) | 72.9 (9.3) | 74.3 (8.7) |
| Uninsured population, 18–64 years old,e 2017 (%) | 13.6 (6.3) | 15.1 (6.8) | 13.8 (6) | 12.1 (5.7) |
| Number of hospital beds,e 2017 (per 100,000 capita) | 295.4 (489.7) | 264.9 (407.2) | 276.2 (357.7) | 342.9 (645) |
| Number of ICU beds,e 2017 (per 100,000 capita) | 11.7 (29.6) | 9.7 (18.2) | 12.3 (23.8) | 13.0 (41.1) |
| Premature mortality,f 2017 (years per 100,000 capita) | 8528 (2714) | 9159 (2913) | 8413 (2496) | 8052 (2616) |
| County-level COVID-19 Measures | ||||
| Cumulative COVID-19 Cases,g March 1, 2020 – February 28, 2022 (per 100,000 capita) | 24,202 (5700) | 24,605 (6476) | 24,470 (5276) | 23,561 (5262) |
| Cumulative COVID-19 Deaths,g March 1, 2020 – February 28, 2022 (per 100,000 capita) | 355 (155) | 386 (157) | 355 (151) | 327 (151) |
CMS = Centers for Medicare & Medicaid Services; CHD = Coronary Heart Disease; ICU = Intensive Care Unit; SD = standard deviation; Proportion race variables = race alone or in combination; Premature mortality = age-adjusted years of potential life lost before age 75; Sources of data: aU.S. Census Bureau, bCenters for Medicare & Medicaid Services, cNational Center for Health Statistics, dCenters for Disease Control & Prevention Atlas, eAmerican Health Resource Files, fRobert Wood Johnson Foundation, gJohns Hopkins University Center for Systems Science and Engineering & USAFacts.org, hTotal population size was not included as a regression covariate (see Supplemental Table 1 for additional details on sources).
Table 2.
Associations Between County-level Public Health Expenditure Per Capita Tertiles and Community Health Assessment & Improvement Plan with COVID-19 Incidence and Mortality from March 1, 2020 to February 28, 2022.
| Model + Variables | Overall Cases per 100,000 |
Overall Deaths per 100,000 |
||
|---|---|---|---|---|
| Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | |
| Public Health Expenditure Per Capita Tertile | ||||
| Unadjusted model | ||||
| Tertile 1 (≤ $30) | ref | – | ref | – |
| Tertile 2 ($30–105) | −135 (-632, 363) | 0.596 | −31 (-44, −18) | <0.001 |
| Tertile 3 (>$105) | −1044 (-1540, −548) | <0.001 | −59 (-72, −46) | <0.001 |
| Multi-variable adjusted modela | ||||
| Tertile 1 (≤ $30) | ref | – | ref | – |
| Tertile 2 ($30–105) | 244 (-201, 689) | 0.282 | −4 (-15, 7) | 0.462 |
| Tertile 3 (>$105) | −542 (-1004, −81) | 0.021 | −21 (–32, −10) | <0.001 |
| Community Health Assessment | ||||
| Unadjusted model | ||||
| Without community health assessment | ref | – | ref | – |
| With community health assessment | −706 (-1224, −188) | 0.008 | −55 (-70, −41) | <0.001 |
| Multi-variable adjusted modelb | ||||
| Without community health assessment | ref | – | ref | – |
| With community health assessment | −83 (-537, 370) | 0.719 | −11 (–23, 1) | 0.076 |
| Community Health Improvement Plan | ||||
| Unadjusted model | ||||
| Without community health improvement plan | ref | – | ref | – |
| With community health improvement plan | −269 (-772, 234) | 0.295 | −46 (-60, –32) | <0.001 |
| Multi-variable adjusted modelb | ||||
| Without community health improvement plan | ref | – | ref | – |
| With community health improvement plan | 415 (–23, 854) | 0.063 | −6 (-18, 5) | 0.286 |
| Both Community Health Assessment & Improvement Plan | ||||
| Unadjusted model | ||||
| Without community health assessment & improvement plan | ref | – | ref | – |
| With community health assessment & improvement plan | −473 (-971, 25) | 0.063 | −45 (-59, −31) | <0.001 |
| Multi-variable adjusted modelb | ||||
| Without community health assessment & improvement plan | ref | – | ref | – |
| With community health assessment & improvement plan | 187 (-245, 619) | 0.396 | −8 (-19, 4) | 0.189 |
95% CI = 95% confidence interval; aLinear regression models were used and adjusted models contain additional covariates of county-level variables (percentages of population over 70 years old; living under poverty line; living in group quarters; race alone or in combination (American Indian and Alaska Native, Asian, Black or African American, Native Hawaiian and Other Pacific Islander); Hispanic ethnicity; over 65 years old living alone; with broadband internet; and between 18 and 64 years old without health insurance; as well as in-patient costs per capita; median household income; total county expenditures per capita; prevalence of diabetes; coronary heart disease and hypertension-related hospitalizations; average household size; percentage of households with grandparents living with grandchildren; percentage of households that are renter-occupied; population size (log-transformed); population density; number of hospital and ICU beds; premature mortality; and U.S. Census Region). bLinear regression models were used and adjusted for the same covariates as the aforementioned model, in addition to a log-transformed continuous measure of U.S. Census public health expenditures per capita and county health department characteristics (presence of a governing local board of health; administrative authority centralized to the state level; and full-time employment status of the county health department’s top executive and health officer). Data for COVID-19 include measures from March 1, 2020 to February 28, 2022 for 3050 U.S. counties and county equivalents for public health expenditure analyses, and for 1728 U.S. counties and county equivalents for community health activity analyses.
Fig. 1 maps COVID-19 measures intersected with public health expenditure tertiles. Among 1045 counties in the highest public health expenditure tertile, there was a greater proportion in the lowest tertiles of cases (low case tertile: 37.5%; moderate case tertile: 33.2%; high case tertile: 29.3%) and of deaths (low death tertile: 41.3%; moderate case tertile: 32.6%; high case tertile: 26.0%), as shown in the shade of blue from the bottom left legend color. Among 976 counties in the lowest public health expenditure tertile, there was a greater proportion in the highest tertiles of cases (low case tertile: 31.5%; moderate case tertile: 33.5%; high case tertile: 35.0%) and of deaths (low death tertile: 25.3%; moderate case tertile: 32.0%; high case tertile: 42.7%), as shown in the shade of pink from the top right legend color. Scatterplots that show bivariate density plots of public health expenditures and COVID-19 measures are displayed with the maps in Supplemental Fig. 3. Additional intersection numbers are reported in Supplemental Table 3.
Fig. 1.
U.S. Maps of County-level Public Health Expenditure Tertiles vs. COVID-19 Measures from March 1, 2020 to February 28, 2022. Fig. 1 Footnotes: Data for COVID-19 include measures per 100,000 population from March 1, 2020 to February 28, 2022 for 3050 U.S. counties and county equivalents. Data from the state of Nebraska was excluded due to state-wide lack of data reporting.
Fig. 2 plots average daily cumulative and non-cumulative COVID-19 measures by public health expenditure tertile over time. Generally, cumulative curves for the lowest public health expenditure tertile appear consistently above the curves for higher public health expenditure tertiles, while non-cumulative curves for the lowest public health expenditure tertile appear above other curves during surges.
Fig. 2.
Average U.S. Cumulative and Daily County-Level COVID-19 Measures Over Time, by County-Level Public Health Expenditure Tertile from March 1, 2020 to February 28, 2022. Fig. 2 Footnotes: The lowest tertile is in magenta, the middle tertile is in gray (dotted), and the highest tertile is in blue. Data for COVID-19 include measures per 100,000 population from March 1, 2020 to February 28, 2022 for 3050 U.S. counties and county equivalents. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
3.2. Public health expenditure regression analyses
For unadjusted linear regression analyses of cumulative COVID-19 measures, counties in the highest public health expenditure tertile had 1044 fewer cases per 100,000 population (95% CI, −1549 to −548) and 59 fewer deaths per 100,000 population (95% CI, −72 to −46), as compared to counties in the lowest tertile (Table 2). After adjusting for covariates, these estimates were attenuated with 542 fewer cases per 100,000 population (95% CI, −1004 to −81) and 21 fewer deaths per 100,000 population (95% CI, –32 to −10). As for COVID-19 measures over time by 2-month periods, while there were differences in unadjusted analyses, many estimates were attenuated after adjusting for covariates (Supplemental Table 4 and Supplemental Fig. 4).
In our generalized additive model analyses, increases in public health expenditures were associated with decreased COVID-19 cases and deaths (Supplemental Fig. 5). Smoothed terms of public health expenditures indicated continuous associations for both case and death models, with respective F statistic values of 5.12 (P < 0.001) and 7.92 (P < 0.001). Complete model coefficients are reported in Supplemental Table 5.
3.3. Community health planning activities
Among NACCHO’s 2019 Profile Study sample of 1728 counties and their respective county health department, 64.4% counties completed a community health assessment, 58.1% counties completed a community health improvement plan, and 54.3% of counties completed both within 3 years prior to 2019. The proportion of counties that implemented these activities increased from lowest to highest public health expenditure tertiles. Additional descriptive statistics are summarized in Supplemental Tables 6–7. The difference between time series curve for counties with and without a community health assessment was wider among the lowest public health expenditure tertile and narrow among the highest public health expenditure tertile (Supplemental Figs. 6–7).
Table 2 summarizes linear regression analyses of COVID-19 measures on community health activities. For unadjusted analyses, counties with a community health assessment had on average 706 fewer cases per 100,000 population (95% CI, −1224 to −188) and 55 fewer deaths per 100,000 population (95% CI, −70 to −41), as compared to counties without a community health assessment; counties with a community health improvement plan had 46 fewer deaths per 100,000 population (95% CI, −61 to –32), as compared to counties without a community health improvement plan; and counties with both a community health assessment and improvement plan had 45 fewer deaths per 100,000 population (95% CI, −59 to −31), as compared to counties without both activities. Unadjusted estimates of cases for the models examining community health improvement plans and both activities had confidence intervals with negative and positive values.
When adjusting for county and county health department characteristics, estimates were consistently attenuated for deaths such that the coefficients remained negative, but estimates were less precise and confidence intervals included negative and positive values. Estimates after model adjustment were not consistently attenuated for cases. When examining coefficients over time, estimates from linear regression models were variably attenuated after adjusting for county and county health department characteristics (Supplemental Table 8 and Supplemental Fig. 8).
4. Discussion
While there is renewed attention to the underfunded U.S. public health system, (DeSalvo et al., 2021, Maani and Galea, 2020, Alfonso et al., 2021) our study is the first to our knowledge that examines associations between COVID-19 burden with measures of both prior public health expenditures and community health planning activities. Counties in the lowest tertile of public health expenditures had greater county-level risk factors at baseline prior to the pandemic and greater measures of COVID-19. Geographic variation appeared not only across states, but also within states at the county level as shown in Fig. 1, thus highlighting the need to consider local differences in pandemic-related research. In our exploratory study, higher prior public health expenditures were associated with lower measures of COVID-19. More research is warranted to determine whether increased public health expenditures and infrastructure play a role in county-level factors that prevent severe disease and deaths caused by COVID-19.
In several of our analyses, measures of COVID-19 were similar for the lowest ($0-$30) and middle ($30–105) tertiles of public health expenditures per capita. The difference between lowest and middle tertiles could be less apparent because those ranges nearly overlap with estimates of costs for providing public health services recommended by the Institute of Medicine, ranging from $32 per capita for foundational capabilities to $82 per capita for full service implementation. (Mamaril et al., 2018).
Analyses of categorical tertiles and continuous measures of public health expenditures revealed associations between public health expenditures with COVID-19 burden. The confidence intervals for generalized additive model results were wide given that 95% of counties had public health expenditures under $404 per capita, with $2000 per capita approximately at the 99.5th percentile. Separate regression estimates varied when examining associations by time period. This could be due to smaller case and death counts captured in a 2-month period, especially in counties with smaller populations. Also, since diagnosed and reported COVID-19 cases are only a fraction of total cases, (Li et al., 2020) and better-resourced counties may have increased case finding, associations between public health expenditures and COVID-19 measures could be attenuated because less-resourced counties may experience underreporting.
The completion of community health planning activities within three years prior to 2019 was associated with decreased COVID-19 measures in certain time periods, even after adjusting for public health expenditures. Counties whose health departments conducted a community health assessment may be more knowledgeable about and have built more trust with their community, therefore preventing COVID-19 cases and deaths through means such as tailored allocation of resources and increased public adherence to public health recommendations (e.g., vaccinations and masking). However, adjusted results over time were more consistent for deaths than for cases. These discrepancies could indicate while existing public health infrastructure have not been able to control case numbers indefinitely, certain factors among county health departments with better preparedness and existing community engagement may have contributed to preventing COVID-19 deaths. In addition, researchers have previously demonstrated that static county-level covariates are not consistently correlated with dynamic COVID-19 measures, especially as public policies and population behavior change over time. (Krieger and Christian; Chen, Jarvis T., Waterman, Pamela D., Hanage, William P. , 2020) Lower-resourced counties may also underreport COVID-19 cases and deaths, (Stokes et al., 2021) leading to results potentially biased towards the null and even counterintuitive findings of higher-resourced counties being associated with increased COVID-19 measures during certain time periods. Future research is crucial to understanding how local health departments can help reduce preventable deaths in the current and future pandemics.
There are several policy and advocacy implications to our study. The reimagined Public Health 3.0 framework has been proposed by the U.S. Department of Health and Human Services since 2017, and much progress has yet to be made. (DeSalvo et al., 2017;14:E78.) Among several recommendations, Public Health 3.0 highlights engagement with community stakeholders. While our study examined community health planning activities conducted by county health departments, we recognize that hospitals also play a role in ensuring population health. Since non-profit hospitals are required to conduct community health planning activities to maintain tax exemption status, (Wilson et al., 2014) stronger partnerships could be formed between hospitals and local health departments to better understand the community’s needs, as opposed to current decentralized efforts. (Beatty et al., 2015) Previous research has suggested increased hospital investments in community health initiatives when local health departments were involved in hospitals’ community health implementation strategies. (Carlton and Singh, 2018) Long-standing relationships between local health departments, federally qualified health centers, and other agencies can be strengthened to increase access to services, such as vaccinations. (Allen et al., 2022) In addition to hospitals and clinics, there are calls within academic medicine for building cross-agency collaborations, integrating medical and public health schools, and expanding the pipeline of physicians considering public health careers. (Blazer et al., 2022).
Our study findings are broadly consistent with aforementioned public health spending literature (Leider et al., 2018, McCullough and Leider, 2016, Singh, 2014) and are supportive of increasing local public health funding. Public Health 3.0 emphasizes the securement of enhanced, flexible funding for public health. Given that local health departments have been experiencing trends of shrinking workforces and budgets that have not increased since 2008, additional resources and training should be priorities in rebuilding public health infrastructure. (Association, 2019) Future studies should evaluate causal and mediating pathways by which increased local public health spending improves outcomes using methods such as dynamic panels and natural experiments. (Leatherdale, 2019, Brown, 2014) Vaccination rates, non-pharmaceutical interventions (e.g., masking and stay-at-home policies) and other county-level characteristics should also be examined. For example, in Supplementary Table 9, we noted strong associations between public health expenditures and vaccination rates. As COVID-19 vaccine effectiveness is greater against death than against infection, (Ioannou et al., 2022) increased public health expenditures may have been more inversely related to COVID-19 deaths as compared to cases through greater vaccination rates. Lack of insurance may also be related because it reduces access to health care and preventive services liked vaccinations. (Sudano and Baker, 2003).
Our study noted large funding disparities: the average public health expenditures per capita for counties in Tertile 3 was five times that of Tertile 2 and twenty-nine times that of Tertile 1 ($317, $63, and $11, respectively). As decreased expenditures were associated with increased COVID-19 burden, future studies should examine ways to reduce resource disparities for the least funded and often more rural counties, such as through state or federal mechanisms.
Discussions of increasing funding to local health departments should include insights on how those funds are best utilized, as there is generally a lack of state or federal guidelines on how to prioritize public health funding. (Alford et al., 2021) More detailed reporting of public health expenditures leading to improved research studies may help better inform such guidelines. (Bekemeier et al., 2018) For example, medical expenditures have previously been mapped out by payers and health conditions; and while another study similarly attempted to disentangle personal medical expenditures from public health spending, the study was only able to evaluate federally-funded programs. Investments in modernized and digitized public health data systems may also increase the effectiveness of public health departments, while providing data that would fill gaps in knowledge between public health and medicine.
4.1. Limitations
Government-reported public health expenditures are non-specific and may be inflated as compared to specific expenditures. Although total expenditures have been associated with general outcomes such as all-cause mortality and county health rankings, total expenditures may not always be associated with specific outcomes. In a study of the early pandemic ending in July 2020, previous public health expenditures were not found to be associated with greater control of COVID-19 cases at the county-level. However, more specific measures of public health expenditures could reveal associations with their respective specific outcomes. Increased availability and accessibility of more detailed data on local public health expenditures, as well as state-level characteristics, could better inform public health expenditure studies on pandemic-related and other specific outcomes. Additional variable limitations are discussed in the online supplement (Supplemental Methods).
5. Conclusion
Prior county-level public health expenditures and community health planning activities were found to be associated with COVID-19 cases and deaths in the U.S. The results of our study on county health department characteristics and COVID-19 outcomes underscore calls to action for building a more robust public health system. We hope our study will spur additional research to understand the effects of public health characteristics on COVID-19 and to consider the perspective of public health infrastructure when studying other health outcomes.
Funding Sources & Acknowledgements
This work was supported in part by the National Institute on Aging of the National Institutes of Health (R01AG059791) and the National Institute on Drug Abuse (R00DA051534). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The National Institutes of Health had no involvement in the study besides funding. The authors would also like to express their gratitude to Dr. Debra Dekker, PhD from the National Association of County and City Health Officials for her help in gaining data access and sharing thoughtful comments for this project. Dr. Dekker received no compensation for her contributions.
CRediT authorship contribution statement
Richard Liang: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. Mathew V. Kiang: Data curation, Methodology, Writing – review & editing. Philip Grant: Methodology, Writing – review & editing. Christian Jackson: Formal analysis, Validation, Writing – review & editing. David H. Rehkopf: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102410.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
The authors do not have permission to share data from the 2019 National Profile of Local Health Departments Study. Requests can be made to the National Association of County and City Health Officials.
References
- Alfonso Y.N., Leider J.P., Resnick B., McCullough J.M., Bishai D. US Public Health Neglected: Flat Or Declining Spending Left States Ill Equipped To Respond To COVID-19. Health Aff. 2021;40(4):664–671. doi: 10.1377/hlthaff.2020.01084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alford A.A., Feeser K., Kellie H., Biesiadecki L. Prioritization of Public Health Emergency Preparedness Funding Among Local Health Departments Preceding the COVID-19 Pandemic: Findings From NACCHO's 2019 National Profile of Local Health Departments. J. Public Health Manag. Pract. 2021;27(2):215–217. doi: 10.1097/PHH.0000000000001338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen P., Walsh-Bailey C., Hunleth J., Carothers B.J., Brownson R.C. Facilitators of Multisector Collaboration for Delivering Cancer Control Interventions in Rural Communities: A Descriptive Qualitative Study. Prev. Chronic Dis. 2022;2022(19):19. doi: 10.5888/pcd19.210450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of County and City Health Officials (NACCHO). NACCHO’s 2019 Profile Study: Changes in Local Health Department sWorkforce and Finance Capacity Since 2008. 2020.
- Beatty K.E., Wilson K.D., Ciecior A., Stringer L. Collaboration Among Missouri Nonprofit Hospitals and Local Health Departments: Content Analysis of Community Health Needs Assessments. Am. J. Public Health. 2015;105(S2):S337–S344. doi: 10.2105/AJPH.2014.302488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekemeier B., Singh S.R., Schoemann A.W. A Uniform Chart of Accounts for Public Health Agencies: An “Essential Ingredient” for a Strong Public Health System. J. Public Health Manag. Pract. 2018;24(3):289–291. doi: 10.1097/PHH.0000000000000793. [DOI] [PubMed] [Google Scholar]
- Bilinski A., Emanuel E.J. COVID-19 and Excess All-Cause Mortality in the US and 18 Comparison Countries. J. Am. Med. Assoc. 2020;324(20):2100–2102. doi: 10.1001/jama.2020.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilinski A., Thompson K., Emanuel E. COVID-19 and Excess All-Cause Mortality in the US and 20 Comparison Countries, June 2021-March 2022. J. Am. Med. Assoc. 2023;329(1):92–94. doi: 10.1001/jama.2022.21795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer, D.G., Colenda, C.C., Applegate, W.B., Reifler, B.V., The great health paradox: a call for increasing investment in public health. Academic Medicine. 2022;97(4). [DOI] [PubMed]
- Bor, J., Stokes, A.C., Raifman, J., et al., Missing Americans: Early death in the United States—1933–2021. PNAS Nexus. 2023;2(6). [DOI] [PMC free article] [PubMed]
- Brown T.T. How effective are public health departments at preventing mortality? Econ. Hum. Biol. 2014;13:34–45. doi: 10.1016/j.ehb.2013.10.001. [DOI] [PubMed] [Google Scholar]
- Carlton E.L., Singh S.R. Joint Community Health Needs Assessments as a Path for Coordinating Community-Wide Health Improvement Efforts Between Hospitals and Local Health Departments. Am. J. Public Health. 2018;108(5):676–682. doi: 10.2105/AJPH.2018.304339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin T., Kahn R., Li R., Chen J.T., Krieger N., Buckee C.O., Balsari S., Kiang M.V. US-county level variation in intersecting individual, household and community characteristics relevant to COVID-19 and planning an equitable response: a cross-sectional analysis. BMJ Open. 2020;10(9):e039886. doi: 10.1136/bmjopen-2020-039886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSalvo, K., Hughes, B., Bassett, M., et al., Public health COVID-19 impact assessment: lessons learned and compelling needs. NAM perspectives. 2021;2021. [DOI] [PMC free article] [PubMed]
- DeSalvo K.B., Wang Y.C., Harris A., Auerbach J., Koo D., O'Carroll P. Public Health 3.0: A Call to Action for Public Health to Meet the Challenges of the 21st Century. Prev. Chronic Dis. 2017;14:E78. doi: 10.5888/pcd14.170017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards R.T., Charles J.M., Lloyd-Williams H. Public health economics: a systematic review of guidance for the economic evaluation of public health interventions and discussion of key methodological issues. BMC Public Health. 2013;13(1):1001. doi: 10.1186/1471-2458-13-1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman L.T. COVID-19—The Historical Lessons of the Pandemic Reinforce Systemic Flaws and Exacerbate Inequity. Am. J. Public Health. 2021;111(S3):S176–S178. doi: 10.2105/AJPH.2021.306543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gmeinder, M., Morgan, D., Mueller, M., How much do OECD countries spend on prevention? OECD Health Working Papers. 2017. https://www.oecd-ilibrary.org/content/paper/f19e803c-en.
- Heuveline P., Lanza Queiroz B. The Covid-19 pandemic and the expansion of the mortality gap between the United States and its European peers. PLoS One. 2023;18(3):e0283153. doi: 10.1371/journal.pone.0283153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoornbeek J., Morris M., Libbey P., Pezzino G. Consolidating Local Health Departments in the United States: Challenges, Evidence, and Thoughts for the Future. Public Health Rep. 2019;134(2):103–108. doi: 10.1177/0033354919829054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee for the Study of the Future of Public Health. The Future of Public Health. In: Summary and Recommendations. Washington (DC): National Academies Press (US); 1988: https://www.ncbi.nlm.nih.gov/books/NBK218215/.
- Ioannou G.N., Locke E.R., O’Hare A.M., Bohnert A.S.B., Boyko E.J., Hynes D.M., Berry K. COVID-19 Vaccination Effectiveness Against Infection or Death in a National U.S. Health Care System. Ann. Intern. Med. 2022;175(3):352–361. doi: 10.7326/M21-3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger, N.T., Christian, Chen, Jarvis T., Waterman, Pamela D., Hanage, William P. Warning against using static US county-level community data to guide equity in COVID-19 vaccine distribution: Temporal and spatial correlations of community characteristics with COVID-19 cases and deaths vary enormously and are increasingly uninformative. HCPDS Working Paper Series. 2020;20. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/1266/2020/12/20_Krieger-et-al_equity-in-vaccine-distribution_Volume-20_No-_5_final.pdf.
- Lash, T.L., VanderWeele, T.J., Haneause, S., Rothman, K., Modern Epidemiology. Wolters Kluwer Health; 2020.
- Leatherdale S.T. Natural experiment methodology for research: a review of how different methods can support real-world research. Int. J. Soc. Res. Methodol. 2019;22(1):19–35. [Google Scholar]
- Leider J.P., Alfonso N., Resnick B., Brady E., McCullough J.M., Bishai D. Assessing The Value Of 40 Years Of Local Public Expenditures On Health. Health Aff. 2018;37(4):560–569. doi: 10.1377/hlthaff.2017.1171. [DOI] [PubMed] [Google Scholar]
- Li R., Pei S., Chen B., Song Y., Zhang T., Yang W., Shaman J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368(6490):489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maani N., Galea S. COVID-19 and underinvestment in the public health infrastructure of the United States. Milbank Q. 2020;98(2):250–259. doi: 10.1111/1468-0009.12463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamaril C.B.C., Mays G.P., Branham D.K., Bekemeier B., Marlowe J., Timsina L. Estimating the Cost of Providing Foundational Public Health Services. Health Serv. Res. 2018;53:2803–2820. doi: 10.1111/1475-6773.12816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough J.M., Leider J.P. Government Spending In Health And Nonhealth Sectors Associated With Improvement In County Health Rankings. Health Aff. 2016;35(11):2037–2043. doi: 10.1377/hlthaff.2016.0708. [DOI] [PubMed] [Google Scholar]
- National Association of County and City Health Officials (NACCHO). National Profile of Local Health Departments. https://www.naccho.org/resources/lhd-research/national-profile-of-local-health-departments#data-requests.
- Rabarison K.M., Timsina L., Mays G.P. Community Health Assessment and Improved Public Health Decision-Making: A Propensity Score Matching Approach. Am. J. Public Health. 2015;105(12):2526–2533. doi: 10.2105/AJPH.2015.302795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah G.H., Leep C.J., Ye J., Sellers K., Liss-Levinson R., Williams K.S. Public Health Agencies' Level of Engagement in and Perceived Barriers to PHAB National Voluntary Accreditation. J. Public Health Manag. Pract. 2015;21(2):107–115. doi: 10.1097/PHH.0000000000000117. [DOI] [PubMed] [Google Scholar]
- Singh S.R. Public Health Spending and Population Health: A Systematic Review. Am. J. Prev. Med. 2014;47(5):634–640. doi: 10.1016/j.amepre.2014.05.017. [DOI] [PubMed] [Google Scholar]
- Stokes A.C., Lundberg D.J., Elo I.T., Hempstead K., Bor J., Preston S.H., Suthar A.B. COVID-19 and excess mortality in the United States: A county-level analysis. PLoS Med. 2021;18(5):e1003571. doi: 10.1371/journal.pmed.1003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudano J.J., Jr., Baker D.W. Intermittent lack of health insurance coverage and use of preventive services. Am. J. Public Health. 2003;93(1):130–137. doi: 10.2105/ajph.93.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [dataset] U.S. Census Bureau. Census of Governments. 2021; https://www.census.gov/programs-surveys/cog.html.
- USAFacts. US COVID-19 cases and deaths by state. 2021; https://usafacts.org/visualizations/coronavirus-covid-19-spread-map.
- Wilson K.D., Mohr L.B., Beatty K.E., Ciecior A. Describing the Continuum of Collaboration Among Local Health Departments With Hospitals Around the Community Health Assessments. J. Public Health Manag. Pract. 2014;20(6):617–625. doi: 10.1097/PHH.0000000000000030. [DOI] [PubMed] [Google Scholar]
- Wood S.N. CRC Press; 2017. Generalized Additive Models: An Introduction with R. [Google Scholar]
- Woolf S.H. Falling Behind: The Growing Gap in Life Expectancy Between the United States and Other Countries, 1933–2021. Am. J. Public Health. 2023;113(9):970–980. doi: 10.2105/AJPH.2023.307310. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors do not have permission to share data from the 2019 National Profile of Local Health Departments Study. Requests can be made to the National Association of County and City Health Officials.