This systematic review and meta-analysis evaluates whether children admitted to hospitals following trauma who receive definitive treatment in a pediatric trauma center have better outcomes than those treated in adult trauma centers.
Key Points
Question
Do children admitted to hospitals following trauma who receive definitive treatment in a pediatric trauma center (PTC) have better outcomes than those treated in adult trauma centers (ATCs)?
Findings
Results of this systematic review and meta-analysis of 56 studies with 286 051 participants suggest that compared with ATCs, PTCs were associated with a reduction of 41%, 52%, and 64% in the odds of mortality, computed tomography, and operative management for blunt solid organ injury, respectively, for children hospitalized following trauma. Certainty of evidence was very low.
Meaning
These results suggest treating children in PTCs leads to better outcomes, but future studies should strive to address selection and confusion biases.
Abstract
Importance
Adult trauma centers (ATCs) have been shown to decrease injury mortality and morbidity in major trauma, but a synthesis of evidence for pediatric trauma centers (PTCs) is lacking.
Objective
To assess the effectiveness of PTCs compared with ATCs, combined trauma centers (CTCs), or nondesignated hospitals in reducing mortality and morbidity among children admitted to hospitals following trauma.
Data Sources
MEDLINE, Embase, and Web of Science through March 2023.
Study Selection
Studies comparing PTCs with ATCs, CTCs, or nondesignated hospitals for pediatric trauma populations (aged ≤19 years).
Data Extraction and Synthesis
This systematic review and meta-analysis was performed following the Preferred Reporting Items for Systematic Review and Meta-analysis and Meta-analysis of Observational Studies in Epidemiology guidelines. Pairs of reviewers independently extracted data and evaluated risk of bias using the Risk of Bias in Nonrandomized Studies of Interventions tool. A meta-analysis was conducted if more than 2 studies evaluated the same intervention-comparator-outcome and controlled minimally for age and injury severity. Subgroup analyses were planned for age, injury type and severity, trauma center designation level and verification body, country, and year of conduct. Grading of Recommendations Assessment, Development, and Evaluation (GRADE) was used to assess certainty of evidence.
Main Outcome(s) and Measure(s)
Primary outcomes were mortality, complications, functional status, discharge destination, and quality of life. Secondary outcomes were resource use and processes of care, including computed tomography (CT) and operative management of blunt solid organ injury (SOI).
Results
A total of 56 studies with 286 051 participants were included overall, and 34 were included in the meta-analysis. When compared with ATCs, PTCs were associated with a 41% lower risk of mortality (OR, 0.59; 95% CI, 0.46-0.76), a 52% lower risk of CT use (OR, 0.48; 95% CI, 0.26-0.89) and a 64% lower risk of operative management for blunt SOI (OR, 0.36; 95% CI, 0.23-0.57). The OR for complications was 0.80 (95% CI, 0.41-1.56). There was no association for mortality for older children (OR, 0.71; 95% CI, 0.47-1.06), and the association was closer to the null when PTCs were compared with CTCs (OR, 0.73; 95% CI, 0.53-0.99). Results remained similar for other subgroup analyses. GRADE certainty of evidence was very low for all outcomes.
Conclusions and Relevance
In this systematic review and meta-analysis, results suggested that PTCs were associated with lower odds of mortality, CT use, and operative management for SOI than ATCs for children admitted to hospitals following trauma, but certainty of evidence was very low. Future studies should strive to address selection and confounding biases.
Introduction
Injury is the medical condition with the greatest burden on US children and youth.1 In the US, 4.1 million children get injured every year at an annual cost of US $396 billion.2 The human and societal burden of childhood injury are even greater. For every injury fatality, 10 children are left with lifelong disabilities resulting in enormous emotional and financial hardship for the injured and their families.3
Trauma systems constitute a population-based, multidisciplinary response to injury from prehospital and hospital care to rehabilitation and community services and have been shown to improve patient outcomes.4,5,6,7,8 Systematic reviews provide evidence that adults treated at designated trauma centers have better outcomes than those treated in nondesignated hospitals.5,9,10 The first pediatric trauma centers (PTCs) were established in the 1970s,11 soon after the creation of adult trauma centers (ATCs), in recognition of the distinct physiological, psychological, and social needs of children.12 Studies comparing outcomes of injured children treated at PTCs, ATCs, or combined (adult and pediatric) trauma centers (CTCs) have shown divergent results,13,14,15,16,17,18,19 and a synthesis of this evidence is lacking.
Our primary objective was to synthesize evidence on the effectiveness of PTCs compared with ATCs, CTCs, or nondesignated hospitals for improving clinical outcomes and quality of life in children admitted to hospitals following trauma. Secondary objectives were to assess associations with resource utilization and processes of care. We hypothesized that children receiving definitive treatment in a PTC would have more favorable outcomes than those treated in other hospitals.
Methods
We conducted this systematic review following Cochrane methodology20 and reported results according to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guideline21 and Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.22 The protocol was registered with PROSPERO. The study was designed and conducted in collaboration with an interdisciplinary advisory committee comprising 12 pediatric clinicians (including prehospital, emergency medicine, trauma surgery, neurosurgery, orthopedics, critical care medicine, nursing, and rehabilitation specialties), 3 trauma program medical directors, and 2 trauma accreditation agency representatives.
Inclusion Criteria and Search Strategy
We included prospective or retrospective cohort and case-control or case-cohort studies that compared outcomes of children or adolescents (aged ≤19 years) admitted to hospitals following trauma in PTCs to those in ATCs, CTCs, or nondesignated hospitals (see eTable 1 in Supplement 1 for definitions). We searched MEDLINE, Embase, Web of Science, and CINAHL through March 2023 (eTable 2 in Supplement 1). Thesis repositories and references of included studies were screened. Our primary outcomes of interest, defined a priori, were mortality, complications, functional status, discharge destination, and quality of life (see eTable 3 in Supplement 1 for definitions). Secondary outcomes were resource utilization and processes of care including use of computed tomography (CT) or operative management of blunt solid organ injuries (SOI).
Risk of Bias Assessment
Three content experts (L.M., P.A.T., J.G.) independently rated studies using the Risk of Bias in Nonrandomized Studies of Interventions tool.23 We assessed publication bias using a contour-enhanced funnel plot and estimated the magnitude of the potential bias with the trim-and-fill method.24
Statistical Analysis
Data Synthesis
We restricted data synthesis to studies presenting measures of association minimally adjusted for age and injury severity. In the context of a review limited to observational studies with a very high risk of indication bias, unadjusted comparisons were considered not to produce meaningful results. When 2 studies or more evaluated the same exposure-outcome association, we conducted meta-analyses (see eAppendix 1 in Supplement 1). We measured the heterogeneity of included studies using the I2 statistic and interpreted as low if 0% to 40%, moderate if 30% to 60%, substantial if 50% to 90%, and considerable if 75% to 100%.20 Two content experts (L.M., P.A.T.) independently applied Grading of Recommendations Assessment, Development and Evaluation criteria (eAppendix 1 in Supplement 1).25
Subgroup and Sensitivity Analyses
We conducted prespecified subgroup analyses for factors thought to modify the associations of interest, identified on consultation with our advisory committee: age, type of injury, injury severity, country, year of study conduct, PTC and ATC designation levels and verification body, and risk of bias (see eTable 4 in Supplement 1 for definitions). We added post-hoc subgroup analyses on how transfers were handled in analyses, as this was felt to be a major source of potential bias. We conducted sensitivity analyses for outliers.26 All analyses were conducted using R Statistical Software version 4.2.1 (R Project for Statistical Computing) and statistical significance was set at P < 0.05.
Results
Among 6860 records identified in the databases, 5369 titles and abstracts were screened, and 212 manuscripts were assessed for eligibility, of which 56,4,8,12,13,14,18,19,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75 with 286 051 total participants, were included in the review (eFigure 1 in eAppendix 2 in Supplement 1). Forty-four studies (79%) were published after 2010 (eTable 5 in Supplement 1). Forty-three studies (77%) were conducted in the USA, 3 in Australia, and 2 in Canada with recruitment periods spanning from 1985 to 2019. Forty-seven studies (84%) compared PTCs with ATCs, and 18 compared PTCs with CTCs. Only 1 compared PTCs with nondesignated hospitals.61 Thirty-nine studies (76%) presented measures of association minimally adjusted for age and injury severity.
Risk of Bias
Overall risk of bias was critical in 6 studies13,32,35,18,54,70 (25%) for mortality, critical in all studies for complications, serious in all studies for CT use, and serious in 5 studies31,52,54,64,69 (71%) for operative management of SOI (Table 1). Selection bias was rated critical or serious in 288,13,14,18,27,29,31,32,33,34,35,38,41,50,54,55,57,58,62,63,67,69,70 studies (82%), either because participation in the trauma registry was voluntary or because a substantial proportion of patients were excluded (eg, missing data or patients transferred in). Confounding bias was rated serious for 11 studies13,29,47,52,53,58,59,60,63,64,67 (17%), mostly due to the absence of physiological parameters (eg, Glasgow coma scale or hemodynamic stability) in administrative data. Bias due to classification of the intervention was rated low for 27 studies4,13,14,18,27,29,31,33,38,41,50,67,52,53,54,57,59,60,63,64,65,66,69,70 (79%), with some studies rated moderate because trauma centers were not accredited or verified by the same organizations (eg, state-designated with or without American College of Surgeons [ACS] verification). Similarly, deviations from the intervention were rated low for 26 studies4,14,18,29,31,32,33,35,38,41,47,50,54,55,57,58,59,62,65,66 (76%), with 11 rated moderate because they included but did not control for interhospital transfers. Bias in the measurement of outcomes was rated low for mortality, CT, and surgery but critical for complications, vulnerable to misclassification.76 Bias in reported results was rated serious for 13 studies4,8,14,27,32,33,35,47,50,55,59,62 (38%), which conducted unplanned subgroup analysis. Finally, a small-study effect (proxy for publication bias) was observed for mortality with an adjusted 95% CI covering the null value (OR, 0.79; 95% CI, 0.58-1.06) (eFigure 2 in Supplement 1).
Table 1. Risk Of Bias of Studies Included in Meta-Analysesa.
| Outcome and source | Confounding | Selection | Classification of intervention | Deviations from interventions | Missing data | Measurement of outcomes | Reported results | Overall |
|---|---|---|---|---|---|---|---|---|
| Mortality | ||||||||
| Derderian et al,13 2022 | Serious | Critical | Low | Moderate | NI | Low | Moderate | Critical |
| Lewit et al,29 2022 | Serious | Serious | Low | Low | Serious | Low | Moderate | Serious |
| Pulido et al,31 2022 | Moderate | Serious | Low | Low | NI | Low | Moderate | Serious |
| Sheff et al,32 2022 | Moderate | Critical | Moderate | Low | Serious | Low | Serious | Critical |
| Stephenson et al,33 2022 | Moderate | Serious | Low | Low | NI | Low | Serious | Serious |
| Ali et al,34 2021 | Moderate | Serious | Moderate | Moderate | Moderate | Low | Moderate | Serious |
| Evans et al,14 2021 | Moderate | Serious | Low | Low | Moderate | Low | Serious | Serious |
| Khalil et al,35 2021 | Moderate | Critical | Moderate | Low | Serious | Low | Serious | Critical |
| Scantling et al,38 2021 | Moderate | Serious | Low | Low | Serious | Low | Moderate | Serious |
| Swendiman et al,18 2021 | Moderate | Critical | Low | Low | Moderate | Low | Moderate | Critical |
| Hatchimonji et al,41 2020 | Moderate | Serious | Low | Low | Moderate | Low | Moderate | Serious |
| Myers et al,47 2019 | Serious | Low | Moderate | Low | NI | Low | Serious | Serious |
| Bardes et al,50 2018 | Moderate | Serious | Low | Low | NI | Low | Serious | Serious |
| Mitchell et al,67 2017 | Serious | Serious | Low | Moderate | Low | Low | Moderate | Serious |
| Miyata et al,54 2017 | Moderate | Serious | Low | Low | NI | Low | Moderate | Serious |
| Miyata et al,55 2017 | Moderate | Critical | Moderate | Low | NI | Low | Serious | Critical |
| Walther et al,63 2016 | Serious | Serious | Low | Moderate | NI | Low | Moderate | Serious |
| Webman et al,8 2016 | Moderate | Serious | Moderate | Low | Moderate | Low | Serious | Serious |
| Sathya et al,62 2015 | Moderate | Serious | Moderate | Low | Moderate | Low | Serious | Serious |
| Walther et al,59 2014 | Serious | Low | Low | Low | NI | Low | Serious | Serious |
| Matsushima et al,65 2013 | Moderate | Moderate | Low | Low | NI | Low | Moderate | Moderate |
| Mitchell et al,53 2013 | Serious | Low | Low | Moderate | NI | Low | Moderate | Serious |
| Amini et al,4 2011 | Moderate | Low | Low | Low | Moderate | Low | Serious | Serious |
| Osler et al,70 2001 | Moderate | Critical | Low | Moderate | NI | Low | Moderate | Critical |
| Complications | ||||||||
| Ali et al,34 2022 | Moderate | Serious | Moderate | Moderate | Moderate | Critical | Moderate | Critical |
| Khalil et al,35 2021 | Moderate | Critical | Moderate | Low | Serious | Critical | Serious | Critical |
| Matsushima et al,65 2013 | Moderate | Moderate | Low | Low | NI | Critical | Moderate | Critical |
| Computed tomography | ||||||||
| Gerber et al,27 2023 | Moderate | Serious | Low | Low | Serious | Low | Serious | Serious |
| Ali et al,34 2022 | Moderate | Serious | Moderate | Moderate | Moderate | Low | Moderate | Serious |
| Pandit et al,57 2016 | Moderate | Serious | Low | Low | NI | Low | Moderate | Serious |
| Kelley-Quon et al,60 2015 | Serious | Low | Low | Serious | NI | Low | Moderate | Serious |
| Operative management of solid organ injury | ||||||||
| Pulido et al,31 2022 | Moderate | Serious | Low | Low | NI | Low | Moderate | Serious |
| Adams et al,52 2017 | Serious | Low | Low | Moderate | NI | Low | Moderate | Serious |
| Miyata et al,54 2017 | Moderate | Serious | Low | Low | NI | Low | Moderate | Serious |
| Safavi et al,58 2016 | Serious | Critical | Moderate | Low | Serious | Low | Moderate | Critical |
| Lippert et al,64 2013 | Serious | Moderate | Low | Moderate | NI | Low | Moderate | Serious |
| Matsushima et al,66 2013 | Moderate | Moderate | Low | Low | NI | Low | Moderate | Moderate |
| Potoka et al,69 2002 | Moderate | Serious | Low | Moderate | NI | Low | Moderate | Serious |
Abbreviation: NI, no information.
Using the Risk Of Bias In Nonrandomized Studies of Interventions tool.
PTCs vs ATCs
Mortality
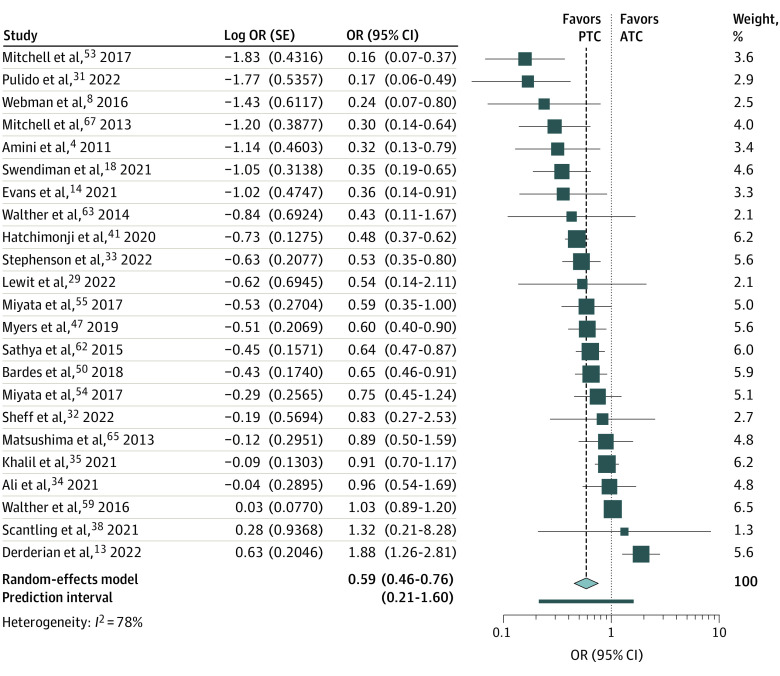
PTCs were associated with 40% lower odds of mortality than ATCs (23 studies; OR, 0.59; 95% CI, 0.46-0.76) (Table 2 and Figure). However, statistical heterogeneity was considerable (I2 = 78%) and prediction intervals included nonbeneficial effect estimates.
Table 2. Summary of Meta-Analyses Results for Children Admitted to Hospitals Following Trauma Treated at a Pediatric Trauma Center vs an Adult Trauma Center or a Combined Adult and Pediatric Center.
| Outcome | Pooled effect estimates OR (95% CI; 95% PI) |
No. (I2, %) | Risk of biasa |
|---|---|---|---|
| Mortality | |||
| PTC vs ATC, all | 0.59 (0.46-0.76; 0.22-1.59) | 23 (78) | Serious |
| Aged ≤16 y | 0.50 (0.31-0.81; 0.15-1.71) | 9 (64) | Serious |
| Aged ≥14 y | 0.71 (0.47-1.06; 0.21-2.38) | 11 (76) | Serious |
| Head injuries | 0.66 (0.51-0.84; 0.08-5.13) | 3 (<1) | Serious |
| Blunt solid organ injuries | 0.67 (0.03-12.79; NA) | 3 (91) | Serious |
| Penetrating injuries | 0.48 (0.35-0.67; 0.30-0.77) | 4 (<1) | Serious |
| ISS ≥12 | 0.60 (0.16-2.25; NA) | 3 (77) | Serious |
| Level I | 0.48 (0.30-0.76; 0.13-1.72) | 8 (87) | Serious |
| Level I and II | 0.56 (0.41-0.76; 0.34-0.93) | 10 (44) | Serious |
| Level I and II with same verification organization | 0.38 (0.20-0.75; 0.09-1.57) | 4 (34) | Serious |
| US | 0.68 (0.53-0.86; 0.29-1.57) | 19 (77) | Serious |
| Other countries | 0.27 (0.15-0.48; 0.11-0.69) | 4 (<1) | Serious |
| 2010 to 2014b | 0.65 (0.45-0.94; 0.26-1.62) | 10 (74) | Serious |
| 2015 to 2019b | 0.60 (0.37-0.99; 0.14-2.58) | 10 (81) | Serious |
| Moderate or serious risk of biasc | 0.53 (0.41-0.69; 0.23-1.25) | 18 (76) | Serious |
| Critical risk of bias | 0.80 (0.36-1.76; 0.10-6.42) | 5 (84) | Serious |
| Transfers excluded | 0.58 (0.47-0.71; 0.34-0.99) | 14 (49) | Serious |
| Transfers included, adjustment | 0.70 (0.40-1.22; 0.30-1.60) | 4 (41) | Serious |
| Transfers included, no adjustment | 0.42 (0.12-1.45; 0.01-12.62) | 5 (91) | Serious |
| PTC vs CTC | 0.73 (0.53-0.99; 0.36-1.46) | 1 (69) | Serious |
| Complications | |||
| PTC vs ATC, all | 0.80 (0.41-1.56; 0.03-24.19) | 3 (69) | Critical |
| Level I and II | 0.80 (0.41-1.56; 0.03-24.19) | 3 (69) | Serious |
| Computed tomography imaging | |||
| PTC vs ATC, all | 0.48 (0.26-0.89; 0.08-2.75) | 7 (96) | Serious |
| Operative management of blunt solid organ injury | |||
| PTC vs ATC, all | 0.36 (0.23-0.57; 0.10-1.29) | 8 (76) | Serious |
| Level I | 0.24 (0.24-0.24; NA) | 2 (NA) | Serious |
| Level I and II | 0.38 (0.21-0.69; 0.09-1.71) | 6 (79) | Serious |
| Level I and II with same verification organization | 0.59 (0.03-12.30; NA) | 2 (20) | Serious |
Abbreviations: ATC, adult trauma centers; CTC, combined trauma centers; ISS, injury severity score; NA, not applicable; PI, prediction intervals; PTC, pediatric trauma centers.
Using the Risk of Bias in Nonrandomized Studies of Interventions tool.
Dates correspond to last year of patient recruitment.
One study with moderate and 17 with serious risk of bias.
Figure. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs).
ORs of mortality for PTC vs ATC were comparable to the main analysis for children aged 16 years or younger (9 studies; OR, 0.50; 95% CI, 0.31-0.81) (Table 2; eFigure 3 in Supplement 1), but the 95% CI covered the null value for older adolescents (11 studies; OR, 0.71; 95% CI, 0.47-1.06) (Table 2; eFigure 4 in Supplement 1). Analyses by type of injury showed lower mortality at PTCs when compared with ATCs for head injury (3 studies; OR, 0.66; 95% CI, 0.51-0.84) (Table 2; eFigure 5, eFigure 6, eFigure 7, and eFigure 8 in Supplement 1) and penetrating injuries (4 studies; OR, 0.48; 95% CI, 0.35-0.67). Analyses for blunt SOI and injury severity scores (ISS) of 12 or higher led to low sample sizes with wide confidence intervals, but effect estimates were similar to the main analysis. When we restricted to studies with the same designation level in intervention and control groups and to trauma centers verified by the same organizations, results were similar (OR, 0.48; 95% CI, 0.30-0.76 for level I; OR, 0.56; 95% CI, 0.41-0.6 for levels I and II; and OR, 0.38; 95% CI, 0.20-0.75 for centers verified by the same organization) (Table 2; eFigure 9, eFigure 10, and eFigure 11 in Supplement 1). Subgroup analyses by country and by period of data collection also led to similar effect estimates (OR, 0.68; 95% CI, 0.53-0.86 for studies conducted in the US; OR, 0.27; 95% CI, 0.15-0.48 for other countries; OR, 0.65; 95% CI, 0.45-0.94 for 2010 to 2014; and OR, 0.60; 95% CI, 0.37-0.99 for 2015 to 2019) (Table 2; eFigure 12, eFigure 13, eFigure 14, and eFigure 15 in Supplement 1). Results remained unchanged in studies at moderate or serious risk of bias (OR, 0.53; 95% CI, 0.41-0.69) but the difference was not significant in studies at critical risk of bias (OR, 0.80; 95% CI, 0.36-1.76) (Table 2; eFigure 16 and eFigure 17 in Supplement 1). Subgroup analyses according to how transfers were handled led to similar ORs but were only significant in studies that excluded transfers (OR, 0.58; 95% CI, 0.47-0.71; OR, 0.70; 95% CI, 0.40-1.22 for studies including transfers with adjustment; and OR, 0.42; 95% CI, 0.12-1.45 for studies including transfers without adjustment) (Table 2; eFigure 18, eFigure 19, and eFigure 20 in Supplement 1). Removing outliers from the main analysis did not alter the conclusions (OR, 0.68; 95% CI, 0.57-0.81 when 7 studies were removed; and OR, 0.57; 95% CI, 0.46-0.71 when 3 studies were removed) (eFigure 21 and eFigure 22 in Supplement 1) and led to a reduction in heterogeneity (I2 = 21% and I2 = 54%, respectively).
Complications
The confidence interval of the pooled effect estimate comparing PTCs with ATCs for complications covered the null value (3 studies; OR, 0.80; 95% CI, 0.41-1.56) (eFigure 23 in Supplement 1). Results were similar when we restricted to studies with the same designation level in intervention and control groups (OR, 0.80; 95% CI, 0.41-1.57 for level I and II) (Table 2; eFigure 24 in Supplement 1). There were insufficient studies for other subgroup analyses.
Processes of Care
Compared with ATCs, PTCs were associated with a reduction of 52% in the odds of CT use (7 studies; OR, 0.48; 95% CI, 0.26-0.89) and 64% in operative management for SOI (8 studies; OR, 0.36; 95% CI, 0.23-0.57) (Table 2; eFigure 25, and eFigure 26 in Supplement 1). However, heterogeneity was considerable (I2 = 96% and I2 = 76%, respectively) and prediction intervals included nonbeneficial effect estimates.
When we restricted to studies with the same designation level in intervention and control groups and to trauma centers verified by the same organization, results were similar for operative management of SOI (OR, 0.38; 95% CI, 0.21-0.67 for levels I and II; and OR, 0.24; 95% CI, 0.24-0.24 for centers verified by the same organization) (Table 2; eFigure 27, eFigure 28, and eFigure 29 in Supplement 1). There were insufficient studies for other subgroup analyses.
PTCs vs CTCs
In the 11 studies comparing PTCs with CTCs for mortality, the 95% CI on the pooled OR was closer to the null value but was still statistically significant (OR, 0.73; 95% CI, 0.53-0.99) (Table 2; eFigure 30 in Supplement 1). There were insufficient studies for subgroup analyses.
Results Not Included in Meta-Analyses
Studies not included in the meta-analyses suggested that PTCs may be associated with a more favorable discharge destination, lower resource use, fewer blood product transfusions, less interventional radiology, and fewer tracheostomies. Results are shown in eTable 6 in Supplement 1.
Certainty of Evidence
Certainty of evidence was very low for all outcomes (Table 3). It was upgraded for mortality because of a dose-response association but then downgraded for possible risk of publication bias.
Table 3. Grading of Recommendations Assessment, Development and Evaluation of Evidence for Outcomes Included in Meta-Analyses.
| Outcomes (No. of studies) | Risk of biasa | Inconsistency | Indirectness | Imprecision | Publication biasb | Magnitude | Residual bias | Dose-response | Certainty of evidence |
|---|---|---|---|---|---|---|---|---|---|
| Mortality (25) | Serious | No | No | No | Yes | No | No | Yesc | Very low |
| Imaging (3) | Serious | No | No | No | NA | No | No | No | Very low |
| Surgery (7) | Serious | No | No | No | NA | No | No | No | Very low |
| Complications (5) | Critical | Yes | No | No | NA | No | No | No | Very low |
Risk of bias is based on Risk of Bias in Nonrandomized Studies of Interventions tool with its 7 components (bias due to confounding, selection of study participants, classification of intervention, deviations from intended interventions, missing data, measurement of outcomes, and selection in the reported results).
Could only be evaluated for mortality.
Association was greater in younger than in older children and effect was greater for pediatric trauma centers vs adult trauma centers than for pediatric trauma centers vs combined adult and pediatric trauma centers.
Discussion
The results of our systematic review and meta-analysis suggest that compared with ATCs, PTCs are associated with 40% lower odds of mortality, 50% lower odds of CT use, and 60% lower odds of operative SOI management for children admitted to hospitals following trauma. Statistical heterogeneity was considerable overall but was low to moderate when outliers were removed. Associations with mortality were closer to the null and not statistically significant for adolescents and for studies with critical risk of bias. Results for other subgroup and sensitivity analyses were similar to the main analysis. PTCs were associated with a 30% lower odds of mortality compared with CTCs. No association was observed between complications and trauma center type. Certainty of evidence was very low for all outcomes.
The reduction in mortality observed in our study was greater than that reported in a 2006 meta-analysis5 comparing mortality before and after the establishment of trauma systems in all age groups (15% reduction). However, we observed similar reductions in mortality to meta-analyses comparing level I trauma centers to other hospitals for adults with major trauma (33% reduction)10 or trauma centers vs nontrauma centers for all trauma admissions (36%).9 In this last meta-analysis, a subgroup analysis suggested 60% lower odds of mortality when children younger than 19 years were treated in a mature trauma system compared with a nontrauma or early-stage trauma system. Our findings are also in keeping with a large body of literature suggesting that adherence to guidelines and patient outcomes are better when children are treated at pediatric institutions, across a variety of conditions.77,78 This could be due to additional pediatric specialty training,79 better pediatric readiness and access to pediatric-specific equipment or interventions,80 or volume-outcome effects.81 The association for mortality comparing PTCs with CTCs supports these hypotheses. Our results also suggest that the advantage of PTCs over ATCs holds whatever the designation level or verification status.
We did not observe a statistically significant association between trauma center type and mortality for older adolescents, which suggests that the advantage of PTCs may not hold for this population. However, our results do not clarify what the optimal age cutoff should be or whether other factors such as pubertal status and size should be accounted for. Although the American Academy of Pediatrics discourages the use of arbitrary age limits to guide clinical care,82 the absence of age criteria in clinical decision rules, including triage tools83 and clinical practice guidelines,84 is a major barrier to their implementation.
Our results support the advantage of PTCs in the subpopulation of children with head injuries and penetrating injuries. Results on SOI were not statistically significant but also suggested an association with more favorable outcomes in PTCs than ATCs. Our observations may reflect the differences in treatment recommendations for these injuries between children and adults.85,86 We did not have sufficient data to evaluate associations for other types of injuries including rare pathologies such as vascular or urological injuries, for which expertise in PTCs may be lacking.87,88
Given the risks of exposure to ionizing radiation in children, multiple guidelines emit recommendations on limiting the use of CT in pediatric populations.89,90,91 Similarly, guidelines suggest operative management can be avoided in favor of interventional radiology or watchful waiting in higher-grade injuries in children than in adults.86,92 Our results suggest that PTCs have higher adherence to these guidelines than ATCs. However, we were unable to isolate inappropriate CT use or operative management, as this information was not reported in most studies. One of the studies included suggested that less aggressive approaches to SOIs among adolescents in PTCs may lead to higher mortality.13
Limitations
Limitations of Evidence
The risk of bias was serious or critical in all included studies, mostly due to confounding or selection bias. The improved outcomes observed in PTC could be explained by immortal time bias, whereby very sick children are not stable enough to transfer to PTCs. However, studies excluding or adjusting for transfers-in did not observe different results. Results could also be explained by a lower threshold for admission in PTCs or increased bed pressure in ATCs, but most studies did not include children with minor injuries and meta-analysis restricted to major trauma did not change our observations. Included studies based on trauma registries with facultative participation may be subject to selection bias, whereby hospitals with more quality improvement resources are more likely to participate. However, this would be expected to lead to an underestimation of the advantage of PTCs. Additionally, complications may be better recorded or more thoroughly screened in PTCs,93 which may explain the lack of benefit of PTCs for this outcome.
Other limits of the body of evidence include the lack of studies on outcomes related to functional status and quality of life, which may be more important to injured children and their families, and the lack of data on costs, which is critical to providing high-value and sustainable health care.94 Furthermore, we were unable to conduct subgroup analyses for outcomes other than mortality and low sample sizes led to very imprecise estimates of association in most subgroup analyses. Additionally, heterogeneity of our pooled estimates was high and was not reduced for subgroup analyses other than type of injury. There are therefore likely to be other factors explaining heterogeneity that could not be explored in this study.
Limitations of the Review Process
We had to rely on authors’ definitions of trauma center designation, which likely varied across systems. However, analyses limited to ACS-verified centers led to similar results. We were unable to limit our review to major trauma because studies used heterogeneous criteria to define injury severity (ISS, abbreviated injury scale, physiological criteria, length of stay, interventions). Along with heterogeneous age criteria, this likely reflects the lack of consensus on which patients should be sent to a PTC, highlighted by the imperfect accuracy of trauma triage tools, particularly in pediatric populations.95 Additionally, the evaluation of publication bias and its inclusion in grades of evidence is controversial96; without this criterion, the evidence on mortality would have been rated low rather than very low.
Conclusions
The results of our study suggest that PTCs may be associated with better outcomes than ATCs or CTCs for children hospitalized following trauma. Results suggest there could be an age cutoff beyond which transfer to a PTC may not be beneficial, but current literature does not provide sufficient evidence on what that cutoff should be. Similarly, our results suggest that PTCs are associated with better outcomes than ATCs for children with head injuries and penetrating injuries, but we did not identify sufficient evidence to extend results to other types of injury. We recommend that future studies better address selection bias by conducting studies on samples that are population-based or have uniform and clearly justified inclusion or exclusion criteria. Confounding control could be improved by adequately adjusting for important confounders including physiological status on arrival and using state-of-the-art methods such as target trial emulation. Future research should also strive to further clarify which patients most benefit from definitive treatment in a PTC, to evaluate functional status and quality of life, and to study the cost-effectiveness of PTCs.
eAppendix 1. Methods
eTable 1. Definitions Used for Study Inclusion Criteria
eTable 2. Search Strategies
eTable 3. Definitions Used for Study Outcomes
eTable 4. Subgroup and Sensitivity Analyses
eFigure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analysis Flow Diagram
eAppendix 2. Excluded Studies
eTable 5. Characteristics of Included Studies
eAppendix 3. Included Studies
eFigure 2. Enhanced Funnel Plot of Studies Evaluating the Odds of mortality in Pediatric Major Trauma at Pediatric Trauma Centers vs Adult Trauma Centers (Trim and Fill Method)
eFigure 3. Forest Plots Describing the Odds of Mortality for Children Aged 15 Years or Less Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) Versus Adult Trauma Centers (ATCs)
eFigure 4. Forest Plots Describing the Odds of Mortality for Children Aged 14 Years or Less Admitted to Hospitals Following Trauma Treated at pediatric Trauma Centers (PTCs) Versus Adult Trauma Centers (ATCs)
eFigure 5. Forest Plots Describing the Odds of Mortality for Children With Head Injury Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 6. Forest Plots Describing the Odds of Mortality for Children With Blunt Solid Organ Injury Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 7. Forest Plots Describing the Odds of Mortality for Children With Penetrating Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 8. Forest Plots Describing the Odds of Mortality for Children With Major Trauma (ISS ≥ 12) Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 9. Forest Plots Describing the Odds of Mortality for children Admitted to Hospitals Following Trauma Treated at Level I Pediatric Trauma Centers (PTCs) vs Level I Adult Trauma Centers (ATCs)
eFigure 10. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs)
eFigure 11. Forest Plots Describing the Odds of Mortality for children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs) With the Same Verification Organization
eFigure 12. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in the US
eFigure 13. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in Other Countries
eFigure 14. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in Studies Recruiting Patients between 2010 to 2014
eFigure 15. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in Studies Recruiting Patients between 2015 to 2023
eFigure 16. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With Studies at Moderate (n=1) or Serious Risk of Bias
eFigure 17. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With Studies at Critical Risk of Bias
eFigure 18. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) for Studies With Transfers Excluded
eFigure 19. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) for Studies With Transfers Included and Adjusted For
eFigure 20. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) for Studies With Transfers Included and Not Adjusted For
eFigure 21. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With 7 Outliers Removed
eFigure 22. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With 3 Outliers Removed
eFigure 23. Forest Plots Describing the Odds of Complications for Children Admitted to Hospitals Following Trauma Treated at pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 24. Forest Plots Describing the Odds of Complications for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs)
eFigure 25. Forest Plots Describing the Odds of Computed Tomography (CT) Imaging for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 27. Forest Plots Describing the Odds of Operative Management for Children Admitted to Hospitals Following Trauma Treated at Level I Pediatric Trauma Centers (PTCs) vs Level I Adult Trauma Centers (ATCs)
eFigure 26. Forest Plots Describing the Odds of Operative Management for Children With Blunt Solid Organ Injuries Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 28. Forest Plots Describing the Odds of Operative Management for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs)
eFigure 29. Forest Plots Describing the Odds of Operative Management for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs) With the Same Verification Organization
eFigure 30. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Combined Adult and Pediatric Centers (CTCs)
eTable 6. Results Not Included in Meta-Analyses
Data Sharing Statement
References
- 1.Centers for Disease Control and Prevention . Injuries among children and teens. 2021. Accessed March 15, 2023. https://www.cdc.gov/injury/features/child-injury/index.html
- 2.Peterson C, Miller GF, Barnett SBL, Florence C. Economic cost of injury—United States, 2019. MMWR Morb Mortal Wkly Rep. 2021;70(48):1655-1659. doi: 10.15585/mmwr.mm7048a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNICEF . World report on child injury prevention. 2008. Accessed August 21, 2023. https://www.who.int/publications/i/item/9789241563574
- 4.Amini R, Lavoie A, Moore L, Sirois MJ, Emond M. Pediatric trauma mortality by type of designated hospital in a mature inclusive trauma system. J Emerg Trauma Shock. 2011;4(1):12-19. doi: 10.4103/0974-2700.76824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Celso B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60(2):371-378. doi: 10.1097/01.ta.0000197916.99629.eb [DOI] [PubMed] [Google Scholar]
- 6.Densmore JC, Lim HJ, Oldham KT, Guice KS. Outcomes and delivery of care in pediatric injury. J Pediatr Surg. 2006;41(1):92-98. doi: 10.1016/j.jpedsurg.2005.10.013 [DOI] [PubMed] [Google Scholar]
- 7.Mooney DP, Gutierrez IM, Chen Q, Forbes PW, Zurakowski D. Impact of trauma system development on pediatric injury care. Pediatr Surg Int. 2013;29(3):263-268. doi: 10.1007/s00383-012-3232-1 [DOI] [PubMed] [Google Scholar]
- 8.Webman RB, Carter EA, Mittal S, et al. Association between trauma center type and mortality among injured adolescent patients. JAMA Pediatr. 2016;170(8):780-786. doi: 10.1001/jamapediatrics.2016.0805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alharbi RJ, Shrestha S, Lewis V, Miller C. The effectiveness of trauma care systems at different stages of development in reducing mortality: a systematic review and meta-analysis. World J Emerg Surg. 2021;16(1):38. doi: 10.1186/s13017-021-00381-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Ditshuizen JC, Van Den Driessche CRL, Sewalt CA, Van Lieshout EMM, Verhofstad MHJ, Den Hartog D. The association between level of trauma care and clinical outcome measures: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2020;89(4):801-812. doi: 10.1097/TA.0000000000002850 [DOI] [PubMed] [Google Scholar]
- 11.Wesson DE. Pediatric trauma centers: coming of age. Tex Heart Inst J. 2012;39(6):871-873. [PMC free article] [PubMed] [Google Scholar]
- 12.Alexander M, Zaghal A, Wetjen K, Shelton J, Shilyansky J. Pediatric trauma center verification improves quality of care and reduces resource utilization in blunt splenic injury. J Pediatr Surg. 2019;54(1):155-159. doi: 10.1016/j.jpedsurg.2018.10.004 [DOI] [PubMed] [Google Scholar]
- 13.Derderian SC, Meier M, Bensard DD, Partrick DA, Acker SN. Adolescent blunt solid organ injury: Differences in management strategies and outcomes between pediatric and adult trauma centers. Am J Surg. 2022;224(1 Pt A):13-17. doi: 10.1016/j.amjsurg.2022.02.054 [DOI] [PubMed] [Google Scholar]
- 14.Evans J, Murch H, Begley R, et al. Mortality in adolescent trauma: a comparison of children’s, mixed and adult major trauma centres. Emerg Med J. 2021;38(7):488-494. doi: 10.1136/emermed-2020-210384 [DOI] [PubMed] [Google Scholar]
- 15.Green PA, Wilkinson DJ, Bouamra O, Fragoso M, Farrelly PJ. Variations in the management of adolescents with blunt splenic trauma in England and Wales: are we preserving enough? Ann R Coll Surg Engl. 2020;102(7):488-492. doi: 10.1308/rcsann.2020.0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahran A, Fernstrum A, Swindle M, et al. Impact of trauma center designation in pediatric renal trauma: National Trauma Data Bank analysis. J Pediatr Urol. 2020;16(5):658.e1-658.e9. doi: 10.1016/j.jpurol.2020.07.019 [DOI] [PubMed] [Google Scholar]
- 17.Rogers FB, Horst MA, Morgan ME, et al. A comparison of adolescent penetrating trauma patients managed at pediatric versus adult trauma centers in a mature trauma system. J Trauma Acute Care Surg. 2020;88(6):725-733. doi: 10.1097/TA.0000000000002643 [DOI] [PubMed] [Google Scholar]
- 18.Swendiman RA, Luks VL, Hatchimonji JS, et al. Mortality after adolescent firearm injury: effect of trauma center designation. J Adolesc Health. 2021;68(5):978-984. doi: 10.1016/j.jadohealth.2020.09.004 [DOI] [PubMed] [Google Scholar]
- 19.Yanchar NL, Lockyer L, Ball CG, Assen S. Pediatric versus adult paradigms for management of adolescent injuries within a regional trauma system. J Pediatr Surg. 2021;56(3):512-519. doi: 10.1016/j.jpedsurg.2020.07.032 [DOI] [PubMed] [Google Scholar]
- 20.Higgins J, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2022. Accessed February 17, 2023. http://www.training.cochrane.org/handbook
- 21.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71):n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455-463. doi: 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 25.Brozek JL, Akl EA, Alonso-Coello P, et al. ; GRADE Working Group . Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64(5):669-677. doi: 10.1111/j.1398-9995.2009.01973.x [DOI] [PubMed] [Google Scholar]
- 26.Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1(2):112-125. doi: 10.1002/jrsm.11 [DOI] [PubMed] [Google Scholar]
- 27.Gerber N, Munnangi S, Vengalasetti Y, Gupta S. Trauma center variation of head computed tomography utilization in children presenting with mild traumatic brain injury. Clin Imaging. 2023;94:125-131. doi: 10.1016/j.clinimag.2022.11.024 [DOI] [PubMed] [Google Scholar]
- 28.Hairr M, Tumin D, Greene E, Ledoux M, Longshore S. Facility size and risk factors for mortality in pediatric trauma. Am Surg. 2022;31348221121555. doi: 10.1177/00031348221121555 [DOI] [PubMed] [Google Scholar]
- 29.Lewit RA, Veras LV, Kocak M, Nouer SS, Gosain A. Pediatric traumatic brain injury: resource utilization and outcomes at adult versus pediatric trauma centers. Surg Open Sci. 2022;7:68-73. doi: 10.1016/j.sopen.2021.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Killien EY, Grassia KL, Butler EK, et al. Variation in tracheostomy placement and outcomes following pediatric trauma among adult, pediatric, and combined trauma centers. J Trauma Acute Care Surg. 94(4):615-623 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pulido OR, Morgan ME, Bradburn E, Perea LL. A statewide analysis of pediatric liver injuries treated at adult versus pediatric trauma centers. J Surg Res. 2022;272:184-189. doi: 10.1016/j.jss.2021.12.022 [DOI] [PubMed] [Google Scholar]
- 32.Sheff ZT, Engbrecht BW, Rodgers R, Jacobson LE, Smith JL. Mortality of adolescents with isolated traumatic brain injury does not vary with type of level I trauma center. J Trauma Acute Care Surg. 2022;93(4):538-544. doi: 10.1097/TA.0000000000003611 [DOI] [PubMed] [Google Scholar]
- 33.Stephenson KJ, Shewmake CN, Bowman SM, et al. Elder child or young adult? Adolescent trauma mortality amongst pediatric and adult facilities. Am J Surg. 2022;224(6):1445-1449. doi: 10.1016/j.amjsurg.2022.08.017 [DOI] [PubMed] [Google Scholar]
- 34.Ali A, Tatum D, Jones G, et al. Computed tomography for pediatric pelvic fractures in pediatric versus adult trauma centers. J Surg Res. 2021;259:47-54. doi: 10.1016/j.jss.2020.11.015 [DOI] [PubMed] [Google Scholar]
- 35.Khalil M, Alawwa G, Pinto F, O’Neill PA. Pediatric mortality at pediatric versus adult trauma centers. J Emerg Trauma Shock. 2021;14(3):128-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim W, Ahn N, Ata A, Adamo MA, Entezami P, Edwards M. Pediatric cervical spine injury in the United States: defining the burden of injury, need for operative intervention, and disparities in imaging across trauma centers. J Pediatr Surg. 2021;56(2):293-296. doi: 10.1016/j.jpedsurg.2020.05.009 [DOI] [PubMed] [Google Scholar]
- 37.Massoumi R, Wertz J, Duong T, Tseng CH, Jen HC. Variation in pediatric cervical spine imaging across trauma centers—a cause for concern? J Trauma Acute Care Surg. 2021;91(4):641-648. doi: 10.1097/TA.0000000000003344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scantling D, Hatchimonji J, Williamson J, et al. Adjacent adult and pediatric trauma centers: which way to turn with the injured adolescent? Am Surg. 2021;89(4):641-649. [DOI] [PubMed] [Google Scholar]
- 39.Swendiman RA, Abramov A, Fenton SJ, et al. Use of angioembolization in pediatric polytrauma patients: with blunt splenic injury angioembolization in pediatric blunt splenic injury. J Pediatr Surg. 2021;56(11):2045-2051. doi: 10.1016/j.jpedsurg.2021.04.014 [DOI] [PubMed] [Google Scholar]
- 40.Filipescu R, Powers C, Yu H, et al. The adherence of adult trauma centers to American Pediatric Surgical Association guidelines on management of blunt splenic injuries. J Pediatr Surg. 2020;55(9):1748-1753. doi: 10.1016/j.jpedsurg.2020.01.001 [DOI] [PubMed] [Google Scholar]
- 41.Hatchimonji JS, Swendiman RA, Goldshore MA, et al. Pediatric firearm mortality in the United States, 2010 to 2016: a National Trauma Data Bank analysis. J Trauma Acute Care Surg. 2020;88(3):402-407. doi: 10.1097/TA.0000000000002573 [DOI] [PubMed] [Google Scholar]
- 42.Prieto JM, Van Gent JM, Calvo RY, et al. Pediatric extremity vascular trauma: it matters where it is treated. J Trauma Acute Care Surg. 2020;88(4):469-476. doi: 10.1097/TA.0000000000002595 [DOI] [PubMed] [Google Scholar]
- 43.Prieto JM, Van Gent JM, Calvo RY, et al. Evaluating surgical outcomes in pediatric extremity vascular trauma. J Pediatr Surg. 2020;55(2):319-323. doi: 10.1016/j.jpedsurg.2019.10.014 [DOI] [PubMed] [Google Scholar]
- 44.Strait L, Sussman R, Ata A, Edwards MJ. Utilization of CT imaging in minor pediatric head, thoracic, and abdominal trauma in the United States. J Pediatr Surg. 2020;55(9):1766-1772. doi: 10.1016/j.jpedsurg.2020.01.006 [DOI] [PubMed] [Google Scholar]
- 45.Swendiman RA, Goldshore MA, Fenton SJ, Nance ML. Defining the role of angioembolization in pediatric isolated blunt solid organ injury. J Pediatr Surg. 2020;55(4):688-692. doi: 10.1016/j.jpedsurg.2019.04.036 [DOI] [PubMed] [Google Scholar]
- 46.Yung N, Solomon D, Schuster K, Christison-Lagay E. Closing the gap in care of blunt solid organ injury in children. J Trauma Acute Care Surg. 2020;89(5):894-899. doi: 10.1097/TA.0000000000002757 [DOI] [PubMed] [Google Scholar]
- 47.Myers SR, Branas CC, French B, Nance ML, Carr BG. A national analysis of pediatric trauma care utilization and outcomes in the United States. Pediatr Emerg Care. 2019;35(1):1-7. doi: 10.1097/PEC.0000000000000902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sathya C, Alali AS, Wales PW, et al. Computed tomography rates and estimated radiation-associated cancer risk among injured children treated at different trauma center types. Injury. 2019;50(1):142-148. doi: 10.1016/j.injury.2018.09.036 [DOI] [PubMed] [Google Scholar]
- 49.Vassallo J, Webster M, Barnard EBG, Lyttle MD, Smith JE; PERUKI (Paediatric Emergency Research in the UK and Ireland) . Epidemiology and aetiology of paediatric traumatic cardiac arrest in England and Wales. Arch Dis Child. 2019;104(5):437-443. doi: 10.1136/archdischild-2018-314985 [DOI] [PubMed] [Google Scholar]
- 50.Bardes JM, Benjamin E, Escalante AA, Wu J, Demetriades D. Severe traumatic brain injuries in children: does the type of trauma center matter? J Pediatr Surg. 2018;53(8):1523-1525. doi: 10.1016/j.jpedsurg.2017.09.017 [DOI] [PubMed] [Google Scholar]
- 51.Schlegel C, Greeno A, Chen H, et al. Evolution of a level I pediatric trauma center: changes in injury mechanisms and improved outcomes. Surgery. 2018;163(5):1173-1177. doi: 10.1016/j.surg.2017.10.070 [DOI] [PubMed] [Google Scholar]
- 52.Adams SE, Holland A, Brown J. Management of paediatric splenic injury in the New South Wales trauma system. Injury. 2017;48(1):106-113. doi: 10.1016/j.injury.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 53.Mitchell RJ, Curtis K, Testa L, Holland AJ, Sv Soundappan S, Adams S. Differences in survival outcome for severely injured paediatric trauma by type of trauma centre. J Paediatr Child Health. 2017;53(8):808-813. doi: 10.1111/jpc.13514 [DOI] [PubMed] [Google Scholar]
- 54.Miyata S, Cho J, Matsushima K, et al. Association between pediatric blunt splenic injury volume and the splenectomy rate. J Pediatr Surg. 2017;52(11):1816-1821. doi: 10.1016/j.jpedsurg.2017.02.007 [DOI] [PubMed] [Google Scholar]
- 55.Miyata S, Cho J, Lebedevskiy O, Matsushima K, Bae E, Bliss DW. Trauma experts versus pediatric experts: comparison of outcomes in pediatric penetrating injuries. J Surg Res. 2017;208:173-179. doi: 10.1016/j.jss.2016.09.040 [DOI] [PubMed] [Google Scholar]
- 56.Baudin F, Floccard B, Desgranges FP, et al. Effectiveness of management of children with severe trauma in a pediatric trauma center and in an adult trauma center: A before-after study. [in French] Arch Pediatr. 2016;23(4):367-372. doi: 10.1016/j.arcped.2015.12.023 [DOI] [PubMed] [Google Scholar]
- 57.Pandit V, Michailidou M, Rhee P, et al. The use of whole body computed tomography scans in pediatric trauma patients: are there differences among adults and pediatric centers? J Pediatr Surg. 2016;51(4):649-653. doi: 10.1016/j.jpedsurg.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 58.Safavi A, Skarsgard ED, Rhee P, et al. Trauma center variation in the management of pediatric patients with blunt abdominal solid organ injury: a national trauma data bank analysis. J Pediatr Surg. 2016;51(3):499-502. doi: 10.1016/j.jpedsurg.2015.08.012 [DOI] [PubMed] [Google Scholar]
- 59.Walther AE, Falcone RA, Pritts TA, Hanseman DJ, Robinson BR. Pediatric and adult trauma centers differ in evaluation, treatment, and outcomes for severely injured adolescents. J Pediatr Surg. 2016;51(8):1346-1350. doi: 10.1016/j.jpedsurg.2016.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kelley-Quon LI, Crowley MA, Applebaum H, et al. Academic-community partnerships improve outcomes in pediatric trauma care. J Pediatr Surg. 2015;50(6):1032-1036. doi: 10.1016/j.jpedsurg.2015.03.033 [DOI] [PubMed] [Google Scholar]
- 61.Marin JR, Wang L, Winger DG, Mannix RC. Variation in computed tomography imaging for pediatric injury-related emergency visits. J Pediatr. 2015;167(4):897-904.e3. doi: 10.1016/j.jpeds.2015.06.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sathya C, Alali AS, Wales PW, et al. Mortality among injured children treated at different trauma center types. JAMA Surg. 2015;150(9):874-881. doi: 10.1001/jamasurg.2015.1121 [DOI] [PubMed] [Google Scholar]
- 63.Walther AE, Pritts TA, Falcone RA, Hanseman DJ, Robinson BR. Teen trauma without the drama: outcomes of adolescents treated at Ohio adult versus pediatric trauma centers. J Trauma Acute Care Surg. 2014;77(1):109-116. doi: 10.1097/TA.0000000000000277 [DOI] [PubMed] [Google Scholar]
- 64.Lippert SJ, Hartin CW Jr, Ozgediz DE, et al. Splenic conservation: variation between pediatric and adult trauma centers. J Surg Res. 2013;182(1):17-20. doi: 10.1016/j.jss.2012.07.036 [DOI] [PubMed] [Google Scholar]
- 65.Matsushima K, Schaefer EW, Won EJ, Nichols PA, Frankel HL. Injured adolescents, not just large children: difference in care and outcome between adult and pediatric trauma centers. Am Surg. 2013;79(3):267-273. doi: 10.1177/000313481307900325 [DOI] [PubMed] [Google Scholar]
- 66.Matsushima K, Kulaylat AN, Won EJ, Stokes AL, Schaefer EW, Frankel HL. Variation in the management of adolescent patients with blunt abdominal solid organ injury between adult versus pediatric trauma centers: an analysis of a statewide trauma database. J Surg Res. 2013;183(2):808-813. doi: 10.1016/j.jss.2013.02.050 [DOI] [PubMed] [Google Scholar]
- 67.Mitchell RJ, Curtis K, Chong S, et al. Comparative analysis of trends in paediatric trauma outcomes in New South Wales, Australia. Injury. 2013;44(1):97-103. doi: 10.1016/j.injury.2011.11.012 [DOI] [PubMed] [Google Scholar]
- 68.Wang NE, Saynina O, Vogel LD, Newgard CD, Bhattacharya J, Phibbs CS. The effect of trauma center care on pediatric injury mortality in California, 1999 to 2011. J Trauma Acute Care Surg. 2013;75(4):704-716. doi: 10.1097/TA.0b013e31829a0a65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Potoka DA, Schall LC, Ford HR. Risk factors for splenectomy in children with blunt splenic trauma. J Pediatr Surg. 2002;37(3):294-299. doi: 10.1053/jpsu.2002.30824 [DOI] [PubMed] [Google Scholar]
- 70.Osler TM, Vane DW, Tepas JJ, Rogers FB, Shackford SR, Badger GJ. Do pediatric trauma centers have better survival rates than adult trauma centers? An examination of the National Pediatric Trauma Registry. J Trauma. 2001;50(1):96-101. doi: 10.1097/00005373-200101000-00017 [DOI] [PubMed] [Google Scholar]
- 71.Potoka DA, Schall LC, Ford HR. Improved functional outcome for severely injured children treated at pediatric trauma centers. J Trauma. 2001;51(5):824-832. doi: 10.1097/00005373-200111000-00002 [DOI] [PubMed] [Google Scholar]
- 72.Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of pediatric trauma centers on mortality in a statewide system. J Trauma. 2000;49(2):237-245. doi: 10.1097/00005373-200008000-00009 [DOI] [PubMed] [Google Scholar]
- 73.Frumiento C, Vane DW. Changing patterns of treatment for blunt splenic injuries: an 11-year experience in a rural state. J Pediatr Surg. 2000;35(6):985-988. doi: 10.1053/jpsu.2000.6948 [DOI] [PubMed] [Google Scholar]
- 74.Bernardo LM, Gardner MJ, Miracle TB, Henker R. Analgesic prescription and administration to adolescents admitted to an adult versus pediatric trauma center. J Trauma Nurs. 1997;4(1):13-21. doi: 10.1097/00043860-199701000-00006 [DOI] [PubMed] [Google Scholar]
- 75.Nakayama DK, Copes WS, Sacco W. Differences in trauma care among pediatric and nonpediatric trauma centers. J Pediatr Surg. 1992;27(4):427-431. doi: 10.1016/0022-3468(92)90328-5 [DOI] [PubMed] [Google Scholar]
- 76.Moore L, Lauzier F, Stelfox HT, et al. Validation of complications selected by consensus to evaluate the acute phase of adult trauma care: a multicenter cohort study. Ann Surg. 2015;262(6):1123-1129. doi: 10.1097/SLA.0000000000000963 [DOI] [PubMed] [Google Scholar]
- 77.Auerbach M, Whitfill T, Gawel M, et al. Differences in the quality of pediatric resuscitative care across a spectrum of emergency departments. JAMA Pediatr. 2016;170(10):987-994. doi: 10.1001/jamapediatrics.2016.1550 [DOI] [PubMed] [Google Scholar]
- 78.Michelson KA, Lyons TW, Hudgins JD, et al. Use of a national database to assess pediatric emergency care across united states emergency departments. Acad Emerg Med. 2018;25(12):1355-1364. doi: 10.1111/acem.13489 [DOI] [PubMed] [Google Scholar]
- 79.Evans C, van Woerden HC. The effect of surgical training and hospital characteristics on patient outcomes after pediatric surgery: a systematic review. J Pediatr Surg. 2011;46(11):2119-2127. doi: 10.1016/j.jpedsurg.2011.06.033 [DOI] [PubMed] [Google Scholar]
- 80.Newgard CD, Lin A, Olson LM, et al. ; Pediatric Readiness Study Group . Evaluation of emergency department pediatric readiness and outcomes among US trauma centers. JAMA Pediatr. 2021;175(9):947-956. doi: 10.1001/jamapediatrics.2021.1319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Morche J, Mathes T, Pieper D. Relationship between surgeon volume and outcomes: a systematic review of systematic reviews. Syst Rev. 2016;5(1):204. doi: 10.1186/s13643-016-0376-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hardin AP, Hackell JM; COMMITTEE ON PRACTICE AND AMBULATORY MEDICINE . Age limit of pediatrics. Pediatrics. 2017;140(3):e20172151. doi: 10.1542/peds.2017-2151 [DOI] [PubMed] [Google Scholar]
- 83.Centers for Disease Control and Prevention . Guidelines for field triage of injured patients. 2012. Accessed March 15, 2023. https://www.cdc.gov/mmwr/pdf/rr/rr6101.pdf
- 84.Freire GC, Beno S, Yanchar N, et al. Clinical practice guideline recommendations for pediatric multisystem trauma care: a systematic review. Ann Surg. 2023. doi: 10.1097/SLA.0000000000005966 [DOI] [PubMed] [Google Scholar]
- 85.Brain Trauma Foundation . Guidelines for the management of pediatric severe TBI, 3rd Ed. 2019. Accessed August 21, 2023. https://braintrauma.org/coma/guidelines/pediatric
- 86.Gates RL, Price M, Cameron DB, et al. Non-operative management of solid organ injuries in children: an American Pediatric Surgical Association Outcomes and Evidence Based Practice Committee systematic review. J Pediatr Surg. 2019;54(8):1519-1526. doi: 10.1016/j.jpedsurg.2019.01.012 [DOI] [PubMed] [Google Scholar]
- 87.Bonasso PC, Gurien LA, Smith SD, Gowen ME, Dassinger MS. Pediatric vascular trauma practice patterns and resource availability: a survey of American College of Surgeon-designated pediatric trauma centers. J Trauma Acute Care Surg. 2018;84(5):758-761. doi: 10.1097/TA.0000000000001799 [DOI] [PubMed] [Google Scholar]
- 88.Dunn CL, Burjonrappa S. Pediatric cerebrovascular trauma: incidence, management, and outcomes. J Pediatr Surg. 2023;58(2):310-314. doi: 10.1016/j.jpedsurg.2022.10.034 [DOI] [PubMed] [Google Scholar]
- 89.Choosing Wisely Canada . Radiology—five tests and treatments to question. 2022. Accessed March 14, 2023. https://choosingwiselycanada.org/recommendation/radiology/
- 90.American College of Radiology . ACR appropriateness criteria. 2022. Accessed March 14, 2023. https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria
- 91.American College of Surgeons Trauma Quality Improvement Program . ACS TQIP best practices guidelines in imaging. 2018. Accessed March 14, 2023. https://www.facs.org/media/oxdjw5zj/imaging_guidelines.pdf
- 92.Hagedorn JC, Fox N, Ellison JS, et al. Pediatric blunt renal trauma practice management guidelines: Collaboration between the Eastern Association for the Surgery of Trauma and the Pediatric Trauma Society. J Trauma Acute Care Surg. 2019;86(5):916-925. doi: 10.1097/TA.0000000000002209 [DOI] [PubMed] [Google Scholar]
- 93.Moore L, Lauzier F, Stelfox HT, et al. Derivation and validation of a quality indicator to benchmark in-hospital complications among injury admissions. JAMA Surg. 2016;151(7):622-630. doi: 10.1001/jamasurg.2015.5484 [DOI] [PubMed] [Google Scholar]
- 94.Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477-2481. doi: 10.1056/NEJMp1011024 [DOI] [PubMed] [Google Scholar]
- 95.Gianola S, Castellini G, Biffi A, et al. ; Italian National Institute of Health guideline working group . Accuracy of pre-hospital triage tools for major trauma: a systematic review with meta-analysis and net clinical benefit. World J Emerg Surg. 2021;16(1):31. doi: 10.1186/s13017-021-00372-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Simieniuk R, Guyatt G. What is GRADE? Accessed March 7, 2023. https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Methods
eTable 1. Definitions Used for Study Inclusion Criteria
eTable 2. Search Strategies
eTable 3. Definitions Used for Study Outcomes
eTable 4. Subgroup and Sensitivity Analyses
eFigure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analysis Flow Diagram
eAppendix 2. Excluded Studies
eTable 5. Characteristics of Included Studies
eAppendix 3. Included Studies
eFigure 2. Enhanced Funnel Plot of Studies Evaluating the Odds of mortality in Pediatric Major Trauma at Pediatric Trauma Centers vs Adult Trauma Centers (Trim and Fill Method)
eFigure 3. Forest Plots Describing the Odds of Mortality for Children Aged 15 Years or Less Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) Versus Adult Trauma Centers (ATCs)
eFigure 4. Forest Plots Describing the Odds of Mortality for Children Aged 14 Years or Less Admitted to Hospitals Following Trauma Treated at pediatric Trauma Centers (PTCs) Versus Adult Trauma Centers (ATCs)
eFigure 5. Forest Plots Describing the Odds of Mortality for Children With Head Injury Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 6. Forest Plots Describing the Odds of Mortality for Children With Blunt Solid Organ Injury Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 7. Forest Plots Describing the Odds of Mortality for Children With Penetrating Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 8. Forest Plots Describing the Odds of Mortality for Children With Major Trauma (ISS ≥ 12) Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 9. Forest Plots Describing the Odds of Mortality for children Admitted to Hospitals Following Trauma Treated at Level I Pediatric Trauma Centers (PTCs) vs Level I Adult Trauma Centers (ATCs)
eFigure 10. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs)
eFigure 11. Forest Plots Describing the Odds of Mortality for children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs) With the Same Verification Organization
eFigure 12. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in the US
eFigure 13. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in Other Countries
eFigure 14. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in Studies Recruiting Patients between 2010 to 2014
eFigure 15. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) in Studies Recruiting Patients between 2015 to 2023
eFigure 16. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With Studies at Moderate (n=1) or Serious Risk of Bias
eFigure 17. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With Studies at Critical Risk of Bias
eFigure 18. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) for Studies With Transfers Excluded
eFigure 19. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) for Studies With Transfers Included and Adjusted For
eFigure 20. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) for Studies With Transfers Included and Not Adjusted For
eFigure 21. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With 7 Outliers Removed
eFigure 22. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs) With 3 Outliers Removed
eFigure 23. Forest Plots Describing the Odds of Complications for Children Admitted to Hospitals Following Trauma Treated at pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 24. Forest Plots Describing the Odds of Complications for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs)
eFigure 25. Forest Plots Describing the Odds of Computed Tomography (CT) Imaging for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 27. Forest Plots Describing the Odds of Operative Management for Children Admitted to Hospitals Following Trauma Treated at Level I Pediatric Trauma Centers (PTCs) vs Level I Adult Trauma Centers (ATCs)
eFigure 26. Forest Plots Describing the Odds of Operative Management for Children With Blunt Solid Organ Injuries Treated at Pediatric Trauma Centers (PTCs) vs Adult Trauma Centers (ATCs)
eFigure 28. Forest Plots Describing the Odds of Operative Management for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs)
eFigure 29. Forest Plots Describing the Odds of Operative Management for Children Admitted to Hospitals Following Trauma Treated at Level I and II Pediatric Trauma Centers (PTCs) vs Level I and II Adult Trauma Centers (ATCs) With the Same Verification Organization
eFigure 30. Forest Plots Describing the Odds of Mortality for Children Admitted to Hospitals Following Trauma Treated at Pediatric Trauma Centers (PTCs) vs Combined Adult and Pediatric Centers (CTCs)
eTable 6. Results Not Included in Meta-Analyses
Data Sharing Statement