Abstract
Statins are inhibitors of β-hydroxy β-methylglutaryl-CoA (HMG-CoA) reductase (HMGCR). They are used in patients with cardiovascular risk and/or suffering with cardiovascular disease. In addition to their efficient lipid-lowering effects, statins exhibit independent so called pleiotropic effects potentially affecting several immune response properties including immune cell activation, migration, cytokine generation, immune metabolism, and survival. Statins also regulate innate and acquired immunity. The focus of this review is to highlight the role of statins in modulating the function and differentiation of various blood cells. Given the proposed wider application of these medicines and their potentially important advantages in treatment of inflammatory and autoimmune disorders, more studies are needed with special focus on the molecular targets of statins included in regulating the immune response.
Keywords: statins, lipid-lowering therapies, cardiovascular health, cell differentiation
Statins
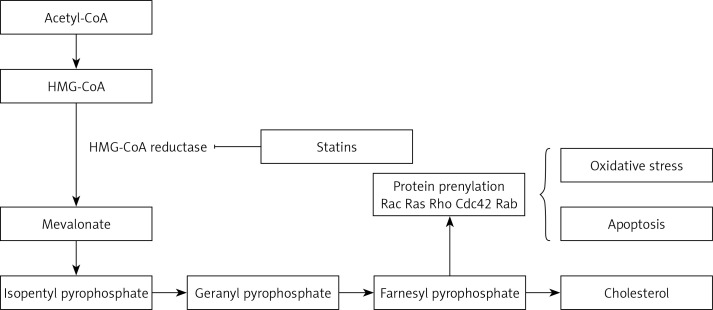
Statins are inhibitors of HMG-CoA reductase (HMGCR) and widely administered as lipid-modulatory agents in primary and secondary prevention of cardiovascular disease (CVD). HMGCR inhibition has a rate-limiting effect in the cholesterol synthesis pathway through conversion of 3-hydroxy-3-methyl glutaryl-CoA (HMG-CoA) to mevalonate. Statins are designed to match the enzymatic active site, resulting in structural changes, reduced enzyme activity and subsequent reduction in cholesterol synthesis [1].
Statins decrease low-density lipoprotein (LDL) cholesterol levels more effectively than most of the other cholesterol-lowering drugs. Despite the introduction of newer cholesterol-lowering agents [2–5], statins are still the most widely used drugs for this purpose. They also reduce triglyceride and increase high-density lipoprotein (HDL) cholesterol levels [6–8]. Additional pharmacological effects include enhancing LDL uptake, reducing protein prenylation, improving endothelial function, modulating inflammation, preserving plaque stability and inhibiting thrombosis [9–22]. Overall, statins have a key role in cardiovascular treatment regimens reducing the risk of atherosclerotic diseases with different levels of effectiveness based on underlying risk factors and CVD history. Clinical practice protocols typically suggest in the first place lifestyle amendment, with potential benefits from adopting a cholesterol-reducing diet and increased physical activity. In those who struggle with lifestyle interventions or are unable to meet their lipid-lowering goals by these measures alone, statins may prove beneficial [23–26]. Their use is not without controversy and their advantageous therapeutic effects are sometimes overshadowed by reported negative effects. Prolonged use of statins can cause adverse effects such as myopathy, neurological effects, e.g. fatigue and impaired cognition, and enhanced diabetes risk [27–29].
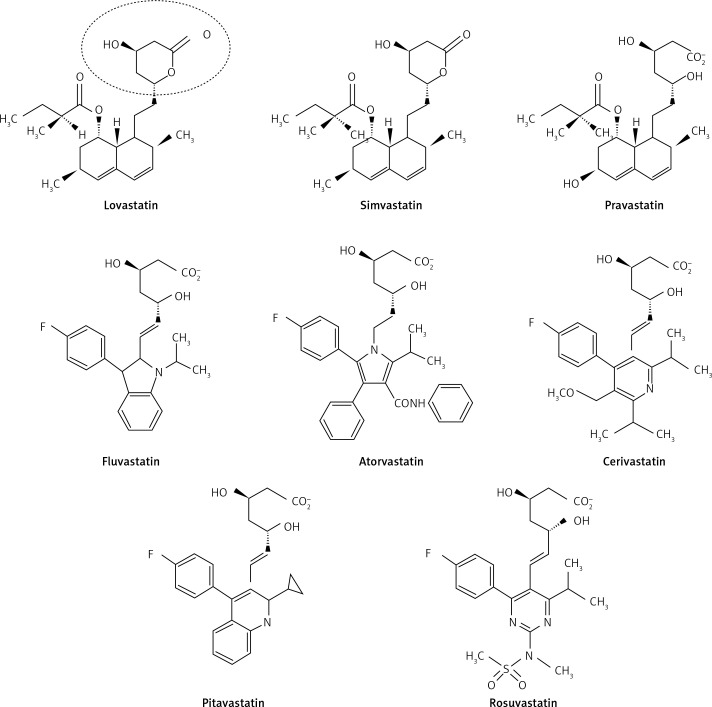
Statins are derived from two origins; 1. biological – extracted from Penicillium and Aspergillus fungal metabolites (examples include lovastatin, pravastatin and simvastatin); and 2. synthetic – including atorvastatin, cerivastatin, fluvastatin, pitavastatin and rosuvastatin [30, 31]. According to their lipophilicity they are divided into two groups: lipophilic statins including atorvastatin, simvastatin, lovastatin, fluvastatin, cerivastatin and pitavastatin which are susceptible to cytochrome P450; and hydrophilic ones including pravastatin and rosuvastatin, which are not susceptible to cytochrome P450 [32].
As with all medicinal classes, statins have similar mechanisms of action but vary in terms of chemical structure; therefore their pharmacokinetic properties and ability to modify lipid levels also vary. In terms of LDL-C lowering, rosuvastatin has proven most effective, whilst pravastatin and simvastatin are better for increasing HDL-C, and atorvastatin in reducing triglyceride levels [31, 32] (Figure 1).
Figure 1.
Structure of different forms of statins [29]
Secondary to their important lipid-lowering effects, statins also display pleiotropic or non-lipid lowering effects. They have the potential to affect several immune responses including immune cell activation, migration, cytokine generation, immune metabolism, and survival. Statins also demonstrate immunomodulatory effects regulating innate and acquired immunity through modulating interactions of T-cells and antigen presenting cells (APCs), thus altering inflammatory cytokine levels. They could affect the volume of red blood cells (RBC) and platelets (PLT) as well. In the following section their effects on blood cells will be discussed.
Blood cell differentiation
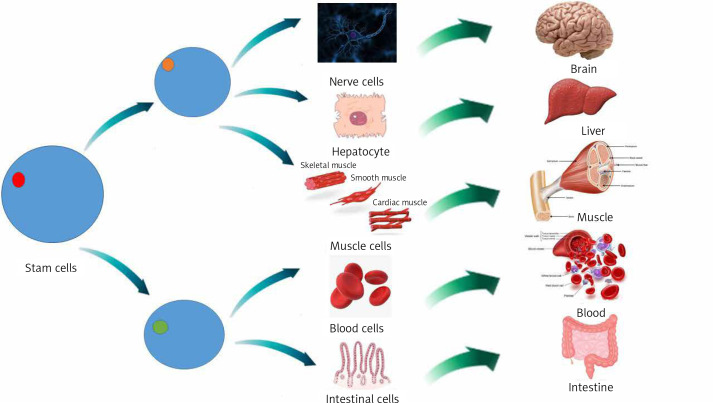
The changing of cells from one type to another is called cellular differentiation [33, 34]. The cell usually converts to a more specific kind (Figure 2). Differentiation happens many times throughout the evolution of a multicellular organism while it switches from a simple zygote to a complicated system of tissues and cell groups (Figure 2). Stem cells are divided during tissue repair and cellular circulation, and produce completely differentiated daughter cells, with differentiation maintained in adult cells. There is some differentiation when an antigen is located on the cell surface. Size, structure, membrane potential, metabolic function and signal reflection of a cell are radically modified by differentiation. These modifications are attributable to extremely controlled changes in gene expression (understood by epigenetics). Except for some cases, cell differentiation never results in a change in the DNA sequence. Therefore, even with a similar genome, cells have potentially numerous physical differences [35].
Figure 2.
Stem cell differentiation to various types of cells
Mesenchymal stem cells (MSCs) are tissue-resident multipotent stem cells that have demonstrated the ability to differentiate into various cell lines, including mesodermal adipogenic, chondrogenic, osteogenic hepatogenic, ectodermal neurogenic lines and, also into blood cells [36].
MSCs are disseminated throughout all tissues and aid tissue repair and homeostasis. At first MSCs are commonly discovered in a dormant phase and it is proposed that they re-enter the cell cycle when stimulated internally or externally and progress towards proliferation and differentiation [37]. This primary contact of MSCs with other cell types is essential for ordinary tissue homeostasis. For instance, it was revealed that a mixture of endothelial cells with MSCs is engaged in the development of vascular networks [38]. Moreover tissue-resident stem cells can differentiate into macrophages (MQ), as demonstrated by gene expression, cell surface marker attributes, cytokine manufacture or even functional behavior [39].
Effects of statins on cells which play roles in immunity
T cells
As mentioned above, statins may be immunomodulatory and can affect T cells. Two different pathways have been suggested in relation to this action; an HMGCR-independent pathway, including allosteric hindrance of lymphocyte function-associated antigen 1 (LFA-1), which represses activation, proliferation, and cellular migration of T cells [40] and HMGCR-dependent mechanisms, which rely on their ability to prevent prenylation of small GTPases [41, 42]. Moreover, new records have presented data that some statins change T helper cell differentiation through developing T helper 2 polarization and repressing T helper 1 polarization both in vitro and in vivo [43, 44]. Work by Arora et al. showed that simvastatin develops T helper 2 cell polarization through up-regulation of the chitinase family member Ym1 in dendritic cells (DCs) [45]. Moreover, statins prevent T cells from differentiating by interfering with the function, differentiation and maturity of APCs. Statins impede APC development through down-regulation of CCR7, CD40, CD83, and CD86 on cytokine-excited DCs [46].
CD8+ T-cells
Deficient T-cell homing is associated with an increased inability of T cells to interact with peptide antigens offered by APC, a mechanism that happens in peripheral lymphoid organs. However, statins have been reported to prevent the activation and proliferation of T cells interacting with agonistic anti-CD3 monoclonal antibody (mAb) or Staphylococcus aureus enterotoxin (SEB), an impact attributed to the deficiency of pathways regulated by small Ras-like GTPases in T-cell receptor (TCR) signaling for the former stimulus through lymphocyte function-associated antigen 1 (LFA-1) blockage [47, 48]. Bu et al. discovered that simvastatin or pitavastatin significantly hinders proliferative responses of immature murine cytotoxic T lymphocytes (CTL) for TCR stimulation due to Kruppel-like factor 2 (KLF2). They furthermore found that statins negatively affect the effectors of CTL proliferation and IFN-γ expression. These findings indicate that statins can affect both the priming and the effector stages of T-cell responses. Simvastatin and pitavastatin also hindered the modest proliferative response of T cells triggered by α-CD3, and more vigorous proliferative response of human T cells to αCD3 and anti-CD28. Human T cell IFN-γ up-regulation, resulting from PHA plus IL-2 stimulation, has also been drastically decreased by simvastatin. Decreased IFN-γ expressed by human T-cells induced by PHA and IL-2 was also demonstrated [49].
As outlined above, statins disrupt processing and presentation of antigens by MHC class II in human DCs and B lymphocytes via reduced antigen uptake by both receptor-mediated endocytosis and macropinocytosis [50]. Activation of Rho and Rab GTPases leads to the primary phase of extracellular antigen cross-presentation in which antigens are absorbed through phagocytosis or receptor-mediated endocytosis [51, 52]. Moreover, hydrophilic proteins need localization into specific organelles defined by the expression of Rab5 and EEA1 to be cross-presented [53]. It is proposed that statins disrupt this process, as in simvastatin-treated APCs, cross-presentation was dramatically repressed. This repression was inverted by adding mevalonate, demonstrating that simvastatin’s repressing influence on cross-presentation depends on its HMGCR inhibiting ability [54]. Mannose receptor endocytosis of particulate antigens is crucial for cross-presentation [53]. To determine simvastatin’s influence on mannose receptor-dependent endocytosis, absorption of fluorescein isothiocyanate (FITC) labeled dextrans, which are internalized through both fluid-phase and mannose-dependent endocytosis, was evaluated [55, 56]. Simvastatin treatment led to a considerable decrease in splenocyte absorption of dextran-FITC, an impact that was modified by mevalonate. While simvastatin can prevent extra levels in antigen cross-presentation through APC, poor absorption of soluble antigen seems to be key in cross-presentation malfunction.
Statins and Treg cells
There is increasing evidence aiding understanding of the mechanisms behind the immunomodulatory effects of statins from in vivo and in vitro investigations. This includes proposed up-regulation of endothelial nitric oxide synthase (NOS3), decreased stimulation of endothelial cells, development of anti-oxidative responses, decreased migration of inflammatory cells, decreased antigen presentation because of suppressed MHC II expression in endothelial cells [57] resulting from promoter IV of class II trans-activator (CIITA) [58], down-regulation of pro-inflammatory cytokines, decreased PLT accumulation, development of 15-epi-lipoxin (15-epi-LXB4), which operates through preventing the signaling pathways engaged in the stimulation of the inflammatory response induced by lipid agents [59, 60] and, finally, enhanced migration, differentiation, and prohibitory functions of Treg cells [59, 61]. It is well affirmed from recent experimental findings that interleukin 6 (IL-6) signaling via STAT-3 contributes to repression of foxp3 transcription, so the probable repression of IL-6 signaling by statins may indirectly support foxp3 expression, leading to an improved proportion of Treg cells [62].
Statins and Th1 cells
It is proposed that statins affect Tregs’ operation through suppressing T helper 1 immune reactions. In accordance with this, statins can regulate various stages of T helper1 induction. Another mechanism includes modulating CD40 expression in addition to recognition on developed B cells and some epithelial cells. It stimulates IL-12 expression, facilitating differentiation and clonal expansion of TH cells toward T helper1 cells [63]. Atorvastatin downregulates CD40 and IFN-γ induced generation of TNF-α on human endothelial cells and monocytes; this effect is altered by administration of exogenous mevalonic acid. In addition to HMGCR impairment, statins also alter differentiation of white blood cells in T helper1 and T helper17 phenotypes, resulting in development of regulatory T cells which express the Foxp3 transcription factor in vitro and in vivo [64]. Also, utilizing a geranylgeranyl transferase inhibitor (GGTI-289) and farnesyltransferase inhibitor (FTI-227), GGTI-289 but not FTI-227 imitates the impact of simvastatin, recommending that hindrance of geranylgeranylation protein dictates the decreased differentiation of T helper17 cells and the expanded differentiation of Treg cells [65].
Statins and Th17 cells
Research on murine models (BALB/c mice) by Li et al. indicated that simvastatin suppresses T helper17 cell differentiation and improves regulatory T cell differentiation in spleen cells grown under varying polarizing circumstances. The researchers also observed that simvastatin treatment in mice reduced infiltration of inflammatory cells toward the peripheral nervous system (PNS) and reduced the rate of IFNγ and IL17 constructing lymphocytes [66]. Moreover, atorvastatin treatment led to downregulation of co-stimulatory molecules for T-cell stimulation, for example, CD80, and enhanced the number of regulatory T cells in mononuclear cell lymph nodes [66]. Accordingly, this information suggests that atorvastatin may work as a suppressor of inflammatory T helper-1 and -17 reactions, downregulating co-stimulatory molecules and concentration of Tregs.
Statin and B cells
Atorvastatin-stimulated naive DC to stem cell conversion in vitro was demonstrated by Li et al. Treatment of these tolerogenic DCs improves experimental autoimmune myasthenia (EAMG) via repressing expansion of lymphocyte cells, development of Treg cells, transformation of T helper1 and T helper17 to T helper2 cells and reducing pathogenic antibody levels [67]. However, the defined systems by which tolerogenic DC treatment decreases antibodies were not completely comprehended. Li et al. discovered that immature bone marrow-derived dendritic cells (BMDCs) were effectively stimulated by atorvastatin under laboratory conditions, which in turn suppressed CD80, CD86, and MHC II molecules [68]. Atorvastatin-modified BMDCs (AT-BMDCs) repressed the number, and the relative affinity, of antiR97-116 IgG antibodies’ further germinal center (GC) function. In addition, T-follicular helper (Tfh) cells and IL21 were reduced by AT-BMDC treatment. Furthermore, the level of CD19+ B cells was somewhat affected, while regulatory B cells were enhanced via AT-BMDCs. One may conclude that AT-BMDCs might improve myasthenia gravis (MG) by controlling humoral immune function and could present a possible approach for MG treatment.
Statins and mast cell and basophil IgE
Kolawole et al. reported that a variety of statins hinder IgE-incited cytokine generation of mast cells and basophils with differing levels of effectiveness [69]. In addition, to prevent fluvastatin repressing vascular reactions to histamine, mice were pre-treated with fluvastatin and by infusing histamine the activity of mast cells was inhibited, which created conditions in which fluvastatin had no effect. This confirms the hypothesis that mast cells are inhibited in vivo by fluvastatin, and supports the use of statins for treatment of mast cell-related disorders. Kolawole et al. also studied the effects of fluvastatin on both C57 black 6 (B6) and 129/SvImJ (also called 129) basophils [69]. They demonstrated that culture for 24 h with fluvastatin before IgE+antigen-mediated activation decreased IL-4, IL-6, IL-13, TNF, and monocyte chemoattractant protein-1 (MCP-1) construction, and prevented degranulation among B6 basophils, but had no major consequence for SvImJ basophils [69].
Statins and neutrophils
The most plentiful type of blood granulocytes is neutrophils, which play an important role in protecting the body against pathogens [70]. Statins interfere with these as outlined earlier, by repression of HMGCR, inhibiting the transformation of HMG-CoA to mevalonate with the downstream restraint of cholesterol construction [71]. Also, metabolites that are constructed during the formation of cholesterol are utilized in other cell-signaling pathways. For instance, some products of the cholesterol synthesis pathway, such as geranylgeranyl pyrophosphate (GGP) and farnesyl pyrophosphate (FPP), are included in the prenylation and subsequent activation of the small GTPase group of signaling molecules including RhoA with its effector Rho kinase [72]. Maher observed that pravastatin and simvastatin decreased the proportion of neutrophils that moved through collagen-coated filters [73].
Statin treatment has been revealed to promote overall longevity, decrease the prevalence of graft vasculopathy and decrease the intensity of cardiac allograft rejection incidents [74, 75]. Furthermore, statin use after lung transplantation is correlated with less acute rejection episodes, reduced bronchoalveolar lavage (BAL) neutrophil numbers and enhanced 6-year survival [76]. Chello et al. also found that atorvastatin greatly decreased expression of neutrophil CD11b and neutrophil-endothelial adhesion in patients before cardiopulmonary bypass (CPB) [77]. Simvastatin has additionally been discovered to weaken fMLP-stimulated IL-8 secretions from neutrophils, in addition to considerably decreasing ROS production [78]. Cerivastatin and pravastatin also appear to restrain neutrophil transendothelial movement [79].
Statins and eosinophils
Statins can influence chemokines, e.g. IL-8, IL-12, IL-17, IL-6, and MCP, and adhesion molecules such as CCR7, CD40, LFA-1, CD83, and CD86, thus interfering with the migration of inflammatory cells from the blood into airways. Because eosinophils and MQs both express LFA-1 molecules, this suggests a possible goal for treatments targeting airway inflammation. Medications besides statins targeted at down-regulation of LFA-1 expression have been useful in reducing airway eosinophil count in murine models of allergic asthma [80], and have decreased sputum eosinophil count following allergen challenge in asthmatics [81]. Statins have an ability to prevent LFA-1/ICAM-1 correlation, like those observed in AIDS [82]. There is potential for an equivalent effect in asthma where the etiology is correlated with eosinophil aggregation. The perception that statins enhance eosinophil apoptosis in individuals [83] suggests an additional curative function. This is likely attributable to the quick decrease of cellular CD40 expression following statin treatment, which completely suppresses eosinophil survival [84].
Statins and macrophages
Statins are typically prescribed long term; it is therefore necessary to realize the impact of persistent statin administration, and how they influence biological features of stem cells. Izadpanah et al. [85] administered MSCs with atorvastatin or pravastatin at clinically appropriate levels and evaluated MSC generation, differentiation possibility, and gene expression profile. Atorvastatin and pravastatin decreased the overall development rate of stem cells. Primarily, statins decreased the potential of stem cells to differentiate into MQs as they showed no direct impact on MQ activity. The conclusions were that MSCs’ insufficient ability to differentiate into MQs may lead to reduced MQ frequency inside the arterial plaque, decreased inflammation, and afterward increased plaque stability. This reveals the non-lipid-related decrease in CVD. In terms of adverse effects, statins reduced stem cells’ osteogenic and chondrogenic differentiation potential and enhanced cell senescence and apoptosis, as shown through p16 (CDKN2A), p53 (TP53) and caspase 3, 8 and 9 upregulation. Statins also downregulate DNA repairing genes, containing X-ray repair cross-complementing protein 4 (XRCC4X), XRCC6, and Apex1. As the impact on MQ differentiation highlights the advantageous side of statins, their influence on other biologic features of stem cells presents an original description of their unfavorable clinical consequences.
Statins and human monocyte-derived DCs
Kwak et al. [86] stated that statins repress MHC expression on human MQs and endothelial cells stimulated by IFN-γ, resulting in a decreased capability of these cells to stimulate T cells. The priming of mice naive T cells with spleen APC in the presence of statins resulted in prevention of Th1 cell differentiation [43]. Moreover, atorvastatin treatment reduced the expression of HLA-DR and CD38 in healthy people [87]. Statins primarily repress the expression of MHC-II antigens on human MQs, endothelial cells, and smooth muscle cells (SMC) excited by IFN-γ [86, 88]. This result was applied by different kinds of statins, lipophilic and hydrophilic, at nanomolar to micromolar levels, but it was restricted to APC cells needing co-stimulation via IFN-γ. Professional APC cells, such as B lymphocytes, and DCs which fundamentally express MHC class II molecules, were not affected.
DCs are disseminated everywhere and demonstrate the specific strength to trigger a basic immune response through naive T cell stimulation [89]. In order to have the capability to activate T cells, DCs are matured by increasing surface MHC class II and co-stimulatory molecule expression. DCs have been observed in atherosclerotic plaques, confirming their involvement in arteriosclerotic vascular disease [90, 91]. Moreover, some atherogenic agents such as LDL, cholesterol [92], LPC [93], nicotine [94], and angiotensin II [95] facilitate DC maturation. Research has also shown that development of DCs in atherosclerotic plaques, specifically in colocalization with T lymphocytes, relates to plaque developments and ischemic syndromes, outlining DCs’ role in plaque instability as a result of triggering inflammation [96]. In the study of Yilmaz et al. some mature DCs and a higher constant plaque morphology were identified in atherosclerotic plaques of cases treated with a prevalent statin (simvastatin or atorvastatin (0.1–1 µM)). For this reason, we presumed that DC movement into atheroma could be decreased via statins [97]. Researchers have revealed that statin treatment reduces DC adhesion and migration across the endothelial monolayer [98]. It has also been demonstrated that abnormal levels of cholesterol and other lipids induce a decline in DC migration from atherosclerotic plaques into environmental lymph nodes, resulting in their local enhancement [99].
Statin effects on the endothelium might be related both to their hypolipidemic effects and or direct effects on endothelial cells. For instance, intracellular signals of Rho-kinases, Rac, and Cdc42, which precipitate prothrombotic and anti-inflammatory activity of endothelial cells, are suppressed by statins (Figure 3) [59]. resulting in reduced oxidative stress and inflammation. Furthermore, statins can remarkably enhance cellular communication network factor 3 (CCN3) expression, prevent expression of pro-inflammatory VCAM-1 cell adhesion molecule, and inhibit monocyte adherence to endothelial cells through the KLF-2 transcription factor pathway, lowering endothelial inflammation [65].
Figure 3.
HMG-CoA reductase pathway; intracellular signals of Rho-kinases, Rac, and Cdc42 are suppressed by statins
Statins and platelets and RBCs
In the study of Xian-Yu et al., patients were administered atorvastatin or simvastatin. Lipids and hematological variables were assessed as well as risk factors for CVD at baseline and 4-week treatment points. The data showed that lipids were modified considerably following 4 weeks’ treatment, mean platelet volume (MPV) dropped dramatically for hematological variables, and the decrease was similar between the two statins. There was no association between MPV and lipid changes [100]. RBC deformation is associated with cell release of ATP [101]. It has been demonstrated that membrane cholesterol changes the features of the cell membrane, e.g. fluidity and bending rigidity [102], and in some CVDs, enhanced membrane cholesterol is found. Therefore, one of the mechanisms contributing to the antithrombotic effects of statins is their induced reduction in the structure of the erythrocyte membrane lipid that enhances RBC deformation and then reduces accumulation of RBC. Xian-Yu reported that MCV discrete degree (SD) became higher following 1 month of statin treatment, 93.1 ±1.42 vs. 93.4 ±2.72 for simvastatin, 93.1 ±1.08 vs. 94.4 ±3.51 for atorvastatin, and substantial variations were observed between before and after atorvastatin treatment. Statins may influence the volume of RBC; however, the extent of this varies between statins. Clapp et al. reported that simvastatin administration to rats or incubation of healthy human RBCs with geranylgeranyl transferase inhibitor-2133 (GGTI-2133) enhanced RBC deformability but diminished low O2 tension-induced ATP release. This suggests that unlike the Rho kinase inhibitor Y-27632, that enhances RBC deformation and raises the release of low O2 tension-induced ATP, simvastatin blocks low O2 tension-induced ATP release through uncoupling RBC deformation and low O2 tension-induced release of ATP. Accordingly, in vivo, simvastatin administration can interfere with the erythrocyte’s strength to cooperate in optimizing blood perfusion distribution to meet O2 tissue needs in the skeletal muscle [103]. In addition, treatment with rosuvastatin dramatically enhanced phosphorylation of NOS, NO-forming dependent on NOS, and deformability of erythrocytes. Rosuvastatin’s stimulating impact on RBC-NOS function was reversed by the NOS inhibitor NG-monomethyl-L-arginine. This NO-dependent impact of rosuvastatin may have a significant effect on the microcirculation and can offer new potential for statin therapy application in the clinic [104].
Conclusions and future perspectives
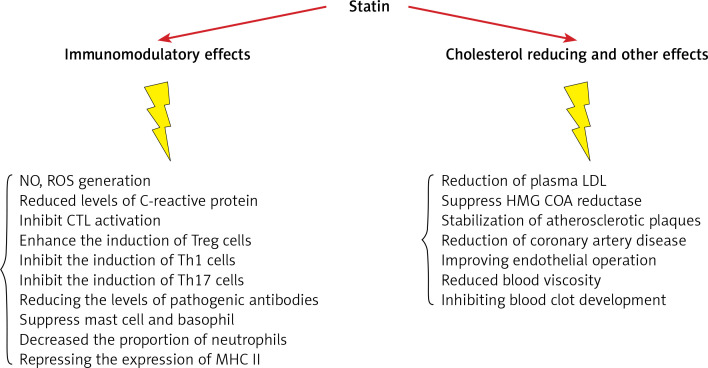
Research to date proves that statins have important anti-inflammatory and immune-modulatory features that may be relevant to their effectiveness in CVD prevention and remedy (Figure 4, Table I) [105–119]. Statins have several effects on the differentiation and function of immune cells. They increase the amount of Treg cells and inhibit Th17, Th1, Th2 and CTL cells. They also have a large effect on various cytokines, such as IL-17, IL-6, IL-4, IL-23, IL-10, IL-21. It has also been proven that statins lead to the suppression of mast cells and basophils and reduce antibody levels. Physicians should be aware that combining statins with other immunomodulatory drugs requires caution as dual therapy may precipitate reactivation of latent infectious diseases and drive tumor progression. Given the proposed wider application of these medicines and their potentially important advantages in treatment of inflammatory and autoimmune disorders, more studies are needed with special focus on the molecular targets of statins included in regulating the immune response. This will allow further conclusions to be met and build an evidence base for wider application of statins in the clinic.
Figure 4.
The figure shows some immune-modulatory and cholesterol reducing effects of statins [32]
Table I.
Evidence on immunomodulatory effect of statins in humans and mice
| Statin | Dose | Experimental model | Possible mechanism | Ref. |
|---|---|---|---|---|
| Simvastatin | In vitro: 2 µM | Mice, Treg/Th17 differentiation | ↑ Differentiation of CD4 into Treg ↓ Differentiation of Th17 ↑ SOCS3 |
[105] |
| Simvastatin | In vitro: 5 µM | Human | ↑ IL-4, IL-5, IL-13 ↓ INF-γ ↓ T-bet expression ↑ GATA 3 and B220 expression |
[106] |
| Simvastatin | In vitro: 10 nM | Human, PBMCs from MS patients and healthy controls | ↓ IL-6 and IL-23 ↑ INF-γ, IL-4, and Il-27 ↓ RORC and IL17 gene expression ↑ SOCS3 |
[107] |
| Simvastatin | 10, 50 mg/kg | Mice, tumor growth of 3LL cell line | ↑ Fox-p3, IDO, IL-10, and TGF-β | [108] |
| Simvastatin | In vitro: 10 mM | Human, PBMC from SCA patients | ↑ Treg cells’ number ↑ Treg cells’ suppressive activity |
[109] |
| Simvastatin | In vitro: 10 mM | Human , monocytes | ↑ SOCS 3 and 7 ↑ INF-γ, IL-4 and IL-27 ↓ JAK-STAT expression ↓ IL-6, IL-23 and IL-17 |
Reference |
| Simvastatin | In vitro: 10 µM | Human, mDC from asthmatic patients | ↓ Th17 cells, ↓ IL-6, ↓ IL-23 ↑ Treg cells ↑ IDO and ↑ IL-10 |
[110] |
| Simvastatin | In vitro: 0.5–2 µM | Mice, Treg differentiation | ↑ Differentiation of Treg ↑ Foxp3 expression ↓ SMAD6 and SMAD7 ↓ Methylation of foxp3 promoter |
[111] |
| Fluvastatin, lovastatin, and simvastatin, | In vitro: all at 10 µM | Mice, T cell | ↑ Kruppel-like factor 2 (KLF2) expression ↓ INF-γ ↓ Differentiation of T-cells |
[49] |
| Rosuvastatin | 5 mg/kg i.v. | Mice, Ischemia-reperfusion injury | ↑ Foxp3 expression | [112] |
| Fluvastatin | 0.1, 1.0, or 10 µM | Human, PBMCs from 7 patients with asthma | ↓ IL-5, IFN-γ, CCL17, and CXCL10 Prevention of Th1 and Th2 cell migration |
[113] |
| Lovastatin | 10 mg/kg i.p. | Mice, DTH (C. albicans) | ↑ Migration of Tregs to the foot-pad ↑ CCl1 and IL-10 |
[114] |
| Lovastatin | 6.25, 12.5, 25 µM | Human | ↑ Bak expression (apoptosis regulators) ↓ Bcl-XL expression activation of caspase-3/8/9 ↓ Collagen and platelet aggregation |
[115] |
| Lovastatin | 0.5–25 mM | Human, PBMC from patients with CIU | ↓ T-cell proliferation ↓ IL-10 and IL-17 ↔ Neither Socs3 nor RORc |
[116] |
| Atorvastatin | 10 mg/kg | Mice, experimental autoimmune glomerulonephritis | ↑ IL-10, ↓ IL-17, IFN-γ ↓ TNF-γ IL-21 Treg |
[117] |
| Atorvastatin | 20 mg/kg | Human, twenty-seven healthy volunteers | ↓ HLA-DR and CD38 expression ↑ Superantigen-mediated T cell activation |
|
| Atorvastatin | In vitro: 10 mM | Human endothelial cell culture | ↓ Expression of CD40 | [64] |
| Atorvastatin | 10 mg/kg/day | Mice with EAE, control mice | ↑ Th2 cytokine secretion ↓ Th1 cytokine secretion |
[118] |
| Atorvastatin | In vitro: 10 mM | Mice, experimental autoimmune myasthenia gravis | ↑ Foxp3 expression, ↑ Treg number ↓ Lymphocyte proliferation ↓ Th1/Th17, ↑ Th2 |
[67] |
| Atorvastatin | In vitro: 5–10 mM | Human, PBMC culture | ↑ Treg cells’ number ↑ Suppressive function of Tregs |
[119] |
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Endo A. The discovery and development of HMG-CoA reductase inhibitors. J Lipid Res 1992; 33: 1569-82. [PubMed] [Google Scholar]
- 2.Ruscica M, Ferri N, Santos RD, Sirtori CR, Corsini A. Lipid lowering drugs: present status and future developments. Curr Atheroscler Rep 2021; 23: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sahebkar A, Watts GF. New therapies targeting apoB metabolism for high-risk patients with inherited dyslipidaemias: what can the clinician expect? Cardiovasc Drugs Ther 2013; 27: 559-67. [DOI] [PubMed] [Google Scholar]
- 4.Sahebkar A, Watts GF. New LDL-cholesterol lowering therapies: pharmacology, clinical trials, and relevance to acute coronary syndromes. Clin Ther 2013; 35: 1082-98. [DOI] [PubMed] [Google Scholar]
- 5.Banach M, Reiner Z, Cicero AFG, et al. 2022: the year in cardiovascular disease – the year of upfront lipid lowering combination therapy. Arch Med Sci 2022; 18: 1429-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maron DJ, Fazio S, Linton MF. Current perspectives on statins. Circulation 2000; 101: 207-13. [DOI] [PubMed] [Google Scholar]
- 7.Pedersen TR. Statin trials and goals of cholesterol-lowering therapy after AMI. Am Heart J 1999; 138: S177-S82. [DOI] [PubMed] [Google Scholar]
- 8.Vaughan CJ, Gotto AM, Basson CT. The evolving role of statins in the management of atherosclerosis. J Am Coll Cardiol 2000; 35: 1-10. [DOI] [PubMed] [Google Scholar]
- 9.Amin F, Fathi F, Reiner Ž, Banach M, Sahebkar A. The role of statins in lung cancer. Arch Med Sci 2022; 18: 141-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bahrami A, Parsamanesh N, Atkin SL, Banach M, Sahebkar A. Effect of statins on toll-like receptors: a new insight to pleiotropic effects. Pharmacol Res 2018; 135: 230-8. [DOI] [PubMed] [Google Scholar]
- 11.Khalifeh M, Penson PE, Banach M, Sahebkar A. Statins as anti-pyroptotic agents. Arch Med Sci 2021; 17: 1414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sohrevardi SM, Nasab FS, Mirjalili MR, et al. Effect of atorvastatin on delirium status of patients in the intensive care unit: a randomized controlled trial. Arch Med Sci 2021; 17: 1423-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vahedian-Azimi A, Mohammadi SM, Beni FH, et al. Improved COVID-19 ICU admission and mortality outcomes following treatment with statins: a systematic review and meta-analysis. Arch Med Sci 2021; 17: 579-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahrami A, Bo S, Jamialahmadi T, Sahebkar A. Effects of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors on ageing: Molecular mechanisms. Ageing Res Rev 2020; 58: 101024. [DOI] [PubMed] [Google Scholar]
- 15.Kouhpeikar H, Delbari Z, Sathyapalan T, Simental-Mendía LE, Jamialahmadi T, Sahebkar A. The effect of statins through mast cells in the pathophysiology of atherosclerosis: a review. Current Atheroscler Rep 2020; 22: 19. [DOI] [PubMed] [Google Scholar]
- 16.Koushki K, Shahbaz SK, Mashayekhi K, et al. Anti-inflammatory action of statins in cardiovascular disease: the role of inflammasome and toll-like receptor pathways. Clin Rev Allergy Immunol 2021; 60: 175-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parizadeh SMR, Azarpazhooh MR, Moohebati M, et al. Simvastatin therapy reduces prooxidant-antioxidant balance: results of a placebo-controlled cross-over trial. Lipids 2011; 46: 333-40. [DOI] [PubMed] [Google Scholar]
- 18.Sahebkar A, Chew GT, Watts GF. Recent advances in pharmacotherapy for hypertriglyceridemia. Progress Lipid Res 2014; 56: 47-66. [DOI] [PubMed] [Google Scholar]
- 19.Sahebkar A, Kotani K, Serban C, et al. Statin therapy reduces plasma endothelin-1 concentrations: a meta-analysis of 15 randomized controlled trials. Atherosclerosis 2015; 241: 433-42. [DOI] [PubMed] [Google Scholar]
- 20.Sahebkar A, Serban C, Mikhailidis DP, et al. Association between statin use and plasma d-dimer levels: a systematic review and meta-analysis of randomised controlled trials. Thromb Haemost 2015; 114: 546-57. [DOI] [PubMed] [Google Scholar]
- 21.Vahedian-Azimi A, Mannarino MR, Shojaie S, et al. The effect of statins on the prevalence and mortality of influenza virus infection: a systematic review and meta-analysis. Arch Med Sci 2022; 18: 1513-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Serban C, Sahebkar A, Ursoniu S, et al. A systematic review and meta-analysis of the effect of statins on plasma asymmetric dimethylarginine concentrations. Sci Rep 2015; 5: 9902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Furberg CD. Natural statins and stroke risk. Circulation 1999; 99: 185-8. [DOI] [PubMed] [Google Scholar]
- 24.Kones R. Rosuvastatin, inflammation, C-reactive protein, JUPITER, and primary prevention of cardiovascular disease–a perspective. Drug Des devel Ther 2010; 4: 383-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferdinand KC. Are cardiovascular benefits in statin lipid effects dependent on baseline lipid levels. Curr Atheroscler Rep 2011; 13: 64-72. [DOI] [PubMed] [Google Scholar]
- 26.Devaraj S, Siegel D, Jialal I. Statin therapy in metabolic syndrome and hypertension post-JUPITER: what is the value of CRP? Curr Atheroscler Rep 2011; 13: 31-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamann PD, Cooper RG, McHugh NJ, Chinoy H. Statin-induced necrotizing myositis–a discrete autoimmune entity within the “statin-induced myopathy spectrum”. Autoimmun Rev 2013; 12: 1177-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murinson BB, Haughey NJ, Maragakis N. Selected statins produce rapid spinal motor neuron loss in vitro. BMC Musculoskelet Disord 2012; 13: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sattar N, Preiss D, Murray HM, et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 2010; 375: 735-42. [DOI] [PubMed] [Google Scholar]
- 30.Davidson MH. Rosuvastatin: a highly efficacious statin for the treatment of dyslipidaemia. Exp Opin Investig Drugs 2002; 11: 125-41. [DOI] [PubMed] [Google Scholar]
- 31.Endo A. The discovery and development of HMG-CoA reductase inhibitors. J Lipid Res 1992; 33: 1569-82. [PubMed] [Google Scholar]
- 32.Schachter M. Chemical, pharmacokinetic and pharmacodynamic properties of statins: an update. Fundamental Clin Pharmacol 2005; 19: 117-25. [DOI] [PubMed] [Google Scholar]
- 33.Slack JMW. Metaplasia and transdifferentiation: from pure biology to the clinic. Nat Rev Mol Cell Biol 2007; 8: 369-78. [DOI] [PubMed] [Google Scholar]
- 34.Pradeu T. Regenerating theories in developmental biology. In: Towards a Theory of Development. Minelli A, Pradeu T (eds.). Oxford Academic; 2014: 15-32. [Google Scholar]
- 35.Okita K, Yamanaka S. Induced pluripotent stem cells: opportunities and challenges. Philos Trans R Soc Lond B Biol Sci 2011; 366: 2198-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alt E, Pinkernell K, Scharlau M, et al. Effect of freshly isolated autologous tissue resident stromal cells on cardiac function and perfusion following acute myocardial infarction. Int J Cardiol 2010; 144: 26-35. [DOI] [PubMed] [Google Scholar]
- 37.Sharpless NE, DePinho RA. Telomeres, stem cells, senescence, and cancer. J Clin Investig 2004; 113: 160-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Traktuev DO, Merfeld-Clauss S, Li J, et al. A population of multipotent CD34-positive adipose stromal cells share pericyte and mesenchymal surface markers, reside in a periendothelial location, and stabilize endothelial networks. Circ Res 2008; 102: 77-85. [DOI] [PubMed] [Google Scholar]
- 39.Izadpanah R, Schachtele DJ, Pfnur AB, et al. The impact of statins on biological characteristics of stem cells provides a novel explanation for their pleiotropic beneficial and adverse clinical effects. Am J Physiol Cell Physiol 2015; 309: C522-31. [DOI] [PubMed] [Google Scholar]
- 40.Weitz-Schmidt G, Welzenbach K, Brinkmann V, et al. Statins selectively inhibit leukocyte function antigen-1 by binding to a novel regulatory integrin site. Nat Med 2001; 7: 687-92. [DOI] [PubMed] [Google Scholar]
- 41.Ghittoni R, Patrussi L, Pirozzi K, et al. Simvastatin inhibits T-cell activation by selectively impairing the function of Ras superfamily GTPases. FASEB J 2005; 19: 605-7. [DOI] [PubMed] [Google Scholar]
- 42.Brinkkoetter PT, Gottmann U, Schulte J, van der Woude FJ, Braun C, Yard BA. Atorvastatin interferes with activation of human CD4(+) T cells via inhibition of small guanosine triphosphatase (GTPase) activity and caspase-independent apoptosis. Clin Exp Immunol 2006; 146: 524-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sato K, Nuki T, Gomita K, Weyand CM, Hagiwara N. Statins reduce endothelial cell apoptosis via inhibition of TRAIL expression on activated CD4 T cells in acute coronary syndrome. Atherosclerosis 2010; 213: 33-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dunn SE, Youssef S, Goldstein MJ, et al. Isoprenoids determine Th1/Th2 fate in pathogenic T cells, providing a mechanism of modulation of autoimmunity by atorvastatin. J Exp Med 2006; 203: 401-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arora M, Chen L, Paglia M, et al. Simvastatin promotes Th2-type responses through the induction of the chitinase family member Ym1 in dendritic cells. Proc Natl Acad Sci USA 2006; 103: 7777-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yilmaz A, Reiss C, Tantawi O, et al. HMG-CoA reductase inhibitors suppress maturation of human dendritic cells: new implications for atherosclerosis. Atherosclerosis 2004; 172: 85-93. [DOI] [PubMed] [Google Scholar]
- 47.Hillyard DZ, Cameron AJ, McIntyre AH, et al. Inhibition of proliferation and signalling mechanisms in human lymphocytes by fluvastatin. Clin Exp Pharmacol Physiol 2002; 29: 673-8. [DOI] [PubMed] [Google Scholar]
- 48.Blank N, Schiller M, Krienke S, et al. Atorvastatin inhibits T cell activation through 3-hydroxy-3-methylglutaryl coenzyme A reductase without decreasing cholesterol synthesis. J Immunol 2007; 179: 3613-21. [DOI] [PubMed] [Google Scholar]
- 49.Bu DX, Tarrio M, Grabie N, et al. Statin-induced Krüppel-like factor 2 expression in human and mouse T cells reduces inflammatory and pathogenic responses. J Clin Investig 2010; 120: 1961-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghittoni R, Napolitani G, Benati D, et al. Simvastatin inhibits the MHC class II pathway of antigen presentation by impairing Ras superfamily GTPases. Eur J Immunol 2006; 36: 2885-93. [DOI] [PubMed] [Google Scholar]
- 51.Kerksiek KM, Niedergang F, Chavrier P, Busch DH, Brocker TJB. Selective Rac1 inhibition in dendritic cells diminishes apoptotic cell uptake and cross-presentation in vivo. Blood 2005; 105: 742-9. [DOI] [PubMed] [Google Scholar]
- 52.Shurin GV, Tourkova IL, Chatta GS, et al. Small rho GTPases regulate antigen presentation in dendritic cells. J Immunol 2005; 174: 3394-400. [DOI] [PubMed] [Google Scholar]
- 53.Burgdorf S, Kautz A, Böhnert V, Knolle PA, Kurts CJs. Distinct pathways of antigen uptake and intracellular routing in CD4 and CD8 T cell activation. Science 2007; 316: 612-6. [DOI] [PubMed] [Google Scholar]
- 54.Ulivieri C, Fanigliulo D, Benati D, Laghi Pasini F, Baldari C. Simvastatin impairs humoral and cell-mediated immunity in mice by inhibiting lymphocyte homing, T-cell activation and antigen cross-presentation. Eur J Immunol 2008; 38: 2832-44. [DOI] [PubMed] [Google Scholar]
- 55.Sallusto F, Cella M, Danieli C, Lanzavecchia A. Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: downregulation by cytokines and bacterial products. J Exp Med 1995; 182: 389-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guermonprez P, Valladeau J, Zitvogel L, Théry C, Amigorena S. Antigen presentation and T cell stimulation by dendritic cells. Annu Rev Immunol 2002; 20: 621-67. [DOI] [PubMed] [Google Scholar]
- 57.Geissler I, Collins L, Schofield R, Fabre JW. In vivo suppression of major histocompatibility complex class II expression on porcine vascular endothelial cells by an HMG-CoA reductase inhibitor. Transplantation 2006; 81: 922-6. [DOI] [PubMed] [Google Scholar]
- 58.Yamakuchi M, Greer JJ, Cameron SJ, et al. HMG-CoA reductase inhibitors inhibit endothelial exocytosis and decrease myocardial infarct size. Circ Res 2005; 96: 1185-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou Q, Liao JK. Pleiotropic effects of statins: basic research and clinical perspectives. Circ J 2010; 74: 818-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lin Z, Natesan V, Shi H, et al. A novel role of CCN3 in regulating endothelial inflammation. J Cell Commun Signaling 2010; 4: 141-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Antonopoulos AS, Margaritis M, Lee R, Channon K, Antoniades C. Statins as anti-inflammatory agents in atherogenesis: molecular mechanisms and lessons from the recent clinical trials. Curr Pharm Design 2012; 18: 1519-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Josefowicz SZ, Lu LF, Rudensky AY. Regulatory T cells: mechanisms of differentiation and function. Annu Rev Immunol 2012; 30: 531-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Trinchieri G. Proinflammatory and immunoregulatory functions of interleukin-12. Int Rev Immunol 1998; 16: 365-96. [DOI] [PubMed] [Google Scholar]
- 64.Wagner AH, Gebauer M, Guldenzoph B, Hecker M. 3-hydroxy-3-methylglutaryl coenzyme A reductase-independent inhibition of CD40 expression by atorvastatin in human endothelial cells. Arteriosclerosis Thromb Vasc Biol 2002; 22: 1784-9. [DOI] [PubMed] [Google Scholar]
- 65.Forero-Pena DA, Gutierrez FRS. Statins as modulators of regulatory T-cell biology. Mediators Inflamm 2013; 2013: 167086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li XL, Dou YC, Liu Y, et al. Atorvastatin ameliorates experimental autoimmune neuritis by decreased Th1/Th17 cytokines and up-regulated T regulatory cells. Cell Immunol 2011; 271: 455-61. [DOI] [PubMed] [Google Scholar]
- 67.Li XL, Liu Y, Cao LL, et al. Atorvastatin-modified dendritic cells in vitro ameliorate experimental autoimmune myasthenia gravis by up-regulated Treg cells and shifted Th1/Th17 to Th2 cytokines. Mol Cell Neurosci 2013; 56: 85-95. [DOI] [PubMed] [Google Scholar]
- 68.Li XL, Li H, Zhang M, et al. Exosomes derived from atorvastatin-modified bone marrow dendritic cells ameliorate experimental autoimmune myasthenia gravis by up-regulated levels of IDO/Treg and partly dependent on FasL/Fas pathway. J Neuroinflammation 2016; 13: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kolawole EM, McLeod JJ, Ndaw V, et al. Fluvastatin suppresses mast cell and basophil IgE responses: genotype-dependent effects. J Immunol 2016; 196: 1461-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kougias P, Chai H, Lin PH, Yao Q, Lumsden AB, Chen C. Defensins and cathelicidins: neutrophil peptides with roles in inflammation, hyperlipidemia and atherosclerosis. J Cell Mol Med 2005; 9: 3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dunzendorfer S, Rothbucher D, Schratzberger P, Reinisch N, Kahler CM, Wiedermann CJ. Mevalonate-dependent inhibition of transendothelial migration and chemotaxis of human peripheral blood neutrophils by pravastatin. Circ Res 1997; 81: 963-9. [DOI] [PubMed] [Google Scholar]
- 72.Alblas J, Ulfman L, Hordijk P, Koenderman L. Activation of Rhoa and ROCK are essential for detachment of migrating leukocytes. Mol Biol Cell 2001; 12: 2137-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Maher BM, Dhonnchu TN, Burke JP, Soo A, Wood AE, Watson RW. Statins alter neutrophil migration by modulating cellular Rho activity--a potential mechanism for statins-mediated pleotropic effects? J Leukocyte Biol 2009; 85: 186-93. [DOI] [PubMed] [Google Scholar]
- 74.Kobashigawa JA, Katznelson S, Laks H, et al. Effect of pravastatin on outcomes after cardiac transplantation. N Engl J Med 1995; 333: 621-7. [DOI] [PubMed] [Google Scholar]
- 75.Wenke K, Meiser B, Thiery J, et al. Simvastatin initiated early after heart transplantation: 8-year prospective experience. Circulation 2003; 107: 93-7. [DOI] [PubMed] [Google Scholar]
- 76.Johnson BA, Iacono AT, Zeevi A, McCurry KR, Duncan SR. Statin use is associated with improved function and survival of lung allografts. Am J Respir Citi Care Med 2003; 167: 1271-8. [DOI] [PubMed] [Google Scholar]
- 77.Chello M, Patti G, Candura D, et al. Effects of atorvastatin on systemic inflammatory response after coronary bypass surgery. Crit Care Med 2006; 34: 660-7. [DOI] [PubMed] [Google Scholar]
- 78.Marino F, Maresca AM, Castiglioni L, et al. Simvastatin down-regulates the production of interleukin-8 by neutrophil leukocytes from dyslipidemic patients. BMC Cardiovasc Disord 2014; 14: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kaneider NC, Reinisch CM, Dunzendorfer S, Meierhofer C, Djanani A, Wiedermann CJ. Induction of apoptosis and inhibition of migration of inflammatory and vascular wall cells by cerivastatin. Atherosclerosis 2001; 158: 23-33. [DOI] [PubMed] [Google Scholar]
- 80.Winn M, Reilly EB, Liu G, et al. Discovery of novel p-arylthio cinnamides as antagonists of leukocyte function-associated antigen-1/intercellular adhesion molecule-1 interaction. 4. Structure-activity relationship of substituents on the benzene ring of the cinnamide. J Med Chem 2001; 44: 4393-403. [DOI] [PubMed] [Google Scholar]
- 81.Gauvreau GM, Becker AB, Boulet LP, et al. The effects of an anti-CD11a mAb, efalizumab, on allergen-induced airway responses and airway inflammation in subjects with atopic asthma. J Allergy Clin Immunol 2003; 112: 331-8. [DOI] [PubMed] [Google Scholar]
- 82.Giguere JF, Tremblay MJ. Statin compounds reduce human immunodeficiency virus type 1 replication by preventing the interaction between virion-associated host intercellular adhesion molecule 1 and its natural cell surface ligand LFA-1. J Virol 2004; 78: 12062-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Luo FJC. Simvastatin induces eosinophil apoptosis in vitro. Chest 2004; 126: 721S. [PubMed] [Google Scholar]
- 84.Bureau F, Seumois G, Jaspar F, et al. CD40 engagement enhances eosinophil survival through induction of cellular inhibitor of apoptosis protein 2 expression: possible involvement in allergic inflammation. J Allergy Clin Immunol 2002; 110: 443-9. [DOI] [PubMed] [Google Scholar]
- 85.Izadpanah R, Schächtele DJ, Pfnür AB, et al. The impact of statins on biological characteristics of stem cells provides a novel explanation for their pleiotropic beneficial and adverse clinical effects. Am J Physiol cell Physiol 2015; 309: C522-31. [DOI] [PubMed] [Google Scholar]
- 86.Kwak B, Mulhaupt F, Myit S, Mach F. Statins as a newly recognized type of immunomodulator. Nat Med 2000; 6: 1399-402. [DOI] [PubMed] [Google Scholar]
- 87.Fehr T, Kahlert C, Fierz W, et al. Statin-induced immunomodulatory effects on human T cells in vivo. Atherosclerosis 2004; 175: 83-90. [DOI] [PubMed] [Google Scholar]
- 88.Palinski W. Immunomodulation: a new role for statins? Nat Med 2000; 6: 1311-2. [DOI] [PubMed] [Google Scholar]
- 89.Banchereau J, Briere F, Caux C, et al. Immunobiology of dendritic cells. Annu Rev Immunol 2000; 18: 767-811. [DOI] [PubMed] [Google Scholar]
- 90.Bobryshev YV, Lord RS. Ultrastructural recognition of cells with dendritic cell morphology in human aortic intima. Contacting interactions of Vascular Dendritic Cells in athero-resistant and athero-prone areas of the normal aorta. Arch Histol Cytol 1995; 58: 307-22. [DOI] [PubMed] [Google Scholar]
- 91.Bobryshev YV, Lord RS. S-100 positive cells in human arterial intima and in atherosclerotic lesions. Cardiovasc Res 1995; 29: 689-96. [PubMed] [Google Scholar]
- 92.Alderman CJ, Bunyard PR, Chain BM, Foreman JC, Leake DS, Katz DR. Effects of oxidised low density lipoprotein on dendritic cells: a possible immunoregulatory component of the atherogenic micro-environment? Cardiovasc Res 2002; 55: 806-19. [DOI] [PubMed] [Google Scholar]
- 93.Coutant F, Agaugue S, Perrin-Cocon L, Andre P, Lotteau V. Sensing environmental lipids by dendritic cell modulates its function. J Immunol 2004; 172: 54-60. [DOI] [PubMed] [Google Scholar]
- 94.Aicher A, Heeschen C, Mohaupt M, Cooke JP, Zeiher AM, Dimmeler S. Nicotine strongly activates dendritic cell-mediated adaptive immunity: potential role for progression of atherosclerotic lesions. Circulation 2003; 107: 604-11. [DOI] [PubMed] [Google Scholar]
- 95.Nahmod KA, Vermeulen ME, Raiden S, et al. Control of dendritic cell differentiation by angiotensin II. FASEB J 2003; 17: 491-3. [DOI] [PubMed] [Google Scholar]
- 96.Sun L, Zhang W, Zhao Y, et al. Dendritic cells and T cells, partners in atherogenesis and the translating road ahead. Front Immunol 2020; 11: 1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yilmaz A, Reiss C, Weng A, et al. Differential effects of statins on relevant functions of human monocyte-derived dendritic cells. J Leukocyte Biol 2006; 79: 529-38. [DOI] [PubMed] [Google Scholar]
- 98.Weis M, Schlichting CL, Engleman EG, Cooke JP. Endothelial determinants of dendritic cell adhesion and migration: new implications for vascular diseases. Arterioscler Thromb Vasc Biol 2002; 22: 1817-23. [DOI] [PubMed] [Google Scholar]
- 99.Angeli V, Llodra J, Rong JX, et al. Dyslipidemia associated with atherosclerotic disease systemically alters dendritic cell mobilization. Immunity 2004; 21: 561-74. [DOI] [PubMed] [Google Scholar]
- 100.Xian-Yu JB, Feng JF, Chen YC, Yang YW. Effects of simvastatin and atorvastatin on biochemical and hematological markers in patients with risk of cardiovascular diseases. Int J Clin Exp Med 2015; 8: 13983-9. [PMC free article] [PubMed] [Google Scholar]
- 101.Wan J, Forsyth AM, Stone HA. Red blood cell dynamics: from cell deformation to ATP release. Integr Biol 2011; 3: 972-81. [DOI] [PubMed] [Google Scholar]
- 102.Forsyth AM, Braunmuller S, Wan J, Franke T, Stone HA. The effects of membrane cholesterol and simvastatin on red blood cell deformability and ATP release. Microvasc Res 2012; 83: 347-51. [DOI] [PubMed] [Google Scholar]
- 103.Clapp KM, Ellsworth ML, Sprague RS, Stephenson AH. Simvastatin and GGTI-2133, a geranylgeranyl transferase inhibitor, increase erythrocyte deformability but reduce low O(2) tension-induced ATP release. Am J Physiol Heart Circ Physiol 2013; 304: H660-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ludolph B, Bloch W, Kelm M, Schulz R, Kleinbongard P. Short-term effect of the HMG-CoA reductase inhibitor rosuvastatin on erythrocyte nitric oxide synthase activity. Vasc Health Risk Manag 2007; 3: 1069-73. [PMC free article] [PubMed] [Google Scholar]
- 105.Kagami S, Owada T, Kanari H, et al. Protein geranylgeranylation regulates the balance between Th17 cells and Foxp3+ regulatory T cells. Int Immunol 2009; 21: 679-89. [DOI] [PubMed] [Google Scholar]
- 106.Arora M, Chen L, Paglia M, et al. Simvastatin promotes Th2-type responses through the induction of the chitinase family member Ym1 in dendritic cells. Proc Natl Acad Sci USA 2006; 103: 7777-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang X, Jin J, Peng X, Ramgolam VS, Markovic-Plese S. Simvastatin inhibits IL-17 secretion by targeting multiple IL-17-regulatory cytokines and by inhibiting the expression of IL-17 transcription factor RORC in CD4+ lymphocytes. J Immunol 2008; 180: 6988-96. [DOI] [PubMed] [Google Scholar]
- 108.Lee KJ, Moon JY, Choi HK, et al. Immune regulatory effects of simvastatin on regulatory T cell-mediated tumour immune tolerance. Clin Exp Immunol 2010; 161: 298-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Meng X, Zhang K, Li J, et al. Statins induce the accumulation of regulatory T cells in atherosclerotic plaque. Mol Med 2012; 18: 598-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Maneechotesuwan K, Kasetsinsombat K, Wamanuttajinda V, Wongkajornsilp A, Barnes PJ. Statins enhance the effects of corticosteroids on the balance between regulatory T cells and Th17 cells. Clin Exp Allergy 2013; 43: 212-22. [DOI] [PubMed] [Google Scholar]
- 111.Kim YC, Kim KK, Shevach EM. Simvastatin induces Foxp3+ T regulatory cells by modulation of transforming growth factor-beta signal transduction. Immunology 2010; 130: 484-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ke D, Fang J, Fan L, Chen Z, Chen L. Regulatory T cells contribute to rosuvastatin-induced cardioprotection against ischemia-reperfusion injury. Coronary Artery Dis 2013; 24: 334-41. [DOI] [PubMed] [Google Scholar]
- 113.Samson KT, Minoguchi K, Tanaka A, et al. Inhibitory effects of fluvastatin on cytokine and chemokine production by peripheral blood mononuclear cells in patients with allergic asthma. Clin Exp Allergy 2006; 36: 475-82. [DOI] [PubMed] [Google Scholar]
- 114.Mira E, Leon B, Barber DF, et al. Statins induce regulatory T cell recruitment via a CCL1 dependent pathway. J Immunol 2008; 181: 3524-34. [DOI] [PubMed] [Google Scholar]
- 115.Zhao Q, Li M, Chen M, et al. Lovastatin induces platelet apoptosis. Environm Toxicol Pharmacol 2016; 42: 69-75. [DOI] [PubMed] [Google Scholar]
- 116.Azor MH, dos Santos JC, Futata EA, et al. Statin effects on regulatory and proinflammatory factors in chronic idiopathic urticaria. Clin Exp Immunol 2011; 166: 291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Eller P, Eller K, Wolf AM, et al. Atorvastatin attenuates murine anti-glomerular basement membrane glomerulonephritis. Kidney Intern 2010; 77: 428-35. [DOI] [PubMed] [Google Scholar]
- 118.Stüve O, Youssef S, Weber MS, et al. Immunomodulatory synergy by combination of atorvastatin and glatiramer acetate in treatment of CNS autoimmunity. J Clin Investig 2006; 116: 1037-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mausner-Fainberg K, Luboshits G, Mor A, et al. The effect of HMG-CoA reductase inhibitors on naturally occurring CD4+CD25+ T cells. Atherosclerosis 2008; 197: 829-39. [DOI] [PubMed] [Google Scholar]