Abstract
The extracellular matrix (ECM) is a crucial component of the stem cell microenvironment, or stem-cell niches, and contributes to the regulation of cell behavior and fate. Accumulating evidence indicates that different types of stem cells possess a large variety of molecules responsible for interactions with the ECM, mediating specific epigenetic rearrangements and corresponding changes in transcriptome profile. Signals from the ECM are crucial at all stages of ontogenesis, including embryonic and postnatal development, as well as tissue renewal and repair. The ECM could regulate stem cell transition from a quiescent state to readiness to perceive the signals of differentiation induction (competence) and the transition between different stages of differentiation (commitment). Currently, to unveil the complex networks of cellular signaling from the ECM, multiple approaches including screening methods, the analysis of the cell matrixome, and the creation of predictive networks of protein–protein interactions based on experimental data are used. In this review, we consider the existing evidence regarded the contribution of ECM-induced intracellular signaling pathways into the regulation of stem cell differentiation focusing on mesenchymal stem/stromal cells (MSCs) as well-studied type of postnatal stem cells totally depended on signals from ECM. Furthermore, we propose a system biology-based approach for the prediction of ECM-mediated signal transduction pathways in target cells.
Video Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s12964-023-01252-8.
Keywords: Mesenchymal stem/stromal cells, Signaling pathways, Extracellular matrix, System biology
Introduction
Tissue structure homeostasis, function, and renewal depend on cellular composition. Generally, terminally differentiated cells define the structure and normal function of tissue and organs, while the adult stem and progenitor cells determine renewal and regeneration potential [1–3]. Stem cell stability is based on the sustainable work of cell signaling pathways, which is controlled by intracellular (non-coding RNAs and transcription factors) and extracellular (growth factors, morphogens, environmental cues) factors [4, 5]. Changes to microenvironment conditions cause the transition of stem cells from a quiescent to an activated state, which initiates proliferation and differentiation [6, 7]. The combination of external microenvironmental factors that support the functioning of stem cells has been labelled a “stem cell niche” [8]. An integral component of the niche is the extracellular matrix (ECM), which provides most of the clues from the microenvironment, i.e., physical characteristics, the conduction of specific signals from structural components, and the anchorage of components to the ECM, e.g., soluble factors (growth factors and morphogens) and matrix-bound vesicles [9]. Thus, the ECM stimulates various intracellular signaling cascades required to maintain the homeostasis of stem cell niches [10]. Herefore, interpreting the research results obtained from cells isolated from their microenvironmental context is complex.
Stem cell niches contain cells that regulate the maintenance of stem cells homeostasis and fate through the secretion of various niche components. Almost in all tissues and organs mesenchymal stem/stromal cells (MSC) play this role being the critical regulators of stem cell niche functioning [11–15]. MSC can secrete a variety of niche ECM components, paracrine factors, and bioactive molecules within extracellular vesicles in response to changes in the microenvironment (e.g., injury). In addition, under activating stimuli, multipotent stem cell subpopulation of MSC is capable of self-renewal of their own pool as well as differentiation, leading to modification of the microenvironment by replenishing deficient components or recruiting other supporting cells to the niche [16, 17]. According to one of the minimal criteria to define multipotent MSC are capable of adipogenic, chondrogenic and osteogenic differentiation in vitro [17]. Until recently, scientists used the term "mesenchymal stem cells" to discuss these cells, but it was considered incorrect due to the collected data proving that the main physiological function of MSC is not exclusively the presence of stem cells [18]. Therefore, the current recommended name is “mesenchymal stromal cells”, and the presence of multipotent stem cells in MSCs should be carefully evaluated using appropriate tests [17]. Nonetheless, all MSC are heavily reliant on the ECM clues, so we focus on these cells to analyze the diversity of ECM-induced signal pathways in postnatal stem cells.
The interaction of cells with the microenvironment, in particular with the components of the ECM, is mediated by specific receptors, leading to the activation of various signaling cascades within the cell and, as a consequence, to changes in its behavior. Looking at the identification of the main receptors and participants in ECM signaling cascades from a historical point of view can help to summarize the knowledge on this issue in the field of matrix biology (Table 1). Even though many receptors and key participants of their signaling cascades have been known for a long time, there are many gaps among the other participants of these cascades, as well as in the case of changing microenvironment and the nature of their network interactions, and for a specific type of cell. This tendency highlights the importance of the analytical reviews covering the mechanisms of ECM-mediated regulation of cell function, here in particular the stem cell differentiation. In parallel with investigation of the ECM, the signaling cascades of postnatal stem cells remain an important issue for cell and matrix biology and regenerative medicine. In this review, we focus on analyzing the data obtained from MSC in vitro and in vivo for a better understanding of the regeneration processes relevant to native postnatal stem cells. Accumulating ECM signaling observations, we suggest a system biology-based approach for examining the predicted networks of such signal transduction pathways on the example of DDR1-initiated signaling in MSC.
Table 1.
General discovery dates for ECM signaling molecules
| Time of discovery | Discovered phenomena | References |
|---|---|---|
| 1942 | The discovery of glycosphingolipids was by the German scientist Ernst Klenk after their isolation from brain tissue | [19] |
| 1980 | CD44 was first described as a surface molecule of lymphocytes, platelets, and granulocytes. Currently, it is a receptor primarily for hyaluronic acid, but also for lipoproteins and proteoglycans of the ECM, growth factors, cytokines, and matrix metalloproteinases (MMP) | [20, 21] |
| 1983, 1989 | Syndecans were first identified in 1983; a few years later they were named using the Greek term syndein, meaning “to bind together”, which emphasized their importance for cellular adhesion to the ECM | [22, 23] |
| 1985, 1993, 1997 | The receptor discoidin-1, a lectin, involved in the adhesion, aggregation, and tightly regulated migration of cellular slime mold (Dictyostelium discoideum) was discovered. Subsequently, receptor tyrosine kinases with a domain to discoidin homologous were discovered. Investigation of these proteins resulted in the discovery of discoidin domain receptor tyrosine kinase 1 and 2 (DDR1, DDR2) | [24–27] |
| 1985 | Transient receptor potential (TRP) channels were found first in Drosophila as rhodopsin-triggered phospholipase C (PLC). Later, TRP channels were found in fungi and animals, where they act as mechanosensitive ion channels | [28–30] |
| 1986 | Integrins, major receptors that interact with the ECM, were discovered. They were named to represent their participation in the transmembrane glycoprotein complex, that provides conjunction between ECM and the cell actin cytoskeleton | [31] |
| 1989, 1990, 1992 | Paxillin, a phosphotyrosine-containing protein, was identified. Furthermore, its role in cell adhesion to the ECM proteins was studied in detail | [32–34] |
| 1996, 2009 | Integrin-linked kinase (ILK) was observed as a protein that associates with cytoplasmic tail integrin β1 subunits. However, it was later determined that ILK has a pseudoactive kinase domain and forms the center of protein–protein interactions | [35, 36] |
| 1999 | Since its discovery, talin has been considered the only mediator of integrin activation | [37] |
| 2000, 2004, 2009 | Subsequently, it was found to be essential for integrin activation and signal transduction of kindlins | [38–40] |
| 2010 | Other mechanosensitive ion channels, e.g., Piezo, was described in 2010. Their activation under mechanical forces was reported for several cell types | [41, 42] |
ECM receptor signaling pathways during MSC differentiation
Many ECM components were found in stem-cell niches, including collagens, laminins, fibronectin, and proteoglycans [43], and also paracrine factors affecting the interaction of stem cells with the ECM [44]. The ECM supports the appropriate position of cells within their microenvironment and regulates such properties as proliferation, polarization, migration, and differentiation [45]. Several studies have demonstrated that the ECM directs the differentiation of stem cells into specialized cells of the organ from which it was isolated. This data confirms that the ECM has tissue specificity for maintaining a certain niche [46].
It is presumed that the tissue specificity of the ECM is provided due to differences in the cellular composition of tissue types. Nevertheless, it is known that cells with similar phenotypes and functions isolated from different tissue types differ in the expression profile of ECM proteins. Thus, a comparative proteomic analysis of the ECM, secreted by MSC from bone marrow or adipose tissue, showed the presence of unique sets of proteins produced by each cell type. This allows us to assume that ECM tissue specificity is established at histo- and organogenesis stages and subsequently maintained throughout life [47]. The composition of ECM components, which are distinguished not only among different tissues and organs but also within niches, was confirmed for niches of the intestinal crypt, hematopoietic niche, and limb [48, 49]. Such diversity among ECM components within the niche provides a further indication for stem cell outcomes. Each component supports important functions, from keeping the stem cell in the quiescent state to asymmetric division, migration along to ECM components or soluble factors, and the termination of differentiation [50–52]. These functions are mediated by the activation of a specific signal cascade. The interaction of participants in the cell signaling pathways, including MSC, with the microenvironment is carried out using special molecules, the most important of them are discussed below.
Integrins
The main class of ECM receptors is integrins, heterodimeric proteins comprising α and β subunits. There are 18 determined α-subunits and 8 β-subunits in humans, and these are responsible for recognizing ECM proteins and their physical properties (e.g., stiffness and stretching), and for intercellular communications. Some reviews can provide more detailed information on modern representations of the structure of integrins [53–55].
Integrins realize bi-directional signaling. The high-affinity interaction between integrins and their ECM ligands activates the “outside-in” signaling pathway. Then, focal adhesion kinase (FAK) and Src-mediated phosphorylation of the integrin adhesion complex (IAC) and cytoskeletal components initiate intracellular molecular reorganization and phosphorylation events among many adapters [56]. Crosstalk between FAK and Src kinases provides signaling pathways induced by mechanical forces and RTK signaling, leading to control of stem cell fate transitions [57]. For example, initiation of FAK/Src/Rac1-mediated myosin IIA recruitment into FAs increased the osteogenic commitment of human bone marrow MSC [58]. On other occasions, intracellular signals interact with the cytoplasmic tails of integrins, which leads to conformational changes in the extracellular ligand binding domain. This mechanism fine-tunes the control of ligand affinity [56, 59].
Integrins are considered crucial receptors for stem cell functioning. Various integrins are widely represented on the surface of different types of stem cells [60]. Subunit β1 is often associated with stem cell phenotype because, for several tissue-specific stem cells, this integrin supports the homing to stem-cell niche [61, 62], the maintenance of stemness [63], and the quantity of stem/progenitor cells in tissue [64].
There is no exception in the case of MSC. It has been shown that integrins α2β1 or α11β1 provide adequate interaction of human bone marrow MSC with type I collagen, which ensures cell survival and osteogenic differentiation by activating the protein kinase B (PKB/Akt) survival pathway [65]. Similar results were obtained in the study of integrin α5 activated signaling cascades in human bone marrow MSC during osteoblast differentiation. In this case, osteogenic differentiation of human bone marrow MSC was mediated by activation of FAK/ERK1/2 MAPKs and PI3K signaling pathways [66, 67]. Knockdown of α2 integrin in human bone marrow MSC during osteogenic differentiation on stiffer matrices was downregulated by ROCK, FAK and ERK1/2 axis [68]. Involvement of integrin α2 in human bone marrow MSC osteogenesis through activation of the p38 MAPK pathway was also demonstrated [69]. Results of another study showed that integrins in rat bone marrow MSC activate FAK-GSK3β phosphorylation, which prevents β-catenin degradation and nuclear translocation to bind to the wnt1 promoter [70]. In addition, silencing of the β1 subunit reduces both osteogenic and chondrogenic differentiation of human bone marrow MSC [71].
Discoidin domain receptors
Discoidin domain receptors (DDRs) (DDR1 and DDR2) are collagen-binding receptors in mammals [72]. Several articles have described the structure and existing isoforms of DDRs [73–76]. DDRs are transmembrane proteins with receptor tyrosine kinase (RTK) activity [74, 76]. They are an unusual subfamily of RTKs. In comparison with typical RTKs, DDRs bind a large ligand–collagen, which stimulates autophosphorylation over several hours and forms dimers in the absence of a ligand [77]. The detection of microenvironment stability is included in DDR functions, as ectodomain shedding mediated by matrix metalloproteinases regulates the level of DDRs on the cell surface [73, 78, 79].
Additionally, DDR1 demonstrated regulation of collagen transcription by translocating to the cell It appears that DDRs regulate the directed differentiation of progenitor cells. The depletion of DDR1 expression in human adipose-derived MSC suppresses chondrogenic differentiation by decreasing the chondrogenic genes and cartilaginous matrix deposition [80]. Furthermore, DDR1 regulates the terminal differentiation of human articular chondrocytes [81]. DDR2, as a collagen receptor, plays a crucial role in regulating bone development. DDR2 knockout in limb bud chondroprogenitors inhibited chondrogenic and osteogenic differentiation [82]. Moreover, DDR2 was found as one of the potential markers of osteoblastic progenitors derived from periosteum [83]. The expression of DDR2 and integrin α11β1 was increased when human bone marrow MSC were cultured on a substrate with type 1 collagen. It was found that the expression of integrin α11β1 prevailed during chondrogenic differentiation, while the expression of DDR2 was also significantly higher during osteogenic differentiation [84].
CD44
CD44 is primarily a receptor for hyaluronic acid (HA) but can also bind to several ligands, such as ECM components (fibronectin, laminin, osteopontin, HA), as well as some cytokines and growth factors [85]. CD44 represents a family of non-kinase transmembrane protein receptors. The structure and functions of various CD44 isoforms have previously been considered [85–87].
CD44 is a participant in multiple ECM-induced signaling pathways [85, 87] being also a well-known stem cell marker because it is represented in many stem-cell niches [88–90]. The activation of certain signaling pathways through CD44 is conditioned from the molecular weight of HA. CD44 is responsible for the migration/homing and differentiation of stem cells [85, 91–93]. The Wnt-induced/β-catenin signaling pathway is crucial for MSC commitment in osteogenic differentiation [94], and CD44 has a complex role because it is one of the gene targets and regulators of Wnt activation [85]. Moreover, CD44 is a key regulator of chondrogenic differentiation of human adipose-derived stem cells and human amniotic MSC via ERK1/2 signaling [95–97]. When the HA molecular weight is higher than CD44 human adipose-derived MSC form clusters, which stimulates chondrogenesis via ERK/SOX-9 pathway [95]. Moreover, CD44 inhibits apoptosis and enhances cell survival by ERK signaling in mouse bone marrow derived MSC and human chodrocytes [92, 98].
Proteoglycans
Proteoglycans are ubiquitous components of the cellular microenvironment, which includes several families. They also act as membrane-bound receptors. These molecules include heparan sulfate proteoglycans (HSPGs), comprising two distinct families: syndecans (4 members) and glypicans (6 members) [99, 100]. Numerous articles give detailed descriptions of the structure and functioning of HSPGs [99, 101–106].
Syndecans
There is abundant evidence that syndecans activate different signaling pathways. Studies show that syndecans have no kinase activity, but other kinases can phosphorylate their intracellular domains [105]. The interaction of syndecans with different signaling pathways became obvious during shedding processes. The results of these processes showed that the representation of syndecans on the cell surface reduced, and many growth factors lost their possible binding sites on the heparan sulfate chains and showed a decreased affinity to their receptors [73].
SDC-1 knockdown in mice leads to the inhibition of canonical Wnt signaling because of deficient levels of β-catenin [107]. Temporary knockdown of SDC-1 by RNA interference in primary human MSC cultures revealed a pro-adipogenic phenotype with enhanced osteoblast maturation. These findings implicate SDC-1 as a facilitator of balance during early induction of adipoblast and osteoblast lineage differentiation [108]. Overexpression of SDC-2 in mice decreased osteoblastic and osteoclastic precursors in bone marrow, as well as Wnt/β-catenin signaling in osteoblasts [109]. SDC-3 increased the canonical Wnt signaling that controls murine osteoblast maturation in vivo [110].
Glypicans
Glypicans are globular glycosylphophatidylinositol (GPI) anchored proteins [99, 111]. Typically, glypicans have an N-terminal cysteine-rich domain similar to that of Frizzled receptors and mediate Wnt binding [101]. Glypicans, like syndecans, are affected by shedding. Particularly, Notum lipase cleaves glypicans and inhibits Wnt signaling [112]. GPC3 lacking mutation in mouse embryos reduced Wnt/JNK signaling [113]. GPC6 inhibited the activity of the Wnt signaling pathway in GPC6-null mice [114]. A hedgehog signaling pathway in mouse GPC3 null embryos was hyperactivated [115]). It was observed that dysregulation of glypican in human bone marrow MSC isolated from tissues of osteoarthritis patients decreased the protein level of NOTUM (extracellular negative regulator of the WNT/β-catenin signaling pathway) during osteogenic differentiation [116].
Glycosphingolipids
Glycosphingolipids (GSLs) are amphiphilic membrane lipids of the eucaryotic plasma membrane consisting of glycan chains that are covalently linked to the sphingolipid backbone [117, 118]. GSL-associated glycans range from one and to more than 20 sugar residues, with 11 different monosaccharide types being used in vertebrates [119].
Numerous in vivo studies have reported that the composition of GSLs in the plasma membrane varies depending on the embryonic stage [117] Similar changes in GST expression can also be observed during stem cell differentiation in vitro. Thus, the GSLs composition of MSC dynamically changes according to the direction of lineage differentiation: MSC express SSEA-3 (stage-specific embryonic antigen), SSEA-4 along with GD1a and GD2 gangliosides, whereas the major GSLs of MSC-derived adipoblasts have GM3 and GD1a, MSC-derived chondrocytes have GM3 and GD3 [117, 120, 121]. A subpopulation of SSEA3( +) cells was isolated from MSC [122]. These cells, known as multilineage-differentiating stress-enduring (MUSE) cells, are endogenous and express pluripotency master genes and their capability to differentiate into cells of the three embryonic layers was established. At the same time MUSE are able to withstand stress and have an excellent ability to repair DNA damage [122, 123]. Recently, SSEA-3 was shown to act as an FGF-2 co-receptor in MUSE cells isolated from human bone marrow MSC. Their interaction activates the FGF-2 signaling cascade through PI3 kinase [122]. GM3 treatment enhanced TGF-β signaling through SMAD 2/3 during the chondrogenic differentiation of human synovial-derived MSC [124].
Mechanosensitive ion channels
Mechanosensitive ion channels in mammals include transient receptor potential channels (TRP) and Piezo channels [125]. TRP channels comprise eight subfamilies, i.e., TRPA (ankyrin), TRPC (canonical), TRPM (melastatin), TRPML (mucolipin), TRPP (polycystin), TRPV (vanilloid), TRPN (Drosophila No mechanoreceptor potential C), and TRPY (yeast). Only the first six are found in mammals [126]. The structures of these channels have been described in detail in various works [127, 128]. Piezo channels are nonselective cationic mechanosensitive channels, which include two members, i.e., Piezo1 and Piezo2 channels [129]. Various scientific publications describe the structure and features of functioning Piezo channels [130–135].
In the various stem cell niches MSC are involved in the microenvironmental control process. TRPV4 modulates the formation of collagen fibrils by human bone marrow MSC. The inhibition of this channel in MSC disrupts aligned collagen matrix assemblies. In contrast, TRPV4 activation promotes collagen deposition [136].
Tissue-specific Piezo2 isoforms are formed as a result of alternative splicing, where each isoform may have its own specific function. The diversity of splice isoforms is performed in the neuronal tissue and cells. Only one splice isoform is expressed in non-neuronal tissue [125]. Piezo1 regulates cross-talk between osteoblasts and osteoclasts in mice. In the osteoblastic cells, the expression of type II and IX collagens is controlled by Piezo1-YAP-signaling axis. The deficiency of these collagen isoforms results in an increase in osteoclast differentiation and bone resorption in vivo [137]. Furthermore, mouse bone marrow MSC with Piezo-channel loss demonstrated the inhibition of osteoblast differentiation because of a reduction of YAP and β-catenin [138]. The effect of mechanosensitive channels on stem cell behavior is disclosed in more detail in reviews [139, 140].
Based on the studied scientific sources, we arrange a general table of known intracellular signaling pathways from ECM receptors in stem and committed progenitor cells with several examples of their realization in MSC (Table 2).
Table 2.
Interactions of stem cell functions and signaling pathways for major ECM receptors
| Receptor | α1β1 | β1 | α2β1 | α5β1 | α11β1 | |
|---|---|---|---|---|---|---|
| Signalling pathway | ? | Wnt/β-catenin pathway | Protein kinase B (PKB/Akt) survival pathway; MAPK p38 signaling; ROCK, FAK, and ERK1/2 signaling axis; ? |
Wnt/β-catenin signaling pathway; PI3K, FAK, and ERK1/2 signaling axis; ? |
Protein kinase B (PKB/Akt) survival pathway | |
| Stem cell function | Osteogenic differentiation on nanotopography surface |
Chondrogenic differentiation and maintenance of cell phenotype; Osteogenic differentiation; Chondrogenic differentiation under fluid shear stress |
Viability and osteogenic differentiation; osteogenic differentiation; osteogenic differentiation on matrices with 42.1 ± 3.2 kPa; Chondrogenic differentiation under fluid shear stress |
Osteogenic differentiation on the tunable polyacrylamide hydrogels coated with fibronectin and Young’s modulus 62–68 kPa; Osteogenic differentiation; Chondrogenic differentiation under fluid shear stress |
Viability and osteogenic differentiation | |
| Stem cell type | Rat bone marrow MSC [141] |
Mouse chondrocytes and rat bone marrow MSC [70]; human bone marrow MSC [71]; Rat chondrocytes [142] |
Human bone marrow MSC [65, 68, 69]; Rat chondrocytes [142] |
hMSC [67]; human bone marrow MSC [66]; Rat chondrocytes [142] |
Human bone marrow MSC [65] | |
| Receptor | DDRs | CD44 | Syndecans | Mechanosensing ion channels | ||
| DDR1 | DDR2 | SDC-2 | SDC-3 | TRPV4 | ||
| Signalling pathway | Indian hedgehog/Gli1/Gli2/Col-X pathway | p38 MAPK kinase pathway | ERK1/2 signaling | cortactin and Survivin axis; Wnt/β-catenin signaling; | WNT signaling | TRPV4 and SOX9 axis; TRPV4/ERK/RUNX2; TRPV4 increased intracellular Ca2 + , NFATc1 nuclear translocation, and Wnt/β-catenin signaling |
| Stem cell function | terminal chondrocyte differentiation | osteoblast mineralization | Chondrogenic differentiation | migration; control population of osteoblastic and osteoclastic precursors in bone marrow; | osteoblast maturation |
Chondrogenic differentiation; Osteogenic differentiation |
| Stem cell type | mouse chondrocytes [81] | rat osteoblasts [143] |
human amniotic mesenchymal stem cells (hAMSC) [96]; rat and human adipose derived MSC [95] |
human bone marrow MSC [93]; mice osteoblastic and osteoclastic precursors [109] |
osteoblastic progenitors [110] |
murine MSC [144]; Murine bone marrow MSC [145]; Rat bone marrow MSC [146]s |
The symbol “?” mean unclear signaling pathway for specific process
Potential therapeutic strategies targeting ECM-induced signaling in postnatal stem cells for regenerative medicine
Among the promising regenerative medicine strategies involving ECM receptors, two main approaches can be distinguished: 1) blocking of receptors to ECM components and their intracellular signaling pathway, and 2) activation of ECM receptors by functionalization of various surfaces and materials with specific peptides or ECM components.
It is well-known that integrins are involved in the tissue regeneration processes. The role of MSC-expressed integrins for each tissue type remains a promising area of research. Thus, following an injury, MSC are recruited from surrounding tissue to the injury site in an integrin-dependent manner [147]. Some recent studies have shown that the expression of certain integrins in MSC ensures the maintenance of the blood–brain barrier in vivo models of traumatic brain injury or ischemic stroke [148, 149]. Integrins also play a vital role in wound healing. According to the results of several preclinical studies blocking the integrins αvβ5, αvβ3, α3β1 effectively decreased myofibroblast differentiation of human dermal fibroblasts in vitro and murine lung fibroblasts in vivo in association with TGFβ signaling [150–152]. Evaluation of therapeutic success of biomaterials which functionalized with integrin-targeting peptides has been recently reviewed [147, 153]. In this context, it has been repeatedly shown that human bone marrow MSC increase the expression of osteogenic markers if cultured on materials modified with RGD-peptide (adhesion site of fibronectin) [154, 155]. Similar results were obtained for human bone marrow MSCs in osteogenic differentiation using materials functionalized with collagen-based cell adhesion motifs: GFPGER (binding integrins α1 and α2), GFPGEN (binding integrin α1 only), GFOGER (a2b1 integrin) [69, 156, 157]. Key features of integrin-binding peptides in combination with biomaterials and their strong potential as biomimetic tools for regenerative medicine are described in a recent review [158].
The role of DDRs in wound healing is still poorly understood. It is known that DDR2 regulated wound healing by activating p38 and ERK1/2 kinases and inducing matrix metalloproteinase (MMP) expression [159]. Recent studies demonstrated the crucial role of DDR2 in the regeneration of cranial bone [160]. For integrins, materials conjugated with specific collagen sequence peptides have been developed that stimulate DDR activation. For example, the GVMGFO peptide interacts with the DDR2 receptor, leading to DDR2 Y740 phosphorylation and stimulation of osteoblast differentiation [161]. A potentially novel approach in regenerative medicine is the use of extracellular vesicles or exosomes from the mouse adipose derived MSC secretome to restore ECM receptor expression. It has been shown that MSC-derived exosomes can accelerate cutaneous wound healing by suppressing miR-96-5p and restoring DDR2 expression [162].
Previously, it was shown that MSC encapsulated in HA-based hydrogels expressed more markers of cartilage tissue both in vitro and in vivo compared to control samples [163]. This was also confirmed by a study using antibody CD44 blockade, which led to the offset of this effect when MSC were cultured on HA hydrogels [164]. A recent study demonstrated the efficacy of combined therapy on angiogenesis in ischemic diseases using HA with human umbilical cord blood-derived endothelial colony-forming cells and human umbilical cord derived MSC [165].
Syndecans and glypicans regulated the normal regeneration of different tissues [166–169]. SDC-3 increased new bone formation in vivo [110]. SDC-4 is essential for regenerating damaged muscle in mouse model [170]. Exosomes derived from rat bone marrow MSC showed chondroprotective effects through the regulatory role of exosomal microRNA-9-5p (miR-9-5p) to inhibit syndecan-1 in a rat model of osteoarthritis [171]. At the same time, SDC3 deletion enhances the efficacy of murine bone marrow MSC treatment of inflammatory arthritis in vivo [172]. Among other materials alginate hydrogels containing integrin and syndecan binding peptides (cyclic RGD and AG73, respectively) were developed which exhibited higher human nucleus pulposus (NP) cell viability, biosynthetic activity, and NP-specific protein expression than alginate alone [173].
Currently, there are not many publications on the use of MSC glycosphingolipids in the field of regenerative medicine. However, some data support the idea that glycosphingolipids could be a promising target for the treatment of various diseases [174, 175].
Mechanotransduction is also involved in regenerative processes. For example, the hematoma formed after a bone fracture is highly viscoelastic, and such viscoelasticity is necessary to allow infiltration of MSCs and osteogenic stimulation of MSC in vivo [176]. Cultivation of MSC in RGD-coupled alginate hydrogels leads to the activation of TRPV4 ion channels and then nuclear translocation of RUNX2 which drives osteogenic differentiation [177].
Biofunctionalization of tissue engineering materials improves cellular interaction and tissue integration. Currently, a large number of functionalization methods of tissue engineering materials are known, ranging from single peptides and components of ECM, including enzymes responsible for its remodeling, to decellularization of tissues and whole organs, which is described in detail in the reviews [158, 178–180]. The success of the approach to obtain ECM secreted by a specific cell type, such as MSC, can be assessed based on recent studies in this area [181–183]. Furthermore, the use of ECM-derived materials for tissue repair targeting the stem cell differentiation including MSC is also a promising approach that has been confirmed by several registered clinical trials [184–187].
Predicting the ECM receptor networks for the signaling pathway using the system biology approaches
Several approaches of network biology are widely used to study the activation of contributing factors in intracellular signaling cascades, which can subsequently find application in predictive medicine [187]. Nowadays, computational network modeling is used to determine niche-induced signaling pathways that identify stem cell outcome determinants [188]. Several network models that are used to help assess the effects of drugs on key signaling participants have been created for cancer cells [189]. The application of network biology approaches in the context of signaling pathways from the ECM led to the consideration of the integrin adhesome, which are responsible, together with integrins and integrin-associated proteins, for stabilizing cell adhesion and signal transduction [190, 191]. In addition, the “consensus adhesome” was formulated based on 60 proteins, defined by merging mass spectrometry datasets obtained from three cancer cell lines, telomerase-immortalized human foreskin fibroblasts and mouse embryonic fibroblasts attached in fibronectin-coated dishes [192].
Subsequently, with the development of omics technology and the rapid evolution of big data analysis, different approaches and specialized databases have been created by the scientific community. This is also relevant to matrix biology. One such database comprising ECM component adhesomes and interactions is MatrixDB (http://matrixdb.univ-lyon1.fr/) [193]. Another database is MatrisomeDB, which integrates experimental proteomic data on the ECM composition of normal and diseased tissue types (https://matrisomedb.org/) [194]. Recent studies reported the creation of a database (MatriNet) that will enable the study of structural changes in ECM network architectures as a function of their protein–protein interaction strengths across 20 different tumor types (www.matrinet.org) [195].
For the construction of protein–protein interactions (PPIs), many investigators are using databases that aggregate standard information from large resources (e.g., PDB, IntAct, BioGRID, HPRD). Examples of such PPI databases are STRING and Mint (http://www.string-db.org) [196, 197]; STRING was used to create molecule interactions for syndecans and Piezo channels [104, 198].
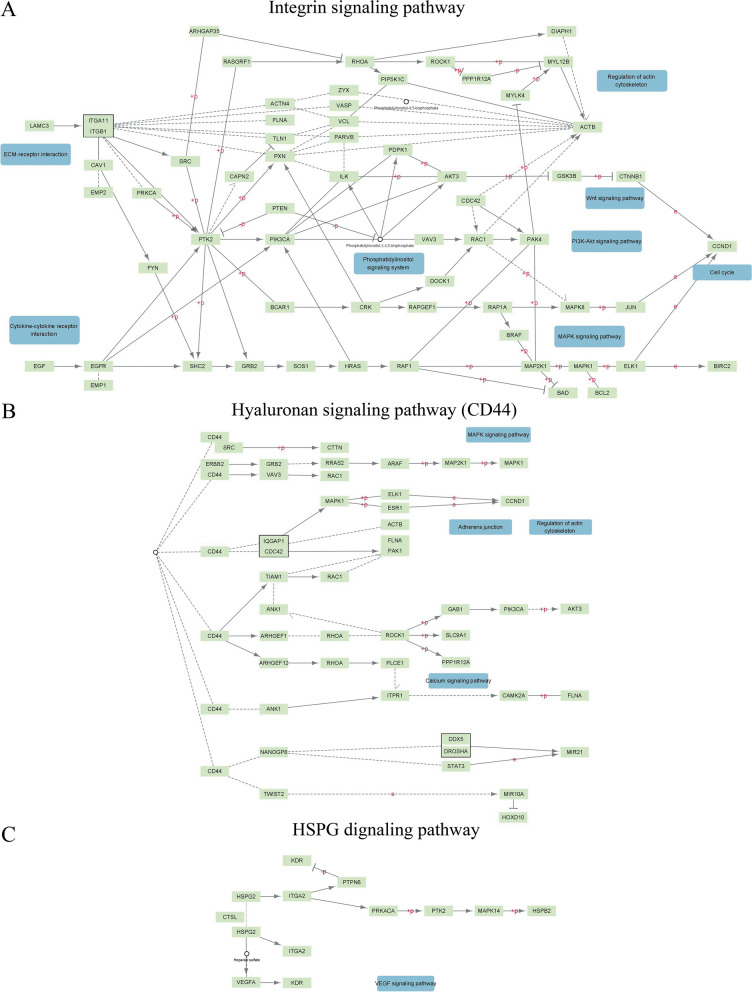
In our review, prior to creating our PPI networks for ECM receptors, we checked preexisting networks of signaling pathways from ECM receptors in the KEGG PATHWAY Database (https://www.kegg.jp/kegg/pathway.html). We revealed the signaling pathways for integrins, CD44, and HSPG (Fig. 1).
Fig. 1.
General networks of signaling pathways from ECM receptors obtained from the KEGG PATHWAY Database: A—integrins, B—CD44, and C—HSPG
General networks for ECM receptors included a small quantity of signaling molecules or signaling members, from receptors to growth factors, and demonstrated crosstalk between them. However, it gives rise to new difficulties in determining the function of ECM signaling pathway participants. Here, we decided to try using an approach for the definition of specific signaling pathways for individual ECM receptors.
First, we created PPI networks for integrin β1 and CD44 as one of the well-studied surface markers of stem cells and employed DDR1 as an example of a less-investigated receptor but potentially useful for application to mechanosensing. PPI networks were created using the STRING database with the following settings: network type – physical subnetworks; meaning of network edges – evidence; active interaction sources; experiments; minimum required interactions score – 0.4, 2 shell; maximum number of interactors to show – 150. In addition, Cytoscape was used for analysis and network visualization (v.3.9.1; https://cytoscape.org/) [199]. As mentioned above, the majority of data utilizing omics technology have to date been obtained from cancer cells and tissue. We verified how many signaling molecules would be excluded from our data for network construction if we used only data obtained from isolated human primary cells or human cell lines, excluding cancer cells or cell lines obtained from patients with disease, on the PPIs network for integrin β1 (Fig. 1 Supplement). As a result of this analysis, we found that only 13 of 23 members of different types of signal transduction pathways met in normal cell lines.
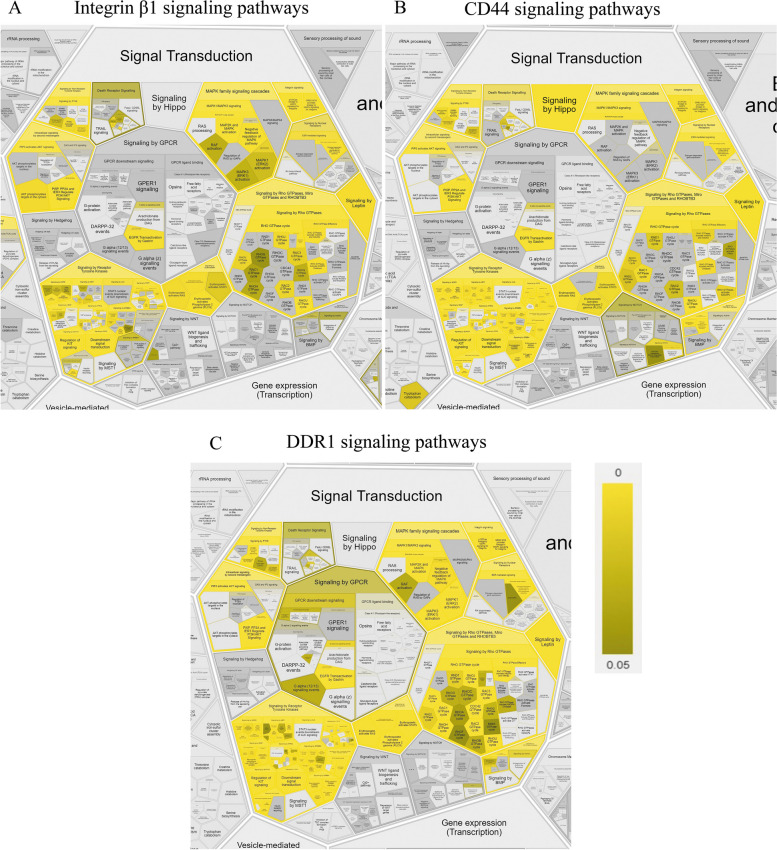
Next, we analyzed the contributing factors of the signaling pathway for integrin β1, CD44, and DDR1 using ReactomeFIPlugIn in Cytoscape, which accessed the Reactome pathways stored in this database (https://reactome.org/) [200]. We selected the signal transduction database to analyze our networks, and the obtained results are presented as Reactfoam (Fig. 2 Supplement) as an illustration of analysis results using a false discovery rate (FDR) scalebar (p-value ranging from 0–0.05) according to not only the type of signaling pathways (Fig. 2) but also cellular function (Fig. 2_Supplement).
Fig. 2.
Illustration of contributing factors of the signaling pathway for integrin β1 (A), CD44 (B), and DDR1 (C), which generated using ReactomeFIPlugIn in Cytoscape. The obtained results are presented as part of Reactfoam according to the type of signaling pathways using a false discovery rate (FDR) scalebar (p-value ranging from 0–0.05)
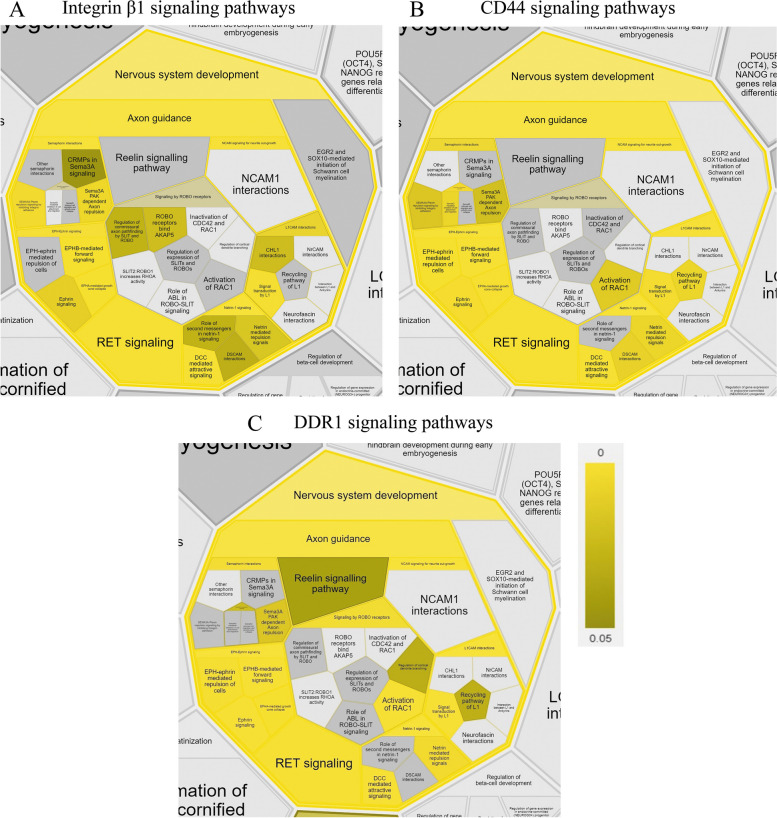
We reveal that the signaling pathway members of integrin β1, CD44, and DDR1 are vital for nervous system development (Fig. 3).
Fig. 3.
Illustration of contributing factors of the signaling pathway for integrin β1 (A), CD44 (B), and DDR1 (C), which generated using ReactomeFIPlugIn in Cytoscape. The obtained results are presented as part of Reactfoam according to the cellular function using a false discovery rate (FDR) scalebar (p-value ranging from 0–0.05)
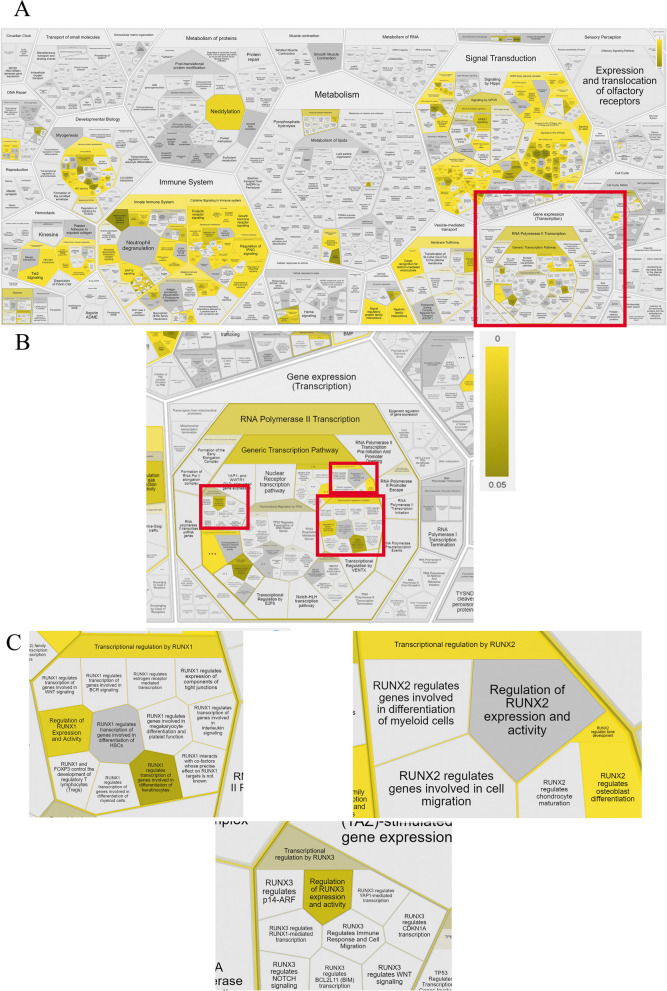
In addition, we build a prediction network of PPIs for DDR1 pathway members in human adipose-derived MSC. For this step, we normalized the data of PPIs using RNAseq data describing the transcriptome of human adipose-derived MSC obtained in our laboratory (Fig. 4).
Fig. 4.
Illustration of contributing factors of the signaling pathway for DDR1 in human adipose-derived MSC (A), (B), (C), which generated using ReactomeFIPlugIn in Cytoscape (B and C—enlarged parts of the image A). The obtained results are presented as part of Reactfoam according to the cellular function using a false discovery rate (FDR) scalebar (p-value ranging from 0–0.05)
Conclusions
ECM-induced signaling pathways within the stem cells may define the functionality and homeostasis of the whole tissue. Trying to understand the complicated molecular interactions between ECM and stem and progenitor cells, scientists are developing new approaches based on a general view obtained from big data analysis. The application of system biology methods for this purpose has been an observable current trend in matrix biology [201].
In this review, we discussed the results of recent studies covering the participation of cellular receptors to ECM components in the maintenance of postnatal tissue homeostasis as well as tissue regeneration after various types of damage through the regulation of MSC functions. We also focused on summarizing the data of the currently known ECM-induced signaling cascades in human stem and progenitor cells. However, literature analysis revealed that very few and only the most common participants of these signal pathways are investigating; moreover, they are involved in multiple cellular processes which makes them not suitable as a potential therapeutic target to modulate stem cell functioning for the purposes of regenerative medicine. Therefore, to detect more specific ECM-induced signaling pathways in stem and progenitor cells as well as to search for novel targets for fine-tuning regeneration processes, we suggest using the approaches of systems biology.
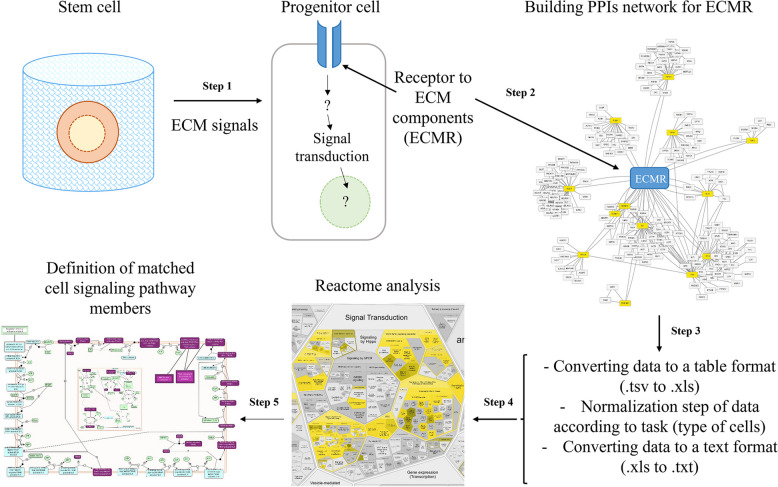
Utilizing the established changes in the stem cell profile of ECM receptors (Step 1), it is possible to build predictive networks of PPIs (Step 2). Such networks can be analyzed based on the well-known and available databases described in this review. After receiving the list of participants in the signaling cascade, a normalization step can be added to the data of the proteome or transcriptome of cells of interest to researchers (Step 3). Then, the created network can be compared with a database of known signal pathways to select specific signaling pathways and processes accumulating the most of participants from the previously predicted network of PPIs (Step 4 and Step 5). The resulting theoretical model could be useful in designing the further experimental research exploring the ECM-mediated regulation of stem and progenitor cells (Fig. 5).
Fig. 5.
Summary illustration of review
This review is the first to detail the major types of ECM receptors in postnatal stem cells, using MSC as an example, and to evaluate the involvement of ECM-induced signaling cascades in the process of MSC differentiation. In addition, a detailed algorithm of action using state-of-the-art methods in the field of systems biology is proposed to explore the variability of ECM signaling pathways in different cells. It may help other researchers in the field to discover new targets for tissue and organ regeneration with the ability to fine-tune cellular mechanisms rather than inhibiting members of cascades that are responsible for multiple processes and could potentially lead to pathology or cell death (e.g., such as Src, Erk, Akt).
Shortly, we suppose that the suggested approach of generating the predictive networks of PPI could serve as a useful tool which is complementary or even partially replacing the omics experimental work. Combining the known data about ECM receptor on the specific target cells and desirable functional processes one could reveal novel expected or unexpected signal transduction pathways induced by ECM. Few examples are demonstrated in the review. Indeed, these results have limited value until experimental validation. However, the suggested algorithm could intensify the search of ECM-induced signaling pathways in stem and progenitor cells and shorten the time to the potential breakthroughs in the field.
Thus, following the current trends in the field of matrix biology, it could allow to identify new promising directions in the study of stem and committed cell behavior within their matrix microenvironment. Importantly, these approaches expand the number of tools in regenerative medicine using to search for the mechanisms regulating tissue and organ renewal and repair.
Supplementary Information
Additional file 1: Fig. 1_Supplement. Predicting the integrin β1 PPIs networks for signal transduction molecules before (A) and after (B) excluded data obtained from cancer cells.
Additional file 2: Fig. 2_Supplement. Illustration of contributing factors of the signaling pathway for integrin β1 (A), CD44 (B), and DDR1 (C), which generated using ReactomeFIPlugIn in Cytoscape. The obtained results are presented as Reactfoam using a false discovery rate (FDR) scalebar (p-value ranging from 0–0.05).
Additional file 3: Fig. 3_Supplement. Predicting the DDR1 signaling pathway members participate in semaphorin interactions (A), and regulate the activity of RUNX1, RUNX2, and RUNX3 transcription factors in the case of osteogenic differentiation (B).
Acknowledgements
The authors thanks Novoseletsky Valery for the thoughtful and helpful discussions.
Abbreviations
- CD44
Cluster of differentiation 44
- DDR1
Discoidin domain receptor tyrosine kinase 1
- DDR2
Discoidin domain receptor tyrosine kinase 2
- ECM
Extracellular matrix
- FAK
Focal adhesion kinase
- GPI
Glycosylphophatidylinositol
- GSLs
Glycosphingolipids
- HA
Hyaluronic acid
- HSPGs
Heparan sulfate proteoglycans
- IAC
Integrin adhesion complex
- ILK
Integrin-linked kinase
- MMP
Matrix metalloproteinases
- MSC
Mesenchymal stromal cells
- MUSE
multilineage-differentiating stress-enduring cells
- PLC
phospholipase C
- PPIs
protein–protein interactions
- RNA
ribonucleic acid
- RTK
eceptor tyrosine kinase
- TRP
Transient receptor potential channels
Authors’ contributions
Novoseletskaya E.S. made substantial contributions to the conception of the work and the acquisition, analysis and interpretation of data and wrote the entire paper. Evdokimov P.V. revised work critically for important intellectual content. Efimenko A.Yu. made substantial contributions to the conception of the work and revised work critically for important intellectual content. All authors read and approved the final manuscript.
Funding
The work was financially supported by Russian Science Foundation (grant #20–79-10210).
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
In this review only open source software platforms, web-services and databases were used.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aghlmandi A, Nikshad A, Safaralizadeh R, Warkiani ME, Aghebati-Maleki L, Yousefi M. Microfluidics as efficient technology for the isolation and characterization of stem cells. EXCLI J. 2021. [DOI] [PMC free article] [PubMed]
- 2.van Velthoven CTJ, Rando TA. Stem Cell Quiescence: Dynamism, Restraint, and Cellular Idling. Cell Stem Cell. 2019;24:213–25. Available from: https://pubmed.ncbi.nlm.nih.gov/30735649/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 3.Gola A, Fuchs E. Environmental control of lineage plasticity and stem cell memory. Curr Opin Cell Biol. 2021;69:88–95. Available from: https://pubmed.ncbi.nlm.nih.gov/33535130/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 4.Chen J, Sun T, You Y, Wu B, Wang X, Wu J. Proteoglycans and Glycosaminoglycans in Stem Cell Homeostasis and Bone Tissue Regeneration. Front Cell Dev Biol. 2021;9. Available from: https://pubmed.ncbi.nlm.nih.gov/34917612/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 5.Mannino G, Russo C, Maugeri G, Musumeci G, Vicario N, Tibullo D, et al. Adult stem cell niches for tissue homeostasis. J Cell Physiol. 2022;237:239–57. Available from: https://pubmed.ncbi.nlm.nih.gov/34435361/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 6.Cho IJ, Lui PPW, Obajdin J, Riccio F, Stroukov W, Willis TL, et al. Mechanisms, Hallmarks, and Implications of Stem Cell Quiescence. Stem Cell Rep. 2019;12.6:1190–200. Available from: 10.1016/j.stemcr.2019.05.012. Cited 2019 Jun 11. [DOI] [PMC free article] [PubMed]
- 7.Baghdadi MB, Castel D, Machado L, Fukada SI, Birk DE, Relaix F, et al. Reciprocal signalling by Notch-Collagen V-CALCR retains muscle stem cells in their niche. Nature. 2018;557:714–8. Available from: https://pubmed.ncbi.nlm.nih.gov/29795344/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 8.Schofield R. The relationship between the spleen colony-forming cell and the haemopoietic stem cell. A hypothesis. Blood Cells. 1978;4(1-2):7–25. Available from: https://europepmc.org/article/med/747780. Cited 1978 Jan 01. [PubMed]
- 9.Novoseletskaya ES, Grigorieva OA, Efimenko AY, Kalinina NI. Extracellular Matrix in the Regulation of Stem Cell Differentiation. Biochemistry (Moscow). 2019;84:232–40. Available from: https://link.springer.com/article/10.1134/S0006297919030052. Cited 2023 Jul 31. [DOI] [PubMed]
- 10.Isomursu A, Lerche M, Taskinen ME, Ivaska J, Peuhu E. Integrin signaling and mechanotransduction in regulation of somatic stem cells. Exp Cell Res. 2019;378:217–25. Available from: https://pubmed.ncbi.nlm.nih.gov/30817927/. Cited 2023 Apr 23. [DOI] [PubMed]
- 11.Wosczyna MN, Konishi CT, Perez Carbajal EE, Wang TT, Walsh RA, Gan Q, et al. Mesenchymal Stromal Cells Are Required for Regeneration and Homeostatic Maintenance of Skeletal Muscle. Cell Rep. 2019;27:2029–2035.e5. Available from: http://www.cell.com/article/S2211124719305546/fulltext. Cited 2023 Jul 17. [DOI] [PMC free article] [PubMed]
- 12.Technologies Inc S. WA900280-Roles_for_mesenchymal_stem_cells_as_medicinal_signaling_cells. 2015; Available from: www.stemcell.com/MesenCult. Cited 2023 Jul 17.
- 13.Degirmenci B, Valenta T, Dimitrieva S, Hausmann G, Basler K. GLI1-expressing mesenchymal cells form the essential Wnt-secreting niche for colon stem cells. Nature 2018 558:7710. 2018;558:449–53. Available from: https://www.nature.com/articles/s41586-018-0190-3. Cited 2023 Jul 17. [DOI] [PubMed]
- 14.Morrison SJ, Scadden DT. The bone marrow niche for haematopoietic stem cells. Nature 2014 505:7483. 2014;505:327–34. Available from: https://www.nature.com/articles/nature12984. Cited 2023 Jul 17. [DOI] [PMC free article] [PubMed]
- 15.HETEROTOPIC TRANSPLANTS OF BONE MARROW : Transplantation.. Available from: https://journals.lww.com/transplantjournal/Abstract/1968/03000/HETEROTOPIC_TRANSPLANTS_OF_BONE_MARROW.9.aspx. Cited 2023 Jul 17.
- 16.Itkin T, Ludin A, Gradus B, Gur-Cohen S, Kalinkovich A, Schajnovitz A, et al. FGF-2 expands murine hematopoietic stem and progenitor cells via proliferation of stromal cells, c-Kit activation, and CXCL12 down-regulation. Blood. 2012;120:1843–55. Available from: https://dx.doi.org/10.1182/blood-2011-11-394692. Cited 2023 Jul 17. [DOI] [PubMed]
- 17.Viswanathan S, Shi Y, Galipeau J, Krampera M, Leblanc K, Martin I, et al. Mesenchymal stem versus stromal cells: International Society for Cell & Gene Therapy (ISCT®) Mesenchymal Stromal Cell committee position statement on nomenclature. Cytotherapy. 2019;21:1019–24. Available from: http://www.isct-cytotherapy.org/article/S1465324919308412/fulltext. Cited 2023 Jul 17. [DOI] [PubMed]
- 18.Caplan AI. Mesenchymal Stem Cells: Time to Change the Name! Stem Cells Transl Med . 2017;6:1445–51. Available from 10.1002/sctm.17-0051. Cited 2023 Jul 17. [DOI] [PMC free article] [PubMed]
- 19.Belarbi K, Cuvelier E, Bonte MA, Desplanque M, Gressier B, Devos D, et al. Glycosphingolipids and neuroinflammation in Parkinson’s disease. Molecular Neurodegeneration. 2020;15:1–16. doi: 10.1186/s13024-020-00408-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dalchau R, Kirkley J, Fabre JW. Monoclonal antibody to a human leukocyte-specific membrane glycoprotein probably homologous to the leukocyte-common (L-C) antigen of the rat. Eur J Immunol. 1980;10:737–44. doi: 10.1002/eji.1830101003. [DOI] [PubMed] [Google Scholar]
- 21.Ponta H, Sherman L, Herrlich PA. CD44: from adhesion molecules to signalling regulators. Nat Rev Mol Cell Biol. 2003;4:33–45. Available from: https://pubmed.ncbi.nlm.nih.gov/12511867/. Cited 2023 Apr 23. [DOI] [PubMed]
- 22.Rapraeger AC, Bernfield# M. Heparan sulfate proteoglycans from mouse mammary epithelial cells. A putative membrane proteoglycan associates quantitatively with lipid vesicles. J Biol Chem. 1983;258:3632–6. [PubMed]
- 23.Saunders S, Jalkanen M, O’Farrell S, Bernfield M. Molecular cloning of syndecan, an integral membrane proteoglycan. J Cell Biol. 1989;108:1547–56. Available from: https://pubmed.ncbi.nlm.nih.gov/2494194/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 24.Gabius HJ, Springer WR, Barondes SH. Receptor for the cell binding site of discoidin I. Cell. 1985;42:449–56. Available from: https://pubmed.ncbi.nlm.nih.gov/2411421/. Cited 2023 Apr 23. [DOI] [PubMed]
- 25.Structure, expression and chromosomal mapping of TKT from man and mouse: a new subclass of receptor tyrosine kinases with a factor VIII-like domain - PubMed.. Available from: https://pubmed.ncbi.nlm.nih.gov/8247548/. Cited 2023 Apr 23. [PubMed]
- 26.Marco E Di, Cutuli N, Guerra L, Cancedda R, De Luca M. Molecular cloning of trkE, a novel trk-related putative tyrosine kinase receptor isolated from normal human keratinocytes and widely expressed by normal human tissues. J Biol Chem. 1993;268:24290–5. Available from: https://pubmed.ncbi.nlm.nih.gov/8226977/. Cited 1993 Nov 15. [PubMed]
- 27.Vogel W, Gish GD, Alves F, Pawson T. The discoidin domain receptor tyrosine kinases are activated by collagen. Mol Cell [Internet]. 1997 [cited 2023 Apr 23];1:13–23. Available from: https://pubmed.ncbi.nlm.nih.gov/9659899/ [DOI] [PubMed]
- 28.Montell C, Jones K, Hafen E, Rubin G. Rescue of the Drosophila phototransduction mutation trp by germline transformation. Science. 1985;230:1040–3. Available from: https://pubmed.ncbi.nlm.nih.gov/3933112/. Cited 2023 Apr 23. [DOI] [PubMed]
- 29.Wes PD, Chevesich J, Jeromin A, Rosenberg C, Stetten G, Montell C. TRPC1, a human homolog of a Drosophila store-operated channel. Proc Natl Acad Sci U S A. 1995;92:9652–6. Available from: https://pubmed.ncbi.nlm.nih.gov/7568191/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 30.Liu C, Montell C. Forcing open TRP channels: Mechanical gating as a unifying activation mechanism. Biochem Biophys Res Commun. 2015;460:22–5. Available from: https://pubmed.ncbi.nlm.nih.gov/25998730/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 31.Tamkun JW, DeSimone DW, Fonda D, Patel RS, Buck C, Horwitz AF, et al. Structure of integrin, a glycoprotein involved in the transmembrane linkage between fibronectin and actin. Cell. 1986;46:271–82. Available from: https://pubmed.ncbi.nlm.nih.gov/3487386/. Cited 2023 Apr 23. [DOI] [PubMed]
- 32.Glenney JR, Zokas L. Novel tyrosine kinase substrates from Rous sarcoma virus-transformed cells are present in the membrane skeleton. J Cell Biol. 1989;108:2401–8. Available from: https://pubmed.ncbi.nlm.nih.gov/2472406/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 33.Turner CE, Glenney JR, Burridge K. Paxillin: a new vinculin-binding protein present in focal adhesions. J Cell Biol. 1990;111:1059–68. Available from: https://pubmed.ncbi.nlm.nih.gov/2118142/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 34.Burridge K, Turner CE, Romer LH. Tyrosine phosphorylation of paxillin and pp125FAK accompanies cell adhesion to extracellular matrix: a role in cytoskeletal assembly. J Cell Biol. 1992;119:893–903. Available from: https://pubmed.ncbi.nlm.nih.gov/1385444/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 35.Hannigan GE, Leung-Hagesteijn C, Fitz-Gibbon L, Coppolino MG, Radeva G, Filmus J, et al. Regulation of cell adhesion and anchorage-dependent growth by a new beta 1-integrin-linked protein kinase. Nature. 1996;379:91–6. Available from: https://pubmed.ncbi.nlm.nih.gov/8538749/. Cited 2023 Apr 23. [DOI] [PubMed]
- 36.Fukuda K, Gupta S, Chen K, Wu C, Qin J. The pseudoactive site of ILK is essential for its binding to alpha-Parvin and localization to focal adhesions. Mol Cell. 2009;36:819–30. Available from: https://pubmed.ncbi.nlm.nih.gov/20005845/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 37.Calderwood DA, Zent R, Grant R, Rees DJG, Hynes RO, Ginsberg MH. The Talin head domain binds to integrin beta subunit cytoplasmic tails and regulates integrin activation. J Biol Chem. 1999;274:28071–4. Available from: https://pubmed.ncbi.nlm.nih.gov/10497155/. Cited 2023 Apr 23. [DOI] [PubMed]
- 38.Rogalski TM, Mullen GP, Gilbert MM, Williams BD, Moerman DG. The UNC-112 gene in Caenorhabditis elegans encodes a novel component of cell-matrix adhesion structures required for integrin localization in the muscle cell membrane. J Cell Biol. 2000;150:253–64. Available from: https://pubmed.ncbi.nlm.nih.gov/10893272/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 39.Kloeker S, Major MB, Calderwood DA, Ginsberg MH, Jones DA, Beckerle MC. The Kindler syndrome protein is regulated by transforming growth factor-beta and involved in integrin-mediated adhesion. J Biol Chem. 2004;279:6824–33. Available from: https://pubmed.ncbi.nlm.nih.gov/14634021/. Cited 2023 Apr 23. [DOI] [PubMed]
- 40.Harburger DS, Bouaouina M, Calderwood DA. Kindlin-1 and -2 directly bind the C-terminal region of beta integrin cytoplasmic tails and exert integrin-specific activation effects. J Biol Chem. 2009;284:11485–97. Available from: https://pubmed.ncbi.nlm.nih.gov/19240021/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 41.Coste B, Mathur J, Schmidt M, Earley TJ, Ranade S, Petrus MJ, et al. Piezo1 and Piezo2 are essential components of distinct mechanically activated cation channels. Science. 2010;330:55–60. Available from: https://pubmed.ncbi.nlm.nih.gov/20813920/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 42.Coste B, Xiao B, Santos JS, Syeda R, Grandl J, Spencer KS, et al. Piezo proteins are pore-forming subunits of mechanically activated channels. Nature. 2012;483:176–81. Available from: https://pubmed.ncbi.nlm.nih.gov/22343900/. Cited 2023 Apr 23. [DOI] [PMC free article] [PubMed]
- 43.Omelyanenko NP, Karpov IN. Patterns of Cell—Matrix Interactions during Formation the Distraction Bone Regenerates. Bull Exp Biol Med. 2017;163:510–4. Available from: https://link.springer.com/article/10.1007/s10517-017-3840-9. Cited 2017 Aug 29. [DOI] [PubMed]
- 44.Muncie JM, Weaver VM. The Physical and Biochemical Properties of the Extracellular Matrix Regulate Cell Fate. Curr Top Dev Biol. 2018;130:1–37. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0070215318300346. Cited 2018 Mar 21. [DOI] [PMC free article] [PubMed]
- 45.Gattazzo F, Urciuolo A, Bonaldo P. Extracellular matrix: A dynamic microenvironment for stem cell niche. Biochim Biophys Acta Gen Subj. 2014;1840.8:2506–19. Available from: https://www.sciencedirect.com/science/article/pii/S0304416514000129. Cited 2014 Jan 10. [DOI] [PMC free article] [PubMed]
- 46.Agmon G, Christman KL. Controlling stem cell behavior with decellularized extracellular matrix scaffolds. Curr Opin Solid State Mater Sci. 2015;20.4:193–201. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1359028616300043. Cited 2016 Feb 15. [DOI] [PMC free article] [PubMed]
- 47.Ragelle H, Naba A, Larson BL, Zhou F, Prijić M, Whittaker CA, et al. Comprehensive proteomic characterization of stem cell-derived extracellular matrices. Biomaterials. 2017;128:147–59. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0142961217301448. Cited 2017 Mar 7. [DOI] [PMC free article] [PubMed]
- 48.Duckworth CA. Identifying key regulators of the intestinal stem cell niche. Biochem Soc Trans. 2021;49:2163–76. Available from: https://pubmed.ncbi.nlm.nih.gov/34665221/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 49.Robertson SYT, Roberts JS, Deng SX. Regulation of Limbal Epithelial Stem Cells: Importance of the Niche. Int J Mol Sci. 2021;22. Available from: https://pubmed.ncbi.nlm.nih.gov/34769405/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 50.Elbediwy A, Vincent-Mistiaen ZI, Thompson BJ. YAP and TAZ in epithelial stem cells: A sensor for cell polarity, mechanical forces and tissue damage. BioEssays. 2016;38:644–653. doi: 10.1002/bies.201600037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yamada T, Hasegawa S, Miyachi K, Date Y, Inoue Y, Yagami A, et al. Laminin-332 regulates differentiation of human interfollicular epidermal stem cells. Mech Ageing Dev. 2018;171:37–46. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0047637417302592. Cited 2018 Mar 16. [DOI] [PubMed]
- 52.Patel DF, Peiró T, Shoemark A, Akthar S, Walker SA, Grabiec AM, et al. An extracellular matrix fragment drives epithelial remodeling and airway hyperresponsiveness. Sci Transl Med. 2018; [DOI] [PMC free article] [PubMed]
- 53.Orré T, Rossier O, Giannone G. The inner life of integrin adhesion sites: From single molecules to functional macromolecular complexes. Exp Cell Res. 2019;379:235–44. Available from: https://pubmed.ncbi.nlm.nih.gov/30943383/. Cited 2023 Apr 24. [DOI] [PubMed]
- 54.Kadry YA, Calderwood DA. Chapter 22: Structural and signaling functions of integrins. Biochim Biophys Acta Biomembr. 2020;1862. Available from: https://pubmed.ncbi.nlm.nih.gov/31991120/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 55.Wang L, Zheng F, Song R, Zhuang L, Yang M, Suo J, et al. Integrins in the Regulation of Mesenchymal Stem Cell Differentiation by Mechanical Signals. Stem Cell Rev Rep. 2022;18:126–41. Available from: https://pubmed.ncbi.nlm.nih.gov/34536203/. Cited 2023 Apr 24. [DOI] [PubMed]
- 56.Chastney MR, Conway JRW, Ivaska J. Integrin adhesion complexes. Curr Biol. 2021;31:R536–42. Available from: https://pubmed.ncbi.nlm.nih.gov/34033786/. Cited 2023 Apr 24. [DOI] [PubMed]
- 57.De Belly H, Paluch EK, Chalut KJ. Interplay between mechanics and signalling in regulating cell fate. Nature Reviews Molecular Cell Biology 2022 23:7. 2022;23:465–80. Available from: https://www.nature.com/articles/s41580-022-00472-z. Cited 2023 Jul 17. [DOI] [PubMed]
- 58.Han P, Frith JE, Gomez GA, Yap AS, O’Neill GM, Cooper-White JJ. Five Piconewtons: The Difference between Osteogenic and Adipogenic Fate Choice in Human Mesenchymal Stem Cells. ACS Nano. 2019;13:11129–43. Available from: 10.1021/acsnano.9b03914. Cited 2023 Jul 17. [DOI] [PubMed]
- 59.Lee-Thedieck C, Schertl P, Klein G. The extracellular matrix of hematopoietic stem cell niches. Adv Drug Deliv Rev. 2022;181. Available from: https://pubmed.ncbi.nlm.nih.gov/34838648/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 60.Prowse ABJ, Chong F, Gray PP, Munro TP. Stem cell integrins: implications for ex-vivo culture and cellular therapies. Stem Cell Res. 2011;6:1–12. Available from: https://pubmed.ncbi.nlm.nih.gov/21075697/. Cited 2023 Apr 24. [DOI] [PubMed]
- 61.Kanatsu-Shinohara M, Takehashi M, Takashima S, Lee J, Morimoto H, Chuma S, et al. Homing of mouse spermatogonial stem cells to germline niche depends on beta1-integrin. Cell Stem Cell. 2008;3:533–42. Available from: https://pubmed.ncbi.nlm.nih.gov/18983968/. Cited 2023 Apr 24. [DOI] [PubMed]
- 62.Taniguchi Ishikawa E, Chang KH, Nayak R, Olsson HA, Ficker AM, Dunn SK, et al. Klf5 controls bone marrow homing of stem cells and progenitors through Rab5-mediated β1/β2-integrin trafficking. Nat Commun. 2013;4. Available from: https://pubmed.ncbi.nlm.nih.gov/23552075/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 63.Gottschling S, Saffrich R, Seckinger A, Krause U, Horsch K, Miesala K, et al. Human mesenchymal stromal cells regulate initial self-renewing divisions of hematopoietic progenitor cells by a beta1-integrin-dependent mechanism. Stem Cells. 2007;25:798–806. Available from: https://pubmed.ncbi.nlm.nih.gov/17110618/. Cited 2023 Apr 24. [DOI] [PubMed]
- 64.Lambert AW, Weinberg RA. Linking EMT programmes to normal and neoplastic epithelial stem cells. Nat Rev Cancer. 2021;21:325–38. Available from: https://pubmed.ncbi.nlm.nih.gov/33547455/. Cited 2023 Apr 24. [DOI] [PubMed]
- 65.Popov C, Radic T, Haasters F, Prall WC, Aszodi A, Gullberg D, et al. Integrins α2β1 and α11β1 regulate the survival of mesenchymal stem cells on collagen I. Cell Death Dis. 2011;2. Available from: https://pubmed.ncbi.nlm.nih.gov/21796158/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 66.Hamidouche Z, Fromigué O, Ringe J, Häupl T, Vaudin P, Pagès JC, et al. Priming integrin alpha5 promotes human mesenchymal stromal cell osteoblast differentiation and osteogenesis. Proc Natl Acad Sci U S A. 2009;106:18587–91. Available from: https://pubmed.ncbi.nlm.nih.gov/19843692/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 67.Sun M, Chi G, Xu J, Tan Y, Xu J, Lv S, et al. Extracellular matrix stiffness controls osteogenic differentiation of mesenchymal stem cells mediated by integrin α5. Stem Cell Res Ther. 2018;9. Available from: https://pubmed.ncbi.nlm.nih.gov/29490668/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 68.Shih YR V., Tseng KF, Lai HY, Lin CH, Lee OK. Matrix stiffness regulation of integrin-mediated mechanotransduction during osteogenic differentiation of human mesenchymal stem cells. J Bone Miner Res. 2011;26:730–8. Available from: https://pubmed.ncbi.nlm.nih.gov/20939067/. Cited 2023 Apr 26. [DOI] [PubMed]
- 69.Becerra-Bayona SM, Guiza-Arguello VR, Russell B, Höök M, Hahn MS. Influence of collagen-based integrin α1 and α2 mediated signaling on human mesenchymal stem cell osteogenesis in three dimensional contexts. J Biomed Mater Res A. 2018;106:2594–604. Available from: 10.1002/jbm.a.36451. Cited 2023 Jul 18. [DOI] [PMC free article] [PubMed]
- 70.Du J, Zu Y, Li J, Du S, Xu Y, Zhang L, et al. Extracellular matrix stiffness dictates Wnt expression through integrin pathway. Sci Rep. 2016;6. Available from: https://pubmed.ncbi.nlm.nih.gov/26854061/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 71.Navarrete RO, Lee EM, Smith K, Hyzy SL, Doroudi M, Williams JK, et al. Substrate Stiffness Controls Osteoblastic and Chondrocytic Differentiation of Mesenchymal Stem Cells without Exogenous Stimuli. PLoS One. 2017;12. Available from: https://pubmed.ncbi.nlm.nih.gov/28095466/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 72.Franceschi RT, Hallett SA, Ge C. Discoidin domain receptors; an ancient family of collagen receptors has major roles in bone development, regeneration and metabolism. Frontiers in Dental Medicine. 2023;4:1181817. doi: 10.3389/fdmed.2023.1181817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Itoh Y. Modulation of Microenvironment Signals by Proteolytic Shedding of Cell Surface Extracellular Matrix Receptors. Front Cell Dev Biol. 2021;9. Available from: https://pubmed.ncbi.nlm.nih.gov/34796172/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 74.Itoh Y. Discoidin domain receptors: Microenvironment sensors that promote cellular migration and invasion. Cell Adh Migr. 2018;12:378–85. Available from: https://pubmed.ncbi.nlm.nih.gov/29671358/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 75.Farzadi A, Renner T, Calomeni EP, Presley KF, Karn N, Lannutti J, et al. Modulation of biomimetic mineralization of collagen by soluble ectodomain of discoidin domain receptor 2. Mater Sci Eng C Mater Biol Appl. 2019;104. Available from: https://pubmed.ncbi.nlm.nih.gov/31499975/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 76.Ma R, Xie X, Zhao L, Wu Y, Wang J. Discoidin domain receptors (DDRs): Potential implications in periodontitis. J Cell Physiol. 2022;237:189–98. Available from: https://pubmed.ncbi.nlm.nih.gov/34431091/. Cited 2023 Apr 24. [DOI] [PubMed]
- 77.Sammon D, Hohenester E, Leitinger B. Two-step release of kinase autoinhibition in discoidin domain receptor 1. Proc Natl Acad Sci U S A. 2020;117:22051–60. doi: 10.1073/pnas.2007271117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fu HL, Valiathan RR, Arkwright R, Sohail A, Mihai C, Kumarasiri M, et al. Discoidin domain receptors: unique receptor tyrosine kinases in collagen-mediated signaling. J Biol Chem. 2013;288:7430–7. doi: 10.1074/jbc.R112.444158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shitomi Y, Thøgersen IB, Ito N, Leitinger B, Enghild JJ, Itoh Y. ADAM10 controls collagen signaling and cell migration on collagen by shedding the ectodomain of discoidin domain receptor 1 (DDR1) Mol Biol Cell. 2015;26:659–73. doi: 10.1091/mbc.E14-10-1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wu SC, Hsiao HF, Ho ML, Hung YL, Chang JK, Wang GJ, et al. Suppression of discoidin domain receptor 1 expression enhances the chondrogenesis of adipose-derived stem cells. Am J Physiol Cell Physiol. 2015;308:C685–96. doi: 10.1152/ajpcell.00398.2014. [DOI] [PubMed] [Google Scholar]
- 81.Chou LY, Chen CH, Lin YH, Chuang SC, Chou HC, Lin SY, et al. Discoidin domain receptor 1 regulates endochondral ossification through terminal differentiation of chondrocytes. FASEB J. 2020;34:5767–81. doi: 10.1096/fj.201901852RR. [DOI] [PubMed] [Google Scholar]
- 82.Mohamed FF, Ge C, Cowling RT, Lucas D, Hallett SA, Ono N, et al. The collagen receptor, discoidin domain receptor 2, functions in Gli1-positive skeletal progenitors and chondrocytes to control bone development. Bone Res. 2022;10. Available from: https://pubmed.ncbi.nlm.nih.gov/35140200/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 83.Yang H, Sun L, Cai W, Gu J, Xu D, Deb A, et al. DDR2, a discoidin domain receptor, is a marker of periosteal osteoblast and osteoblast progenitors. J Bone Miner Metab. 2020;38:670–7. doi: 10.1007/s00774-020-01108-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Xue F, Zhou W, Lan Z. The expression of two collagen receptor subfamilies, integrins and discoidin domains during osteogenic and chondrogenic differentiation of human mesenehymal stem cells. Biomed Mater Eng. 2021;32:195–205. doi: 10.3233/BME-201151. [DOI] [PubMed] [Google Scholar]
- 85.Sevic I, Vitale DL, Spinelli FM, Valenzuela Alvarez M, Gutiérrez L, Bolontrade MF, et al. The Hyaluronic Acid–CD44 Interaction in the Physio- and Pathological Stem Cell Niche. 2021;237–62. Available from: 10.1007/978-3-030-73453-4_10. Cited 2023 Apr 25.
- 86.Weng X, Maxwell-Warburton S, Hasib A, Ma L, Kang L. The membrane receptor CD44: novel insights into metabolism. Trends Endocrinol Metab. 2022;33:318–32. doi: 10.1016/j.tem.2022.02.002. [DOI] [PubMed] [Google Scholar]
- 87.Lyu J, Cheng C. Regulation of Alternative Splicing during Epithelial-Mesenchymal Transition. Cells Tissues Organs. 2022;211:238–51. doi: 10.1159/000518249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Naruse M, Shibasaki K, Yokoyama S, Kurachi M, Ishizaki Y. Dynamic changes of CD44 expression from progenitors to subpopulations of astrocytes and neurons in developing cerebellum. PLoS One . 2013;8. Available from: https://pubmed.ncbi.nlm.nih.gov/23308146/. cited 2023 Apr 25. [DOI] [PMC free article] [PubMed]
- 89.Zöller M. CD44, Hyaluronan, the Hematopoietic Stem Cell, and Leukemia-Initiating Cells. Front Immunol . 2015;6. Available from: https://pubmed.ncbi.nlm.nih.gov/26074915/. Cited 2023 Apr 25. [DOI] [PMC free article] [PubMed]
- 90.Mildmay-White A, Khan W. Cell Surface Markers on Adipose-Derived Stem Cells: A Systematic Review. Curr Stem Cell Res Ther. 2017;12. Available from: https://pubmed.ncbi.nlm.nih.gov/27133085/. Cited 2023 Apr 25. [DOI] [PubMed]
- 91.Williams K, Motiani K, Giridhar PV, Kasper S. CD44 integrates signaling in normal stem cell, cancer stem cell and (pre)metastatic niches. Exp Biol Med (Maywood). 2013;238:324–38. doi: 10.1177/1535370213480714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yu B, Sondag GR, Malcuit C, Kim MH, Safadi FF. Macrophage-Associated Osteoactivin/GPNMB Mediates Mesenchymal Stem Cell Survival, Proliferation, and Migration Via a CD44-Dependent Mechanism. J Cell Biochem. 2016;117:1511–21. doi: 10.1002/jcb.25394. [DOI] [PubMed] [Google Scholar]
- 93.Ouhtit A, Thouta R, Zayed H, Gaur RL, Fernando A, Rahman M, et al. CD44 mediates stem cell mobilization to damaged lung via its novel transcriptional targets, Cortactin and Survivin. Int J Med Sci. 2020;17:103–11. doi: 10.7150/ijms.33125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Baron R, Kneissel M. WNT signaling in bone homeostasis and disease: from human mutations to treatments. Nature Medicine. 2013;2013(19):179–92. doi: 10.1038/nm.3074. [DOI] [PubMed] [Google Scholar]
- 95.Wu SC, Chen CH, Wang JY, Lin YS, Chang JK, Ho ML. Hyaluronan size alters chondrogenesis of adipose-derived stem cells via the CD44/ERK/SOX-9 pathway. Acta Biomater. 2018;66:224–37. doi: 10.1016/j.actbio.2017.11.025. [DOI] [PubMed] [Google Scholar]
- 96.Xu Y, Wang YQ, Wang AT, Yu CY, Luo Y, Liu RM, et al. Effect of CD44 on differentiation of human amniotic mesenchymal stem cells into chondrocytes via Smad and ERK signaling pathways. Mol Med Rep. 2020;21:2357–66. doi: 10.3892/mmr.2020.11044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xu Y, Wang AT, Xiao JH. CD44 mediates hyaluronan to promote the differentiation of human amniotic mesenchymal stem cells into chondrocytes. Biotechnol Lett. 2023;45:411–22. doi: 10.1007/s10529-022-03322-2. [DOI] [PubMed] [Google Scholar]
- 98.Grishko V, Xu M, Ho R, Mates A, Watson S, Kim JT, et al. Effects of hyaluronic acid on mitochondrial function and mitochondria-driven apoptosis following oxidative stress in human chondrocytes. J Biol Chem. 2009;284:9132–9. doi: 10.1074/jbc.M804178200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Peall IW, Okolicsanyi RK, Griffiths LR, Haupt LM. Three-Dimensional Human Neural Stem Cell Models to Mimic Heparan Sulfate Proteoglycans and the Neural Niche. Semin Thromb Hemost. 2021;47:308–15. doi: 10.1055/s-0041-1724117. [DOI] [PubMed] [Google Scholar]
- 100.Okolicsanyi RK, Oikari LE, Yu C, Haupt LM. Proteoglycans, Neurogenesis and Stem Cell Differentiation. 2021;111–52. Available from: 10.1007/978-3-030-73453-4_6. Cited 2023 Apr 26.
- 101.Mii Y, Takada S. Heparan Sulfate Proteoglycan Clustering in Wnt Signaling and Dispersal. Front Cell Dev Biol. 2020;8. Available from: https://pubmed.ncbi.nlm.nih.gov/32760727/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 102.Jang B, Jung H, Hong H, Oh ES. Syndecan transmembrane domain modulates intracellular signaling by regulating the oligomeric status of the cytoplasmic domain. Cell Signal. 2018;52:121–6. doi: 10.1016/j.cellsig.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 103.Kim JM, Lee K, Kim MY, Shin HI, Jeong D. Suppressive effect of syndecan ectodomains and N-desulfated heparins on osteoclastogenesis via direct binding to macrophage-colony stimulating factor. Cell Death Dis. 2018;9. Available from: https://pubmed.ncbi.nlm.nih.gov/30389911/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 104.Gondelaud F, Ricard-Blum S. Structures and interactions of syndecans. FEBS J. 2019;286:2994–3007. doi: 10.1111/febs.14828. [DOI] [PubMed] [Google Scholar]
- 105.Jones FK, Kehoe O, Daroszewska A, van’t Hof RJ, Pisconti A. Syndecan-3: A Signaling Conductor in the Musculoskeletal System. 2021;153–77. Available from: 10.1007/978-3-030-73453-4_7. Cited 2023 Apr 26.
- 106.Afratis NA, Nikitovic D, Multhaupt HAB, Theocharis AD, Couchman JR, Karamanos NK. Syndecans - key regulators of cell signaling and biological functions. FEBS J. 2017;284:27–41. doi: 10.1111/febs.13940. [DOI] [PubMed] [Google Scholar]
- 107.Wang Q, Yang L, Alexander C, Temple S. The niche factor syndecan-1 regulates the maintenance and proliferation of neural progenitor cells during mammalian cortical development. PLoS One. 2012;7. Available from: https://pubmed.ncbi.nlm.nih.gov/22936997/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 108.Yu C, Peall IW, Pham SH, Okolicsanyi RK, Griffiths LR, Haupt LM. Syndecan-1 Facilitates the Human Mesenchymal Stem Cell Osteo-Adipogenic Balance. International Journal of Molecular Sciences. 2020;21:3884. doi: 10.3390/ijms21113884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mansouri R, Jouan Y, Hay E, Blin-Wakkach C, Frain M, Ostertag A, et al. Osteoblastic heparan sulfate glycosaminoglycans control bone remodeling by regulating Wnt signaling and the crosstalk between bone surface and marrow cells. Cell Death Dis. 2017;8. Available from: https://pubmed.ncbi.nlm.nih.gov/28661485/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 110.Johnson de Sousa Brito FM, Butcher A, Pisconti A, Poulet B, Prior A, Charlesworth G, et al. Syndecan-3 enhances anabolic bone formation through WNT signaling. FASEB J. 2021;35. Available from: https://pubmed.ncbi.nlm.nih.gov/33769615/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 111.Filmus J. Glypicans, 35 years later. Proteoglycan Research. 2023;1:e5. doi: 10.1002/pgr2.5. [DOI] [Google Scholar]
- 112.Traister A, Shi W, Filmus J. Mammalian Notum induces the release of glypicans and other GPI-anchored proteins from the cell surface. Biochem J. 2008;410:503–11. doi: 10.1042/BJ20070511. [DOI] [PubMed] [Google Scholar]
- 113.Song HH, Shi W, Xiang YY, Filmus J. The loss of glypican-3 induces alterations in Wnt signaling. J Biol Chem. 2005;280:2116–25. doi: 10.1074/jbc.M410090200. [DOI] [PubMed] [Google Scholar]
- 114.Shi W, Kaneiwa T, Cydzik M, Gariepy J, Filmus J. Glypican-6 stimulates intestinal elongation by simultaneously regulating Hedgehog and non-canonical Wnt signaling. Matrix Biol. 2020;88:19–32. doi: 10.1016/j.matbio.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 115.Capurro MI, Xu P, Shi W, Li F, Jia A, Filmus J. Glypican-3 inhibits Hedgehog signaling during development by competing with patched for Hedgehog binding. Dev Cell. 2008;14:700–11. doi: 10.1016/j.devcel.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 116.González-Guede I, López-Ramos M, Rodriguez LR, Abasolo L, Fernandez B. POS0409 Implication Of Glypicans And Notum In Bone Marrow Mesenchymal Stromal Cells During Osteogenic Differentiation In Osteoarthritic Disease. Ann Rheum Dis. 2023;82:459–60. [Google Scholar]
- 117.Russo D, Capolupo L, Loomba JS, Sticco L, D’Angelo G. Glycosphingolipid metabolism in cell fate specification. J Cell Sci. 2018;131. Available from: 10.1242/jcs.219204. Cited 2023 Jul 20. [DOI] [PubMed]
- 118.Liang YJ. Glycosphingolipids in human embryonic stem cells and breast cancer stem cells, and potential cancer therapy strategies based on their structures and functions. Glycoconjugate J. 2022;39(2):177–95. doi: 10.1007/s10719-021-10032-w. [DOI] [PubMed] [Google Scholar]
- 119.D’Angelo G, Capasso S, Sticco L, Russo D. Glycosphingolipids: synthesis and functions. FEBS J. 2013;280:6338–53. doi: 10.1111/febs.12559. [DOI] [PubMed] [Google Scholar]
- 120.Santilli F, Fabrizi J, Pulcini F, Santacroce C, Sorice M, Delle Monache S, et al. Gangliosides and Their Role in Multilineage Differentiation of Mesenchymal Stem Cells. Biomedicines. 2022;10:3112. doi: 10.3390/biomedicines10123112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hohenwallner K, Troppmair N, Panzenboeck L, Kasper C, El Abiead Y, Koellensperger G, et al. Decoding Distinct Ganglioside Patterns of Native and Differentiated Mesenchymal Stem Cells by a Novel Glycolipidomics Profiling Strategy. JACS Au. 2022;2:2466–80. doi: 10.1021/jacsau.2c00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Aprile D, Alessio N, Squillaro T, Di Bernardo G, Peluso G, Galderisi U. Role of glycosphingolipid SSEA-3 and FGF2 in the stemness and lineage commitment of multilineage differentiating stress enduring (MUSE) cells. Cell Prolif. 2023;56. Available from: https://pubmed.ncbi.nlm.nih.gov/36225120/. Cited 2023 Jul 21. [DOI] [PMC free article] [PubMed]
- 123.Aprile D, Alessio N, Demirsoy IH, Squillaro T, Peluso G, Di Bernardo G, et al. Muse stem cells can be isolated from stromal compartment of mouse bone marrow, adipose tissue, and ear connective tissue: A comparative study of their in vitro properties. Cells. 2021;10:761. doi: 10.3390/cells10040761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ryu JS, Seo SY, Jeong EJ, Kim JY, Koh YG, Kim Y Il, et al. Ganglioside GM3 Up-Regulate Chondrogenic Differentiation by Transform Growth Factor Receptors. International Journal of Molecular Sciences 2020, Vol 21, Page 1967. 2020;21:1967. Available from: https://www.mdpi.com/1422-0067/21/6/1967/htm. Cited 2023 Jul 21. [DOI] [PMC free article] [PubMed]
- 125.Szczot M, Pogorzala LA, Solinski HJ, Young L, Yee P, Le Pichon CE, et al. Cell-Type-Specific Splicing of Piezo2 Regulates Mechanotransduction. Cell Rep. 2017;21:2760–71. doi: 10.1016/j.celrep.2017.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ji C, McCulloch CA. TRPV4 integrates matrix mechanosensing with Ca2+ signaling to regulate extracellular matrix remodeling. FEBS J. 2021;288:5867–87. doi: 10.1111/febs.15665. [DOI] [PubMed] [Google Scholar]
- 127.Samanta A, Hughes TET, Moiseenkova-Bell VY. Transient Receptor Potential (TRP) Channels. Subcell Biochem. 2018;87:141–65. doi: 10.1007/978-981-10-7757-9_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hasan R, Zhang X. Ca2+ Regulation of TRP Ion Channels. Int J Mol Sci. 2018;19. Available from: https://pubmed.ncbi.nlm.nih.gov/29690581/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 129.Qin L, He T, Chen S, Yang D, Yi W, Cao H, et al. Roles of mechanosensitive channel Piezo1/2 proteins in skeleton and other tissues. Bone Res. 2021;9. Available from: https://pubmed.ncbi.nlm.nih.gov/34667178/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 130.Djamgoz MBA, Pchelintseva E. Mechanosensitive Ion Channels and Stem Cell Differentiation. Bioelectricity. 2021;3:249–254. [Google Scholar]
- 131.Wang L, Zhou H, Zhang M, Liu W, Deng T, Zhao Q, et al. Structure and mechanogating of the mammalian tactile channel PIEZO2. Nature. 2019;573:225–9. doi: 10.1038/s41586-019-1505-8. [DOI] [PubMed] [Google Scholar]
- 132.Gnanasambandam R, Bae C, Gottlieb PA, Sachs F. Ionic Selectivity and Permeation Properties of Human PIEZO1 Channels. PLoS One. 2015;10. Available from: https://pubmed.ncbi.nlm.nih.gov/25955826/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 133.Zhao Q, Wu K, Geng J, Chi S, Wang Y, Zhi P, et al. Ion Permeation and Mechanotransduction Mechanisms of Mechanosensitive Piezo Channels. Neuron. 2016;89:1248–63. doi: 10.1016/j.neuron.2016.01.046. [DOI] [PubMed] [Google Scholar]
- 134.Fang XZ, Zhou T, Xu JQ, Wang YX, Sun MM, He YJ, et al. Structure, kinetic properties and biological function of mechanosensitive Piezo channels. Cell Biosci. 2021;11. Available from: https://pubmed.ncbi.nlm.nih.gov/33422128/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 135.Zhao Q, Zhou H, Chi S, Wang Y, Wang J, Geng J, et al. Structure and mechanogating mechanism of the Piezo1 channel. Nature. 2018;554:487–92. doi: 10.1038/nature25743. [DOI] [PubMed] [Google Scholar]
- 136.Gilchrist CL, Leddy HA, Kaye L, Case ND, Rothenberg KE, Little D, et al. TRPV4-mediated calcium signaling in mesenchymal stem cells regulates aligned collagen matrix formation and vinculin tension. Proc Natl Acad Sci U S A. 2019;116:1992–7. doi: 10.1073/pnas.1811095116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wang L, You X, Lotinun S, Zhang L, Wu N, Zou W. Mechanical sensing protein PIEZO1 regulates bone homeostasis via osteoblast-osteoclast crosstalk. Nat Commun. 2020;11. Available from: https://pubmed.ncbi.nlm.nih.gov/31941964/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 138.Zhou T, Gao B, Fan Y, Liu Y, Feng S, Cong Q, et al. Piezo1/2 mediate mechanotransduction essential for bone formation through concerted activation of NFAT-YAP1-ß-catenin. Elife. 2020;9. Available from: https://pubmed.ncbi.nlm.nih.gov/32186512/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 139.He L, Ahmad M, Perrimon N. Mechanosensitive channels and their functions in stem cell differentiation. Exp Cell Res. 2019;374:259–65. doi: 10.1016/j.yexcr.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 140.Kao TW, Liu YS, Yang CY, Lee O. Mechanotransduction of mesenchymal stem cells and hemodynamic implications. Chinese J Physiology. 2023;66:55. doi: 10.4103/cjop.CJOP-D-22-00144. [DOI] [PubMed] [Google Scholar]
- 141.Rosa AL, Kato RB, Castro Raucci LMS, Teixeira LN, De Oliveira FS, Bellesini LS, et al. Nanotopography drives stem cell fate toward osteoblast differentiation through α1β1 integrin signaling pathway. J Cell Biochem. 2014;115:540–8. Available from: https://pubmed.ncbi.nlm.nih.gov/24122940/. Cited 2023 Apr 25. [DOI] [PubMed]
- 142.Boyan BD. Fluid Shear Stress Inhibits Differentiation of Growth Plate Chondrocytes, Partially Via Integrin Beta 1. Curr Trends Biomed Eng Biosci. 2017;3.
- 143.Zhu Y Sen, Zhang JN, Mo TT, Jiang C, Ma RC, Chen L. Discoidin domain receptor 2 activation of p38 mitogen-activated protein kinase as an important pathway for osteonectin-regulating osteoblast mineralization. J Orthop Surg Res. 2021;16. Available from: https://pubmed.ncbi.nlm.nih.gov/34876214/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 144.Muramatsu S, Wakabayashi M, Ohno T, Amano K, Ooishi R, Sugahara T, et al. Functional gene screening system identified TRPV4 as a regulator of chondrogenic differentiation. J Biol Chem. 2007;282:32158–67. Available from: https://pubmed.ncbi.nlm.nih.gov/17804410/. Cited 2023 Apr 26. [DOI] [PubMed]
- 145.Lee H pyo, Stowers R, Chaudhuri O. Volume expansion and TRPV4 activation regulate stem cell fate in three-dimensional microenvironments. Nat Commun. 2019;10. Available from: https://pubmed.ncbi.nlm.nih.gov/30705265/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 146.Hou W, Fu H, Liu X, Duan K, Lu X, Lu M, et al. Cation Channel Transient Receptor Potential Vanilloid 4 Mediates Topography-Induced Osteoblastic Differentiation of Bone Marrow Stem Cells. ACS Biomater Sci Eng. 2019;5:6520–9. Available from: https://pubmed.ncbi.nlm.nih.gov/33417804/. Cited 2023 Apr 26. [DOI] [PubMed]
- 147.Dhavalikar P, Robinson A, Lan Z, Jenkins D, Chwatko M, Salhadar K, et al. Review of Integrin-Targeting Biomaterials in Tissue Engineering. Adv Healthc Mater. 2020;9. Available from: https://pubmed.ncbi.nlm.nih.gov/32940020/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 148.Bhowmick S, D’Mello V, Caruso D, Wallerstein A, Abdul-Muneer PM. Impairment of pericyte-endothelium crosstalk leads to blood-brain barrier dysfunction following traumatic brain injury. Exp Neurol. 2019;317:260–70. doi: 10.1016/j.expneurol.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 149.Nakamura K, Ikeuchi T, Nara K, Rhodes CS, Zhang P, Chiba Y, et al. Perlecan regulates pericyte dynamics in the maintenance and repair of the blood-brain barrier. J Cell Biol. 2019;218:3506–25. doi: 10.1083/jcb.201807178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lygoe KA, Norman JT, Marshall JF, Lewis MP. αv integrins play an important role in myofibroblast differentiation. Wound Repair and Regeneration. 2004;12:461–70. doi: 10.1111/j.1067-1927.2004.12402.x. [DOI] [PubMed] [Google Scholar]
- 151.Asano Y, Ihn H, Yamane K, Jinnin M, Tamaki K. Increased expression of integrin αvβ5 induces the myofibroblastic differentiation of dermal fibroblasts. American Journal of Pathology. 2006;168:499–510. doi: 10.2353/ajpath.2006.041306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kim KK, Wei Y, Szekeres C, Kugler MC, Wolters PJ, Hill ML, et al. Epithelial cell α3β1 integrin links β-catenin and Smad signaling to promote myofibroblast formation and pulmonary fibrosis. J Clin Invest. 2009;119:213–24. doi: 10.1172/JCI36940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhao J, Santino F, Giacomini D, Gentilucci L. Integrin-Targeting Peptides for the Design of Functional Cell-Responsive Biomaterials. Biomedicines. 2020;8:307. doi: 10.3390/biomedicines8090307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bilem I, Plawinski L, Chevallier P, Ayela C, Sone ED, Laroche G, et al. The spatial patterning of RGD and BMP-2 mimetic peptides at the subcellular scale modulates human mesenchymal stem cells osteogenesis. J Biomed Mater Res A. 2018;106:959–70. doi: 10.1002/jbm.a.36296. [DOI] [PubMed] [Google Scholar]
- 155.Bilem I, Chevallier P, Plawinski L, Sone ED, Durrieu MC, Laroche G. Interplay of Geometric Cues and RGD/BMP-2 Crosstalk in Directing Stem Cell Fate. ACS Biomater Sci Eng. 2017;3:2514–23. doi: 10.1021/acsbiomaterials.7b00279. [DOI] [PubMed] [Google Scholar]
- 156.Clark AY, Martin KE, García JR, Johnson CT, Theriault HS, Han WM, et al. Integrin-specific hydrogels modulate transplanted human bone marrow-derived mesenchymal stem cell survival, engraftment, and reparative activities. Nature Communications. 2020;11:1–14. doi: 10.1038/s41467-019-14000-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kolambkar YM, Bajin M, Wojtowicz A, Hutmacher DW, García AJ, Guldberg RE. Nanofiber Orientation and Surface Functionalization Modulate Human Mesenchymal Stem Cell Behavior In Vitro. 2013;20:398–409. doi: 10.1089/ten.tea.2012.0426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Malcor JD, Mallein-Gerin F. Biomaterial functionalization with triple-helical peptides for tissue engineering. Acta Biomater. 2022;148:1–21. doi: 10.1016/j.actbio.2022.06.003. [DOI] [PubMed] [Google Scholar]
- 159.Hayuningtyas RA, Han M, Choi S, Kwak MS, Park IH, Lee JH, et al. The collagen structure of C1q induces wound healing by engaging discoidin domain receptor 2. Mol Med. 2021;27. Available from: https://pubmed.ncbi.nlm.nih.gov/34602056/. Cited 2023 Apr 24. [DOI] [PMC free article] [PubMed]
- 160.Binrayes A, Ge C, Mohamed FF, Franceschi RT. Role of Discoidin Domain Receptor 2 in Craniofacial Bone Regeneration. J Dent Res. 2021;100:1359–66. doi: 10.1177/00220345211007447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ge C, Li Y, Wu F, Ma P, Franceschi RT. Synthetic peptides activating discoidin domain receptor 2 and collagen-binding integrins cooperate to stimulate osteoblast differentiation of skeletal progenitor cells. Acta Biomater. 2023;166:109–118. doi: 10.1016/j.actbio.2023.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhu J, Quan H. Adipose-derived stem cells-derived exosomes facilitate cutaneous wound healing by delivering XIST and restoring discoidin domain receptor 2. Cytokine. 2022;158:155981. doi: 10.1016/j.cyto.2022.155981. [DOI] [PubMed] [Google Scholar]
- 163.Burdick JA, Chung C. Influence of Three-Dimensional Hyaluronic Acid Microenvironments on Mesenchymal Stem Cell Chondrogenesis. 2008;15:243–54. doi: 10.1089/ten.tea.2008.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Bian L, Guvendiren M, Mauck RL, Burdick JA. Hydrogels that mimic developmentally relevant matrix and N-cadherin interactions enhance MSC chondrogenesis. Proc Natl Acad Sci U S A. 2013;110:10117–22. doi: 10.1073/pnas.1214100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Luo Y, Liang F, Wan X, Liu S, Fu L, Mo J, et al. Hyaluronic Acid Facilitates Angiogenesis of Endothelial Colony Forming Cell Combining With Mesenchymal Stem Cell via CD44/ MicroRNA-139-5p Pathway. Front Bioeng Biotechnol. 2022;10:794037. doi: 10.3389/fbioe.2022.794037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Guo M, Xu J, Zhao S, Shen D, Jiang W, Zhang L, et al. Suppressing Syndecan-1 Shedding to Protect Against Renal Ischemia/Reperfusion Injury by Maintaining Polarity of Tubular Epithelial Cells. Shock. 2022;57:256–63. doi: 10.1097/SHK.0000000000001838. [DOI] [PubMed] [Google Scholar]
- 167.Pisconti A, Banks GB, Babaeijandaghi F, Betta ND, Rossi FMV, Chamberlain JS, et al. Loss of niche-satellite cell interactions in syndecan-3 null mice alters muscle progenitor cell homeostasis improving muscle regeneration. Skelet Muscle. 2016;6. Available from: https://pubmed.ncbi.nlm.nih.gov/27757223/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 168.Chung H, Multhaupt HAB, Oh ES, Couchman JR. Minireview: Syndecans and their crucial roles during tissue regeneration. FEBS Lett. 2016;590:2408–17. doi: 10.1002/1873-3468.12280. [DOI] [PubMed] [Google Scholar]
- 169.Bertrand J, Stange R, Hidding H, Echtermeyer F, Nalesso G, Godmann L, et al. Syndecan 4 supports bone fracture repair, but not fetal skeletal development, in mice. Arthritis Rheum. 2013;65:743–52. doi: 10.1002/art.37817. [DOI] [PubMed] [Google Scholar]
- 170.Rønning SB, Carlson CR, Aronsen JM, Pisconti A, Høst V, Lunde M, et al. Syndecan-4-/- Mice Have Smaller Muscle Fibers, Increased Akt/mTOR/S6K1 and Notch/HES-1 Pathways, and Alterations in Extracellular Matrix Components. Front Cell Dev Biol. 2020;8. Available from: https://pubmed.ncbi.nlm.nih.gov/32850844/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 171.Jin Z, Ren J, Qi S. Exosomal miR-9–5p secreted by bone marrow–derived mesenchymal stem cells alleviates osteoarthritis by inhibiting syndecan-1. Cell Tissue Res. 2020;381:99–114. doi: 10.1007/s00441-020-03193-x. [DOI] [PubMed] [Google Scholar]
- 172.Jones FK, Stefan A, Kay AG, Hyland M, Morgan R, Forsyth NR, et al. Syndecan-3 regulates MSC adhesion, ERK and AKT signalling in vitro and its deletion enhances MSC efficacy in a model of inflammatory arthritis in vivo. Scientific Reports. 2020;10:1–10. doi: 10.1038/s41598-020-77514-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Tan X, Jain E, Barcellona MN, Morris E, Neal S, Gupta MC, et al. Integrin and syndecan binding peptide-conjugated alginate hydrogel for modulation of nucleus pulposus cell phenotype. Biomaterials. 2021;277:121113. doi: 10.1016/j.biomaterials.2021.121113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Schneider JS. GM1 Ganglioside as a Disease-Modifying Therapeutic for Parkinson’s Disease: A Multi-Functional Glycosphingolipid That Targets Multiple Parkinson’s Disease-Relevant Pathogenic Mechanisms. International Journal of Molecular Sciences. 2023;24:9183. doi: 10.3390/ijms24119183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Naito S, Nakayama K, Kawashima N. Enhanced Levels of Glycosphingolipid GM3 Delay the Progression of Diabetic Nephropathy. International Journal of Molecular Sciences. 2023;24:11355. doi: 10.3390/ijms241411355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Saraswathibhatla A, Indana D, Chaudhuri O. Cell–extracellular matrix mechanotransduction in 3D. Nature Reviews Molecular Cell Biology. 2023;24(7):495–516. doi: 10.1038/s41580-023-00583-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lee H pyo, Stowers R, Chaudhuri O. Volume expansion and TRPV4 activation regulate stem cell fate in three-dimensional microenvironments. Nat Commun. 2019;10. Available from: https://pubmed.ncbi.nlm.nih.gov/30705265/. Cited 2023 Jul 20. [DOI] [PMC free article] [PubMed]
- 178.Phutane P, Telange D, Agrawal S, Gunde M, Kotkar K, Pethe A. Biofunctionalization and Applications of Polymeric Nanofibers in Tissue Engineering and Regenerative Medicine. Polymers. 2023;15:1202. doi: 10.3390/polym15051202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zhang Y, Zhang C, Li Y, Zhou L, Dan N, Min J, et al. Evolution of biomimetic ECM scaffolds from decellularized tissue matrix for tissue engineering: A comprehensive review. Int J Biol Macromol. 2023;246:125672. doi: 10.1016/j.ijbiomac.2023.125672. [DOI] [PubMed] [Google Scholar]
- 180.Magno V, Werner C. Tissue-Derived Decellularized Materials for Biomedical Applications. Handbook of the Extracellular Matrix. 2023;1–33. Available from: 10.1007/978-3-030-92090-6_42-1. Cited 2023 Jul 20.
- 181.Novoseletskaya E, Grigorieva O, Nimiritsky P, Basalova N, Eremichev R, Milovskaya I, et al. Mesenchymal Stromal Cell-Produced Components of Extracellular Matrix Potentiate Multipotent Stem Cell Response to Differentiation Stimuli. Front Cell Dev Biol. 2020;8:555378. doi: 10.3389/fcell.2020.555378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Kojima H, Kushige H, Yagi H, Nishijima T, Moritoki N, Nagoshi N, et al. Combinational Treatment Involving Decellularized Extracellular Matrix Hydrogels With Mesenchymal Stem Cells Increased the Efficacy of Cell Therapy in Pancreatitis. Cell Transplant. 2023;32. Available from: 10.1177/09636897231170437. Cited 2023 Jul 20. [DOI] [PMC free article] [PubMed]
- 183.Zhang X, Wang B, Hong H, Wang Y, Liu J, Liu C, et al. Decellularized extracellular matrix and mesenchymal stem cells promote recovery in traumatic brain injury by synergistically enhancing neurogenesis and attenuating neuroinflammation. J Mater Sci Technol. 2023;138:17–28. [Google Scholar]
- 184.Parnes N, Bartoszewski NR, Defranco MJ. Arthroscopic repair of full-thickness rotator cuff tears in active patients younger than 40 years: 2- To 5-year clinical outcomes. Orthopedics. 2018;41:e52–e57. doi: 10.3928/01477447-20171114-02. [DOI] [PubMed] [Google Scholar]
- 185.Omidi E, Fuetterer L, Reza Mousavi S, Armstrong RC, Flynn LE, Samani A. Characterization and assessment of hyperelastic and elastic properties of decellularized human adipose tissues. J Biomech. 2014;47:3657–3663. doi: 10.1016/j.jbiomech.2014.09.035. [DOI] [PubMed] [Google Scholar]
- 186.Wu I, Nahas Z, Kimmerling KA, Rosson GD, Elisseeff JH. An injectable adipose matrix for soft-tissue reconstruction. Plast Reconstr Surg. 2012;129:1247–1257. doi: 10.1097/PRS.0b013e31824ec3dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Hastings JF, Skhinas JN, Fey D, Croucher DR, Cox TR. The extracellular matrix as a key regulator of intracellular signalling networks. Br J Pharmacol. 2019;176.1:82–92. Available from: https://bpspubs.onlinelibrary.wiley.com/doi/full/10.1111/bph.14195. [DOI] [PMC free article] [PubMed]
- 188.Ali M, Ribeiro MM, del Sol A. Computational Methods to Identify Cell-Fate Determinants, Identity Transcription Factors, and Niche-Induced Signaling Pathways for Stem Cell Research. Methods Mol Biol. 2022;2471:83–109. doi: 10.1007/978-1-0716-2193-6_4. [DOI] [PubMed] [Google Scholar]
- 189.Hetmanski JHR, Schwartz JM, Caswell PT. Modelling GTPase dynamics to understand RhoA-driven cancer cell invasion. Biochem Soc Trans. 2016;44:1695–700. doi: 10.1042/BST20160184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Zaidel-Bar R, Itzkovitz S, Ma’ayan A, Iyengar R, Geiger B. Functional atlas of the integrin adhesome. Nat Cell Biol. 2007;9:858–67. Available from: https://pubmed.ncbi.nlm.nih.gov/17671451/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 191.Dong JM, Tay FPL, Swa HLF, Gunaratne J, Leung T, Burke B, et al. Proximity biotinylation provides insight into the molecular composition of focal adhesions at the nanometer scale. Sci Signal. 2016;9. Available from: https://pubmed.ncbi.nlm.nih.gov/27303058/. Cited 2023 Apr 26. [DOI] [PubMed]
- 192.Horton ER, Byron A, Askari JA, Ng DHJ, Millon-Frémillon A, Robertson J, et al. Definition of a consensus integrin adhesome and its dynamics during adhesion complex assembly and disassembly. Nat Cell Biol. 2015;17:1577–87. doi: 10.1038/ncb3257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Clerc O, Deniaud M, Vallet SD, Naba A, Rivet A, Perez S, et al. MatrixDB: integration of new data with a focus on glycosaminoglycan interactions. Nucleic Acids Res. 2019;47:D376–81. doi: 10.1093/nar/gky1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Shao X, Gomez CD, Kapoor N, Considine JM, Grams C, Gao YT, Matrisome, et al. updates to the ECM-protein knowledge database. Nucleic Acids Res. 2023;2023(51):D1519–30. doi: 10.1093/nar/gkac1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kontio J, Soñora VR, Pesola V, Lamba R, Dittmann A, Navarro AD, et al. Analysis of extracellular matrix network dynamics in cancer using the MatriNet database. Matrix Biol. 2022;110:141–50. doi: 10.1016/j.matbio.2022.05.006. [DOI] [PubMed] [Google Scholar]
- 196.Szklarczyk D, Kirsch R, Koutrouli M, Nastou K, Mehryary F, Hachilif R, et al. The STRING database in 2023: protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 2023;51:D638–46. doi: 10.1093/nar/gkac1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Licata L, Briganti L, Peluso D, Perfetto L, Iannuccelli M, Galeota E, et al. MINT, the molecular interaction database: 2012 update. Nucleic Acids Res. 2012;40. Available from: https://pubmed.ncbi.nlm.nih.gov/22096227/. Cited 2023 Apr 26. [DOI] [PMC free article] [PubMed]
- 198.Barzegari A, Omidi Y, Ostadrahimi A, Gueguen V, Meddahi-Pellé A, Nouri M, et al. The role of Piezo proteins and cellular mechanosensing in tuning the fate of transplanted stem cells. Cell Tissue Res. 2020;381. Available from: https://pubmed.ncbi.nlm.nih.gov/32215723/. Cited 2023 Apr 26. [DOI] [PubMed]
- 199.Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Gillespie M, Jassal B, Stephan R, Milacic M, Rothfels K, Senff-Ribeiro A, et al. The reactome pathway knowledgebase 2022. Nucleic Acids Res. 2022;50:D687–92. doi: 10.1093/nar/gkab1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Kyriakopoulou K, Piperigkou Z, Tzaferi K, Karamanos NK. Trends in extracellular matrix biology. Mol Biol Rep. 2023;50:853–63. doi: 10.1007/s11033-022-07931-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Fig. 1_Supplement. Predicting the integrin β1 PPIs networks for signal transduction molecules before (A) and after (B) excluded data obtained from cancer cells.
Additional file 2: Fig. 2_Supplement. Illustration of contributing factors of the signaling pathway for integrin β1 (A), CD44 (B), and DDR1 (C), which generated using ReactomeFIPlugIn in Cytoscape. The obtained results are presented as Reactfoam using a false discovery rate (FDR) scalebar (p-value ranging from 0–0.05).
Additional file 3: Fig. 3_Supplement. Predicting the DDR1 signaling pathway members participate in semaphorin interactions (A), and regulate the activity of RUNX1, RUNX2, and RUNX3 transcription factors in the case of osteogenic differentiation (B).
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its supplementary information files].