Abstract
Objective
This study evaluated whether the hepatic steatosis index (HSI) at antineutrophil cytoplasmic antibody-associated vasculitis (AAV) diagnosis could forecast poor outcomes during the disease course in AAV patients.
Methods
This study included 260 AAV patients. The equation for HSI is as follows HSI=8×(alanine aminotransferase/aspartate aminotransferase)+body mass index+(2, diabetes mellitus)+(2, female). The cut-off of HSI was obtained using the receiver operating characteristic curve.
Results
The median age of the 260 patients was 59.5 years, and 65.0% were female. Among the continuous variables excluding the parameters composing the equation for HSI, HSI was significantly correlated with Birmingham vasculitis activity score, five-factor score, haemoglobin, blood urea nitrogen, serum creatinine, and total cholesterol. Among poor outcomes, the area under the curve of HSI for end-stage renal disease (ESRD) was significant, and the cut-off of HSI for ESRD was set at ≤30.82. AAV patients with HSI ≤30.82 exhibited a significantly higher risk of ESRD (relative risk 3.489) and a significantly lower cumulative ESRD-free survival rate than those with HSI >30.82.
Conclusion
This study is the first to demonstrate that HSI at AAV diagnosis could forecast ESRD during the disease course in AAV patients.
Keywords: Hepatic steatosis index, End-stage renal disease, Antineutrophil cytoplasmic antibody, Vasculitis, Forecasting
INTRODUCTION
Small vessel vasculitis is divided into two categories, antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) and immune complex vasculitis, in accordance with the 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides and the 2007 European Medicine Agency algorithm for the classification of AAV and polyarteritis nodosa [1,2]. The Birmingham vasculitis activity score (BVAS) has nine systemic and major organ-based items; however, an item of liver manifestation is not included in BVAS [3]. The five-factor score (FFS) and the vasculitis damage index are used for forecasting poor outcomes of AAV and evaluating major-organ damage owing to AAV, respectively. These two indices also do not include items related to liver manifestation [4,5]. In fact, serious and advanced liver damage in AAV patients, in particular, at the time of AAV diagnosis or in the early phase of AAV, has rarely been reported to date [6,7].
Meanwhile, apart from the liver involvement of AAV, several studies on the link between liver fibrosis-related indices and poor outcomes of AAV have been conducted [8-12]. These studies found that although AAV did not directly cause serious liver fibrosis, liver fibrosis-related indices at AAV diagnosis could forecast poor outcomes of AAV during the disease course. Recently, the hepatic steatosis index (HSI), an additional non-invasive index, was developed to evaluate the extent of liver fibrosis [13]. Furthermore, in addition to liver fibrosis, non-alcoholic fatty liver disease (NAFLD) can also be estimated by the range of HSI values [14,15]. Therefore, as in previous studies [12-15], it could be reasonably assumed that HSI at AAV diagnosis may forecast poor outcomes of AAV during the disease course; however, to date, there has been no study regarding the potential of HSI for forecasting poor outcomes of AAV. Hence, this study evaluated whether HSI at AAV diagnosis could forecast poor outcomes of AAV during the disease course in AAV patients.
MATERIALS AND METHODS
Patients
This study retrospectively screened 287 AAV patients by reviewing their medical records and included 260 patients in this study based on the inclusion criteria as follows: i) all patients met both the 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides and the 2007 European Medicine Agency algorithm for the classification of AAV [1,2]; ii) the first classification of AAV was made at this hospital from October 2000 to December 2021; iii) the electronic medical records were well-written sufficiently for collecting clinical, laboratory, radiological, and histological data [3,4]; iv) the parameters composing the equation for HSI were particularly included in clinical and laboratory data [13,14]; v) patients with the concurrent serious medical conditions mimicking AAV, such as malignancies and infectious diseases at AAV diagnosis, were excluded [9-12]; vi) the follow-up duration was more than three months after the AAV diagnosis; vii) AAV patients who have been exposed to glucocorticoids >20 mg (equivalent to prednisolone) or immunosuppressive drugs before the AAV diagnosis were excluded [9-12]; and viii) patients who took drugs that could provoke false positivity of ANCA, such as propylthiouracil and hydralazine, were also excluded [16].
Ethical disclosure
This study was approved by the Institutional Review Board (IRB) of Severance Hospital (Seoul, Korea, IRB No. 4-2020-1071) and was conducted in accordance with the Declaration of Helsinki. Given the retrospective design of the study and the use of anonymized patient data, the requirement for written informed consent was waived by the IRB.
Clinical data at the time of AAV diagnosis
The clinical and laboratory variables are described in Table 1. Demographic data included age, sex, and body mass index (BMI). AAV-related variables were presented as AAV subtype, ANCA type, and positivity and AAV-specific indices (BVAS and FFS). Diabetes mellitus (DM), hypertension, and dyslipidaemia were considered comorbidities. Data on acute-phase reactants, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) were also collected. Myeloperoxidase (MPO)-ANCA and proteinase 3 (PR3)-ANCA were measured using an immunoassay, whereas, perinuclear (P)-ANCA and cytoplasmic (C)-ANCA were assessed using an indirect immunofluorescence assay [17].
Table 1.
Characteristics of AAV patients at diagnosis and during follow-up (n=260)
| Variable | Value |
|---|---|
| At the time of diagnosis | |
| Demographic data | |
| Age (yr) | 59.5 (20.0) |
| Female sex (%) | 169 (65.0) |
| BMI (kg/m2) | 22.5 (4.2) |
| AAV subtype (%) | |
| MPA | 139 (53.5) |
| GPA | 69 (26.5) |
| EGPA | 52 (20.0) |
| ANCA type and positivity (%) | |
| MPO-ANCA (or P-ANCA) positivity | 174 (66.9) |
| PR3-ANCA (or C-ANCA) positivity | 46 (17.7) |
| Both ANCA positivity | 10 (3.8) |
| ANCA negativity | 50 (19.2) |
| AAV-specific indices | |
| BVAS | 12.0 (11.0) |
| FFS | 1.0 (1.5) |
| Comorbidities (%) | |
| DM | 66 (25.4) |
| Hypertension | 103 (39.6) |
| Dyslipidaemia | 50 (19.2) |
| Laboratory result | |
| White blood cell count (/mm3) | 9,110.0 (6,485.0) |
| Haemoglobin (g/dL) | 11.4 (3.7) |
| Platelet count (×1000/mm3) | 295.0 (164.0) |
| Fasting glucose (mg/dL) | 101.0 (33.8) |
| Blood urea nitrogen (mg/dL) | 17.7 (18.5) |
| Serum creatinine (mg/dL) | 0.9 (1.1) |
| Protein (g/dL) | 6.7 (1.1) |
| Serum albumin (g/dL) | 3.7 (1.1) |
| Acute phase reactant | |
| ESR (mm/hr) | 59.0 (74.0) |
| CRP (mg/L) | 13.8 (65.4) |
| Liver-related variable | |
| ALP (IU/L) | 73.0 (36.3) |
| AST (IU/L) | 18.0 (9.0) |
| ALT (IU/L) | 16.0 (14.0) |
| Total bilirubin (mg/dL) | 0.5 (0.3) |
| Cholesterol profile | |
| Total cholesterol (mg/dL) | 168.0 (65.0) |
| HSI-related variable | |
| ALT (IU/L) | 18.0 (9.0) |
| AST (IU/L) | 16.0 (14.0) |
| BMI (kg/m2) | 22.5 (4.2) |
| Female gender (%) | 169 (65.0) |
| DM (%) | 66 (25.4) |
| HSI | 31.4 (6.8) |
| During the follow-up duration | |
| Poor outcome (%) | |
| All-cause mortality | 33 (12.7) |
| Relapse | 82 (31.5) |
| CVA | 19 (7.3) |
| ACS | 11 (4.2) |
| ESRD | 42 (16.2) |
| Follow-up duration based on each poor outcomes (mon) | |
| All-cause mortality | 37.2 (65.4) |
| Relapse | 22.3 (44.2) |
| CVA | 33.7 (65.5) |
| ACS | 36.9 (65.6) |
| ESRD | 28.7 (60.9) |
| Medication (%) | |
| Glucocorticoids | 244 (93.8) |
| Cyclophosphamide | 145 (55.8) |
| Mycophenolate mofetil | 37 (14.2) |
| Azathioprine | 139 (53.5) |
| Tacrolimus | 22 (8.5) |
| Rituximab | 44 (16.9) |
| Methotrexate | 25 (9.6) |
Values are presented as a median (interquartile range) or number (%). AAV: ANCA-associated vasculitis, ANCA: antineutrophil cytoplasmic antibody, BMI: body mass index, MPA: microscopic polyangiitis, GPA: granulomatosis with polyangiitis, EGPA: eosinophilic granulomatosis with polyangiitis, MPO: myeloperoxidase, P: perinuclear, PR3: proteinase 3, C: cytoplasmic, BVAS: Birmingham vasculitis activity score, FFS: five-factor score, DM: diabetes mellitus, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, ALP: alkaline phosphatase, AST: aspartate aminotransferase, ALT: alanine aminotransferase, HSI: hepatic steatosis index, CVA: cerebrovascular accident, ACS: acute coronary syndrome, ESRD: end-stage renal disease.
Equation for HSI
The equation for HSI is as follows: HSI=8×(alanine aminotransferase [ALT]/aspartate aminotransferase [AST])+BMI+(2, DM)+(2, female) [13-15]. When HSI is less than 30, NAFLD can be ruled out [18].
Poor outcomes of AAV and Medications administered during the disease course
Five poor outcomes of AAV were assessed in this study including all-cause mortality, relapse, end-stage renal disease (ESRD), cerebrovascular accident (CVA), and acute coronary syndrome (ACS). For patients with each poor outcome, the follow-up duration based on each poor outcome was defined as the period between AAV diagnosis and each poor outcome occurrence. Conversely, for patients who did not have a poor outcome, it was defined as the period between AAV diagnosis and the last visit [9,10]. The number of patients who had taken glucocorticoids and immunosuppressive drugs during the disease course was counted.
Statistical analyses
All statistical analyses were performed using the SPSS Statistics for Windows version 26 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as medians with interquartile ranges, whereas categorical variables were expressed as numbers (percentages). The correlation coefficient (r) between the two variables was obtained using Pearson correlation analysis. The optimal cut-off was extrapolated using the receiver operating characteristic (ROC) curve analysis, and one value with the maximum sum of sensitivity and specificity was selected. The odds ratio (OR) of the cut-off for each poor outcome of AAV was analyzed using contingency tables and the chi-square test. A comparison of the cumulative survival rates between the two groups was performed using Kaplan-Meier survival analysis with the log-rank test. p<0.05 was considered statistically significant.
RESULTS
Characteristics of AAV patients at AAV diagnosis and during the disease course
In terms of the variables at AAV diagnosis, the median age of the patients was 59.5 years, and 65.0% were female. Among them, 139, 69, and 52 had microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA), and eosinophilic GPA (EGPA), respectively, and 103, 66, and 50 patients were diagnosed with concurrent hypertension, DM, and dyslipidaemia, respectively. The median BVAS, FFS, ESR, and CRP levels were 12.0, 1.0, 59.0 mm/h, and 13.8 mg/L, respectively. Regarding the parameters composing the equation for HSI, the median ALT, AST, and BMI were 18.0 IU/L, 16.0 IL/L, and 22.5 kg/m2, respectively, and finally, the median HSI was 31.4. The remaining clinical and laboratory data are presented in Table 1. Regarding the variables during the disease course, 33 of the 260 AAV patients died, and 82 patients experienced a relapse. Forty-two, 19, and 11 patients had ESRD, CVA, and ACS, respectively. Glucocorticoids were administered to 244 patients (93.8%); the most commonly administered immunosuppressive drug was cyclophosphamide (55.8%), followed by azathioprine (53.5%) (Table 1).
Correlation analysis of HSI with continuous variables
Among the continuous variables excluding the parameters composing the equation for HSI, HSI was significantly correlated with BVAS (r=–0.159), FFS (r=–0.168), haemoglobin (r=0.212), blood urea nitrogen (r=–0.141), serum creatinine (r=–0.174), and total cholesterol (r=0.141). Among the parameters comprising the equation for HSI, HSI was significantly correlated with BMI and ALT but not with AST (Table 2).
Table 2.
Correlation of HSI with continuous variables at diagnosis in AAV patients (n=260)
| Correlation coefficient (r) | p-value | |
|---|---|---|
| Age (yr) | −0.077 | 0.214 |
| BMI (kg/m2)* | 0.668 | <0.001 |
| BVAS | −0.159 | 0.010 |
| FFS | −0.168 | 0.007 |
| White blood cell count (/mm3) | −0.047 | 0.453 |
| Haemoglobin (g/dL) | 0.212 | 0.001 |
| Platelet count (×1,000/mm3) | −0.008 | 0.892 |
| Fasting glucose (mg/dL) | 0.103 | 0.097 |
| Blood urea nitrogen (mg/dL) | −0.141 | 0.023 |
| Serum creatinine (mg/dL) | −0.174 | 0.005 |
| Protein (g/dL) | −0.068 | 0.277 |
| Serum albumin (g/dL) | 0.085 | 0.172 |
| ESR (mm/h) | −0.080 | 0.198 |
| CRP (mg/L) | −0.001 | 0.987 |
| ALP (IU/L) | 0.118 | 0.057 |
| AST (IU/L)* | 0.076 | 0.223 |
| ALT (IU/L)* | 0.417 | <0.001 |
| Total bilirubin (mg/dL) | 0.064 | 0.303 |
| Total cholesterol (mg/dL) | 0.141 | 0.023 |
HSI: hepatic steatosis index, AAV: ANCA-associated vasculitis, BMI: body mass index, BVAS: Birmingham vasculitis activity score, FFS: five-factor score, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, ALP: alkaline phosphatase, AST: aspartate aminotransferase, ALT: alanine aminotransferase. *The parameters composing the equation for HSI=8×(ALT/AST)+BMI+2×(if female=1)+2×(if diabetes=1).
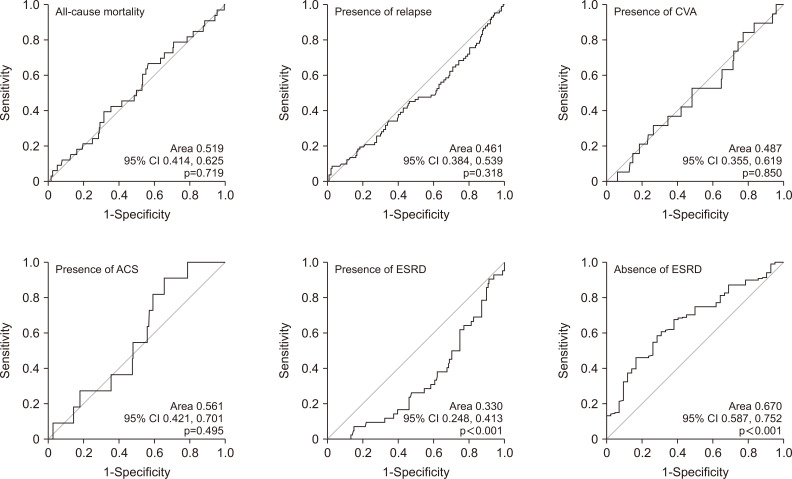
ROC curve analysis of HSI for each poor outcome
Among five poor outcomes of AAV, the area under the curve (AUC) of HSI for ESRD was statistically significant. According to the presence or absence of ESRD, the AUCs of the HSI were 0.330 (95% confidence interval [CI] 0.248, 0.413; p<0.001) and 0.670 (95% CI 0.587, 0.752; p<0.001), respectively. Since there was a tendency toward an inverse association between HSI at AAV diagnosis and progression to ESRD during the disease course, the latter of the two AUCs was selected and used to obtain the cut-off for forecasting progression to ESRD (Figure 1).
Fig. 1.
Receiver operator characteristic curve analysis. Among five poor outcomes of antineutrophil cytoplasmic antibody-associated vasculitis, only hepatic steatosis index (HIS) for ESRD showed statistical significance (area under the curve 0.333 for the presence of ESRD, p<0.001 and 0.670 for the absence of ESRD, p<0.001). The optimal cut-off of HSI for ESRD was set at ≤30.82. CI: confidence interval, CVA: cerebrovascular accident, ACS: acute coronary syndrome, ESRD: end-stage renal disease.
The relative risk of the cut-off of HSI for ESRD
When the optimal cut-off of HSI for progression to ESRD was set at ≤30.82, the sensitivity and specificity were 58.3% and 71.4%, respectively. When AAV patients were divided into two groups based on HSI ≤30.82, 121 and 139 patients belonged to a group of HSI ≤30.82 and a group of HSI >30.82, respectively. ESRD was identified more frequently in AAV patients with HSI ≤30.82 (30 of 121 patients [24.8%]) than in those with HSI >30.82 (12 of 139 patients [8.6%]) (p<0.001). Furthermore, AAV patients with HSI ≤30.82 exhibited a significantly higher risk of progression to ESRD than those with HSI >30.82 (OR 3.489, 95% CI 1.696, 7.179) (Figure 2).
Fig. 2.
Relative risk for ESRD. Antineutrophil cytoplasmic antibody-associated vasculitis patients with HSI ≤30.82 exhibited a significantly higher risk of progression to ESRD than those with HSI >30.82. ESRD: end-stage renal disease, HSI: hepatic steatosis index.
Comparison of cumulative ESRD-free survival rates
AAV patients with HSI ≤30.82 exhibited a significantly lower cumulative ESRD-free survival rate than those with HSI >30.82 (p=0.001) (Figure 3).
Fig. 3.
Cumulative ESRD-free survival rates. Antineutrophil cytoplasmic antibody-associated vasculitis patients with HSI ≤30.82 exhibited a significantly lower cumulative ESRD-free survival rate than those with HSI >30.82 (p=0.001). ESRD: end-stage renal disease, HSI: hepatic steatosis index.
DISCUSSION
In this study, we investigated whether HSI, an index for estimating the extent of hepatic steatosis and the presence of NAFLD, could forecast poor outcomes of AAV in AAV patients, and obtained several new findings [18]. First, HSI was inversely correlated with BVAS, FFS, and serum creatinine levels. Second, HSI exhibited the potential for forecasting ESRD in AAV patients. Third, when the cut-off of HSI for ESRD was set at 30.82, AAV patients with HSI ≤30.82 exhibited a significantly higher risk for ESRD than those with HSI >30.82, and AAV patients with HSI ≤30.82 showed a significantly lower cumulative ESRD-free survival rate than those with HSI >30.82.
To date, it has been reported that liver and kidney fibrosis could share several pathogenic mechanisms, such as nuclear transcription factors, cellular sensors, and effectors of redox regulation, which may increase insulin resistance, cholesterol accumulation, oxidative stress, proinflammatory cytokine/chemokine production and fibrogenesis [19]. In addition, focusing on the relationship between HSI and chronic kidney disease (CKD) occurrence, a previous study reported that, compared to individuals with HSI <30, both individuals with 30≤HSI≤36 and those with HSI >36 exhibited significantly higher risks for CKD among middle-aged individuals in Japan [20]. Therefore, given that CKD is a strong risk factor for ESRD progression, it could be theoretically assumed that ESRD during the disease course may be identified more often in AAV patients having higher HSI at diagnosis. However, the present study showed an inverse association between HSI at diagnosis and ESRD during the disease course in AAV patients. On the other hand, in the correlation analysis, HSI was significantly correlated with BVAS, FFS, and serum creatinine levels, which have been known as important risk factors for poor renal prognosis in AAV patients [21,22]. Therefore, we conclude that HSI at diagnosis could forecast ESRD during the disease course by an indirect correlation of HSI with the initial risk factors for ESRD rather than a direct relation with substantial liver fibrosis in AAV patients.
In terms of the clinical implication of HSI for forecasting ESRD based on the AAV subtype, we divided the study population into two groups according to the subtype of AAV such as MPA/GPA and EGPA and reanalyzed the ability of HSI at diagnosis for forecasting ESRD during the disease course. First, we included 208 MPA/GPA patients and performed the ROC curve of HSI for ESRD. The AUC of HSI for ESRD was statistically significant (AUC 0.333, 95% CI 0.247, 0.419; p=0.001). When the optimal cut-off of HSI for ESRD was set at ≤30.82, the sensitivity and specificity were 60.1% and 70.0%, respectively. Coincidently, the cut-off obtained in MPA/GPA patients was the same as that obtained among all AAV patients. When MPA/GPA patients were divided into two groups according to HSI of 30.82, ESRD was identified more often in patients with HSI ≤30.82 than in those without (29.5% vs. 10.6%, p=0.001). OR was as high as 3.517 (95% CI 1.672, 7.398) (Supplementary Figure 1A).
Additionally, MPA/GPA patients with HSI ≤30.82 exhibited a significantly lower cumulative ESRD-free survival rate than those without (Supplementary Figure 1B). Second, we included only 52 EGPA patients and performed the ROC curve of HSI for ESRD, which showed no significant AUC of HSI for ESRD. We concluded that the ability of HSI for forecasting ESRD was valid in MPA/GPA patients but not EGPA patients. Nevertheless, we suggest applying the results of the present study to all patients with AAV for the following reasons: first, there may be discordance in the diagnosis of the subtypes of AAV among several classification criteria and definitions; second, there may be cases which could fulfil the classification criteria for the two subtypes of AAV; and third, there may be cases which could change from one subtype to another during the disease course [23-25].
In addition, in terms of the clinical usefulness of HSI in forecasting ESRD based on ANCA type, we included 174 AAV patients having MPO-ANCA (P-ANCA) at diagnosis and performed the ROC curve, which showed a significant AUC of HSI for ESRD (AUC 0.346, 95% CI 0.249, 0.442, p=0.005). When the optimal cut-off of HSI for ESRD was set at ≤30.82, the sensitivity and specificity were 55.0% and 73.5%, respectively. AAV patients with MPO-ANCA (or P-ANCA) and HSI ≤30.82 exhibited a significantly higher risk of ESRD than those without (OR 3.395, 95% CI 1.478, 7.797, p=0.003). Furthermore, AAV patients with MPO-ANCA (or P-ANCA) and HSI ≤30.82 exhibited a significantly lower cumulative ESRD-free survival rate than those without (p=0.005) (Supplementary Figure 2). However, the clinical usefulness of HSI for forecasting ESRD disappeared among AAV patients with PR3-ANCA (or C-ANCA). Nevertheless, suggest applying the results of the present study to all patients with AAV regardless of the ANCA type. This is because the detection methods for ANCA include both an immunoassay and an indirect immunofluorescence assay in the new classification criteria for AAV proposed in 2022, which made the clinical meaning of the ANCA type less clinically significant.
This study has several limitations. First of all, the small number of AAV patients and the retrospective study design were primary limitations. Another critical limitation of this study was that liver ultrasonography and transient elastography were not performed to confirm the extent of liver fibrosis or the presence of NAFLD. Additionally, given that the frequency of DM was relatively high and kidney biopsy was not performed in all patients with ESRD, we could not totally exclude the contribution of DM nephropathy to ESRD occurrence in AAV patients in the present study. Nevertheless, the advantage of this study is that it is the first to demonstrate the potential of HSI for forecasting ESRD in AAV patients as a pilot study. We believe that a multicentre and prospective future study with more patients will overcome these limitations and validate the results of this study.
CONCLUSION
This study is the first to demonstrate that HSI at AAV diagnosis could forecast ESRD during the disease course in AAV patients. Therefore, as a complementary index, it is expected that assessing HSI at diagnosis in patients newly diagnosed with AAV will help to cope with the development of ESRD in AAV patients.
SUPPLEMENTARY DATA
Supplementary data can be found with this article online at https://doi.org/10.4078/jrd.2023.0032.
ACKNOWLEDGMENTS
None.
Footnotes
FUNDING
This work was supported by grants from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health and Welfare (HI14C1324), and CELLTRION PHARM, Inc. Chungcheongbuk-do, Republic of Korea (NCR 2019-6).
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
H.J.C., P.G.P., J.H.H., and S.W.L. conceived the work. H.J.C. and P.G.P. performed data curation. All authors performed formal analysis. Y.B.P. and S.W.L. performed funding acquisitions. H.J.C. and P.G.P. wrote the original draft. J.H.H. and S.W.L. reviewed and edited the manuscript. All authors approved the final version of manuscript.
REFERENCES
- 1.Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65:1–11. doi: 10.1002/art.37715. [DOI] [PubMed] [Google Scholar]
- 2.Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 2007;66:222–7. doi: 10.1136/ard.2006.054593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, et al. Modification and validation of the Birmingham Vasculitis Activity Score (version 3) Ann Rheum Dis. 2009;68:1827–32. doi: 10.1136/ard.2008.101279. [DOI] [PubMed] [Google Scholar]
- 4.Guillevin L, Pagnoux C, Seror R, Mahr A, Mouthon L, Toumelin PL French Vasculitis Study Group (FVSG), author The Five-Factor Score revisited: assessment of prognoses of systemic necrotizing vasculitides based on the French Vasculitis Study Group (FVSG) cohort. Medicine (Baltimore) 2011;90:19–27. doi: 10.1097/MD.0b013e318205a4c6. [DOI] [PubMed] [Google Scholar]
- 5.Bhamra K, Luqmani R. Damage assessment in ANCA-associated vasculitis. Curr Rheumatol Rep. 2012;14:494–500. doi: 10.1007/s11926-012-0291-1. [DOI] [PubMed] [Google Scholar]
- 6.Willeke P, Schlüter B, Limani A, Becker H, Schotte H. Liver involvement in ANCA-associated vasculitis. Clin Rheumatol. 2016;35:387–94. doi: 10.1007/s10067-015-2882-5. [DOI] [PubMed] [Google Scholar]
- 7.Masiak A, Drobińska A, Zdrojewski Z. Hepatic involvement in granulomatosis with polyangiitis - diagnostic difficulties. Reumatologia. 2017;55:318–22. doi: 10.5114/reum.2017.72630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee SW, Kim DY, Ahn SH, Park YB, Han KH, Park JY. Subclinical but significant liver fibrosis in patients with ANCA-associated vasculitis. Clin Exp Rheumatol. 2019;37 Suppl 117(2):26–31. [PubMed] [Google Scholar]
- 9.Pyo JY, Ahn SS, Lee LE, Choe HN, Song JJ, Park YB, et al. Efficacy of the fibrosis index for predicting end-stage renal disease in patients with antineutrophil cytoplasmic antibody-associated vasculitis. Int J Clin Pract. 2021;75:e13929. doi: 10.1111/ijcp.13929. [DOI] [PubMed] [Google Scholar]
- 10.Pyo JY, Ahn SS, Lee LE, Choi GM, Song JJ, Park YB, et al. The novel fibrosis index at diagnosis may predict all-cause mortality in patients with antineutrophil cytoplasmic antibody-associated vasculitis without substantial liver diseases. Clinics (Sao Paulo) 2021;76:e2501. doi: 10.6061/clinics/2021/e2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwon HC, Song JJ, Park YB, Lee SW. Fibrosis-5 predicts end-stage renal disease in patients with microscopic polyangiitis and granulomatosis with polyangiitis without substantial liver diseases. Clin Exp Med. 2021;21:399–406. doi: 10.1007/s10238-021-00691-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park HJ, Park JY, Jung SM, Song JJ, Park YB, Lee SW. Fibrosis-4 index at diagnosis is associated with all-cause mortality in patients with microscopic polyangiitis and granulomatosis with polyangiitis. BMC Gastroenterol. 2019;19:90. doi: 10.1186/s12876-019-1007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu L, Lu W, Li P, Shen F, Mi YQ, Fan JG. A comparison of hepatic steatosis index, controlled attenuation parameter and ultrasound as noninvasive diagnostic tools for steatosis in chronic hepatitis B. Dig Liver Dis. 2017;49:910–7. doi: 10.1016/j.dld.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Sviklāne L, Olmane E, Dzērve Z, Kupčs K, Pīrāgs V, Sokolovska J. Fatty liver index and hepatic steatosis index for prediction of non-alcoholic fatty liver disease in type 1 diabetes. J Gastroenterol Hepatol. 2018;33:270–6. doi: 10.1111/jgh.13814. [DOI] [PubMed] [Google Scholar]
- 15.Wang C, Cai Z, Deng X, Li H, Zhao Z, Guo C, et al. Association of hepatic steatosis index and fatty liver index with carotid atherosclerosis in type 2 diabetes. Int J Med Sci. 2021;18:3280–9. doi: 10.7150/ijms.62010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weng CH, Liu ZC. Drug-induced anti-neutrophil cytoplasmic antibody-associated vasculitis. Chin Med J (Engl) 2019;132:2848–55. doi: 10.1097/CM9.0000000000000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McAdoo SP, Medjeral-Thomas N, Gopaluni S, Tanna A, Mansfield N, Galliford J, et al. Long-term follow-up of a combined rituximab and cyclophosphamide regimen in renal anti-neutrophil cytoplasm antibody-associated vasculitis. Nephrol Dial Transplant. 2019;34:63–73. doi: 10.1093/ndt/gfx378. Erratum in: Nephrol Dial Transplant 2018;33:899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee JH, Kim D, Kim HJ, Lee CH, Yang JI, Kim W, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis. 2010;42:503–8. doi: 10.1016/j.dld.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Musso G, Cassader M, Cohney S, De Michieli F, Pinach S, Saba F, et al. Fatty liver and chronic kidney disease: novel mechanistic insights and therapeutic opportunities. Diabetes Care. 2016;39:1830–45. doi: 10.2337/dc15-1182. [DOI] [PubMed] [Google Scholar]
- 20.Ochiai H, Shirasawa T, Yoshimoto T, Nagahama S, Sakamoto K, Azuma M, et al. Hepatic steatosis index and chronic kidney disease among middle-aged individuals: a large-scale study in Japan. Dis Markers. 2021;2021:9941834. doi: 10.1155/2021/9941834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo Q, Yu L, Zhang X, Shang J, Duan X. Analysis of the risk factors for end-stage renal disease and mortality in ANCA-associated vasculitis: a study from a single center of the Chinese Rheumatism Data Center. Clin Rheumatol. 2023;42:489–99. doi: 10.1007/s10067-022-06419-1. [DOI] [PubMed] [Google Scholar]
- 22.Toraman A, Soysal Gündüz Ö. Predictors of renal and patient outcomes in anti-neutrophil cytoplasmic antibody-associated vasculitis: our single-center, tertiary care experience. Arch Rheumatol. 2021;36:445–57. doi: 10.46497/ArchRheumatol.2021.8687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pyo JY, Ahn SS, Song JJ, Park YB, Lee SW. Application of the 2022 ACR/EULAR criteria for microscopic polyangiitis to patients with previously diagnosed microscopic polyangiitis. Clin Exp Rheumatol. 2023;41:792–9. doi: 10.55563/clinexprheumatol/vmrk76. [DOI] [PubMed] [Google Scholar]
- 24.Pyo JY, Ahn SS, Song JJ, Park YB, Lee SW. Reclassification of previously diagnosed GPA patients using the 2022 ACR/EULAR classification criteria. Rheumatology (Oxford) 2023;62:1179–86. doi: 10.1093/rheumatology/keac267. [DOI] [PubMed] [Google Scholar]
- 25.Pyo JY, Ahn SS, Song JJ, Park YB, Lee SW. The reclassification of patients with previously diagnosed eosinophilic granulomatosis with polyangiitis based on the 2022 ACR/EULAR criteria for antineutrophil cytoplasmic antibody-associated vasculitis. J Rheumatol. 2023;50:213–8. doi: 10.3899/jrheum.220560. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.