Abstract
Introduction and importance
Eosinophilic cholecystitis is an unusual condition in which more than 90 % of the inflammatory infiltrate in the gallbladder wall is comprised of eosinophils. The pathogenesis of eosinophilic cholecystitis is still unknown, but in some cases, it is related to hyper-eosinophilic syndrome, parasitosis, infections, and drugs.
Case presentation
We described two cases in which a woman aged 27 years and a man aged 30 years presented with acute and chronic cholecystitis symptoms, respectively. The ultrasound revealed calculous cholecystitis. The cholecystectomy was performed, and the pathological examination of the surgical specimen revealed eosinophilic cholecystitis.
Clinical discussion
Eosinophilic cholecystitis is a rare disease of the gallbladder. It accounts for 0.25 to 6.4 % of cholecystitis cases. It is characterized by eosinophils infiltration in the lamina propria and the muscle layer. There are no specific symptoms of this disease; it presents as typical cholecystitis. The histopathological investigation is the gold standard for diagnosing eosinophilic cholecystitis, and cholecystectomy is the ultimate treatment for it.
Conclusion
Eosinophilic cholecystitis is a rare condition characterized by acute cholecystitis with eosinophilic infiltration of the gallbladder. In patients with eosinophilic cholecystitis, a comprehensive assessment of the underlying causes is recommended.
Keywords: Eosinophilic, Cholecystitis, Gallbladder, Cholelithiasis
Highlights
-
•
Eosinophilic cholecystitis is a rare disease of the gallbladder. It accounts for 0.25 to 6.4 % of cholecystitis cases.
-
•
It is a condition in which more than 90 % of the inflammatory infiltrate in the gallbladder wall is comprised of eosinophils.
-
•
We described two cases presented with acute and chronic cholecystitis symptoms, respectively.
-
•
The histopathological investigation is the gold standard for diagnosing eosinophilic cholecystitis.
-
•
A comprehensive assessment of the underlying causes is recommended in patients with eosinophilic cholecystitis.
1. Introduction
Eosinophilic cholecystitis (EC) is a rare disease that is characterized by eosinophilic infiltration of the gallbladder [1]. Although the etiology remains obscure, it has been linked to allergies, parasites, hyper-eosinophilic syndrome, eosinophilic gastroenteritis, cholelithiasis, and acalculous cholecystitis [[2], [3], [4], [5], [6]]. The diagnosis is based on a combination of classic cholecystitis symptoms and transmural inflammatory infiltration of the gallbladder wall, more than 90 % of which is composed of eosinophils [7]. Lymphoeosinophilic cholecystitis is the term used when the infiltrate contains between 50 and 75 % eosinophils as well as other inflammatory cells [8]. However, cholecystectomy is the preferred treatment, and the prognosis is usually favourable [1]. Each underlying pathology should be specifically treated when EC is secondary to it [9]. We present two unusual cases of idiopathic eosinophilic cholecystitis with cholelithiasis. This case report has been reported in line with SCARE Criteria [10].
2. Case presentation
Case 1.
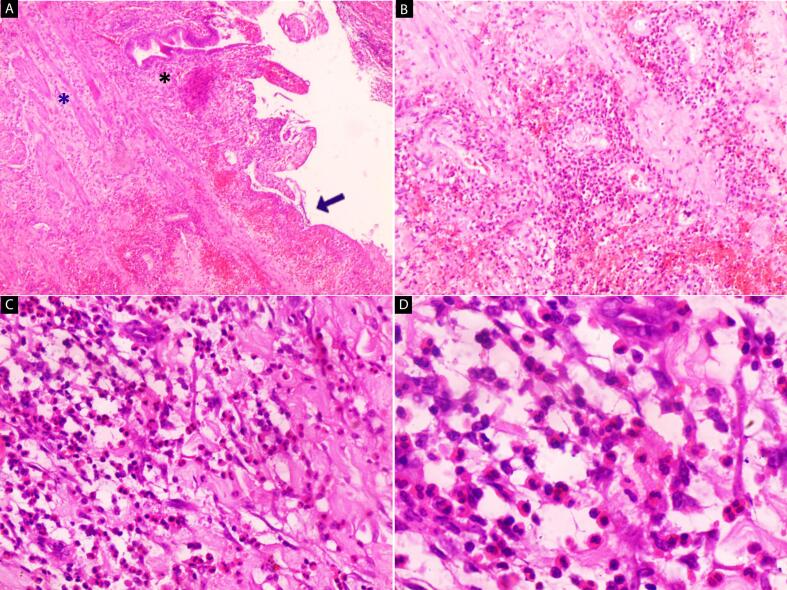
A 27-year-old woman comes to the emergency department due to severe abdominal pain that has persisted for a day without responding to analgesics. The pain was in the right upper quadrant and radiated to the right shoulder. She had nausea and vomiting, and her temperature was normal (37)°C. The patient had no remarkable personal or family history. She is a smoker and a non-alcoholic. The physical examination revealed a good general condition. No skin changes, organomegaly, lymphadenopathy, or signs of systemic involvement were noted. Laboratory investigation revealed the following: Blood white cell count: 11.3 × 10^9/L (range: 4.8–10.8 × 10^9/L); granulocytes: 83 %. Hemoglobin: 12.8 g/dL (range 12.0–15.5 g/dL). Platelet count: 213 × 10^9/L. Total bilirubin: 0.45 mg/dL (range 0.1–1.2 mg/dL). Direct bilirubin: 0.22 mg/dL (range 0.1–0.5 mg/dL). The eosinophil count and serum IgE level were within normal limits. Abdominal ultrasound showed the gallbladder wall thickening by about 4 mm with pericholecystic fluid and multiple gallstone shadows, the largest one was about 17 mm [Fig. 1]. She was diagnosed with acute cholecystitis and underwent laparoscopic cholecystectomy under general anaesthesia. The specimen was sent to the pathology department. On gross examination, the excised gallbladder was 75 mm in length with a 35 mm average diameter. The average wall thickness was 12 mm with a rubbery grayish-yellow cut section. Microscopically, the mucosa revealed ulceration, edema, and chronic inflammatory cell infiltrates. A marked eosinophilic infiltration constituting more than 90 % of the inflammatory infiltrates, was observed transmurally [Fig. 2]. The diagnosis of eosinophilic cholecystitis with cholelithiasis was made. She was stable and discharged two days later, without any complications. No infections, allergies, or asthma attacks were found when the patient returned to the clinic for follow-up care.
Fig. 1.
Abdominal ultrasound shows gallbladder wall thickening of about 4 mm and large gallstone shadows of 17 mm.
Fig. 2.
H&E stain (A - D): Microscopic images of the gallbladder. (A) The mucosa reveals ulceration (blue arrow), edema, and eosinophilic inflammatory cell infiltrates in the lamina propria (black star) and muscularis propria (blue star) (40×). (B—D) Marked eosinophilic infiltration transmurally (100×, 200×, 400×). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Case 2.
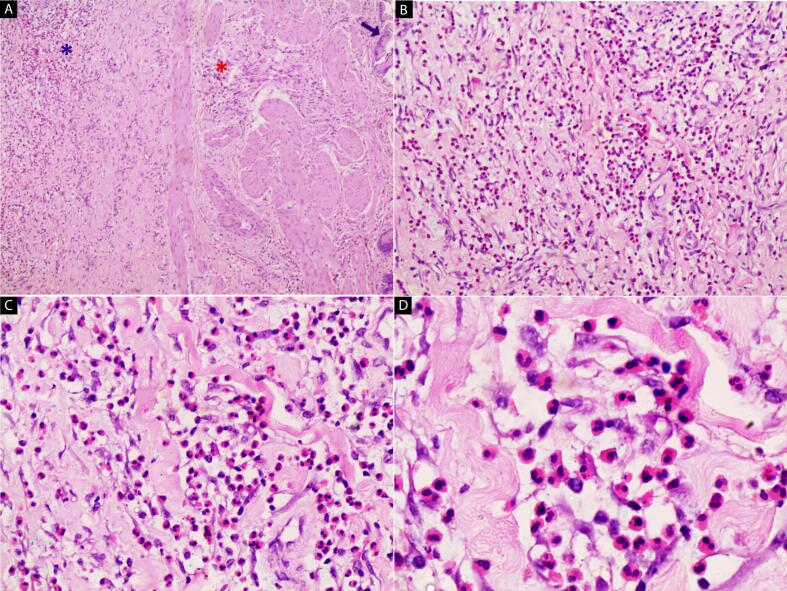
A 30-year-old man comes to the emergency department with a seven-day history of severe abdominal pain while responding to analgesics. The pain was in the right upper quadrant, along with a fever and chills. There was no nausea or vomiting. The patient had no remarkable personal or family history. He is a smoker and a non-alcoholic. Physical examination revealed tenderness in the right upper quadrant that radiated to the epigastrium. No skin changes, organomegaly, lymphadenopathy, or signs of systemic involvement were present. Laboratory investigation revealed the following: Blood white cell count: 11.6 × 10^9/L (range: 4.8–10.8 × 10^9/L); granulocytes: 68 %. Hemoglobin: 15.8 g/dL (range 13.6–17.5 g/dL). Platelet count: 426 × 10^9/L. Total bilirubin: 0.6 mg/dL (range 0.1–1.2 mg/dL). Direct bilirubin: 0.3 mg/dL (range 0.1–0.5 mg/dL). The eosinophil count and serum IgE level were within normal limits. Abdominal ultrasound showed the gallbladder wall thickening by about 4 mm with pericholecystic fluid and two gallstone shadows. The largest one was about 16.5 mm, and another was 10 mm. He was diagnosed with chronic cholecystitis and underwent laparoscopic cholecystectomy under general anaesthesia. The specimen was sent to the pathology department. On gross examination, the gall bladder was 65 mm in length with a 40 mm average diameter. The average wall thickness was 7 mm. Multiple gallstones were noted [Fig. 3]. Microscopically, eosinophils, consisting of greater than 90 % of the chronic inflammatory cells, were observed infiltrating the lamina propria and the muscularis propria [Fig. 4]. A diagnosis of chronic eosinophilic cholecystitis with cholelithiasis was reported. His postoperative course was uneventful, and he was discharged two days later. The patient had a thorough clinical check-up during their outpatient follow-up, where parasitic disease, hypereosinophilia, asthma, and herbal medicine were ruled out.
Fig. 3.
Gross image of excised gallbladder representing a rubbery, grayish-green wall with an irregular mucosal surface. Multiple gallstones are present. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 4.
H&E stain (A - D): Microscopic images of the gallbladder. (A) The mucosa was un-ulcerated (blue arrow) and eosinophilic infiltrating the muscularis propria (red star) and serosa (blue star) (40×). (B—D) Large magnifications reveal marked eosinophilic infiltration transmurally (100×, 200×, 400×). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
Eosinophilic cholecystitis is a rare disease of the gallbladder. It accounts for 0.25 to 6.4 % of cholecystitis cases [11]. It is characterized by eosinophils infiltration in the lamina propria and the muscle layer [11]. Despite being documented for the first time in 1949, the pathogenic mechanism has yet to be pinpointed [1,9]. There are several reports of EC in the literature, but the disease has a low incidence and no recognised or well-studied etiology [9]. However, many cases have been reported as being associated with hyper-eosinophilic syndrome, parasitism, infections, allergies, medications, and medicinal herbs [[2], [3], [4], [5], [6]]. After ruling out the aforementioned etiologies, reports of a subset of idiopathic EC have also been made [8]. In our two cases, histories and investigation did not reveal any known etiology; therefore, these cases are considered idiopathic eosinophilic cholecystitis. On the other hand, patients with acalculous cholecystitis, which results in eosinophil infiltration of the mucosal surface, are three- to four times more likely than patients with gallstones to have EC [11]. In contrast, cholelithiasis was seen in two of our patients. On clinical examination, there are no specific symptoms of this disease; it presents as typical acute cholecystitis, which is diagnosed using the Tokyo criteria, which include right upper quadrant abdominal pain or tenderness, a positive Murphy's sign, elevated CRP, fever, an elevated WBC count, and imaging findings typical of acute cholecystitis [12]. The patient must be examined carefully to investigate symptoms that may indicate various associated disorders, which may represent the fundamental quandary [11,13]. The histopathological investigation is the gold standard for diagnosing eosinophilic cholecystitis and cholecystectomy is the ultimate treatment for it [1,7,9,11]. Other underlying causes should be treated in a particular way when they are found with steroids or antiparasitic medications [9].
4. Conclusion
Eosinophilic cholecystitis is a rare condition characterized by acute cholecystitis with eosinophilic infiltration of the gallbladder. Other eosinophilic illnesses, such as eosinophilic gastroenteritis, parasite infections, medication responses, and food allergies, are frequently associated with EC. In patients with eosinophilic cholecystitis, a comprehensive assessment of the underlying causes is recommended.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
No ethical approval was needed for this case report.
Registration of research studies
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Declaration of competing interest
The authors have no conflicts of interest to declare.
References
- 1.del Moral-Martínez M., Barrientos-Delgado A., Crespo-Lora V., Cervilla-Sáez-de-Tejada M.E., Salmerón-Escobar J. Eosinophilic cholecystitis: an infrequent cause of acute cholecystitis. Revista Espanola de Enfermedades Digestivas: Organo Oficial de la Sociedad Espanola de Patologia Digestiva. 2015;107(1):45–47. (PMID: 25603333) [PubMed] [Google Scholar]
- 2.Sánchez-Pobre P., López-Ríos Moreno F., Colina F., Yela C., Manzano M., Rodríguez S., Martín A., Casís B., Garfia C., Castellano G., Solís-Herruzo J.A. Colecistitis eosinofílica: una causa poco frecuente de colecistectomía [Eosinophilic cholecystitis: an infrequent cause of cholecystectomy] Gastroenterol Hepatol. 1997;20(1):21–23. Spanish. PMID: 9072192. [PubMed] [Google Scholar]
- 3.Hepburn A., Coady A., Livingstone J., Pandit N. Eosinophilic cholecystitis as a possible late manifestation of the eosinophiliamyalgia syndrome. Clin. Rheumatol. 2000;19:470–472. doi: 10.1007/s100670070008. [DOI] [PubMed] [Google Scholar]
- 4.Tajima K., Katagiri T. Deposits of eosinophil granule proteins in eosinophilic cholecystitis and eosinophilic colitis associated with hypereosinophilic syndrome. Digest Dis Sci. 1996;41:282–288. doi: 10.1007/BF02093816. [DOI] [PubMed] [Google Scholar]
- 5.Russel C.O.H., Dowling J.P., Marshall R.D. Acute eosinophilic cholecystitis in association with hepatic echinococcosis. Gastroenterology. 1979;77:758–760. [PubMed] [Google Scholar]
- 6.Parry S.W., Pelias M.E., Browder W. Acalculous hypersensitivity cholecystitis: hypothesis of a new clinicopathologic entity. Surgery. 1988:911–916. [PubMed] [Google Scholar]
- 7.Shakov R., Simoni G., Villacin A., Baddoura W. Eosinophilic cholecystitis, with a review of the literature. Ann. Clin. Lab. Sci. 2007;37(2):182–185. (PMID: 17522376) [PubMed] [Google Scholar]
- 8.Choudhury Monisha, Pujani Mukta, Katiyar Yogita, Lalita Jyotsna P., Rautela Archna. Idiopathic eosinophilic cholecystitis with cholelithiasis: a report of two cases. Turkish. J. Pathol. 2014 doi: 10.5146/tjpath.2014.01235. [DOI] [PubMed] [Google Scholar]
- 9.Gutiérrez-Moreno L.I., Trejo-Avila M.E., Díaz-Flores A., Dávila-Zenteno M.R., Montoya-Fuentes I.M., Cárdenas-LailsonLE. Colecistitis eosinofílica: estudio retrospectivo de 14 anos. Rev. Gastroenterol. Mex. 2018;83:405–409. doi: 10.1016/j.rgmx.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Matani N., Soleimani N., Mohammadzadeh S. Eosinophilic cholecystitis, a rare case report with a review of the literature. Iranian Journal of Colorectal Research. 2020;8(4):206–208. doi: 10.30476/acrr.2020.87773.1062. [DOI] [Google Scholar]
- 12.Hirota M., Takada T., Kawarada Y., et al. Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo guidelines. J. Hepato-Biliary-Pancreat. Surg. 2007;14:78–82. doi: 10.1007/s00534-006-1159-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gutierrez-Alvarez M., Vallarta S., Cruz R., et al. Eosinophilic cholecystitis as an atypical etiology of biliary colic: a case report and review of the literature. Cureus. 2023;15(3) doi: 10.7759/cureus.35831. [DOI] [PMC free article] [PubMed] [Google Scholar]