Abstract
Introduction and importance
Adnexal torsion is an uncommon but urgent surgical situation more frequently observed during the reproductive years and rarely in postmenopausal women.
Case presentation
This case report describes a postmenopausal woman with a large left ovarian cyst measuring 18 × 20 × 22 cm who experienced adnexal torsion, which is a rare occurrence in this age group. To avoid the potential requirement for additional surgical procedures in case of cyst recurrence in the remaining ovary or the development of uterine diseases a total abdominal hysterectomy and bilateral salpingo-oophorectomy with cystectomy were performed. Histopathological analysis of the cyst confirmed that it was a benign serous cystadenoma of the ovary.
Clinical discussion
Adnexal torsion can happen at any age but is less likely to occur after menopause. Moreover, giant ovarian cysts (>10 cm) are uncommon, making adnexal torsion on these cysts a rare event. While laparotomy remains the gold standard surgical intervention, laparoscopy is beginning to play a role in management of giant cyst.
Conclusions
This report documenting a rare case of adnexal torsion in a postmenopausal woman following a serous giant cystadenoma emphasizes that this surgical emergency can occur at any age. In addition, the report highlights that the presence of an ovarian mass or cyst increases the risk of adnexal torsion, regardless of age.
Keywords: Postmenopausal, Adnexal, Ovarian, Torsion, Cystadenoma. Giant serous cystadenoma
Highlights
-
•
Adnexal torsion can occur at any age.
-
•
The presence of ovarian mass or cyst predispose to adnexal torsion at any age.
-
•
Pelvic ultrasonography is the first diagnostic tool for diagnosis of adnexal mass or cyst.
-
•
When torsion of the adnexa or ovary is suspected, surgery is the main line of treatment, whether conservative or radical.
1. Background
Adnexal torsion is a rare surgical emergency, occurring most often in active women and rarely in postmenopausal women. The main risk factor for torsion is the presence of an ovarian cyst. Rare cases are reported in the literature of adnexal torsion following a giant cyst [1,2].
As reported by Madhu et al., there are instances where ovarian cysts can grow to a substantial size, requiring the collaboration of multiple medical specialties to safeguard the patient's life [3].
According to previous definitions, an ovarian cyst was considered giant if its diameter exceeded 10 cm. However, due to the increased utilization of routine imaging techniques, the incidence of large ovarian masses has decreased over the past two decades [4].
This case report describes a postmenopausal woman with a large left ovarian cyst measuring 20 × 19 cm who experienced adnexal torsion, which is a rare occurrence in this age group. Due to the patient's age and menopausal status, a total abdominal hysterectomy (TAH) and bilateral salpingo-oophorectomy (BSO) with cystectomy were performed. Histopathological analysis of the cyst confirmed that it was a benign serous cystadenoma of the ovary.
The purpose of this report is to draw attention to the fact that adnexal torsion is a diagnosis to be considered in the presence of acute abdominal-pelvic pain in women, even postmenopausal, and in the case of chronic pain with pelvic discomfort, pelvic ultrasound should be performed to explore the adnexa for a mass or cyst, which is a potential risk factor for torsion, regardless of age. The work has been reported in line with the SCARE criteria [17].
2. Case report
A 63-year-old postmenopausal woman, G3P3, presented to the emergency department with sudden onset of severe lower abdominal pain that had started earlier that day. She reported feeling nauseous. She was being treated for type 2 diabetes on insulin and had no history of surgery. The patient reported pelvic discomfort with attacks of mild paroxysmal pain. She had no history of constipation, anorexia, or urinary signs.
The patient was clinically stable. On abdominal examination, the abdomen was distended, and bowel sounds diminished. On gynecological examination, vaginal touch coupled with abdominal palpation reveals an enormous pelvic abdominal mass, and tenderness noted on deep palpation.
Transvaginal ultrasound was performed, which showed a normal-sized uterus with endometrial thickness within the normal range for a post-menopausal woman (4 mm) with a giant multilocular cystic mass in the right adnexa measuring approximately 20 × 22 cm in diameter, with numerous thin septations, and the locules contained fluid of different echogenicity.
The MRI revealed the presence of a large, multilocular cyst located in the right adnexa, measuring 18 × 20 × 22 cm. The cyst contained fluid with variable signal intensities on both T1 and T2 sequences, giving it a stained-glass appearance. Based on these imaging characteristics, the cyst is most likely a mucinous cystadenoma (Fig. 1, Fig. 2).
Fig. 1.

Magnetic resonance image of the pelvi-abdominal mass sagittal section.
Fig. 2.
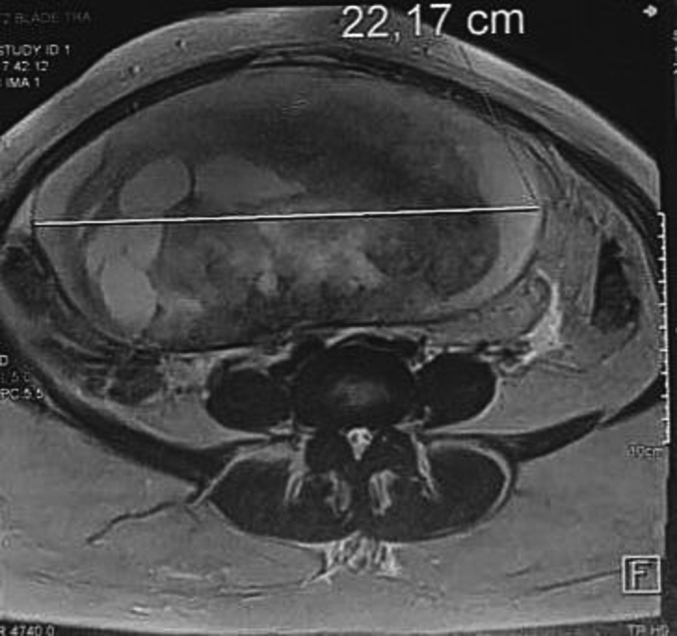
Magnetic resonance image of the pelvi-abdominal mass transverse section.
The findings were in line with the diagnosis of adnexal torsion, which was attributed to the presence of the giant cyst.
The patient underwent emergency surgery and was taken to the operating room. A laparotomy was performed, which revealed that the right adnexal cyst had become twisted on its pedicle. The cyst was successfully untwisted and removed during the procedure (Fig. 3).
Fig. 3.
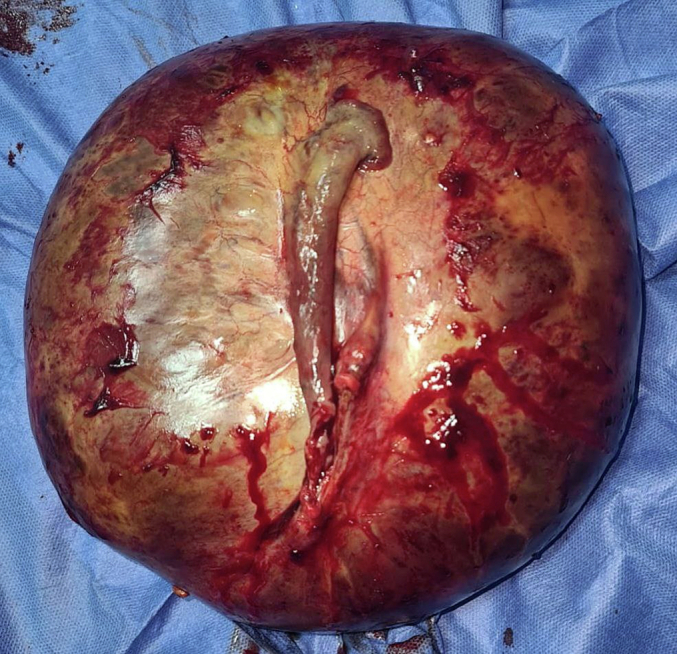
Image showing giant cyst after resection.
Considering the patient's age, it was decided to proceed with a TAH with BSO. Following the surgery, the patient's recovery was uncomplicated, and she was discharged on the third day after the operation.
Histological examination revealed a multilocular cyst lined by a single layer of bland flattened epithelial cells with occasional cuboidal epithelial cells. The cyst was filled with clear serous fluid. No malignant cells or nuclear atypia were observed. The histopathology was suggestive of benign serous cystadenoma of the ovary.
3. Discussion
Adnexal cysts that measure >10 cm in diameter are considered giant cysts and are usually benign. Histopathological analysis of these cysts typically reveals either serous or mucinous cystadenomas [5].
Mucinous cystadenoma of the ovary is a type of benign tumor that arises from the epithelial cells that line the surface of the ovary and constitutes 15 % of all ovarian tumors. These tumors are composed of multiple cysts filled with thick, gelatinous, or mucinous fluid. Mucinous cystadenomas can vary in size, with some growing to be giant. They are most commonly found in women of reproductive age and may be detected incidentally during routine medical imaging [6].
Regarding the mode of the presentation of giant cysts, we conducted a literature search that concluded that abdominal pain and distension, as well as anorexia, are common symptoms associated with the presence of a giant adnexal mass [7]. No cases have been revealed with a clinical presentation of adnexal torsion as in our case (Table 1).
Table 1.
Giant ovarian cysts in postmenopausal women: literature review.
| Study (year) | Age | Symptom | Site | Size of the cyst | CA 125 U/mL | Type of the cyst | Surgery |
|---|---|---|---|---|---|---|---|
| Sujatha et al. (2009) [13] | 66 | Vague abdominal pain, anorexia | Unilateral | 60 × 47 × 30 cm | 46.61 | Serous cyst adenoma | TAH + BSO |
| Alobaid et al. (2013) [4] | 69 | Abdominal distention and discomfort | Unilateral | Max diameter 20 cm | Normal | Serous cyst adenoma | LAVH + BSO |
| Madhu et al. (2013) [14] | 55 | Mechanical discomfort due to distended abdomen | Unilateral | 50 × 39 × 47 cm | No data | Mucinous cyst adenoma | TAH + BSO |
| Bhasin et al. (2017) [15] | 85 | Diffuse abdominal pain | Unilateral | 58 × 46 cm | No data | Mucinous cyst adenoma | Total excision of the cyst |
| Agrawal et al. (2015) [12] | 65 | Dull aching pain in the lower back, shortness of breath | Unilateral | 25 × 28 × 15 cm | 31.31 | Serous cyst adenoma | TAH + BSO |
| Kim et al. (2016) [16] | 52 | Abdominal distention | Unilateral | 36 × 21 × 30 cm | 109.5I | Benign cystic lesion with hemorrhage | Total excision of the cyst |
| Nishat Fatema et al. [3] (2018) | 57 | Asymptomatic | Unilateral | 17.5 × 17.3 × 9.5 cm | 12. | Benign serous cystadenoma of the ovary | TAH + BSO |
| Current case (2023) | 63 | Sudden abdominal pain | Unilateral | 18 × 20 × 22 cm | 14 | Benign serous cystadenoma of the ovary | TAH + BSO |
Against this backdrop, our patient presented to our department with acute abdominopelvic pain with nausea. It should be noted that the patient reported pelvic discomfort with attacks of mild paroxysmal pain.
High-frequency transvaginal ultrasound and color Doppler imaging are essential for diagnosing and characterizing adnexal masses. These imaging modalities are well-tolerated, cost-effective, and widely available to clinicians. The International Ovarian Tumor Analysis (IOTA) group has proposed an objective method for evaluating adnexal lesions, which is particularly helpful for less-experienced operators. Color Doppler is used to assess blood flow after grayscale imaging and benign masses are recognized by thin walls, absence of papillary projections, septations, solid components, and no blood flow on color Doppler. Common ultrasound findings that suggest malignancy include large size, papillary components, irregular walls, and septations. However, the ultrasound characteristics alone may not always be enough to classify adnexal masses as benign or malignant [8].
With its ability to provide detailed tissue characterization based on signal properties, MRI is highly effective at diagnosing benign ovarian lesions such as hemorrhagic cysts, endometriomas, and benign cystic teratomas. Nevertheless, MRI is typically employed as a problem-solving tool when dealing with complex or sonographically indeterminate adnexal masses. By providing precise anatomical and functional information, MRI can aid in surgical planning and help clinicians determine the most appropriate management strategy for adnexal masses [9,10]. However, it should be noted that, given the high cost of imaging such as MRI, the clinical examination remains the key to diagnosis.
CA 125 is primarily a marker for epithelial ovarian carcinoma, and it is only elevated in 50 % of early-stage cases.CA 125 is a commonly studied serum marker for assessing the likelihood of malignant tumors in adnexal masses, but it is not reliable in differentiating between benign and malignant ovarian masses, particularly in premenopausal women. It is mainly useful in postmenopausal women, with a value >35 U/mL indicating the need for referral to a gynecologic oncology service. CA 125 is primarily a marker for epithelial ovarian carcinoma, and it is only elevated in 50 % of early-stage cases [10].
The CA-125 level of our patient was found to be within the normal range, measuring 14 U/mL (Table 1).
Although other clinical variables may be relevant, the IOTA model and CA-125 can be combined to distinguish between benign and malignant ovarian masses [11].
When adnexal torsion is suspected, surgery is generally considered the first course of action. Laparoscopic surgery is the method used to manage adnexal torsion, but the large size of the ovarian mass makes laparotomy the conventional method of surgical management [1]. However, Laparoscopic surgery is increasingly being used for benign adnexal masses. Compared to laparotomy, it offers advantages such as less postoperative pain, faster recovery, and smaller incisions. However, it may be limited by the size of the mass, limited visualization, and risks of rupture and implantation of malignant cells. To reduce cyst size Laparoscopic-guided aspiration is a common technique. Other techniques, ultrasound-guided aspiration, and nephrostomy tube aspiration are used [12].
To this date, no randomized controlled trial has evaluated the laparoscopic management of ovarian giant cysts. Consequently, laparotomy remains the best surgical approach.
When performing surgical removal of large ovarian masse, it is crucial to exercise strict vigilance to prevent potential complications, as previous studies have described intraoperative risks such as hypotension, splanchnic dilatation, and venous pooling. Given the high-risk nature of these cases, multidisciplinary management is recommended. This may involve collaboration between gynecologic oncologists, urologists, and other specialists to ensure the best possible outcomes for patients. By working together, these experts can develop a comprehensive plan for managing potential complications and ensuring the safety and success of the procedure [13].
4. Conclusion
Adnexal torsion and giant cysts are two related gynecological conditions that can occur in postmenopausal women. While adnexal torsion is a rare but serious emergency, giant cysts are usually benign but can cause discomfort and other complications. Diagnostic imaging aids in diagnosis. Prompt diagnosis and management are crucial in preventing complications. Multidisciplinary care is necessary for optimal patient outcomes.
SCARE criteria
The work has been reported in line with the SCARE criteria.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Guarantor of submission
The corresponding author is the guarantor of submission.
Ethical approval
Ethics approval has been obtained to proceed with the current study.
Sources of funding
None.
CRediT authorship contribution statement
Abdelhamid Benlghazi, Moad Belouad,Hamza Messaoudi were responsible for the patient's diagnosis and clinical management. Abdelhamid Benlghazi wrote the manuscript. Hamza Messaoudi contributed to the analysis, supervision, writing, reviewing, and editing of the manuscript for intellectual content. All authors have read and approved the final manuscript.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
None.
Data availability
Supporting material is available if further analysis is needed.
References
- 1.Ci H., Hong M., Ding D. A review of ovary torsion. Ci Ji Yi Xue Za Zhi. 2017;29(3):143–147. doi: 10.4103/tcmj.tcmj_55_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robertson J.J., Long B., Koyfman A. Myths in the evaluation and management of ovarian torsion. J. Emerg. Med. 2017;52(4):449–456. doi: 10.1016/j.jemermed.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 3.Madhu Y., Harish K., Gotam P. Complete resection of a giant ovarian tumour. Gynecol. Oncol. Case Rep. 2013;6:4. doi: 10.1016/j.gynor.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fatema N., Al Badi Mubarak, M. A postmenopausal woman with giant ovarian serous cyst adenoma: a case report with brief literature review. Case Rep. Obstet. Gynecol. 2018;2018 doi: 10.1155/2018/5478328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alobaid A., Memon A., Alobaid S., Aldakhil L. Laparoscopic management of huge ovarian cysts. Obstet. Gynecol. Int. 2013;2013 doi: 10.1155/2013/380854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamel R.M. A massive ovarian mucinous cystadenoma: a case report. Reprod. Biol. Endocrinol. 2010;8(1):1–3. doi: 10.1186/1477-7827-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karaman E., Beger B., Çetin O., Melek M., Karaman Y. Ovarian torsion in the normal ovary: a diagnostic challenge in postmenarchal adolescent girls in the emergency department. Med. Sci. Monit. 2017;23:1312. doi: 10.12659/MSM.902099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thakur M., Timmerman D. Imaging of adnexal masses. Clin. Obstet. Gynecol. 2017;60(1):38–45. doi: 10.1097/GRF.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 9.Naffaa L., Deshmukh T., Tumu S., Johnson C., Boyd K.P., Meyers A.B. Imaging of acute pelvic pain in girls: ovarian torsion and beyond☆. Curr. Probl. Diagn. Radiol. 2017;46(4):317–329. doi: 10.1067/j.cpradiol.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Shaaban A., Rezvani M. Ovarian cancer: detection and radiologic staging. Top. Magn. Reson. Imaging. 2010;21(4):247–259. doi: 10.1097/RMR.0b013e31823d8063. [DOI] [PubMed] [Google Scholar]
- 11.Nowak A., Soja M., Masternak M., Mokros Ł., Wilczyński J., Szubert M. Evaluation of adnexal tumours in the international ovarian tumor analysis system in reference to histopathological results. Menopause Review/Przegląd Menopauzalny. 2019;18(3):141–145. doi: 10.5114/pm.2019.90812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sagiv R., Golan A., Glezerman M. Laparoscopic management of extremely large ovarian cysts. Obstet. Gynecol. 2005;105(6):1319–1322. doi: 10.1097/01.AOG.0000159690.18634.f0. [DOI] [PubMed] [Google Scholar]
- 13.Agrawal S.P., Rath S., Aher G., Gavali U. Large ovarian tumor: a case report. J. Sci. Study. 2015;3(3):144–146. [Google Scholar]
- 14.Madhu Y., Harish K., Gotam P. Complete resection of a giant ovarian tumour. Gynecol. Oncol. Case Rep. 2013;6:4. doi: 10.1016/j.gynor.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhasin S.K., Kumar V., Kumar R. Giant ovarian cyst: a case report. JK science. 2014;16(3):131. [Google Scholar]
- 16.Kim H.Y., Cho M.K., Bae E.H., Kim S.W., Ma S.K. Hydronephrosis caused by a giant ovarian cyst. International braz j urol. 2016;42:848–849. doi: 10.1590/S1677-5538.IBJU.2015.0354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Supporting material is available if further analysis is needed.


