Abstract
Doreen is a 79-year-old woman referred by her general practitioner to the ED for intravenous antibiotics for a urinary tract infection (UTI). She lives in a residential aged care facility (RACF) and staff report malodourous and cloudy urine. She denies dysuria or frequency. On examination Doreen is frail with vital signs of: temperature 37.7°C, pulse 87 bpm, blood pressure 130/70; there is no suprapubic or flank tenderness. Do you perform a dipstick test on Doreen’s urine for a suspected UTI?
UTI in older persons
Accurate diagnosis of UTI in older persons is hindered by high rates of asymptomatic bacteriuria (ASB); lack of a definitive test to support accurate timely diagnosis; and comorbidities, such as immunosuppression and cognitive impairment, which impede assessment for symptoms and signs of UTI.
Both under-diagnosis and over-diagnosis1–3 is common, but over-diagnosis seems the more pressing problem in geriatric emergency medicine and is the focus of this article. A retrospective study of emergency admissions of those aged 75+ years treated with intravenous antibiotics for a UTI found that 43% did not meet defined criteria for that diagnosis. Myriad problems then result: 8% of those treated developed Clostridium difficile diarrhoea;3 emerging evidence shows the urinary microbiome helps to prevent overgrowth of pathogenic bacteria, so inappropriate antibiotics actually promote UTI;4–6 and multi-resistant antimicrobial resistance is promoted. Multiple studies show that antibiotics do not provide any benefit in older persons with ASB, and in fact expose them to risks of allergies, multi-resistant organisms and Clostridium difficile infection.7–10
Definitions
UTI is defined as the presence of both urinary tract symptoms (e.g. suprapubic tenderness, costovertebral angle pain or tenderness, urinary urgency or frequency or dysuria) and isolation of a urinary pathogen at ≥105 colony forming units/mL in a freshly voided mid-stream urine specimen.11,12 Some definitions also include reference to one of the following additional criteria:13–15
no more than two species of organisms identified on urine culture;
pyuria (>10 white blood cells/mm3 per high-power field);
growth of only ≥103 colony forming units/mL of a urinary pathogen on urine culture, in those with a catheter-acquired UTI.
ASB is defined as ≥105 colony forming units/mL in a correctly collected urine specimen from an individual with no typical symptoms or signs of urinary system disease.12 ASB is associated with pyuria to no less an extent than in UTI.16 Table 1 describes the prevalence of ASB in older people.
TABLE 1.
| Sub-population of older persons | Gender | |
|---|---|---|
| Female | Male | |
| Community-dwelling | 6–16% | 4–7% |
| Aged care facility | 25–55% | 15–37% |
| With urodome catheter | Not applicable | 85% |
| With indwelling catheter | 98% | |
These definitions, together with the high prevalence of ASB in older persons, present the following challenges in the ED:
Definitive diagnosis of a UTI requires results of a urine culture that is not available at the time of ED discharge.
Culture results need interpretation based on the clinical symptoms and signs of a UTI, usually by a down-stream provider who did not order them.
Studies of the diagnosis of UTI are associated with significant risk of misclassification bias due to their lack of use of established definitions of UTI.17
Microbiology
Escherichia coli is the most commonly isolated organism in urine cultures from both community-dwelling older persons and RACF residents.18 Antibiotic resistance in E. coli is a significant problem. The prevalence of extended spectrum beta-lactamase-producing E. coli is growing, most particularly in hospital-acquired UTI, where prevalence is up to 44%.19 Extended-spectrum cephalosporin-resistant E. coli prevalence in Australia and New Zealand is reported at 3%.20
Clinical assessment
The first two aims in assessing an older person with a suspected UTI are to look for evidence of sepsis, before determining the likelihood of UTI. Given the high prevalence of ASB in older persons, considering the probability of UTI based on history and examination findings prior to ordering a urine microscopy and culture may be the most important step we can take to reduce over-diagnosis.
Establish the pre-test probability of UTI
Assessing pre-test probability of UTI should include assessment for:
Features of past history that increase risk for UTI (Table 2): presence of one or more of these features increases probability of UTI;
History and examination findings of UTI (Table 3);
Absence of an alternate cause of symptoms.
TABLE 2.
| Domain | Feature |
|---|---|
| Past medical history | Immunocompromise Diabetes Cognitive impairment Immobility Impairment in activities of daily living, particularly disability in drinking and feeding self and disability in washing hands and face |
| Past urological history | Prior antibiotic treatment for UTI Urinary incontinence Cystoceles (women) Prostatic hypertrophy (men) Recent instrumentation of urinary tract Renal stones |
TABLE 3.
Likelihood ratios for positive urine culture of features found on history and examination in adults with suspected UTI24,48–50
| Study population (setting) | Feature | Positive LR (95% CI) | Negative LR (95% CI) | ||
|---|---|---|---|---|---|
| Female adults (ED)† | Older adults (outpatients and RACF) | Female adults (ED) | Older adults (outpatients and RACF) | ||
| History | Dysuria | 2.1 (1.4–3.3) | 2.06 (1.18–3.59) | 0.2 (0.0–0.6) | 0.91 (0.84–0.98) |
| Urinary urgency | 1.3 (0.8–2.1) | 1.06 (0.37–3.04) | 0.9 (0.8–1.1) | 1.0 (0.96–1.04) | |
| Urinary frequency | 2.3 (1.4–3.6) | 0.10 (0.01–1.7) | 0.2 (0.0–0.6) | 1.03 (1.01–1.06) | |
| Change in voiding pattern | 9.33 (3.03–28.7) | 0.56 (0.41–0.76) | |||
| Incontinence (in older adults - self-reported) | 1.65 (1.37–2.0) | 0.61 (0.49–0.77) | |||
| Flank pain | 31.2 (1.87–521) | 0.76 (0.64–0.91) | |||
| Haematuria | 1.4 (0.6–3.4) | 1.0 (0.9–1.0) | |||
| Previous UTI | 1.4 (0.9–2.0) | 0.9 (0.7–1.0) | |||
| Examination | Temperature‡ | 1.9 (1.2–3.0) | 1.25 (0.77–2.04) | 0.8 (0.6–0.9) | 0.96 (0.87–1.06) |
| Costovertebral angle tenderness | 1.4 (0.8–2.4) | 0.9 (0.8–1.0) | |||
| Confusion | 0.33 (0.10–1.11) | 1.05 (1.01–1.09) | |||
Where more than one study results reported, that with highest positive LR and/or lowest negative LR presented.
In female adults’ temperature >37.2°C reported; in older adults’ temperature >37.9°C reported. CI, confidence interval; LR, likelihood ratio; RACF, residential aged care facility.
Definitions of UTI mandate the presence of genitourinary symptoms. However, the accuracy of genitourinary symptoms alone (Table 3) is poor. This may in part, be contributed to by lack of precision in defining the symptoms examined in these studies. For example, dysuria is widely described as a symptom of UTI. However, in older people, it is critical to establish whether the dysuria is acute or chronic. Chronic dysuria may be due to atrophic vaginitis in females and chronic prostatitis in males, or bladder malignancy.21
Isolated malodorous22–24 or cloudy urine23,24 are not represented in Table 3. Australian Therapeutic Guidelines: Antibiotics25 state that there is no indication to test urine in RACF residents on the basis of isolated malodour or cloudiness.
A significant proportion of urine tests in ED occur in the context of non-specific symptoms, altered mental state and falls.1 Delirium alone does not increase the likelihood ratio for UTI, but it should be considered in the entire context of assessing UTI risk, including assessment for alternative causes of delirium.26,27 Falls may be associated with UTI in the setting of urinary urgency, frequency, nocturia and incontinence.28 However, there is no routine indication for urine testing in those presenting with a fall without localising urinary symptoms.12,29
A history of rigors or shaking chills is a predictor of bacteraemia in older persons (adjusted odds ratio 3.06, 95% confidence interval [CI] 1.3–7.19), with UTI being the most common cause of bacteraemia in this cohort;30 therefore those presenting to ED with rigors and no obvious alternative aetiology should have UTI considered as a potential cause.
Testing
Urine collection method
Most mid-stream urines collected in ED are collected from older patients with no staff assistance and receiving no instructions on urine collection.31 Correct midstream clean-catch technique, in one study, was used in only 6% of collected specimens.31 In both men and women, it is recommended that midstream urine collection with prior cleansing be used.32 A prospective study, albeit in younger women, found that instructions to hold labia apart during sampling halved contamination rates of urine samples.33 Use of catheterisation to obtain urine specimens is associated with a significantly lower proportion of contaminated urines on both microscopy and culture, bearing in mind the procedure may cause harm and distress.1 This is the preferred approach for urine collection in those with significant cognitive impairment.
For patients with a long-term indwelling catheter, it is imperative to remove it and collect urine from a freshly inserted catheter to test for UTI.
The dipstick urine
ED studies of the utility of dipstick urine in older persons are limited by inclusion of those with contaminated urine samples and/or ASB, with resultant significant misclassification bias. In a study that included patients with UTI associated with bacteraemia, dipstick urine was 96.9% sensitive (95% CI 93.7–98.6) when both leukocyte esterase and nitrites were positive, with a false-positive rate of 42.4% (95% CI 41–43.8).34 Addition of urine microscopy with a cut-point of >10 white blood cells per high power field, decreased sensitivity to 78.1% (95% CI 72.2–83.0) but false positives decreased to 20.1% (95% CI 19–21.3). In a prospective observational study of older ED patients without focal urinary symptoms, dipstick urine had a positive predictive value of 37% and a negative predictive value of 92%.26 Therefore, the value of a negative urinalysis in ruling out UTI is greater than the rule-in value of a positive result, but neither should be relied on in isolation of history and examination findings.
Urine microscopy
Urine microscopy for leucocyte counts in those aged 60 years and older has a 80% sensitivity and 67% specificity for positive urine culture, with an associated 40.5% positive predictive value and 92.2% negative predictive value.35 Pyuria on microscopy is generally defined as >10 leukocytes per high powered field.14 In contrast, bacterial counts on microscopy have a sensitivity of 92.3% and specificity of 91.4% with a positive predictive value of 75% and a negative predictive value of 97.4% for positive culture.35 These results must still be interpreted in the complete context of initial likelihood of UTI and severity of current illness when determining whether to proceed with empiric antibiotic treatment, because pyuria is found in 94% of those with ASB.36
Urine culture
Jones et al. developed a protocol, which entailed reflex urine culture cancellation on the basis of low-risk findings for infection on urinalysis, with a reduction in performance of cultures by 39.1%, with 1.8% of those cultures identified to be suitable for cancellation, subsequently being positive for an organism.37 Validation studies of this protocol have identified a 34.6% absolute reduction in number of urine cultures completed, with 2.3% of cultures suitable for cancellation in males and 6.9% in females being positive for an organism.38
Additional assessment to guide management
If UTI is deemed likely, the next steps are to determine:
Is the UTI uncomplicated or complicated? A complicated UTI is one with structural or functional abnormality in the urinary tract; a history of urinary instrumentation; or concurrent systemic diseases such as renal impairment, transplantation or immunodeficiency.39
Is this a lower UTI (cystitis) versus upper UTI (pyelonephritis)?
In older men with lower UTI symptoms, is the prostate tender on rectal examination, suggesting potential prostatitis?40
Are there risk factors for multi-resistant organisms, such as recent travel to developing countries, antibiotic usage or hospitalisation?
Who to treat, and when, if diagnosis is not definitive?
As we have noted, the definition of UTI requires a culture result mostly unavailable in ED. In older community-dwelling adults, the decision to prescribe antibiotics for a presumptive diagnosis of UTI should be individualised against the following criteria (summarised in Fig. 1):
Figure 1.

Decision-making process in assessment of community-dwelling older persons for UTI.14 (Reprinted and adapted from Infectious Diseases Clinics 31(4). Copyright (2017), with permission from Elsevier).
The presence or absence of localising symptoms;
Where non-localising symptoms alone are present, including results of an assessment to identify infection at an alternate site;
Results of the non-definitive urine test you have done in ED (dipstick or microscopy);
Presence of clinical instability.
In RACF residents, a cluster randomised controlled trial identified that implementation of a diagnostic algorithm for UTIs in RACFs was associated with fewer courses of antibiotics, with no significant increase in admissions to hospital or mortality.41 The Australian Therapeutic Guidelines: Antibiotics suggest a similar algorithm for UTI diagnosis in RACF residents (Fig. 2), where urine testing is selective.25
Figure 2.
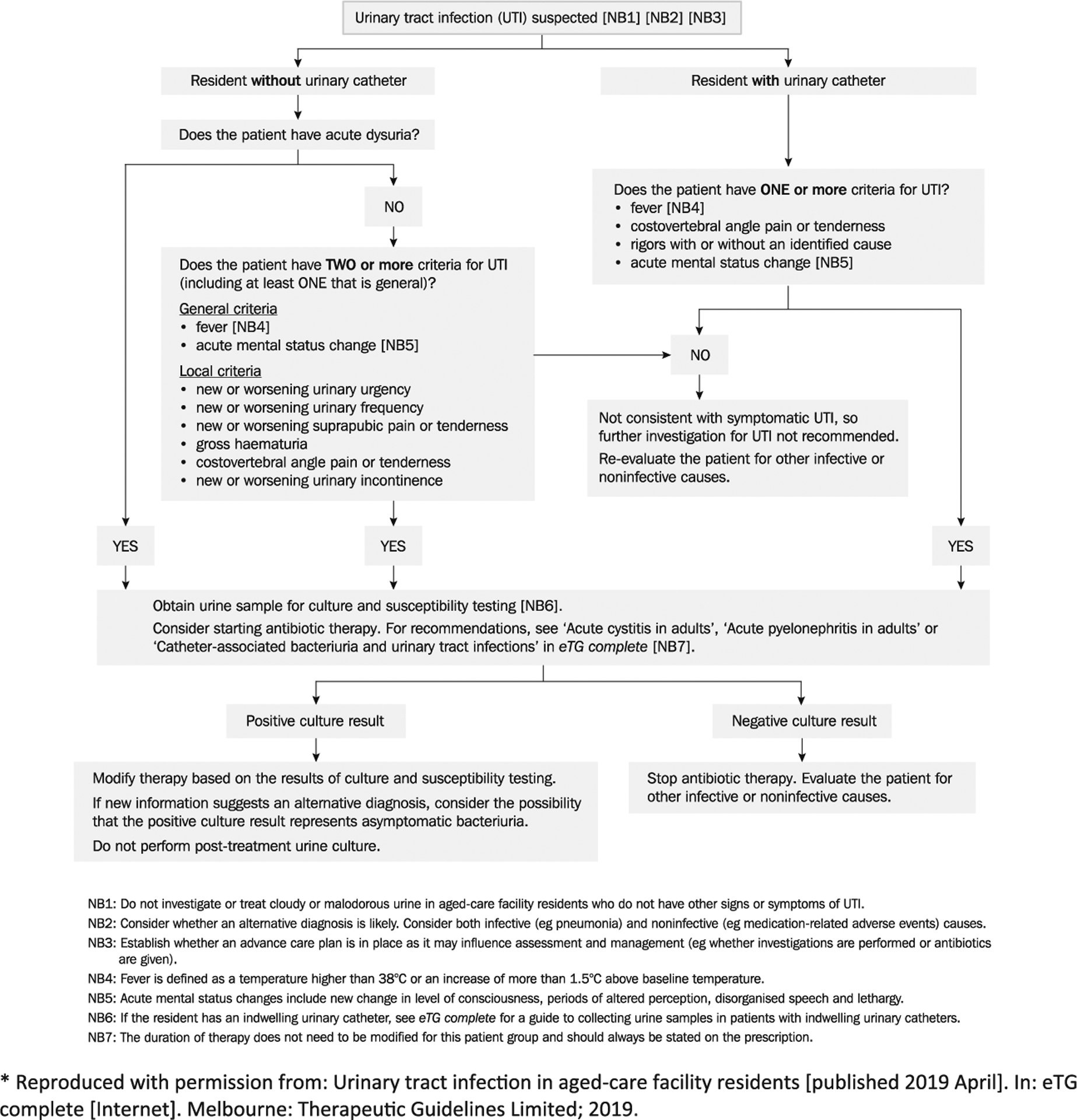
Assessment and treatment of aged-care facility residents with suspected urinary tract infection.25 (Reproduced with permission from: Urinary tract infection in aged-care facility residents [published 2019 April]. In: eTG complete [Internet]. Melbourne: Therapeutic Guidelines Limited; 2019).
Transitional communication and risk minimisation
Transitional communication to the general practitioner when discharging an older person from ED with a diagnosis of UTI may emphasise recommendations to reduce recurrent UTI, including where relevant:
Treatment of atrophic vaginitis with vaginal oestrogens – this may reduce recurrent UTIs in post-menopausal women;42
Assessment for incomplete bladder emptying and addressing causes of high post-void residuals of ≥200 mL, such as prostatic hypertrophy;13
Review of the indication for indwelling catheters and arrangement of a trial of void where appropriate;
Implementation of a falls risk minimisation plan where the older person is experiencing symptoms such as urinary urgency, frequency, nocturia or incontinence. This may include, for instance, use of continence pads, keeping a commode at the bedside and increased supervision of mobilisation; and
It may also be emphasised that if clinical cure has been achieved, there is no role for repeat urine testing in the older person after completion of the course of antibiotics for uncomplicated lower UTI.
Conclusion
There are several critical points for the ED physician to consider in diagnosing UTI in older adults:
Urinalysis or urine microscopy should only be ordered where the history and examination suggest likely UTI.
Routine indiscriminate urinalysis or urine microscopy is to be avoided.
For those unwell with non-localising acute symptoms where UTI is part of the differential diagnosis, err on the side of looking for alternative diagnoses before testing urine, as the risk of detecting ASB that has no causal relationship to the nonspecific symptoms is substantial.
Meticulous attention to how the urine is collected is required. However, catheter specimen urine collection of people with cognitive and sensory impairments is distressing, invasive and only necessary if the pre-test probability for UTI is sufficient.
There is significant room for improvement of ED assessment of UTI in older persons with an imperative to assess clinical probability of UTI prior to ordering urine microscopy and culture. The current practice of widespread, indiscriminate testing of urines for UTI in older persons risks avoidable morbidity for individuals and may contribute to increasing prevalence of multi-resistant organisms. Furthermore, anchoring onto a diagnosis of UTI in settings where this is not clinically supported, means that the true underlying cause of the persons presentation may go unrecognised and untreated.
Footnotes
Competing interests
None declared.
Antibiotic Expert Groups, Therapeutic Guidelines: Antibiotics. Vol. Version 16. 2019, Melbourne: Therapeutic Guidelines limited.
References
- 1.Gordon LB, Waxman MJ, Ragsdale L, Mermel LA. Over-treatment of presumed urinary tract infection in older women presenting to the emergency department. J. Am. Geriatr. Soc 2013; 61: 788–92. [DOI] [PubMed] [Google Scholar]
- 2.Caterino JM, Leininger R, Kline DM et al. Accuracy of current diagnostic criteria for acute bacterial infection in older adults in the emergency department. J. Am. Geriatr. Soc 2017; 65: 1802–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J. Am. Geriatr. Soc 2009; 57: 107–14. [DOI] [PubMed] [Google Scholar]
- 4.Finucane TE. ‘Urinary tract infection’: requiem for a heavyweight. J. Am. Geriatr. Soc 2017; 65: 1650–5. [DOI] [PubMed] [Google Scholar]
- 5.Aragon IM, Herrera-Imbroda B, Queipo-Ortuño M et al. The urinary tract microbiome in health and disease. Eur. Urol. Focus 2018; 4: 128–38. [DOI] [PubMed] [Google Scholar]
- 6.Mulder M, Radjabzadeh D, Hassing RJ et al. The effect of antimicrobial drug use on the composition of the genitourinary microbiota in an elderly population. BMC Microbiol. 2019; 19: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abrutyn E, Mossey J, Berlin JA et al. Does asymptomatic bacteriuria predict mortality and does antimicrobial treatment reduce mortality in elderly ambulatory women? Ann. Intern. Med 1994; 120: 827–33. [DOI] [PubMed] [Google Scholar]
- 8.Abrutyn E, Berlin J, Mossey J, Pitsakis P, Levison M, Kaye D. Does treatment of asymptomatic bacteriuria in older ambulatory women reduce subsequent symptoms of urinary tract infection? J. Am. Geriatr. Soc 1996; 44: 293–5. [DOI] [PubMed] [Google Scholar]
- 9.Boscia JA, Kobasa WD, Knight RA, Abrutyn E, Levison ME, Kaye D. Therapy vs no therapy for bacteriuria in elderly ambulatory non-hospitalized women. JAMA 1987; 257: 1067–71. [PubMed] [Google Scholar]
- 10.Nicolle LE, Mayhew WJ, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am. J. Med 1987; 83: 27–33. [DOI] [PubMed] [Google Scholar]
- 11.Rowe TA, Juthani-Mehta M. Urinary tract infection in older adults. Aging Health 2013; 9: 519–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicolle LE, Gupta K, Bradley SF et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin. Infect. Dis 2019; 68: 1611–5. [DOI] [PubMed] [Google Scholar]
- 13.Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect. Dis. Clin. North Am 2014; 28: 75–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cortes-Penfield NW, Trautner BW, Jump RLP. Urinary tract infection and asymptomatic bacteriuria in older adults. Infect. Dis. Clin. North Am 2017; 31: 673–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonkat G, Bartoletti RR, Bruyère F et al. European Association of Urology Urological Infections Guideline: 2019. [Cited 2 May 2019.] Available from URL: https://uroweb.org/guideline/urological-infections/#3 [Google Scholar]
- 16.Yu Y, Zielinski MD, Rolfe MA et al. Similar neutrophil-driven inflammatory and antibacterial responses in elderly patients with symptomatic and asymptomatic bacteriuria. Infect. Immun 2015; 83: 4142–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mayne S, Bowden A, Sundvall PD, Gunnarsson R. The scientific evidence for a potential link between confusion and urinary tract infection in the elderly is still confusing - a systematic literature review. BMC Geriatr. 2019; 19: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amarsy R, Guéret D, Benmansour H et al. Determination of Escherichia coli phylogroups in elderly patients with urinary tract infection or asymptomatic bacteriuria. Clin. Microbiol. Infect 2019; 25: 839–44. [DOI] [PubMed] [Google Scholar]
- 19.Artero A, Esparcia A, Alberola J, Madrazo M, Nogueira JM, Eiros JM. Prospective cohort study of risk factors for extended-spectrum ß-lactamase-producing Escherichia coli urinary tract infections in elderly patients admitted to hospital. Int J Clin Pract. 2017; 71: e13001. [DOI] [PubMed] [Google Scholar]
- 20.Rogers BA, Ingram PR, Runnegar N et al. Community-onset Escherichia coli infection resistant to expanded-spectrum cephalosporins in low-prevalence countries. Antimicrob. Agents Chemother 2014; 58: 2126–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts RG, Hartlaub PP. Evaluation of dysuria in men. Am. Fam. Physician 1999; 60: 865–72. [PubMed] [Google Scholar]
- 22.Midthun SJ, Paur R, Lindseth G. Urinary tract infections. Does the smell really tell? J. Gerontol. Nurs 2004; 30: 4–9. [DOI] [PubMed] [Google Scholar]
- 23.Loeb M, Bentley DW, Bradley S et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect. Control Hosp. Epidemiol 2001; 22: 120–4. [DOI] [PubMed] [Google Scholar]
- 24.Gbinigie O, Ordóñez-Mena JM, Fanshawe TR, Plüddemann A, Heneghan C. Diagnostic value of symptoms and signs for identifying urinary tract infection in older adult outpatients: systematic review and meta-analysis. J. Infect. 2018; 77: 379–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antibiotic Expert Groups. Therapeutic Guidelines: Antibiotics. Vol. Version 16. Melbourne: Therapeutic Guidelines Limited, 2019. [Google Scholar]
- 26.Ducharme J, Neilson S, Ginn J. Can urine cultures and reagent test strips be used to diagnose urinary tract infection in elderly emergency department patients without focal urinary symptoms? CJEM 2007; 9: 87–92. [DOI] [PubMed] [Google Scholar]
- 27.Caterino JM, Kline DM, Leininger R et al. Nonspecific symptoms lack diagnostic accuracy for infection in older patients in the emergency department. J. Am. Geriatr. Soc 2019; 67: 484–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soliman Y, Meyer R, Baum N. Falls in the elderly secondary to urinary symptoms. Rev. Urol 2016; 18: 28–32. [PMC free article] [PubMed] [Google Scholar]
- 29.Schulz L, Hoffman RJ, Pothof J, Fox B. Top ten myths regarding the diagnosis and treatment of urinary tract infections. J. Emerg. Med 2016; 51: 25–30. [DOI] [PubMed] [Google Scholar]
- 30.Taniguchi T, Tsuha S, Takayama Y, Shiiki S. Shaking chills and high body temperature predict bacteremia especially among elderly patients. Springerplus 2013; 2: 624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pallin DJ, Ronan C, Montazeri K et al. Urinalysis in acute care of adults: pitfalls in testing and interpreting results. Open Forum Infect. Dis 2014; 1: ofu019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.LaRocco MT, Franek J, Leibach EK et al. Effectiveness of preanalytic practices on contamination and diagnostic accuracy of urine cultures: a laboratory medicine best practices systematic review and meta-analysis. Clin. Microbiol. Rev 2016; 29: 105–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baerheim A, Digranes A, Hunskaar S. Evaluation of urine sampling technique: bacterial contamination of samples from women students. Br. J. Gen. Pract 1992; 42: 241–3. [PMC free article] [PubMed] [Google Scholar]
- 34.Shimoni Z, Glick J, Hermush V, Froom P. Sensitivity of the dipstick in detecting bacteremic urinary tract infections in elderly hospitalized patients. PLoS One 2017; 12: e0187381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yusuf E, Van Herendael B, van Schaeren J. Performance of urinalysis tests and their ability in predicting results of urine cultures: a comparison between automated test strip analyser and flow cytometry in various sub-populations and types of samples. J. Clin. Pathol 2017; 70: 631–6. [DOI] [PubMed] [Google Scholar]
- 36.Boscia JA, Abrutyn E, Levison ME, Pitsakis PG, Kaye D. Pyuria and asymptomatic bacteriuria in elderly ambulatory women. Ann. Intern. Med 1989; 110: 404–5. [DOI] [PubMed] [Google Scholar]
- 37.Jones CW, Culbreath KD, Mehrotra A, Gilligan PH. Reflect urine culture cancellation in the emergency department. J. Emerg. Med 2014; 46: 71–6. [DOI] [PubMed] [Google Scholar]
- 38.Hertz JT, Lescallette RD, Barrett TW, Ward MJ, Self WH. External validation of an ED protocol for reflex urine culture cancelation. Am. J. Emerg. Med 2015; 33: 1838–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mody L, Juthani-Mehta M. Urinary tract infections in older women: a clinical review. JAMA 2014; 311: 844–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sharp VJ, Takacs EB, Powell CR. Prostatitis: diagnosis and treatment. Am. Fam. Physician 2010; 82: 397–406. [PubMed] [Google Scholar]
- 41.Loeb M, Brazil K, Lohfeld L et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ 2005; 331: 669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Obstet. Gynecol 2008; 112: 689–90. [DOI] [PubMed] [Google Scholar]
- 43.Nicolle LE, Bradley S, Colgan R et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin. Infect. Dis 2005; 40: 643–54. [DOI] [PubMed] [Google Scholar]
- 44.Nicolle LE. Asymptomatic bacteriuria in the elderly. Infect. Dis. Clin. North Am 1997; 11: 647–62. [DOI] [PubMed] [Google Scholar]
- 45.Rodhe N, Löfgren S, Matussek A et al. Asymptomatic bacteriuria in the elderly: high prevalence and high turnover of strains. Scand. J. Infect. Dis 2008; 40: 804–10. [DOI] [PubMed] [Google Scholar]
- 46.Nicolle LE. Urinary tract infections in the older adult. Clin. Geriatr. Med 2016; 32: 523–38. [DOI] [PubMed] [Google Scholar]
- 47.Norris DL Young JD 2nd. Urinary tract infections: diagnosis and management in the emergency department. Emerg. Med. Clin. North Am 2008; 26: 413–30, ix. [DOI] [PubMed] [Google Scholar]
- 48.Meister L, Morley EJ, Scheer D, Sinert R. History and physical examination plus laboratory testing for the diagnosis of adult female urinary tract infection. Acad. Emerg. Med 2013; 20: 631–45. [DOI] [PubMed] [Google Scholar]
- 49.Leman P Validity of urinalysis and microscopy for detecting urinary tract infection in the emergency department. Eur. J. Emerg. Med 2002; 9: 141–7. [DOI] [PubMed] [Google Scholar]
- 50.Wigton RS, Hoellerich VL, Ornato JP, Leu V, Mazzotta LA, Cheng IH. Use of clinical findings in the diagnosis of urinary tract infection in women. Arch. Intern. Med 1985; 145: 2222–7. [PubMed] [Google Scholar]


