Abstract
Traditional Chinese medicine (TCM) has been successfully used to treat asthmatic conditions for centuries. Nevertheless, the current hotspots and research frontiers on TCM for asthma have not been systematically investigated on the basis of bibliometric analysis. In this study, a scientometric analysis (1991-2021) was carried out on 3081 journal articles obtained from the Web of Science Core Collection database to explore the basic characteristics, research hotspots, and frontiers of TCM in asthma research. The results revealed the following: (1) Research on TCM in asthma has received widespread attention since the beginning of the 21st century; perhaps 2009 was an important turning point. TCM in asthma research shows a trend of interdisciplinary development. (2) Well-known universities/institutions in China, the United States, and South Korea have conducted the main body of current TCM research in asthma. JingCheng Dong (Fudan University, China) and XiuMin Li (Mount Sinai School of Medicine, USA) are the top 2 leading authors in this field. However, there is still a lack of international cooperation in the field of TCM in asthma research, and the influence of researchers in China and South Korea still needs improvement. (3) The Journal of Allergy and Clinical Immunology ranks first in the research field on the influence of TCM in asthma. (4) Hotspots and frontiers of TCM in asthma are provided according to the timeline analyses of the research. In the former, complementary medicine, alternative treatment, allergic rhinitis, airway remodeling, Dietary Approach to Stop Hypertension diet, and eosinophilic esophagitis are in the exploratory stage. In the latter, pharmacology, essential oil, gut microbiota, and oxidative stress were investigated from 2006 until late 2021 as period B, which contradicts period A (1991-2005). Moreover, limitations of this bibliometric analysis and the study of TCM research in asthma still exist, which are sufficiently important to warrant further investigations. Finally, we propose the significant importance of the real quintessence and characteristics of TCM in clinical and future research.
Key words: Traditional Chinese Medicine, asthma, bibliometric analysis, hotspot, frontier
Asthma is a chronic inflammatory disease that affects the airways of the lungs and is now a major public health problem. Asthma affects 262 million people worldwide and causes almost half a million deaths per year.1,2 Epidemiologic studies show an annual increase in the number of diagnosed patients with asthma, indicating that half a billion people will suffer from some kind of asthma-related condition by 2025.3 Asthma is still an incurable disease, and the concept of continuous “asthma control” was proposed by the Global INitiative for Asthma in 2009.4 Thereafter, current treatments have targeted asthma symptoms to reduce the risk of severe inflammation and obstruction of the airways.1 However, despite asthma control treatments, a significant proportion of patients with asthma do not achieve sustained asthma control5,6 and the long-term use of medication for managing this condition places a substantial burden on health care resources.7 Under these circumstances, potential alternatives to asthma treatment are needed.
Traditional Chinese medicine (TCM) involves a broad range of therapies that share common medicinal concepts developed in China for more than 2500 years.8 TCM includes different, but complementary, forms of treatments, such as herbal medicine, acupuncture, moxibustion, and manipulation. A series of Chinese herbal formulas have been cataloged since the Eastern Han Dynasty (25-220 AD) to treat asthma and asthmatic conditions. For example, the classic monograph “Treatise on Cold Damage and Miscellaneous Diseases” written by Zhang Zhongjing (150-219 AD), the medical saint in China, reported the treatment of different types of asthma with herbal formulas (eg, Xiao Qing Long Tang, Ma Xing Shi Gan Tang, and Ma Huang Tang). Currently, these herbal formulas still play an important role in Chinese society and health care. Fundamental and clinical studies have suggested that TCM-based therapies do prevent asthma attacks and improve the patient’s condition.9, 10, 11
With asthma problems increasing globally, studies based on TCM and asthma control have intensified12,13 and expanded in scope from the medical field to include human society and the national economy.14 However, considering the large number of publications and the diversity of topics covered, a quantitative analysis of studies on TCM in asthma is needed to understand the current status, hotspots, and frontiers. Research hotspots are current science issues or special subjects addressed by a cluster of studies with interconnections over a short period of time. Research frontiers are research issues and fields with the featuresof being the newest, most advanced, and with potential development.15 In the present study, we conducted a systematic review and a visual bibliometric analysis (CiteSpace software and the Online Analysis Platform of Literature Metrology [OAPLM]) of published data on TCM in asthma treatment to explore research hotspots and frontiers, and form a panoramic knowledge network structure.
Methods
In the present study, CiteSpace software16, 17, 18 and the OAPLM platform (http://bibliometric.com/) were used to conduct a visual bibliometric analysis of published works on TCM and asthma from 1991 to 2021. CiteSpace software, as the primary analysis software, is used for analyzing collaborative institutions, authors with the most publications, preferred journals, most-cited publications, hotspots, and frontiers. The OAPLM platform, as a supplementary analysis tool, is used to analyze the trends of publication and cooperation between countries. We obtained different visual knowledge maps by setting different parameters, such as term source (keyword) and node type (country/institution, cited author, keyword/term, and cited reference).
Data sources and search strategies
A literature search was conducted using the Web of Science Core Collection database on September 14, 2021. We used the following keywords: for traditional Chinese medicine, Topic = (Traditional Chinese Medicine or Traditional Chinese and Western Medicine or Chinese Medicine or Chinese Patent Medicine or TCM or a decoction of medicinal ingredients or decoction or herb or Chinese herbology or herbal or ethnodrug or popular prescription or Chinese herbal pieces or hospital preparations or acupuncture or needling or needle or acupoints or acupoint application or trigger point or fire needle or electroacupuncture or electro-acupuncture or manual acupuncture or hand acupuncture or auricular needle or auriculo-acupuncture or ear acupuncture or pyonex or three-edged needle or plum blossom needle or scalp acupuncture or dermal needle or channels and collaterals or meridian or acupuncture and moxibustion or moxibustion or moxa-moxibustion or burnt mugwort therapy or acupotomy or sunken cord or cupping or heated cup therapy or gallipot or manipulation or massage or tuina or scraping or guasha or scraping therapy or qigong or Tai Ji or five-element music or Tao yin or dietary therapy or treatment based on syndrome differentiation). For asthma, Topic = (asthma or asthmatic or anti-asthmatic or antiasthma or bronchial hyperreactivity or respiratory hypersensitivity). After a primary data search, researchers screened the manuscripts to ensure their relevance to the present study. The inclusion criteria were as follows: (1) Document Type: Articles and Review articles; (2) Timespan: January 1, 1991, to September 14, 2021; (3) For the OAPLM platform, Web of Science Index: Science Citation Index Expanded. Exclusion criteria: Duplicated articles were removed.
CiteSpace software analysis
Full records and cited references of these publications were downloaded from the Web of Science Core Collection database, saved in text format (.txt), and then imported into CiteSpace software V5.8 R1 SE, 64 bits (Drexel University, Philadelphia, Pa), using the following settings: time slicing from January 1991 to September 2021, years per slice choosing 1. We used the method conducted by Luo et al.19 The selection used a modified g index in each slice: . For interinstitutional analysis, we selected “Institution” as the node type and default values for other settings. For coauthorship network analysis, we selected “Author” as the node type. For document cocitation, we selected the following parameters: “References” as the node type, and “Pathfinder” and “Pruning the merged network” as the Pruning parameter to highlight important structural features. For keywords detection, we selected “Keywords” as node type and “Burst Terms” as term type and the “Cosine” option to calculate burst strength. We selected the first 24 keywords with the strongest burst strength. In CiteSpace, betweenness centrality measures the number of times a node (eg, 1 article, 1 author) lies on the shortest path between other nodes. Generally, a node of high centrality is usually one that connects 2 or more large groups of nodes, and has a significant influence on a network.20
Bibliometric online platform analysis
For publication trends among countries and intercountry/regional cooperation analysis, we used the OAPLM platform (http://bibliometric.com/). Full records and cited references of these publications were downloaded from the Web of Science Core Collection database. We set the Web of Science Index to “Science Citation Index Expanded,” and saved it in UTF-8 format. We then exported all filtered data into the OAPLM platform for a “total literature analysis.” For intercountry/regional analysis, we chose “partnership analysis.”
Results
Analysis of published articles
A total of 3082 publications met the inclusion criteria, and 1 publication was removed because of duplication. We then identified 2343 articles, 640 review articles, 64 proceedings papers, 17 book chapters, 16 early access articles, and 1 data article from the 3081 selected studies. A total of 3081 articles were included in the final analysis in CiteSpace software. Meanwhile, 2820 Science Citation Index Expanded articles were qualified and included in the final analysis on the OAPLM platform.
From our initial results, we divided TCM and asthma publications into 2 separate periods (Fig 1, A): an early stage (1991-2008) with fewer than 100 publications/y and a late stage (2009-2021) with more than 100 publications/y, reaching more than 200 publications/y in the last 5 years of the study. To determine which countries/regions published the highest number of works related to TCM and asthma, we used the online analysis OAPLM platform. The bar chart shows the total number of articles published by the top 10 countries/regions over a 30-year time period, with China ranking first followed by the United States and South Korea (Fig 1, B). Overall, these results indicate a growing trend in TCM in asthma research and it has attracted considerable worldwide attention.
Fig 1.
A, Number of annual research publications and publication trends on TCM in asthma from 1991 to 2021. B, Number of annual publications and publication trends of the top 10 countries/regions on TCM research in asthma from 1991 to 2021. Data for 2021 were collected until September 14.
Analysis of intercountry/regional and interinstitutional cooperation
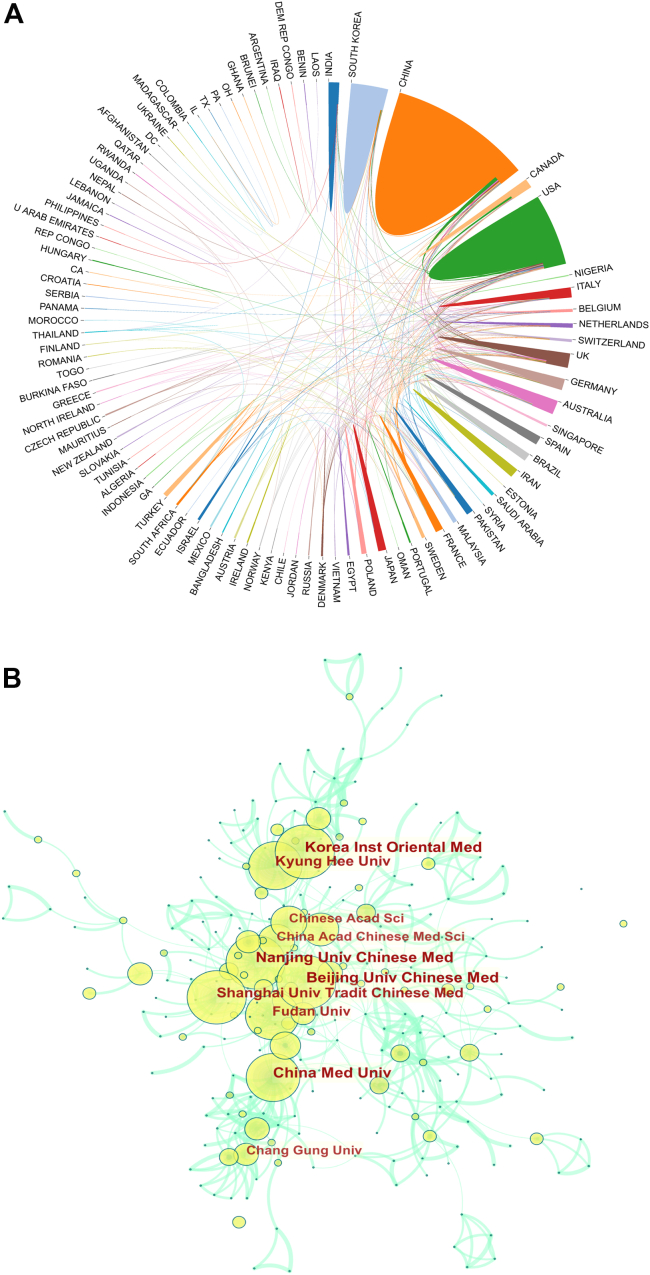
We analyzed the scientific cooperation among countries/regions with the OAPLM platform. Our results indicate that research partnerships occurred in 90 countries/regions, with special attention to China, the United States, and South Korea (Fig 2, A). We then determined the cooperative strength among institutions with CiteSpace software, and our results revealed 783 nodes and 804 links from different institutions (Fig 2, B). The Beijing University of Chinese Medicine and the Korea Institute of Oriental Medicine ranked as the most collaborative institutions, followed by the Nanjing University of Chinese Medicine and the China Medicine University. Among the top 10 institutions, 8 are Chinese and 2 are South Korean (Fig 2, B; Table I).
Fig 2.
A, Collaboration efforts between 90 countries/regions on TCM in asthma from 1991 to 2021. B, CiteSpace network map of institutions involved in TCM and asthma research. Each circle in the map represents an institution. The size of the circle is positively correlated with the number of articles published by the institution, and the link between the 2 circles represents the collaboration between 2 institutions on the same article. There is a positive correlation between the line thickness and cooperation frequency. The top 10 institutions with the most publications are shown. (Beijing Univ Chinese Med, Korea Inst Oriental Med, Nanjing Univ Chinese Med, China Med Univ, Kyung Hee Univ, Shanghai Univ Tradit Chinese Med, Fudan Univ, Chinese Acad Sci, Chang Gung Univ, and China Acad Chinese Med Sci were in the top 10.) Timespan: 1991 to 2021; Slice length = 1.
Table I.
The top 10 institutions related to TCM in asthma research publications from 1991 to 2021 (sorted by the number of publications, alternatively sorted by the year)
| Rank | Institutions | Year | Publication | Centrality |
|---|---|---|---|---|
| 1 | Beijing University of Chinese Medicine | 2009 | 55 | 0.02 |
| 1 | Korea Institute of Oriental Medicine | 2010 | 55 | 0.02 |
| 3 | Nanjing University of Chinese Medicine | 2009 | 54 | 0.01 |
| 4 | China Medical University | 2003 | 52 | 0.04 |
| 5 | Kyung Hee University | 2004 | 45 | 0.02 |
| 6 | Shanghai University of Traditional Chinese Medicine | 2012 | 44 | 0.01 |
| 7 | Fudan University | 2013 | 39 | 0.03 |
| 8 | Chinese Academy of Sciences | 2008 | 29 | 0.05 |
| 9 | Chang Gung University | 2003 | 28 | 0.01 |
| 9 | China Academy of Chinese Medical Sciences | 2009 | 28 | 0.03 |
Analysis of coauthorship network and core author distribution
The contribution of each author and coauthors in an article is ranked depending on where their names are placed in a list of authors. However, usually the corresponding authors who contribute the most are the last listed, and sometimes the authors are listed alphabetically. To avoid the above factors, we ranked authors and coauthors on the basis of the number of publications. Our results revealed 1041 nodes and 1366 links that showed the top 7 researchers with the highest number of publications (14 researchers in total) (Fig 3). JingCheng Dong (24 articles) from Huashan Hospital, Fudan University, China, ranks first on the list, followed by XiuMin Li (23 articles) from Mount Sinai School of Medicine, USA (Fig 3). Table II lists the authors, their respective institutions, total citations, and average citations per article. It reveals that the impact of most of these authors’ publications on the scientific community is low, and the overall impact of articles published by Chinese and South Korean authors is low despite their large number of publications. For example, the citation index of published works from China and South Korea reached 10.99 and 9.98, respectively. However, studies from the United States showed an impact index more than twice as high as that of their Asian counterparts at 25.07.
Fig 3.
CiteSpace network of coauthorship in the field of TCM on asthma research. Each circle in the network represents an author. The size of the circle is positively correlated with the number of articles published by the author, and the links between 2 circles represent the collaboration between 2 authors of the same article. There is a positive correlation between line thickness and cooperation frequency. The top 7 authors with the most publications are shown. Timespan: 1991 to 2021; Slice length = 1.
Table II.
The top 14 authors related to TCM in asthma research publications from 1991 to 2021 (sorted by the number of articles, alternatively sorted by the year)
| Rank | Author | Articles | Year | Total citations | Average citation per article | Institution | Country |
|---|---|---|---|---|---|---|---|
| 1 | JingCheng Dong | 24 | 2013 | 274 | 11.42 | Huashan Hospital, Fudan University | China |
| 2 | XiuMin Li | 23 | 2009 | 778 | 33.83 | Mount Sinai School of Medicine | United States |
| 3 | Meeyoung Lee | 15 | 2010 | 159 | 10.60 | Korea Institute of Oriental Medicine | South Korea |
| 4 | G. Ciprandi | 11 | 1993 | 695 | 63.18 | Casa di Cura Villa Mont allegro | Italy |
| 4 | Lijen Lin | 11 | 2012 | 77 | 7.00 | China Medical University | China of Taiwan |
| 4 | Jing Sun | 11 | 2014 | 139 | 12.64 | Huashan Hospital, Fudan University | China |
| 4 | Ying Wei | 11 | 2015 | 107 | 9.73 | Huashan Hospital, Fudan University | China |
| 8 | Qingli Luo | 10 | 2013 | 181 | 18.10 | Huashan Hospital, Fudan University | China |
| 8 | Changseob Seo | 10 | 2014 | 79 | 7.90 | Korea Institute of Oriental Medicine | South Korea |
| 10 | Hyeunkyoo Shin | 9 | 2014 | 103 | 11.44 | Korea Institute of Oriental Medicine | South Korea |
| 11 | Nan Yang | 8 | 2010 | 261 | 16.31 | New York Medical College | United States |
| 11 | Shungte Kao | 8 | 2012 | 75 | 9.38 | National Yang Ming Chiao Tung University | China of Taiwan |
| 11 | Yu Wang | 8 | 2012 | 69 | 8.63 | Shanghai Research Institute Acupuncture & Meridian | China |
| 11 | Jing Wang | 8 | 2014 | 38 | 4.75 | University of Geneva | Switzerland |
According to Place’s square root law,21 the core author formula is
Nmax is the number of articles of the most productive authors in the statistical period, and the authors who publish more than Nmin articles are the core authors in this field. In this study, the value of Nmax is 24; then, Nmin ≈ 3:669 is obtained, and the integer is 4. Therefore, if there are at least 4 published papers, then the author is called a core author. According to the price law, only when the core author group accounts for 50% of the total can a discipline core author group be formed. After calculation, the number of core authors in this field accounts for only 7.6% (79 authors, 468 articles) of the total number of articles (1041 authors, 1915 articles), indicating that researchers in TCM for asthma are relatively scattered and have not formed a core author group.
Analysis of journals and cocited journals
Our analysis with the Web of Science revealed that works were published in 1071 periodic journals, with the top 10 most cited journals listed in Table III. A total of 199 publications appeared in the Journal of Ethnopharmacology, followed by Evidence-Based Complementary and Alternative Medicine (86 publications) and Annals of Allergy, Asthma & Immunology (60 publications). Cocited journals refer to important journals cited in an article, and we list the top 10 journals with the highest number of citations in Table IV. The Journal of Allergy and Clinical Immunology (impact factor = 10.7) ranked first (1462 citations), followed by the American Journal of Respiratory and Critical Care Medicine (impact factor = 21.4; 904 citations) and Allergy (impact factor = 13.1; 870 citations).
Table III.
The top 10 journals related to TCM in asthma research from 1991 to 2021 (sorted by the record count)
| Rank | Journal | Record count | IF (2020) | JCR | Country |
|---|---|---|---|---|---|
| 1 | Journal of Ethnopharmacology | 199 | 4.36 | Q1/Q2 | The Netherlands |
| 2 | Evidence Based Complementary and Alternative Medicine | 86 | 2.629 | Q2 | Egypt |
| 3 | Annals of Allergy, Asthma & Immunology | 60 | 6.347 | Q1 | United States |
| 4 | Journal of Allergy and Clinical Immunology | 56 | 10.793 | Q1 | United States |
| 5 | Medicine | 37 | 1.889 | Q3 | United States |
| 6 | Journal of Asthma | 35 | 2.515 | Q3 | United States |
| 7 | PLoS One | 34 | 3.24 | Q2 | United States |
| 8 | Clinical and Experimental Allergy | 33 | 5.018 | Q2 | United Kingdom |
| 9 | Frontiers in Pharmacology | 33 | 5.81 | Q1 | Switzerland |
| 10 | International Immunopharmacology | 33 | 4.932 | Q2 | Netherlands |
IF, Impact factor; JCR, Quartile Journal Citation Report.
Table IV.
The top 10 cocited journals related to TCM in asthma research from 1991 to 2021 (sorted by the number of citations)
| Rank | Journal | Citation | Centrality | IF (2020) | JCR | Country |
|---|---|---|---|---|---|---|
| 1 | Journal of Allergy and Clinical Immunology | 1462 | 0.01 | 10.793 | Q1 | United States |
| 2 | American Journal of Respiratory and Critical Care Medicine | 904 | 0.01 | 21.405 | Q1 | United States |
| 3 | Allergy | 870 | 0.01 | 13.146 | Q1 | United Kingdom |
| 4 | Journal of Ethnopharmacology | 863 | 0.04 | 4.36 | Q1/Q2 | The Netherlands |
| 5 | New England Journal of Medicine | 856 | 0.01 | 91.245 | Q1 | United States |
| 6 | Lancet | 825 | 0 | 79.321 | Q1 | United Kingdom |
| 7 | Clinical and Experimental Allergy | 805 | 0.01 | 5.018 | Q2 | United Kingdom |
| 8 | European Respiratory Journal | 753 | 0 | 16.671 | Q1 | United Kingdom |
| 9 | Journal of Immunology | 713 | 0.01 | 5.422 | Q2 | United States |
| 10 | Thorax | 681 | 0.01 | 9.139 | Q1 | United Kingdom |
IF, Impact factor.
Analysis of document cocitation, clustered network, and hotspots
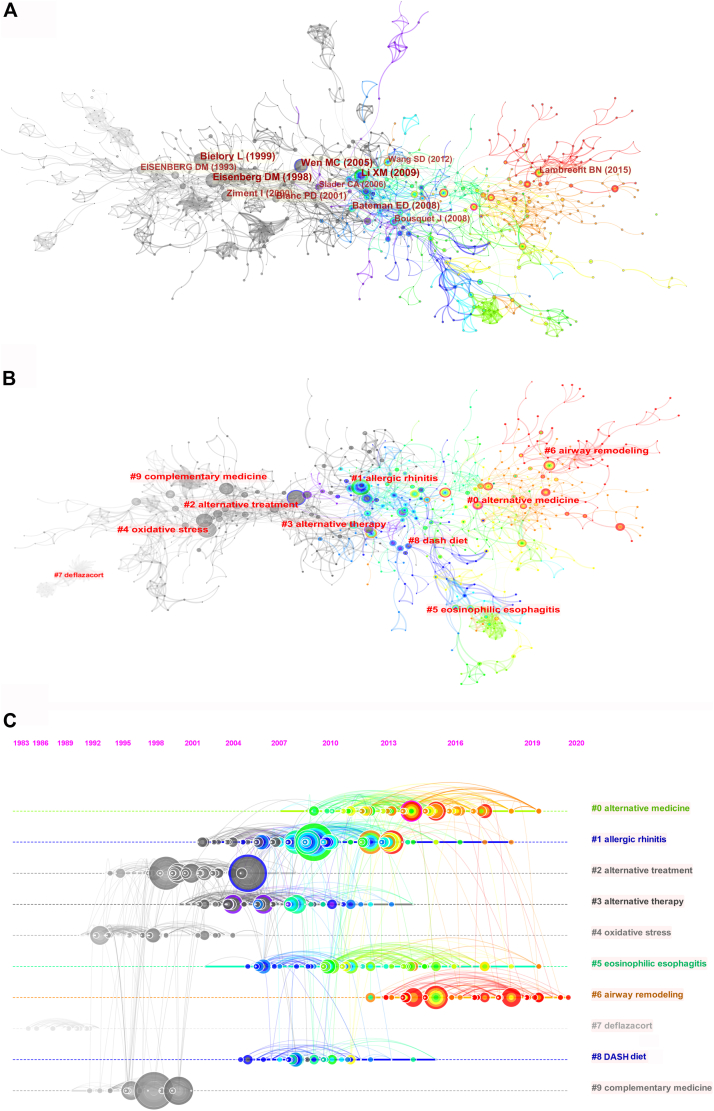
Document cocitation is a method developed by bibliometric research to identify articles cocited by a group of authors, and it measures the relationship between 2 different citations by their co-occurrence on the citation list.22 We used CiteSpace to analyze 116,137 valid references from the 3081 selected studies and identified homogeneous clusters of highly cited documents. We then built a network map with 1446 nodes and 3670 links (network density of 0.0035), as shown in Fig 4, A. The top 10 most cited references according to their cocited frequencies are listed in Table V.23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34
Fig 4.
A, CiteSpace cocitation map of 116,137 references on TCM in asthma research. The filter option shows the largest-connected component only. The year and first author of the top 10 most-cited publications are shown. Each circle in the map represents a reference. Circle size is positively correlated with the frequency of citations, and the links between 2 circles represent 2 references in the same article among the 3081 retrieved articles from this study. Similarly, line thickness is positively correlated with the cocitation frequency. Timespan: 1991 to 2021; Slice length = 1. B, Clustered networks of cocitation status of the 116,137 investigated references and the 3081 articles via CiteSpace. The filter option shows the minimum visible cluster size = 50 only. The top 10 largest clusters of citing publications are shown. C, The timeline view of the top 10 largest clusters of citing publications in the 116,137 investigated references and the 3081 articles via CiteSpace. The bolded timeline indicates that the clustering topic was a hotspot during this period. Citation tree-ring sizes on the timeline represent the high citation rates of the key reference. Right side = cluster labels.
Table V.
The top 12 most highly cited articles in TCM in asthma research from 1991 to 2021 (sorted by the cited frequency, alternatively sorted by the year)
| Rank | Title | First author | Journal | Year | Cited frequency | DOI |
|---|---|---|---|---|---|---|
| 1 | Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey | Eisenberg23 | JAMA-J Am Med Assoc | 1998 | 39 | 10.1001/jama.280.18.1569 |
| 2 | Efficacy and mechanisms of action of traditional Chinese medicines for treating asthma and allergy | Li24 | J Allergy Clin Immunol | 2009 | 37 | 10.1016/j.jaci.2008.12.026 |
| 3 | Efficacy and tolerability of anti-asthma herbal medicine intervention in adult patients with moderate-severe allergic asthma | Wen25 | J Allergy Clin Immunol | 2005 | 35 | 10.1016/j.jaci.2005.05.029 |
| 4 | Herbal interventions in asthma and allergy | Bielory26 | J Asthma | 1999 | 34 | 10.3109/02770909909065150 |
| 5 | Global strategy for asthma management and prevention: GINA executive summary | Bateman27 | Eur Respir J | 2008 | 29 | 10.1183/09031936.00138707 |
| 6 | Alternative medicine for allergy and asthma | Ziment28 | J Allergy Clin Immunol | 2000 | 27 | 10.1067/mai.2000.109432 |
| 7 | Alternative therapies among adults with a reported diagnosis of asthma or rhinosinusitis: data from a population-based survey | Blanc29 | Chest | 2001 | 26 | 10.1378/chest.120.5.1461 |
| 8 | The immunology of asthma | Lambrecht30 | Nat Immunol | 2015 | 25 | 10.1038/ni.3049 |
| 9 | Unconventional medicine in the United States. Prevalence, costs, and patterns of use | Eisenberg31 | N Engl J Med | 1993 | 23 | 10.1056/NEJM199301283280406 |
| 9 | Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen) | Bousquet32 | Allergy | 2008 | 23 | 10.1111/j.1398-9995.2007.01620.x |
| 11 | Complementary and alternative medicine use in asthma: who is using what? | Slader33 | Respirology | 2006 | 21 | 10.1111/j.1440-1843.2006.00861.x |
| 11 | Xiao-Qing-Long-Tang attenuates allergic airway inflammation and remodeling in repetitive Dermatogoides pteronyssinus challenged chronic asthmatic mice model | Wang34 | J Ethnopharmacol | 2012 | 21 | 10.1016/j.jep.2012.05.033 |
Our results revealed that the top-ranked reference is a national follow-up survey published in JAMA in 199823 followed by a review published in the Journal of Allergy and Clinical Immunology in 200924 and a randomized controlled trial published in the Journal of Allergy and Clinical Immunology in 2005.25 In the follow-up survey, the authors found that health expenditure on alternative medicine increased substantially between 1990 and 1997 due to an increase in the proportion of the population seeking alternative therapies, rather than increased visits per patient. The review analyzed 5 clinical studies published between 2005 and 2007 that used traditional Chinese herbal remedies to treat asthmatic conditions and discussed their effects and physiological mechanisms, including anti-inflammation, inhibition of airway smooth muscle (ASM) contraction, and immunomodulation. Finally, the randomized controlled trial compared the efficacy and safety of an extract of 3 herbs (Ling-Zhi [Ganoderma lucidum], Ku-Shen [Radix Sophora flavescentis], and Gan-Cao [Radix Glycyrrhiza uralensis]) versus prednisone therapy in patients with moderate to severe asthma and indicated that herbal therapy is a safe and efficient antiasthmatic therapy with fewer collateral effects than standard prednisone.
Cocitation analysis classifies relevant references in accordance with the degree of similarity in content, and then analyzes these references in each cluster. We generated cluster networks in a hierarchical order on the basis of cocitation status of the 116,137 references, revealing a significant modularity (Q = 0.873) of the clustering effect with a reliable silhouette (Silhouette = 0.8666). We identified 10 major clusters and cluster labels from citing articles with an log-likelihood ratio algorithm, including #0 alternative medicine, #1 allergic rhinitis, #2 alternative treatment, #3 alternative therapy, #4 oxidative stress, #5 eosinophilic esophagitis, #6 airway remodeling, #7 deflazacort, #8 Dietary Approach to Stop Hypertension (DASH) diet, and #9 complementary medicine (Fig 4, B). The number of cluster tags was inversely correlated with the number of articles for each cluster included (eg, the cluster of #0 contains the largest number of articles).
We then distributed cluster timelines according to their appearance in the literature and divided TCM and asthma into 2 stages: initial and exploratory (Fig 4, C). For example, #7, #9, #4, and #2 ran from approximately 1983 to 1993 (the initial stage of the research); #3, #1, #5, #8, #0, and #6 ran from approximately 1999 to 2012 (the exploratory stage of the research). In the initial stage (#7, #9, #4, and #2), publications cited 4 main literature topics, deflazacort (an oral corticosteroid), complementary medicine, oxidative stress, and alternative treatment. The publications focused on 2 main topics: oxidative stress and alternative treatment. In the exploratory stage (#3, #1, #8, #5, #0, and #6), studies referred to 6 major literature topics, alternative therapy, allergic rhinitis, DASH diet, eosinophilic esophagitis, alternative medicine, and airway remodeling. In addition, citation tree-rings of different sizes on the timeline represent key references with high citation rates.
Analysis of keywords, co-occurrence cluster, and research frontier
Keywords represent a summary of the research methods, objects, and contents of the article.35 The frequency of a keyword in an article reveals what topics are being explored.16 We then extracted the frequency of keywords in each article to identify research frontiers and trends by building a co-occurrence network. The most frequent keywords were “asthma,” “inflammation,” “children,” “expression,” “prevalence,” “airway inflammation,” “cell,” “acupuncture,” “extract,” “therapy,” “in vitro,” “disease,” “bronchial asthma,” “activation,” “allergy,” “cytokine,” “alternative medicine,” “inhibition,” “double blind,” and “allergic rhinitis” (Table VI). Combining the co-occurrence of keywords, we built a cluster map that reveals frontiers centered on #0 alternative medicine and #1 allergic asthma and the systematic analysis (#2 comprehensive review) of TCM (#0 alternative medicine) for asthma (#1 allergic asthma) control (#3 potential effect) (Fig 5, A). In fundamental research, medical diagnosis (#4 allergen-specific conjunctival challenge) with pathogenic factors (#5 oxidative stress and #6 lung microbiome) is often cited as a reason to explore TCM for asthma.
Table VI.
The top 20 most frequently used keywords related to TCM in asthma research from 1991 to 2021
| Rank | Keywords | Count | Centrality | Rank | Keywords | Count | Centrality |
|---|---|---|---|---|---|---|---|
| 1 | Asthma | 1215 | 0.18 | 11 | In vitro | 135 | 0.03 |
| 2 | Inflammation | 307 | 0.07 | 12 | Disease | 130 | 0.03 |
| 3 | Children | 280 | 0.05 | 13 | Bronchial asthma | 127 | 0.06 |
| 4 | Expression | 238 | 0.04 | 14 | Activation | 125 | 0.04 |
| 5 | Prevalence | 186 | 0.03 | 15 | Allergy | 124 | 0.06 |
| 6 | Airway inflammation | 174 | 0.03 | 16 | Cytokine | 121 | 0.02 |
| 7 | Cell | 165 | 0.04 | 17 | Alternative medicine | 118 | 0.02 |
| 8 | Acupuncture | 157 | 0.05 | 18 | Inhibition | 113 | 0.04 |
| 9 | extract | 149 | 0.05 | 19 | Double-blind | 112 | 0.04 |
| 10 | Therapy | 139 | 0.03 | 20 | Allergic rhinitis | 108 | 0.02 |
Fig 5.
A, Clustered networks of keywords of the 3081 articles via CiteSpace. All 7 clusters of keywords are shown. #0 alternative medicine, #1 allergic asthma, #2 comprehensive review, #3 potential effect, #4 allergen-specific conjunctival challenge, #5 oxidative stress, #6 lung microbiome. B, Keywords with the strongest burst strength of the 3081 articles on TCM in asthma research between 1991 and 2021. Keywords marked in red indicate a sudden increase in usage frequency of this keyword during this period. Keywords marked in blue indicate a relatively unpopular period.
Keywords burst refers to keywords whose frequency of citation increased over a short period of time. They are generally used as indicators of emerging topics and research frontiers.15 We generated burst keywords through CiteSpace (Fig 5, B). Combining keyword bursts with the analysis of research frontiers, we identified the research frontiers of 2 periods.
Period A, ranging from 1991 to 2005, explored the effects of TCM on controlling asthmatic conditions. Bronchial asthma ranked first (strength = 23.5), followed by alternative medicine (strength = 16.45), as the main research trend in publications from 1994 to 2008, a period in which randomized controlled trials showed a high number of publications.
Period B, ranging from 2006 until 2021, explored the mechanisms of TCM in asthma by modifying immune-cell (dendritic cells, T cells, regulatory T cells, etc) activity. Studies from this period targeted the biological mechanisms of asthma control in other tissues rather than the airways, such as the gut microbiota, as well as the development of new antiasthmatic drugs.
Discussion
In the present study, we analyzed 3081 studies over 30 years (1991-2021) of TCM therapies for asthmatic conditions. We identified and ranked studies on the basis of research publication trends, collaborative institutions, authors with the most publications, preferred journals, and most-cited publications. Analyses using CiteSpace revealed research hotspots through the cited literature and frontiers based on burst keywords over the years.
Publications related to TCM and asthma presented a significant increase after 2000, reaching approximately 150 articles/y by 2012 and almost 300 articles/y by 2020. China, the United States, and South Korea published the largest number of studies. However, Chinese and South Korean publications revealed a low scientific impact as measured by the total citations. Eight institutions from China and 2 from South Korea had the highest number of published studies. Beijing University of Chinese Medicine and the Korean Institute of Oriental Medicine were in the first ranks. Research hotspot and frontier analysis revealed that, during the 1990s, studies explored the effectiveness of TCM for controlling asthma symptoms, whereas from 2000 onward studies sought to explain the mechanisms of TCM in asthma control.
Discussion of hotspots
From the analysis of the cluster of networks and hotspots, we revealed a hotspot timeline of TCM in asthma since approximately 1983. TCM has spread rapidly around the world since the 1950s36 as a type of complementary and alternative medicine. Many international universities, colleges, and institutes of TCM have been established worldwide. There were 80 colleges of TCM in the United States from 1980 to 2005.37 During the initial stage of TCM in asthma research from 1983 to 1993, alternative treatment was the major hotspot, followed by oxidative stress, deflazacort, and complementary medicine. Oxidative stress is considered one of the pathophysiological mechanisms of asthma and has attracted the attention of asthma researchers in TCM.38 However, since approximately 2007, it has no longer been a hotspot in this field. Deflazacort used to be an oral medication for asthma39; however, it is now the first corticosteroid to be approved by the Food and Drug Administration for treating patients with Duchenne muscular dystrophy.40
During the exploratory stage from 1999 to 2012, alternative medicine became the major hotspot, followed by allergic rhinitis, alternative therapy, eosinophilic esophagitis, airway remodeling, and DASH diet. Among these, allergic rhinitis, airway remodeling, DASH diet, and eosinophilic esophagitis are the 4 emerging hotspot topics. A large number of studies have indicated that allergic rhinitis and asthma commonly occur together,41, 42, 43 and patients with allergic rhinitis are likely to develop bronchial asthma.44 Both allergic rhinitis and asthma organ systems are equipped with a common lymphoid network and can respond to airborne allergens by activating similar effector cells. There is strong anatomical, epidemiologic, pathophysiologic, clinical, and therapeutic evidence supporting the connection between allergic rhinitis and asthma.45 Currently, the prevalence of allergic rhinitis is on the rise. Studies have suggested that treating allergic rhinitis may interfere with disease progression and prevent the onset of asthma.46 However, very little is known about the risk factors responsible for the progression from allergic rhinitis to asthma. Further prospective studies on the effect of allergic rhinitis treatment on the development of asthma are needed. Similarly, asthma is often a comorbid condition in eosinophilic esophagitis in both children and adults.47 Both eosinophilic esophagitis and asthma are chronic immune-mediated conditions characterized by inflammatory changes in the mucosa and submucosa with infiltration of eosinophils.48 Indeed, facing the very same type of situation, the eosinophilic esophagitis-asthma relationship remains poorly characterized mechanistically and clinically. The good thing is that there is strong therapeutic evidence supporting that the use of certain herbs that relieve the symptoms of allergic rhinitis49 or eosinophilic esophagitis50 is usually also helpful in the treatment of asthma. Therefore, significant clinical and mechanistic work needs to be accomplished to understand better the relationship between asthma, allergic rhinitis, and eosinophilic esophagitis, and their interaction with other allergic diseases.
The DASH diet was the hotspot from approximately 2004 to 2015 in the field of TCM in asthma. According to both modern research and traditional Chinese knowledge, diet is an essential factor in the development of diseases. The influence of food on asthma outcomes is of growing interest, and some studies have suggested that a Western diet pattern could contribute to asthma symptoms in adults.51 Simultaneously, dietary changes, such as the introduction of the DASH diet, may have beneficial effects on reducing inflammatory status in adults with uncontrolled asthma.52 Because the central tenet in TCM “medicine and food share a common origin,” food materials can therefore be used to prevent or treat medical disorders. However, the dietary habits of patients with asthma and the diets beneficial to their rehabilitation are not commonly investigated in clinical practice.
Airway remodeling is another hotspot, and it occurs as a primary pathological feature of asthma. Studies reported that TCM formulas, such as Bu-Shen-Yi-Qi,53 Gu-Ben-Fang-Xiao,54 and Yang-He-Ping-Chuan,55 can decrease airway remodeling. Other studies reported that active ingredients extracted from Chinese herbal medicine, such as Icariin56 and Astragalus membranaceus,57 prevent airways remodeling. In asthma, excessive contraction of ASM is responsible for most symptoms of asthma. The ASM changes in asthma are based on 3 aspects: ASM structure, ASM function, and airway inflammation. Airway remodeling is the typical structural change that occurs in both large and small airways. Because Chinese medicine can alleviate the structural and functional changes in ASM, researchers have carried out many studies for antiasthma drug screening. However, most TCM studies focus on the structure and function of ASM, and not enough attention has been focused on the changes in ASM caused by airway inflammation.
Discussion of frontiers
We found that the frontiers of TCM asthma research in different historical periods are constantly changing. Dating back to the 19th century, TCM practice and development have been severely affected because of the increasing adoption of Western medicine in China.8 After the foundation of the People’s Republic of China (1949), the newly formed government endorsed TCM protection and development.58 However, with the spread of TCM worldwide, the “safety, efficacy, quality, availability, preservation and further development” of TCM are being questioned because of its seemingly underdeveloped scientific knowledge.37 Before TCM can be accepted partly or completely as a health-promoting resource, the chief problem is testing the efficacy of TCM. The second problem is generated inevitably from the idea that TCM is not as effective as Western medicine, and great efforts must be made to prove its efficacy in comparisons with Western medicine. Thus, hundreds of clinical trials with standardized guidelines for clinical research59,60 were conducted annually to evaluate the efficacy of TCM61, 62, 63 from 1994 to 2008 (controlled and clinical trials) in period A.
However, currently, TCM is still considered a secondary or underdeveloped type of medical science mostly due to issues related to its unsure efficacy when compared with Western medicine. However, instead of focusing on its effectiveness, starting in 2006, researchers seemed to be turning to exploring the mechanisms of TCM treatment for asthma since 2006. As shown in period B, in addition to modifying immune-cell (dendritic cells, T cells, regulatory T cells, etc) activity, we found some emerging new areas of research in recent years such as pharmacology, essential oil, gut microbiota, and oxidative stress. Before the 1980s, asthma was viewed simply as allergen-induced mast cell degranulation, resulting in the release of mediators, such as histamine and leukotrienes, which contracted the ASMs.64 Since then, it has become clear that asthma is a chronic inflammatory disease involving many interacting cells,65 including dendritic cells,66 T cells, and regulatory T cells.67 Although immune cells have not been the focus of research in this field recently, they still play a very important role in the study of asthma.
A network pharmacology strategy has been adopted for investigating the mechanism of action underlying the effectiveness of Chinese drugs68 and TCM formulas.69,70 To some extent, the application of network pharmacology will accelerate the research process of TCM in asthma. In addition, essential oils contained in medicinal plants with proven antiasthmatic properties have the possibility of being used as bronchodilators, mast cell stabilizers, expectorants, and so on.71 A connection between allergic asthma and the gut microbiota has been reported. A study found that the TCM pentaherbs formula can ameliorate symptoms of allergic diseases, such as allergic asthma, influencing the gut microbiota.72 Other studies have confirmed that the Gancao-Gansui combination can impact gut microbiota diversity,73 and Gansui is a Chinese herb often used to treat asthma. In addition, some studies found that TCM treatment of asthma works by relieving oxidative stress. For example, formononetin (bioactive isoflavone isolated from Huangqi),74 Bu-Shen-Yi-Qi formula,53 and laser acupuncture.75 All of the above research frontiers lasted for only 2 to 6 years, indicating that TCM in asthma research is still in the exploratory stage.
Reviewing the development of TCM in asthma research over the past 30 years, we found that the theory and technology of modern science development provided a possibility for the development of TCM in asthma research. During period A, ranging from 1991 to 2005, TCM in asthma research was deeply influenced by clinical trials. By the late 1980s and 1990s, “evidence-based” medicine and controlled randomized clinical trials were very rapidly developing. TCM has widely adopted the most advanced science technology and methods to carry out Chinese medicine research, and relevant TCM clinical trial guidelines and standards have been issued.76 Then, in approximately 2006, TCM ushered in the second phase of asthma research, period B, with the development of immunology. During 1998 to 2008, immunologic research in China has developed rapidly.77 With the support of 2 rounds of the 973 National Program in Immunology (2002-2006 and 2007-2011), a national network for immunologic research has been established in China.77 At the same time, it drove the research upsurge of TCM in the field of immunity. Since approximately 2016, with the development of various modern sophisticated instruments and the vigorous development of various science and technology tools, the development of TCM in asthma has been extended and diversified. For example, DNA fingerprinting and bar-coded pyrosequencing of 16S rRNA genes were used to profile gut microbiota structures and to identify the key population changes relevant to metabolic syndrome development.78 This study set off a surge in the study of gut microbiota and TCM research in gut microbiota. In addition, network pharmacology has promoted the development of TCM pharmacology. Metabonomic studies have promoted research on the microbiome in TCM. In the near future, with the increasingly mature and innovative development of modern science and technology, it will, of course, provide forefront techniques and methods that can be used for experimental research of TCM. However, the application of modern science and technology to study TCM is still a double-edged sword.
Discussion of issues affecting future development
According to the bibliometric analysis in this study, 2 outstanding issues have been identified in the research of TCM treatment in asthma. The first is the uncertainty about the effectiveness of TCM in treating asthma. The second is that TCM research in asthma is carried out in an imitative way, closely following the research progress of asthma, but it lacks its own discipline characteristics.
Over the centuries, TCM contributed to the prosperity and population health of China by preventing the spread of pestilences and treating diseases, which allowed the development of Chinese society and the expansion of Chinese culture. However, the effectiveness of TCM, not only in treating asthma, is still being questioned. TCM is still considered a secondary or underdeveloped type of medical science mostly due to issues related to its poor efficacy when compared with Western medicine. The existing statistical evidence and evaluation methods do little to show the value of TCM. Many experienced and thoughtful TCM doctors in China have proposed that the reason lies in somewhat neglecting TCM theory.79 The accessibility and efficacy of TCM have been limited, because the evaluation procedure and norms are almost the same as those of chemical drugs.80 TCM has been systematized and theorized in practice and has developed many methods to maintain health for thousands of years in China. TCM theory has the characteristic of directional thinking, which shapes a medical theory that is integrated, systemic, and advanced. However, Western medicine has evolved through Western science, and is based on human anatomy, biology, biochemistry, and molecular biology, relying more on laboratory test results.81 It is rather difficult to estimate the value of TCM because of the lack of practical standards fitted to the characteristics of TCM to evaluate its safety and efficacy.82 If the research method is not a TCM theory-based method, the research result will certainly not be consistent with the character of TCM.83,84
Furthermore, based on the bibliometric analysis results of this study, there is no hotspot or frontier research on the characteristics of TCM. Most TCM researchers closely follow the research progress of asthma and the technique trend. The negative effect is that the traditional theories of TCM are ignored. Even the clinical performance of indigenous TCM practitioners has been affected, because most practitioners lack comprehensive knowledge of TCM.85 During the process of the modernization of TCM, the application of modern science and technology and the inheritance of tradition have not been well integrated. TCM is gradually losing its characteristics and clinical advantages, not only in the field of TCM for asthma but also in other fields.
In view of these 2 issues, the following suggestions need to be considered: (1) The national administrations should create a reasonable policy environment for the growth of the TCM industry containing the real quintessence and characteristics of TCM. Only then can policies and guidelines suitable for the development of TCM be formulated. (2) For learners from all over the world, it is important to understand the essential function of traditional knowledge and make full use of the resources of Chinese medications. Policies need to be made to encourage TCM providers to use TCM in clinics and research.
Study limitations
Limitations of the current study include data omission, because we only considered publications in the Web of Science Core Collection database and did not include data from the Chinese databases. In addition, we selected only “Article” and “Review articles” for analysis, whereas we discarded books and conference papers for the current analysis, because many of these publications are not tracked by bibliometric searches. Future research can further supplement the relevant literature records by incorporating a larger data set including books and conference papers. Furthermore, in the author analysis, the author’s contribution as the first author or corresponding author in each article was not analyzed, and the results can only represent the number of articles in which the author participated. Finally, in the hotspot and frontier analysis of the study, we did not consider the impact of the government and relevant policies on this TCM research area, and the research results need to be objectively combined with policies for deeper thinking.
Conclusions
Our study has identified the timeline of the hotspots (complementary medicine, alternative treatment, allergic rhinitis, airway remodeling, DASH diet, eosinophilic esophagitis) and predicted the frontiers (pharmacology, essential oil, gut microbiota, oxidative stress.) in the field of TCM in asthma in recent years. Based on the current literature, TCM research on asthmatic conditions is still in the exploratory stage. Furthermore, 2 outstanding issues that exist in TCM research on asthma have been proposed and discussed, which can provide new directions and ideas to inform policymaking and clinical guidelines in the future.
Footnotes
This study was supported by the National Natural Science Foundation of China (Grant No. 82105013, 81973951), Shanghai Sailing Program (Grant No. 20YF1445300), National Key R&D Program of China (Grant No. 2018YFC1704600), and the Scientific Research Project of Shanghai Municipal Health Commission (Grant No. 20194Y0164).
Disclosure of potential conflict of interest: The authors declare that they have no relevant conflicts of interest.
References
- 1.Global INitiative for Asthma Global strategy for asthma management and prevention. 2021. https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf 2021.
- 2.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dharmage S.C., Perret J.L., Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;7:246. doi: 10.3389/fped.2019.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global INitiative for Asthma Global strategy for asthma management and prevention. 2009. https://ginasthma.org/wp-content/uploads/2019/01/2009-GINA.pdf 2009.
- 5.Yaghoubi M., Adibi A., Safari A., FitzGerald J.M., Sadatsafavi M. The projected economic and health burden of uncontrolled asthma in the United States. Am J Respir Crit Care Med. 2019;200:1102–1112. doi: 10.1164/rccm.201901-0016OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadek S.H., El-kholy M.M., Mohammed F.A., El-Morshedy R.M. Bronchial asthma control, quality of life, and psychiatric disorders vicious cycle: Asyut society point of view. Egypt J Bronchol. 2022;16:2. [Google Scholar]
- 7.Rice J.B., White A.G., Scarpati L.M., Wan G., Nelson W.W. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther. 2017;39:2216–2229. doi: 10.1016/j.clinthera.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Cheung F. TCM: made in China. Nature. 2011;480:S82–S83. doi: 10.1038/480S82a. [DOI] [PubMed] [Google Scholar]
- 9.Zou J., Wang W., Xie X. Analysis of the effect of moxibustion combined with antisensitive and antispasmodic decoction on immunoglobulin in children with cough variant asthma. Minerva Pediatr (Torino) 2022;74:90–92. doi: 10.23736/S2724-5276.21.06397-7. [DOI] [PubMed] [Google Scholar]
- 10.Liao P.F., Wang Y.T., Wang Y.H., Chiou J.Y., Wei J.C.C. Traditional Chinese medicine use may reduce medical utility in patients with asthma: a nationwide population-based retrospective cohort study. QJM. 2022;114:857–864. doi: 10.1093/qjmed/hcaa252. [DOI] [PubMed] [Google Scholar]
- 11.Nurwati I., Muthmainah M., Huda K.N. Acupuncture for asthma: its potential significance in clinical practice. Med Acupunct. 2020;32:272–279. doi: 10.1089/acu.2020.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang W., Yao Q., Teng F., Cui J., Dong J., Wei Y. Active ingredients from Chinese medicine plants as therapeutic strategies for asthma: overview and challenges. Biomed Pharmacother. 2021;137 doi: 10.1016/j.biopha.2021.111383. [DOI] [PubMed] [Google Scholar]
- 13.Chan H.H.L., Ng T. Traditional Chinese medicine (TCM) and allergic diseases. Curr Allergy Asthma Rep. 2020;20:67. doi: 10.1007/s11882-020-00959-9. [DOI] [PubMed] [Google Scholar]
- 14.Land M.H., Wang J. Complementary and alternative medicine use among allergy practices: results of a nationwide survey of allergists. J Allergy Clin Immunol Pract. 2018;6:95–98.e3. doi: 10.1016/j.jaip.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Chen C. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. 2006;57:359–377. [Google Scholar]
- 16.Chen C. Science mapping: a systematic review of the literature. J Data Info Sci. 2017;2:1–40. [Google Scholar]
- 17.Synnestvedt M.B., Chen C., Holmes J.H. CiteSpace II: visualization and knowledge discovery in bibliographic databases. AMIA Annu Symp Proc. 2005;2005:724–728. [PMC free article] [PubMed] [Google Scholar]
- 18.Chen C., Song M. Visualizing a field of research: a methodology of systematic scientometric reviews. PLoS One. 2019;14 doi: 10.1371/journal.pone.0223994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luo J., Shi Y., Wang X., Zhang R., Chen S., Yu W., et al. A 20-year research trend analysis of the influence of anesthesia on tumor prognosis using bibliometric methods. Front Oncol. 2021;11 doi: 10.3389/fonc.2021.683232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sabe M., Pillinger T., Kaiser S., Chen C., Taipale H., Tanskanen A., et al. Half a century of research on antipsychotics and schizophrenia: a scientometric study of hotspots, nodes, bursts, and trends. Neurosci Biobehav Rev. 2022;136 doi: 10.1016/j.neubiorev.2022.104608. [DOI] [PubMed] [Google Scholar]
- 21.Nicholls P.T. Price’s square root law: empirical validity and relation to Lotka’s law. Inform Process Manag. 1988;24:469–477. [Google Scholar]
- 22.Hou J., Yang X., Chen C. Emerging trends and new developments in information science: a document co-citation analysis (2009-2016) Scientometrics. 2018;115:869–892. [Google Scholar]
- 23.Eisenberg D.M., Davis R.B., Ettner S.L., Appel S., Wilkey S., Van Rompay M., et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 24.Li X.M., Brown L. Efficacy and mechanisms of action of traditional Chinese medicines for treating asthma and allergy. J Allergy Clin Immunol. 2009;123:297–306. doi: 10.1016/j.jaci.2008.12.026. quiz 7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wen M.C., Wei C.H., Hu Z.Q., Srivastava K., Ko J., Xi S.T., et al. Efficacy and tolerability of anti-asthma herbal medicine intervention in adult patients with moderate-severe allergic asthma. J Allergy Clin Immunol. 2005;116:517–524. doi: 10.1016/j.jaci.2005.05.029. [DOI] [PubMed] [Google Scholar]
- 26.Bielory L., Lupoli K. Herbal interventions in asthma and allergy. J Asthma. 1999;36:1–65. doi: 10.3109/02770909909065150. [DOI] [PubMed] [Google Scholar]
- 27.Bateman E.D., Hurd S.S., Barnes P.J., Bousquet J., Drazen J.M., FitzGerald J.M., et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31:143–178. doi: 10.1183/09031936.00138707. [DOI] [PubMed] [Google Scholar]
- 28.Ziment I., Tashkin D.P. Alternative medicine for allergy and asthma. J Allergy Clin Immunol. 2000;106:603–614. doi: 10.1067/mai.2000.109432. [DOI] [PubMed] [Google Scholar]
- 29.Blanc P.D., Trupin L., Earnest G., Katz P.P., Yelin E.H., Eisner M.D. Alternative therapies among adults with a reported diagnosis of asthma or rhinosinusitis—data from a population-based survey. Chest. 2001;120:1461–1467. doi: 10.1378/chest.120.5.1461. [DOI] [PubMed] [Google Scholar]
- 30.Lambrecht B.N., Hammad H. The immunology of asthma. Nat Immunol. 2015;16:45–56. doi: 10.1038/ni.3049. [DOI] [PubMed] [Google Scholar]
- 31.Eisenberg D.M., Kessler R.C., Foster C., Norlock F.E., Calkins D.R., Delbanco T.L. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 32.Bousquet J., Khaltaev N., Cruz A.A., Denburg J., Fokkens W.J., Togias A., et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen) Allergy. 2008;63:8–160. doi: 10.1111/j.1398-9995.2007.01620.x. [DOI] [PubMed] [Google Scholar]
- 33.Slader C.A., Reddel H.K., Jenkins C.R., Armour C.L., Bosnic-Anticevich S.Z. Complementary and alternative medicine use in asthma: who is using what? Respirology. 2006;11:373–387. doi: 10.1111/j.1440-1843.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- 34.Wang S.D., Lin L.J., Chen C.L., Lee S.C., Lin C.C., Wang J.Y., et al. Xiao-Qing-Long-Tang attenuates allergic airway inflammation and remodeling in repetitive Dermatogoides pteronyssinus challenged chronic asthmatic mice model. J Ethnopharmacol. 2012;142:531–538. doi: 10.1016/j.jep.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 35.Li X., Du J., Long H. Dynamic analysis of international green behavior from the perspective of the mapping knowledge domain. Environ Sci Pollut Res Int. 2019;26:6087–6098. doi: 10.1007/s11356-018-04090-1. [DOI] [PubMed] [Google Scholar]
- 36.Unschuld P. Oxford University Press; United Kingdom: 2022. Traditional Chinese medicine and public health. [Google Scholar]
- 37.World Health Organization Traditional Chinese Medicine could make “Health for one” true. 2005. https://library.uerm.edu.ph/kohaimages/UERM/repository/WHO%20Publications/009549%20part3.pdf 2005.
- 38.Bowler R.P. Oxidative stress in the pathogenesis of asthma. Curr Allergy Asthma Rep. 2004;4:116–122. doi: 10.1007/s11882-004-0056-7. [DOI] [PubMed] [Google Scholar]
- 39.Chapela R. Comparative study of the effectiveness of 2 oral corticoids in the control of severe crisis of bronchial asthma: deflazacort and prednisone. Rev Alerg Mex. 1995;42:64–68. [PubMed] [Google Scholar]
- 40.Bylo M., Farewell R., Coppenrath V.A., Yogaratnam D. A review of deflazacort for patients with Duchenne muscular dystrophy. Ann Pharmacother. 2020;54:788–794. doi: 10.1177/1060028019900500. [DOI] [PubMed] [Google Scholar]
- 41.Haccuria A., Van Muylem A., Malinovschi A., Doan V., Michils A. Small airways dysfunction: the link between allergic rhinitis and allergic asthma. Eur Respir J. 2018;51 doi: 10.1183/13993003.01749-2017. [DOI] [PubMed] [Google Scholar]
- 42.Tohidinik H.R., Mallah N., Takkouche B. History of allergic rhinitis and risk of asthma; a systematic review and meta-analysis. World Allergy Organ J. 2019;12 doi: 10.1016/j.waojou.2019.100069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ma T., Chen Y., Pang Y., Wang X., Dai D., Zhuang Y., et al. Prevalence and risk factors of allergic rhinitis and asthma in the southern edge of the plateau grassland region of northern China: a cross-sectional study. World Allergy Organ J. 2021;14 doi: 10.1016/j.waojou.2021.100537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Luthra M., Bist S.S., Mishra S., Bharti B., Aggarwal V., Monga U. Evaluation of association of allergic rhinitis with bronchial asthma. Indian J Otolaryngol Head Neck Surg. 2019;71:1687–1691. doi: 10.1007/s12070-015-0931-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Licari A., Castagnoli R., Denicolo C.F., Rossini L., Marseglia A., Marseglia G.L. The nose and the lung: united airway disease? Front Pediatr. 2017;5:44. doi: 10.3389/fped.2017.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morjaria J.B., Caruso M., Emma R., Russo C., Polosa R. Treatment of allergic rhinitis as a strategy for preventing asthma. Curr Allergy Asthma Rep. 2018;18:23. doi: 10.1007/s11882-018-0781-y. [DOI] [PubMed] [Google Scholar]
- 47.Durrani S.R., Mukkada V.A., Guilbert T.W. Eosinophilic esophagitis: an important comorbid condition of asthma? Clin Rev Allergy Immunol. 2018;55:56–64. doi: 10.1007/s12016-018-8670-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Virchow J.C. Eosinophilic esophagitis: asthma of the esophagus? Dig Dis. 2014;32:54–60. doi: 10.1159/000357010. [DOI] [PubMed] [Google Scholar]
- 49.Hoang M.P., Chitsuthipakorn W., Snidvongs K. Herbal medicines for allergic rhinitis: a systematic review and meta-analysis. Curr Allergy Asthma Rep. 2021;21:25. doi: 10.1007/s11882-021-00999-9. [DOI] [PubMed] [Google Scholar]
- 50.Soffer G., Kaman K., Li X.-M. Successful management of eosinophilic esophagitis using traditional Chinese medicine: a case report. Yale J Biol Med. 2020;93:685–688. [PMC free article] [PubMed] [Google Scholar]
- 51.Brigham E.P., Kolahdooz F., Hansel N., Breysse P.N., Davis M., Sharma S., et al. Association between Western diet pattern and adult asthma: a focused review. Ann Allergy Asthma Immunol. 2015;114:273–280. doi: 10.1016/j.anai.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nygaard U.C., Xiao L., Nadeau K.C., Hew K.M., Lv N., Camargo C.A., et al. Improved diet quality is associated with decreased concentrations of inflammatory markers in adults with uncontrolled asthma. Am J Clin Nutr. 2021;114:1012–1027. doi: 10.1093/ajcn/nqab063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cui J., Xu F., Tang Z., Wang W.Q., Hu L.L., Yan C., et al. Bu-Shen-Yi-Qi formula ameliorates airway remodeling in murine chronic asthma by modulating airway inflammation and oxidative stress in the lung. Biomed Pharmacother. 2019;112 doi: 10.1016/j.biopha.2019.108694. [DOI] [PubMed] [Google Scholar]
- 54.Xing Q.Q., You Y.N., Zhao X., Ji J.J., Yan H., Dong Y.M., et al. iTRAQ-based proteomics reveals Gu-Ben-Fang-Xiao decoction alleviates airway remodeling via reducing extracellular matrix deposition in a murine model of chronic remission asthma. Front Pharmacol. 2021;12 doi: 10.3389/fphar.2021.588588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pan L.Y., Han Y.Q., Wang Y.Z., Chen Q.Q., Wu Y., Sung Y. Mechanism of Yanghe Pingchuan granules treatment for airway remodeling in asthma. Drug Des Dev Ther. 2018;12:1941–1951. doi: 10.2147/DDDT.S159428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hu L.L., Li L.L., Zhang H.Y., Li Q.P., Jiang S., Qiu J., et al. Inhibition of airway remodeling and inflammatory response by Icariin in asthma. BMC Complement Altern Med. 2019;19:316. doi: 10.1186/s12906-019-2743-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang Z.C., Yi M.J., Ran N., Jin L.Y., Fu P., Feng X.Y., et al. Astragalus extract inhibits TGF-beta 1-induced EMT of bronchial epithelial cells and airway remodeling in asthmatic mice. Int J Clin Exp Med. 2016;9:1281–1289. [Google Scholar]
- 58.Traditional Chinese medicine in China. China Daily. China, 2016-12-07.
- 59.World Health Organization WHO traditional medicine strategy: 2002–2005. 2002. https://www.beovita.eu/pdf/WHO_EDM_TRM_2004.pdf Available at:
- 60.World Health Organization WHO traditional medicine strategy: 2014–2023. 2013. https://apps.who.int/iris/bitstream/handle/10665/92455/9789241506090_eng.pdf Available at:
- 61.Huntley A., Ernst E. Herbal medicines for asthma: a systematic review. Thorax. 2000;55:925–929. doi: 10.1136/thorax.55.11.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gruber W., Eber E., Malle-Scheid D., Pfleger A., Weinhandl E., Dorfer L., et al. Laser acupuncture in children and adolescents with exercise induced asthma. Thorax. 2002;57:222–225. doi: 10.1136/thorax.57.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu H.Z., Tong L., Gao P., Hu Y., Wang H.J., Chen Z.M., et al. Combination of ipratropium bromide and salbutamol in children and adolescents with asthma: a meta-analysis. Plos One. 2021;16 doi: 10.1371/journal.pone.0237620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barnes P.J. Our changing understanding of asthma. Respir Med. 1989;83:17–22. doi: 10.1016/s0954-6111(89)80246-x. discussion -3. [DOI] [PubMed] [Google Scholar]
- 65.Hammad H., Lambrecht B.N. The basic immunology of asthma. Cell. 2021;184:1469–1485. doi: 10.1016/j.cell.2021.02.016. [DOI] [PubMed] [Google Scholar]
- 66.Morianos I., Semitekolou M. Dendritic cells: critical regulators of allergic asthma. Int J Mol Sci. 2020;21:7930. doi: 10.3390/ijms21217930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Khan M.A. Regulatory T cells mediated immunomodulation during asthma: a therapeutic standpoint. J Transl Med. 2020;18:456. doi: 10.1186/s12967-020-02632-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bi J.J., Lin Y.H., Sun Y.P., Zhang M.Z., Chen Q.G., Miu X.Y., et al. Investigation of the active ingredients and mechanism of Polygonum cuspidatum in asthma based on network pharmacology and experimental verification. Drug Des Dev Ther. 2021;15:1075–1089. doi: 10.2147/DDDT.S275228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang R.Y., Lin J.T. Analysis of the mechanism of Zhichuanling oral liquid in treating bronchial asthma based on network pharmacology. Evid-Based Compl Alt. 2020;2020 doi: 10.1155/2020/1875980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen X.L., Xiao Q.L., Pang Z.H., Tang C., Zhu Q.Y. Molecular mechanisms of An-Chuan granule for the treatment of asthma based on a network pharmacology approach and experimental validation. Bioscience Rep. 2021;41 doi: 10.1042/BSR20204247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Adesina S.K., Johnny, Olayiwola G. Plants in respiratory disorders, I-anti-asthmatics, a review. Br J Pharm Res. 2017;16:1–21. [Google Scholar]
- 72.Tsang M.S.M., Cheng S.W., Zhu J., Atli K., Chan B.C.L., Liu D.H., et al. Anti-inflammatory activities of Pentaherbs formula and its influence on gut microbiota in allergic asthma. Molecules. 2018;23:2776. doi: 10.3390/molecules23112776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yu J.G., Guo J.M., Tao W.W., Liu P., Shang E.X., Zhu Z.H., et al. Gancao-Gansui combination impacts gut microbiota diversity and related metabolic functions. J Ethnopharmacol. 2018;214:71–82. doi: 10.1016/j.jep.2017.11.031. [DOI] [PubMed] [Google Scholar]
- 74.Yi L., Cui J., Wang W.Q., Tang W.F., Teng F.Z., Zhu X.Y., et al. Formononetin attenuates airway inflammation and oxidative stress in murine allergic asthma. Front Pharmacol. 2020;11 doi: 10.3389/fphar.2020.533841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Elsheikh M.S., Mohamed N.H., Alsharkawy A.A.A. Improvement of asthma control after laser acupuncture and its impact on exhaled 8-isoprostane as an oxidative biomarker in chronic bronchial asthma. Resp Med. 2019;156:15–19. doi: 10.1016/j.rmed.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 76.World Health Organization . WHO Regional Office for the Western Pacific; Manila: 1995. Regional Office for the Western Pacific. Guidelines for clinical research on acupuncture. [Google Scholar]
- 77.Cao X. Immunology in China: the past, present and future. Nat Immunol. 2008;9:339–342. doi: 10.1038/ni0408-339. [DOI] [PubMed] [Google Scholar]
- 78.Zhang C., Zhang M., Wang S., Han R., Cao Y., Hua W., et al. Interactions between gut microbiota, host genetics and diet relevant to development of metabolic syndromes in mice. ISME J. 2010;4:232–241. doi: 10.1038/ismej.2009.112. [DOI] [PubMed] [Google Scholar]
- 79.Lv W. Understanding traditional Chinese medicine. Hepatobil Surg Nutr. 2021;10:846–848. doi: 10.21037/hbsn-2021-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang T., Bai G., Han Y., Xu J., Gong S., Li Y., et al. The method of quality marker research and quality evaluation of traditional Chinese medicine based on drug properties and effect characteristics. Phytomedicine. 2018;44:204–211. doi: 10.1016/j.phymed.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 81.Jansen C., Baker J.D., Kodaira E., Ang L., Bacani A.J., Aldan J.T., et al. Medicine in motion: opportunities, challenges and data analytics-based solutions for traditional medicine integration into western medical practice. J Ethnopharmacol. 2021;267 doi: 10.1016/j.jep.2020.113477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dai L., Cheng C.W., Tian R., Zhong L.L., Li Y.P., Lyu A.P., et al. Standard protocol items for clinical trials with traditional Chinese medicine 2018: recommendations, explanation and elaboration (SPIRIT-TCM Extension 2018) Chin J Integr Med. 2019;25:71–79. doi: 10.1007/s11655-018-2999-x. [DOI] [PubMed] [Google Scholar]
- 83.Chen Q., Wang Q., Ding S., Li S., Zhang Y., Chen S., et al. Problems lowering the study quality in traditional medicine, introspection from an example of meta-analysis of acupuncture. BMC Complement Med Ther. 2020;20:41. doi: 10.1186/s12906-019-2806-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang W., Zhou H., Wang Y., Sang B., Liu L. Current policies and measures on the development of traditional Chinese medicine in China. Pharmacol Res. 2021;163 doi: 10.1016/j.phrs.2020.105187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gall A., Anderson K., Adams J., Matthews V., Garvey G. An exploration of healthcare providers’ experiences and perspectives of traditional and complementary medicine usage and disclosure by indigenous cancer patients. BMC Complement Altern Med. 2019;19:259. doi: 10.1186/s12906-019-2665-7. [DOI] [PMC free article] [PubMed] [Google Scholar]