Abstract
Introduction
The report on Levonorgestrel⁃releasing intrauterine system (LNG⁃IUS) suture under hysteroscopy is very rare, and currently only three articles have been reported. We reported a patient with adenomyosis who had previously had LNG-IUS, but the LNG-IUS moved downward. We sutured and fixed the LNG-IUS under hysteroscopy.
Case presentation
A 42-year-old woman presented with a 7-year history of adenomyosis of the uterus and adenomyoma adenomyosis. Half a year ago, due to increased menstrual flow, LNG-IUS was placed in the uterine cavity, and the treatment effect was satisfactory. Nine days ago, vaginal bleeding occurred, and ultrasound showed that LNG-IUS had moved downward. We performed LNG-IUS suturing under hysteroscopy for her, and a half-year follow-up ultrasound showed that the position of LNG-IUS was normal.
Clinical discussion
For adenomyosis, LNG-IUS is the most promising medical therapy due to its ability to suppress hormones to improve symptoms with a low profile of adverse effects while enabling women to maintain fertility. However, the high excretion rate of LNG-IUS may cause patients with adenomyosis to lose confidence in continuing to use this treatment method.
Conclusion
Our case report demonstrated the feasibility and effectiveness of LNG-IUS suture fixation under hysteroscopy. It provided another reliable treatment option for those patients with adenomyosis for whom the LNG-IUS fell off or fell down.
Keywords: Fixation, Suture, Hysteroscopy, Operative hysteroscope, Levonorgestrel⁃releasing intrauterine system, LNG⁃IUS
Highlights
-
•
Innovation of Chinese Gynecologists: Hysteroscopic Suturing Surgery
-
•
A new hysteroscopy technique
-
•
Expanded the scope of hysteroscopic surgery
1. Introduction
Adenomyosis is a prevalent condition in women of childbearing age that can cause symptoms such as heavy menstruation and dysmenorrhea. One of the most effective therapy modalities is LNG-IUS [1]. According to the literature, the chance of falling off the LNG-IUS in patients with adenomyosis is significant due to uterine cavity growth and heavy menstruation, and the cumulative rate of falling off is 11 % in 12 months [2]. LNG-IUS suture fixation through hysteroscopic suture is a revolutionary minimally invasive approach. An adenomyosis patient with a history of LNG-IUS fell off and had hysteroscopic suturing of the LNG-IUS to obtain long-term therapeutic benefit, we reported.
This case is written based on the SCARE checklist [3].
2. Case report
A 42-year-old woman with gravida 2 para 1, she had a regular menstrual cycle with an average amount of flow. She has moderate intensity periodic congestive dysmenorrhea and has previously required 1–2 painkillers during her menstrual period. But since 7 years ago, the intensity of her abdominal pain has been increasing, and an ultrasound examination indicates adenomyosis. The patient underwent curettage and had LNG-IUS placed in the uterine cavity six months ago due to excessive menstrual flow. After treatment, the menstrual flow was minimal, and the symptoms of dysmenorrhea disappeared. The patient was very satisfied with this treatment. The patient experienced vaginal bleeding again nine days ago and needs to replace four sanitary pads a day. She came to our hospital for treatment. A vaginal examination showed a small amount of dark red blood in the vagina, and an ultrasound examination showed that LNG-IUS had moved down. The size of the uterus is 88 × 85 × 79 mm, and the posterior wall of the uterus is an adenomyoma with a size of 84 × 53 mm. The intrauterine device is moved downwards, about 61 mm away from the serous layer of the uterine floor (Fig. 1). Based on the patient's medical history and ultrasound results, we provided various treatment options, including medical treatment, hysteroscopic ING-IUS suture, and laparoscopic hysterectomy, and explained the benefits and risks. After obtaining informed consent, an experienced chief physician performed a hysteroscopic LNG-IUS suture. The levonorgestrel release intrauterine device was sutured and fixed to the anterior uterine wall using an Intergrative Operative Hysteroscope surgical system and non-absorbable suture (Fig. 2). The surgical time is 30 min, with 5 ml of intraoperative bleeding and 5000 ml of distending media. After surgery, oral antibiotics (0.25 g of cefuroxime sodium twice a day for 3 days) were taken to prevent infection. At the 6-month postoperative follow-up, dysmenorrhea was relieved and menstrual flow decreased, and she informed us that there was no discomfort. The ultrasound shows that the uterus has shrunk to 76 × 76 × 78 mm, and the position of the contraceptive device is normal (Fig. 3).
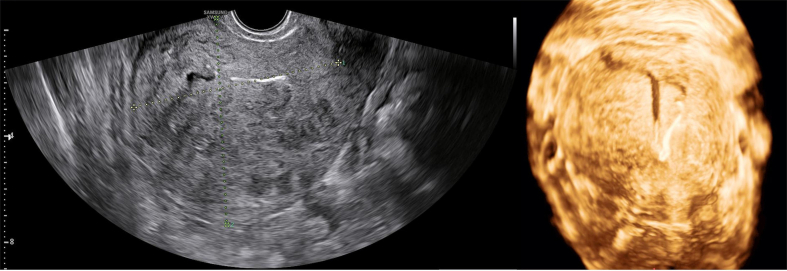
Fig. 1.
The size of the uterus is 88 × 85 × 79 mm, and the posterior wall of the uterus is an adenomyoma with a size of 84 × 53 mm. The intrauterine device is moved downwards, about 61 mm away from the serous layer of the uterine floor.
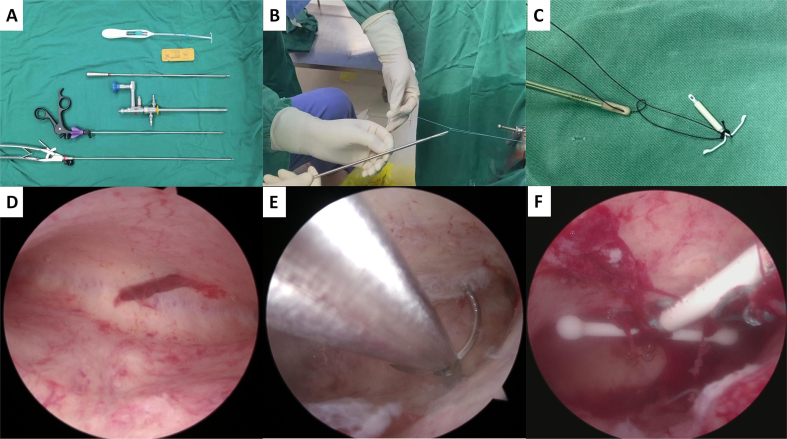
Fig. 2.
A was the required equipment. B and C were the external knotting processes. D was the uterine cavity. E was the process of suturing under hysteroscopy. F was LNG-IUS fixed to the anterior wall of the uterine cavity.
Fig. 3.
At 6-month postoperative follow-up, the ultrasound shows that the uterus has shrunk to 76 × 76 × 78 mm, and the position of the contraceptive device is normal.
2.1. Operative procedure
Materials (Fig. 2A): Operative Hysteroscope (KMS Medical Technology Co., Ltd.), endoscopic needle holder, endoscopic scissors, levonorgestrel-releasing intrauterine system (Manufacturer: Bayer; 52 mg; 20 μg/24 h), ETHIBOND EXCEL Polybutylate coated braided Polyester Suture (X519H, Johnson & Johnson).
Under intravenous anesthesia, the patient emptied the bladder and took the lithotomy position. The irrigation fluid was 0.9 % sodium chloride. 1. We first assessed the uterine cavity's morphology, size, and endometrial condition (Fig. 2D). 2. Putting the needle into the uterine cavity with hemostatic forceps. The method is to suture with a 3 mm needle holder through the operating channel (Fig. 2E). 3. After a needle was sutured in the intrauterine cavity, the needle was pulled out, and the middle part of the suture was fixed at the head and end of LNG-IUS (Fig. 2C). 4. The knot was tied with a knot push device, and the hysteroscopy was performed again to determine the position of the knot. The end of the suture was cut 1 cm from the knot (Fig. 2B, C, F). For detailed operation methods, please refer to articles published in our previously published videos [4]. If the device needs to be removed in the future, the suture needs to be cut under hysteroscopy.
3. Discussion
The most effective treatment for uterine adenomyosis at this time is a complete hysterectomy [5]. However, given that many patients have a strong desire to preserve the uterus. LNG-IUS is the most promising medical therapy, due to its ability to suppress hormones to improve symptoms with a low profile of adverse effects while enabling women to maintain fertility [6]. However, high rates of LNG-IUS expulsion may be a deterrent to patients who have discontinued treatment of adenomyosis [7]. With a length and width of 32 mm, the only model of LNG-IUS available in China is rigid and unable to adapt to various uterine sizes and shapes. At this time, there is no effective treatment for patients who have big uteri and LNG-IUS display or loss. In order to keep LNG-IUS from sliding off, several clinicians attempt to fix it in the uterus. Recently, a brand-new technology was created that effectively fixes the LNG-IUS shedding issue [4,8,9]. To prevent separation, gynecologists stitch LNG-IUS into the uterine cavity. Zhu et al. [9] first reported the fixation of LNG-IUS under hysteroscopy. Huang et al. [4] shown two paths of fixation of LNG-IUS under hysteroscopy. According to Huishi Zhang's research that has been published [8], they used absorbable polydioxone (PDO) for hysteroscopic sutures, with 1 case being expulsion and 2 cases being moved downwards (Table 1). They were switched to hysteroscopic sutures with nonabsorbable surgical sutures (ETHICON), and no further expulsion of the LNG-IUS occurred. For people with this condition, there is genuinely another associated therapeutic choice. It is proven that this method is a minimally invasive and effective alternative treatment for adenomyosis and decreases the risk of LNG-IUS expulsion. We sutured LNG-IUS under hysteroscopy, and the surgical process was safe and effective. The patient was followed up for six months with satisfactory results. This case further confirms that Intergrative Operative Hysteroscope suturing and fixation of a LNG-IUS as a new minimally invasive technique can provide effective treatment for patients with adenomyosis that preserves fertility function.
Table 1.
Characteristics of the studies.
4. Conclusion
Our case report demonstrated the feasibility and effectiveness of LNG-IUS suture fixation under hysteroscopy. It provided another reliable treatment option for those patients with adenomyosis for whom the LNG-IUS fell off or fell down.
Patient consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval for this study was provided by the Ethics Committee of Dongguan Songshan Lake Central Hospital on September 19, 2022 (Approval number: 2022-106-01).
Funding
The study was funded by the Dongguan Social Development Science and Technology Project (Grant Number20231800903812).
Author contribution
HaiHong Cui: Data collection and analysis, drafting, revision and final approval.
JinCheng Huang: Read and checked the case report before submission and final approval.
Guarantor
JinCheng Huang.
Research registration number
Not applicable.
Conflict of interest statement
There are no conflicts of interest.
References
- 1.Lang J.H., et al. Chinese expert panel consensus recommendations on the clinical application of levonorgestrel-releasing intrauterine system. Zhonghua Fu Chan Ke Za Zhi. 2019;54(12):815–825. doi: 10.3760/cma.j.issn.0529-567x.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Andersson K., Odlind V., Rybo G. Levonorgestrel-releasing and copper-releasing (Nova T) IUDs during five years of use: a randomized comparative trial. Contraception. 1994;49(1):56–72. doi: 10.1016/0010-7824(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 3.Agha R.A., et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Huang, J.C., et al., Two paths of suture fixation for levonorgestrel-releasing intrauterine devices under hysteroscopy. Indian J. Surg.
- 5.Osada H. Uterine adenomyosis and adenomyoma: the surgical approach. Fertil. Steril. 2018;109(3):406–417. doi: 10.1016/j.fertnstert.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 6.Pontis A., et al. Adenomyosis: a systematic review of medical treatment. Gynecol. Endocrinol. 2016;32(9):696–700. doi: 10.1080/09513590.2016.1197200. [DOI] [PubMed] [Google Scholar]
- 7.Lee K.H., et al. Relationship between uterine volume and discontinuation of treatment with levonorgestrel-releasing intrauterine devices in patients with adenomyosis. Arch. Gynecol. Obstet. 2016;294(3):561–566. doi: 10.1007/s00404-016-4105-y. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H., et al. An innovative surgical approach: suture fixation of the levonorgestrel-releasing intrauterine system in the treatment of adenomyosis. BMC Womens Health. 2022;22(1):451. doi: 10.1186/s12905-022-01932-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu L., et al. The suture fixation of levonorgestrel-releasing intrauterine device using the hysteroscopic cold-knife surgery system: an original method in treatment of adenomyosis. Fertil. Steril. 2021;116(4):1191–1193. doi: 10.1016/j.fertnstert.2021.05.113. [DOI] [PubMed] [Google Scholar]