To the Editor:
Managing surgical wounds on the lower legs can be challenging in older patients (>65yrs) with comorbidities known to compromise wound healing.1 Timolol is a beta-blocker with multiple off-label uses in dermatology that has been shown to have anti-inflammatory and pro-wound healing properties.2 In this study, we evaluate timolol’s efficacy to improve secondary intention wound healing in surgical wounds below the knee in patients at risk for prolonged wound healing.
Initially, we identified characteristics in literature which were associated with suboptimal wound healing. We compared these findings with patients in clinic and defined our inclusion criteria for sub-optimal healing conditions as patients older than age 65 with at least one comorbidity associated with poor wound healing (diabetes mellitus, cardiovascular disease, peripheral vascular disease, venous insufficiency, smoking).1,3–4
We routinely manage patients with lower leg wounds healing by secondary intention after Mohs surgery with petroleum jelly and a non-adherent dressing. Starting in January 2020, we began to supplement standard care with topical 0.5% timolol maleate ophthalmic solution (1-drop or 2-drops per day on wounds ≤2cm or >2cm, respectively) for patients with suboptimal healing conditions.3 As such, we conducted a retrospective cohort study of patients with post-Mohs lower leg wounds healing by secondary intention between January 2019 and December 2020, grouping patients into one of three cohorts: a healthier group (Group A) that did not fit criteria for suboptimal healing, a group of potentially suboptimal healers seen in 2019 (Group B), and a group of potentially suboptimal healers seen in 2020 (Group C). Group A and B were managed with standard wound care and Group C supplemented this wound care with topical timolol. Patients were seen for follow-up at 3-week intervals until complete re-epithelization was appreciated on clinical examination (Figure 1) (full methods and references in Supplemental Material via Mendeley https://doi.org/10.17632/gz2d4xc249.1). Two patients in Group C discontinued timolol and were excluded from analysis: one with wound pain and the other with signs of infection. Because Timolol is absorbed similarly in wound and ophthalmic applications, side effects to be aware of include arrhythmia, bronchospasm, and bradycardia.5
Figure 1.
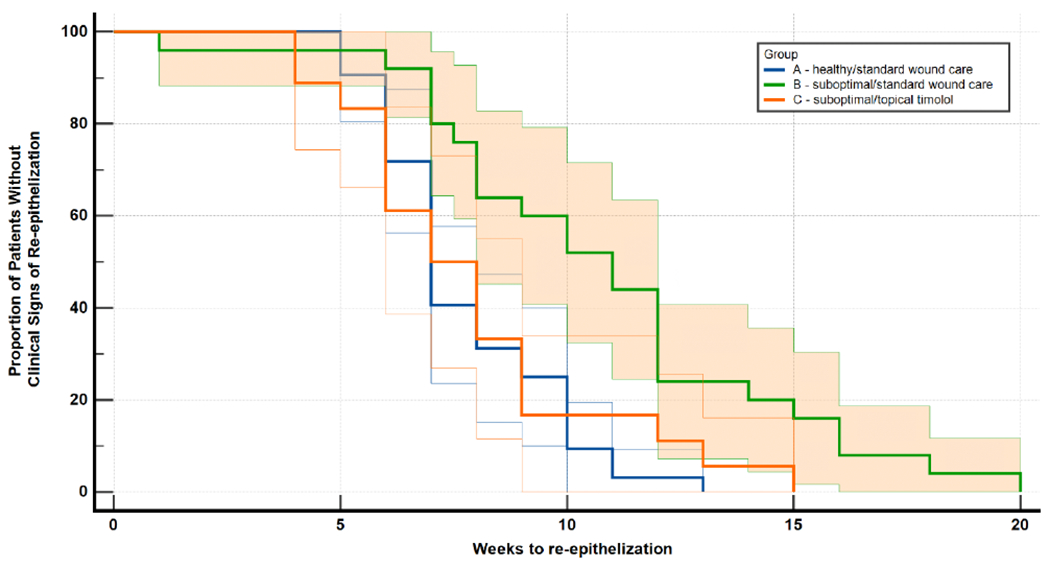
Kaplan-Meier survival curves for time complete re-epithelization in each study group.
Without topical timolol, the suboptimal healers (Group B) demonstrated prolonged healing time (p=0.001)*. The addition of topical timolol to the wound care regimen accelerated re-epithelialization of suboptimal healers (Group C), in which the rate of re-epithelialization was comparable to that observed in the healthier group (Group A) (p=0.7734)*. Logrank analysis of the Kaplan-Meier curve supports this association (X2 (2) = 10.52, p=0.0052).
*p-values calculated using the independent two-sample t-test.
Using the independent two-sample t-test to compare the average times to re-epithelialization, we observed a significant difference between the healthier group (Group A) and the group of suboptimal healers that only received the standard wound care regimen (Group B) (7.7 (SD 2.0) and 10.8 (SD 4.2) weeks, respectively (p=0.001)). When supplemented with topical timolol, no such difference was found between the healthier group (Group A) and the suboptimal healers supplementing standard wound care with topical timolol (Group C) (7.7 (SD 2.0) and 7.9 (SD 3.0) weeks, respectively (p=0.7734)) (Table 1).
Table 1.
Comparison of Wound Healing and Patient Characteristics by Study Grouping
| Group A − healthier group + standard wound care (2019+2020) (n=32) |
Group B − suboptimal group + standard wound care (2019) (n=25) |
Group C − suboptimal group + standard wound care + topical timolol (2020) (n=18) |
||
|---|---|---|---|---|
| Age, Mean (standard deviation) | 64.3 (5.1) | 78.4 (6.4) | 75.3 (5.6) | |
| Average Post-op Wound Size, mm2 (SD) | 174† (93) | 172† (50) | 259† (129) | |
| Wound Thickness | Partial | 25 (78.1%) | 21 (84%) | 13 (72.2%) |
| Full | 7 (21.9%) | 4 (16%) | 5 (27.8%) | |
| Time to Re-Epithelization, weeks (SD) | 7.7‡ (2.0) | 10.8‡ (4.2) | 7.9‡ (3.0) | |
| Clinical Characteristics, No. (%) | ||||
| Atrophic skin | 3 (9.4%) | 12 (48%) | 12 (66.7%) | |
| Varicose veins | 4 (12.5%) | 13 (52%) | 5 (27.8%) | |
| Edematous lower extremities§ | 3 (9.4%) | 16 (64%) | 10 (55.6%) | |
| Stasis dermatitis/ changes§ | 1 (3.1%) | 3 (12%) | 7 (38.9%) | |
| Comorbidities, No. (%) | ||||
| Current/Former smoker | 6 (18.8%) | 7 (28%) | 5 (27.8%) | |
| Diabetes mellitus | 1 (3.1%) | 4 (16%) | 1 (5.6%) | |
| Hypertension / heart disease§ | 7 (21.9%) | 20 (80%) | 12 (66.7%) | |
| Immuno-suppression | 2 (6.3%) | 1 (4%) | 0 (0%) | |
| Deep vein thrombosis history | 0 (0%) | 1 (4%) | 1 (5.6%) | |
P-value* for the difference in means of groups A and B = 0.910; groups B and C = 0.004; groups A and C = 0.010.
P-value* for the difference in means of groups A and B = 0.001; groups B and C = 0.012; groups A and C = 0.773
Statistically significant difference in characteristic 104 found across groups via Chi-squared analysis.
Timolol may enhance wound healing by accelerating re-epithelialization in those expected to have inadequate or prolonged healing of the lower extremity. Limitations of this study include its retrospective design, small sample size, large interval between follow-up visits, and lack of rater-blinding. Timolol may provide a different and likely a simpler, less expensive option for clinicians who are managing difficult healing wounds on the lower legs.
Funding sources:
Supported in part by Memorial Sloan Kettering Cancer Center’s NIH/National Cancer Institute Cancer Center support grant P30 CA008748.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None declared for all authors.
IRB approval status: Reviewed and approved by Memorial Sloan Kettering IRB, #16-458
References
- 1.Khalil H, Cullen M, Chambers H, Carroll M, Walker J. Elements affecting wound healing time: An evidence based analysis. Wound Repair and Regeneration. 2015;23(4):550–556. doi: 10.1111/wrr.12307 [DOI] [PubMed] [Google Scholar]
- 2.Thomas B, Kurien JS, Jose T, Ulahannan SE, et al. Topical timolol promotes healing of chronic leg ulcer. J Vasc Surg Venous Lymphat Disord 2017;5(6):844–850. [DOI] [PubMed] [Google Scholar]
- 3.Chetter IC, Oswald AV, McGinnis E, et al. Patients with surgical wounds healing by secondary intention: A prospective, cohort study. Int J Nurs Stud. 2019;89:62–71. doi: 10.1016/j.ijnurstu.2018.09.011 [DOI] [PubMed] [Google Scholar]
- 4.Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res 2010;89(3):219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoon DJ, Kaur R, Gallegos A, et al. Adverse effects of topical timolol: Safety concerns and implications for dermatologic use. Journal of the American Academy of Dermatology. 2021;84(1):199–200. doi: 10.1016/j.jaad.2020.04.101 [DOI] [PubMed] [Google Scholar]


