Abstract
Background
The relationship between migraine and breast cancer risk has generated conflicting findings. We attempted to assess the association between migraine and breast cancer risk using Mendelian randomization (MR) analysis.
Methods
We selected genetic instruments associated with migraine from a recently published genome-wide association studies (GWAS). Inverse variant weighted (IVW) analysis was adopted as the main method, and we also performed the weighted-median method and the MR‒Egger, MR pleiotropy residual sum and outlier (MR-PRESSO), and MR Robust Adjusted Profile Score (MR-RAPS) methods as supplements.
Results
Our MR suggested that any migraine (AM) was a risk factor for overall breast cancer (IVW: odds ratio (OR) = 1.072, 95% confidence intervals (CI) = 1.035–1.110, P = 8.78 × 10− 5, false discovery rate (FDR) = 7.36 × 10− 4) and estrogen receptor-positive (ER+) breast cancer (IVW: OR = 1.066, 95% CI = 1.023–1.111, P = 0.0024; FDR = 0.0108) but not estrogen receptor-negative (ER-) breast cancer. In its subtype analysis, women with a history of migraine without aura (MO) had an increased risk of ER- breast cancer (IVW: OR = 1.089, 95% CI = 1.019–1.163, P = 0.0118, FDR = 0.0354), and MO was suggestively associated with the risk of overall breast cancer (FDR > 0.05 and IVW P < 0.05). No significant heterogeneity or horizontal pleiotropy was found in the sensitivity analysis.
Conclusion
This study suggested that women with AM have an increased risk of overall breast cancer and ER + breast cancer. MO was suggestively associated with the risk of overall breast cancer and ER- breast cancer.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-023-11337-9.
Keywords: Breast cancer, Migraine with aura, Migraine without aura, Any migraine, Mendelian randomization.
Introduction
Migraine is a clinically common neurological disorder that is most common in women aged 25–55 [1, 2]. Nowadays, migraine is highly prevalent [3]. Notably, migraine is associated with many poor health outcomes, such as cardiovascular disease [4], dementia [5] and cancer [6]. Therefore, migraine appears to be a major public health problem. Breast cancer is the most prevalent female malignant tumour and poses a huge public health and economic burden [7]. Evidence on the association between migraine and risk of breast cancer is limited and inconsistent [8–12]. Evidence from the Nurses’ Health Studie didn’t find the association between migraine and breast cancer [11]. However, an association between migraine and breast cancer was revealed in another two study [8, 12]. Inconsistent findings and limitations of observational studies, such as undetectable confounders, hamper causal assessment of the relationship between migraine and breast cancer.
Traditional observational studies have inherent shortcomings in exploring casual links between exposure and outcome. Mendelian randomization (MR) studies, a new approach to epidemiological research, allow the use of large samples of pooled genome-wide association studies (GWAS) data to explore the relationship between risk factors and outcomes [13–15]. MR studies effectively reduce the impact of reverse causality and causal confounding estimates in observed data. In addition, measurement error has less impact on the results due to the high precision of single nucleotide polymorphisms (SNPs) measurement [16]. In addition, many published GWAS provide a rich resource of data [17]. Here, we aimed to estimate the causal relationship between genetic liability for migraine and breast cancer by applying a two-sample MR analysis [18].
Materials and methods
Study design
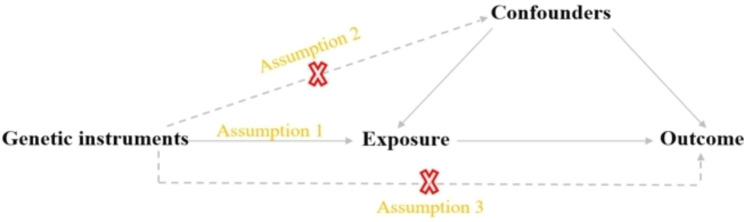
We conducted a two-sample MR study to examine the causal relationship between exposure and outcome. Genetic variation as an instrumental variable must follow three assumptions: [1] Genetic variations are strongly related to exposure [2]. Genetic variations are not associated with potential confounding [3]. Genetic variations do not influence outcomes directly [19] (Fig. 1).
Fig. 1.
A. Basic assumptions of Mendelian randomization. B. Flow chart of the analytical methods and how the MR analysis was performed step by step
Data sources
This MR analysis utilized the largest published GWAS data; all of the participants in those cohorts being of European descent (Table 1). Ethical approval and consent information for the summarized statistics were taken from the original publication.
Table 1.
Characteristics of genome-wide association studies used in the analyses
| Traits | Case/Control | Cohort | PMID |
|---|---|---|---|
| Migraine | |||
| Any migraine (AM) | 102,084/ 771,257 |
IHGC2016 (European descent) UKBB (European, British) deCODE (European, Icelandic) DBDS (European, Danish) LUMINA (European, Dutch) |
35,115,687 |
| Migraine with aura (MA) | 14,624/682,301 | ||
| Migraine without aura (MO) | 15,055/703,852 | ||
| Breast Cancer | |||
| Overall BC | 122,977/105,974 |
Oncoarray (European descent) iCOGS (European descent |
29,059,683 |
| ER + BC | 69,501/105,974 | ||
| ER- BC | 21,468/105,974 | ||
BC: breast cancer; ER + BC: estrogen positive breast cancer; ER- BC: estrogen negative breast cancer
The data on any migraine (AM) were derived from a recently published article composed of 102,804 cases and 771,257 controls, which included 14,624 cases of migraine with aura (MA) and 15,055 cases of migraine without aura (MO) from five study collections (IHGC2016, UKBB, 23andMe, GeneRISK, and HUNT) after removing overlapping participants. Patients without subtype information were not included in the subtype analysis [18]. The meta-analysis of the study collections was conducted in a fixed-effect model using GWAMA [20]. All study collections were adjusted for sex and more than four leading principal components, and age was conducted as a covariate if it was available in the genetic population [18].
The GWAS summary statistics of breast cancer were derived from the Breast Cancer Association Consortium (BCAC) with 122,977 cases (69,501 estrogen receptor positive (ER+) and 21,468 estrogen receptor negative (ER−)) and 105,974 controls of European ancestry from OncoArray and ICOGS arrays [21]. Overlapping participants were removed from the iCOGS dataset because of the better genomic coverage provided by the OncoArray array. The iCOGS and OncoArray cohorts were adjusted for study and country, respectively [21].
Selection of instrumental variables
A series of rigorous steps were applied to the screening of single nucleotide polymorphisms (SNPs). First, we selected the SNPs as instrument variants (IVs) of migraine in the threshold of P < 5 × 10 − 8, and the P was derived from original exposure-GWAS with fixed-model [18]. Second, SNPs were removed if the minor allele frequency was less than 0.01, and linkage disequilibrium (LD) estimates were performed (R2 < 0.001, window size 10,000 kb). Third, the SNPs were removed if they were directly related to the outcome (P < 5 × 10 − 8) and the P was derived from original outcome-GWAS with fixed-model. Fourth, all candidate SNPs were checked to avoid any possible confounders (P < 5 × 10 − 8) by PhenoScanner (http://www.phenoscanner.medschl.cam.ac.uk/phenoscanner); the removed SNPs as possible confounders for breast cancer, such as body mass index (BMI), NSAIDs, age of menarche or age of menopause. The F statistics were used to detect weak instrumental variables, and there were no weak instrumental variables when F > 10.
Primary MR analysis
The Wald ratio was used to assess the effect of migraine on breast cancer for each SNP. All SNP effects were meta-analysed by the inverse-variance weighted (IVW) method [22]. We performed Cochran’s Q test to check heterogeneity, and the random-effects model of the IVW method was adopted if the heterogeneity existed; otherwise, the fixed-effects model of the IVW method was used as the primary result in our study [23].
Sensitivity analysis
In sensitivity analyses, MR‒Egger and weighted median (WM) methods were applied to account for horizontal pleiotropic effects. The MR‒Egger method was based on the Instrument Strength Independent of Direct Effect assumption, which often provides imprecise and low statistical power MR results, especially when meeting small sizes of SNPs (e.g., < 10) [24]. In our MR study, MR‒Egger was mainly used to detect pleiotropy; a statistically significant intercept indicates directional pleiotropy [24]. The WM method was more reliable if more than 50% of SNPs were invalid instruments (e.g., due to pleiotropy) [25]. Considering measurement error in the effects of SNP, a newly developed analysis, called the Robust Adjusted Profile Score (MR-RAPS), was performed to reduce bias from weak IV. However, this method was applicable when the sample size of SNPs was greater than 7 [26]. In addition, MR-PRESSO analysis was used to detect outliers, which can reduce heterogeneity by removing those outliers that may lead to heterogeneity [27]. We performed leave-one-out method analysis to determine potentially influential SNPs by removing each SNP. We adjusted the multiple testing by false discovery rate (FDR). Summary of the different methods used for MR analysis was shown in Supplementary Table 1.
MR procedures
We performed three steps for our study to eliminate biased results due to heterogeneity (Supplementary Fig. 1). Step 1: We first conducted MR analysis with all the above-selected SNPs, and then the MRPRESSO outlier test was performed; we went to the second step if the MRPRESSO outliers were excited (P < 0.05). Step 2: We reassessed the MR analysis after removing all outliers (P < 0.05). Step 3: If heterogeneity was still present, we excluded all SNPs with a P value less than 1 in the MR-PRESSO test and reevaluated the MR analysis. Finally, if there were potentially influential SNPs examined by the leave-one-out test, we will explain the results with caution.
The “TwoSampleMR”, “mr.raps” and “MRPRESSO” packages were applied in our MR study. All statistical analyses were performed based on R software 4.1.1.
Results
Detailed information on the selected SNPs is shown in Supplementary Table 2. The F statistics for all SNPs ranged from 29.9 to 314.8. For AM and MO, most associations were well powered (Supplementary Table 3), For MA, statistical power was lower, we deemed that it might result from low explained variance, as it had only three IVs, suggesting that the relationships between MA and breast cancer should be cautious.
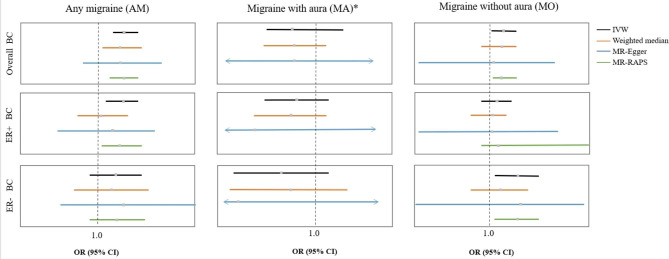
Four SNPs associated with the confounders for the AM were removed; three of them are related to BMI (rs1472662, rs42854, and rs12708529), and another one (rs1019990) is related to age at menarche. rs10828247 was excluded when the exposure was AM because of the directivity relationship with the outcome (P < 5 × 10 − 8). The MR estimates at different steps of the causal effect of migraine on breast cancer from the series of analysis methods are presented in Supplementary Tables 4–6. The last step of MR analysis is shown in Table 2; Fig. 2.
Table 2.
MR estimates of assessing the causal effect of migraine on breast cancer in IVW method
| Outcome | Step# | Overall BC IVW method | ER + BC IVW method | ER- BC IVW method | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NSNP | OR (95%CI) | P | NSNP | OR (95%CI) | P | NSNP | OR (95%CI) | P | ||
| AM | 3 | 79 | 1.072 (1.035, 1.110) | 8.78 × 10 − 5 | 81 | 1.066 (1.023, 1.111) | 0.0024 | 80 | 1.045 (0.979, 1.115) | 0.1871 |
| MA | 1 | 3 | 0.922 (0.840, 1.103) | 0.0919 | 3 | 0.939 (0.840, 1.051) | 0.2739 | 3 | 0.883 (0.745, 1.047) | 0.1518 |
| MO | 1 | 12 | 1.042 (1.005, 1.081) | 0.0267 | 12 | 1.022 (0.979, 1.068) | 0.3217 | 12 | 1.089 (1.019, 1.163) | 0.0118 |
Step#: 1, MR analysis with the all remained SNPs; 2, MR analysis after eliminating MRPRESSO outlier (with P < 0.05); 3, MR analysis after removing all the SNPs (with P < 1.00 in MR-PRESSO test); NSNP, number of single nucleotide polymorphism; MR, Mendelian randomization; IVW: inverse variance weighting; OR, odds ratio; CI, confidence interval; BC: breast cancer; ER + BC: estrogen positive breast cancer; ER- BC: estrogen negative breast cancer; AM: any migraine; MA: migraine with aura; MO: migraine without aura; Bold font: The p-values < 0.05 are statistically significant. The ORs were scaled to a 1-unit increase in log-transformed OR of migraine. P values are for ORs (95% CIs)
Fig. 2.
The forest figure for MR analysis. Migraine with aura (MA)*: The MR-RAPS method did not apply to MA (3 SNPs) because this method was applicable when the sample size of SNPs was greater than 7. ER + BC: breast cancer; ER + BC: estrogen-positive breast cancer; ER- BC: estrogen-negative breast cancer; MA: migraine with aura. IVW: inverse variance weighting. MR-RAPS: Robust adjusted profile score. The black line represents the results of the IVW method. The orange line represents the results of the weighted median method. The blue line represents the results of the MR‒Egger method. The green line represents the results of the MR-RAPS method
The effect of AM on breast cancer
The MR analysis showed that genetically predicted AM (per log-odds ratio increase) was associated with a 7.2% higher risk of overall breast cancer (IVW: OR = 1.072, 95% CI = 1.035–1.110, P = 8.78 × 10− 5; WM: OR = 1.063, 95% CI = 1.006–1.123, P = 0.0283; MR-Egger: OR = 1.062, 95% CI = 0.956–1.179, P = 0.2639; MR-RAPS: OR = 1.069, 95% CI = 1.026–1.113, P = 0.0015) and a 6.6% higher risk of ER + breast cancer (IVW: OR = 1.066, 95% CI = 1.023–1.111, P = 0.0024; WM: OR = 1.010, 95% CI = 0.947–1.078, P = 0.7533; MR-Egger: OR = 1.038, 95% CI = 0.902–1.160, P = 0.7277; MR-RAPS: OR = 1.064, 95% CI = 1.013–1.117, P = 0.0128). However, no causal effect of AM on ER- breast cancer was found (IVW: OR = 1.045, 95% CI = 0.979–1.115, P = 0.1871; WM: OR = 1.037, 95% CI = 0.940–1.144, P = 0.4728; MR-Egger: OR = 1.077, 95% CI = 0.880–1.319, P = 0.4714; MR-RAPS: OR = 1.059, 95% CI = 0.982–1.142, P = 0.1357). The effect estimations from various sensitive analysis all pointed to the same direction, which indicated that the results are robust. An additional, adjusted P value of IVW after FDR was corrected suggested that AM was still a risk factor for overall breast cancer (FDR = 7.36 × 10− 4) and ER + breast cancer (FDR = 0.0108). Detailed information on the MR analysis for different steps is shown in Supplementary Table 4.
No horizontal pleiotropy was detected in this part of the MR analysis (Table 3). Heterogeneity was eliminated after performing Step 3 MR estimate (MR analysis after removing all the SNPs whose P value was less than 1 after the MRPRESSO test). Moreover, the leave-one-out test showed that there were no potentially influential SNPs in this part (Supplementary Fig. 2). Therefore, we can draw a robust conclusion.
Table 3.
Heterogeneity and horizontal pleiotropy analyses results
| Outcome | AM | MA | MO | |||||
|---|---|---|---|---|---|---|---|---|
| P(Heterogeneity) | P(Pleiotropy) | P(Heterogeneity) | P(Pleiotropy) | P(Heterogeneity) | P(Pleiotropy) | |||
| Overall BC | 0.084 | 0.846 | 0.092 | 0.998 | 0.347 | 0.300 | ||
| ER + BC | 0.068 | 0.728 | 0.274 | 0.773 | 0.545 | 0.480 | ||
| ER- BC | 0.187 | 0.750 | 0.152 | 0.863 | 0.499 | 0.515 | ||
ER + BC: BC: breast cancer; ER + BC: estrogen positive breast cancer; ER- BC: estrogen negative breast cancer; AM: ang migraine; MA: migraine with aura; MO: migraine without aura. P(Heterogeneity): p value of Cochrane’s Q value in heterogeneity test; P(Pleiotropy): The P value for the intercept in the MR-Egger regression was used present the pleiotropy (p < 0.05)
The effect of MA on breast cancer
In our MR analysis, only three SNPs were selected as IVs at the criteria of P < 5 × 10 − 8, and the results showed no causal effect of MA on overall breast cancer (IVW: OR = 0.922, 95% CI = 0.840–1.103, P = 0.0919; WM: OR = 0.933, 95% CI = 0.835–1.043, P = 0.2253; MR-Egger: OR = 0.926, 95% CI = 0.051–16.97, P = 0.9672), ER + breast cancer (IVW: OR = 0.939, 95% CI = 0.840–1.051, P = 0.2739; WM: OR = 0.921, 95% CI = 0.809–1.084, P = 0.2127; MR-Egger: OR = 0.817, 95% CI = 0.056–58.71, P = 0.7931) or ER- breast cancer (IVW: OR = 0.883, 95% CI = 0.745–1.047, P = 0.1518; WM: OR = 0.911, 95% CI = 0.740–1.121, P = 0.3763; MR-Egger: OR = 0.629, 95% CI = 0.003–119.2, P = 0.8907). The MR estimates of the effect of AM on breast cancer for different methods are presented in Supplementary Table 5. The MR-RAPS method was not available because this method was applicable when the sample size of SNPs was greater than 7, but there were only 3 SNPs as IVs for MA exposure. In this part of the sensitivity analysis, we did not find any horizontal pleiotropy or significant heterogeneity (Table 3). We did not detect any MRPRESSO outliers. The plots of the leave-one-out test presented no potentially influential SNPs in this part (Supplementary Fig. 3). Therefore, we can draw a robust conclusion.
The effect of MO on breast cancer
In the two-sample MR analysis, we found that MO (per log-odds ratio increase) was associated with a 4.2% higher risk of overall breast cancer (IVW: OR = 1.042, 95% CI = 1.005–1.081, P = 0.0267; WM: OR = 1.030, 95% CI = 0.977–1.086, P = 0.2741; MR-Egger: OR = 1.012, 95% CI = 0.777–1.235, P = 0.5324; MR-RAPS: OR = 1.041, 95% CI = 1.003–1.082, P = 0.0332) and an 8.9% higher risk of ER- breast cancer (IVW: OR = 1.089, 95% CI = 1.019–1.163, P = 0.0118; WM: OR = 1.037, 95% CI = 0.948–1.133, P = 0.4313; MR-Egger: OR = 1.102, 95% CI = 0.700-1.354, P = 0.8782; MR-RAPS: OR = 1.085, 95% CI = 1.013–1.163, P = 0.0205). No causal effect of AM on ER + breast cancer was found (IVW: OR = 1.022, 95% CI = 0.979–1.068, P = 0.3217; WM: OR = 1.003, 95% CI = 0.940–1.053, P = 0.8582; MR-Egger: OR = 1.002, 95% CI = 0.760–1.272, P = 0.6136; MR-RAPS: OR = 1.026, 95% CI = 0.982–1.722, P = 0.2556). MO might elevate the risk of ER- breast cancer after FDR control (FDR = 0.0354). The effect estimations from various sensitive analysis all pointed to the same direction, which indicated that the results are robust. However, MO was suggestively associated with the risk of overall breast cancer (FDR > 0.05 and IVW P < 0.05). Detailed information on the MR analysis for different steps is shown in Supplementary Table 6.
No horizontal pleiotropy or heterogeneity was detected in this part of the MR analysis (Table 3). We did not detect any MRPRESSO outliers. Moreover, the leave-one-out test showed that there were potentially influential SNPs in this part (Supplementary Fig. 4). Thus, we should carefully interpret the conclusion.
Discussion
Our study is the first to investigate the relationship between migraine and breast cancer risk using MR analysis. In our research, we found that migraine prevalence is positively associated with breast cancer. We especially drew the robust conclusion that AM may increase the risk of overall breast cancer or ER- breast cancer, and MO was the risk factor for ER- breast cancer. Additionally, we deemed that MO was suggestively associated with the risk of overall breast cancer because the corrected FDR was more than 0.05.
Although all of the above MR‒Eggers suggest no statistical significance, MR‒Egger has the characteristics of inaccuracy and low statistical power, and it is provided as the primary reference result only when horizontal pleiotropy exist. In this study, IVW was applied as the main result, while other sensitivity analysis methods only required consistency of the direction rather than the significance of estimates [28].
Migraine is a common primary headache that occurs more frequently in women than in men [3, 29, 30]. The concentration of estrogen is the main trigger for migraine headaches, and breast cancer is also associated with changes in estrogen [31]. Therefore, there may be a link between migraine and breast cancer [9]. The first clinically controlled study of migraine and breast cancer was published in 2008. Mathes et al. suggested that women who have had migraines in the past have a lower risk of invasive breast cancer in the future (OR, 0.67; 95% CI, 0.54–0.82) [32]. However, Mathes et al. also believed that they did not collect data on the use of NSAIDs, which has been shown in many studies to reduce the incidence of breast cancer [33–35]. There is also an explanation that patients with a history of migraine avoid migraine triggers (i.e., cigarette smoking, alcohol, stress, poor sleep), and some may increase the breast cancer risk [30, 36–39]. In addition, migraine was not associated with breast cancer risk, as reported by a 2015 meta-analysis of 115,378 Nurses Health Studies (HR = 0.95, 95% CI = 0.87 to 1.04) [11]. A recent observational study with a follow-up of up to 7.3 years concluded that women who see more than 4 medical visits per year for migraines tend to be at a nearly twofold higher risk of breast cancer than the control cohort [12]. Although most observational studies suggest that migraine sufferers have a lower risk of breast cancer, migraine and breast cancer, the mechanism of action of estrogen is very complex, which makes the relationship between them unclear [40]. Possible reasons for conflicting conclusions include those studies being conducted in different regions, and they may have different confounding factors affecting breast cancer risk; for example, in women with migraine, independent risk factors for breast cancer include age and alcohol-related disorders, and independent protective factors include the use of antihypertensive drugs, statins, and NSAIDs [12]. In addition, Fan et al. suggested that breast cancer patients may have underestimated the history of migraine because of recall bias, and unmeasured selection bias and confounding factors may have influenced the results [12]. Observational studies are challenging to avoid, and MR studies use genetic proxy tools to study the relationship between exposure and outcome, which can largely avoid this effect. In addition, this study excluded some IVs related to confounding factors by performing the PhenoScanner GWAS datasets. Another strength of our MR study was that two large sample size European datasets were used for SNP-longevity associations. Moreover, there were no indications of pleiotropy or heterogeneity observed in the sensitivity analysis at the last step. We deem that our results differ from those of most previous observational studies because our MR studies can avoid selection bias and confounding factors, which may be unmeasured for observational studies.
It is worth noting that the findings of this study are difficult to interpret as the subtype analysis shows conflicting results when the sample of another subtype is added. For example, AM was associated with a higher risk of ER + breast cancer, but not ER- breast cancer. Some observational studies also shown that the relationship between migraine and breast cancer differed according to hormone receptor status [10, 32]. A meta-analysis about the relationship between migraine and breast cancer also found that there is some subtle heterogeneity by hormone-receptor status of breast cancer [11]. The findings of these observational studies are consistent with our MR analysis.
The mechanisms by which migraine might increase breast cancer risk are probably multifactorial. Migraine patients are more likely to have negative moods, anxiety, insomnia and even depression [41, 42], which are risk factors for breast cancer [43–45]. In addition, Migraine patients tend to reduce physical activity and increase sedentary time to reduce symptoms during a headache attack [46]. But these life behaviors can increase breast cancer risk [47–49].
There are still several limitations in our study. First, most migraine diagnoses are self-reported. Therefore, we cannot rule out misdiagnosis; for example, tension headaches are reported as migraine. Second, we were unable to obtain complete GWAS data of migraine due to the data limitations, so we were unable to perform multivariate MR to adjusted potential confounders, and we were still unable to perform the LDSC to make the genetic correlations of migraine and breast cancer, but we excluded confounder-related IVs as much as possible by browsing the PhenoScanner GWAS datasets. We can believe that the independent genetic variants related to migraine were reliable due to the rigorous investigation on the GWAS study. The lack of multivariate MR analysis should not diminish the role of migraine as etiological for breast cancer. Women with a history of migraine should strengthen breast cancer screening to be diagnosed early and treated adequately. Third, our outcomes and exposures are all of European descent and lack universality. Research on other races will be necessary for the future because of the high heterogeneity of migraine and breast cancer. Forth, we cannot rule out the existence of potential horizontal pleiotropy leading to biased results in MR studies, although comprehensive array of sensitivity analysis didn’t detect any pleiotropy. Fifth, we could not evaluate the nonlinear associations between migraine and breast cancer without individual-level data. In addition, the relatively small phenotypic variance of MA (approximately 0.9%) due to only 3 SNPs were selected, which requires larger GWAS studies to obtain more genetic data in the future study.
Conclusion
Previous observational studies have been controversial as to whether women with a history of migraine have an increased risk of breast cancer. We, as the first study to utilize MR analysis, also made significant discoveries. Our study found that migraine may be a risk factor for overall breast cancer and ER + breast cancer but not ER- breast cancer. In subtype analysis, MO may increase the risk of ER- breast cancer and is suggestively associated with the risk of overall breast cancer but not ER + breast cancer. No evidence to support the association of MA with breast cancer and its subtypes. Therefore, women with a history of migraine, especially MO, should strengthen breast cancer screening to be diagnosed early and treated adequately.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We want to thank the BCAC, the IHGC for sharing data. We would like to thank American Journal Experts (www.aje.com) for English language editing.
Abbreviations
- MR
Mendelian randomization
- GWAS
Genome-wide association studies
- IVW
Inverse variant weighted
- MR-PRESSO
MR pleiotropy residual sum and outlier
- MR-RAPS
MR-Robust Adjusted Profile Score
- AM
Any migraine
- MO
Migraine without aura
- MA
Migraine with aura
- OR
Odds ratio
- CI
Confidence intervals
- FDR
False discovery rate
- ER+
Estrogen receptor-positive
- ER-
Estrogen receptor-negative
- NSAIDs
Nonsteroidal anti-inflammatory drugs
- SNPs
Single nucleotide polymorphisms
- IVs
Instrument variants
- LD
Linkage disequilibrium
- BMI
Body mass index
- WM
Weighted median
Authors’ contributions
TF, ZZ designed the study. ZZ, TF, ZH, WW, FJ conducted data analysis. TF conceived the project and wrote the manuscript. LZ revised and approved the paper. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Incubation Project, West China Hospital, Sichuan University (2019HXFH053).
Data Availability
The data of breast cancer can be obtained in MRCIEU (https://gwas.mrcieu.ac.uk/; ieu-a-1126; ieu-a-1127; ieu-a-1128). The data of IVs for migraine is reported in the supplementary tables of the published papers (DOI: 10.1038/s41588-021-00990-0). The code used in this article was shown in the Supplementary File Code.
Declarations
Ethics approval and consent to participate
Our study used publicly available datasets, the ethical approval and consent information for the above summary statistics were taken from the original publication.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tian Fang and Zhihao Zhang contributed equally to this work.
References
- 1.Smith LJ, Henderson JA, Abell CW, Bethea CL. Effects of ovarian steroids and raloxifene on proteins that synthesize, transport, and degrade serotonin in the raphe region of macaques. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology. 2004;29(11):2035–45. doi: 10.1038/sj.npp.1300510. [DOI] [PubMed] [Google Scholar]
- 2.Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267(1):64–9. [PubMed] [Google Scholar]
- 3.Lipton RB, Bigal ME. Migraine: epidemiology, impact, and risk factors for progression. Headache. 2005;45(Suppl 1):3–s13. doi: 10.1111/j.1526-4610.2005.4501001.x. [DOI] [PubMed] [Google Scholar]
- 4.Kalkman DN, Couturier EGM, El Bouziani A, Dahdal J, Neefs J, Woudstra J et al. Migraine and cardiovascular disease: what cardiologists should know. Eur Heart J. 2023. [DOI] [PubMed]
- 5.Islamoska S, Hansen ÃM, Wang HX, Garde AH, Andersen PK, Garde E, et al. Mid- to late-life migraine diagnoses and risk of dementia: a national register-based follow-up study. J Headache Pain. 2020;21(1):98. doi: 10.1186/s10194-020-01166-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elser H, Skajaa N, Ehrenstein V, Fuglsang CH, Farkas DK, Sørensen HT. Cancer risk in patients with migraine: a population-based cohort study in Denmark. Headache. 2022;62(1):57–64. doi: 10.1111/head.14251. [DOI] [PubMed] [Google Scholar]
- 7.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 8.Li CI, Mathes RW, Malone KE, Daling JR, Bernstein L, Marchbanks PA, et al. Relationship between migraine history and breast cancer risk among premenopausal and postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2009;18(7):2030–4. doi: 10.1158/1055-9965.EPI-09-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghorbani A, Moradi A, Gookizadeh A, Jokar S, Sonbolestan SA. Evaluation of relationship between breast cancer and migraine. Adv Biomed Res. 2015;4:14. doi: 10.4103/2277-9175.148297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winter AC, Rexrode KM, Lee IM, Buring JE, Tamimi RM, Kurth T. Migraine and subsequent risk of breast cancer: a prospective cohort study. Cancer Causes Control. 2013;24(1):81–9. doi: 10.1007/s10552-012-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winter AC, Rice MS, Fortner RT, Eliassen AH, Kurth T, Tamimi RM. Migraine and breast cancer risk: a prospective cohort study and meta-analysis. J Natl Cancer Inst. 2015;107(1):381. doi: 10.1093/jnci/dju381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fan CY, Lin CS, Huang WY, Lin KT, Chao HL, Tsao CC, et al. Association between migraine and breast Cancer risk: a Population-Based Cohort Study and Literature Review. J Womens Health (Larchmt) 2018;27(12):1499–507. doi: 10.1089/jwh.2018.6929. [DOI] [PubMed] [Google Scholar]
- 13.Badsha MB, Fu AQ. Learning causal Biological Networks with the Principle of mendelian randomization. Front Genet. 2019;10:460. doi: 10.3389/fgene.2019.00460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Z, Fang T, Chen L, Qiu B, Lv Y. Thyroid function and COVID-19 susceptibility and its severity: a two-sample mendelian randomization study. Endocrinology. 2022;163(11). [DOI] [PubMed]
- 15.Zhang Z, Fang T, Lv Y. Causal associations between thyroid dysfunction and COVID-19 susceptibility and severity: a bidirectional mendelian randomization study. Front Endocrinol (Lausanne) 2022;13:961717. doi: 10.3389/fendo.2022.961717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haycock PC, Burgess S, Wade KH, Bowden J, Relton C, Davey Smith G. Best (but oft-forgotten) practices: the design, analysis, and interpretation of mendelian randomization studies. Am J Clin Nutr. 2016;103(4):965–78. doi: 10.3945/ajcn.115.118216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swerdlow DI, Kuchenbaecker KB, Shah S, Sofat R, Holmes MV, White J, et al. Selecting instruments for mendelian randomization in the wake of genome-wide association studies. Int J Epidemiol. 2016;45(5):1600–16. doi: 10.1093/ije/dyw088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hautakangas H, Winsvold BS, Ruotsalainen SE, Bjornsdottir G, Harder AVE, Kogelman LJA, et al. Genome-wide analysis of 102,084 migraine cases identifies 123 risk loci and subtype-specific risk alleles. Nat Genet. 2022;54(2):152–60. doi: 10.1038/s41588-021-00990-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23(R1):R89–98. doi: 10.1093/hmg/ddu328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mägi R, Morris AP. GWAMA: software for genome-wide association meta-analysis. BMC Bioinformatics. 2010;11:288. doi: 10.1186/1471-2105-11-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Michailidou K, Lindström S, Dennis J, Beesley J, Hui S, Kar S, et al. Association analysis identifies 65 new breast cancer risk loci. Nature. 2017;551(7678):92–4. doi: 10.1038/nature24284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–65. doi: 10.1002/gepi.21758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–25. doi: 10.1093/ije/dyv080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some Invalid Instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304–14. doi: 10.1002/gepi.21965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhao Q, Chen Y, Wang J, Small DS. Powerful three-sample genome-wide design and robust statistical inference in summary-data mendelian randomization. Int J Epidemiol. 2019;48(5):1478–92. doi: 10.1093/ije/dyz142. [DOI] [PubMed] [Google Scholar]
- 27.Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–8. doi: 10.1038/s41588-018-0099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeung CHC, Schooling CM. Systemic inflammatory regulators and risk of Alzheimer’s disease: a bidirectional mendelian-randomization study. Int J Epidemiol. 2021;50(3):829–40. doi: 10.1093/ije/dyaa241. [DOI] [PubMed] [Google Scholar]
- 29.Buse DC, Loder EW, Gorman JA, Stewart WF, Reed ML, Fanning KM, et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2013;53(8):1278–99. doi: 10.1111/head.12150. [DOI] [PubMed] [Google Scholar]
- 30.Hesari E, Ahmadinezhad M, Arshadi M, Azizi H, Khodamoradi F. The association between migraine and breast cancer risk: a systematic review and meta-analysis. PLoS ONE. 2022;17(2):e0263628. doi: 10.1371/journal.pone.0263628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reddy N, Desai MN, Schoenbrunner A, Schneeberger S, Janis JE. The complex relationship between estrogen and migraines: a scoping review. Syst Reviews. 2021;10(1):72. doi: 10.1186/s13643-021-01618-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mathes RW, Malone KE, Daling JR, Davis S, Lucas SM, Porter PL, et al. Migraine in postmenopausal women and the risk of invasive breast cancer. Cancer Epidemiol Biomarkers Prev. 2008;17(11):3116–22. doi: 10.1158/1055-9965.EPI-08-0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khuder SA, Mutgi AB. Breast cancer and NSAID use: a meta-analysis. Br J Cancer. 2001;84(9):1188–92. doi: 10.1054/bjoc.2000.1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hofer S, Linnebank M, Weller M, Bahmanyar S, Montgomery SM, Hillert J, et al. Cancer risk among patients with multiple sclerosis and their parents. Neurology. 2010;74(7):614–5. doi: 10.1212/WNL.0b013e3181c777b7. [DOI] [PubMed] [Google Scholar]
- 35.Cui Y, Deming-Halverson SL, Shrubsole MJ, Beeghly-Fadiel A, Cai H, Fair AM, et al. Use of nonsteroidal anti-inflammatory drugs and reduced breast cancer risk among overweight women. Breast Cancer Res Treat. 2014;146(2):439–46. doi: 10.1007/s10549-014-3030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li CI, Mathes RW, Bluhm EC, Caan B, Cavanagh MF, Chlebowski RT, et al. Migraine history and breast cancer risk among postmenopausal women. J Clin Oncol. 2010;28(6):1005–10. doi: 10.1200/JCO.2009.25.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu X, Wang M, Li S, Zhang Y. Migraine and breast cancer risk: a meta-analysis of observational studies based on MOOSE compliant. Medicine. 2016;95(30):e4031. doi: 10.1097/MD.0000000000004031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarker MA, Rahman M, Harun-Or-Rashid M, Hossain S, Kasuya H, Sakamoto J, et al. Association of smoked and smokeless tobacco use with migraine: a hospital-based case-control study in Dhaka, Bangladesh. Tob Induc Dis. 2013;11(1):15. doi: 10.1186/1617-9625-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pimhanam C, Sangrajrang S, Ekpanyaskul C. Tobacco smoke exposure and breast cancer risk in thai urban females. Asian Pac J cancer Prevention: APJCP. 2014;15(17):7407–11. doi: 10.7314/apjcp.2014.15.17.7407. [DOI] [PubMed] [Google Scholar]
- 40.Arnesen S, Blanchard Z, Williams MM, Berrett KC, Li Z, Oesterreich S, et al. Estrogen receptor alpha mutations in breast Cancer cells cause gene expression changes through constant activity and secondary Effects. Cancer Res. 2021;81(3):539–51. doi: 10.1158/0008-5472.CAN-20-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lv X, Xu B, Tang X, Liu S, Qian JH, Guo J, et al. The relationship between major depression and migraine: a bidirectional two-sample mendelian randomization study. Front Neurol. 2023;14:1143060. doi: 10.3389/fneur.2023.1143060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chu S, Wu Z, Wu Z, Wu J, Qian Y. Association between Insomnia and Migraine Risk: a case-control and bidirectional mendelian randomization study. Pharmgenomics Pers Med. 2021;14:971–6. doi: 10.2147/PGPM.S305780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu HP, Wei JC, Yip HT, Yeh MH. Association of Insomnia, Depressive Disorders, and Mood Disorders as risk factors with breast Cancer: a Nationwide Population-Based Cohort Study of 232,108 women in Taiwan. Front Oncol. 2021;11:757626. doi: 10.3389/fonc.2021.757626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu L, Bao H, Wang F, Yu L, Cong S, Zhou F, et al. Depressive symptoms and sleep duration as risk factors for breast Cancer - China, 2020. China CDC Wkly. 2023;5(15):333–9. doi: 10.46234/ccdcw2023.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ohi K. Shared genetic correlation and causal association between major depressive disorder and breast cancer. BMC Med. 2023;21(1):203. doi: 10.1186/s12916-023-02905-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Farris SG, Thomas JG, Abrantes AM, Lipton RB, Burr EK, Godley FA, et al. Anxiety sensitivity and intentional avoidance of physical activity in women with probable migraine. Cephalalgia. 2019;39(11):1465–9. doi: 10.1177/0333102419861712. [DOI] [PubMed] [Google Scholar]
- 47.Dixon-Suen SC, Lewis SJ, Martin RM, English DR, Boyle T, Giles GG, et al. Physical activity, sedentary time and breast cancer risk: a mendelian randomisation study. Br J Sports Med. 2022;56(20):1157–70. doi: 10.1136/bjsports-2021-105132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guo W, Fensom GK, Reeves GK, Key TJ. Physical activity and breast cancer risk: results from the UK Biobank prospective cohort. Br J Cancer. 2020;122(5):726–32. doi: 10.1038/s41416-019-0700-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee J, Lee J, Lee DW, Kim HR, Kang MY. Sedentary work and breast cancer risk: a systematic review and meta-analysis. J Occup Health. 2021;63(1):e12239. doi: 10.1002/1348-9585.12239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data of breast cancer can be obtained in MRCIEU (https://gwas.mrcieu.ac.uk/; ieu-a-1126; ieu-a-1127; ieu-a-1128). The data of IVs for migraine is reported in the supplementary tables of the published papers (DOI: 10.1038/s41588-021-00990-0). The code used in this article was shown in the Supplementary File Code.