Abstract
Body lice and head lice are the most common ectoparasites of humans. Head lice (Pediculus humanus capitis) occur worldwide in children and their caretakers, irrespective of their social status. In contrast, body lice (Pediculus humanus corporis) are confined to marginalized population groups in countries of the Global South, homeless people, and refugees. Body lice are known to transmit an array of bacterial pathogens, such as R. prowazekii, R. rickettsii, C. burneti, B. quintana, B. recurrentis, and Y. pestis. The vector capacity of head lice is still a matter of debate. The objective of the review was to scrutinize the existing evidence on the vector capacity of head lice for the transmission of bacterial pathogens. The PUBMED database was searched using a combination of the terms “pediculus humanus” OR “body lice” OR “head lice” AND “pathogen” OR “Rickettsia prowazekii” OR “Bartonella quintana” OR “Borrelia recurrentis” OR “Coxiella burneti” without a time limit. Data from epidemiological studies as well as historical observations demonstrate that body lice and head lice can carry the same array of pathogens. Since the presence of a bacterial pathogen in an arthropod is not sufficient to state that it can be transmitted to humans, and since experimental models are lacking, as yet one cannot conclude with certainty that head lice serve as vectors, although this review presents circumstantial evidence that they do. Adequately designed experimental and epidemiological studies are needed to ascertain the exact transmission potential of head lice.
Keywords: Pediculus humanus, Head lice, Body lice, Bacterial pathogen
Background
Human lice, Pediculus humanus, have been known as human ectoparasites for thousands of years. They have been identified at burying sites in Israel from 60 A.D. [1] and in mummies from Amerindians buried in Peru at an altitude of 3000 m around 3000 years ago [2]. Lice are obligate blood-sucking parasites. Phylogenetically, they belong to different mitochondrial clades of which the geographical distribution shows some differences, although overlapping of clades is common [3, 4]. Head lice occur globally and affect millions of children and their caretakers, irrespective of their social level. In contrast, nowadays body lice infest only marginalized population groups, such as homeless people and refugees, and occur in special settings such as in impoverished communities situated at high altitude in Ethiopia or in prisons in low-income countries, where hygienic conditions are poor, and crowding is common [5]. Until a few years ago, scientists assumed that only body lice can transmit bacterial pathogens. If head lice have a similar vector capacity for the transmission of important bacterial pathogens, then the potential health threat caused by head lice infestation should be several orders of magnitude greater compared to body lice. The objective of the review was to summarize the existing knowledge on the vector capacity of head lice for the transmission of bacterial pathogens in a comprehensive manner.
Materials and methods
Search strategies and selection criteria
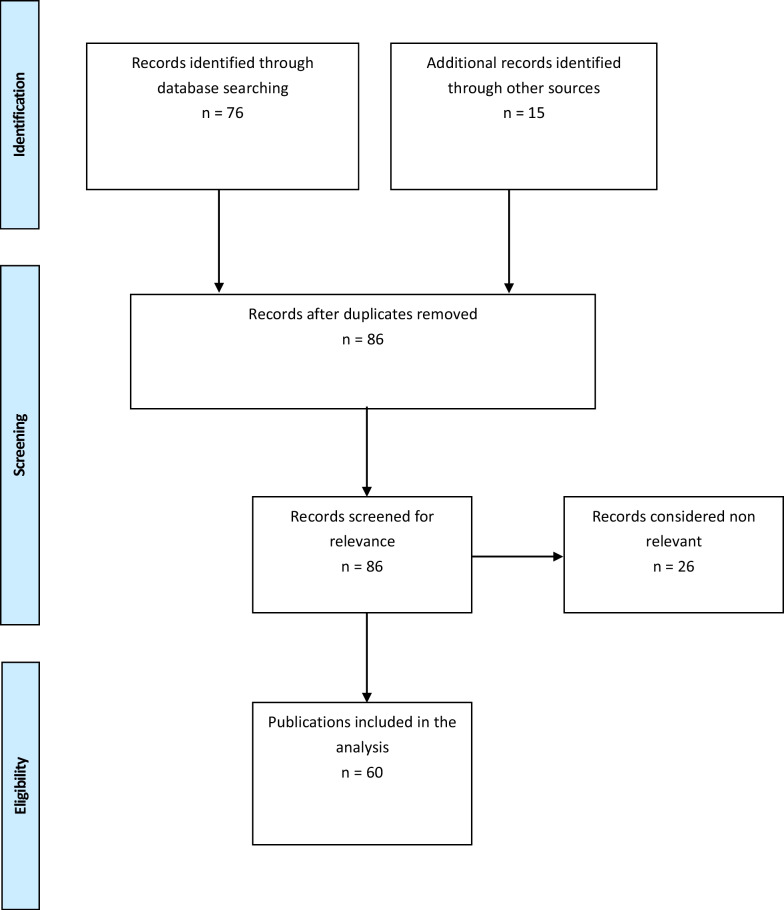
The results of this study are reported according to the Preferred Reporting Items for Systematic Reviews (PRISMA). The PUBMED database was searched using a combination of the terms “pediculus humanus” OR “body lice” OR “head lice” AND “pathogen” OR “Rickettsia prowazekii” OR “Bartonella quintana” OR “Borrelia recurrentis” OR “Coxiella burneti” without a time limit. Additional searches were undertaken in textbooks. Reference lists of papers included in the analysis were manually searched. Historical or anecdotal articles were taken from the library of the author. The abstracts of the articles were screened for relevance with regard to the objective of the study. The full-text articles were reviewed for eligibility. Articles were considered eligible when methods and results were described comprehensively and adequately (see flow chart Fig. 1).
Fig. 1.
Flow diagram of the literature search
Data extraction and analysis
Data extracted included study origin, design of the study, characteristics of settings and participants, and results. All data extracted are summarized in Tables 1, 2 and 3 and narratively described in the text.
Table 1.
Experimental studies confirming body lice as vectors of bacterial pathogens
Table 2.
Epidemiological studies in population groups infested with head lice
| Country; area/city | Year | Study design/detection of DNA of | Number of persons/lice examined | Number of lice positive (%) | Pathogens identified | Remarks | References |
|---|---|---|---|---|---|---|---|
| Democratic Republic of Congo; Kinshasa | 2019 | Examination of patients hospitalized at the Monkole Hospital Center/B. quintana, B. recurrentis, R. prowazekii, Anaplasma spp., Y. pestis, C. burneti, Acinetobacter spp. | 27/181 |
54/181 (29.8%) |
A. baumannii; A. johnsonii; A. sai; A. pittii; A. guillouiae; A. pediculi | Head lice belonged to clade A, D, E; 44% of the infested patients had head lice from different clades | [28] |
| Madagascar; rural communities in the Southeast | 2019 | Collection of head lice from inhabitants of rural communities/B. quintana, Acinetobacter spp. | 33/151 |
20/151 (30.2%) |
B. quintana 12.6%; Acinetobacter 42.1% |
Frequency of pathogens varied considerably between villages | [23] |
|
Algeria; Algier |
2019 |
Collection of head lice from refugees from Niger and school children/ Rickettsia spp., Borrelia spp., B. quintana; Y. pestis, C. burneti; Anaplasma spp.; Acinetobacter spp. |
70 refugees, 101 school children/ 37 lice from refugees, 45 lice from school children |
C. burneti: lice positive school children 0/45 (0%)] refugees 3/31 (9.7%) Acinetobacter spp. school children 25/45 (55.6%) refugees 25/31 (80.6%) |
C. burneti; A. baumanii; A. johnsonii; A. variabilis |
Head lice belonged to clade A, B, E | [25] |
| Mali; Koulikoro region | 2017 | Collection of head lice from patients presenting at rural health centers Patients were examined for presence of head and body lice; only head lice were present/B. quintana, Rickettsia spp., Anaplasma spp. | 117/600 |
B. quintana lice positive 3/600 (0.5%) C. burneti: lice positive 6/117 (5.1%) Rickettsia spp. lice positive 4/600 (0.6%) |
B. quintana C. burneti Rickettsia spp. Anaplasma spp. |
Lice belonged to clade E but showed many different haplotypes | [24] |
| Democratic Republic of Congo; tropical rain forest inhabited by pygmies | 2016 |
Collection of head lice from healthy individuals of 3 communities/ Borrelia spp., Bartonella spp., Acinetobacter spp., Rickettsia spp., R. prowazekii, Y. pestis, Anaplasma spp. |
120/630 |
lice positive 246/630 (39.0%) Borrelia spp. 11/630 (1.7%) (B. recurrentis 10/11 (90.9%) B. theileri 1/11 (9.1%), |
Borrelia spp. A. junii, A. ursingii, A. baumannii, A. johnsonii, A. schindleri, A. lwoffii, A. nosocomialis, A. towneri, Moraxella spp. |
lice belonged to clade A, C, D; distribution of clades differed between villages | [26] |
| Thailand; schools in different areas of the country | 2015 | Head lice collected from school children/Bartonella spp., Acinetobacter spp. | 26/275 | lice positive 10/275 (3.7%) |
A. baumannii, A. radioresistens, A. schindleri |
[29] | |
| Ethiopia | 2013 | Head lice collected from patients with louse-borne relapsing fever | 24/35 |
Lice positive 8/35 (23.0%) |
B. recurrentis | [27] | |
| France | 2011 |
Head lice collected from school children during an epidemiological survey/ B. quintana A. baumannii |
?/288 |
A. baumannii lice positive 95/288 (33.0%) |
A. baumannii | [30] |
Table 3.
Epidemiological studies in population groups co-infested with head lice and body lice
| Country; area/city | Year | Study design/detection of DNA of | Number of persons/lice examined | Number of lice positive (%) | Pathogens identified | Remarks | References |
|---|---|---|---|---|---|---|---|
| France; town near Paris | 2018 | Head lice and body lice were collected from in-patients of the Avicenne Hospital and homeless people/Acinetobacter spp.; R. prowazekii; Y. pestis; Borrelia spp.; B. quintana; C. burneti; Anaplasma spp. | 141/head lice: 235; body lice: 24 |
B. quintana: Head lice: 0/235 (0%) Body lice: 4/24 (16.7%) Acinetobacter spp.: Head lice 27/235 (11.5%) Body lice 7/24 (29.1%) |
B. quintana Acinetobacter spp. |
Lice belonged to Clade A, B, E | [3] |
| Democratic Republic of Congo; Oriental province | 2015 | Collection of head lice and body lice from healthy individuals living in a Y. pestis endemic area/B. quintana, Y. pestis |
37/examined for B. quintana Head lice: 7 Body lice: 30 Examined for Y. pestis Head lice: 31 Body lice: 143 |
B. quintana Head lice: 6/31 (19.4%) Body lice: 48/143 (33.5%) Y. pestis Head lice 1/31 (3.2%) Body lice 2/148 (1.4%) |
B. quintana, Y. pestis | Lice of 7 persons were infected with B. quintana, Y. pestis or both pathogens; Clade A contained head lice and body lice; Clade D contained only body lice | [4] |
| USA, San Francisco | 2014 | Collection of head lice and body lice from self-selected homeless people/B. quintana | 203/head lice: 10/203; body lice: 60/203; both types 6/203 |
Head lice: 37.5% Body lice: 15.9%a |
B. quintana | [50] | |
| Ethiopia; Bahir Da Hospital | 2013 | Examination of head lice + body lice collected from in-patients in whom Borrelia spp. were identified microscopically in blood smear/B. recurrentis | 24/35 head lice; 62 body lice |
Head lice: 8/35 (22.9%) Body lice: 25/62 (40.3%) |
B. recurrentis | Clades not determined; in co-infested patients B. recurrentis DNA was detected more often in body lice than in head lice | [27] |
| Democratic Republic of Congo; Oriental province, Rethy Health District | 2013 | Head and body lice were collected from individuals living in a Y. pestis endemic area/R. prowazekii, B. recurrentis, B. quintana, Y. pestis | Number of persons not detailed/35 head lice; 154 body lice |
B. quintana: Head lice 6/35 (17.1%) Body lice 50/154 (32.5%) Y. pestis 1/35 head lice (2.9%) 2/154 body lice (1.3%) |
B. quintana Y. pestis |
[31] | |
| Ethiopia; 8 villages located at different altitudes in SW Ethiopia | 2011 | Collection of head lice + body lice from individuals living in a B. quintana endemic area/B. quintana | 134/head lice:271; body lice: 424 |
Head lice: 19/271 (7.0%) Body lice: 76/424 (17.9% |
B. quintana | Head lice belonged to clade C, body lice belonged to clade A; in co-infested persons only head lice or only body lice were infected with B. quintana | [32] |
| Burundi; various sites | 2002 | Lice were collected during an outbreak of epidemic typhus in Burundi/R. prowazekii, B. quintana | No data provided/no data provided |
Body lice: R. prowazekii 7–35% B. quintana 2–90% Head lice: no data provided |
R. prowazekii B. quintana |
Not clear how many body and head lice were collected/examined | [20] |
| Nepal; Pokhara town + slum in Katmandu | 2006 | Lice were collected from healthy children/B. quintana | No data provided/no data provided |
Town: Head lice: 0% Body lice: 12.5% Slum: Head lice: 25% Body lice: 19% |
B. quintana | [21] | |
| USA; San Francisco | 2009 | Head and body lice were collected from homeless persons/B. quintana | 138/no data provided |
Head lice: 8% Body lice: 5%b |
B. quintana | [22] | |
| Ethiopia; rural communities in the Southeast | 2012 | Head and body lice collected from healthy individuals/A. baumannii | 134/head lice: 115; body lice: 109 |
Head lice: 54/115 (47%) Body lice: 77/109 (71%) |
A. baumannii | [34] | |
| Algeria, Mali, Senegal, Ethiopia, Democratic Republic of Congo, Rwanda, Burundi, Kenya, Madagascar | 2014 | Not details provided where and how lice were collected/B. quintana | Not detailed/1040 lice in total; head lice: 616; body lice: 424c |
Head lice: 10/616 (1.6%) Body lice: 228/424 (54.0%) |
B. quintana |
Proportion of head and/or body lice infected differed considerably between settings Range head lice: 0–17.1% Range body lice: 4.5–89.7% All head and body lice infected with B. quintana belonged to clade A2 |
[33] |
aHead lice and body lice were examined as pools
bPositivity rate from pools of lice
cAbsolute and relative number of head and body lice differed considerably between collection on sites; in some sites only head lice were collected
Main text
Historical evidence
In 2001, a mass grave of Napoleon’s soldiers was detected in Vilnius, Lithuania. About 3000 soldiers had obviously been buried in a hurry, the skeletons being in close proximity and in positions indicating that they were buried before rigor mortis had set in [6]. At a site where 717 individuals were buried in a trench, teeth were extracted from corpses and remains of five lice were recovered. Using suicide PCR in the pulpa of 4 out of 72 teeth, DNA of R. prowazekii was identified. The recovered lice were considered to be body lice on the basis of morphology and sequence data [6]. B. quintana DNA was identified in ten teeth and three lice.
The hygienic conditions during the retreat of Napoleon’s army in the winter of 1812 must have been very poor and crowding in shelters where the soldiers passed the nights must have been intense, making the propagation of both head lice and body lice very likely. Hence, if the soldiers who died from typhus obviously were infested with body lice, it is highly probable that they were also infested with head lice.
There is circumstantial evidence that in the Second Plague Pandemic in Europe (fourteenth–nineteenth century), including the period of the Black Death (1346–1353), Pediculus humanus acted as vector for Yersinia pestis and that the role of fleas in the transmission of the pathogen was overestimated for centuries [7]. Historical data convincingly indicate that during the period of the Second Plague Pandemic the great majority of people were extremely poor and lived in miserable conditions. Poor hygiene was the rule and head lice and body lice were extremely widespread [8]. Using a compartment model for plague transmission kinetics, Dean et al. [9] showed that transmission by Pediculus humanus fitted significantly better to the mortality curves from nine local outbreaks during the Second Plague Pandemic than models for airborne transmission (as it occurs in pneumonic plague) or rodent transmission. Even at the end of the nineteenth century, in cities, such as Hamburg, Germany, Pediculus humanus capitis was rampant in impoverished population groups, and head lice occurred in all age groups [10].
In World War I, a relapsing fever of unknown origin developed into an epidemic affecting around 400,000 German soldiers and 800 000 allied troops stationed in Northern France between 1915 and 1918 [11]. In 1916, the German bacteriologist Hans Töpfer identified a Rickettsia microorganism in body lice from a patient with a similar type of relapsing fever [12]. The infectious agent was called R. quintana, later the name was changed to Bartonella quintana. The disease got the name trench fever, as it emerged in soldiers living for months/years under very poor hygienic conditions in the trenches of the battlefield [11]. Besides, the shelters in the trenches, where soldiers lived and slept, were extremely crowded, making the propagation of body and head lice very likely.
Anecdotal reports mention that trench fever occurred in relatives of returning soldiers [11]. However, this does not indicate that B. quintana was only transferred by body lice: as a general rule, soldiers immediately changed infested clothes when they returned home, so that the likelihood of the presence of body lice was low. In contrast, head lice may have gone unnoticed for some time, because only about one-third of infested individuals develop symptoms.
Between 1940 and 1942, a devastating typhus epidemic occurred in the Warsaw Ghetto causing an estimated 16,000–22,000 deaths [13]. The Ghetto was declared as a “restricted infectious disease area” by the German military administration and was fenced off with a 3 m high wall. The residents became trapped in a kind of oversized prison from which escape was not possible. In the hermetically sealed area, 445,000 people lived temporarily, corresponding to 131,000 inhabitants per square kilometer—the highest population density ever recorded. The hygienic conditions under which the people lived were extremely poor: water pipes and sewers were destroyed by bombs and toilets did not work properly. Water was scarce, and the majority of the public bathhouses was closed down. As soon as a case of typhus became known, the whole family was forced into quarantine for two weeks, which in turn increased crowding and made adequate hygiene impossible.
According to the biography of Dr. Ludwig Hirszfeld, a physician and microbiologist who spent 3 years in the Ghetto and who developed a method to cultivate R. prowazekii, the infestation with head and body lice was omnipresent [14]. Supposedly, in the living conditions of the Ghetto, infection of body and head lice through sucking of blood from a patient with typhus had the same likelihood. Interestingly, the incidence rate of typhus started to decrease when hygienic measures directed against both body and head lice were implemented [13].
Evidence from experimental studies
Since the pioneering work of Nicolle in 1912 cited in [15], an impressive number of experimental studies showed that body lice can transmit an array of highly pathogenic bacteria (Table 1). In contrast, rather few experimental studies were performed with head lice. In 1912, Goldberger and Anderson [16] collected head lice from the hair of patients with typhus and used these lice to infect rhesus monkeys with R. prowazekii. Their findings were later confirmed by Murray and Torrey [17], who infected head lice with R. prowazekii by feeding these lice on a rabbit infected with this pathogen. Using labelled antibodies, the authors demonstrated that 6 days after feeding head lice passed infective Rickettsiae in their faeces. These findings were confirmed by Robinson et al. 2003 [18]. Recently, using laboratory-raised head and body lice, it was shown that after oral feeding with blood containing a defined number of B. quintana bacteria, the number of B. quintana present in the faeces was almost the same in body and in head lice [19]. However, the authors observed that the average viability of B. quintana became lower in head than in body lice during an observation period of 11 days. Whether this might have an impact on the transmission of B. quintana through contact with flea faeces was not investigated. These findings corroborate previous observation showing the presence of B. quintana DNA in head lice [20–22].
Evidence from epidemiological studies
Since 2015, an impressive number of epidemiological studies showed that head lice are infected with a panel of bacterial pathogens. In one group of studies, participants were infested only with head lice and lived in different settings in Thailand, Algeria, Mali, Democratic Republic of Congo, and Madagascar (Table 2). Study sites were selected, such that Borrelia recurrentis, Bartonella quintana or Coxiella burneti were expected to occur in the local population. B. quintana was detected in head lice from inhabitants of rural areas in Madagascar and Mali [23, 24], C. burneti in head lice collected from school children in Algiers as well as in refugees and healthy individuals from Niger [24, 25]. B. recurrentis was detected in head lice collected from pygmies living in the tropical rainforest in the Democratic Republic of Congo [26] and in inpatients with louse-borne relapsing fever in Ethiopia [27]. In addition, 14 different species of Acinetobacter were identified in head lice, including hitherto unknown species [23, 25, 26, 28–30].
In the second group of studies, participants were infested with both head lice and body lice (Table 3). Here, settings were selected, such that B. recurrentis, B. quintana, R. prowazekii or Y. pestis were likely to circulate in the local population. B. quintana-DNA was detected in head lice collected from healthy individuals in the Democratic Republic of Congo [4, 31], Ethiopia [32], Nepal [21] and other African countries [33]. In a study on trench fever in Ethiopia, either head lice or body lice were infected with B. quintana [32]. Bonilla et al. [22] examined 138 homeless adults from San Francisco for the presence of body lice and head lice. 23.9% of the individuals were infested with body lice, 8.7% with head lice, and 4.3% had co-infestations. Bartonella DNA was detected in 33.3% of body lice-infested persons and in 25.0% of head lice-infested persons. When pools of lice were compared, the positive rate for B. quintana DNA was 5.0% in body lice and 8.3% in head lice.
In a study on B. quintana in head lice of Nepalese children Sasaki et al. [21] identified B. quintana in 0% of head lice recovered from healthy school children living in a rural town, but in 12.5% of head lice collected from the scalp of street children. Homeless children were significantly more often co-infested with body lice than children from the rural town.
40.3% of head lice from double-infested patients with louse-borne relapsing fever in Ethiopia carried B. recurrentis [27]. B. recurrentis was also identified in head lice of pygmies from the Democratic Republic of Congo [28].
Yersinia pestis was detected in head lice from double-infested individuals living in a Y. pestis endemic area [4, 31]. In the latter study 2.9% of the head lice were infected with Y. pestis in contrast to 1.3% of body lice.
Acinetobacter spp. were recovered from head lice collected from school children in France [3, 29] and healthy individuals living in Southeast Ethiopia [34]. In the double-infested Ethiopians 47% of the head lice and 71% of the body lice carried A. baumannii [34]. None of the studies was designed to determine whether the infection rates in head lice and body lice were significantly different.
Evidence from louse-borne relapsing fever imported to Europe by refugees
When in 2015 thousands of asylum-seeking young Africans reached Europe, louse-borne relapsing fever emerged in intensive care units in Italy, Switzerland, The Netherlands, Germany and even Finland [35–42]. Diagnosis of louse-borne relapsing fever was confirmed by PCR in all cases. Twenty-three of the patients were from Somalia and three from Eritrea. They had all taken a similar travel route through Kenya, Ethiopia, the Sudan, Libya and Italy. Before crossing the Mediterranean Sea, they had stayed in Libya in a concentration-camp-like setting for up to a year. Head lice as well as body lice are likely to occur in such settings and transmission of B. recurrentis must have been common [43].
Louse-borne relapsing fever developed between 3 days and 3 years after the refugee had reached the city, where he fell sick and was admitted to the hospital [40, 44]. Only in one case a louse was detected. It was judged to be a body louse by macroscopic examination [41]. As head lice were not systematically looked for, the presence of head lice cannot be ruled out. The observation that refugees spent a few weeks (in some cases up to 1 year) in Rome or Turin in crowding conditions before developing relapsing fever, and the fact that the clothes of refugees arriving in Italy had to be completely changed immediately after arrival, make it likely that head lice were responsible for the transmission of B. recurrentis [36, 44].
Conclusions and discussion
Head lice occur worldwide in children and their caretakers with prevalences up to 40% in resource-poor settings [45]. In contrast, body lice only occur in homeless people and refugees, or occur in impoverished communities situated at high altitude in rural Ethiopia or in prisons in low-income countries, where hygienic conditions are poor, and crowding is common [46–48]. In 1999, Raoult and Roux assumed that body lice most probably can “transmit any agent ingested with a blood meal and capable of surviving in the insect’s midgut” [49]. Actually, there is plenty of evidence from experimental studies that body lice can transmit a broad array of pathogens (Table 1). Hitherto, only for R. prowazekii it was demonstrated that head lice can actively transmit this pathogen [15–17]. However, these studies were done in a time when no animal model suitable for head lice existed.
It should be noted that transmission of B. quintana is particular in the sense that faecal material of lice containing the pathogen has to be actively introduced into the skin, usually by scratching. Intense itch leading to scratching is typical for both types of lice infestation. Particularly in children with head lice infestation, excoriations of the scalp caused by scratching are common (H. Feldmeier, unpublished observation 2010). The odds that B. quintana is transmitted through scratching might, therefore, be higher.
Data from epidemiological studies indicate that head lice carry the same panel of bacterial pathogens as body lice, namely, R. prowazekii, B. quintana, B. recurrentis, Y. pestis, C. burneti and even Acinetobacter spp. (Tables 2, 3). Although in some studies the proportion of body lice infected with a defined pathogen seemed to be higher than in head lice, in other studies the contrary was the case [3, 4, 20, 21, 27, 31–33, 50]. Since none of the studies was powered to demonstrate a higher risk for infection of body lice compared to head lice with a defined pathogen, no conclusion can be drawn by comparing proportions of infected body lice versus infected head lice as done by the authors. Besides, the proportion of head lice infestation to body lice infestation in co-infested individuals is not a constant and depends on the setting in which the study was performed as well as on cultural attitudes, such as length and thickness of hair or type of clothing. This is highlighted by studies from the Democratic Republic of Congo [4, 31], Ethiopia [32], Nepal [21], and homeless adults from San Francisco [22].
Moreover, some of the epidemiological studies seem to have been biased, because the differentiation of body and head lice was done based on morphological criteria or at which part of the body the louse was identified (body versus scalp). Studies performed on head and body lice from nine different African countries showed surprising morphological difference even within a country [33, 34]. Not only the size and the body proportion differed from country to country, but also the color. Whereas all head lice from Senegal, Madagascar and Ethiopia were of black color, body lice were black in Madagascar and Rwanda, brown in Kenya and grey in Ethiopia. Body and head lice from Ethiopia and Rwanda were black and indistinguishable by body size [33]. Assumably, in older studies head lice were mistaken for body lice, making a conclusion of their susceptibility to infection with a defined pathogen impossible [20].
Historical observations indicate that body lice and head lice could have transferred Y. pestis, B. quintana, and R. prowazekii from sick to healthy individuals [6–9, 11, 13, 14, 46]. In 1998, a puzzling case was reported concerning a traveler from Algeria who developed typhus after returning to France [51]. No body lice were found, but the patient did recall having had intensive pruritus of the scalp during his stay in Algeria indicating the presence of head lice.
It goes without saying that the presence of a bacterial pathogen in an arthropod is not sufficient to conclude that it can transmit to humans. Whether body lice and head lice actually have the same potential to transmit bacterial pathogens cannot be ascertained from the existing data. Further research is needed using standardized experimental models.
Acknowledgements
Not applicable.
Author contributions
Not applicable.
Funding
No funding.
Availability of data and materials
Data sharing is not applicable to this article as no data sets were generated or analyzed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mumcuoglu KY, Zias J, Tarshis M, Lavi M, Stiebel GD. Body louse remains found in textiles excavated at Masada, Israel. J Med Entomol. 2003;40(4):585–587. doi: 10.1603/0022-2585-40.4.585. [DOI] [PubMed] [Google Scholar]
- 2.Raoult D, Reed DL, Dittmar K, Kirchman JJ, Rolain JM, Guillen S, et al. Molecular identification of lice from pre-Columbian mummies. J Infect Dis. 2008;197(4):535–543. doi: 10.1086/526520. [DOI] [PubMed] [Google Scholar]
- 3.Candy K, Amanzougaghene N, Izri A, Brun S, Durand R, Louni M, et al. Molecular survey of head and Body Lice, Pediculus humanus, in France. Vector Borne Zoonotic Dis. 2018;18(5):243–251. doi: 10.1089/vbz.2017.2206. [DOI] [PubMed] [Google Scholar]
- 4.Drali R, Shako JC, Davoust B, Diatta G, Raoult D. A new clade of african body and head lice infected by Bartonella quintana and Yersinia pestis-Democratic Republic of the Congo. Am J Trop Med Hyg. 2015;93(5):990–993. doi: 10.4269/ajtmh.14-0686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Houhamdi L, Parola P, Raoult D. Les poux et les maladies transmises à l'homme. Med Trop. 2005;65(1):1–11. [PubMed] [Google Scholar]
- 6.Raoult D, Dutour O, Houhamdi L, Jankauskas R, Fournier PE, Ardagna Y, et al. Evidence for louse-transmitted diseases in soldiers of Napoleon's grand army in Vilnius. J Infect Dis. 2006;193:112–120. doi: 10.1086/498534. [DOI] [PubMed] [Google Scholar]
- 7.Ayyadurai S, Sabbane F, Raoult D, Drancourt M. Body Lice, Yersinia pestis orientalis and black death. Emerg Infect Dis. 2010;16(5):892. doi: 10.3201/eid1605.091280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Winkle S. Geißeln der Menschheit. Kulturgeschichte der Seuchen. Düsseldorf: Artemis & Winkler Verlag; 2005. p. 2005. [Google Scholar]
- 9.Dean KR, Krauer F, Walloe L, Lingjaerde OC, Bramanti B, Stenseth NC, et al. Human ectoparasites and the spread of plague in Europe during the Second Pandemic. Proc Natl Acad Sci U S A. 2018;115(6):1304–1309. doi: 10.1073/pnas.1715640115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evans RJ. Tod in Hamburg: Stadt, Gesellschaft und Politik in den Cholera-Jahren 1830–1910. Reinbek bei Hamburg: Rowohlt; 1990. [Google Scholar]
- 11.Ruiz J. Bartonella quintana, past, present, and future of the scourge of World War I. APMIS. 2018;126(11):831–837. doi: 10.1111/apm.12895. [DOI] [PubMed] [Google Scholar]
- 12.Töpfer H. Zur Ursache und Uebertragung des Wolhynischen Fiebers. Münch med Wschr. 1916;63:1495–1496. [Google Scholar]
- 13.Feldmeier H. Typhus in the Warsaw Ghetto 1940–1942: how an epidemic increased exponentially, was abated and eventually disappeared. One Health Implement Res. 2021;2(3):51–55. [Google Scholar]
- 14.Hirszfeld L. Geschichte eines Lebens. Leiden: Verlag Ferdinand Schöningh; 2018. [Google Scholar]
- 15.Gross L. How Charles Nicolle of the Pasteur Institute discovered that epidemic typhus is transmitted by lice: reminiscences from my years at the Pasteur Institute in Paris. Proc Natl Acad Sci USA. 1996;93:10539–10540. doi: 10.1073/pnas.93.20.10539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberger J, Anderson JF. The transmission of typhus fever, with especial reference to transmission by the head louse (Pediculus capitis). Public Health Rep. 1912:297–307.
- 17.Murray ES, Torrey SB. Virulence of Rickettsia prowazekii for head lice. Ann NY Acad Sci. 1975;266:25–34. doi: 10.1111/j.1749-6632.1975.tb35086.x. [DOI] [PubMed] [Google Scholar]
- 18.Robinson D, Leo N, Prociv P, Barker SC. Potential role of head lice, Pediculus humanus capitis, as vectors of Rickettsia prowazekii. Parasitol Res. 2003;90(3):209–211. doi: 10.1007/s00436-003-0842-5. [DOI] [PubMed] [Google Scholar]
- 19.Kim JH, Previte DJ, Yoon KS, Murenzi E, Koehler JE, Pittendrigh BR, et al. Comparison of the proliferation and excretion of Bartonella quintana between body and head lice following oral challenge. Insect Mol Biol. 2017;26(3):266–276. doi: 10.1111/imb.12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fournier PE, Ndihokubwayo JB, Guidran J, Kelly PJ, Raoult D. Human pathogens in body and head lice. Emerg Infect Dis. 2002;8(12):1515–1518. doi: 10.3201/eid0812.020111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sasaki T, Poudel SKS, Isawa H, Hayashi T, Seki N, Tomita T, et al. First molecular evidence of Bartonella quintana in Pediculus humanus capitis (Phthiraptera: Pediculidae), collected from Nepalese children. J Med Entomol. 2006;43(1):110–112. doi: 10.1093/jmedent/43.1.110. [DOI] [PubMed] [Google Scholar]
- 22.Bonilla DL, Kabeya H, Henn J, Kramer VL, Kosoy MY. Bartonella quintana in body lice and head lice from homeless persons, San Francisco, California, USA. Emerg Infect Dis. 2009;15(6):912–915. doi: 10.3201/eid1506.090054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eremeeva ME, Warang SS, Anderson ML, Capps D, Zohdy S, Durden LA. Molecular survey for pathogens and markers of permethrin resistance in human head lice (Phthiraptera: Pediculidae) from Madagascar. J Parasitol. 2019;105(3):459–468. [PubMed] [Google Scholar]
- 24.Amanzougaghene N, Fenollar F, Sangare AK, Sissoko MS, Doumbo OK, Raoult D, et al. Detection of bacterial pathogens including potential new species in human head lice from Mali. PLoS ONE. 2017;12(9):e0184621. doi: 10.1371/journal.pone.0184621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Louni M, Amanzougaghene N, Mana N, Fenollar F, Raoult D, Bitam I, et al. Detection of bacterial pathogens in clade E head lice collected from Niger's refugees in Algeria. Parasit Vectors. 2018;11(1):348. doi: 10.1186/s13071-018-2930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amanzougaghene N, Akiana J, Mongo Ndombe G, Davoust B, Nsana NS, Parra HJ, et al. Head lice of pygmies reveal the presence of relapsing fever Borreliae in the Republic of Congo. PLoS Negl Trop Dis. 2016;10(12):e0005142. doi: 10.1371/journal.pntd.0005142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boutellis A, Medlannikov O, Bilcha KD, Ali J, Campelo D, Barker SC, et al. Borrelia recurrentis in Head Lice, Ethiopia. Emerg Infect Dis. 2013;19:796–798. doi: 10.3201/eid1905.121480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boumbanda Koyo CS, Amanzougaghene N, Davoust B, Tshilolo L, Lekana-Douki JB, Raoult D, et al. Genetic diversity of human head lice and molecular detection of associated bacterial pathogens in Democratic Republic of Congo. Parasit Vectors. 2019;12(1):290. doi: 10.1186/s13071-019-3540-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sunantaraporn S, Sanprasert V, Pengsakul T, Phumee A, Boonserm R, Tawatsin A, et al. Molecular survey of the head louse Pediculus humanus capitis in Thailand and its potential role for transmitting Acinetobacter spp. Parasit Vectors. 2015;8:127. doi: 10.1186/s13071-015-0742-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bouvresse S, Socolovshi C, Berdjane Z, Durand R, Izri A, Raoult D, et al. No evidence of Bartonella quintana but detection of Acinetobacter baumannii in head lice from elementary schoolchildren in Paris. Comp Immunol Microbiol Infect Dis. 2011;34(6):475–477. doi: 10.1016/j.cimid.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 31.Piarroux R, Abedi AA, Shako JC, Kebela B, Karhemere S, Diatta G, et al. Plague epidemics and lice, Democratic Republic of Congo. Emerg Infect Dis. 2013;19(3):505–506. doi: 10.3201/eid1903.121542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Angelakis E, Diatta G, Trape JF, Richet H, et al. Altitude-dependent Bartonella quintana Genotype C in Head Lice, Ethiopia. Emerg Infect Dis. 2011;17(12):2357–2359. doi: 10.3201/eid1712.110453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sangare AK, Boutellis A, Drali R, Socolovschi C, Barker SC, Diatta G, et al. Detection of Bartonella quintana in African body and head lice. Am J Trop Med Hyg. 2014;91(2):294–301. doi: 10.4269/ajtmh.13-0707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kempf M, Abdissa A, Diatta G, Trape JF, Angelakis E, Mediannikov O, et al. Detection of Acinetobacter baumannii in human head and body lice from Ethiopia and identification of new genotypes. IJID. 2012;16(9):e680–e683. doi: 10.1016/j.ijid.2012.05.1024. [DOI] [PubMed] [Google Scholar]
- 35.Ciervo A, Mancini F, di Bernardo F, Giammanco A, Vitale G, Dones P, et al. Louseborne relapsing fever in young migrants, Sicily, Italy, July-September 2015. Emerg Infect Dis. 2016;22(1):152–153. doi: 10.3201/eid2201.151580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldenberger D, Claas GJ, Bloch-Infanger C, Breidthardt T, Suter B, Martínez M, et al. Louse-borne relapsing fever (Borrelia recurrentis) in an Eritrean refugee arriving Switzerland, August 2015. Euro Surveill. 2015;20:32. [PubMed] [Google Scholar]
- 37.Hoch M, Wieser A, Loscher T, Margos G, Purner F, Zuhl J, et al. Louse-borne relapsing fever (Borrelia recurrentis) diagnosed in 15 refugees from northeast Africa: epidemiology and preventive control measures, Bavaria, Germany, July to October 2015. Euro Surveill. 2015;20:42. doi: 10.2807/1560-7917.ES.2015.20.42.30046. [DOI] [PubMed] [Google Scholar]
- 38.Hytönen J, Khawaja T, Grönroos JO, Jalava A, Meri S, Oksi J. Louse-borne relapsing fever in Finland in two asylum seekers from Somalia. APMIS. 2016;125:59–62. doi: 10.1111/apm.12635. [DOI] [PubMed] [Google Scholar]
- 39.Keller C, Zumblick M, Streubel K, Eickmann M, Muller D, Kerwat M, et al. Hemorrhagic diathesis in Borrelia recurrentis infection imported to Germany. Emerg Infect Dis. 2016;22(5):917–919. doi: 10.3201/eid2205.151557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lucchini A, Lipani F, Costa C, Scarvaglieri M, Balbiano R, Carosella S, et al. Louseborne relapsing fever among East African Refugees, Italy, 2015. Emerg Infect Dis. 2016;22(2):298–301. doi: 10.3201/eid2202.151768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilting KR, Stienstra Y, Sinha M, Braks M, Cornish D, Grundmann H. Louse-borne relapsing fever (Borrelia recurrentis) in asylum seekers from Eritrea, the Netherlands July 2015. Euro Surveill. 2015;20:30. doi: 10.2807/1560-7917.es2015.20.30.21196. [DOI] [PubMed] [Google Scholar]
- 42.Cutuli SL, De Pascale G, Spanu T, Dell'Anna AM, Bocci MG, Pallavicini F, et al. Lice, rodents, and many hopes: a rare disease in a young refugee. Crit Care. 2017;21:81. doi: 10.1186/s13054-017-1666-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bise G, Coninx R. Epidemic typhus in a prison in Burundi. Trans R Soc Trop Med Hyg. 1997;91(2):133–134. doi: 10.1016/s0035-9203(97)90198-x. [DOI] [PubMed] [Google Scholar]
- 44.Antinori S, Mediannikov O, Corbellino M, Raoult D. Louse-borne relapsing fever among East African refugees in Europe. Travel Med Infect Dis. 2016;14(2):110–114. doi: 10.1016/j.tmaid.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 45.Feldmeier H, Heukelbach J. Epidermal parasitic skin diseases: a neglected category of poverty-associated plagues. Bull Wrld Health Org. 2009;87(2):152–159. doi: 10.2471/BLT.07.047308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raoult D, Roux V, Ndihokubwayo JB, Bise G, Baudon D, Martet G, et al. Jail fever (epidemic typhus)—outbreak in Burundi. Emerg Infect Dis. 1997;3(3):357–360. doi: 10.3201/eid0303.970313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rydkina EB, Roux V, Gagua EM, Predtechenski AB, Tarasevich IV, Raoult D. Bartonella quintana in body lice collected from homeless persons in Russia. Emerg Infect Dis. 1999;5(1):176–178. doi: 10.3201/eid0501.990126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Louni M, Mana N, Bitam I, Dahmani M, Parola P, Fenollar F, et al. Body lice of homeless people reveal the presence of several emerging bacterial pathogens in northern Algeria. PLoS Negl Trop Dis. 2018;12(4):e0006397. doi: 10.1371/journal.pntd.0006397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Raoult D, Roux V. The body louse as a vector of reemerging human diseases. Clin Infect Dis. 1999;29:888–911. doi: 10.1086/520454. [DOI] [PubMed] [Google Scholar]
- 50.Bonilla DL, Cole-Porse C, Kjemtrup A, Osikowicz L, Kosoy M. Risk factors for Human Lice and Bartonellosis among the Homeless, San Francisco, California, USA. Emerg Infect Dis. 2014;20(10):1645–1651. doi: 10.3201/eid2010.131655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Niang M, Brouqui P, Raoult D. Epidemic typhus imported from Algeria. Emerg Infect Dis. 1999;5(5):716–718. doi: 10.3201/eid0505.990515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fang R, Houhamdi L, Raoult D. Detection of Rickettsia prowazekii in body lice and their feces by using monoclonal antibodies. J Clin Microbiol. 2002;40(9):3358–3363. doi: 10.1128/JCM.40.9.3358-3363.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Houhamdi L, Raoult D. Experimentally infected human body lice (pediculus humanus humanus) as vectors of Rickettsia rickettsii and Rickettsia conorii in a rabbit model. Am J Trop Med Hyg. 2006;74(4):521–525. [PubMed] [Google Scholar]
- 54.Houhamdi L, Fournier PE, Fang R, Raoult D. An experimental model of human body louse infection with Rickettsia typhi. Ann N Y Acad Sci. 2006;990:617–627. doi: 10.1111/j.1749-6632.2003.tb07436.x. [DOI] [PubMed] [Google Scholar]
- 55.Fournier PE, Minnick MF, Lepidi H, Salvo E, Raoult D. Experimental model of human body louse infection using green fluorescent protein-expressing Bartonella quintana. Infect Immun. 2001;69(3):1876–1879. doi: 10.1128/IAI.69.3.1876-1879.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sparrow H. Study of the Ethiopian source of recurrent fever. Bull World Health Organ. 1958;19(4):673–710. [PMC free article] [PubMed] [Google Scholar]
- 57.Houhamdi L, Raoult D. Excretion of living Borrelia recurrentis in feces of infected human body lice. J Infect Dis. 2005;191(11):1898–1906. doi: 10.1086/429920. [DOI] [PubMed] [Google Scholar]
- 58.Houhamdi L, Lepidi H, Drancourt M, Raoult D. Experimental model to evaluate the human body louse as a vector of plague. J Infect Dis. 2006;194(11):1589–1596. doi: 10.1086/508995. [DOI] [PubMed] [Google Scholar]
- 59.La Scola B, Raoult D. Acinetobacter baumannii in human body louse. Emerg Infect Dis. 2004;10:1671. doi: 10.3201/eid1009.040242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Houhamdi L, Raoult D. Experimental infection of human body lice with Acinetobacter baumannii. Am J Trop Med Hyg. 2006;74(4):526–531. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no data sets were generated or analyzed during the current study.