Abstract
Background:
Coronary angiography is currently the gold standard anatomic imaging method used to diagnose obstructive epicardial coronary artery disease. In patients with critical coronary stenosis, surgical or percutaneous revascularization is provided. Normal coronary artery ratio in coronary angiography is an indirect indicator of patient selection quality. The aim of our study is to evaluate the efficiency of coronary angiography by examining the revascularization rates according to years in patients who underwent coronary angiography.
Methods:
Revascularization rates will be determined by analyzing retrospectively the number of patients who underwent coronary angiography in our country between 2016 and 2021 and were revascularized interventionally or surgically. The number of patients who underwent percutaneous, surgical, and total revascularization were proportioned to the number of coronary angiography, and their percentages were determined.
Results:
From 2016 to 2019, there was a continuous increase in the number of coronary angiography. In 2020, the lowest coronary angiography numbers (n = 222.159) of the last 6 years were seen with the effect of the COVID-19 pandemic. In 2021, it was observed that the number of coronary angiography increased again with the relaxation of pandemic measures and the approaching of hospital admissions to old levels. It is seen that revascularization is performed in up to one-third of the patients who underwent coronary angiography.
Conclusion:
Similar to the rest of the world, revascularization rates as a result of coronary angiography procedures performed in our country are low. With this result, it should not be concluded that coronary angiography is not used effectively; on the contrary, the efficiency of coronary angiography can be increased by more effective use of noninvasive tests.
Keywords: Coronary artery bypass surgery, coronary artery disease, coronary computed tomographic angiography, percutaneous coronary intervention, coronary angiography
Highlights
Normal coronary artery ratio in coronary angiography (CAG) is an indirect indicator of patient selection quality.
Similar to the rest of the world, revascularization rates as a result of CAG procedures performed in our country are low.
Efficiency of CAG can be increased by more effective use of noninvasive tests.
Introduction
Coronary angiography (CAG) is currently the gold standard imaging method used to diagnose obstructive coronary artery disease (CAD). Approximately 4 million angiograms are performed each year in Europe and the United States (USA).1,2 Patients who have undergone CAG and have critical epicardial coronary artery stenosis can be revascularized with percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABG). However, the fact that CAG is invasive and carries some complication risks has increased the use of noninvasive imaging methods in detecting epicardial obstructive coronary stenosis, especially in patients with stable CAD. Coronary computed tomographic angiography (CCTA) is a diagnostic noninvasive anatomical imaging method that is increasingly used for this purpose. With CCTA, obstructive coronary stenosis defined by invasive CAG can be detected with a high accuracy.3
Numerous large-scale studies have shown the positive effects of both percutaneous and surgical revascularization on survival in patients with angiographically high-risk stable CAD.4,5 On the contrary, there are no randomized controlled studies showing the superiority of PCI over medical treatment in patients with stable CAD who do not have angiographic or clinical high-risk criteria.6,7 In the American College of Cardiology (ACC) Revascularization Guidelines published in 2021, revascularization is not recommended in order to increase survival in patients with stable CAD who do not have high-risk criteria.8 It is known that survival is improved with early revascularization in patients with acute coronary syndrome (ACS).9-11 The diagnosis of ACS is mostly made in emergency departments (ED). About 20 million patients present with symptoms possibly suggestive of ACS to ED in North America and Europe each year.12-14
In our study, the revascularization rates will be determined by analyzing the number of patients who underwent CAG in our country between 2016 and 2021 and were revascularized interventionally or surgically. Coronary angiography efficiency will be evaluated by comparing the obtained data with the existing literature data.
Methods
Our study is retrospective and descriptive. The data of patients who were admitted to the second- and third-level public health facilities emergency services and cardiology outpatient clinics in Türkiye between 2016 and 2021 and underwent CAG, PCI, and CABG were discussed. Selective CAG, coronary angioplasty and/or coronary stent, coronary artery bypass graft examination, and treatment codes were scanned in the system, and the number of patients was analyzed retrospectively according to years. All patients who underwent CAG for ACS and stable CAD were included in the study. The number of patients who underwent CAG, PCI, CABG, and total revascularization was determined according to years. The number of patients who underwent PCI, CABG, and total revascularization was proportioned to the number of CAG, and their percentages were determined.
The data were examined by obtaining the necessary permissions from the Ministry of Health. The study began after the Local Ethics Committee approval was obtained (number: E2-22-1882 and date 27.05.2022). Due to the nature of the study, consent was not obtained from the patients. Study was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki and its subsequent amendments.
Results
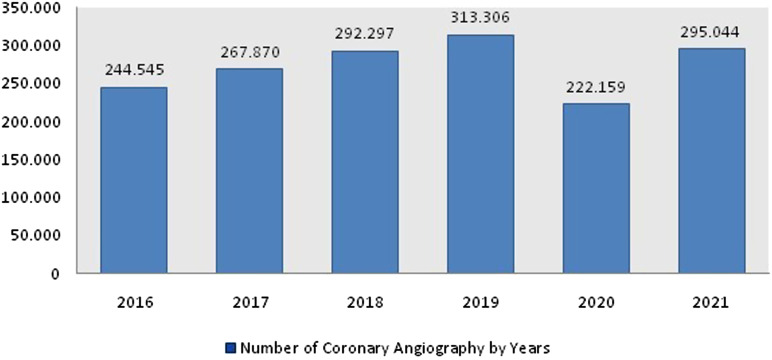
The number of CAG performed in our country by years is shown in Figure 1. From 2016 to 2019, there was a continuous increase in the number of CAG. In 2020, the lowest CAG numbers of the last 6 years were seen with the effect of the COVID-19 pandemic. In 2021, it was observed that the number of CAG increased again with the relaxation of pandemic measures and the approaching of hospital admissions to old levels.
Figure 1.
Number of coronary angiography by years.
The number of PCI, CABG, and total revascularization and their ratio to the total number of CAG are shown in Table 1. Although 2019 was the year with the highest number of CAG (n = 313.306), it was the year with the lowest PCI/CAG and total revascularization/CAG rates. The highest PCI/CAG and total revascularization/CAG rates were realized in 2017 with 36.2% and 37.16%, respectively. When the revascularization rates are evaluated according to the years, it is seen that revascularization is performed in up to one-third of the patients who underwent CAG.
Table 1.
The Number of Percutaneous Coronary Intervention, Bypass, and Total Revascularization by Years and Their Ratios to the Total Number of Coronary Angiography
| Years | PCI (n) | PCI/CAG Rate (%) | CABG (n) | CABG/CAG Rate (%) | Total Revascularization (n) | Total Revascularization/CAG Rate (%) |
|---|---|---|---|---|---|---|
| 2016 | 67.290 | 27.51 | 5.272 | 2.15 | 72.562 | 29.67 |
| 2017 | 96.988 | 36.2 | 2.567 | 0.95 | 99.555 | 37.16 |
| 2018 | 104.034 | 35.59 | 2.975 | 1.01 | 107.009 | 36.6 |
| 2019 | 73.731 | 23.5 | 13.241 | 4.22 | 86.972 | 27.75 |
| 2020 | 68.904 | 31.01 | 9.013 | 4.05 | 77.917 | 35.07 |
| 2021 | 88.362 | 29.94 | 13.927 | 4.72 | 102.289 | 34.66 |
CABG, coronary artery bypass graft; CAG, coronary angiography; PCI, percutaneous coronary intervention.
Discussion
Coronary angiography has an important role in the diagnosis of obstructive CAD. We can avoid both the risk of unnecessary complications and the cost of CAG by careful selection of patients who will undergo CAG.15,16 Normal coronary artery ratio in CAG is an indirect indicator of patient selection quality. In patients with a low probability of CAD, the normal coronary artery ratio increases with increased use of CAG.17 In our country, it was observed that the rate of revascularization was the lowest in 2019, the year in which the most CAG was performed. In the reports, it has been shown that the normal rate of coronary artery in the USA is 39%, and this rate increases up to 70% by varying between centers.2,18 In an another report published by Bredley et al19 in 2014, they reported that the normal coronary artery rate in the USA is approximately 20%. In the study published by Luciano et al.20 which included ACS excluding STEMI and examined a total of 737 CAG, no obstructive CAD was found in 41.2% of CAG. In a study by Patel et al.2 it was reported that critical coronary stenosis was detected in approximately one-third of CAG performed in the USA. Similarly, the rate of patients who were revascularized due to critical coronary stenosis in our study was approximately one-third.
The role of PCI on symptoms in patients with stable angina was investigated in the ORBITA trial. No additional benefit was observed in patients who underwent PCI.21 In a meta-analysis published in 2020, 14 877 patients were included in the analysis and compared medical treatment with routine revascularization in patients with stable CAD. It has been shown that routine revascularization does not affect survival.22 The ISCHEMIA trial compared the results of initial invasive or conservative treatment in patients with stable CAD and included 5179 patients. The included patients had moderate or severe ischemia and were followed for an average of 3.2 years. No difference was found between the two groups in ischemic cardiovascular events and deaths from any cause.6
Coronary computed tomographic angiography is an anatomical imaging modality that has become increasingly popular in recent years due to its noninvasive nature. Chow et al23 reported that the use of CCTA had a positive effect on CAG by reducing the ratio of normal coronary arteries. In a study published in 2021 evaluating the cost-effectiveness of CCTA and invasive CAG in diagnosing CAD, CAG was found to be more effective in patients with a high probability of CAD, while CCTA was found to be more effective in patients with a low and moderate probability of CAD.24 In a study published in 2012, the effect of medical treatment and revascularization on all-cause mortality was investigated in patients with no known CAD history and CAD detected by CCTA, the mortality benefit with revascularization was seen only in patients with high-risk CAD diagnosed through CCTA.25 In a study published in 2018 evaluating the effects of CCTA on the 5-year risk of MI, a decrease in deaths due to nonfatal MI and CAD was observed with CCTA, which is used in addition to standard tests.26 In a retrospective study of 1305 patients published by Birkl et al.27 CAG was performed on patients diagnosed with CAD by CCTA, and PCI was applied to 39.2% of them. It was found that CCTA was similarly beneficial in all risk groups. In the 2019 European Society of Cardiology, Chronic Coronary Syndrome Guideline, CCTA is recommended for the exclusion of CAD in low- and intermediate-risk patients.28
The revascularization rates between 2016 and 2021 in our country are examined, and the highest rate of revascularization/CAG was in 2017 with 37%. When the worldwide data are analyzed, the revascularization rates in patients undergoing CAG show great differences between countries and centers and vary between 20% and 70%. In addition, there are conflicting data in the literature regarding the benefit of routine revascularization, especially in patients with low- and intermediate-risk CAD. For these reasons, we think that noninvasive tests should be used more before deciding on invasive intervention, due to the low revascularization rates in the world and in our country, and the contradictory benefits of routine revascularization.
In our study, patients who underwent CAG for ACS were not examined as a separate group. Considering the proportions of patients who underwent CAG for myocardial infarction and were not found to have obstructive coronary artery stenosis (MINOCA), the revascularization/CAG ratios in patients who underwent elective CAG will further decrease with the exclusion of patients with ACS from the study. In the study published by Bainey et al.29 the rate of MINOCA was reported to be 5.8%. In the MINOCA-TR study published in 2020 based on data from our country, the rate of MINOCA was 6.7%.30
Study Limitations
The data in the study include public health facilities and does not include private hospital data. Private hospital data were not included in the study because they were not recorded regularly. In addition, patients who underwent intermittent and/or repeated revascularization could not be differentiated, but exclusion of these patients would further reduce the revascularization rate. Presence of patients who are accepted as inoperable in terms of revascularization, not being suitable for revascularization, or patients not wanting revascularization also may have decreased revascularization rate. The patient population includes both the ACS and stable angina groups. And also, among patients, there are those who underwent CAG due to incorrect elevation of troponin and those who underwent preoperative CAG for valve problems or other reasons. There is no data on how many of the procedures applied to these patients were after the emergency service admission and how many were after the outpatient clinic admission.
Conclusion
Revascularization rates as a result of CAG procedures performed in our country are similar to the rest of the world. The rate of patients with critical coronary stenosis and revascularization is an indication that we should use risk grading and noninvasive diagnostic tests more effectively. In this way, the number of unnecessary CAG and revascularization will be reduced, and the complication rates related to these procedures will decrease and the amount of radiation received by the healthcare staff will decrease. Ultimately, CAG efficiency will increase. Considering all these situations, it does not mean that CAG is not used effectively, it just emphasizes that noninvasive imaging methods should be used more effectively.
Footnotes
Ethics Committee Approval: The data were examined by obtaining the necessary permissions from the Ministry of Health. Ethics Committee Approval Number; E2-22-1882 and date 27.05.2022.
Informed Consent: Due to the nature of the study, consent was not obtained from the patients.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – Z.A, A.Y.K., Design – A.B, Z.A., Supervision – A.Y.K., Resources – A.Y.K., Materials – A.B., Data Collection and/or Processing – A.B., Z.A., A.Y.K., Analysis and/or Interpretation – A.B., Z.A., A.Y.K., Literature Search – Z.A., A.Y.K., Writing – Z.A., A.Y.K., Critical Review – A.Y.K.
Declaration of Interests: The authors have no conflict of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Cook S, Walker A, Hügli O, Togni M, Meier B. Percutaneous coronary interventions in Europe: prevalence, numerical estimates, and projections based on data up to 2004. Clin Res Cardiol. 2007;96(6):375 382. ( 10.1007/s00392-007-0513-0) [DOI] [PubMed] [Google Scholar]
- 2. Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886 895. ( 10.1056/NEJMoa0907272) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Knuuti J, Ballo H, Juarez-Orozco LE, et al. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: a meta-analysis focused on post-test disease probability. Eur Heart J. 2018;39:3322 3330. ( 10.1093/eurheartj/ehy267) [DOI] [PubMed] [Google Scholar]
- 4. Holmes DR, Davis KB, Mock MB, et al. The effect of medical and surgical treatment on subsequent sudden cardiac death in patients with coronary artery disease: a report from the coronary artery surgery study. Circulation. 1986;73(6):1254 1263. ( 10.1161/01.cir.73.6.1254) [DOI] [PubMed] [Google Scholar]
- 5. Mark DB, Nelson CL, Califf RM, et al. Continuing evolution of therapy for coronary artery disease. Initial results from the era of coronary angioplasty. Circulation. 1994;89(5):2015 2025. ( 10.1161/01.cir.89.5.2015) [DOI] [PubMed] [Google Scholar]
- 6. Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395 1407. ( 10.1056/NEJMoa1915922) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Katritsis DG, Ioannidis JPA. Percutaneous coronary intervention versus conservative therapy in non acute coronary artery disease: a meta-analysis. Circulation. 2005;111(22):2906 2912. ( 10.1161/CIRCULATIONAHA.104.521864) [DOI] [PubMed] [Google Scholar]
- 8. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in Circulation. 2022 Mar 15;145(11):e771]. Circulation. 2022;145(11):e771].35286170 [Google Scholar]
- 9. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13 20. ( 10.1016/S0140-6736(03)12113-7) [DOI] [PubMed] [Google Scholar]
- 10. Hochman JS, Sleeper LA, Webb JG, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK investigators. should we emergently revascularize occluded coronaries for cardiogenic shock. N Engl J Med. 1999;341(9):625 634. ( 10.1056/NEJM199908263410901) [DOI] [PubMed] [Google Scholar]
- 11. Qayyum R, Khalid MR, Adomaityte J, Papadakos SP, Messineo FC. Systematic review: comparing routine and selective invasive strategies for the acute coronary syndrome. Ann Intern Med. 2008;148(3):186 196. ( 10.7326/0003-4819-148-3-200802050-00005) [DOI] [PubMed] [Google Scholar]
- 12. Thygesen K, Mair J, Katus H, et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J. 2010;31(18):2197 2204. ( 10.1093/eurheartj/ehq251) [DOI] [PubMed] [Google Scholar]
- 13. Thygesen K, Mair J, Giannitsis E, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J. 2012;33(18):2252 2257. ( 10.1093/eurheartj/ehs154) [DOI] [PubMed] [Google Scholar]
- 14. Möckel M, Searle J, Hamm C, et al. Early discharge using single cardiac troponin and copeptin testing in patients with suspected acute coronary syndrome (ACS): a randomized, controlled clinical process study. Eur Heart J. 2015;36(6):369 376. ( 10.1093/eurheartj/ehu178) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/ AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2012;60:e44 e164. [DOI] [PubMed] [Google Scholar]
- 16. Patel MR, Bailey SR, Bonow RO, et al. ACCF/SCAI/AATS/AHA/ ASE/ASNC/HFSA/HRS/SCCM/SCCT/SCMR/STS 2012 appropriate use criteria for diagnostic catheterization: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2012;59:1995 2027. [DOI] [PubMed] [Google Scholar]
- 17. Bashore TM, Bates ER, Berger PB, et al. American College of Cardiology/Society for Cardiac Angiography and Interventions Clinical Expert Consensus Document on cardiac catheterization laboratory standards. A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001;37:2170 2144. [DOI] [PubMed] [Google Scholar]
- 18. Douglas PS, Patel MR, Bailey SR, et al. Hospital variability in the rate of finding obstructive coronary artery disease at elective, diagnostic coronary angiography. J Am Coll Cardiol. 2011;58(8):801 809. ( 10.1016/j.jacc.2011.05.019) [DOI] [PubMed] [Google Scholar]
- 19. Bradley SM, Maddox TM, Stanislawski MA, et al. Normal coronary rates for elective angiography in the Veterans Affairs healthcare system. J Am Coll Cardiol. 2014;63(5):417 426. ( 10.1016/j.jacc.2013.09.055) [DOI] [PubMed] [Google Scholar]
- 20. Luciano LSC, Silva RLD, Londero Filho OM, et al. Analysis of the appropriate use criteria for coronary angiography in two cardiology services of Southern Brazil. Arq Bras Cardiol. 2019;112(5):526 531. ( 10.5935/abc.20190055) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018;391(10115):31 40. ( 10.1016/S0140-6736(17)32714-9) [DOI] [PubMed] [Google Scholar]
- 22. Bangalore S, Maron DJ, Stone GW, Hochman JS. Routine revascularization versus initial medical therapy for stable ischemic heart disease: a Systematic Review and Meta-Analysis of Randomized Trials. Circulation. 2020;142(9):841 857. ( 10.1161/CIRCULATIONAHA.120.048194) [DOI] [PubMed] [Google Scholar]
- 23. Chow BJW, Abraham A, Wells GA, et al. Diagnostic accuracy and impact of computed tomographic coronary angiography on utilization of invasive coronary angiography. Circ Cardiovasc Imaging. 2009;2(1):16 23. ( 10.1161/CIRCIMAGING.108.792572) [DOI] [PubMed] [Google Scholar]
- 24. Mansour HH, Alajerami YS. Cost-effectiveness analysis of coronary computed tomography angiography and invasive coronary angiography for diagnosis of coronary artery disease. J Cardiovasc Dis Res. 2021;12(3):1440-1453. [Google Scholar]
- 25. Min JK, Berman DS, Dunning A, et al. All-cause mortality benefit of coronary revascularization vs. medical therapy in patients without known coronary artery disease undergoing coronary computed tomographic angiography: results from CONFIRM (COronary CT Angiography EvaluatioN ForClinical Outcomes: an InteRnational Multicenter Registry). Eur Heart J. 2012;33:3088 3097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. SCOT-HEART Investigators, Newby DE, Adamson PD, et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med. 2018;379(10):924 933. ( 10.1056/NEJMoa1805971) [DOI] [PubMed] [Google Scholar]
- 27. Birkl K, Beyer C, Plank F, Feuchtner GM, Friedrich G. Evaluation of the appropriate use of coronary computed tomography angiography: a retrospective, single-center analysis. J Cardiovasc Dev Dis. 2022;9(6):180. ( 10.3390/jcdd9060180) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41(3):407 477. ( 10.1093/eurheartj/ehz425) [DOI] [PubMed] [Google Scholar]
- 29. Bainey KR, Welsh RC, Alemayehu W, et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA): insights from the Alberta contemporary acute coronary syndrome patients invasive treatment strategies (COAPT) study. Int J Cardiol. 2018;264:12 17. ( 10.1016/j.ijcard.2018.04.004) [DOI] [PubMed] [Google Scholar]
- 30. Kilic S, Aydın G, Çoner A, et al. Prevalence and clinical profile of patients with myocardial infarction with non- obstructive coronary arteries in Turkey (MINOCA-TR): A national multi-center, observational study. Anatol J Cardiol. 2020;23(3):176 182. ( 10.14744/AnatolJCardiol.2019.46805) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a