Abstract
Background:
Underscreened, low-income, and uninsured or publicly insured women in the United States bear a greater burden of cervical cancer morbidity and mortality and may face unique barriers that preclude screening adherence.
Methods:
Participants were 710 My Body My Test-3 clinical trial participants who were publicly insured or uninsured with incomes ≤250% of the U.S. Federal Poverty Level, aged 25–64 years, and not up to date on cervical cancer screening as per national guidelines. Using Health Belief Model constructs, we assessed screening-related knowledge, perceptions, and behaviors—overall and stratified by race and ethnicity—and estimated associations with past-year attempted screening using multivariable regression models.
Results:
Overall, knowledge was low about the human papillomavirus, purpose of a Pap test, and recommended screening interval. Perceived severity of cervical cancer was high (3.63 on a 4-point scale). Black and Latina/Hispanic women were more likely to perceive screening as lowering their risk of cervical cancer than White women. Black women reported lower perceived risk of cervical cancer compared with White women (p = 0.03), but Black women were more likely to have sought screening in the past year (p = 0.01). Having at least three doctor visits in the past year was associated with a screening attempt. Greater perceived risk of cervical cancer, more positive perceptions of screening, and feeling more nervousness about screening were also associated with a screening attempt (all p < 0.05).
Conclusions:
Addressing knowledge gaps and misconceptions about cervical cancer screening and leveraging positive perceptions of screening may improve screening uptake and adherence among diverse underscreened U.S. women. Clinical Trial Registration Number: NCT02651883.
Keywords: cancer screening, cervical cancer, Health Belief Model, health disparities, human papillomavirus, under-screened populations
Introduction
Invasive cervical cancer (ICC) is a highly preventable disease through population-based screening and vaccination against oncogenic human papillomavirus (HPV).1 However, ICC morbidity and mortality persist in the United States, with poor, uninsured, and Black, indigenous, and people of color (BIPOC) bearing a greater burden of disease.2–4 Poor access to and uptake of screening contributes to ICC burden, with over 50% of cases occurring among women with insufficient screening.5
Approximately 15% of eligible U.S. women are not up to date with cervical cancer screening.6 Low-income and uninsured women are more likely to be underscreened or never screened, placing them at greater risk for cervical precancerous lesions to go undetected and progress to malignancy.7–9 Understanding reasons for screening nonadherence among underscreened women is critical to inform interventions to improve regular participation in screening.
An individual's knowledge, perceptions, and beliefs about cervical cancer and related screening practices may influence screening participation. According to the Health Belief Model (HBM), health-seeking behaviors—such as participation in screening—are influenced by perceptions about disease severity and their personal susceptibility to disease, the perceived benefits of and barriers to engaging in protective action, their self-efficacy to take action, and cues to action.10
Perceptions about a disease and related health behaviors are affected by demographic and other contextual variables. For example, the social constructs of race and ethnicity can shape cultural beliefs about health and illness, personal experiences within the health care system, and an individual's ability to access health-related resources. Namely, structural racism in the United States has led to the historic exclusion of BIPOC individuals from the health care system, which may drive many observed racial differences in health care utilization, health literacy, and health outcomes.11,12
To our knowledge, no studies have systematically quantified the utility of HBM constructs to explain cervical cancer screening knowledge, perceptions, and beliefs among underscreened, uninsured, or Medicaid-insured women in the United States. Prior studies evaluating HBM constructs among underserved cervical cancer screening populations generally utilized small samples and were restricted to homogeneous social groups or specific settings.
Moreover, recent systematic reviews highlight a gap in knowledge concerning screening-related perceptions and beliefs when comparing different racial and ethnic groups.13,14 Studies that have included multiple racial and ethnic groups have been qualitative focus group assessments of health beliefs.15,16 Finally, many screening studies have recruited participants through health clinics, a strategy that excludes those without regular health care. Research that includes large diverse groups of women who are not typically represented in cervical cancer screening studies is needed to better understand their health beliefs and behaviors.
This study aims to describe relationships between race and ethnicity and cervical cancer screening knowledge, perceptions, and beliefs among participants in the My Body My Test-3 (MBMT-3) trial. Using the HBM framework, we compare HBM domains—such as perceived susceptibility to disease, perceived severity of disease, perceived benefits and barriers to action, and self-efficacy—among participants of different races and ethnicities and report predictors of attempting to receive cervical cancer screening in the past year.
MBMT-3 recruited exclusively low-income and uninsured or Medicaid-insured women overdue for cervical cancer screening. Thus, this study addresses key gaps in the current literature on cervical cancer screening uptake and adherence in medically underserved populations.
Materials and Methods
Study population
The MBMT-3 trial was a two-arm, randomized clinical trial examining the effect of mailed HPV self-collection kits on cervical cancer screening uptake among low-income, underscreened women. Participants were recruited between April 2016 and December 2019. Participants were between age 25 and 64, as the FDA approved HPV testing for primary screening of women aged 25 or older, and uninsured women up to age 64 may be covered by Medicaid or the North Carolina Breast and Cervical Cancer Control Program (NC BCCCP).17
Additionally, individuals were study eligible if they were not pregnant, had an intact cervix (no history of hysterectomy), had income ≤250% of the U.S. Federal Poverty Level (FPL), were uninsured or enrolled in Medicaid/Medicare, and were living within the catchment area of a study-associated clinic (covering 22 North Carolina counties). Women were eligible only if they self-reported not having a Pap test in 4 years or more and not having an HPV test in 6 years or more, which is considered overdue for screening as per national guidelines (U.S. Preventive Services Task Force, 2018).18
Recruitment methods utilized printed materials (i.e., flyers and posters), online sources (Facebook and Craigslist), radio advertisements, the United Way 2-1-1 social assistance helpline, community events, and outreach through community organizations.19 Eligible women received and returned informed consent forms via mail. Eligibility and baseline questionnaires were administered verbally in English or Spanish by interviewers either in person or by phone. Approval for this study was granted by the University of North Carolina Institutional Review Board.
Measures
Data were drawn from the eligibility screener and baseline questionnaire administered as part of the MBMT-3 trial. The eligibility screener included sociodemographic characteristics (i.e., race, ethnicity, education, income, and insurance status). Eligible participants then completed the baseline questionnaire, which assessed barriers, knowledge, health-seeking behaviors, and attitudes related to cervical cancer and screening. The questionnaire items are shown in Supplementary Table S1.
Awareness of HPV, HPV/Pap cotesting, and clinics that offer low-cost screening was assessed via yes/no questions and categorized as “aware” or “not aware.” Knowledge about HPV and cervical cancer was assessed through a series of yes/no questions, categorized as correct or incorrect; responses of “Don't know” or “Refused” were coded as incorrect. To categorize open-ended responses to the question “As far as you know, what is a Pap smear for?” two study team members developed and applied a standardized coding scheme.
Perceptions of cervical cancer and screening were evaluated with a series of statements to which participants indicated their agreement on four-level scales (i.e., strongly agree, somewhat agree, somewhat disagree, or strongly disagree). Perception items were considered for inclusion in summary scales determined via exploratory factor analysis (EFA). Mean values were used to impute missing items.
Eigen analysis was used to identify factors for inclusion in the EFA, which was performed using the principal axis factoring method with oblique rotation.20 Items with a maximum loading <0.3 were dropped from consideration, and EFA was repeated until all maximum loadings were ≥0.3. Scales identified in the EFA were further assessed with Cronbach's alpha; scales with alpha <0.6 were excluded from consideration.
Race and ethnicity were ascertained by participant responses to two questionnaire items. First, “Are you Latina or Hispanic?” included “yes,” “no,” “refused,” or “don't know” responses. Second, “What is your race or ethnicity?” included a “mark all that apply” response with the following options: “Black or African American,” “White,” “American Indian or Alaska Native,” “Asian,” “Native Hawaiian or Pacific Islander,” “Hispanic/Latina,” “Refused,” “Don't know,” or “Other.” An open-ended textbox was used to record a response other than those listed.
We conceptualized race and ethnicity as social constructs that impact an individuals' perceptions, experiences of discrimination, access to resources, and relationship with the health care system and, ultimately, their health outcomes.11,21
Analytic sample
Of 4256 women who volunteered to participate in the study, 2770 (65%) did not meet inclusion criteria and 587 (14%) did not fully complete eligibility screening, resulting in 899 study-eligible women. Of these, 791 (88%) completed the baseline survey, of which 32 (4%) were excluded after being found screening ineligible postrandomization (n = 24) or due to the trial being stopped due to the COVID-19 pandemic (n = 8).
Thus, 759 women were eligible for baseline analyses. Of these, 49 self-identified as a race or ethnicity other than White, Black, or Hispanic or Latina, as multiple or mixed race, or did not self-identify any race or ethnicity; these participants were excluded from analyses due to small numbers for these categories, leaving a final analytic sample of 710.
Statistical analyses
For awareness and knowledge items, the percent “aware” or “correct” were reported overall and stratified by race and ethnicity (White non-Latina/Hispanic, Black non-Latina/Hispanic, and Latina/Hispanic). Logistic regression was used to compare the likelihood of being “aware” or “correct” for Black versus White and Latina/Hispanic versus White participants.
For perception and behavior items with 4-point response scales, responses were transformed as necessary; 1 indicated a low level of agreement/severity and 4 indicated a high level of agreement/severity. Mean and standard deviation of responses were estimated overall and by race and ethnicity. Differences in perceptions by race and ethnicity were assessed with linear regression, using White as the reference. The percentage of participants reporting any attempt to receive screening in the past year was estimated overall and by race and ethnicity, and differences between groups were assessed using logistic regression.
Odds ratios (ORs) and 95% confidence intervals (CIs) describing bivariate associations between sociodemographic characteristics and past-year screening attempts were estimated using logistic regression. Similarly, associations between awareness, knowledge, and perception scales and participant past-year screening attempts were assessed using unadjusted and adjusted logistic regression models. Sociodemographic factors associated with screening attempt at the alpha = 0.05 level were included in adjusted regression models.
All statistical analyses were conducted using R, version 4.0.1 (Vienna, Austria).
Results
Study population characteristics
Among the 710 participants, 287 (40%) identified as White non-Latina/Hispanic, 356 (50%) as Black non-Latina/Hispanic, and 67 (9%) as Latina or Hispanic. Most participants (79%) were uninsured and 21% were publicly insured. Forty-three percent completed a high school-level education or less. The majority (91%) lived in urban counties.
Awareness and knowledge
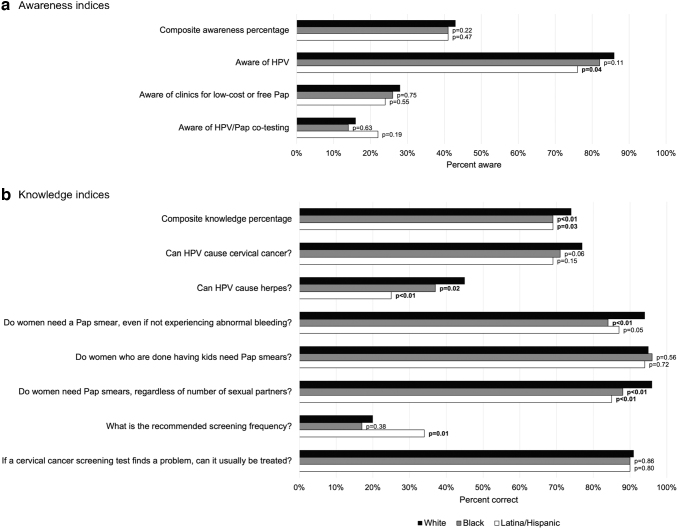
While there was overall a high proportion of participants who had heard of HPV (83% “aware”), there was relatively low awareness of HPV/Pap cotesting (16% aware) and of clinics that offer low-cost or free Pap testing (27% aware) (Fig. 1). Latina/Hispanic participants were less likely than White participants to be aware of HPV (86% vs. 76%, p = 0.04); however, awareness was comparable between groups for the other awareness items.
FIG. 1.
Cervical cancer screening awareness and knowledge (a) among 710 MBMT-3 participants, stratified by race and ethnicity (b). Bold p-values indicate p < 0.05 for comparison with White participants (reference). (a) See Supplementary Table S1 for details on questionnaire questions and responses. (b) Sample restricted to MBMT-3 participants who self-identified as White or Black or Latina/Hispanic (n = 47 participants were excluded due to missing race/ethnicity or a self-identification other than White, Black, or Latina/Hispanic). Race/ethnicity based on participant responses to “What is your race or ethnicity?” and “Are you Latina or Hispanic?” MBMT-3, My Body My Test-3.
Overall knowledge of HPV, Pap tests, and screening recommendations was higher among White (74% correct) compared with Black (69% correct, p < 0.01) and Latina/Hispanic (69% correct, p = 0.03) participants (Fig. 1). Participants exhibited the lowest knowledge of recommended screening frequency (20% correct) and whether HPV can cause herpes (39% correct).
Compared with White participants, Black and Latina/Hispanic participants were each less likely to know that HPV could not cause herpes (Black vs. White: 37% vs. 45% correct, p = 0.02; and Latina/Hispanic vs. White: 25% vs. 45% correct, p < 0.01) and that women need Pap tests regardless of the number of sexual partners (Black vs. White: 88% vs. 96% correct, p < 0.01; and Latina/Hispanic vs. White: 85% vs. 96% correct, p < 0.01).
Black participants were less likely to know that a woman needs a Pap test even in the absence of abnormal bleeding (Black vs. White: 84% vs. 94% correct, p < 0.01). Latina/Hispanic women were more likely to correctly identify the appropriate screening frequency (Latina/Hispanic vs. White: 34% vs. 20% correct, p = 0.01).
When asked “What is the purpose of a Pap smear?” 27% of participants responded that it is to check for cervical cancer, although 46% knew that it was to check for cancer more generally (Table 1). Black and Latina/Hispanic participants were less likely than White participants to respond that a Pap test was to “check for cancer” (both p < 0.01) and were more likely to respond that it was to “check reproductive system health” (p < 0.01 and p = 0.02, respectively).
Table 1.
Responses to “What is the purpose of a Pap smear?” Among 710 My Body My Test-3 Participants, Overall and by Participant Race and Ethnicity
| Overall n (%) | White non-Latina/Hispanic n (%) | Black non-Latina/Hispanic n (%) | Latina/Hispanic n (%) | p-Value (Black vs. White)a | p-Value (Latina/Hispanic vs. White)b | |
|---|---|---|---|---|---|---|
| Total unique responsesc | 935 | 380 | 472 | 83 | ||
| Check for cancer | 426 (45.6) | 216 (56.8) | 179 (37.9) | 31 (37.3) | <0.01 | <0.01 |
| Check for cervical cancer | 254 (27.2) | 133 (35.0) | 107 (22.7) | 14 (16.7) | ||
| Check for cancer (general) | 150 (16.0) | 77 (20.3) | 58 (12.3) | 15 (18.1) | ||
| Check for vaginal cancer | 17 (1.8) | 3 (0.8) | 13 (2.8) | 1 (1.2) | ||
| Check for uterine cancer | 11 (1.2) | 5 (1.3) | 4 (0.8) | 2 (2.4) | ||
| Check for ovarian cancer | 3 (0.3) | 0 (0.0) | 3 (0.6) | 0 (0.0) | ||
| Check for infections/STDs | 137 (14.7) | 54 (14.2) | 68 (14.4) | 15 (18.1) | 0.74 | 0.32 |
| Check for STDs | 93 (9.9) | 36 (9.5) | 49 (10.4) | 8 (9.6) | ||
| Check for infections (general) | 34 (3.6) | 12 (3.2) | 17 (3.6) | 5 (6.0) | ||
| Check for HPV | 11 (1.2) | 5 (1.3) | 6 (1.3) | 0 (0.0) | ||
| Check for yeast infections | 4 (0.4) | 2 (0.5) | 2 (0.4) | 0 (0.0) | ||
| Prevent infections/STDs | 3 (0.3) | 1 (0.3) | 0 (0.0) | 2 (2.4) | ||
| Check for HIV | 2 (0.2) | 1 (0.3) | 0 (0.0) | 1 (1.2) | ||
| Check reproductive system health | 204 (21.8) | 58 (15.3) | 125 (26.4) | 21 (25.3) | <0.01 | 0.02 |
| Check reproductive organs (general) | 92 (9.8) | 37 (9.7) | 49 (10.3) | 6 (7.2) | ||
| Check the vagina | 69 (7.4) | 9 (2.4) | 51 (10.8) | 9 (10.8) | ||
| Check the cervix | 40 (4.3) | 12 (3.2) | 24 (5.1) | 4 (4.8) | ||
| Check the uterus | 16 (1.7) | 4 (1.1) | 9 (1.9) | 3 (3.6) | ||
| Check general health | 101 (10.8) | 39 (10.3) | 51 (10.8) | 11 (13.3) | 0.64 | 0.38 |
| Other response | 4 (0.4) | 0 (0.0) | 4 (0.8) | 0 (0.0) | ||
| Check the anus | 1 (0.1) | 0 (0.0) | 1 (0.2) | 0 (0.0) | ||
| Check for pregnancy | 1 (0.1) | 0 (0.0) | 1 (0.2) | 0 (0.0) | ||
| Check for virginity | 1 (0.1) | 0 (0.0) | 1 (0.2) | 0 (0.0) | ||
| Don't know | 20 (2.1) | 4 (1.1) | 15 (3.2) | 1 (1.2) |
Bold p-values indicate p < 0.05.
Sample restricted to MBMT-3 participants who self-identified as White or Black or Latina/Hispanic (n = 47 participants were excluded due to missing race and ethnicity or a self-identification as other than White, Black, or Latina/Hispanic). White or Black identification based on participant response to the multiple-choice question: “What is your race or ethnicity?” Latina/Hispanic identification based on participant response to the question: “Are you Latina or Hispanic?”
p-Value comparing responses among Black versus White participants (reference), using logistic regression.
p-Value comparing responses among Latina/Hispanic versus White participants (reference), using logistic regression.
Participants' open-ended responses to the question “What is the purpose of a Pap smear?” were transcribed directly by interviewers. Open-ended text responses were then coded by two independent study team members into the categories displayed. Responses may be included in more than one category, so the total number of unique responses (n = 935) is larger than the total number of participants.
HPV, human papillomavirus; MBMT-3, My Body My Test-3.
Perceptions and behaviors
Overall, there was a high perceived severity of cervical cancer (mean response 3.63 on a 4-point scale) and high anticipated regret of not getting screened if an abnormality was found in the future (mean response 3.63 on a 4-point scale) (Table 2). Black participants had a relatively lower perceived personal risk of cervical cancer compared with White participants (2.58 vs. 2.71, p = 0.03).
Table 2.
Cervical Cancer Screening Perceptions and Behaviors Among 710 My Body My Test-3 Participants, Overall and by Race and Ethnicity
| Overall (N = 710) | White non-Latina/Hispanic (n = 287) | Black non-Latina/Hispanic (n = 356) | Latina/Hispanic (n = 67) | p-Value (Black vs. White) | p-Value (Latina/Hispanic vs. White) | |
|---|---|---|---|---|---|---|
| Risk appraisal | Mean [1 (low)–4 (high)] (SD) | |||||
| Perceived risk of cervical cancer (3-item scale)a | 2.63 (0.72) | 2.71 (0.66) | 2.58 (0.76) | 2.62 (0.78) | 0.03 | 0.36 |
| Embodiment of risk (2-item scale)b | 2.47 (0.97) | 2.36 (0.91) | 2.54 (1.01) | 2.62 (0.97) | 0.02 | 0.04 |
| Perceived severity of cervical cancer | 3.63 (0.73) | 3.64 (0.69) | 3.60 (0.78) | 3.74 (0.61) | 0.49 | 0.32 |
| Anticipated regret of getting screened if the test ended up being painful | 1.56 (0.89) | 1.45 (0.80) | 1.60 (0.92) | 1.79 (1.02) | 0.03 | <0.01 |
| Anticipated regret of not getting screened if an abnormality was found in the future | 3.63 (0.87) | 3.65 (0.85) | 3.58 (0.93) | 3.87 (0.49) | 0.30 | 0.06 |
| Belief that she personally needs a Pap test even if she takes good care of herself | 3.33 (0.99) | 3.42 (0.92) | 3.29 (1.03) | 3.16 (1.10) | 0.11 | 0.06 |
| Belief that there is little a person can do to reduce her risk of cervical cancer | 1.89 (1.02) | 1.83 (0.94) | 1.90 (1.08) | 2.08 (1.08) | 0.40 | 0.07 |
| Would rather not know if she had cervical cancer | 1.31 (0.80) | 1.31 (0.76) | 1.29 (0.79) | 1.45 (0.96) | 0.87 | 0.19 |
| Screening perceptions | ||||||
| Positive perceptions of screening (3-item scale)c | 3.74 (0.42) | 3.76 (0.34) | 3.73 (0.47) | 3.71 (0.43) | 0.41 | 0.43 |
| Negative perceptions of screening (2-item scale)d | 2.77 (0.86) | 2.70 (0.83) | 2.89 (0.87) | 2.44 (0.91) | <0.01 | 0.03 |
| Perceived effectiveness of screening in lowering chances of getting cervical cancer | 2.91 (1.20) | 2.72 (1.24) | 2.99 (1.18) | 3.25 (1.05) | <0.01 | <0.01 |
| How nervous does screening make you feel?e | 1.88 (0.69) | 1.86 (0.66) | 1.85 (0.71) | 2.06 (0.74) | 0.81 | 0.04 |
| Stigma | ||||||
| Belief that if she had cervical cancer, people would think she slept around | 1.47 (0.94) | 1.36 (0.80) | 1.52 (1.01) | 1.66 (1.08) | 0.03 | 0.02 |
| Screening intent | ||||||
| Has thought about getting a Pap test in the past year | 2.74 (1.08) | 2.63 (1.01) | 2.82 (1.12) | 2.75 (1.08) | 0.03 | 0.44 |
| Competing health priorities are keeping her from getting screened right now | 2.37 (1.17) | 2.51 (1.16) | 2.25 (1.17) | 2.43 (1.20) | <0.01 | 0.61 |
| Confidence in her ability to get screening if she wants | 2.99 (1.14) | 3.02 (1.09) | 2.95 (1.17) | 3.04 (1.21) | 0.45 | 0.86 |
| Seeking screening | N (%) yes | |||||
| Has tried to get screening in the past year | 132 (19) | 40 (14) | 79 (22) | 13 (19) | 0.01 | 0.26 |
Bold p-values indicate p < 0.05.
Based on responses to the following questions: What is your race or ethnicity? Are you Latina or Hispanic?
Perceived risk (three-item scale): (1) worry about getting cervical cancer, (2) chance of getting cervical cancer without regular screening, and (3) agreement/disagreement with the statement “I have almost no chance of getting cervical cancer.” Greater worry, higher perceived likelihood, and disagreement with the statement indicate higher perceived risk. All scales identified via exploratory factor analysis and confirmed with Cronbach's alpha ≥0.6.
Embodiment of risk (two-item scale): agreement/disagreement with statements (1) “I can sense if my cervix is healthy” and (2) “I can sense if there is something wrong with my cervix.” Agreement indicates higher embodiment of risk.
Positive screening perceptions (three-item scale): agreement/disagreement with statements (1) “The responsible thing to do is get regular screening,” (2) “It is important to get regular cervical cancer screening,” and (3) “I trust Pap smears to give accurate information about my health.”
Negative screening perceptions (2-item scale): agreement/disagreement with statements (1) “Cervical cancer screening is physically uncomfortable” and (2) “Cervical cancer screening is embarrassing.”
Responses collected on a 3-point scale: 1 (not nervous), 2 (somewhat nervous), or 3 (very nervous).
Both Black and Latina/Hispanic participants had a higher embodiment of risk compared with White participants (2.54 vs. 2.36, p = 0.02, and 2.62 vs. 2.36, p = 0.04, respectively); in other words, they were more likely to indicate that they could “sense whether something was wrong with their cervix.” Additionally, there was higher anticipated regret of getting screened if the test ended up being painful among both Black and Latina/Hispanic participants (Black vs. White: 1.60 vs. 1.45, p = 0.03; and Latina/Hispanic vs. White: 1.79 vs. 1.45, p < 0.01).
Black participants had more negative perceptions of cancer screening—perceiving screening to be physically uncomfortable or embarrassing—compared with White participants (2.89 vs. 2.70, p < 0.01); Latina/Hispanic participants had less negative perceptions (2.44 vs. 2.70, p = 0.03). Both Black and Latina/Hispanic participants reported higher perceived effectiveness of screening compared with White participants (Black vs. White: 2.99 vs. 2.72, p < 0.01; and Latina/Hispanic vs. White: 3.25 vs. 2.72, p < 0.01). Latina/Hispanic participants reported higher degrees of nervousness when thinking about screening, compared with White participants (2.06 vs. 1.86, p = 0.04).
Both Black and Latina/Hispanic participants were more likely than White participants to believe that if they had cervical cancer, “people would think they slept around” (1.52 vs. 1.36, p = 0.03, and 1.66 vs. 1.36, p = 0.02, respectively). All groups reported similarly high self-efficacy to receive screening, ascertained by asking women how much they agreed with the statement: “I am sure I can get cervical cancer screening if I want to” (3.02, 2.95, and 3.04 for White, Black, and Latina/Hispanic participants, respectively).
Predictors of attempts to receive screening
A notably low percentage (19%, n = 132) reported that they attempted to receive cervical cancer screening in the past year (Table 3). Black participants were more likely than White participants to have a past-year screening attempt (OR: 1.76; 95% CI: 1.16–2.67). Those who attended three or more doctor visits in the past year were more likely to have attempted to receive screening (OR: 2.33; 95% CI: 1.43–3.81) versus those who never saw a doctor. No other associations were observed between sociodemographic characteristics and screening attempt.
Table 3.
Sociodemographic Predictors of 710 My Body My Test-3 Participants' Reported Attempts to Receive Cervical Cancer Screening in the Past Year
| Characteristic | Overall na | Sought screening in the past yearb n (%) yes | Bivariate OR (95% CI) |
|---|---|---|---|
| N (%) | 710 | 132 (19) | |
| Age (years) | |||
| 25–34 | 227 | 44 (19) | 1. |
| 35–49 | 279 | 52 (19) | 0.95 (0.61–1.49) |
| 50–65 | 204 | 36 (18) | 0.89 (0.55–1.45) |
| Race/ethnicityc | |||
| White non-Latina/Hispanic | 287 | 40 (14) | 1. |
| Black non-Latina/Hispanic | 356 | 79 (22) | 1.76 (1.16–2.67) |
| Latina/Hispanic | 67 | 13 (19) | 1.49 (0.74–2.97) |
| Annual household income | |||
| $0–$9999 | 237 | 52 (22) | 1. |
| $10,000–$24,999 | 254 | 49 (19) | 0.85 (0.55–1.32) |
| ≥$25,000 | 175 | 26 (15) | 0.62 (0.37–1.04) |
| Health insurance | |||
| Uninsured | 559 | 99 (18) | 1. |
| Publicly insured | 149 | 33 (22) | 1.32 (0.85–2.06) |
| Number of doctor visits in the past year | |||
| None | 223 | 28 (12.6) | 1. |
| 1–2 | 244 | 43 (17.6) | 1.49 (0.89–2.49) |
| 3 or more | 243 | 61 (25.1) | 2.33 (1.43–3.81) |
| Receipt of social assistanced | |||
| No | 371 | 64 (17) | 1. |
| Yes | 331 | 67 (20) | 1.22 (0.83–1.78) |
| Education | |||
| High school, GED, or less | 305 | 57 (19) | 1. |
| Some college or more | 405 | 75 (19) | 0.99 (0.68–1.45) |
| Primary language | |||
| English | 665 | 121 (18) | 1. |
| Non-English | 38 | 11 (29) | 1.83 (0.88–3.79) |
| Sexual orientation | |||
| Heterosexual or straight | 645 | 121 (19) | 1. |
| Lesbian, gay, bisexual, or other | 59 | 11 (19) | 0.99 (0.50–1.97) |
| Marital status | |||
| Single or never married | 367 | 70 (19) | 1. |
| Married or living with partner | 145 | 26 (18) | 0.93 (0.56–1.53) |
| Divorced, separated, or widowed | 190 | 36 (19) | 0.99 (0.63–1.55) |
| Number of children | |||
| None | 183 | 34 (19) | 1. |
| 1–3 | 416 | 77 (19) | 1.00 (0.64–1.56) |
| 4+ | 104 | 21 (20) | 1.11 (0.60–2.03) |
| Ruralitye | |||
| Urban | 645 | 118 (18) | 1. |
| Rural | 65 | 14 (22) | 1.23 (0.66–2.29) |
Bold values indicate a 95% CI that does not cross the null.
Totals may not add up to overall sample size due to missing values: household income (n = 44), insurance status (n = 2), social assistance (n = 8), primary language (n = 7), sexual orientation (n = 6), marital status (n = 8), and number of children (n = 7).
Ascertained via participant response to the question “In the past year, have you tried to get a Pap smear?”
White or Black identification based on participant response to the multiple-choice question: “What is your race or ethnicity?” Latina/Hispanic identification based on participant response to the question: “Are you Latina or Hispanic?”
Includes food stamps, housing assistance, welfare payments, social security, supplemental security income (SSI), or disability.
Assigned based on the home county of each participant; counties were categorized as rural or urban based on RUCA codes.
CI, confidence interval; OR, odds ratio; RUCA, Rural–Urban Commuting Area.
Participants who reported a higher perceived risk of cervical cancer were more likely to report a past-year screening attempt (OR: 1.58 per one-unit increase in perceived risk scale; 95% CI: 1.20–2.07) (Table 4). This association remained after adjustment for race and ethnicity and number of past-year doctor visits (adjusted OR [aOR]: 1.63; 95% CI: 1.24–2.13).
Table 4.
Associations Between Cervical Cancer Screening Awareness, Knowledge, and Perceptions and Attempts to Receive Screening in the Past Year Among 710 My Body My Test-3 Participants
| Sought screening in past yeara |
|
|||
|---|---|---|---|---|
| Crude OR (95% CI)b | p | Adjusted OR (95% CI)c | p | |
| Awareness | ||||
| Awareness of HPV and cervical cancer (3-item index)d | 2.09 (0.98–4.46) | 0.06 | 2.12 (0.99–4.56) | 0.05 |
| Knowledge | ||||
| Knowledge about HPV and cervical cancer screening (7-item index)e | 1.85 (0.56–6.05) | 0.31 | 2.25 (0.67–7.61) | 0.19 |
| Risk appraisal | ||||
| Perceived risk of cervical cancer (3-item scale)f | 1.58 (1.20–2.07) | <0.01 | 1.63 (1.24–2.13) | <0.01 |
| Embodiment of risk (2-item scale)f | 1.05 (0.87–1.28) | 0.60 | 1.03 (0.85–1.26) | 0.74 |
| Perceived severity of cervical cancer | 1.16 (0.88–1.54) | 0.29 | 1.17 (0.88–1.55) | 0.27 |
| Anticipated regret of getting screened if the test ended up being painful | 1.04 (0.85–1.28) | 0.70 | 1.01 (0.81–1.24) | 0.95 |
| Anticipated regret of not getting screened if an abnormality was found in the future | 1.27 (0.98–1.65) | 0.07 | 1.30 (1.00–1.69) | 0.05 |
| Belief that she needs a Pap test even if she takes good care of herself | 1.26 (1.02–1.56) | 0.03 | 1.27 (1.03–1.58) | 0.03 |
| Belief that there is little a person can do to reduce her risk of cervical cancer | 1.14 (0.95–1.37) | 0.15 | 1.13 (0.94–1.35) | 0.20 |
| Would rather not know if she had cervical cancer | 1.07 (0.85–1.34) | 0.59 | 1.07 (0.85–1.35) | 0.55 |
| Screening perceptions | ||||
| Positive perceptions of screening (3-item scale)f | 2.52 (1.38–4.62) | <0.01 | 2.51 (1.38–4.57) | <0.01 |
| Negative perceptions of screening (2-item scale)f | 1.14 (0.91–1.43) | 0.24 | 1.13 (0.90–1.41) | 0.31 |
| Perceived effectiveness of screening in lowering chances of getting cervical cancer | 1.20 (1.02–1.42) | 0.03 | 1.17 (0.99–1.39) | 0.06 |
| How nervous does screening make you feel? | 1.51 (1.15–1.99) | <0.01 | 1.50 (1.14–1.98) | <0.01 |
| Stigma | ||||
| Belief that if she had cervical cancer, people would think she slept around | 1.17 (0.97–1.41) | 0.10 | 1.15 (0.95–1.38) | 0.16 |
| Screening intent | ||||
| Competing health priorities are keeping her from getting screened right now | 0.92 (0.78–1.08) | 0.28 | 0.93 (0.79–1.09) | 0.37 |
| Confidence in her ability to get screening if she wants | 0.87 (0.74–1.02) | 0.09 | 0.86 (0.73–1.02) | 0.08 |
Bold p-values indicate p < 0.05.
Ascertained via participant response to the question “In the past year, have you tried to get a Pap smear?”
ORs represent the change in odds with a 1-unit increase in the respective index or scale.
Adjusted for participant self-reported race/ethnicity (included as a single categorical variable as White non-Latina/Hispanic, Black non-Latina/Hispanic, or Latina/Hispanic) and the number of doctor visits in the past year (included as a continuous numerical variable).
Index for awareness of HPV and cervical cancer consisting of 3 items, displayed in Figure 1.
Index for knowledge about HPV and cervical cancer screening consisting of 7 items, displayed in Figure 1.
Scales for perceived risk, embodiment of risk, positive screening perceptions, and negative screening perceptions displayed and described in Table 1.
Similarly, participants were more likely to report a screening attempt if they had a greater belief that a woman “needs a Pap even if she takes good care of herself” (aOR: 1.27; 95% CI: 1.03–1.58), a more positive perception of screening (aOR: 2.51; 95% CI: 1.38–4.57), and a higher degree of nervousness about screening (aOR: 1.50; 95% CI: 1.14–1.98).
Discussion
This study assessed cervical cancer screening knowledge, perceptions, and behaviors among 710 underscreened and uninsured or Medicaid-insured women in the United States. We found that knowledge about HPV, the purpose of Pap tests, and screening recommendations was uniformly low. While overall there was a high perceived severity of cervical cancer, perceptions of cervical cancer screening and reported screening behaviors varied among White, Black, and Latina/Hispanic participants.
An attempt to receive cervical cancer screening in the past year was reported among less than one-fifth of participants; screening attempt was more likely among participants with higher perceived personal risk of cervical cancer and more positive perceptions of screening.
Our findings support evidence that cervical cancer screening knowledge can be low among female populations in the United States. A study conducted in Federally Qualified Health Centers in Illinois found that over half of study participants thought that a Pap test screened for sexually transmitted, yeast, or other vaginal infections.22 Another study of African American women eligible for screening in Indiana found that only 26% of women knew the purpose of a Pap test.23
We similarly found that only 27% of low-income underscreened women knew that a Pap test screened for cervical cancer, and it was a common misconception among participants that Pap tests detect sexually transmitted infections. Additionally, we observed differences in knowledge and awareness by race and ethnicity: Black and Latina/Hispanic women were more likely than White women to think that HPV can cause herpes and less likely to know that Pap tests screen for cancer. Low health literacy may be associated with lower uptake of and adherence to cervical cancer screening.24,8
Increased health literacy was associated with Pap test uptake in a safety net clinic in Arizona, with 59% of patients with high health literacy receiving a Pap test compared with just 34% with low health literacy.25 Increased health literacy was also associated with being up to date on cervical cancer screening in a nationally representative U.S. survey.26 Thus, interventions such as provider communication about screening tests and their purpose, as well as patient navigation with education, may improve cervical cancer screening uptake among BIPOC individuals.27,28
We also assessed differences in perceptions of cervical cancer screening by race and ethnicity. Overall, there was a high level of anticipated regret among participants if they were not screened and a cervical abnormality was found later in life. Compared with White participants, both Black and Latina/Hispanic participants had a higher perceived effectiveness of screening in lowering their chances of getting cervical cancer; however, both Black and Latina/Hispanic participants tended to have more negative perceptions of screening (i.e., reporting that screening is both physically uncomfortable and embarrassing).
Black and Latina/Hispanic participants were also more likely to report a higher anticipated regret of getting screened if the screening test ended up being painful. These differences in perceptions may reflect past negative experiences with screening or other medical procedures.
In a qualitative interview study conducted in the United Kingdom, emotional barriers to seeking out screening—such as fear of pain, embarrassment, and anticipated shame—were commonly reported by women belonging to various ethnic minority groups compared with White women.29 Among Black women in Massachusetts, individuals report that poor relationships with and mistreatment by health care providers create mistrust and thus prevent them from returning to clinics to receive screening or follow-up treatment.30
Race predicted past-year screening attempts, with Black women more likely than White women to have attempted to receive screening in the past year. Given that Black women were more likely than White women to have more negative perceptions of screening and a lower perceived risk of cervical cancer, this finding may have been driven by Black women's higher perceived effectiveness of screening.
To our knowledge, no other studies have specifically studied perceptions of cervical cancer screening effectiveness in Black compared with White women in the United States. Thus, this is an area for future research, as health messaging aimed at increasing cervical cancer screening participation among certain subpopulations could focus on promoting awareness of screening's effectiveness in preventing cervical cancer.
Our MBMT-3 findings correspond to observations from other recent U.S. studies that show non-Hispanic Black women are more likely than non-Hispanic White women to report being up to date on cervical cancer screening.31,32 Alternatively, self-reported screening attempts may be subject to over-reporting as studies have shown that reported screening activities are often higher than actual screening activities.33
In our study, no other sociodemographic characteristics, such as income, insurance status, education, marital status, or rurality, were associated with attempted screening. This may be since all participants in the MBMT-3 trial were either publicly insured or uninsured and low-income (income ≤250% of the U.S. FPL) women. Uninsurance, Medicaid insurance, and low-income status have been consistently associated with low screening uptake and adherence.24,8
Participants who attended at least three doctor visits in the past year were more likely to have attempted screening, which may reflect increased access to health care or more positive relationships with the health care system in these individuals. Other studies have similarly shown that a higher number of doctor visits per year is associated with greater screening uptake, which may be mediated by better access to health care, greater opportunity for physician recommendation and education, or a relatively lower burden of other logistical and financial barriers for regular participation in the health care system.24,8
Certain perceptions of cervical cancer and related screening were associated with past-year screening attempts. Women with higher perceived personal risk of cervical cancer were more likely to have a past-year screening attempt. Similarly, more positive perceptions of screening (i.e., trust that Pap tests give accurate information and that it is both important and responsible to get screened) were positively associated with screening attempts.
Interestingly, those reporting higher degrees of nervousness about screening (ascertained by asking participants “When you think about getting cervical cancer screening, how nervous does it make you?”) were more likely to have past-year screening attempts. While studies have shown that fear and anticipated shame are negatively associated with screening uptake, nervousness may actually reflect an individual's higher perceived personal risk of cervical cancer or their worry about a cervical cancer diagnosis. Thus, feeling nervous may increase screening behavior if individuals still perceive screening to be beneficial in mitigating their risk of cervical cancer and they have the resources to seek screening.
Finally, if a woman believed that she needed a Pap test “even if she took good care of herself,” she was more likely to have attempted screening. This may reflect the negative impact that misconceptions about Pap tests can have on screening uptake and adherence.8,29
A major study strength is its inclusion of underscreened, low-income, and underinsured women. Compared with studies conducted in the general screening population, this underscreened population in the United States is relatively understudied and has a higher risk of cervical cancer. By using the baseline data of this large clinical trial of underserved women, we were able to better understand knowledge and perceptions as predictors of screening behaviors in this high-need population.
Compared with a general U.S. screening population, we have found similar trends that knowledge, psychosocial concerns, and beliefs differ among social groups and impact screening behaviors.8,26 However, our focus on underserved women allows for a more granular assessment of these factors, where income and insurance are not driving observed differences among study participants. Therefore, this study's findings may be useful to inform public health outreach strategies focused on improving screening uptake and adherence among U.S. women who bear the greatest burden of cervical cancer.
Limitations of this study include its selected sample of individuals. The MBMT-3 screening trial included only women who were underscreened, had a low income, and were underinsured. Thus, their knowledge, perceptions, and behaviors may not reflect those of the general population of underscreened women in the United States. Studies to compare and contrast knowledge, perceptions, and behaviors among underscreened women versus the general screening population should be conducted to identify any meaningful differences between these groups.
Additionally, the trial was advertised as a means for women to receive free cervical cancer screening and comprised volunteers, thus this sample of recruited participants may be more knowledgeable, motivated, or able to seek out screening than the general population.
Finally, while the trial included mostly Black participants and a smaller proportion of Latina/Hispanic participants, there is a much more limited sample size of other racial and ethnic groups—such as women identifying as Asian or Native American. These groups were not included in final analyses due to small sample sizes, which would have precluded meaningful interpretation of results.
However, a major study strength is its population of underscreened and uninsured or Medicaid-insured women. Individuals in this population are not often represented in screening studies due to difficulties in reliably accessing the health care system, thus their inclusion in this study offers insight into their unique perspectives about cervical cancer screening.
Conclusions
This study contributes to the literature on cervical cancer screening barriers with the unique perspectives of those historically under-represented in cervical cancer studies in the United States. Interventions aimed at educating women about cervical cancer causes and recommendations for screening, including efforts to dispel myths and improve patient–provider communication and relationships with the health care system, have potential to improve cervical cancer screening uptake and adherence among underscreened U.S. women.
Supplementary Material
Acknowledgments
The authors are grateful to the following study team members for their contribution to this study (in alphabetical order): Konyinsope Adewumi, Liz Aguilera, Anna Baker, Caitlin Biddel, Erin Brabble, Johana Bravo De Los Rios, Jessica Islam, Jocelyn Kim, Yesenia Merino, Victoria Monge, Randolph Qiao, Rohanit Singh, Alison Swiatlo, Ruth Tesfalidet, Olivia Vaz, Abigail Warmack, Autumn Watson, Erin Young, and Stephanie Zentz. The authors would also like to thank the American Sexual Health Association; Mecklenburg County Health Department; Charlotte Community Health Clinic, Inc.; Albemarle Regional Health Services; Sampson County Health Department; Cone Health Cancer Center; Stedman–Wade Health Services, Inc.; Advance Community Health Clinic; and their many community outreach partners.
Authors' Contributions
A.B. was involved in conceptualization, data curation, formal analysis, visualization, writing—original draft, and writing—review and editing. J.S.S. and N.T.B. were involved in conceptualization, funding acquisition, methodology, supervision, and writing—review and editing. S.B.W. was involved in funding acquisition, methodology, and writing—review and editing. B.S., F.H.M., and E.Z. were involved in data curation and writing—review and editing. A.C.D.M. was involved in project administration and writing—review and editing. L.B. was involved in project administration, resources, and writing—review and editing. M.G.H. was involved in methodology, supervision, and writing—review and editing. S.J. was involved in data curation, project administration, and writing—review and editing.
Author Disclosure Statement
J.S.S. has received research grants and consultancy fees from Hologic Corporation, BD Diagnostics, Arbor Vita, and Rovers Medical Devices for the past 5 years. A.C.D. has had some conference travel expenses covered by Hologic in the last 5 years. S.B.W. has received research grant funding from Pfizer paid to her institution for unrelated work. All other authors declare no conflicts of interest.
Funding Information
The National Institutes of Health (NIH) sponsored the My Body My Test-3 study (5R01CA183891-03). NIH did not have any role in the study design; collection, management, analysis, and interpretation of data; writing of the manuscript; or the decision to submit the report for publication. A.B. was supported by an NRSA Individual Predoctoral Fellowship (F30CA257181) and Cancer Control and Education Program Predoctoral Traineeship (T32 5T32CA57726-29).
Supplementary Material
References
- 1. Yang DX, Soulos PR, Davis B, et al. . Impact of widespread cervical cancer screening. Am J Clin Oncol 2018;41(3): 289–294; doi: 10.1097/COC.0000000000000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Buskwofie A, David-West G, Clare CA. A review of cervical cancer: Incidence and disparities. J Natl Med Assoc 2020;112(2):229–232; doi: 10.1016/J.JNMA.2020.03.002 [DOI] [PubMed] [Google Scholar]
- 3. Yu L, Sabatino SA, White MC. Rural-urban and racial/ethnic disparities in invasive cervical cancer incidence in the United States, 2010–2014. Prev Chronic Dis 2019;16(6):E70; doi: 10.5888/PCD16.180447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer 2017;123(6):1044–1050; doi: 10.1002/CNCR.30507 [DOI] [PubMed] [Google Scholar]
- 5. Leyden WA, Manos MM, Geiger AM, et al. . Cervical cancer in women with comprehensive health care access: Attributable factors in the screening process. J Natl Cancer Inst 2005;97(9):675–683; doi: 10.1093/JNCI/DJI115 [DOI] [PubMed] [Google Scholar]
- 6. Barlow WE, Beaber EF, Geller BM, et al. . Evaluating screening participation, follow-up, and outcomes for breast, cervical, and colorectal cancer in the PROSPR consortium. J Natl Cancer Inst 2020;112(3):238–246; doi: 10.1093/JNCI/DJZ137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. MacLaughlin KL, Jacobson RM, Radecki Breitkopf C, et al. . Trends over time in pap and pap-HPV cotesting for cervical cancer screening. J Womens Health (Larchmt) 2019;28(2):244–249; doi: 10.1089/JWH.2018.7380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Limmer K, LoBiondo-Wood G, Dains J. Predictors of cervical cancer screening adherence in the United States: A systematic review. J Adv Pract Oncol 2014;5(1):31. [PMC free article] [PubMed] [Google Scholar]
- 9. Chen HY, Kessler CL, Mori N, et al. . Cervical cancer screening in the United States, 1993-2010: Characteristics of women who are never screened. J Womens Health 2012;21(11):1132–1138; doi: 10.1089/jwh.2011.3418 [DOI] [PubMed] [Google Scholar]
- 10. Champion VL, Skinner CS. Chapter 3: The Health Belief Model. In: Health Behavior and Health Education: Theory, Research, and Practice, 4th Edition Jossey-Bass: San Francisco; 2008; pp. 45–65. [Google Scholar]
- 11. Phelan JC, Link BG. Is Racism a Fundamental Cause of Inequalities in Health? Annu Rev Sociol 2015;41(1):311–330; doi: 10.1146/ANNUREV-SOC-073014-112305 [DOI] [Google Scholar]
- 12. Williams DR, Lawrence JA, Davis BA. Racism and health: Evidence and needed research. Annu Rev Public Health 2019;40:105; doi: 10.1146/ANNUREV-PUBLHEALTH-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnson CE, Mues KE, Mayne SL, et al. . Cervical cancer screening among immigrants and ethnic minorities: A systematic review using the Health Belief Model. J Low Genit Tract Dis 2008;12(3):232–241; doi: 10.1097/LGT.0B013E31815D8D88 [DOI] [PubMed] [Google Scholar]
- 14. Austin LT, Ahmad F, McNally MJ, et al. . Breast and cervical cancer screening in Hispanic women: A literature review using the health belief model. Womens Health Issues 2002;12(3):122–128; doi: 10.1016/S1049-3867(02)00132-9 [DOI] [PubMed] [Google Scholar]
- 15. Byrd TL, Chavez R, Wilson KM. Barriers and facilitators of cervical cancer screening among Hispanic women. Ethn Dis 2007;17(1):129–134. [PubMed] [Google Scholar]
- 16. Williams M, Moneyham L, Kempf M-C, et al. . Structural and sociocultural factors associated with cervical cancer screening among HIV-infected African American women in Alabama. AIDS Patient Care STDS 2015;29(1):13–19; doi: 10.1089/APC.2014.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moyer VA. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2012;156(12):880–891. [DOI] [PubMed] [Google Scholar]
- 18. Anonymous. Recommendation: Cervical Cancer: Screening | United States Preventive Services Taskforce. n.d. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screening [Last accessed: August 12, 2021].
- 19. Spees LP, des Marais AC, Wheeler SB, et al. . Impact of human papillomavirus (HPV) self-collection on subsequent cervical cancer screening completion among under-screened US women: MyBodyMyTest-3 protocol for a randomized controlled trial. Trials 2019;20(1):788; doi: 10.1186/S13063-019-3959-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Watkins MW. Exploratory factor analysis: A guide to best practice. J Black Psychol 2018;44(3):219–246; doi: 10.1177/0095798418771807 [DOI] [Google Scholar]
- 21. Krieger N. Refiguring “race”: Epidemiology, racialized biology, and biological expressions of race relations. Int J Health Serv 2000;30(1):211–216; doi: 10.2190/672J-1PPF-K6QT-9N7U [DOI] [PubMed] [Google Scholar]
- 22. Hawkins NA, Benard VB, Greek A, et al. . Patient knowledge and beliefs as barriers to extending cervical cancer screening intervals in Federally Qualified Health Centers. Prev Med (Baltim) 2013;57(5):641; doi: 10.1016/J.YPMED.2013.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kasting ML, Wilson S, Zollinger TW, et al. . Differences in cervical cancer screening knowledge, practices, and beliefs: An examination of survey responses. Prev Med Rep 2017;5:169–174; doi: 10.1016/J.PMEDR.2016.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fuzzell LN, Perkins RB, Christy SM, et al. . Cervical cancer screening in the United States: Challenges and potential solutions for underscreened groups. Prev Med (Baltim) 2021;144:106400; doi: 10.1016/J.YPMED.2020.106400 [DOI] [PubMed] [Google Scholar]
- 25. Heberer MA, Komenaka IK, Nodora JS, et al. . Factors associated with cervical cancer screening in a safety net population. World J Clin Oncol 2016;7(5):406–413; doi: 10.5306/WJCO.V7.I5.406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim K, Han HR. The association between health literacy and breast and cervical cancer screening behaviors: Findings from the behavioral risk factor surveillance system. Nurs Res 2019;68(3):177–188; doi: 10.1097/NNR.0000000000000346 [DOI] [PubMed] [Google Scholar]
- 27. Kindratt TB, Dallo FJ, Allicock M, et al. . The influence of patient-provider communication on cancer screenings differs among racial and ethnic groups. Prev Med Rep 2020;18:101086; doi: 10.1016/J.PMEDR.2020.101086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Alimena S, Manning-Geist B, Pena N, et al. . Outcomes by race among women referred to an academic colposcopy clinic with a patient navigation program. J Womens Health 2021;30(6):902–909; doi: 10.1089/JWH.2020.8381/SUPPL_FILE/SUPP_TABLES4.DOCX [DOI] [PubMed] [Google Scholar]
- 29. Marlow LAV, Waller J, Wardle J. Barriers to cervical cancer screening among ethnic minority women: A qualitative study. J Fam Plann Reprod Health Care 2015;41(4):248–254; doi: 10.1136/JFPRHC-2014-101082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nolan J, Renderos TB, Hynson J, et al. . Barriers to cervical cancer screening and follow-up care among Black Women in Massachusetts. J Obstet Gynecol Neonatal Nurs 2014;43(5):580–588; doi: 10.1111/1552-6909.12488 [DOI] [PubMed] [Google Scholar]
- 31. Sokale IO, Montealegre JR, Oluyomi AO, et al. . Trends and racial/ethnic differences in predictors of cervical cancer screening among US women aged 30–64 years. Cancer Epidemiol Biomarkers Prev 2023;32(1):82–90; doi: 10.1158/1055-9965.EPI-22-0970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Francoeur AA, Liao C-I, Caesar MA, et al. . The increasing incidence of stage IV cervical cancer in the USA: What factors are related? Int J Gynecol Cancer 2022;32:1115–1122; doi: 10.1136/ijgc-2022-003728 [DOI] [PubMed] [Google Scholar]
- 33. Rauscher GH, Johnson TP, Young IC, et al. . Accuracy of self-reported cancer-screening histories: A meta-analysis. Cancer Epidemiol Biomarkers Prev 2008;17(4):748–757; doi: 10.1158/1055-9965.EPI-07-2629 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.