Abstract
Background:
We examined patterns of smoking in relation to health-related socioeconomic vulnerability (HRSV) among U.S. women early in the pandemic and whether mental health symptoms mediated these relationships.
Materials and Methods:
Data were obtained from the April 2020 National U.S. Women's Health COVID-19 Study (N = 3200). Among current smokers, adjusted odds of increased smoking since the start of the pandemic (vs. same or less) by incident and worsening HRSVs were modeled. Structural equation modeling was used to assess anxiety, depression, and traumatic stress symptoms as mediators of the relationship between six HRSVs (food insecurity; housing, utilities, and transportation difficulties; interpersonal violence; financial strain) and increased smoking early in the pandemic.
Results:
Nearly half (48%) of current smokers reported increased smoking since the pandemic started. Odds of increased smoking were higher among women with incident financial strain (aOR = 2.0, 95% CI 1.2–3.3), incident food insecurity (aOR = 2.9, 95% CI 1.7–5.1), any worsening HRSV (aOR = 2.2, 95% CI 1.5–3.0), and worsening food insecurity (aOR = 1.9, 95% CI 1.3–3.0). Anxiety symptoms were a significant, partial mediator of the relationship between increased smoking and any worsening HRSVs (proportion mediated = 0.17, p = 0.001) and worsening food insecurity (0.19, p = 0.023), specifically. Depression symptoms were a significant, partial mediator of the relationship between increased smoking and any worsening HRSVs (0.15, p = 0.004) and incident financial strain (0.19, p = 0.034). Traumatic stress was not a significant mediator of any tested relationship.
Conclusions:
Anxiety and depression symptoms partially explain the relationship between rising socioeconomic vulnerability and increased smoking among women early in the pandemic. Addressing HRSVs and mental health may help reduce increased smoking during a public health crisis.
Keywords: smoking, social risks, COVID-19 pandemic, anxiety, depression, mental health
Introduction
The COVID-19 pandemic, first declared by the World Health Organization in early March 2020,1 had an immediate and profound effect on population health, health behaviors, and economic stability. By mid-March, school and workplace closures, the mobilization of essential workers, stay-at-home orders, disruption of daily routines, and CDC guidance on social isolation led to altered work and social experiences,2 resulting in both positive and negative changes in health behaviors. Multiple studies indicate increased substance use in the United States since the start of the pandemic, including drinking, illicit substance abuse, and nicotine consumption.3,4 Stress, anxiety, depression, boredom, and uncertainty have all been named as possible contributing factors. The health risks of smoking were exacerbated during the pandemic, including increased risk among smokers of severe illness or death from COVID-19.5 Data suggest that people quit smoking due to perceived risk of COVID-196 and the overall prevalence of cigarette use declined in 2020.7 However, cigarette sales increased in 20208 after decades of decline, suggesting that those who smoked were smoking more.
An estimated 11% of U.S. women are current smokers and, each year, the deaths of more than 200,000 women are attributed to cigarettes.9,10 Although women have historically smoked at lower rates than men, the narrowing gender gap in smoking rates as well as differences in the magnitude of disease risk from smoking by gender have led to disproportionately higher rates of smoking-related disease and death in women more recently.11 Also, prepandemic, cigarette use was nearly twice as high among women living below the federal poverty level (FPL) compared with those living at 200% FPL or above. Low socioeconomic status is associated with heavier smoking, less success in quitting smoking, and a longer lifetime duration of smoking.12 In addition to socioeconomic status, prepandemic smoking among women has been associated with several other health-related socioeconomic vulnerabilities (HRSVs), including food insecurity, housing instability, and interpersonal violence.13–17
In April 2020, the National U.S. Women's Health COVID-19 Study found that nearly half of all women had worsening or incident HRSVs, including food insecurity, interpersonal violence, transportation and utilities difficulties, and housing instability;18 more than a quarter of women acquired new HRSVs in the early pandemic. While smoking and HRSVs are closely related, how the change in HRSVs since the pandemic has affected smoking has not been previously reported.
In addition to the effect of the pandemic on rising HRSVs among women, mental health symptoms also increased. In late 2020, more than 50% of Americans reported anxiety and 42% reported experiencing depressive symptoms.19 In women smokers, prepandemic, rates of mental illness have been reported to be as high as 86%.20 When compared with men, women reported significant increases in levels of depression, anxiety, and stress in response to the pandemic.21 Mental health difficulties were closely linked to HRSVs: early in the pandemic, each incident HRSV was associated with a two to three times increased risk in experiencing symptoms of depression, anxiety, and traumatic stress.18
This study aims to (1) evaluate change in smoking among women in the early pandemic in relation to HRSVs and (2) explore to what degree mental health symptoms mediated the relationship between HRSVs and smoking. A stronger mechanistic understanding of how HRSVs relate to smoking is needed to inform public policy targeting smoking cessation.
Materials and Methods
Design, setting, and participants
This study is based on a cross-sectional analysis of data from the National U.S. Women's Health COVID-19 Study conducted April 10–20, 2020. As previously described in detail, the sample of 3200 U.S. English-speaking women ages ≥18 years were recruited from a prospective online health research panel maintained by Opinions 4 Good (Op4G).18,22 The study used a nested quota sampling strategy, matching the age and education of the 2018 U.S. population of adult women. Additionally, the sample was stratified by race and ethnicity, oversampling East/Southeast Asian women (defined as those selecting one or more of the following races: Chinese, Filipino, Japanese, Korean, and/or Vietnamese). The University of Chicago Institutional Review Board approved this study protocol and all participants provided digital documentation of informed consent.
Measures
Validated survey measures were used whenever possible. Survey domains used for this analysis queried: (1) sociodemographic, household, and overall health characteristics, (2) current substance use (i.e., alcohol, tobacco) and change in use since the start of the pandemic, (3) prepandemic HRSVs and change in HRSVs since the start of the pandemic, and (4) mental health conditions.
The analytic sample was stratified by women who were current smokers, including those who responded “some days” or “every day” to the question “Do you smoke cigarettes every day, some days, or not at all,” evaluated using the Behavioral Risk Factor Surveillance System (BRFSS) 2019 questionnaire.23
Change in smoking status from prepandemic to early in the pandemic was assessed with the novel question, “Since the start of the coronavirus pandemic, compared to your usual amount, do you smoke more, less, or about the same?” Those who smoked more (increased smoking) were compared with those who reported smoking less or about the same. Quit attempts were evaluated using the BRFSS 2019 survey question, “During the past 12 months, have you stopped smoking for one day or longer because you were trying to quit smoking?”23 Those who responded affirmatively were categorized as having a quit attempt.
HRSVs, including financial strain, food insecurity, housing instability, interpersonal violence, and transportation and utilities difficulties, were evaluated using the Accountable Health Communities Health-Related Social Needs Screening Tool.24 The change in HRSVs was tabulated by evaluating pre- and early pandemic HRSV status then categorized as: secure (no HRSVs pre- or early pandemic), persistent or improved (HRSV present prepandemic+no change or change for the better since the pandemic), incident (HRSV absent prepandemic+change for the worse since the pandemic), or worsening (HRSV present prepandemic+change for the worse since the pandemic). This categorization of changes in HRSVs was also used in previous studies using data from this survey sample.18,22 Reduced wages or work hours was assessed by responses to the question “Have you experienced any difficulties due to the coronavirus crisis?” from the Stanford COVID-19 Survey.25
Anxiety, depression, and traumatic stress symptoms were evaluated using the General Anxiety Disorder-7,26 Patient Health Questionnaire-2,27 and two items from the Modified Posttraumatic Stress Disorder Checklist (feeling very upset and experiencing disturbing thoughts),28 respectively. A score of 0–9 (none or mild) on the General Anxiety Disorder-7 scale was categorized as no anxiety and a score of 10 or greater (moderate or severe) was categorized as having anxiety. A score of 3 or greater on the Patient Health Questionnaire-2 was categorized as having depression. A response of “quite a bit” or “extremely” on either question on the Modified Posttraumatic Stress Disorder Checklist was categorized as experiencing traumatic stress. Concern about the pandemic was assessed using the adapted National 2009 H1N1 Flu Survey question, “How concerned are you about the coronavirus pandemic?” Responses were dichotomized: those indicating they were very concerned compared with respondents indicating they were somewhat concerned, not very concerned, or not at all concerned.29
Statistical analyses
Sample weights, calibrated using the raking-ratio method, were used to generate pseudo design-based weights with marginal distributions for age, race, education, income, and region matching those of 2018 U.S. population estimates. Rates of HRSVs were stratified by smoking status. Multivariable logistic regression was used to model odds of increased smoking since the start of the pandemic by the (1) presence of each incident or worsening HRSV and (2) presence of any incident or worsening HRSV. Model covariates included age, marital status, education, income category, number of people in household, number of household children, self-reported overall health, and number of comorbidities.
To evaluate if anxiety, depression, or traumatic stress mediated the relationship between incident or worsening HRSVs and increase in smoking since the start of the pandemic, structural equation models were used. Direct, indirect (the effect of HRSVs on smoking through anxiety, depression, or traumatic stress symptoms), and total effects of worsening or incident HRSVs on smoking were calculated. The proportion mediated by anxiety, depression, or traumatic stress was calculated and defined as the indirect effect divided by the total effect.
All analyses used Stata version 16.1 (StataCorp. LLC, College Station, TX).
Results
More than a quarter of women (26%, n = 886) were current smokers early in the pandemic, and nearly half of these women (48%) reported increased smoking since the start of the pandemic (Table 1). Current smokers were younger, less educated, had lower income, and had more people in their households compared to non-smokers (all p < 0.05). Additionally, current smokers reported higher rates of having fair or poor mental health and physical health, as well as higher rates of at least one comorbid illness, compared with nonsmokers. Smokers, compared with nonsmokers, also had significantly higher rates of moderate or severe anxiety (39% vs. 25%), moderate or severe depression (41% vs. 25%), and traumatic stress (23% vs. 16%) early in the pandemic (Table 1).
Table 1.
Weighted Sample Characteristics, Stratified by Smoking Status and Change in Smoking Early in the Pandemic (N = 3166)
| Nonsmoker (n = 2280), % | Smoker (n = 886), % | p | Smoked the same or less (n = 461), % | Smoked more (n = 423), % | p | |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18–44 | 42.5 | 50.4 | <0.001 | 42.0 | 47.7 | 0.462 |
| 45–64 | 31.4 | 37.4 | 34.2 | 31.6 | ||
| 65+ | 26.0 | 12.2 | 23.8 | 20.8 | ||
| Race/ethnicity | ||||||
| White | 63.8 | 69.6 | 0.006 | 65.5 | 68.3 | 0.159 |
| Hispanic | 13.6 | 14.3 | 19.2 | 13.0 | ||
| Black | 11.8 | 7.4 | 8.2 | 7.8 | ||
| Asian | 6.1 | 3.9 | 4.0 | 7.5 | ||
| Other | 4.8 | 4.8 | 3.2 | 3.4 | ||
| Education | ||||||
| Greater than high school | 66.3 | 53.1 | <0.001 | 58.1 | 68.2 | 0.018 |
| High school or less | 33.7 | 47.0 | 41.9 | 31.8 | ||
| Partnership status | ||||||
| Married | 62.7 | 59.7 | 0.176 | 54.1 | 64.4 | 0.026 |
| Unmarried/single | 37.3 | 40.3 | 45.9 | 35.6 | ||
| Income | ||||||
| Less than 25,000/year | 16.2 | 29.2 | <0.001 | 19.9 | 19.3 | 0.796 |
| Between 25,000 and 49,999/year | 20.6 | 23.3 | 21.7 | 20.8 | ||
| Between 50,000 and 99,999/year | 30.4 | 28.8 | 28.4 | 31.9 | ||
| More than 100,000/year | 32.8 | 18.7 | 30.0 | 28.1 | ||
| Employment | ||||||
| Employed | 46.2 | 50.1 | 0.049 | 46.9 | 56.9 | 0.030 |
| Unemployed | 6.8 | 8.0 | 8.0 | 4.8 | ||
| Unemployed by choice or unable to work | 47.2 | 42.0 | 45.1 | 38.4 | ||
| Household composition | ||||||
| Self | 15.4 | 15.9 | <0.001 | 21.3 | 13.4 | 0.030 |
| Self +1 other | 36.5 | 28.4 | 31.3 | 28.5 | ||
| Self +2 or more | 48.1 | 55.8 | 47.4 | 58.1 | ||
| No. of children living at home | ||||||
| None | 64.3 | 52.2 | <0.001 | 63.8 | 48.2 | 0.003 |
| 1 child | 15.7 | 22.4 | 16.5 | 24.8 | ||
| 2 or more children | 20.1 | 25.4 | 19.7 | 27.0 | ||
| Self-rated mental health | ||||||
| Excellent or very good | 53.0 | 44.8 | <0.001 | 56.9 | 40.7 | 0.001 |
| Good | 30.4 | 29.1 | 24.8 | 30.4 | ||
| Fair or poor | 16.6 | 26.1 | 18.3 | 28.9 | ||
| Self-rated overall health | ||||||
| Excellent or very good | 47.0 | 33.1 | <0.001 | 39.5 | 30.7 | 0.067 |
| Good | 36.4 | 39.9 | 38.4 | 38.8 | ||
| Fair or poor | 16.7 | 27.0 | 22.1 | 30.5 | ||
| No. of comorbidities | ||||||
| 0 | 57.3 | 43.7 | <0.001 | 49.2 | 35.2 | <0.001 |
| 1 | 27.9 | 33.6 | 35.0 | 33.2 | ||
| 2 | 9.0 | 14.2 | 11.5 | 18.6 | ||
| 3 or more | 5.8 | 8.6 | 4.3 | 13.0 | ||
| Anxiety | ||||||
| None or mild | 75.1 | 61.0 | <0.001 | 75.1 | 50.3 | <0.001 |
| Moderate or severe | 24.7 | 39.0 | 24.9 | 49.8 | ||
| Depression | ||||||
| None or mild | 74.8 | 58.6 | <0.001 | 70.7 | 47.6 | <0.001 |
| Moderate or severe | 25.2 | 41.4 | 29.3 | 52.4 | ||
| Traumatic stress | ||||||
| None or mild | 84.5 | 77.2 | <0.001 | 76.5 | 74.0 | 0.533 |
| Moderate or severe | 15.5 | 22.8 | 23.5 | 26.0 | ||
Calibration weights were utilized and were generated based on the following variables: age group, race, education, income, and region.
Among current smokers, those who smoked more early in the pandemic (compared with those who smoked the same or less) had more people in their households, higher rates of fair or poor mental and overall health and three or more comorbidities (all p < 0.05). Approximately half of those who smoked more early in the pandemic reported anxiety and depression (50% and 52%, respectively). Rates of anxiety and depression were significantly higher and traumatic stress rates were similar comparing women who smoked more to others (Table 1). Thirty-four percent of those who smoked more in the early pandemic reported reduced work or wage hours, compared with 20% who smoked the same or less (p < 0.001). Women who were very concerned about the pandemic were similarly likely as those who were somewhat, not very, or not at all concerned to be smokers (28% vs. 24%, respectively, p = 0.07), and among current smokers, those who were very concerned had higher rates of quit attempts (21% vs. 17%, p = 0.004), and were more likely to have smoked more early in the pandemic (53% vs. 37%, p = 0.001).
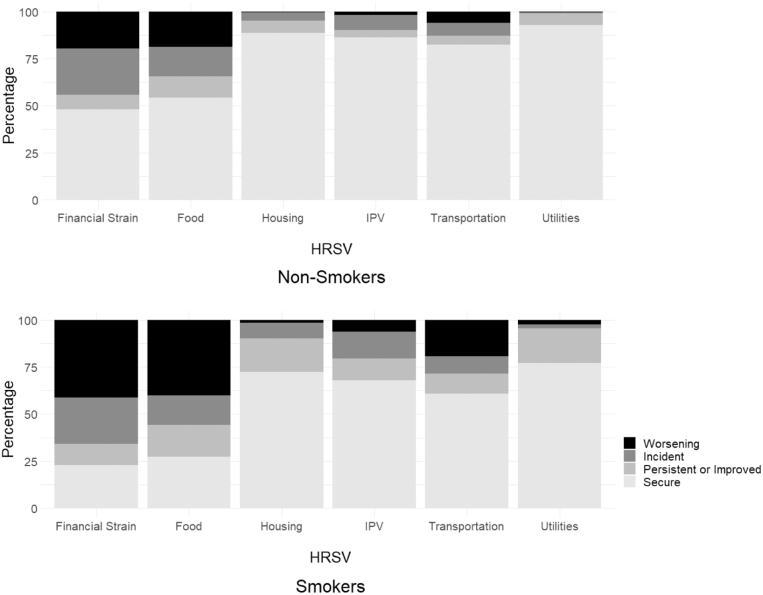
Early in the pandemic, smokers had significantly higher rates of all six HRSVs compared with nonsmokers: financial strain, food insecurity, housing instability, interpersonal violence, utilities difficulties, and transportation difficulties (Table 2, all p < 0.001). Rates of worsening and incident HRSVs early in the pandemic were also higher for smokers compared with nonsmokers (Fig. 1, all p < 0.001).
Table 2.
Rates of Health-Related Socioeconomic Vulnerabilities Prepandemic and Early in the Pandemic (N = 3166)
| Prepandemic (overall), % | Early in the pandemic, % |
p | |||
|---|---|---|---|---|---|
| Nonsmoker (n = 2280) | Smoker (n = 886) | Total | |||
| ≥1 HRSV | 51.9 | 53.7 | 79.9 | 60.5 | <0.001 |
| Financial strain | 34.2 | 52.1 | 77.3 | 58.7 | <0.001 |
| Food insecurity | 37.2 | 45.7 | 72.9 | 52.8 | <0.001 |
| Housing instability | 10.1 | 11.2 | 27.5 | 15.5 | <0.001 |
| Interpersonal violence | 8.7 | 13.8 | 32.0 | 18.6 | <0.001 |
| Utilities difficulties | 10.4 | 7.0 | 23.0 | 11.2 | <0.001 |
| Transportation difficulties | 15.8 | 17.6 | 39.3 | 23.3 | <0.001 |
Calibration weights were utilized and were generated based on the following variables: age group, race, education, income, and region.
HRSV, health-related socioeconomic vulnerability.
FIG. 1.
Prevalence of secure, persistent or improved, worsening, or incident HRSVs since start of pandemic, stratified by current smoking status. 1. Calibration weights were utilized and were generated based on the following variables: age group, race, education, income, and region. 2. Change in each HRSV was categorized as: secure (absent prepandemic and early in the pandemic), incident (absent prepandemic and present early in the pandemic), persistent or improved (present prepandemic and unchanged or improved early in the pandemic), and worsening (present prepandemic and worse early in the pandemic). HRSV, health-related socioeconomic vulnerability.
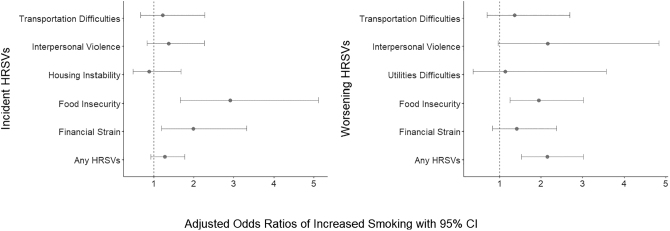
Odds of increased smoking early in the pandemic were higher among women with incident financial strain (aOR = 2.0, 95% CI 1.2–3.3), incident food insecurity (aOR = 2.9, 95% CI 1.7–5.1), one or more worsening HRSV (aOR = 2.2, 95% CI 1.5–3.0), and worsening food insecurity (aOR = 1.9, 95% CI 1.3–3.0) (Fig. 2) compared with those who had secure or persistent/improved HRSVs.
FIG. 2.
Adjusted odds of increased smoking since the start of the pandemic by incident and worsening HRSVs among current smokers early in the pandemic (N = 886). Incident utilities difficulties and worsening housing instability were not included in models due to small sample sizes of those experiencing these conditions.
Anxiety and depression symptoms (but not traumatic stress) were partial and statistically significant mediators of the associations between some incident and worsening HRSVs and increased smoking since the start of the pandemic. Specifically, the indirect or mediated association between incident and worsening HRSVs and increased smoking since the pandemic was significant for anxiety for any worsening HRSVs (proportion mediated = 0.17) and worsening food insecurity (0.19); this relationship was significant for depression for any worsening HRSVs (0.15) and for any incident financial strain (0.19) (Table 3). Traumatic stress was not a significant mediator of any tested relationship (range of proportion mediated = 0.01–0.16).
Table 3.
Estimates of Total, Direct, and Indirect Effects (Mediated Through Anxiety, Depression, or Traumatic Stress) of the Association Between Worsening or Incident Health-Related Socioeconomic Vulnerabilities and Increased Smoking Since the Start of the Pandemic, Adjusted for All Other Covariates
| |
Total effect |
Direct effect |
Indirect effect |
Proportion mediated | ||||
|---|---|---|---|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | β (95% CI) | p | |||
| Mediator | ||||||||
| Incident food insecurity | Anxiety | 0.23 (0.11 to 0.36) | <0.001 | 0.22 (0.09 to 0.35) | 0.001 | 0.02 (−0.01 to 0.04) | 0.153 | 0.07 |
| Incident financial strain | 0.14 (0.02 to 0.26) | 0.025 | 0.11 (−0.01 to 0.23) | 0.080 | 0.03 (0.00 to 0.05) | 0.056 | 0.20 | |
| Any worsening HRSVs | 0.18 (0.10 to 0.26) | <0.001 | 0.14 (0.06 to 0.22) | 0.001 | 0.04 (0.02 to 0.07) | 0.001 | 0.17 | |
| Worsening food insecurity | 0.16 (0.06 to 0.26) | 0.003 | 0.13 (0.02 to 0.24) | 0.017 | 0.03 (0.00 to 0.05) | 0.023 | 0.19 | |
| Incident food insecurity | Depression | 0.25 (0.12 to 0.37) | <0.001 | 0.24 (0.12 to 0.37) | <0.001 | 0.00 (−0.02 to 0.03) | 0.707 | 0.02 |
| Incident financial strain | 0.14 (0.02 to 0.26) | 0.018 | 0.12 (0.00 to 0.24) | 0.059 | 0.03 (0.00 to 0.05) | 0.034 | 0.19 | |
| Any worsening HRSVs | 0.18 (0.10 to 0.26) | <0.001 | 0.17 (0.07 to 0.28) | <0.001 | 0.03 (0.01 to 0.05) | 0.004 | 0.15 | |
| Worsening food insecurity | 0.15 (0.05 to 0.26) | 0.003 | 0.14 (0.04 to 0.24) | 0.008 | 0.01 (0.00 to 0.03) | 0.101 | 0.09 | |
| Incident food insecurity | Traumatic Stress | 0.25 (−0.11 to 0.24) | 0.445 | 0.24 (0.11 to 0.37) | <0.001 | 0.01 (−0.01 to 0.03) | 0.473 | 0.03 |
| Incident financial strain | 0.15 (0.03 to 0.27) | 0.013 | 0.13 (0.01 to 0.25) | 0.040 | 0.02 (0.00 to 0.05) | 0.060 | 0.16 | |
| Any worsening HRSVs | 0.18 (0.10 to 0.26) | <0.001 | 0.17 (0.09 to 0.25) | <0.001 | 0.01 (−0.01 to 0.02) | 0.266 | 0.04 | |
| Worsening food insecurity | 0.15 (0.05 to 0.25) | 0.005 | 0.15 (0.04 to 0.25) | 0.005 | 0.00 (−0.01 to 0.02) | 0.827 | 0.01 | |
Models were adjusted for age, marital status, education, income category, number of people in household, number of household children, self-reported overall health, and number of comorbidities.
Discussion
Using data from a national survey of U.S. women, this study establishes a relationship between pandemic-related HRSVs and smoking early in the pandemic and gives new insights to the role of mental health in mediating this relationship. Smokers reported more than twice the rate of worsening HRSVs compared with nonsmokers. Those with increased smoking early in the pandemic also reported nearly twice the rates of anxiety and depression compared with nonsmokers. This study finds that anxiety was a significant mediator between increased smoking early in the pandemic and any worsening HRSV and worsening food insecurity, specifically. Depression was also a significant mediator between increased smoking and any worsening HRSV and incident financial strain, specifically.
In contrast to other HRSVs examined, both incident and worsening food insecurity predicted odds of increased smoking since the start of the pandemic. Smoking has a unique, physiologic relationship to food insecurity. Food insecurity is a stressful situation and acute administration of nicotine is known to induce a relaxing effect.30 Additionally, although hunger and food insecurity are distinct, nicotine is a known appetite suppressant, which may help those with limited access to food deal with the physical discomfort of food insufficiency.31 This biological relationship between nicotine and food insecurity may help explain why incident food insecurity was a significant predictor of increased smoking early in the pandemic. Worsening food insecurity, in particular, was alarmingly high among smokers: 40% of smokers reported worsening food insecurity early in the pandemic compared with 19% of nonsmokers. While pandemic-related policies under the American Rescue Plan afforded mothers and families temporary relief, the end of the child tax credit in December 2021 resulted in nearly 50% of families reporting not being able to afford enough food.32
The relationships between worsening HRSVs and increased smoking were found to be mediated by anxiety and depression. In contrast, the relationship between incident food insecurity (food insecurity among women who did not experience food insecurity prepandemic) and smoking was not significantly mediated by depression, anxiety, or traumatic stress. These findings suggest that the chronicity and severity of having any HRSVs are drivers of increased smoking since the pandemic began, partially through anxiety and depression. Previous research found that smoking in the setting of financial instability was used to ignore hunger and delay the discomfort of quitting in the midst of instability and that obtaining cigarettes was prioritized over other needs.33
Accordingly, a majority (nearly 80%) of women smokers in our study reported experiencing financial strain early in the pandemic and odds of increased smoking was significantly associated with incident financial strain. In addition, increased smoking was associated with reduced work or wage hours. The relationship between smoking and financial strain is known to be bidirectional.34 Initially, reduced work or wage hours may have availed women smokers more time to smoke, as smoking is restricted in most workplaces. As the pandemic abruptly worsened women's economic stability,35 the cost of smoking may have become newly burdensome. Heavy smoking is associated with greater difficulty paying for household expenses.36 Smoking-related expenditures could cause incident financial strain by reducing the available funds that smokers have for other expenses. In contrast to incident financial strain, worsening financial strain was not associated with increased smoking. One explanation may be that when financial strain becomes more severe, smokers may not be financially able to prioritize obtaining cigarettes.
Last, depression was shown to mediate the relationship between incident financial strain and smoking more: financial strain has been shown to be a strong predictor of depression.37,38
Although this study did not examine quit attempts, COVID-19-related mental health conditions may have affected both positive and negative change in smoking behavior. Given the dose-dependent, addictive nature of nicotine, a small change in smoking status could be hypothesized to lead to long-term impacts on smoking behavior. Concern about the pandemic may have influenced both mental health and smoking behavior, as smokers were more likely to have higher rates of quit attempts and to smoke more in the early pandemic, compared with those who reported that they were somewhat, not very, or not at all concerned. A July 2019–June 2020 study, which comprised mostly women, found that more than half of sustained smokers smoked more in June 2020, compared with 30% smoking the same and 19% smoking less.39 Both smoking more and less, compared with the same amount, was associated with higher levels of COVID-19-related distress and general stress.39 Further research is needed to examine the sustained effects of changes in smoking behavior due to the COVID-19 pandemic.
Low socioeconomic status, financial strain, and poor mental health are established barriers to smoking cessation. People of lower socioeconomic status have lower cessation success rates; income, poverty, health insurance status, experiences of financial strain, and educational attainment all contribute to cessation disparities.40,41 Lifetime diagnoses of depression or anxiety are associated with lower smoking cessation success rates and lower rates of attempting to quit,42 while conversely, receipt of mental health treatment is associated with higher rates of quit success.43 Even when accounting for higher depression rates in women, the presence of depression is independently associated with lower quit success rates in women compared with men.44 Women report anxiety, depression, and stress as primary reasons for smoking relapse at higher levels than men.45 While evidence-based smoking cessation programs are effective in raising quit success rates,46 differing rates of quit success among those with mental illness and financial strain indicate a need to address more systemic social disparities to address smoking rates.
Quit lines that also offer interventions to connect individuals with resources for unmet basic needs have been proposed as a more effective solution to reducing smoking.47 Utilization and knowledge of community-based resources (e.g., food pantry referrals and free food vouchers for food insecurity; promoting financial literacy and asset building for financial strain) have been shown to be effective interventions for addressing these unmet needs.48,49 Universally providing smokers with resources on HRSVs at the primary point of care, in addition to tobacco counseling, may mitigate high rates of HRSVs in smokers.
This cross-sectional study should be interpreted in the context of its limitations. It provides a snapshot of smoking behavior very early in the pandemic, but does not track change over time. While this study queried level of smoking compared with prepandemic levels, accounting for the number of cigarettes smoked and consumption of other nicotine-based products would further elucidate the relationship between HRSVs and smoking. The two-item food security screener used for this survey may contribute to higher estimates of food insecurity compared with more specific measures.50,51
Even with sampling weights, some estimates may not be generalizable, due to limited access to a probability sample in April 2020 of the U.S. population. However, the estimates for domains in this sample have been previously compared and found to be similar.52 The sample was not probability based, although the generalizability of the sample is likely improved by use of a quota sample. Web-based surveys are subject to selection and recall bias. Low rates of incident or worsening housing instability and utilities difficulties in light of pandemic-related policies prohibited sufficient power for these analyses.
While smokers are approximately twice as likely as others to have post-traumatic stress disorder,53 the modified measure of traumatic stress is distinct from experiences of psychological stress or chronic stress. Details regarding occupation types, which were not queried in our survey, could have given additional insight into the relationship among smoking, anxiety, and depression. A previous study found that the essential workforce, comprised heavily of women, experienced high adverse psychological impacts early in the pandemic.54 Because our study asked about quit attempts since the start of the pandemic among current smokers only, we could not analyze positive changes in smoking behavior (i.e., sustained abstinence among women who quit prepandemic) in the overall sample. Additionally, race and ethnicity were not included in the models due to small sample sizes. As only women were queried for this survey, we are unable to make gender-based comparisons.
Conclusions
To our knowledge, this is the first study to show the (1) impact of incident and worsening pandemic-related HRSVs on smoking, and (2) mental health as a mediator of the relationship between HRSVs and increased smoking early in the pandemic. There has been a worsening of key indicators of mental health in women during the pandemic, especially among those experiencing HRSVs. Our findings point to a need to address both modifiable mental health and HRSVs to reduce smoking among women. The toolkit for caring for women smokers during a public health crisis should include strategies to address HRSVs, as well as depression and anxiety.
Acknowledgments
The National Women's Health COVID-19 survey was developed by S.T.L.; Kate Doyle, MPH; Kelly Boyd, BS; Sadia Haider, MD, MPH; Nita K. Lee, MD, MPH; J.A.M.; Elizabeth Pinkerton, MPH; L. Philip Schumm, MA; Marie Tobin, MD; K.E.W.; and Ernst Lengyel, MD, PhD (University of Chicago, 2020). The authors also acknowledge Veera Anand and Delaney Romanchick for assistance with the development of this article.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authors' Contributions
V.A.W. led the writing of the article and design of this study, led the data analysis and contributed to the interpretation of data, and created the visualizations. K.E.W. contributed to the analysis and interpretation of the data and to the writing and editing of the article. J.S.J. contributed to the interpretation and replication of the data and to the writing and editing of the article. J.A.M. contributed to the conceptualization, data curation, data analysis and interpretation, and critical review of the article. S.T.L. led the acquisition of funding and investigation and contributed to the administration, resources, conceptualization, data analysis and interpretation, and critical review and revision of the article. M.V. contributed to the interpretation of the data and results, and to the writing and editing of the article.
Author Disclosure Statement
Under the terms of Grant Number 1C1CMS330997-01-00 (ST Lindau, PI) from the Department of Health and Human Services, Centers for Medicare & Medicaid Services, we were expected to develop a sustainable business model to continue and support the model that we tested after award funding ended. Dr. Stacy Lindau was the founder and owner of a social impact company, NowPow, LLC, which was acquired by Unite USA Inc. in 2021. Dr. Lindau is an unpaid advisor to and holds stock in Unite USA Inc. Dr. Lindau is an editor on Female Sexual Dysfunction for UpToDate and received royalties <$100/year in 2019, 2020 for this work. Subsequent royalties have been paid to the University of Chicago. Neither the University of Chicago nor UChicago Medicine is endorsing or promoting Unite USA Inc. or its business, products, or services. Dr. Lindau and her spouse own equity in Glenbervie Health, LLC. The University of Chicago has filed patents (pending) for the Bionic Breast Project, a project led by S.T.L. All remaining authors have no conflicts of interest or disclosure.
Funding Information
The research effort of S.T.L. was supported in part by 5R01AG064949, 5R01MD012630, R21CA226726, 5R01HL150909, UG3HL154297, T32CA193193, and 1R01DK127961. The research effort of V.A.W., J.S.J., J.A.M., K.E.W., and M.V. was also supported by all or some of these grants.
References
- 1. Keaten J, Cheng M, Leicester J. WHO Declares Coronavirus a Pandemic, Urges Aggressive Action. AP News. 2021. Available from: https://apnews.com/article/united-nations-michael-pence-religion-travel-virus-outbreak-52e12ca90c55b6e0c398d134a2cc286e [Last accessed: January 3, 2022].
- 2. Van Kessel P, Baronavski C, Scheller A, et al. In Their Own Words, Americans Describe the Struggles and Silver Linings of the COVID-19 Pandemic. Pew Research Center. 2021. Available from: https://www.pewresearch.org/2021/03/05/in-their-own-words-americans-describe-the-struggles-and-silver-linings-of-the-covid-19-pandemic/ [Last accessed: January 3, 2023].
- 3. Rogers AH, Shepherd JM, Garey L, et al. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res 2020;293:113407; doi: 10.1016/j.psychres.2020.113407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mejia MC, Zoorob R, Levine RS, et al. Cross-sectional survey of smoking patterns during the COVID-19 pandemic in a tobacco cessation and lung cancer screening program. Ochsner J 2022;22(1):48–60; doi: 10.31486/toj.21.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. COVID-19: People with Certain Medical Conditions. 2022. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html [Last accessed: January 3, 2023].
- 6. Nyman AL, Spears CA, Churchill V, et al. Associations between COVID-19 risk perceptions and smoking and quitting behavior among U.S. adults. Addict Behav Rep 2021;14:100394; doi: 10.1016/j.abrep.2021.100394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention. Smoking & Tobacco Use: Current Cigarette Smoking Among Adults in the United States. 2022. Available from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm/ [Last accessed: January 3, 2023].
- 8. Federal Trade Commission. FTC Report Finds Annual Cigarette Sales Increased for the First Time in 20 Years. 2021. Available from: www.ftc.gov/news-events/news/press-releases/2021/10/ftc-report-finds-annual-cigarette-sales-increased-first-time-20-years [Last accessed: January 3, 2023].
- 9. Centers for Disease Control and Prevention. Smoking & Tobacco Use: Tobacco-Related Mortality. 2020. Available from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/tobacco_related_mortality/index.htm [Last accessed: January 3, 2023].
- 10. Centers for Disease Control and Prevention. Fact Sheets on Smoking and Tobacco Use. 2022. Available from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/index.htm [Last accessed: January 3, 2023].
- 11. American Lung Association. Women and Tobacco Use. 2022. Available from: https://www.lung.org/quit-smoking/smoking-facts/impact-of-tobacco-use/women-and-tobacco-use [Last accessed: January 3, 2023].
- 12. Centers for Disease Control and Prevention. People with Low Socioeconomic Status Experience a Health Burden from Commercial Tobacco. 2022. Available from: https://www.cdc.gov/tobacco/disparities/low-ses/index.htm [Last accessed: January 3, 2023].
- 13. Kim JE, Tsoh JY. Cigarette smoking among socioeconomically disadvantaged young adults in association with food insecurity and other factors. Prev Chronic Dis 2016;13:E08; doi: 10.5888/pcd13.150458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim JE, Flentje A, Tsoh JY et al. Cigarette smoking among women who are homeless or unstably housed: Examining the role of food insecurity. J Urban Health 2017;94(4):514–524; doi: 10.1007/s11524-017-0166-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hosler AS, Michaels IH. Association between food distress and smoking among racially and ethnically diverse adults, Schenectady, New York, 2013–2014. Prev Chronic Dis 2017;14:E71; doi: 10.5888/pcd14.160548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jun HJ, Rich-Edwards JW, Boynton-Jarrett Ret al. Intimate partner violence and cigarette smoking: Association between smoking risk and psychological abuse with and without co-occurrence of physical and sexual abuse. Am J Public Health 2008;98:527–535; doi: 10.2105/AJPH.2003.037663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kim-Mozeleski J, Pandey R. The intersection of food insecurity and tobacco use: A scoping review. Health Promot Pract 2020;21:124S–138S; doi: 10.1177/1524839919874054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lindau ST, Makelarski JA, Boyd K, et al. Change in health-related socioeconomic risk factors and mental health during the early phase of the COVID-19 pandemic: A national survey of U.S. women. J Womens Health 2021;30(4):502–513; doi: 10.1089/jwh.2020.8879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Berkowitz SA, Basu S. Unmet social needs and worse mental health after expiration of COVID-19 federal pandemic unemployment compensation. Health Affairs 2021;40:426–434; doi: 10.1377/hlthaff.2020.01990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jessup MA, Dibble SL, Cooper BA. Smoking and behavioral health of women. J Womens Health 2012;21(7):783–791; doi: 10.1089/jwh.2011.2886 [DOI] [PubMed] [Google Scholar]
- 21. Van Ness M. Baylor University. COVID-19 and Women's Mental Health: The Impact on Wellbeing, Disparities, and Future Implications. Community Connection Magazine; 2021. Available from: https://www.baylor.edu/communityconnection/news.php?action=story&story=222809 [Last accessed January 4, 2023].
- 22. Vu M, Makelarski JA, Winslow VA, et al. Racial and ethnic disparities in health-related socioeconomic risks during the early COVID-19 pandemic: A national survey of U.S. women. J Womens Health 2021;30(10):1375–1385; doi: 10.1089/jwh.2021.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Disease Control and Prevention. 2019 BRFSS Survey Data and Documentation. 2022. Available from: https://www.cdc.gov/brfss/annual_data/annual_2019.html [Last accessed: January 4, 2023].
- 24. The Accountable Health Communities Health-Related Social Needs Screening Tool. Center for Medicare & Medicaid Services. Available from: https://innovation.cms.gov/Files/worksheets/ahcm-screeningtool.pdf [Last accessed: April 11, 2023].
- 25. Stanford University. Stanford COVID-19 Survey. 2020. Available from: https://pcrt.stanford.edu/covid [Last accessed: April 11, 2023].
- 26. Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006;166(10):1092–1097; doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 27. Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: Validity of a two-item depression screener. Med Care 2003;41(11):1284–1292; doi: 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- 28. Schuster MA, Stein BD, Jaycox L, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med 2001;345(20):1507–1512; doi: 10.1056/NEJM200111153452024 [DOI] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention. National 2009 H1N1 Flu Survey Questionnaire [2010 Q1]. 2010. Available from: Interpandemic Questionnaire (cdc.gov) [Last accessed: April 11, 2023].
- 30. Choi D, Ota S, Watanuki S. Does cigarette smoking relieve stress? Evidence from the event-related potential (ERP). Int J Psychophysiol 2015;98(3 Pt 1):470–476; doi: 10.1016/j.ijpsycho.2015.10.005 [DOI] [PubMed] [Google Scholar]
- 31. Kim JE, Tsoh JY. Cigarette smoking among socioeconomically disadvantaged young adults in association with food insecurity and other factors. Prev Chronic Dis 2016;13:E08; doi: 10.5888/pcd13.150458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. ParentsTogether Action. Survey Reveals Families in Serious Financial Crisis With Rising Prices and No Monthly Child Tax Credit Payments in Sight. 2022. Available from: https://parentstogetheraction.org/2022/05/10/survey-reveals-families-in-serious-financial-crisis-with-rising-prices-and-no-monthly-child-tax-credit-payments-in-sight/ [Last accessed January 4, 2023].
- 33. Kim-Mozeleski JE, Shaw SJ, Yen IH, et al. A qualitative investigation of the experiences of tobacco use among U.S. adults with food insecurity. Int J Environ Res Public Health 2022;19(12):7424; doi: 10.3390/ijerph19127424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Grafova IB. Financial strain and smoking. J Fam Econ Issues 2011;32:327–340; doi: 10.1007/s10834-011-9247-2 [DOI] [Google Scholar]
- 35. Goldin C. Understanding the Economic Impact of COVID-19 on Women. 2022. Brookings. Available from: https://www.brookings.edu/bpea-articles/understanding-the-economic-impact-of-covid-19-on-women/ [Last accessed: January 4, 2023].
- 36. Widome R, Joseph AM, Hammett P, et al. Associations between smoking behaviors and financial stress among low-income smokers. Prev Med Rep 2015;2:911–915; doi: 10.1016/j.pmedr.2015.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Guan N, Guariglia A, Moore P, et al. Financial stress and depression in adults: A systematic review. PLoS One 2022;17(2):e0264041; doi: 10.1371/journal.pone.0264041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zimmerman FJ, Katon W. Socioeconomic status, depression disparities, and financial strain: What lies behind the income-depression relationship? Health Econ 2005;14(12):1197–1215; doi: 10.1002/hec.1011 [DOI] [PubMed] [Google Scholar]
- 39. Nagawa CS, Fukunaga MI, Faro JM et al. Characterizing pandemic-related changes in smoking over time in a cohort of current and former smokers. Nicotine Tob Res 2023;25(2):203–210; doi: 10.1093/ntr/ntac033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Centers for Disease Control and Prevention. Smoking Cessation: A Report of the Surgeon General. 2022. Available from: https://www.cdc.gov/tobacco/sgr/2020-smoking-cessation/index.html [Last accessed January 4, 2023].
- 41. Kalkhoran S, Berkowitz SA, Rigotti NA, et al. Financial strain, quit attempts, and smoking abstinence among U.S. adult smokers. Am J Prev Med 2018;55(1):80–88; doi: 10.1016/j.amepre.2018.01.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McClave AK, Dube SR, Strine TW, et al. Associations between smoking cessation and anxiety and depression among U.S. adults. Addict Behav 2009;34(6–7):491–497; doi: 10.1016/j.addbeh.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 43. Cook BL, Wayne GF, Kafali EN, et al. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA 2014;311(2):172–182; doi: 10.1001/jama.2013.284985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cooper J, Borland R, McKee SA, et al. Depression motivates quit attempts but predicts relapse: Differential findings for gender from the international tobacco control study. Addiction 2016;111(8):1438–1447; doi: 10.1111/add.13290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nakajima M, al'Absi M. Predictors of risk for smoking relapse in men and women: A prospective examination. Psychol Addict Behav 2012;26(3):633–637; doi: 10.1037/a0027280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Centers for Disease Control and Prevention. Smoking Cessation—The Role of Healthcare Professionals and Health Systems. 2020. Available from: https://www.cdc.gov/tobacco/data_statistics/sgr/2020-smoking-cessation/fact-sheets/healthcare-professionals-health-systems/index.html [Last accessed January 4, 2023].
- 47. McQueen A, Roberts C, Garg R, et al. Specialized tobacco quitline and basic needs navigation interventions to increase cessation among low income smokers: Study protocol for a randomized controlled trial. Contemp Clin Trials 2019;80:40–47; doi: 10.1016/j.cct.2019.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. De Marchis EH, Torres JM, Fichtenberg C, et al. Identifying food insecurity in health care settings: A systematic scoping review of the evidence. Fam Community Health 2019;42(1):20–29; doi: 10.1097/FCH.0000000000000208 [DOI] [PubMed] [Google Scholar]
- 49. Glenn NM, Allen Scott L, Hokanson T, et al. Community intervention strategies to reduce the impact of financial strain and promote financial well-being: A comprehensive rapid review. Glob Health Promot 2021;28(1):42–50; doi: 10.1177/1757975920984182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126(1):e26–e32; doi: 10.1542/peds.2009-3146 [DOI] [PubMed] [Google Scholar]
- 51. Gattu RK, Paik G, Wang Y, et al. The hunger vital sign identifies household food insecurity among children in emergency departments and primary care. Children (Basel) 2019;6(10):107; doi: 10.3390/children6100107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lindau ST, Jagai JS, Abramsohn EM, et al. Unwanted sexual activity among United States women early in the COVID-19 pandemic. Am J Obstet Gynecol 2023;228(2):209..e1–209.e16; doi: 10.1016/j.ajog.2022.09.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kearns NT, Carl E, Stein AT, et al. Posttraumatic stress disorder and cigarette smoking: A systematic review. Depress Anxiety 2018;35(11):1056–1072; doi: 10.1002/da.22828 [DOI] [PubMed] [Google Scholar]
- 54. Froessi LJ, Abdeen Y. The silent pandemic: The pyshcological burden on frontline healthecare workers during COVID-19. Psychiatry J 2021;2021:2906785; doi: 10.1155/2021/2906785. [DOI] [PMC free article] [PubMed] [Google Scholar]