Abstract
Background:
Non-alcoholic fatty liver disease (NAFLD) is the world’s most common etiology of chronic liver disease. In this systematic review and meta-analysis, we estimated the prevalence of NAFLD in the Iranian children and adult population.
Methods:
A comprehensive search of five international databases, including PubMed, ISI/WOS, ProQuest, Scopus, and Google Scholar, was done from inception to Nov 2022. Studies on NAFLD patients and their risk factors were selected for meta-analysis. The quality of the included studies was assessed by The Joanna Briggs Institute (JBI) Critical Appraisal Checklist for cross-sectional, and cohort studies. The heterogeneity between studies was investigated using Cochran test and I2 statistics. Random and fixed effect models were used for heterogenic and non-heterogenic studies, respectively. We used Comprehensive Meta-Analysis version 3 for conducting meta-analysis.
Results:
Twenty studies were finally included. The total prevalence of NAFLD in children, boys, and girls was 6.7% (95% CI: 0.02–0.18), 12.5% (95% CI: 0.04–0.29) and, 10.1% (95% CI: 0.04–0.21), respectively. The total prevalence of NAFLD in obese children, obese boys, and obese girls was 42% (95% CI: 0.18–0.69), 44% (95% CI: 0.13–0.80), and 33 % (95% CI: 0.13–0.62), respectively. The total prevalence of NAFLD in adults was 36.9% (95% CI: 0.31–0.42). The prevalence of NAFLD in men and women was 33.8% (95% CI: 0.27–0.41) and 29.9% (95% CI: 0.21–0.40), respectively.
Conclusion:
NAFLD prevalence in Iranian adults and obese children is considerable; however, data about the children population was insufficient.
Keywords: Epidemiology, Prevalence, Non-alcoholic fatty liver disease, Systematic review, Meta-analysis, Iran
Introduction
Non-alcoholic fatty liver disease (NAFLD) is considered the most common cause of chronic liver disease in the world (1, 2). It is estimated by 2030, NAFLD will become the major cause of liver transplantation (3).
NAFLD is defined as an accumulation of more than 5% fat deposition in liver parenchyma in the absence of other conditions like excess consumption of alcohol (>20 g/day in women, >30 g/day in men), viral and autoimmune hepatitis, use of hepatotoxic drugs and endocrine conditions (4–6). NAFLD is divided into three grades: mild (less than 33% fat accumulation), moderate (between 33% to 66% fat accumulation), and severe (more than 66% fat accumulation) (7).
The prevalence of NAFLD is estimated to be 25% in the world. East and South America are the highest regions, and Africa is the lowest regarding NAFLD prevalence (2). The prevalence of NAFLD in the United States has been steadily increasing over the past 20 years (8, 9). About 1 billion people worldwide and 80–100 million people in the United States are suffering from NAFLD (10, 11). Previous studies have shown not only adults but children and adolescents are also at risk of NAFLD. The prevalence of NAFLD in children is estimated between 5% and 10% (12). A recent meta-analysis study showed the prevalence of NAFLD is 26% in obese children (13). Although NAFLD is a common condition in children, most obese children don’t have NAFLD (12).
Iran is a country with a high prevalence of metabolic conditions. The prevalence of diabetes, metabolic syndrome, and obesity is estimated at 21.1%, 14.1%, and 21.4%, respectively (14–16). A previous meta-analysis reported the prevalence of NAFLD in Iran at 33.9% in 2015 (17). Due to the significant increase of metabolic conditions in the Iranian population in recent years, in this systematic review and meta-analysis, we sought to estimate the epidemiology of NAFLD in the Iranian children and adult population.
Materials and Methods
The current study is a systematic review and meta-analysis of the prevalence of NAFLD in Iran. The Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guideline was admired for study protocol (18).
Inclusion and exclusion criteria
In this systematic review and meta-analysis, studies that met the following criteria were included: English written cross-sectional and cohort studies on children or adult populations with NAFLD. Those studies that their full-text was not available or were not in English were excluded. Also, systematic review, meta-analysis, narrative review, randomized clinical trial, case-control, editorial, commentary studies, and those who did not report the number of patients were excluded from the present study. In addition, studies assessed NAFLD in patients with a specific underlying disease like patients with diabetes mellitus (DM), polycystic ovary syndrome, lean adults, or immunocompromised patients got excluded.
Search strategy
The range of study cases was from the inception until Nov 2022. Two researchers examined five global databases, namely PubMed, ISI/WOS, ProQuest, Scopus, and Google Scholar, in November 2022. They conducted searches using various keywords such as “non-alcoholic fatty liver disease,” “nonalcoholic fatty liver,” “Nonalcoholic Steatohepatitis,” “NAFLD,” “epidemiology,” “prevalence,” “incidence,” “risk factor,” “Iranian population,” and “Iran.”
Quality assessment
The quality assessment of the included studies was conducted by two researchers, E.AS and S.H, independently. They utilized the Joanna Briggs Institute (JBI) Critical Appraisal Checklist specifically designed for cross-sectional and cohort studies. In cases where there were disagreements, a third researcher, F.MG, was involved to reach a final resolution.
Data extraction
The eligible articles were surveyed and data extraction was performed by two independent researchers. The extraction process was conducted in accordance with the objectives of the current systematic review and meta-analysis. The following information was identified and recorded: the first author’s name, year of publication, study location, study type (cross-sectional or cohort), prevalence of NAFLD, study population (adults, obese children, or children), and sample size.
Statistical analysis
The heterogeneity of the study was examined using Cochran’s test (where the significance level was set at P < 0.1) and I2 statistics (where the significance level was set at more than 50%). In cases where heterogeneity was detected, the random-effect model was employed, while the fixed-effect model was utilized for studies without heterogeneity. In addition, the random effect model was used for calculating the pooled prevalence when the number of available studies was less than 5. To assess each study’s effect on pooled effect and heterogeneity, we performed sensitivity analysis. Subgroup analysis was conducted based on three groups of adults, obese children, and children, respectively. Adult people were defined as individuals older than 18 years. Comprehensive meta-analysis (CMA) statistical software version 3 was used for all the analyses of this systematic review and meta-analysis study.
Results
Study Selection
Upon searching all the international databases, a total of 139 articles were initially identified. After removing 24 duplicate articles, 115 unique studies remained. These studies were further screened based on their titles and abstracts, resulting in the exclusion of 61 studies. The remaining studies underwent a full-text review to assess their eligibility criteria, leading to the exclusion of an additional 34 articles. Eventually, 20 articles met the inclusion criteria and were selected for analysis (Fig.1).
Fig. 1:
Flowchart of the included eligible studies in a systematic review
Characteristics of included studies
Table 1 shows the feature of selected studies. Of 20 articles, 12 articles assessed NAFLD in adults (19–29), five studies in obese children (30–34), and three studies in children (35–37). One study was cohort (28), and the remaining were cross-sectional (19–27,29–37). Regarding the quality of included studies, nine studies were considered high (score more than 6 for cross-sectional and more than 9 for cohort studies) (20,24–26,29,31,33,34,36).
Table 1:
Characteristics of included studies
| Author, year (Ref) | Region | Design of study | Prevalence of NAFLD% | Target population | Sample size | Total score |
|---|---|---|---|---|---|---|
| Adibi ,2017 (19) | Isfahan | Cross-sectional | 39.3 | Adult | 483 | 6/8 |
| Adibi,2009 (35) | Isfahan | Cross-sectional | 16.9 | Children | 952 | 6/8 |
| Alavian, 2009 (36) | Tehran | Cross-sectional | 7.1 | Children | 966 | 7/8 |
| Amirkalali,2014 (20) | Amol | Cross-sectional | 43.8 | Adult | 5023 | 8/8 |
| Bagheri Lankarani,2013 (21) | Shiraz | Cross-sectional | 21.5 | Adult | 819 | 6/8 |
| Birjandi,2016 (22) | Kavar | Cross-sectional | 22.4 | Adult | 1,600 | 6/8 |
| Fattahi,2018 (23) | Sanandaj | Cross-sectional | 35.4 | Adult | 410 | 6/8 |
| Honarvar, 2019 (24) | Shiraz | Cross-sectional | 19.8 | Adult | 478 | 8/8 |
| MansourGhanaei, 2018 (25) | Soomehesara | Cross-sectional | 43.5 | Adult | 960 | 8/8 |
| Montazerifar,2014 (30) | Zahedan | Cross-sectional | 44.1 | Obese children | 34 | 6/8 |
| Motamed,2016 (26) | Amol | Cross-sectional | 58.8 | Adult | 5,052 | 7/8 |
| Motamed,2017 (27) | Amol | Cross-sectional | 50.3 | Adult | 2804 | 6/8 |
| Motamed,2020 (28) | Amol | Cohort | 41.8 | Adult | 5797 | 9/11 |
| Namakin,2018 (31) | Birjand | Cross-sectional | 54 | Obese children | 200 | 8/8 |
| Ostovaneh,2015(1) (29) | Amol | Cross-sectional | 42.95 | Adult | 5645 | 8/8 |
| Ostovaneh,2015(2) (29) | Zahedan | Cross-sectional | 31.37 | Adult | 2078 | 5/8 |
| Rafeey,2009 (37) | Tabriz | Cross-sectional | 2.3 | Children | 1500 | 6/8 |
| Saki,2014 (32) | Shiraz | Cross-sectional | 54.9 | Obese children | 102 | 6/8 |
| Taghavi ardakani,2017 (33) | Kashan | Cross-sectional | 59 | Obese children | 200 | 8/8 |
| Gheibi,2019 (34) | Urmia | Cross-sectional | 11 | Obese children | 843 | 8/8 |
Results of heterogeneity
Table 2 demonstrates the heterogeneity of the included studies. Out of the 18 variables analyzed, four variables showed homogeneous results, namely the prevalence of NAFLD grade 2 in children, the prevalence of NAFLD grade 3 in children, the prevalence of NAFLD grade 3 in obese children, and the prevalence of NAFLD grade 3 in adults. However, significant heterogeneity was observed in the results of the remaining variables.
Table 2:
The result of heterogeneity among included studies
| Variables | # of studies | Q value | I2 (%) | P-value | Selected model |
|---|---|---|---|---|---|
| Prevalence of NAFLD in children | 3 | 139.780 | 98.56 | <0.001 | Random |
| Prevalence of NAFLD in boys | 2 | 24.150 | 95.85 | <0.001 | Random |
| Prevalence of NAFLD in girls | 2 | 18.397 | 94.56 | <0.001 | Random |
| Prevalence of NAFLD grade 1 in children | 2 | 35.986 | 97.22 | <0.001 | Random |
| Prevalence of NAFLD grade 2 in children | 2 | 0.180 | 0.00 | 0.67 | Random |
| Prevalence of NAFLD grade 3 in children | 2 | 0.325 | 0.00 | 0.56 | Random |
| Prevalence of NAFLD in obese children | 5 | 272.765 | 98.53 | <0.001 | Random |
| Prevalence of NAFLD in obese boys | 4 | 166.693 | 98.20 | <0.001 | Random |
| Prevalence of NAFLD in obese girls | 4 | 87.920 | 96.58 | <0.001 | Random |
| Prevalence of NAFLD grade 1 in obese children | 5 | 241.622 | 98.34 | <0.001 | Random |
| Prevalence of NAFLD grade 2 in obese children | 5 | 17.658 | 77.34 | <0.001 | Random |
| Prevalence of NAFLD grade 3 in obese children | 5 | 3.990 | 00.0 | 0.40 | Fixed |
| Prevalence of NAFLD in adults | 12 | 1177.730 | 99.06 | <0.001 | Random |
| Prevalence of NAFLD in men | 7 | 115.533 | 94.80 | <0.001 | Random |
| Prevalence of NAFLD in women | 7 | 285.677 | 97.89 | <0.001 | Random |
| Prevalence of NAFLD grade 1 in adults | 3 | 5.766 | 65.31 | 0.05 | Random |
| Prevalence of NAFLD grade 2 in adults | 3 | 6.47 | 69.12 | 0.03 | Random |
| Prevalence of NAFLD grade 3 in adults | 3 | 2.80 | 28.72 | 0.24 | Random |
Results of meta-analysis
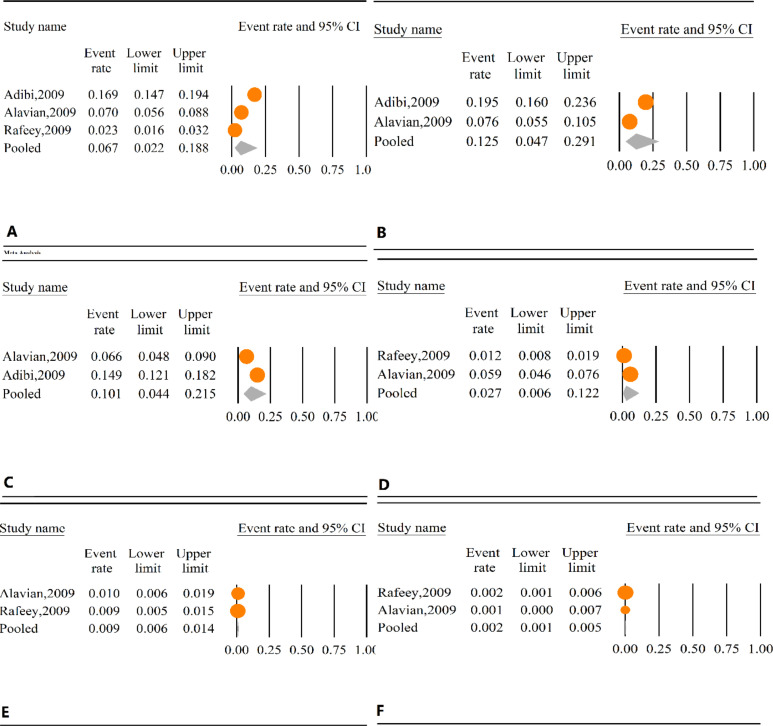
Prevalence of NAFLD in children
Among the studies we included, three studies surveyed the prevalence of NAFLD among children (35–37). The total prevalence of NAFLD among children was 6.7% (95% CI: 0.02–0.18) (Fig. 2A). Two studies also surveyed NAFLD prevalence in boys and girls (35,36). The total prevalence of NAFLD in boys and girls was 12.5% (95% CI: 0.04–0.29) and 10.1% (95% CI: 0.04–0.21), respectively (Fig.2B–C). Based on two studies, the prevalence of NAFLD grade 1, 2, and 3 in children was 2.7% (95% CI: 0.00–0.12), 0.9% (95% CI: 0.00–0.01), and 0.2% (95% CI: 0.001–0.005), respectively (Fig. 2D–F) (36,37). We conducted sensitivity analysis to assess the source of heterogeneity; however, no significant changes were observed after the removal of each study regarding heterogeneity.
Fig. 2:
A: Prevalence of NAFLD in children. B: Prevalence of NAFLD in boys C: Prevalence of NAFLD in girls D: Prevalence of children NAFLD grade 1 E: Prevalence of children NAFLD grade 2 F: Prevalence of children NAFLD grade 3
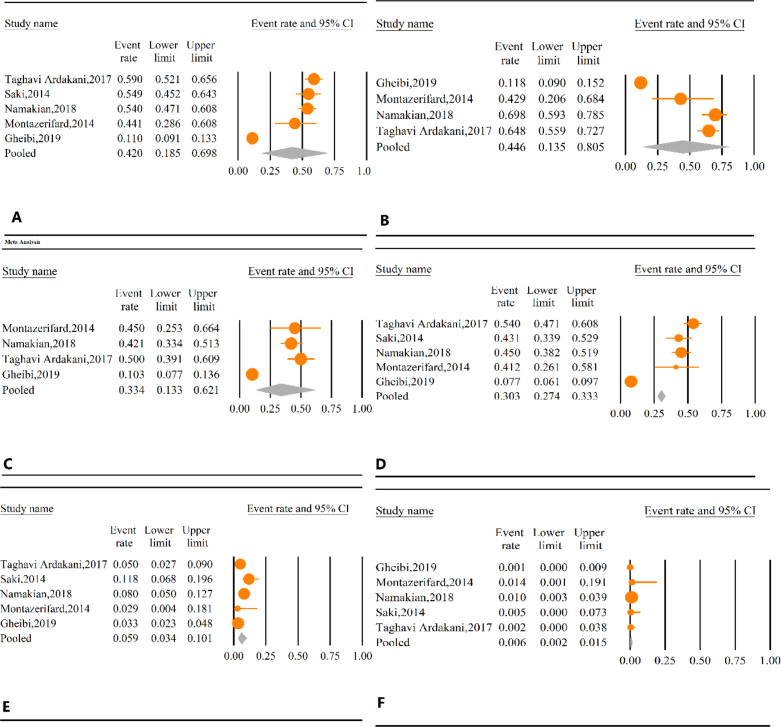
Prevalence of NAFLD in obese children
Five studies searched the prevalence of NAFLD and its grades in obese children (30–34). Four studies also surveyed the NAFLD prevalence in obese boys and girls (30,31,33,34). The total prevalence of NAFLD in obese children, obese boys, and obese girls was 42% (95% CI: 0.18–0.69), 44% (95% CI: 0.13–0.80) and 33 % (95% CI: 0.13–0.62), respectively (Fig.3A–C). The prevalence of NAFLD grade 1, 2, and 3 in obese children was 30% (95% CI: 0.27–0.33), 5.9% (95% CI: 0.03–0.10), and 0.6% (95% CI: 0.00–0.01) respectively (Fig.3D–F). The results of sensitivity analysis showed significant heterogeneity decrease by removal of Gheibi et al. (34) in the prevalence of NAFLD in obese children (I2 0.00%, P =0.40), obese boys (I2 =0.45%, P=0.15), obese girls (I2=0.00%, P=0.55), grade 1 (I2=42%, P=0.16), and grade 2 (I2=44%, P=0.14).
Fig. 3:
A: Prevalence of NAFLD in obese children. B: Prevalence of NAFLD in obese boys C: Prevalence of NAFLD in obese girls D: Prevalence of obese NAFLD grade 1 E: Prevalence of obese NAFLD grade 2 F: Prevalence of obese NAFLD grade 3
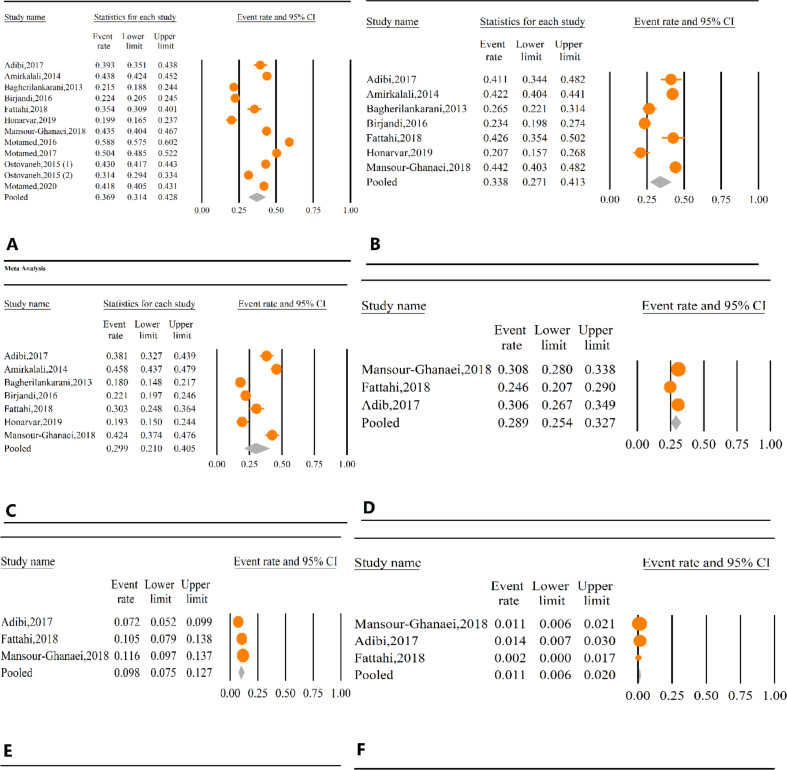
Prevalence of NAFLD in adult
The total prevalence of NAFLD in adults was 36.9% (95% CI: 0.31–0.42). The prevalence of NAFLD in men and women was 33.8% (95% CI: 0.27–0.41) and 29.9% (95% CI: 0.21–0.40), respectively (Fig.4A–C). The prevalence of NAFLD grade 1, 2, and 3 in adults was 28.9% (95% CI: 0.25–0.32), 9.8% (95% CI: 0.07–0.12), and 1.1% (95% CI: 0.00–0.02), respectively (Fig.4D–F). The results of sensitivity analysis showed no significant difference in the total prevalence of NAFLD in adults and the prevalence of NAFLD in men and women; however, by omitting Fattahi et al. (23) and Adibi et al. (19) studies, significant decrease in grade 1 heterogeneity (I2 =0%, P=0.94), and grade 2 heterogeneity (I2 =0%, P=0.56) was observed.
Fig. 4:
A: Prevalence of NAFLD in adult. B: Prevalence of NAFLD in men C: Prevalence of NAFLD in women D: Prevalence of adult NAFLD grade 1 E: Prevalence of adult NAFLD grade 2 F: Prevalence of adult NAFLD grade 3
Discussion
The present study is a systematic review and meta-analysis estimating the prevalence of NAFLD in the Iranian population. In this study, we showed the distribution of NAFLD among children, obese children, and adults. We also showed the prevalence of three grades of this disease and its prevalence in both genders.
In our study, the total prevalence of NAFLD in children was 6.7% in the Iranian population. Other studies reported the prevalence of NAFLD in children between 5% and 10% (12). The Child and Adolescent Liver Epidemiology (SCALE) study reported the prevalence of NAFLD at 9.6% in children aged 2–19 (38). Pediatric NAFLD prevalence was reported at 4.5% in New York City (39). Although the previous studies diagnosed NAFLD by biopsy, all primary studies in our meta-analysis diagnosed NAFLD by ultrasound. A meta-analysis by Anderson et al. estimated the global prevalence of NAFLD in children at 7.6% in 2013, regardless of the method of diagnosis (40).
Based on the result of our study, the prevalence of NAFLD in obese children was 42%, which was almost six-fold higher than children’s NAFLD prevalence. In another study, which surveyed NAFLD among obese children, the prevalence of simple steatosis and NASH were 54.9% and 10.5%, respectively (41). Jimenez-Rivera et al., reported the prevalence of NAFLD at 85% in 97 obese children (42).
The higher NAFLD prevalence in obese children compared to children from the general population was expected due to the close relation between NAFLD and obesity (43). The incidence of pediatric NAFLD has grown significantly from 36 per 100000 persons in 2009 to 58.2 per 100000 persons in 2018, along with the occurrence of the obesity epidemic phenomenon (44). Previous studies surveyed the relationship between NAFLD and other metabolic conditions like insulin resistance, diabetes mellitus, metabolic syndrome, and dyslipidemia (45–49); however, NAFLD in pediatrics is usually asymptomatic, and unspecific symptoms like abdominal pain, fatigue, and concentration difficulties are sometimes present (50). Pediatric NAFLD diagnosis in the early stages of the disease is challenging as most patients are asymptomatic (51, 52). This issue causes the prevalence of NAFLD to be underestimated.
Based on the result of our study, the prevalence of grades 1, 2, and 3 in obese children was 34%, 5.9%, and 0.6%, respectively. These findings imply the progression of NAFLD in obese children. Current knowledge recommends that NAFLD can progress to NASH, described as necroinflammation of the liver (53). NASH can lead to cirrhosis and hepatocellular carcinoma (HCC) (54, 55). The pattern of NAFLD progression in childhood is not understood well. It is unexplored whether NAFLD follows an aggressive pattern, as many children with NAFLD will experience cirrhosis in early adulthood (56).
Based on the results of our study, the prevalence of NAFLD in adults, men, and women was 36.9%, 33.8%, and 29.9%, respectively. The prevalence of NAFLD in Asian countries is estimated at 29.6%, which has risen in recent years (57). In Europe, a recent meta-analysis study showed that the NAFLD prevalence is 26.9% (58). The increasing prevalence of NAFLD in Asian countries like Iran can result from industrialization, improvements in socioeconomic status, sedentary lifestyles, and high-caloric diets (59–62). The prevalence of NAFLD is reported to be higher in urban areas than in rural regions (63–67). The rise in the prevalence of the NAFLD population is accompanied by an increased prevalence of obesity in Asian countries (68, 69). In addition, Asian people are more amenable to obesity complications even with similar body mass index (BMI) as their Western equivalents (70).
Limitations
There were several limitations in our study. The number of studies surveyed NAFLD in children and obese children was low, and we recommend conducting more studies among these patients. In addition, data still need to be included for some provinces of Iran. High heterogeneity was observed among studies, and random-effect model was used for the analysis; hence the results should be interpreted cautiously.
Conclusion
We showed a high prevalence of NAFLD among the Iranian population. Our meta-analysis also showed a higher prevalence of NAFLD in adults compared to global prevalence. This is an alarm sign for us to consider this disease more serious than past. Governments should establish screening protocols in society to prevent the consequent complications and decrease the disease’s burden. People also should change their sedentary lifestyle and have aerobic exercises.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
Not Applicable.
Footnotes
Funding
None.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflict of interest
The authors declare that they have no competing interest.
References
- 1.Bellentani S, Marino M. (2009). Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD). Ann Hepatol, 8 (Supp 1):S4–S8. [PubMed] [Google Scholar]
- 2.Younossi ZM, Koenig AB, Abdelatif D, et al. (2016). Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology, 64(1):73–84. [DOI] [PubMed] [Google Scholar]
- 3.Byrne CD, Targher G. (2015). NAFLD: a multisystem disease. J Hepatol, 62(1 Suppl):S47–64. [DOI] [PubMed] [Google Scholar]
- 4.Aller R, Izaola O, Gómez S, et al. (2015). Effect of silymarin plus vitamin E in patients with non-alcoholic fatty liver disease. A randomized clinical pilot study. Eur Rev Med Pharmacol Sci, 19(16): 3118–24. [PubMed] [Google Scholar]
- 5.Westfall E, Jeske R, Bader AR. (2020). Nonalcoholic Fatty Liver Disease: Common Questions and Answers on Diagnosis and Management. Am Fam Physician, 102(10): 603–12. [PubMed] [Google Scholar]
- 6.Kneeman JM, Misdraji J, Corey KE. (2012). Secondary causes of nonalcoholic fatty liver disease. Therap Adv Gastroenterol, 5(3): 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bedossa P. (2017). Pathology of non-alcoholic fatty liver disease. Liver Int, 37 (Suppl 1): 85–9. [DOI] [PubMed] [Google Scholar]
- 8.Vernon G, Baranova A, Younossi ZM. (2011). Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther, 34(3): 274–85. [DOI] [PubMed] [Google Scholar]
- 9.Younossi ZM, Stepanova M, Afendy M, et al. (2011). Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol, 9(6):524–30. [DOI] [PubMed] [Google Scholar]
- 10.Loomba R, Sanyal AJ. (2013). The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol, 10(11): 686–90. [DOI] [PubMed] [Google Scholar]
- 11.Perumpail BJ, Khan MA, Yoo ER, et al. (2017). Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol, 23(47): 8263–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu EL, Schwimmer JB. (2021). Epidemiology of Pediatric Nonalcoholic Fatty Liver Disease. Clin Liver Dis (Hoboken), 17(3): 196–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu EL, Golshan S, Harlow KE, et al. (2019). Prevalence of Nonalcoholic Fatty Liver Disease in Children with Obesity. J Pediatr, 207: 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazloomzadeh S, Rashidi Khazaghi Z, Mousavinasab N. (2018). The Prevalence of Metabolic Syndrome in Iran: A Systematic Review and Meta-analysis. Iran J Public Health, 47(4): 473–80. [PMC free article] [PubMed] [Google Scholar]
- 15.Mirzaei M, Rahmaninan M, Mirzaei M, et al. (2020). Epidemiology of diabetes mellitus, pre-diabetes, undiagnosed and uncontrolled diabetes in Central Iran: results from Yazd health study. BMC Public Health, 20(1): 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaisi-Raygani A, Mohammadi M, Jalali R, et al. (2019). The prevalence of obesity in older adults in Iran: a systematic review and meta-analysis. BMC Geriatr, 19(1): 371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moghaddasifar I, Lankarani KB, Moosazadeh M, et al. (2016). Prevalence of Non-alcoholic Fatty Liver Disease and Its Related Factors in Iran. Int J Organ Transplant Med, 7(3): 149–60. [PMC free article] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ, 339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adibi A, Maleki S, Adibi P, et al. (2017). Prevalence of nonalcoholic fatty liver disease and its related metabolic risk factors in Isfahan, Iran. Adv Biomed Res, 6: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amirkalali B, Poustchi H, Keyvani H, et al. (2014). Prevalence of non-alcoholic fatty liver disease and its predictors in north of Iran. Iran J Public Health, 43(9): 1275– 83. [PMC free article] [PubMed] [Google Scholar]
- 21.Lankarani KB, Ghaffarpasand F, Mahmoodi M, et al. (2013). Non alcoholic fatty liver disease in southern Iran: a population based study. Hepat Mon, 13(5): e9248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Birjandi M, Ayatollahi SM, Pourahmad S, et al. (2016). Prediction and Diagnosis of Non-Alcoholic Fatty Liver Disease (NAFLD) and Identification of Its Associated Factors Using the Classification Tree Method. Iran Red Crescent Med J, 18(11): e32858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fattahi N, Sharifi K, Moradi G, et al. (2018). Prevalence of non-alcoholic fatty liver disease in Kurdistan province, Iran, 2013–2014: a population based study. Govaresh, 23(2): 107–13. [Google Scholar]
- 24.Honarvar B, Bagheri Lankarani K, Keshani P, et al. (2017). Dietary determinants of non-alcoholic fatty liver disease in lean and non-lean adult patients: a population-based study in shiraz, southern Iran. Hepat Mon, 17(4): e12295. [Google Scholar]
- 25.Mansour-Ghanaei R, Mansour-Ghanaei F, Naghipour M, et al. (2018). The role of anthropometric indices in the prediction of non-alcoholic fatty liver disease in the PERSIAN Guilan Cohort study (PGCS). J Med Life, 11(3): 194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Motamed N, Maadi M, Sohrabi M, et al. (2016). Rural residency has a protective effect and marriage is a risk factor for NAFLD. Hepat Mon, 16(7): e38357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Motamed N, Rabiee B, Poustchi H, et al. (2017). Non-alcoholic fatty liver disease (NAFLD) and 10-year risk of cardiovascular diseases. Clin Res Hepatol Gastroenterol, 41(1):31–8. [DOI] [PubMed] [Google Scholar]
- 28.Motamed N, Khoonsari M, Panahi M, et al. (2020). The incidence and risk factors of non-alcoholic fatty liver disease: A cohort study from Iran. Hepat Mon, 20(2):98531. [Google Scholar]
- 29.Ostovaneh MR, Zamani F, Ansari-Moghaddam A, et al. (2015). Nonalcoholic fatty liver: the association with metabolic abnormalities, body mass index and central obesity—a population-based study. Metabolic Syndrome and Related Disorders,13(7):304–11. [DOI] [PubMed] [Google Scholar]
- 30.Montazerifar F, Karajibani M, Moghaddam AR. (2014). Relationship between fatty liver disease and biochemical. Rawal Medical J, 39(1): 15–18. [Google Scholar]
- 31.Namakin K, Hosseini M, Zardast M, et al. (2017). Prevalence of non-alcoholic fatty liver disease (NAFLD) and its clinical characteristics in overweight and obese children in the south east of Iran. Hepat Mon, 18(12):e83525. [Google Scholar]
- 32.Saki F, Karamizadeh Z. (2014). Metabolic syndrome, insulin resistance and Fatty liver in obese Iranian children. Iran Red Crescent Med J, 16(5): e6656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.TAGHAVI AA, Sharif MR, Kheirkhah D. (2015). Fatty liver disease in obese children in Kashan, Iran. Caspian Journal of Pediatrics,1(1): 17–21. [Google Scholar]
- 34.Gheibi S, Maleki F, Safiri S, et al. (2019). Prevalence and Predictors of Non-Alcoholic Fatty Liver Disease in Obese and Overweight Children in the Northwest of Iran. Hepat Mon, 19(10):e92199. [Google Scholar]
- 35.Adibi A, Kelishadi R, Beihaghi A, et al. (2009). Sonographic fatty liver in overweight and obese children, a cross sectional study in Isfahan. Endokrynol Pol, 60(1): 14–9. [PubMed] [Google Scholar]
- 36.Alavian SM, Mohammad-Alizadeh AH, Esna-Ashari F, et al. (2009). Non-alcoholic fatty liver disease prevalence among school-aged children and adolescents in Iran and its association with biochemical and anthropometric measures. Liver Int, 29(2): 159–63. [DOI] [PubMed] [Google Scholar]
- 37.Rafeey M, Mortazavi F, Mogaddasi N, et al. (2009). Fatty liver in children. Ther Clin Risk Manag, 5(2):371–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwimmer JB, Deutsch R, Kahen T, et al. (2006). Prevalence of fatty liver in children and adolescents. Pediatrics, 118(4):1388–93. [DOI] [PubMed] [Google Scholar]
- 39.Fernandes DM, Pantangi V, Azam M, et al. (2018). Pediatric Nonalcoholic Fatty Liver Disease in New York City: An Autopsy Study. J Pediatr, 200: 174–80. [DOI] [PubMed] [Google Scholar]
- 40.Anderson EL, Howe LD, Jones HE, et al. (2015). The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS One, 10(10):e0140908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peng L, Wu S, Zhou N, et al. (2021). Clinical characteristics and risk factors of nonalcoholic fatty liver disease in children with obesity. BMC Pediatr, 21(1):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jimenez-Rivera C, Hadjiyannakis S, Davila J, et al. (2017). Prevalence and risk factors for non-alcoholic fatty liver in children and youth with obesity. BMC Pediatr, 17(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fabbrini E, Sullivan S, Klein S. (2010). Obesity and nonalcoholic fatty liver disease: biochemical, metabolic, and clinical implications. Hepatology, 51(2):679–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sahota AK, Shapiro WL, Newton KP, et al. (2020). Incidence of nonalcoholic fatty liver disease in children: 2009–2018. Pediatrics, 146(6): e20200771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tomah S, Alkhouri N, Hamdy O. (2020). Nonalcoholic fatty liver disease and type 2 diabetes: where do Diabetologists stand? Clin Diabetes Endocrinol, 6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kitade H, Chen G, Ni Y, et al. (2017). Nonalcoholic Fatty Liver Disease and Insulin Resistance: New Insights and Potential New Treatments. Nutrients, 9(4): 387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paschos P, Paletas K. (2009). Non alcoholic fatty liver disease and metabolic syndrome. Hippokratia, 13(1): 9–19. [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang QQ, Lu LG. (2015). Nonalcoholic Fatty Liver Disease: Dyslipidemia, Risk for Cardiovascular Complications, and Treatment Strategy. J Clin Transl Hepatol, 3(1):78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Naghipour M, Joukar F, Salehi EA, et al. (2022). The association between age at first pregnancy and number of deliveries with metabolic syndrome and its components: Results from Persian Guilan Cohort Study (PGCS). Iran J Obstet Gynecol Infertil, 25(6):1–11. [Google Scholar]
- 50.Nobili V, Alisi A, Valenti L, et al. (2019). NAFLD in children: new genes, new diagnostic modalities and new drugs. Nat Rev Gastroenterol Hepatol, 16(9):517–30. [DOI] [PubMed] [Google Scholar]
- 51.Mencin AA, Lavine JE. (2011). Advances in pediatric nonalcoholic fatty liver disease. Pediatr Clin North Am, 58(6):1375–92. [DOI] [PubMed] [Google Scholar]
- 52.Vajro P, Lenta S, Socha P, et al. (2012). Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr, 54(5):700–13. [DOI] [PubMed] [Google Scholar]
- 53.Brunt EM. (2010). Pathology of nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol, 7(4):195–203. [DOI] [PubMed] [Google Scholar]
- 54.Sheka AC, Adeyi O, Thompson J, et al. (2020). Nonalcoholic Steatohepatitis: A Review. JAMA, 323(12):1175–83. [DOI] [PubMed] [Google Scholar]
- 55.Anstee QM, Reeves HL, Kotsiliti E, et al. (2019). From NASH to HCC: current concepts and future challenges. Nat Rev Gastroenterol Hepatol, 16(7):411–28. [DOI] [PubMed] [Google Scholar]
- 56.Nobili V, Alisi A, Newton KP, et al. (2016). Comparison of the phenotype and approach to pediatric vs adult patients with nonalcoholic fatty liver disease. Gastroenterology, 150(8): 1798–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li J, Zou B, Yeo YH, et al. (2019). Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol, 4(5): 389–98. [DOI] [PubMed] [Google Scholar]
- 58.Cholongitas E, Pavlopoulou I, Papatheodoridi M, et al. (2021). Epidemiology of nonalcoholic fatty liver disease in Europe: a systematic review and meta-analysis. Ann Gastroenterol, 34(3): 404–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Younossi Z, Anstee QM, Marietti M, et al. (2018). Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol, 15(1):11–20. [DOI] [PubMed] [Google Scholar]
- 60.Rayyan YM, Tayyem RF. (2018). Non-alcoholic fatty liver disease and associated dietary and lifestyle risk factors. Diabetes Metab Syndr, 12(4): 569–75. [DOI] [PubMed] [Google Scholar]
- 61.Wong S-W, Chan W-K. (2020). Epidemiology of non-alcoholic fatty liver disease in Asia. Indian J Gastroenterol, 39(1): 1–8. [DOI] [PubMed] [Google Scholar]
- 62.Khosousi MJ, Mansour-Ghanaei F, Heidarzad F, et al. (2022). Epidemiologic Profile of Microscopic Hematuria in Iran: A Systematic Review and Meta-Analysis. Iran J Public Health, 51(10): 2194–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Amarapurkar D, Kamani P, Patel N, et al. (2007). Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol, 6(3): 161–3. [PubMed] [Google Scholar]
- 64.Singh SP, Nayak S, Swain M, et al. (2004). Prevalence of nonalcoholic fatty liver disease in coastal eastern India: a preliminary ultrasonographic survey. Trop Gastroenterol, 25(2): 76–9. [PubMed] [Google Scholar]
- 65.Mohan V, Farooq S, Deepa M, et al. (2009). Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res Clin Pract, 84(1): 84–91. [DOI] [PubMed] [Google Scholar]
- 66.Das K, Das K, Mukherjee PS, et al. (2010). Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology, 51(5): 1593–602. [DOI] [PubMed] [Google Scholar]
- 67.Chen ZW, Chen LY, Dai Hl, et al. (2008). Relationship between alanine aminotransferase levels and metabolic syndrome in nonalcoholic fatty liver disease. J Zhejiang Univ Sci B, 9(8): 616–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Asrani SK, Devarbhavi H, Eaton J, et al. (2019). Burden of liver diseases in the world. J Hepatol, 70(1): 151–171. [DOI] [PubMed] [Google Scholar]
- 69.Wong SW, Chan WK. (2020). Epidemiology of non-alcoholic fatty liver disease in Asia. Indian J Gastroenterol, 39(1): 1–8. [DOI] [PubMed] [Google Scholar]
- 70.Consultation WE. (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet, 363(9403): 157–63. [DOI] [PubMed] [Google Scholar]