Abstract
Objective:
To identify which strain episodes are concurrently reported by several team members; to identify triggers of strain experienced by operating room (OR) team members during the intraoperative phase.
Summary:
OR teams are confronted with many sources of strain. However, most studies investigate strain on a general, rather than an event-based level, which does not allow to determine if strain episodes are experienced concurrently by different team members.
Methods:
We conducted an event-based, observational study, at an academic medical center in North America and included 113 operations performed in 5 surgical departments (general, vascular, pediatric, gynecology, and trauma/acute care). Strain episodes were assessed with a guided-recall method. Immediately after operations, participants mentally recalled the operation, described the strain episodes experienced and their content.
Results:
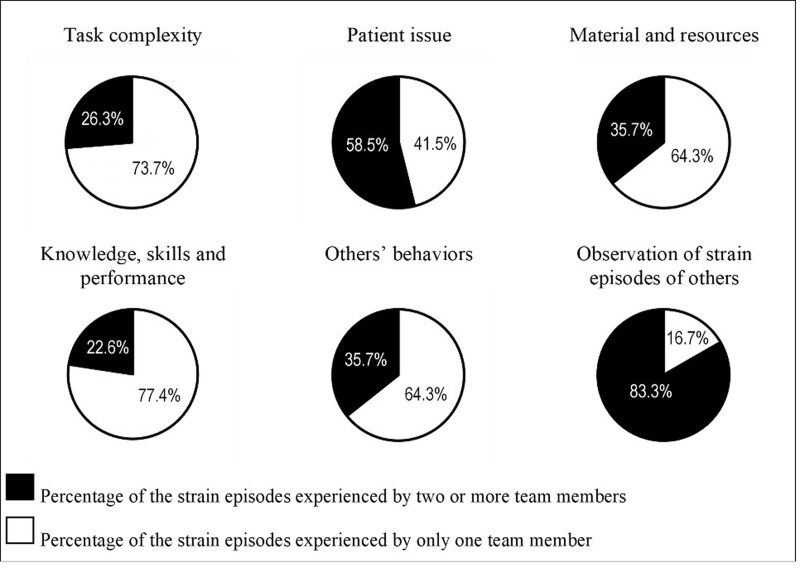
Based on 731 guided recalls, 461 strain episodes were reported; these refer to 312 unique strain episodes. Overall, 75% of strain episodes were experienced by a single team member only. Among different categories of unique strain episodes, those triggered by task complexity, issues with material, or others’ behaviors were typically experienced by 1 team member only. However, acute patient issues (n = 167) and observations of others’ strain (n = 12) (respectively, 58.5%; P < 0.001 and 83.3%; P < 0.001) were often experienced by 2 or more team members.
Conclusions and relevance:
OR team members are likely to experience strain alone, unless patient safety is at stake. This may jeopardize the building of a shared understanding among OR team members.
Keywords: affective linkage, emotional contagion, operating room, strain, stress, teamwork
Mini-Abstract: OR teams are confronted to a variety of strain sources. However, experiences of strain are not concordant within the team members, since 75% of strain episodes are experienced by only 1 team member. Exceptions are strain episodes related to patient issues, likely to be experienced by several team members concurrently.
Members of operating room (OR) teams are exposed to multiple stressors as part of their daily work in the OR. Stressors can elicit strain, defined as stress reactions.1 The impact of strain can affect both patient safety (eg, the surgeons’ hands are shaking)2 and team members satisfaction at work.3–5
Since OR teams members collaborate very closely in a small space and have a common goal, one could expect that team members often experience strain episodes concurrently. If a team member experiences a particular strain, there may be contagion to the rest of the team, defined as the transmission (“infection”) of emotions from 1 person or group to another person or group.6 This process is observed in teams at work, including in OR teams7: either, emotional contagion can occur based on a shared or similar perception and interpretation of a stressful situation by multiple team members (convergent linkage); or, the strain experienced by 1 team member can be perceived by another team members and act as stimulus (complementary linkage).6 The strain of a leader (eg, the main surgeon) may be particularly likely to spread to the rest of the team,7 but contagion may also be a bidirectional process, with the emotional states of team members also having the potential to influence the leaders.8
The spread of negative emotions related to strain episodes in the OR can have detrimental consequences, as multiple team members, instead of 1, may simultaneously experience negative emotions.7 However, the shared experience of negative emotions in stressful situations may also be adaptative, as it can foster appropriate actions by the team in response to the the stress inducing situation. In this case, emotional contagion may be an indicator of shared situation awareness, which refers to a shared understanding of the situation and its development—an important nontechnical skill9 that can help prevent surgical errors.10
Different types of strain may be experienced during an operation and may be convergent, complementary or have no linkage within the OR team. In a literature review, Arora and colleagues found that important sources of intraoperative strain can be task-related issues and situations where patient safety was directly at stake (eg, bleeding) but also distractions and social stressors.11 These stressors may be particularly contagious within the team.
Most previous studies measured stress on a general level (eg, for the whole team or the whole duration of the operation) or, in simulation settings, stress was induced only for specific team members.11 Thus, most studies did not assess specific strain episodes for individual team members during the operation and were thus unable to identify to what extent strain was contagious among OR teams.
The main goal of this study was to assess concordant strains, that is, to what extent members of an OR team experience and report the same strain episodes during operations. The second goal of our study was to identify the nature of strain episodes reported among individual team members and to assess if different types of strain are particularly contagious.
METHODS
Data of this event-based observational study were collected as part of a larger research project that aimed to better understand strain episodes in the OR. Our prior research related to the same operations found that the experience of strain episodes was different for different phases of the operation, different professional groups, and types of procedures.12 The objective of the analyses presented in this study was to test to what extent different types of strain episodes are experienced concurrently by different members of the OR team.
Setting and Recruitment
The study was conducted at 1 medium-size (700 beds), rural teaching hospital in the United States. The study was conducted at this specific hospital because of an ongoing collaboration of the study center team with the hospital and its convenient proximity to the the study center. The study period was between August 2018 and January 2019, with a 2-week break in October 2018 to accommodate holidays.
As part of the recruitment process, 53 surgeons were contacted via an open invitation to participate. Operations of 15 of the 17 surgeons who responded positively were included. In addition, we contacted 10 surgeons directly who had not responded to our initial invitation. All 10 surgeons agreed to participate.
Sample
The sample consisted in a total of 113 general (eg, hernia, colostomy, and cholecystectomy), vascular (eg, aneurysm repair and leg amputation), pediatric (eg, hernia and colostomy), gynecology (eg, salpingectomy and hysterectomy), and trauma/acute care operations (eg, explorative laparotomy and liver laceration repair). Thirty-one of the operations were laparoscopically assisted and 6 were robotic; 23 operations were performed by trauma/acute care surgeons. We used a convenience sampling procedure, selecting operations based on the OR planning tool and the availability of the research team for guided-recall data collection. Days and nights dedicated to data collection were designated each week, taking into account the research team’s other professional or private commitments. Operations performed during these designated time periods were included, independently of their duration or complexity. No a-priory stratification based on characteristics of the operation was performed.
Procedure
Before the start of data collection, the research team conducted information sessions with all surgical, anesthesiology, and nursing teams as well as residents and medical students in the departments involved in the study. In these sessions, included at weekly meetings, the study’s objectives were presented and questions were addressed. An information e-mail was also sent to all team members. In the presentation and mail, team members were informed that they would be asked to fill out guided recalls, and it was emphasized that team members could decline participation at any time when approached by a researcher.
Guided-recall data were collected immediately after the operations: every member of the OR team was invited to complete a guided recall reporting their moments of strain. Team members who were not immediately available typically filled out the guided recall within 40 minutes, after finishing their operation-related tasks such as cleaning the materials in the room or handing over the patient to the postanesthesia care unit. We also included team members present only during a part of the operation due to breaks or shift change. Consent to participate was obtained through verbal opt in. This study was reviewed and approved by the local institutional review board (#2524); participants did not receive any incentive.
Measures
Measure of Strain Episodes and Their Triggers
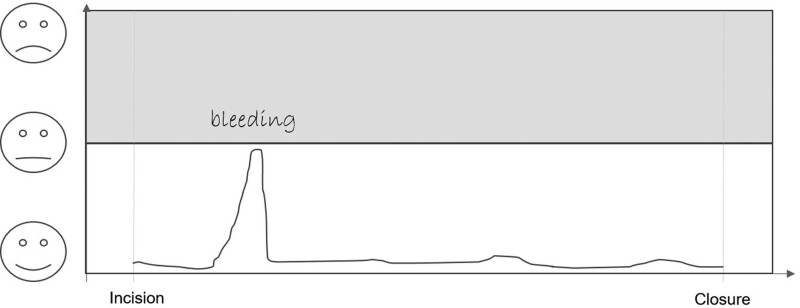
The study used guided recall to collect data on the strain episodes experienced by the participants. Immediately after the operation, a member of the research team handed the paper and pencil guided-recall questionnaire to each person present during the operation. It included an empty drawing, with the x axis representing the time of the operation and the y axis representing strain level (see Figure 1 for an example). OR team members were asked to draw a continuous line that represented their “tension” level during the operation and to draw any tense moment they experienced as bumps. We considered a strain episode every time there was a bump in the line, independently of its magnitude. For each strain episode drawn, the researcher asked the participant to describe the episode and its content, either by writing a comment or as a verbal description, the latter were audio recorded or summarized by the researcher. Team members could not see each other’s episodes reported.
FIGURE 1.
Example of a guided recall of strain episodes during an operation (surgeon).12
Data Preparation: Identifying Different Categories of Strain Episodes
Based on the descriptions, we content coded the trigger of each strain episode and matched strain episodes reported by several team members for each operation.
Content Coding of Strain Episodes
. We identified categories of strain episodes reported using an inductive-deductive approach. In a first step, one of the researcher (SK) identified the categories based on all the material collected but not blind to previous work in the domain. In a second step, a second researcher (VZ) was instructed how to use the categories and, accordingly, coded a subsample of strain episodes. Then, both researchers discussed the problems met and adapted or specified the definition of the categories where needed. Once appropriate agreement was reached, all strain episodes were then categorized independently by 2 coders.
The categories, their definition, and typical examples are described in Table 1. A given strain episode could be classified into 1 or maximal 2 different categories. An example of a strain episode included in 2 categories was a surgeon who had to wait for a computer to reboot to make a device work during a complex phase of an operation (coded as issues with material and resources and task complexity).
TABLE 1.
Description of the Categorization of the Triggers of the Strain Episodes Reported
| Category | Description | Examples |
|---|---|---|
| Task complexity | Tasks reported as particularly difficult. | Dissection of the right hernia sac. Shift change for OR staff |
| Patient acute issue | Potential acute event with the patient care that required a rapid action from the team. | Bleeding, problems with the oxygenation. |
| Material and resources | Pieces of material or other resources such as drugs were missing, not adequate or out of order. | A piece of equipment is missing and a nurse has to find it in the material storage. |
| Knowledge, skills, and performance | The person reporting or another team member did not know how to do something, how to use an instrument, or was critical towards his/her own performance during the operation. | The resident does not know how to use an instrument. |
| Others’ behaviors | Behaviors of other team members reported as a source of strain. | The staff are noisy, someone is late, someone yelled. |
| Observation of others’ strain | The participant observed that another team member was experiencing strain. | The medical student reports that the surgeon was stressed during the middle part of the operation. |
Matching of Strain Episodes Across Team Members.
Based on the description and the temporal location within the operation, we identified and matched episodes reported by more than 1 team member. In an excel file, we pooled and compared all the strain episodes reported for each operation separately; the description of the strain episodes were good enough to allow a straightforward identification of reported episodes referring to the same event. An example from the data is the surgery resident describing a strain episode as “when came closer to aneurysm and bleeding,” the surgeon “This… was when we opened up the large aneurysm and there is some continued bleeding so we had to work expediently to control that any further bleeding. That was basically it” and the anesthesiologist: “acute blood loss” during about the same phase of the operation. These 3 reports were categorized as referring to a same event. However, in the case the anesthesiologist was the only team member describing “low blood pressure” toward the end of the operation, it was classified as not concordant with any other team member. With only few exceptions (eg, observation of another team member’s strain), the reported strain episodes referring to the same event belonged to the same content-coded category.
Quantifying the Magnitude of the Strain Episodes.
Based on the participants’ drawings of the strain episodes, we measured, in centimeters, the distance between the bottom of the y axis and the top of each strain bumps.
Analyses
We performed a univariate ANOVA to compare the prevalence of strain episodes related to different trigger categories across professional groups; comparisons between professional groups were calculated based on Bonferroni corrected post hoc tests. Multilevel binary logistic regression analyses were performed to assess the likelihood of the strain episodes related to each category of strain to be experienced concurrently by different team members. In an additional analysis, the same statistical test was used to assess to what extent the magnitude of the strain episodes drawn by the OR team members related to the reporting of the strain episode by different team members. Analyses were performed with IBM SPSS version 25.
An additional descriptive analysis was performed to identify which were the professional groups most likely to experience strain episodes concurrently. For each professional group separately, we thus calculated the percentages of the strain episodes experienced concurrently with a member of another professional group. We used the software Cytoscape version 3.8.0 to visualize the percentage of strain episodes shared across the different professional groups.13
RESULTS
We analyzed 731 guided recalls completed during 113 operations. A total of 244 different OR team members (3 individuals declined) participated and filled out between 1 and 14 guided recalls. Three operations were included even if one of the team members refused to participate, since this happened very rarely and in each case, all other team members had agreed to participate.
Triggers of the Strain Episodes
A total of 461 strain episodes were reported. At least 1 strain episode was reported in 106 (94%) of the operations; the mean number of episodes reported per participant was 0.6. The 461 strain episodes represent 312 unique events.
Audio-recorded descriptions were available for 156 strain episodes and a written description was available for 212 strain episodes, in addition or in place of the audio recordings. The research team summarized the verbal description of the OR team member for 107 strain episodes. Fifty-one strain episodes were classified into 2 trigger categories (see Table 1), giving a total of 512 triggers of strain episodes. Inter-rater reliability for the different categories of strain ranged from Cohen’s Kappa 0.74 to 0.79, indicating good inter-rater agreement.
Table 1 shows the classification of the strain episodes per trigger category.
Table 2 displays the frequency and percentage of each strain category across the different professional groups; post hoc analysis showing the differences across the professional groups is displayed in Supplemental Digital Content 1, http://links.lww.com/AOSO/A249. Surgeons and residents were more likely to report task complexity as a trigger of strain in comparison to scrub technicians [for surgeons mean (SD) difference = 0.50 (0.08), 95% CI = 0.26–0.74, P < 0.001, and for residents mean (SD) difference = 0.43 (0.08), 95% CI = 0.19–0.67, P < 0.001] and circulators [for surgeons mean (SD) difference = 0.35 (0.08), 95% CI = 0.11–0.58, P < 0.001, and for residents mean(SD) difference = 0.28 (0.08), 95% CI = 0.04–0.51, P = 0.008). Surgeons, but not residents, were more likely than anesthetists to report task complexity as a trigger of strain [mean (SD) difference = 0.26 (0.08), 95% CI = 0.02–0.51, P = 0.027]. Patient issues as triggers were more often reported by anesthetists than scrub technicians [mean (SD) difference = 0.15 (0.04), 95% CI = 0.02–0.27, P = 0.010] and circulators [mean (SD) difference = 0.13 (0.04), 95% CI = 0.01–0.26, P = 0.024]. Medical students experienced more strain episodes related to their own knowledge, skills, or performance than circulators [mean (SD) difference = 0.20 (0.06), 95% CI = 0.03–0.37, P = 0.007] and medical students were more likely to observe others’strain compared with surgeons [mean (SD) difference = 0.10 [0.03], 95% CI = 0.02–0.17, P = .003], residents [mean (SD) difference = 0.08 (0.03), 95% CI = 0.00–0.16, P = 0.027], and scrub technicians [mean (SD) difference = 0.10 (0.03), 95% CI = 0.02–0.17, P = 0.002].
TABLE 2.
Number and Within Profession Percentages of Strain Episodes Per Professional Group and Categories
| Task Complexity | Patient Issue | Tools and Resources | Knowledge, Skills, and Performance | Others’ Behaviors | Observation of Others’ Strain | Other | Missing | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N* | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | ||
| Surgeons (n = 107) | 62 | 49.60 | 15 | 12.00 | 16 | 12.80 | 15 | 12.00 | 11 | 8.80 | 0 | 0.00 | 5 | 4.00 | 1 | 0.80 | 125 |
| Residents† (n = 116) | 59 | 52.21 | 16 | 14.16 | 6 | 5.31 | 13 | 11.50 | 5 | 4.42 | 2 | 1.77 | 8 | 7.08 | 4 | 3.54 | 113 |
| Students (n = 51) | 17 | 34.69 | 3 | 6.12 | 3 | 6.12 | 11 | 22.45 | 5 | 10.20 | 5 | 10.20 | 3 | 6.12 | 2 | 4.08 | 49 |
| Scrub techs (n = 128) | 10 | 18.52 | 3 | 5.56 | 12 | 22.22 | 12 | 22.22 | 11 | 20.37 | 0 | 0.00 | 1 | 1.85 | 5 | 9.26 | 54 |
| Circulators (n = 137) | 32 | 37.65 | 5 | 5.88 | 16 | 18.82 | 2 | 2.35 | 18 | 21.18 | 4 | 4.71 | 4 | 4.71 | 4 | 4.71 | 85 |
| Anesthetists (n = 117) | 37 | 41.11 | 20 | 22.22 | 5 | 5.56 | 10 | 11.11 | 6 | 6.67 | 3 | 3.33 | 2 | 2.22 | 7 | 7.78 | 90 |
| Other professions‡ (n = 36) | 4 | 40.00 | 2 | 20.00 | 2 | 20.00 | 1 | 10.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 10.00 | 10 |
| Total | 221 | 42.02 | 64 | 12.17 | 60 | 11.41 | 64 | 12.17 | 56 | 10.65 | 14 | 2.66 | 23 | 4.37 | 24 | 4.56 | 526 |
| Statistically Significant differences of professional groups§ | Surg>Scrub | Anesth>Scrub | Stud>Circul | Stu>Surg | |||||||||||||
| Surg>Circul | Anesth>Circul | Stu>Res | |||||||||||||||
| Surg>Anesth | Stu>Scrub | ||||||||||||||||
| Res>Scrub | |||||||||||||||||
| Res>Circul Anesth>Scrub |
|||||||||||||||||
N refers to the number of strain episodes for this profession.
Residents are surgery residents.
‡Other professions (students observing the operation, nurse assistants, and x ray techs) were excluded from the comparison between professions.
Based on post hoc tests, we compare the frequency of each category of strain episodes across the different professional groups (see Supplemental Digital Content 1, http://links.lww.com/AOSO/A249, for the details on the post hoc analyses).
Are the Same Strain Episodes Reported by More Than 1 OR Team Member?
When considering strain episodes reported across team members of each operation, a total of 312 different episodes were identified. Among these, most (75.3%) were reported by 1 team member only (n = 235), 48 were reported concurrently by 2 team members and 29 were reported by 3 or more team members.
Results (Table 3) show that episodes related to patient issues were significantly more likely to be reported by more than 1 team member. Patient issues were 6 times more likely to be experienced by 2 or more team members than to be experienced by 1 single team member. Not surprisingly, observations of strain of other team member was also clearly (17 times) more likely to be experienced by at least 2 team members. For all other categories, a strain episode was predominantly reported by 1 team member only. Figure 2 provides a graphical representation of the proportion of strain episodes experienced by one versus several members of the OR team for each category of strain.
TABLE 3.
Two Level Logistic Regression Model Predicting Strain Episodes Experienced Concurrently by 2 or More Team Members versus by 1 Team Member Only (n = 312 Strain Episodes, Nested in 106 Operations)
| Unadjusted Model | Adjusted Model* | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P | Odds ratio | 95% CI | P | |
| Task complexity | 1.19 | (0.70–2.00) | 0.523 | 1.10 | (0.64–1.90) | 0.722 |
| Patient issue | 6.16 | (3.04–12.48) | 0.000 | 7.36 | (3.49–15.52) | 0.000 |
| Material and resources | 1.92 | (0.96–3.87) | 0.066 | 1.76 | (0.85–3.63) | 0.126 |
| Knowledge, skills, and performance | 0.92 | (0.45–1.86) | 0.807 | 0.93 | (0.45–1.94) | 0.856 |
| Others’ behaviour | 1.85 | (0.92–3.71) | 0.083 | 1.76 | (0.86–3.63) | 0.123 |
| Observation of strain episodes of others | 17.34 | (3.69–81.54) | 0.000 | 14.60 | (2.98–71.52) | 0.001 |
Adjusted model for type of operation (emergency vs elective), entry (laparoscopic vs other), time of the day the operation took place and duration of the operation. As covariates, laparoscopic operations, and longer operations are associated with a significant higher probability that strain episodes are experienced concurrently by 2 or more team members; only in the adjusted model with the predictor observation of strain episodes of others, the covariate laparoscopic operation shows no significant effect. We present the detail of the logistic regression model with the covariates only as predictors in Supplemental Digital Content 1, http://links.lww.com/AOSO/A249.
†The concordance of strain episodes between participants (vs as experienced by only 1 participant) was compared for each category of strain against the other categories of strain.
FIGURE 2.
Percentages of strain episodes experienced concurrently by 2 or more team members versus experienced by only 1 team member, for strain related to different categories.
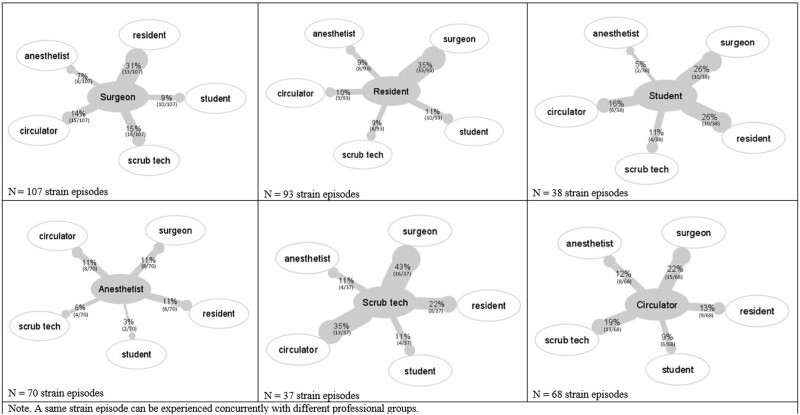
Figure 3 illustrates the proportion of strain episodes reported concurrently with other team members for each profession. Results reveal different patterns for each profession: surgeons, residents, and medical students report a higher proportion of their strain episodes concurrently with one another than with the anesthetists (inferential statistics not performed). The scrub technicians’ reported events converged most often with the surgeons’ and the circulators’ events. The circulators showed equal concordance with all professional groups and anesthetists experienced only very few of the strain episodes concurrently with other professional groups.
FIGURE 3.
Analysis of strain episodes experienced concurrently by 2 or more team members.
We found no effects of the magnitude of the strain episodes as drawn by the OR team members on the likelihood that a strain episode was reported by several team members (OR = 1.10, 95% CI = 0.84–1.43, P = 0.479).
DISCUSSION
We found that 75% of all strain episodes were reported only by one OR team member. These results support the notion that although OR teams share a common overarching goal of safe patient care, individual team members spend a considerable amount of time dealing with specific subgoals and subtasks, related to their specific roles during operations.14,15 These subtasks may draw on team members’ attentional resources and impair their perception of the broader situational development in the OR, including other team members’ strain, particularly in stressful situations.16 Thus, emotional contagion may be contingent on various factors (eg, familiarity with the situation), and does not occur automatically.6
Although acute patient issues lead to a much higher percentage of concurrent strain reports by different team members, emotional contagion is limited, since the percentage of acute patient issues experienced by only a single team member remained high, with more than 40% in our data.
Experiencing other’s behaviors as annoying, distracting, or rude was not likely to be reported by different team members, which is concordant with previous research showing that tensions in the OR are often expressed in a subtle way rather than as open conflicts.17
Overall, most strain episodes experienced by OR team members related to task complexity, followed by patient issues, issues with tools, and resources and issues with knowledge, skills and performance, and others’ behaviors, and to a minor extent to observations of other team members’ strain. A majority of the strain episodes related to acute issues with the patients and observing other team members’ strain were reported by 2 or more team members. Strain related to task complexity, material or resources, knowledge skills, and performance or other’s behaviors were mostly reported only by 1 team member. Professional groups collaborating closely (eg, surgeon-resident and scrub technician-surgeon) reported more similar strain episodes. The categories of triggers of strain that we found were similar to other studies.2,11 Complex tasks (ie, complex phases of the operations) are a known source of strain for the surgeons,18 and more complex patients (ie, higher ASA scores) as sources of strain for the anesthetists.19 Regarding issues with material and resources, a recent study found an association between equipment issues and surgeons’ and nurses’ stress, but not anesthetists’ stress, whereas another similar study failed to find associations between these aspects.20
The finding that dyads who collaborate closely are more likely to experience concurrent episodes of strain, such as the surgeon and surgery resident, is in line with the close collaboration already shown in this dyad in previous work.21 The convergence of the strain episodes reported by the scrub technician with the ones reported by the surgeon is in line with research stressing the importance for the scrub technicians to anticipate the surgeons’ needs and pay attention during phases of very close collaboration with the surgeons22,23 and research showing that scrub technicians more than circulators’ stress was impacted by the operation.24 Our data showed that although scrub technicians’ strain episodes often occur concurrently to the surgeons’, the reverse was rare, with 15% of the strain episodes reported by the surgeons reported concurrently by the scrub technicians, suggesting that scrub technicians did not experience independent strain frequently. This finding is intuitive, in that the scrub technician’s work is deeply linked to the surgeon’s needs and the stage of the operation. This result also underlines the importance of the profession of the OR team members as a predictor of the timing of strain episodes, as previously found.12
Implications and Future Research
Shared perception of important aspects within a team, also called shared mental models, are a key aspect of successful teams, particularly in crisis situations, when teams have to adapt and coordinate quickly.25–27 The finding that patient issues are often experienced by more than 1 team member may indicate a common focus within the team when facing more patient-centric, urgent situations. This may trigger intra-team supportive behaviors, for example, back up behaviors, but also reduce unnecessary distractions because team members are aware of the current patient issue.28,29 It is encouraging that patient-related issues are more commonly perceived by all team members. The lack of shared perception of episodes of strain for nonpatient issues may be positive or negative. Stated positively, limited awareness of other team member’s task-related stress may be beneficial because there will be limited or no stress contagion to other team members and preserve the rest of the team from negative stress effects, such as tunnel vision or emotional exhaustion. It could also be that 1 team member is struggling with strain, and no other team members are aware; therefore, the individual is left to handle the strain alone.
Social support after the operation—for example, from peers or supervisor, or individual coping strategies, may help mitigate the effects of strain on well-being and willingness to stay in the organization. Also, debriefings with the other team members, even if delayed, may foster the development of strategies at the team level to support efficient handling of strain situations in the OR. Future research is needed to identify the effects of these different patterns on team performance and coordination. Also of interest is to determine why strain may not be shared with the rest of the team and to what extent team members do not show their stress because they cope with the stress9 by suppressing any expression of it or if team members’attentional focus hinder their perception of other’s stress. Measurement of behaviors, for example, via video-cameras in the OR, may represent a valuable complementary approach to collect data on each team member’s activities and behaviors during strain episodes.
LIMITATIONS
The study has limitations. It was conducted at a single center, which limits the generalizability of the results. Several types of operations, performed by different surgeons and subteams, were included to mitigate this limitation. We also acknowledge that our list of potential triggers for strain is limited and warrants further exploration of other system factors that may also be contributing to strain. Further studies based on a larger number of operations should take into account duration and important characteristics of the operation, as these aspects were shown to impact strain episodes.
Third, although the guided-recall method facilitates collection of many different strain episodes, one cannot exclude that some strain episodes were not reported. First, memory bias may limit the accuracy of the strain episodes reported; some may be forgotten or the problem underlying a strain episode may be resolved before the end of the operation for 1 of the 2 parties30 and impact the OR team members’ assessment collected at the end of the operation.31 Second, some strain episodes may be considered as not worthy of reporting based on how team members understand the question and define strain, which also constitutes a source of bias.31
Also, there are interindividual differences in the perception of the own and others’ emotions (ie, interoception), reflected in measurable neurobiological individual differences.32 Third, social desirability may also prevent OR team members to share negative or (professional) ego-threatening experiences with the researchers; although this type of bias is minimized when researchers ask study participants questions on a very specific, short period of time rather than their general experience.31 Thus, the guided-recall method we used may underestimate the number of strain episodes; physiological measurement of stress such as heart rate variability or self-confrontation methods (commenting video recordings) may represent opportunities to overcome these biases in future research.
CONCLUSIONS
To conclude, the current study showed that despite the close collaboration, OR team members remained “alone” when they experienced strain episodes, with the partial exception of patient issues. We believe that although not directly relevant for safety, the other strain sources point to systemic issues (even minor), such as problem with the material or a lack of knowledge for a specific aspect of the operation or unwanted distractions. The fear of losing face or letting others lose face may act as a strong barrier to discussing these aspects openly during the operation; sessions to openly discuss and reflect may represent a valuable alternative to constructively deal with recurring strain episodes, increase system efficiency and OR team members’ satisfaction.
ACKNOWLEDGMENTS
We thank Patty Parker for her help in organizing the data collection, and the nurses, anesthesiology, and surgery team leaders whose team members were enrolled in the study. We thank all the study participants who took time to fill out the guided recalls and share with the research team their experience of an operation. We thank Franziska Tschan for reviewing of an earlier version of this article and Tanja Manser for the discussions during the planning and later stages of the study.
Supplementary Material
Footnotes
Published online 12 September 2023
S.K., S.H.P., S.Y., and D.S.S. did conception and design. S.K., S.H.P., V.Z., S.S., and F.A.V. did acquisition of data. S.K., S.H.P., and G.B. did analysis, or interpretation of data. S.K. did drafting of the article. All authors did critical revision of the article for important intellectual content. S.K. and S.H.P. did supervision.
This work was sponsored by the Swiss National Science Foundation, grant number P2NEP1 178574. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Disclosure: The authors declare that they have nothing to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Sonnentag S, Frese M. Stress in organizations. In: Borman WC, Ilgen DR, Klimoski RJ, eds. Comprehensive handbook of psychology. Wiley, 2003:453–491. [Google Scholar]
- 2.Wetzel CM, Kneebone RL, Woloshynowych M, et al. The effects of stress on surgical performance. Am J Surg. 2006;191:5–10. [DOI] [PubMed] [Google Scholar]
- 3.Villafranca A, Hiebert B, Hamlin C, et al. Prevalence and predictors of exposure to disruptive behaviour in the operating room. Can J Anaesth. 2019;66:781–794. [DOI] [PubMed] [Google Scholar]
- 4.Leape LL, Shore MF, Dienstag JL, et al. Perspective: a culture of respect, part 1: the nature and causes of disrespectful behavior by physicians. Acad Med. 2012;87:845–852. [DOI] [PubMed] [Google Scholar]
- 5.Rogers DA, Lingard L. Surgeons managing conflict: a framework for understanding the challenge. J Am Coll Surg. 2006;203:568–574. [DOI] [PubMed] [Google Scholar]
- 6.Elfenbein HA. The many faces of emotional contagion: an affective process theory of affective linkage. Organ Psychol Rev. 2014;4:326–362. [Google Scholar]
- 7.Chrouser KL, Xu J, Hallbeck S, et al. The influence of stress responses on surgical performance and outcomes: literature review and the development of the surgical stress effects (SSE) framework. Am J Surg. 2018;216:573–584. [DOI] [PubMed] [Google Scholar]
- 8.Barsade SG, Coutifaris CG, Pillemer J. Emotional contagion in organizational life. Res Organ Behav. 2018;38:137–151. [Google Scholar]
- 9.Yule S, Flin R, Paterson-Brown S, et al. Non-technical skills for surgeons in the operating room: a review of the literature. Surgery. 2006;139:140–149. [DOI] [PubMed] [Google Scholar]
- 10.Catchpole K, Mishra A, Handa A, et al. Teamwork and error in the operating room: analysis of skills and roles. Ann Surg. 2008;247:699–706. [DOI] [PubMed] [Google Scholar]
- 11.Arora S, Sevdalis N, Nestel D, et al. The impact of stress on surgical performance: a systematic review of the literature. Surgery. 2010;147:318–30, 330.e1. [DOI] [PubMed] [Google Scholar]
- 12.Keller S, Yule S, Smink DS, et al. Episodes of strain experienced in the operating room: impact of the type of surgery, the profession and the phase of the operation. BMC Surg. 2020;20:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shannon P, Markiel A, Ozier O, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498−2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burtscher MJ, Manser T. Team mental models and their potential to improve teamwork and safety: a review and implications for future research in healthcare. Saf Sci. 2012;50:1344–1354. [Google Scholar]
- 15.Fiscella K, Mauksch L, Bodenheimer T, et al. Improving care teams’ functioning: recommendations from team science. Jt Comm J Qual Patient Saf. 2017;43:361–368. [DOI] [PubMed] [Google Scholar]
- 16.Endsley MR. Situation awareness in aviation systems. In: Wise JA, Hopkins VD, Garland DJ, eds. Handbook of Aviation Human Factors. Lawrence Erlbaum Associates, 1999:257–276. [Google Scholar]
- 17.Lingard L, Reznick R, Espin S, et al. Team communications in the operating room: talk patterns, sites of tension, and implications for novices. Acad Med. 2002;77:232–237. [DOI] [PubMed] [Google Scholar]
- 18.Jones KI, Amawi F, Bhalla A, et al. Assessing surgeon stress when operating using heart rate variability and the state trait anxiety inventory: will surgery be the death of us? Colorectal Dis. 2015;17:335–341. [DOI] [PubMed] [Google Scholar]
- 19.Doleman B, Blackwell J, Karangizi A, et al. Anaesthetists stress is induced by patient ASA grade and may impair non-technical skills during intubation. Acta Anaesthesiol Scand. 2016;60:910–916. [DOI] [PubMed] [Google Scholar]
- 20.Wheelock A, Suliman A, Wharton R, et al. The impact of operating room distractions on stress, workload, and teamwork. Ann Surg. 2015;261:1079–1084. [DOI] [PubMed] [Google Scholar]
- 21.Mondada L. Instructions in the operating room: how the surgeon directs their assistant’s hands. Discourse Stud. 2014;16:131–161. [Google Scholar]
- 22.Mitchell L, Flin R, Yule S, et al. Thinking ahead of the surgeon. an interview study to identify scrub nurses’ non-technical skills. Int J Nurs Stud. 2011;48:818–828. [DOI] [PubMed] [Google Scholar]
- 23.Bogdanovic J, Perry J, Guggenheim M, et al. Adaptive coordination in surgical teams: an interview study. BMC Health Serv Res. 2015;15:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sonoda Y, Onozuka D, Hagihara A. Factors related to teamwork performance and stress of operating room nurses. J Nurs Manag. 2018;26:66–73. [DOI] [PubMed] [Google Scholar]
- 25.Wahr JA, Prager RL, Abernathy J, et al. Patient safety in the cardiac operating room: human factors and teamwork a scientific statement from the american heart association. Circulation. 2013;128:1139–1169. [DOI] [PubMed] [Google Scholar]
- 26.Salas E, Wilson KA, Murphy CE, et al. Communicating, coordinating, and cooperating when lives depend on it: tips for teamwork. Jt Comm J Qual Patient Saf. 2008;34:333–341. [DOI] [PubMed] [Google Scholar]
- 27.Waller MJ, Gupta N, Giambatista RC. Effects of adaptive behaviors and shared mental models on control crew performance. Manage Sci. 2004;50:1534–1544. [Google Scholar]
- 28.Salas E, Sims DE, Burke CS. Is there a “Big Five” in teamwork? Small Group Res. 2005;36:555–599. [Google Scholar]
- 29.Wadhera RK, Parker SH, Burkhart HM, et al. Is the “sterile cockpit” concept applicable to cardiovascular surgery critical intervals or critical events? the impact of protocol-driven communication during cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2010;139:312–319. [DOI] [PubMed] [Google Scholar]
- 30.Keller S, Tschan F, Semmer NK, et al. “Disruptive behavior” in the operating room: a prospective observational study of triggers and effects of tense communication episodes in surgical teams. PLoS One. 2019;14:e0226437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwarz N. Retrospective and concurrent self-reports: The rationale for real-time data capture. In: Stone SSS A, Atienza A, Nebeling L, eds. The science of real-time data capture: Self-reports in health research. Oxford University Press. 2007:11–26 [Google Scholar]
- 32.Toller G, Brown J, Sollberger M, et al. Individual differences in socioemotional sensitivity are an index of salience network function. Cortex. 2018;103:211–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.