Abstract
Background:
Creating empathetic healthcare professionals is critical to addressing the health equity challenges of today, particularly as it relates to vulnerable populations.
Methods:
To assess the impact of the Johns Hopkins Center for AIDS Research (CFAR) Generation Tomorrow Summer Health Disparities Scholars (GTSHDS) program on students’ empathy towards individuals living with substance use disorder and differential impact on empathy related to the COVID-19 pandemic, the Attitudes towards Mental Illness Questionnaire (AMIQ), an assessment of stigmatizing attitudes, was administered. Pre- and post-program participation AMIQ survey data were compared using paired t-tests to explore changes within the program year. Unpaired t-tests were used to characterize differences between the mean scores across the two student cohorts.
Results:
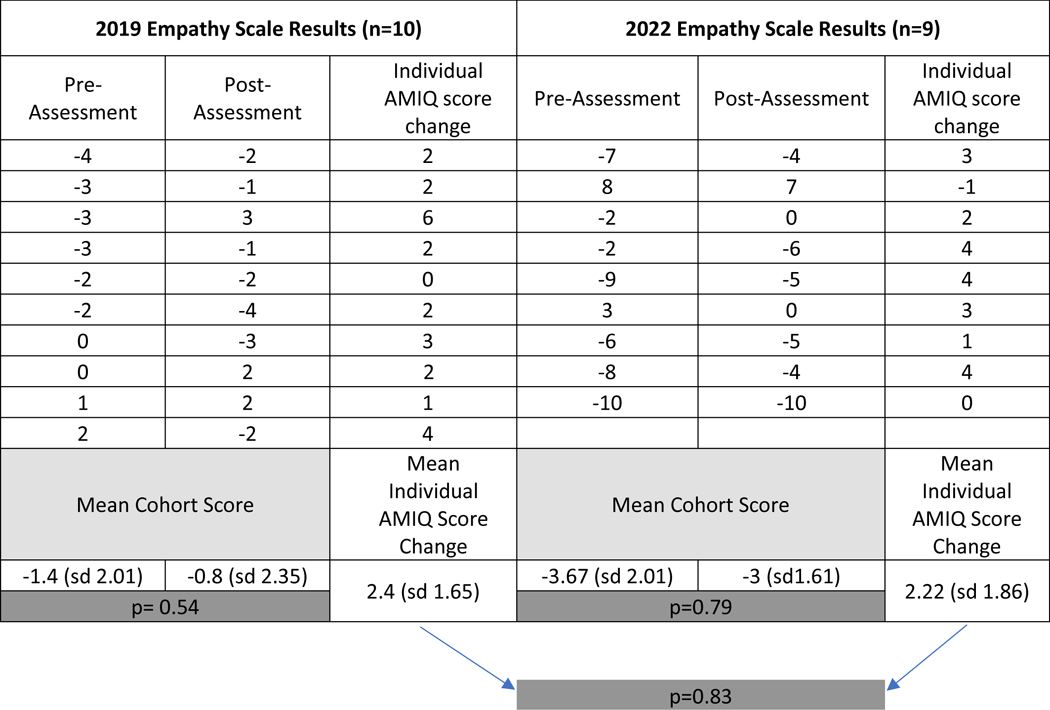
Both GTSHDS cohorts displayed post-program increase in empathy. Mean 2019 cohort AMIQ scores shifting from −1.4 (sd 2.01) to −0.8 (sd 2.35) (p=0.54), and the 2022 cohort shifting from −3.67 (sd 2.01) to –3 (sd 1.61) (p=0.79). On average, individual scores improved by 2.2 (sd 1.65) points in the 2019 cohort and 2.4 (sd 1.86) points in the 2022 cohort (p=0.83). While these were not statistically significant, they suggested a trend towards more empathy.
Conclusion:
Preliminary data suggest that programs such as GTSHDS that expose students to various aspects of healthcare principles can prepare future healthcare professionals in a manner that may reduce healthcare disparities. Future research with larger population sizes is needed to understand the impacts of the curriculum on empathy and related concepts to achieving health equity.
Keywords: Empathy, Health Disparities, Stigma, Education Program, Behavioral Health, HIV/HCV
Introduction
Achieving health equity and eliminating health and healthcare disparities has been a priority for medical and public health professionals for decades1–4. Despite efforts addressing these inequities, health and healthcare disparities remain in the United States healthcare system. According to the National Healthcare Quality and Disparities Report, for approximately 40% of quality measures, Black and American Indians/Alaska Natives received worse health care than Whites5. Similarly, individuals identifying as Hispanic in this report scored worse on one-third of quality measures. Defined as differential outcomes between groups, health disparities result in preventable harms to many and cost the US healthcare system $93 billion in excess medical care..
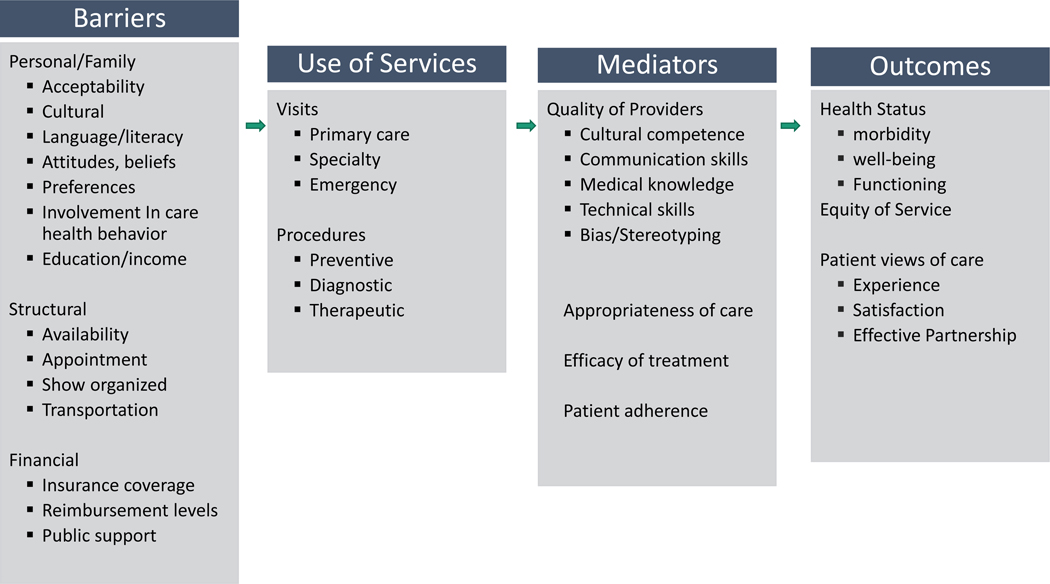
Various underlying factors have been identified that contribute to health and healthcare disparities 6,7. According to the Institute of Medicine’s model of access to health services, personal, financial, and structural barriers exist that prevent persons from accessing care6. Recent models of care highlight the importance of additionally improving the quality of care to reduce disparities6,8,9. These models emphasize that improving the quality of care that healthcare practitioners deliver can be improved by developing soft skills such as cultural competence, addressing bias and stereotyping, and communication 6,8–10. One critical component of this approach is to develop the skill of empathy, which entails both being able to perspective share with an individual and communicate compassion towards them as well 11. Empathy has been shown to help combat negative stereotypes. It has been shown to be helpful in addressing some of the implicit biases that drive the differences in health outcomes we often observe.
Indeed, empathy is an essential consideration for medical care, in particularly for communities that face disproportionate levels of stigma and discrimination. Individuals living with human immunodeficiency virus (HIV) and hepatitis C (HCV), which exemplify preventable and treatable diseases that disproportionately impact racial and ethnic minority groups13, are an important example. Recent evidence suggests that non-judgmental, empathetic care may increase treatment adherence for patients living with HIV and HCV. Similarly, individuals with substance use disorders (SUDs) experience considerable amounts of stigma and campaigns to increase empathy have been an important strategy in helping to address this epidemic13–15.
Recognizing these concerns, we sought to provide programming to help build empathy in future medical care trainees and reduce stigma towards patients living with HIV/HCV and many of the other co-morbidities that these individuals often experience SUDs, mental illness, trauma, and other challenges. In October, 2013 Johns Hopkins Center for AIDS Research (CFAR) launched the Generation Tomorrow (GT) program to increase HIV and HCV awareness/detection in Baltimore and engage the next generation of health professionals (students) and community members (peers) in HIV and HCV outreach services 16. The initial focus of the program was on HIV and HCV. However there was recognition that health disparities related to SUDs, including opioid use disorders (OUDs), had increased, especially during the COVID 19 pandemic19,20. Additionally, HIV and HCV co-infection has been long known to be associated with psychiatric illness severity, substance use, poverty, homelessness, incarceration, urban residence and minority status 18. Therefore, the GT curriculum was augmented in 2019 to create a summer program to expose students to clinical experiences and didactic sessions that would focus on behavioral health (SUDs and other mental illness) in addition to HIV and HCV. It is known that perceived stigma on the part of the patient is a barrier that can lead to decreased engagement in treatment and decreased quality of the patient-provider interaction 21–24. This curriculum expansion sought to address stigma by building empathy and cultural humility in enrollees as a means of decreasing stigmatizing attitudes in potential future healthcare professionals.
As a result of this shift, Generation Tomorrow: Summer Health Disparities Scholars (GTSHDS) was launched in 2019 and serves as a summer program for undergraduate students from across the United States interested in HIV and/or HCV health disparities and their intersection with SUDs (addiction and overdose), violence, mental health, and the social determinants of health. The program promotes comprehensive care of individuals impacted by HIV and HCV infections, creates a conduit to attain health careers for diverse applicants and enhance the cultural competence of all participants. The program was launched in conjunction with Sisters Together and Reaching, Inc. (STAR), a community-based organization focused on HIV and HCV outreach.
Our aim with the present report is to describe the impact the program had on empathy towards individuals with mental illness as measured through shifts in stigmatizing attitudes and to also understand how empathy has changed for learners given the changes that have occurred pre and post pandemic. We hypothesized that program participants would perceive patients living with SUDs more positively and that participation would increase students’ level of empathy as measured through a shift towards more positive attitudes about these populations.
Methods
Student recruitment and selection
The GTSHDS program is advertised through Johns Hopkins University School of Medicine Pathways programs website which highlights available summer internship programs for learners interested in pursuing careers in medicine and research25. Within this website, there is a particular subpage that describes mission and application criteria for GTSHDS. Potential program participants must have completed two years of college by the start of the summer program and be a US citizen or permanent resident to apply. Submitted applications were evaluated for academic and non-academic accomplishments with a focus on UIM status, first-generation college attendees, and individuals from disadvantage backgrounds26. Additionally, GPA and a panel review of each applicant’s research experience and academic references were used to prioritize applicants and determine programmatic fit. While GT: SHDS program did not target students at a specific geographic level, applications came from across the nation. All accepted students were expected to stay on campus and GTSHDS paid for housing.
Curriculum Description
The GTSHDS program is focused on disseminating equitable healthcare practices by training and introducing more diverse and culturally competent providers into the field. A modified version of the Institute of Medicine’s Health Access Model was used as the paradigm upon which the program was built (Cooper et al., 2002; Figure 1). The program encourages cultural competence and cultural humility by exposing a diverse array of learners to diverse populations, topics, and experiences, fostering both transformative and experiential learning theory-based opportunities. Through HIV and HCV training as well as weekly lectures, enhanced communication is emphasized with a particular focus on non-judgmental care. The students also improve their medical knowledge and technical skills which lay the groundwork for future careers in medicine. Lastly, students are required to attend lectures focused on increasing empathy, cultural competency and cultural humility with the hopes that they will use these lessons as they grow into professionals. Addressing all of these mediators in the GTSHDS program is intended to help future professionals internalize skills that will improve health outcomes for racial and ethnic groups and thus reduce health and health care disparities.
Figure 1.
Modified version of the Institute of Medicine’s Health Access Model
In addition to the components established in the parent Generation Tomorrow program, the key program components of GTSHDS include lectures, research, mentorship, community outreach and career advising. In the summer of 2019, students participated in the program and were hosted at Johns Hopkins in Baltimore, Maryland. In 2020 and 2021, the program was hosted virtually due to COVID-19 and had limited offerings. On-site programming resumed in the summer of 2022.
Our community partner, Sisters Together and Reaching, Inc., is a non-profit, community and faith-based organization that was created in 1991 in Baltimore. This organization was founded to address inequities in services to African American women and their families living with HIV/AIDS. They have been providing resources and support services to women with HIV women and their families since 1991 and to men with HIV since 1997. The partnership between STAR and Generation Tomorrow allowed the students to participate in community outreach by providing testing in their mobile clinic, hosting testing events and block parties in East Baltimore. The partnership with this community-based organization began in 2015 and continues to remain in the GT and GTSHDS programs
GTSHDS Program Components
Lecture Series:
The GTSHDS lecture series was presented on Tuesday and Thursday mornings or early afternoons. The guest lecturers included leaders from the CFAR, university-affiliated faculty, health professionals from Baltimore City, and other content experts. The goal of the lecture series was to provide additional knowledge about the relationship between HIV and/or HCV in Baltimore communities and the social determinants of health. Additionally, this curriculum focused on promoting non-judgmental, compassionate, and culturally competent care. Some of the topics included: HIV/HCV Clinical Testing and Care, Mental Health and SUDs, Career Profiles in Infectious Diseases, Social Determinants of Care, Trauma Informed Care, Violence Prevention, Neurological Underpinning of Substance Use Disorders, Motivational Interviewing, HIV Disparities in Men Who Have Sex with Men, Harm Reduction 101, Medical School Admissions, HIV & Sex Workers and International HIV Work.
Research and Mentorship:
The GTSHDS participant interests were assessed through a brief survey and then they were paired with a mentor for their summer research project during the 10-week program. The mentors are typically Johns Hopkins faculty members with ongoing research. The projects focus on health disparities related research, which can be clinical, health services, or biomedical. The students present a poster as well as a presentation highlighting what they worked on throughout the summer. These mentorships are a focal point of the summer program, and many mentors continue to collaborate with students post the formal program, and some students have published with their mentors.
Community Outreach:
The program includes the opportunity for the students to have an internship focused on outreach through community-based organizations or Johns Hopkins-affiliated programs. The 2019 and 2022 GTSHDS participants received training and certifications in HIV and HCV counseling and testing at the beginning of their program. The students then received hands-on training with supervisors at their field assignments before engaging in education, testing, and counseling. The 2020 and 2021 cohorts could not participate in community outreach due to the Coronavirus Pandemic.
Career Advising from Program Leadership:
The Generation Tomorrow program leadership has expertise in HIV and HCV health disparities as well as the other relevant topics discussed during the program. The leadership provides career advising to students through measures such as interview prep, as well as continues to work with students throughout the year on various projects.
Student Data
The program was acknowledged as exempt by the Johns Hopkins University School of Medicine Institutional Review Board (IRB00260569). Student data from 2019 and 2022 is presented in this paper which comprised the two years in which the program was in-person and had all program components.
Demographics:
The following demographic variables were collected at the beginning of the program: age, gender, race/ethnicity, years in college, self-identification of the first generation in college or economically disadvantaged background.
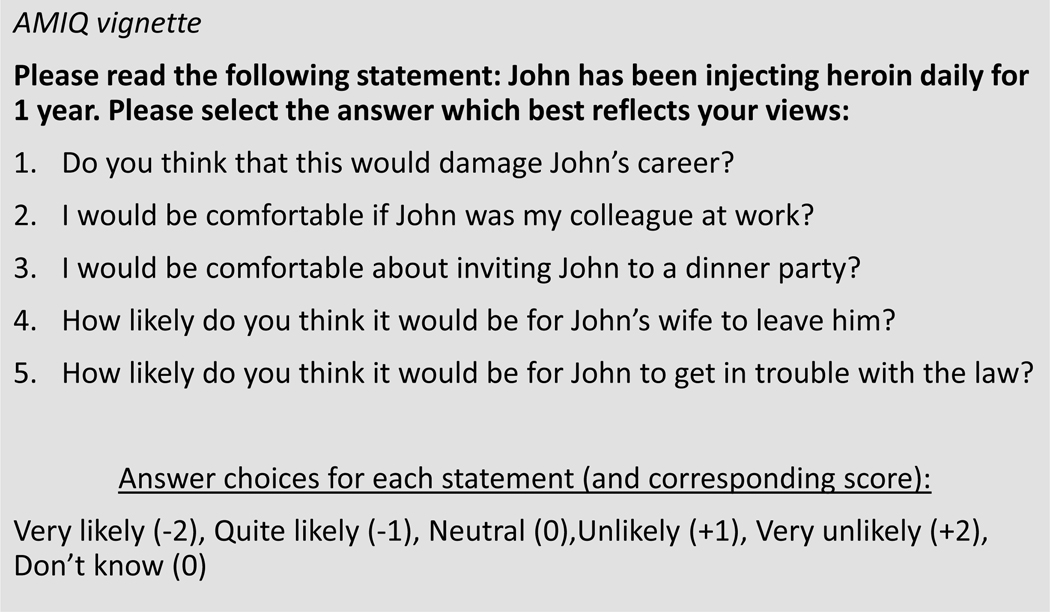
Empathy Assessment (figure 2):
Figure 2.
Attitudes Towards Mental Illness Questionnaire vignette
Students are electronically assessed using a pre-post survey each academic year to assess for elements for changes in multiple spheres. One area of focus is empathy. Potential for GTSHDS participants to harbor stigmatizing attitudes was measured by use of the previously-validated Attitudes towards Mental Illness Questionnaire (AMIQ) 27. While there are several assessments in the literature available to assess empathy in educational settings10,28–30, few have been vaildated for a college population similar to GTSHDS. The AMIQ has multiple vignettes for various health conditions (diabetes, schizophrenia, depression, substance use disorders), however, given the GTSHDS program focus on SUDs, the opioid use disorder vignette “John has been injecting heroin daily for 1 year” was solely administered. Each student was subsequently asked five individual questions which were scored on a 5-point Likert scale (maximum +2, minimum –2) with blank questions, “neutral” and “don’t know” being scored 0. “Those items with question stems that would indicate low empathy had the most negative score if a person strongly agreed or aligned with the stem. Those items with question stems that would indicate high empathy had the most positive score if a person strongly agreed or aligned with the stem.”
The score for the five questions was added giving a total score between –10 and +10 for the vignette, with negative scores representing negative attitudes (or stigma) towards this individual. Decreased stigmatizing behavior occurs when individuals gain knowledge about another situation to reduce misperceptions. Therefore, we felt the AMIQ was a fair proxy for empathy.
Analysis
Descriptive analysis of the student’s demographic data was performed. Pre-post comparison of the Mean total score and mean item responses for the AMIQ were performed using paired t-tests to assess changes within each cohort’s year. The Shapiro-Wilks test was used to confirm normal distribution of data prior to analysis as was an f-test to assess for equal variance. Unpaired t-tests were used to compare the cohorts pre and post pandemic. Only individuals that completed both pre and post program components of the survey were included. We assessed for differences in mean AMIQ scores before and after each cohorts program completion and also assessed differences in changes in scores across the two time periods to understand potential impacts of the pandemic. Statistics were completed using STATA 15.
Results
Demographics (table 1):
Table 1:
Demographic Characteristics of Program participants
| Characteristic | 2019 Cohort (n=10) | 2022 Cohort Completed Pre & Post Data (n=9) | Chi2-Test |
| Self-Reported Race | 1.00 | ||
| Asian | 20% | 22.22% | |
| Black | 50% | 55.56% | |
| White | 20% | 22.22% | |
| Other | 10% | 0% | |
| Hispanic Ethnicity | 10% | 0% | |
| Self-Reported Gender | 0.39 | ||
| Male | 30% | 44.44% | |
| Female | 70% | 44.44% | |
| Other | 0% | 11.11% | |
| First Generation in Medicine? | 40% | 44.44% | 0.64 |
| Attends HBCU/MSI | 20% | 44.44% | 0.25 |
In 2019, the cohort consisted of 10 students whom each completed both the pre and post assessments. Mean age was 20.7 years old, having completed 2.3 years of college. Seventy percent (70%) of the cohort identified themselves as female, 50% were of Black/African American descent. Sixty percent (60%) were underrepresented in medicine, 40% were first generation college students, 30% were economically disadvantaged, and 20% matriculated from Historically Black colleges and Universities (HBCU). The 2022 cohort consisted of 15 students but only nine of which completed both the pre and post assessments. Men represented 44.44% of the cohort, as did women. Nearly 56% were Black, 22% White and 22% Asian. 44% were first generation college students and 44% attending an HBCU.
Empathy Scores (Table 2)
Table 2:
Comparison of Empathy Scores of the 2019 and 2022 GTSHDS cohorts
|
The mean AMIQ total score for 2019 GTSHDS participants was −1.4 (sd 2.01) at baseline compared to −0.8 (sd 2.35) at the end of the program (table 2). While there was a positive increase in the mean AMIQ score, it was not statistically significant (p=0.54). Similarly for the 2022 cohort, the mean AMIQ score shifted from −3.67 (sd 2.01) to –3 (sd 1.61) however these changes were not statistically significant (p=0.79). When comparing the cohorts that participated in the program’s 2019 cohort to those in the 2022 cohort, baseline mean AMIQ individual scores trended more negatively for the post pandemic group(- 0.8 vs –3.67) though were not statistically significant (p=0.22). Engagement in the program also showed a trend towards more positive attitudes with mean difference scores across the cohorts improving by 2.4 (sd 1.65) points for the pre-pandemic group and 2.22 (sd 1.86) points for the post-pandemic group.
Discussion
Our results demonstrate that the GTSHDS program participants showed trends towards increased empathy scores after program participation and that the post-pandemic cohort had more change than the pre-pandemic cohort, though these results were not statistically significant. Nevertheless, there are multiple features to the findings to consider.
The program exposes students from typically underrepresented backgrounds to potential careers that focus on underserved populations which not only widens the recruitment pathway, but also provides a potential solution to address health disparities given the breadth of exposures and content focus on building strength in various areas including community engagement and stigma reduction. The program at this stage has garnered support from the University, the local health department as well as the NIH, making it a promising for sustainability.
While there was a positive shift in the total AMIQ for the student group, the changes were not statistically significant. We attribute this to the low sample size. Additionally, in 2022, the electronic survey was sent post-program completion when many students were returning to school, and not all completed the survey, which limited completion rates. The present report demonstrates that educating these future healthcare professionals has potential to decrease stigma and potentially lead to increasing empathy towards this population. It has been shown that the education of health practitioners can lead to a shift in attitudes towards persons with behavioral health issues 10,23,28These data demonstrate the feasibility of a program like GTSHDS to be effective in shaping the readiness of the healthcare workforce of the future by starting early in the training process. Variability in the mean empathy rating was present between the cohorts participating before (Mean AMIQ [−0.8]) and after the pandemic (Mean AMIQ [−3.67]). Though this trend was not significantly different, widespread COVID isolation protocols may have negatively impacted students’ empathy which should be explored in future research.
Given that many of the GTSHDS program participants come from UIM and disadvantaged backgrounds, and have specific interest in addressing healthcare disparities, there is a possibility that they have already been sensitized to specific health disparities. This sensitization raises the likelihood of a ceiling effect on cultural competency interventions, including those focused on empathy building. The data present in this report was not adequately powered to perform regression analyses, and recognizing that empathy is a multidimensional construct with both affective and cognitive aspects, it would be essential to explore the impact of gender, race/ethnicity, or other demographic factors, including cultural competency and humility and subsequent shifts.
Given the breadth of activities that each student experienced (research, clinic exposures, didactics, service learning), it is difficult to pinpoint which aspects of the program were the most impactful to students. GT: SHDS curriculum goals and objectives should be continuously updated to maximize the impact on future healthcare practitioners’ practices that may help eliminate health disparities. As the curriculum evolves, future research will help identify the critical components of the curriculum research that may help deepen empathetic responses. There may be opportunities to look at interpersonal elements such as a sense of belonging31 that could help inform the structure32 and effectiveness of this pathway programming. Higher-powered studies and collection of qualitative data from program participants and mentors will be helpful in gleaning this information and represents an opportunity to study aspects of the student’s motivation to engage in this career path. Standardized items should also be included to track the effectiveness of lectures and in a reproducible manner to enhance the curriculum and experience for the mentees continuously. Ideally, the choice of outcome measure would help demonstrate short-term effectiveness but also allow for longitudinal tracking after course completion to identify which course themes impact the student’s health career decisions.
The GTSHDS program appears to demonstrate trends towards improving empathy as it relates to attitudes towards individuals with substance use disorders. Though not statistically significant, these findings highlight just one of the positive ways that the program has impacted the future trainees. Future research involving more participants and a more holistic assessment including both quantitative and qualitative data is needed to measure the overall impacts of the program as it continues to evolve.
Sources of Funding:
This publication resulted (in part) from research supported by the District of Columbia Center for AIDS Research, an NIH funded program (P30AI117970), which is supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, NIDDK, NIMHD, NIDCR, NINR, FIC, and OAR. Additionally, this research was funded (in part) by the Johns Hopkins University Center for AIDS Research, an NIH funded program (1P30AI094189), which is supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIGMS, NIDDK, NIMHD. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest
The authors have no relevant conflicts of interest to report.
Bibliography
- 1.Folorunso OO, Burns White K, Alonso-Caraballo Y, et al. Building an intentional and impactful summer research experience to increase diversity in mental health research. Neuropsychopharmacology. 2022;47(13):2189–2193. doi: 10.1038/s41386-022-01461-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoge MA, Morris JA, Stuart GW, et al. A National Action Plan for Workforce Development in Behavioral Health. Psychiatr Serv. 2009;60(7):883–887. doi: 10.1176/ps.2009.60.7.883 [DOI] [PubMed] [Google Scholar]
- 3.Satcher D. Embracing Culture, Enhancing Diversity, and Strengthening Research. Am J Public Health. 2009;99(S1):S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stoff DM, Cargill VA. Building a More Diverse Workforce in HIV/AIDS Research: The Time has Come. AIDS Behav. 2016;20(2):222–230. doi: 10.1007/s10461-016-1501-z [DOI] [PubMed] [Google Scholar]
- 5.Agency for Healthcare Research and Quality. 2019 National Healthcare Quality and Disparities Report. Published June 2021. Accessed February 18, 2023. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html
- 6.Cooper LA, Hill MN, Powe NR. Designing and Evaluating Interventions to Eliminate Racial and Ethnic Disparities in Health Care. J Gen Intern Med. 2002;17(6):477–486. doi: 10.1046/j.1525-1497.2002.10633.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams DR, Cooper LA. Reducing Racial Inequities in Health: Using What We Already Know to Take Action. Int J Environ Res Public Health. 2019;16(4):606. doi: 10.3390/ijerph16040606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing Racial Bias Among Health Care Providers: Lessons from Social-Cognitive Psychology. J Gen Intern Med. 2007;22(6):882–887. doi: 10.1007/s11606-007-0160-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vescio TK, Sechrist GB, Paolucci MP. Perspective taking and prejudice reduction: the mediational role of empathy arousal and situational attributions. Eur J Soc Psychol. 2003;33(4):455–472. doi: 10.1002/ejsp.163 [DOI] [Google Scholar]
- 10.Whitford DK, Emerson AM. Empathy intervention to reduce implicit bias in pre-service teachers. Psychol Rep. 2019;122(2):670–688. [DOI] [PubMed] [Google Scholar]
- 11.Sukhera J. Empathy and Implicit Bias: Can Empathy Training Improve Equity? In: Foster AE, Yaseen ZS, eds. Teaching Empathy in Healthcare: Building a New Core Competency. Springer International Publishing; 2019:223–238. doi: 10.1007/978-3-030-29876-0_14 [DOI] [Google Scholar]
- 12.Jackson CS, Gracia JN. Addressing Health and Health-Care Disparities: The Role of a Diverse Workforce and the Social Determinants of Health. Public Health Rep. 2014;129(1_suppl2):57–61. doi: 10.1177/00333549141291S211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu E, Moumen M, Goforth J, et al. Characterizing the Impact of Clinical Exposure to Patients with Opioid Use Disorder on Medical Students’ Perceptions of Stigma and Patient Care. Teach Learn Med. 2023;35(2):128–142. doi: 10.1080/10401334.2022.2038175 [DOI] [PubMed] [Google Scholar]
- 14.Norberg A, Nelson J, Holly C, Jewell ST, Lieggi M, Salmond S. Experiences of HIV-infected adults and healthcare providers with healthcare delivery practices that influence engagement in US primary healthcare settings: a qualitative systematic review. JBI Evid Synth. 2019;17(6):1154. doi: 10.11124/JBISRIR-2017-003756 [DOI] [PubMed] [Google Scholar]
- 15.Yang J, Mackert M. The Effectiveness of CDC’s Rx Awareness Campaigns on Reducing Opioid Stigma: Implications for Health Communication. Health Commun. 2023;38(5):925–934. doi: 10.1080/10410236.2021.1982561 [DOI] [PubMed] [Google Scholar]
- 16.Irvin R, McAdams-Mahmoud A, White JJ, et al. An Education and Field Experience Program to Increase Detection of Human Immunodeficiency Virus and Hepatitis C Virus. Prog Community Health Partnersh. 2018;12(1):101–109. doi: 10.1353/cpr.2018.0011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Association of American Medical Colleges. Underrepresented in Medicine Definition. AAMC. Published March 2004. Accessed February 19, 2023. https://www.aamc.org/what-we-do/equity-diversity-inclusion/underrepresented-in-medicine [Google Scholar]
- 18.Rosenberg SD, Drake RE, Brunette MF, Wolford GL, Marsh BJ. Hepatitis C virus and HIV co-infection in people with severe mental illness and substance use disorders. AIDS. 2005;19 Suppl 3:S26–33. doi: 10.1097/01.aids.0000192067.94033.aa [DOI] [PubMed] [Google Scholar]
- 19.Gondré-Lewis MC, Abijo T, Gondré-Lewis TA. The Opioid Epidemic: a Crisis Disproportionately Impacting Black Americans and Urban Communities. J Racial Ethn Health Disparities. Published online September 6, 2022. doi: 10.1007/s40615-022-01384-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liao CY, Garcia GGP, DiGennaro C, Jalali MS. Racial Disparities in Opioid Overdose Deaths in Massachusetts. JAMA Netw Open. 2022;5(4):e229081. doi: 10.1001/jamanetworkopen.2022.9081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crapanzano K, Vath RJ, Fisher D. Reducing stigma towards substance users through an educational intervention: harder than it looks. Acad Psychiatry. 2014;38(4):420–425. doi: 10.1007/s40596-014-0067-1 [DOI] [PubMed] [Google Scholar]
- 22.Livingston JD, Milne T, Fang ML, Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction. 2012;107(1):39–50. doi: 10.1111/j.1360-0443.2011.03601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendiola CK, Galetto G, Fingerhood M. An Exploration of Emergency Physicians’ Attitudes Toward Patients With Substance Use Disorder. J Addict Med. 2018;12(2):132–135. doi: 10.1097/ADM.0000000000000377 [DOI] [PubMed] [Google Scholar]
- 24.Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–326. doi: 10.1111/obr.12266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dearey M, Grant Z, Manogue S, et al. Reducing Health Disparities: A Pipeline Program to Increase Diversity and Cultural Competence. J Community Med Health Educ. 2022;12(1). doi:DOI: 10.4172/2168-9717.1000733 [DOI] [Google Scholar]
- 26.National Institutes of Health. Individuals from Disadvantaged Backgrounds | Diversity in Extramural Programs. Published February 2023. Accessed February 19, 2023. https://extramural-diversity.nih.gov/diversity-matters/disadvantaged-backgrounds
- 27.Luty J, Fekadu D, Umoh O, Gallagher J. Validation of a short instrument to measure stigmatised attitudes towards mental illness. Psychiatr Bull R Coll Psychiatr. 2006;30(7):257–260. doi: 10.1192/pb.30.7.257 [DOI] [Google Scholar]
- 28.Jackman KM, Scala E, Nwogwugwu C, Huggins D, Antoine DG. Nursing Attitudes Toward Patients With Substance Use Disorders: A Quantitative Analysis of the Impact of an Educational Workshop. J Addict Nurs. 2020;31(3):213–220. doi: 10.1097/JAN.0000000000000351 [DOI] [PubMed] [Google Scholar]
- 29.van Boekel LC, Brouwers EPM, van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1–2):23–35. doi: 10.1016/j.drugalcdep.2013.02.018 [DOI] [PubMed] [Google Scholar]
- 30.Laughey WF, Atkinson J, Craig AM, et al. Empathy in Medical Education: Its Nature and Nurture — a Qualitative Study of the Views of Students and Tutors. Med Sci Educ. 2021;31(6):1941–1950. doi: 10.1007/s40670-021-01430-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pedler ML, Willis R, Nieuwoudt JE. A sense of belonging at university: student retention, motivation and enjoyment. J Furth High Educ. 2022;46(3):397–408. [Google Scholar]
- 32.Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126–133. doi: 10.1016/j.socscimed.2013.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]