Abstract
Aneurysmal bone cyst (ABC) is a rare lesion that primarily affects young adults and children. The optimal treatment approach for ABC remains controversial and varies depending on the preferences of the medical team. While some advocate for surgery as the treatment of choice, others recommend a less invasive first-line option such as selective embolization.
In this case report, we present the case of a 41-year-old female patient with an ABC in the right iliac bone who underwent surgical treatment following preoperative selective embolization. Additionally, we provide a literature review on the topic.
Keywords: ABC, MRI, Embolization, Surgery
Introduction
Aneurysmal bone cyst (ABC) is a relatively uncommon bone tumor that predominantly occurs in young individuals and can be found in various locations such as long bones, the spine, and the pelvis. It is characterized by an expansive lesion consisting of multiple spaces filled with nonclotted blood, separated by thin or thick partitions, sometimes resulting in a solid appearance [1].
The optimal treatment approach for ABC is the subject of ongoing debate. Surgery has traditionally been considered the treatment modality with the best outcomes, although some authors now favor less invasive approaches as the first-line treatment [2]. Selective embolization can be used as a primary treatment for ABC, particularly in challenging locations, or as an adjuvant measure to reduce bleeding and facilitate surgical curettage [1].
In this case report, we describe the preoperative selective embolization of an ABC followed by surgical removal, and we review relevant literature on the subject.
Case presentation
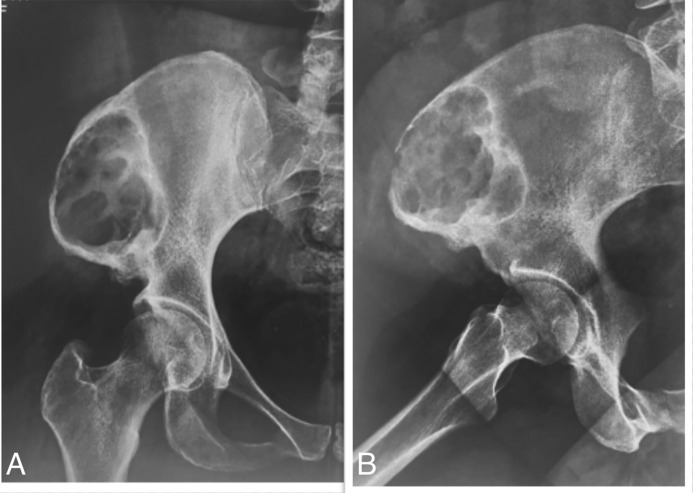
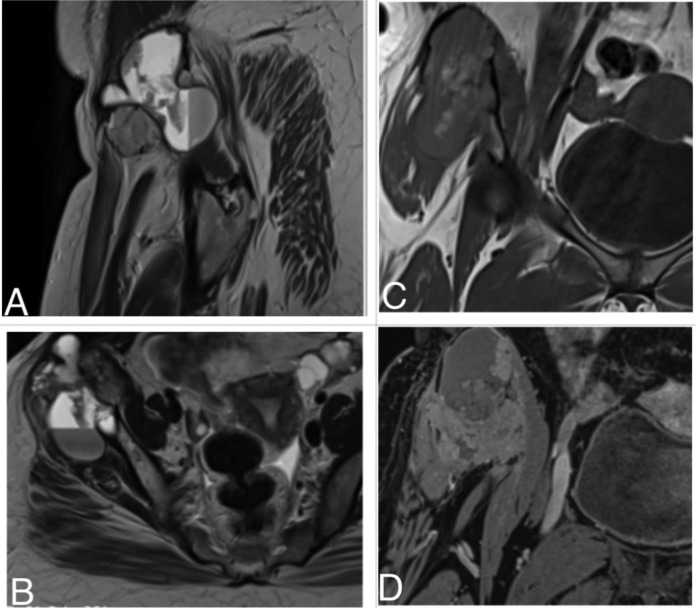
This is a 41-year-old female patient with no previous medical history, who presented with a non-traumatic, painful swelling of the right hip that had been developing over the course of four months. A pelvic X-ray revealed a lytic lesion in the right iliac wing without calcifications, incomplete peripheral sclerosis, and a cortical rupture on its external border (Fig. 1). An MRI was performed using T1, T2, and T1-weighted images with fat suppression, both before and after gadolinium injection in 3 spatial planes. The MRI showed a lesion with mixed content, including tissue portions and liquid components with variable signals. It contained a liquid-liquid level and had sharp contours with a clear cortical break on its external side. The adjacent soft tissues appeared edematous without evident signs of invasion (Fig. 2).
Fig. 1.
Front (A) and profile (B) radiographs of the right hip: Lytic, eccentric lesion of the right iliac wing with incomplete peripheral sclerosis and cortical rupture externally.
Fig. 2.
MRI of the pelvis with T2-weighted sagittal (A) and axial (B); coronal T1 (C) and T1 FAT SAT sequences with gadolinium injection (D): Expansive lesion of the right iliac wing with solid, hemorrhagic and liquid portions of variable signal with a liquid-liquid level.
Following a surgical biopsy and anatomopathological examination, the lesion was diagnosed as a primary or secondary aneurysmal bone cyst. A multidisciplinary consultation involving orthopedic surgeons and interventional radiologists determined that embolization would be the initial treatment, followed by surgical removal. The embolization procedure was performed using a GE Optima IGS 330 monoplane angiography table. The patient was positioned in dorsal decubitus under strict aseptic conditions. A left femoral Seldinger technique was performed, followed by cross-over catheterization of the right common, internal, and external iliac arteries using a Cordis Cobra 04 Fr probe mounted on a Terumo 0.035 hydrophilic guide.
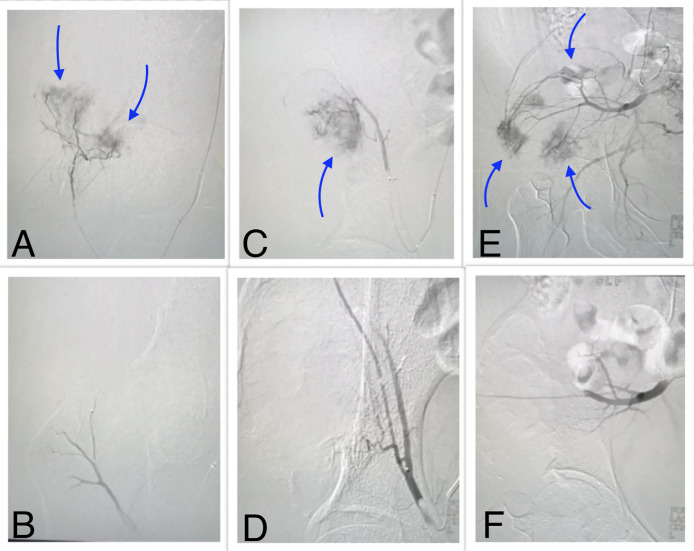
The initial diagnostic acquisitions revealed diffuse bleeding from the right iliac wing, supplied by the medial circumflex artery, the superficial external iliac artery, and branches from the superior gluteal artery. Tumor embolization was performed after selective catheterization of these different feeding arterial branches, followed by the injection of microparticles calibrated at 400 microns (Embosphere®) and resorbable gelatin (Curaspon®)sss. Follow-up angiography demonstrated successful bleeding control and preserved patency of the portal arteries (Fig. 3). No complications were observed during or immediately after the procedure, and the patient was discharged the next day.
Fig. 3.
Angiography Selective microcatheterization of the medial circumflex artery showing sheet-like bleeding (arrows) (A). After embolization with microparticles, bleeding disappeared (B). Selective microcatheterization of the superficial epigastric artery showing sheet-like bleeding (arrow) (C). After embolization with microparticles, bleeding disappeared (D). Selective microcatheterization of the superior gluteal artery showing sheet-like bleeding (arrows) (E). After embolization with microparticles and resorbable gelatin, bleeding disappeared (F).
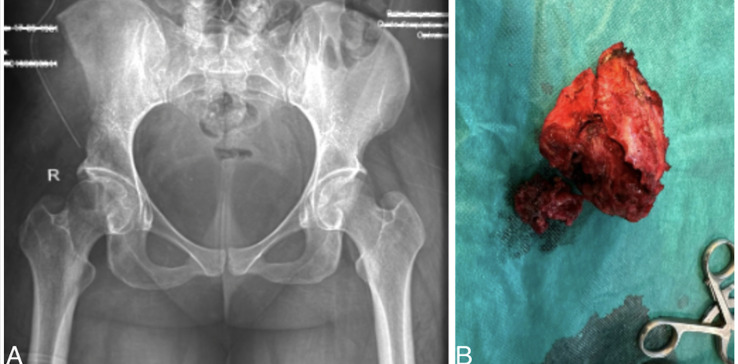
Three days after embolization, she underwent complete tumor removal with minimal intraoperative blood loss. Follow-up pelvic X-ray confirmed the complete removal of the tumor (Fig. 4).
Fig. 4.
Frontal radiograph of the pelvis postoperatively (A) showing complete excision of the lesion with the surgical specimen (B).
Discussion
Described in 1942 by Jaffe and Lichtenstein [3], aneurysmal cysts are relatively rare, classically representing 1% of all biopsied tumors [1]. The lesions mainly occur in adolescents or young adults, with a discrete female predominance in gender distribution [4,5]. The most frequent locations are the femur (22%), tibia (17%), spine (15%), humerus (10%), pelvis (9%), and fibula (9%) [6]. Other locations, such as the sternum or pisiform bone, are more rarely described [7,8].
Primary ABC is recognized as clonal in origin by cytogenetic studies that reveal chromosomal abnormalities in the primary aneurysmal cyst with rearrangements and translocations, particularly on chromosome 17 [9,10]. Histologically, the ABC is an expansive lesion consisting of anastomosing cavernous spaces filled with nonclotted blood and surrounded by fibrous walls of variable thickness, which may contain osteoid tissue or other bony components, giant cells, but no muscle layer or elastic tissue.
Fine-needle specimens have a reliability of only 82% and are uninterpretable in a quarter of cases due to insufficient specimens. Therefore, they can only suggest an aneurysmal cyst when associated with a typical clinical and radiological presentation [11]. In some cases, the solid component may be largely dominant, and these are termed "solid aneurysmal cysts," accounting for about 5% of all primary aneurysmal cysts.
The clinical presentation is not very specific, with pain and local swelling being the 2 most common signs, as observed in our patient [12]. Variable symptoms may result from the compression of surrounding structures. The radiographic appearance depends on the stage of evolution and may vary from case to case. The topography is often eccentric for large long bones or even subperiosteal, while it is of a rather central topography for small long bones [1].
In the developmental phase, the lesions are purely lytic without internal calcification in the vast majority of cases (80%). Lesion margins may appear sclerotic (in 32% of cases), clear but not sclerotic (54%), or poorly defined (14%) [12]. Our patient's right iliac wing lesion was indeed eccentric, purely lytic, and exhibited incomplete peripheral sclerosis.
During the active development phase, the lesion has the typical appearance of a rapidly expanding, quasi-explosive lesion. Differential diagnosis from a malignant tumor can be extremely challenging [12]. In the stabilization phase, the peripheral contour ossifies, forming a thin bony shell, and the internal septa also ossify, giving the lesion a characteristic appearance sometimes referred to as a ``soap bubble''.
Magnetic resonance imaging (MRI) is the most effective method for visualizing the internal organization of the process, which is multilobulated with cavities separated by fibrous septa [13]. Fluid-fluid levels, more frequently visualized on MRI, are somewhat the hallmark of the aneurysmal cyst. These levels were well visualized on our patient's MRI, showing double-density fluid levels, septation, and characteristic signals on T1 and T2 images.
The differential diagnosis primarily includes unicameral bone cysts, with other potential diagnoses being osteolytic lesions such as giant cell tumors, osteoblastoma, metastasis, and myeloma [14]. Therapeutically, considering that ABC mainly affects children and adolescents, "aggressive" surgery for this benign lesion is generally avoided due to the potential for spontaneous healing.
A recent systematic review of the literature confirms that certain less invasive treatments can now be considered as first-line therapies, similar to surgery, for the treatment of ABC, yielding results at least equivalent to surgery with fewer complications [2]. These treatments encompass selective arterial embolization (SAE) and sclerotherapy (using alcohol or polidocanol). Surgery (curettage or resection) remains an option. Some teams employ it as a first-line treatment when embolization or intracystic injections are not feasible (due to the absence of an interventional radiology team) or when noninvasive methods have proven ineffective.
SAE is a challenging technique, dependent on the operator, and is not universally applicable to all cases of ABC. It can be employed as the primary treatment in challenging anatomical locations, such as the spine, or preceding surgery to mitigate bleeding risks and aid in curettage with reduced morbidity compared to surgery [2]. Aneurysmal bone cysts typically receive blood supply from multiple feeding arteries [15]. In our patient, the tumor received supply from both the internal and external iliac arteries. The feeder arteries, their collaterals, their relationship with neighboring vessels, and the potential for arteriovenous fistulas within the tumor must be meticulously assessed during angiography to prevent off-target embolization [15]. Selective catheterization and occlusion of the feeding arteries using the most suitable embolic agent enable tumor devascularization, size reduction, pain relief, and stimulation of new bone formation [16,17]. Multiple procedures are often necessary.
The choice of embolic agents hinges on the desired effect (distal or proximal embolization, temporary or permanent), their availability, and the expertise and preferences of medical professionals. These agents encompass liquid options, such as absorbable gelatin or biological glues, as well as microparticles. In our center, we utilized available microparticles calibrated at 400 and resorbable gelatin.
SAE does have certain limitations, including the need for repeated embolization and patient exposure to radiation. A meta-analysis by Cruz et al. [18] revealed a recurrence risk of 19%. Technical success rates vary between 75% and 94% [17,19]. Complications, occurring in approximately 6% of cases [15], align with the typical complications linked to embolization treatments. These complications may encompass femoral artery dissection at the catheterization site, pain resulting from tumor ischemic necrosis, off-target embolization, infection, and postembolization syndrome.
In conclusion, SAE is a noninvasive technique that can serve as a primary treatment option for ABC or be combined with surgery to minimize intraoperative bleeding. It has demonstrated comparable effectiveness to surgery while presenting fewer complications.
Patient consent
The patient has signed a free and informed consent to the anonymous publication of the material contained in this article
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Malghem J, Lecouvet F, Docquier PL, Galant C, Omoumi P, Maldague B et al. Kyste anévrismal des os. EMC - Radiologie et imagerie médicale - musculosquelettique - neurologique - maxillofaciale 31-491-A-10
- 2.Cottalorda J, Louahem Sabah D, Joly Monrigal P, Jeandel C, Delpont M. Minimally invasive treatment of aneurysmal bone cysts: systematic literature review. Orthop Traumatol Surg Res. 2022;108(4) doi: 10.1016/j.otsr.2022.103272. [DOI] [PubMed] [Google Scholar]
- 3.Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004–1025. [Google Scholar]
- 4.Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R. Aneurysmal bone cyst. A population based epidemiologic study and literature review. Clin Orthop Relat Res. 1999;(363):176–179. [PubMed] [Google Scholar]
- 5.Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC. Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol. 2005;23(27):6756‑62. doi: 10.1200/JCO.2005.15.255. [DOI] [PubMed] [Google Scholar]
- 6.Cottalorda J, Kohler R, Sales de Gauzy J, Chotel F, Mazda K, Lefort G, et al. Epidemiology of aneurysmal bone cyst in children: a multicenter study and literature review. J Pediatr Orthop Part B. 2004;13(6):389‑94. doi: 10.1097/01202412-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Aksu AE, Üstün GG, Uzun H, Gedikoğlu G. Aneurysmal bone cyst of pisiform bone: diagnosis and treatment of a rare entity: case report and a review of the literature. J Hand Surg Asian-Pac. 2021;26(4):722‑7. doi: 10.1142/S2424835521720231. [DOI] [PubMed] [Google Scholar]
- 8.Singh VP, Mir R, Kaul S. Aneurysmal bone cyst of sternum. Ann Thorac Surg. 2010;89(6):e43–e45. doi: 10.1016/j.athoracsur.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 9.Oliveira AM, Hsi BL, Weremowicz S, Rosenberg AE, Dal Cin P, Joseph N, et al. USP6 (Tre2) fusion oncogenes in aneurysmal bone cyst. Cancer Res. 2004;64(6):1920‑3. doi: 10.1158/0008-5472.can-03-2827. [DOI] [PubMed] [Google Scholar]
- 10.Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen CJ, Neff JR, et al. Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes. Oncogene. 2005;24(21):3419‑26. doi: 10.1038/sj.onc.1208506. [DOI] [PubMed] [Google Scholar]
- 11.Creager AJ, Madden CR, Bergman S, Geisinger KR. Aneurysmal bone cyst: fine-needle aspiration findings in 23 patients with clinical and radiologic correlation. Am J Clin Pathol. 2007;128(5):740‑5. doi: 10.1309/VB1M9D9H7QG6L3R4. [DOI] [PubMed] [Google Scholar]
- 12.Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK. Aneurysmal bone cyst. A clinicopathologic study of 238 cases. Cancer. 1992;69(12):2921‑31. doi: 10.1002/1097-0142(19920615)69:12<2921::aid-cncr2820691210>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 13.Mahnken AH, Nolte-Ernsting CCA, Wildberger JE, Heussen N, Adam G, Wirtz DC, et al. Aneurysmal bone cyst: value of MR imaging and conventional radiography. Eur Radiol. 2003;13(5):1118‑24. doi: 10.1007/s00330-002-1668-8. [DOI] [PubMed] [Google Scholar]
- 14.Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res OTSR. 2015;101(1 Suppl):S119–S127. doi: 10.1016/j.otsr.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 15.Rossi G, Mavrogenis AF, Papagelopoulos JP, Rimondi E, Ruggieri P. Successful treatment of aggressive aneurysmal bone cyst of the pelvis with serial embolization. Orthopédics. 2012;35(6):e963–e968. doi: 10.3928/01477447-20120525-43. [DOI] [PubMed] [Google Scholar]
- 16.Meyer S, Reinhard H, Graf N, Kramann B, Schneider G. Arterial embolization of a secondary aneurysmatic bone cyst of the thoracic spine prior to surgical excision in a 15-year-old girl. Eur J Radiol. 2002;43(1):79‑81. doi: 10.1016/s0720-048x(01)00406-5. [DOI] [PubMed] [Google Scholar]
- 17.Rossi G, Rimondi E, Bartalena T, Gerardi A, Alberghini M, Staals EL, et al. Selective arterial embolization of 36 aneurysmal bone cysts of the skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol. 2010;39(2):161‑7. doi: 10.1007/s00256-009-0757-z. [DOI] [PubMed] [Google Scholar]
- 18.Cruz GS, Cuevas-Suárez CE, Saavedra JPA, Giorgis R, Teixeira MRK, Muniz FWMG. Percutaneous treatments of primary aneurysmal bone cysts: systematic review and meta-analysis. Eur J Orthop Surg Traumatol Orthop Traumatol. 2021;31(7):1287‑95. doi: 10.1007/s00590-021-02893-6. [DOI] [PubMed] [Google Scholar]
- 19.Mavrogenis AF, Rossi G, Rimondi E, Papagelopoulos PJ, Ruggieri P. Embolization of bone tumors. Orthopedics. 2011;34(4):303‑10. doi: 10.3928/01477447-20110228-20. [DOI] [PubMed] [Google Scholar]