ABSTRACT
Background: Posttraumatic stress disorder (PTSD) is a debilitating condition affecting millions of people worldwide. Existing treatments often fail to address the complexity of its symptoms and functional impairments resulting from severe and prolonged trauma. Electroencephalographic Neurofeedback (NFB) has emerged as a promising treatment that aims to reduce the symptoms of PTSD by modulating brain activity.
Objective: We conducted a systematic review and meta-analysis of ten clinical trials to answer the question: how effective is NFB in addressing PTSD and other associated symptoms across different trauma populations, and are these improvements related to neurophysiological changes?
Method: The review followed the Preferred Reporting Items for Systematic Reviews and Meta analyses guidelines. We considered all published and unpublished randomised controlled trials (RCTs) and non-randomised studies of interventions (NRSIs) involving adults with PTSD as a primary diagnosis without exclusion by type of trauma, co-morbid diagnosis, locality, or sex. Ten controlled studies were included; seven RCTs and three NRSIs with a total number of participants n = 293 (128 male). Only RCTs were included in the meta-analysis (215 participants; 88 male).
Results: All included studies showed an advantage of NFB over control conditions in reducing symptoms of PTSD, with indications of improvement in symptoms of anxiety and depression and related neurophysiological changes. Meta-analysis of the pooled data shows a significant reduction in PTSD symptoms post-treatment SMD of −1.76 (95% CI −2.69, −0.83), and the mean remission rate was higher in the NFB group (79.3%) compared to the control group (24.4%). However, the studies reviewed were mostly small, with heterogeneous populations and varied quality.
Conclusions: The effect of NFB on the symptoms of PTSD was moderate and mechanistic evidence suggested that NFB leads to therapeutic changes in brain functioning. Future research should focus on more rigorous methodological designs, expanded sample size and longer follow-up.
KEYWORDS: Systematic review, meta-analysis, PTSD, efficacy, neurofeedback, trauma
HIGHLIGHTS
Neurofeedback (NFB) was found to have moderate beneficial effects on PTSD symptoms, and positive effects on secondary outcomes such as depression and anxiety, according to a meta-analysis of seven randomised controlled trials (RCTs).
The beneficial effects of NFB were observed across diverse populations, including those with different types of trauma (military and civilians) and from different ethnic backgrounds.
Results suggest that modulation of alpha rhythm might be a viable NFB protocol in patients with PTSD, as changes in neurophysiological functioning, such as connectivity in the Default Mode Network (DMN) and Salience Network (SN), were observed post-NFB and were correlated with a decrease in PTSD severity.
Abstract
Antecedentes: El trastorno de estrés postraumático (TEPT) es una condición debilitante que afecta a millones de personas en todo el mundo. Los tratamientos existentes a menudo no logran abordar la complejidad de sus síntomas y las deficiencias funcionales resultantes de un trauma grave y prolongado. El neurofeedback electroencefalográfico (NFB en su sigla en inglés) ha surgido como un tratamiento prometedor que tiene como objetivo reducir los síntomas del trastorno de estrés postraumático mediante la modulación de la actividad cerebral.
Objetivo: Realizamos una revisión sistemática y un metanálisis de diez ensayos clínicos para responder a la pregunta: ¿qué tan efectivo es el NFB para abordar el trastorno de estrés postraumático y otros síntomas asociados en diferentes poblaciones de trauma? ¿Estas mejoras están relacionadas con cambios neurofisiológicos?
Método: La revisión siguió las pautas de elementos de reporte preferidos para revisiones sistemáticas y metanálisis (PRISMA en su sigla en inglés). Se consideraron todos los ensayos controlados, aleatorizados y no aleatorizados, publicados y no publicados, que incluyeron a adultos con trastorno de estrés postraumático como diagnóstico principal, sin exclusión por tipo de trauma, diagnóstico de comorbilidad, localidad o sexo. En esta revisión sistemática se incluyeron diez estudios controlados; siete ensayos controlados aleatorizados (ECA) y tres estudios de intervenciones no aleatorizados (NRSI en su sigla en inglés) con un número total de participantes n = 293 (128 hombres). En el metanálisis solo se incluyeron ECA (215 participantes; 88 hombres).
Resultados: Todos los estudios incluidos mostraron una ventaja del NFB sobre las condiciones de control para reducir los síntomas del trastorno de estrés postraumático, con indicaciones de mejoría en los síntomas de ansiedad, depresión y cambios neurofisiológicos relacionados. El metanálisis de los datos combinados muestra una reducción significativa en los síntomas de TEPT después del tratamiento, DME de −1,76 (IC del 95%: −2.69; −0.83), y la tasa media de remisión fue mayor en el grupo con NFB (79.3%) en comparación con el grupo de control (24.4%). Sin embargo, los estudios revisados fueron en su mayoría pequeños, con poblaciones heterogéneas y de calidad variada.
Conclusiones: El efecto del NFB sobre los síntomas del trastorno de estrés postraumático fue moderado y la evidencia mecanicista sugirió que el NFB conduce a cambios terapéuticos en el funcionamiento del cerebro. Las investigaciones futuras deberían centrarse en diseños metodológicos más rigurosos, un tamaño de muestra ampliado y un seguimiento más prolongado.
PALABRAS CLAVE: Revisión sistemática, metanálisis, trastorno de estrés postraumático, eficacia, neurofeedback, trauma
Abstract
背景:创伤后应激障碍(PTSD)是一种使人衰弱的疾病,影响着全世界数百万人。现有治疗方法往往无法解决其症状的复杂性以及由严重和长期创伤引起的功能障碍。脑电图神经反馈(NFB)已成为一种有前途的治疗方法,旨在通过调节大脑活动来减轻 PTSD 的症状。
目的:我们对十项临床试验进行了系统综述和元分析,以回答以下问题: NFB 在不同创伤人群中解决 PTSD 和其他相关症状的效果如何,以及这些改善是否与神经生理改变有关?
方法:本综述遵循系统综述和元分析首选报告项目指南。我们考虑了所有已发表和未发表的涉及成人 PTSD 为主要诊断的随机和非随机对照试验,没有按创伤类型、共病诊断、地点或性别排除。本系统综述纳入了 10 项对照研究;七项随机对照试验(RCTs)和三项干预非随机研究(NRSI),被试总数n = 293(128名男性)。元分析仅纳入了 RCT ( 215 名被试; 88 名男性)。
结果:所有纳入的研究都表明, NFB 在减轻 PTSD 症状方面优于对照组,有迹象表明焦虑和抑郁症状以及相关的神经生理改变有所改善。汇总数据的元分析显示,治疗后 PTSD 症状 SMD 有 –1.76(95% CI −2.69,−0.83)的显著降低, NFB 组的平均缓解率 (79.3%) 高于对照组 (24.4%)。然而,所综述的研究大多规模较小,人群具有异质性,质量参差不齐。
结论: NFB对 PTSD 症状的影响是中等的,机制证据表明 NFB 导致大脑功能的治疗变化。未来的研究应侧重于更严格的方法设计,扩大样本量和更长的随访时间。
关键词: 系统综述, 元分析, PTSD, 疗效, 神经反馈, 创伤
1. Introduction
Posttraumatic stress disorder (PTSD) is a debilitating mental health condition that affects people who have experienced traumatic or life-threatening events, including war experiences, sexual and physical assault, childhood abuse and neglect, witnessing violent harm, and natural disasters. PTSD is characterised by re-experiencing traumatic events, avoiding trauma-related stimuli, increased arousal, and negative alterations in mood and cognition (American Psychiatric Association, 2013), while exposure to severe and chronic trauma, as described in the ICD-11, can also lead to affect dysregulation, altered self-perception, and interpersonal disturbances (World Health Organization, 2019) as seen in Complex PTSD.
A cross-national lifetime prevalence of PTSD among trauma-exposed individuals is substantial (5.6%), with half of the reported global cases experiencing persistent symptoms (Koenen et al., 2017). Psychiatric comorbidities, such as depressive, generalised anxiety and alcohol use disorder, are common in PTSD (Walter et al., 2018), as are increased physical health issues (McFarlane, 2010; Pacella et al., 2013). PTSD can lead to increased direct health care and unemployment costs (Davis et al., 2023), and significant impairment in daily functioning (Jellestad et al., 2021).
In spite of the robust evidence for the effectiveness of trauma-focused psychological interventions for PTSD, such as prolonged exposure therapy, cognitive processing therapy, Eye Movement Desensitisation and Reprocessing (EMDR), and pharmacological interventions such as fluoxetine (Lewis et al., 2020; de Moraes Costa et al., 2020), the existing treatments for PTSD are only partially effective. A systematic review and meta-analysis by Varker et al. (2021) indicated high dropout rates (20.9%) for guideline recommended psychological PTSD treatments. Treatment effects were insufficient in addressing disturbances in self-organisation and emotional dysregulation, which are the core symptoms in those exposed to severe and cumulative traumas (Karatzias et al., 2019; Liddell et al., 2019). Poor self-regulation has been identified as one of the principal causes of failure of exposure-based treatments for PTSD (Coventry et al., 2020; Jaycox & Foa, 1996), suggesting a need for the development of more effective interventions.
Neuroscience research has provided important new insights into the brain mechanisms of PTSD, contributing to the development of new treatment approaches. Recent functional imaging studies show disruptions in intrinsic connectivity networks that contribute to the manifestation and maintenance of PTSD symptoms (Breukelaar et al., 2021; Terpou et al., 2020). Altered functioning of the major brain networks was associated with specific clinical symptoms observed in PTSD (Lanius et al., 2015), including cognitive dysfunction (Central Executive Network), increased and decreased arousal/interoception (Salience Network), and an altered sense of self (Default Mode Network).
Focusing on EEG studies, dysfunctional brain wave patterns have emerged, including reduced relative power of alpha rhythms (Clancy et al., 2017) and elevated relative power of beta rhythms (Huang et al., 2014). Observed alpha deficits were associated with sensory disinhibition, hypervigilance, and chronic hyperarousal linked to altered functioning within the Salience (Nicholson et al., 2016) and Default Mode Networks (Clancy et al., 2020). Increased beta activation in people with PTSD was linked to the general state of hyperarousal (Kay & Buysse, 2017), sleep disturbances (Colombo et al., 2016), or cognitive flexibility deficits (Popescu et al., 2023).
With the increasing evidence for altered functioning of the major brain networks in PTSD (Lanius et al., 2015; Terpou et al., 2020), research that evaluates neuroscience-driven treatment interventions to target specific PTSD symptoms is justified (Lanius et al., 2015).
Electroencephalographic Neurofeedback (EEG-NFB) is an emerging psychophysiological intervention aiming to increase the brain's capacity to self-regulate. The technique involves using electroencephalography (EEG) to measure the patient's ongoing brainwave activity, which is then presented to them in real-time using a simple stimulus (e.g. a visual or auditory cue) as feedback. Through operant conditioning, the patient learns to produce the desired brainwave activity while reducing dysfunctional electrical oscillations (Enriquez-Geppert et al., 2017; Nicholson, Ros, Densmore, et al., 2020; Ros et al., 2014). EEG-NFB aims to tap into the brain's inherent neuroplasticity, allowing it to retrain itself to function more optimally. It is particularly advantageous for patients with PTSD who experience high levels of anxiety, dysregulation, or dissociation, and who may not be receptive to or benefit from other treatment options (Nicholson, Ros, Densmore, et al., 2020). With training, patients become better at self-regulation, and regulation of emotional arousal in particular [van der Kolk et al. (2016), Gapen et al. (2016)].
A significant association was reported between the re-establishment of alpha power and the decrease of PTSD-related symptoms of hyperarousal using an alpha desynchronisation/rebound protocol (Ros et al., 2017), while an alpha/theta training protocol, developed to alleviate anxiety associated with alcoholism (Peniston & Kulkosky, 1989; Peniston & Kulkosky, 1990; Saxby & Peniston, 1995), and to reduce PTSD symptoms (Peniston & Kulkosky, 1991), was associated with increased brainwave synchrony (Peniston & Kulkosky, 1991).
In their single NFB session of alpha-down at Pz placement, Ros et al. (2013) demonstrated that tonic alpha desynchronisation at the midline parietal cortex is associated with amplified dorsal anterior cingulate cortex/midcingulate cortex (dACC/MCC) connectivity, a part of the SN, whose function is disrupted in PTSD (Daniels et al., 2010). Their findings led to the conclusion that NFB has a global rather than local effect on brain functioning (Ros et al., 2014) through activating specific neural networks (Zeynali & Seyedarabi, 2019) and that different electrode placements may have a similar effect on the neural networks affected by trauma.
The previous systematic reviews of the effectiveness of EEG-NFB in PTSD generally reported a moderate to large effect on reducing PTSD symptoms (Hong & Park, 2022; Panisch & Hai, 2020; Reiter et al., 2016: Steingrimsson et al., 2020), with a low certainty of evidence. For example, Steingrimsson et al. (2020) concluded that although there is evidence to suggest that neurofeedback may be an effective treatment for PTSD, the quality of the studies included in the review varied widely. The main limitation of this meta-analysis was the small number of included studies with small sample sizes and heterogeneity of treatment protocols. This limitation prevented any subgroup or sensitivity analyses and limited conclusions about the effectiveness of neurofeedback and its implementation in clinical practice. Since this review, several RCTs have been published, allowing for a more definitive answer to the question of the effectiveness of EEG Neurofeedback for PTSD.
Our systematic review was conducted to answer the question: how effective is EEG-NFB in addressing the symptoms of Chronic PTSD and other associated symptoms, compared with sham EEG-NFB, other interventions, waiting list, or no intervention? We were also interested in investigating any differences in the effectiveness of EEG-NFB across different trauma populations. Lastly, we aimed to explore whether improvements in symptoms were related to neurophysiological changes.
2. Method
The review is registered on PROSPERO (Registration number CRD42021278837) and follows PRISMA guidelines (Moher et al., 2009).
2.1. Eligibility criteria
Eligible studies met the following criteria: a) study participants were traumatised adults diagnosed with PTSD as a primary diagnosis, ≥ 18 years; b) having PTSD symptoms for at least 3 months or longer; c) the Neurofeedback (NFB) intervention was based on an electroencephalogram (EEG); d) the intervention was compared to sham NFB, other treatment, or waitlist; e) primary outcome was change in PTSD symptom score pre to post-intervention as assessed through diagnostic interviews based on the criteria outlined in the DSM-5.
2.2. Search strategy
We undertook a systematic literature search using PubMed, PsycINFO, Embase, ERIC, Web of Science, Cinahl, Scopus, and Cochrane databases in October 2021. The following search profile was used: ‘Neurofeedback’ OR ‘Neurotherapy’ OR ‘EEG Biofeedback’ combined by AND with ‘PTSD’ OR ‘post traumatic stress disorder’ OR ‘developmental trauma’. Search term expansion was used when available. No restrictions were applied to the date of publication. Articles were selected based on relevance as judged by title and abstract screening. References to selected studies were also examined. Only randomised control trials (RCT) and non-randomised studies of interventions (NRSI) enrolling adult patients with a primary diagnosis of PTSD were included. Studies that used NFB, along with other treatment modalities, were also included. No restrictions regarding traumatic events and types of trauma were applied. Cross-sectional and single-arm studies, narrative reviews, single and series case studies, non-human studies, and studies with children were excluded. Search sources also included bibliographic databases, reference lists of eligible studies and review articles, key journals, conference proceedings, trial registers, Internet resources, and contact with study investigators. The additional search with added search terms (‘psychological trauma’ or ‘emotional trauma’) was performed on 14 April 2023, to ensure the most up-to-date review.
2.3. Study selection and data extraction
After the initial screening of titles and abstracts for eligibility by the first reviewer, two reviewers independently reviewed full texts for papers that met inclusion criteria or those in which eligibility was unclear. The authors were blinded to each other's review, and the individual decisions were sent to the third reviewer for final group review and resolution of any disagreement.
Data was extracted on the population demographics (including study population, number of participants, age, gender and context of the study, diagnosis, and type of trauma), study design, exclusion criteria, intervention components (neurofeedback protocol and other interventions), control intervention components, outcome measures.
Primary outcomes were changes in PTSD symptoms score from baseline to the last available follow-up. The outcome measures (e.g. Harvard Trauma Questionnaire, PTSD Checklist for DSM-5, Clinician-Administered PTSD Scale, Davidson Trauma Scale and Impact of Event Scale – Revised) were based on the Diagnostic and Statistical Manual of Mental Disorders criteria (American Psychiatric Association, 2013). In studies where multiple measures were used, all results were added to Table 2. The results of the structured clinical interviews were prioritised over the results based on subjective measures of distress and included in the meta-analysis. In studies where only self-reported measures were used, a measure that was used in most studies (such as PCL-5) was included in the meta-analysis.
Table 2.
Reported effects on PTSD symptoms and risk of bias.
| Study (Author, year) | Type of trauma | Dropout | Results NF Group | Results Control Group | Between Group Difference Pre-Post/Length of follow up | Remission Rate | Risk of Bias | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| rp | dii | md | Mo | srr | o | |||||||
| Peniston & Kulkosky, 1991 | Combat PTSD | NF: 0/15 | Pre: 30.6 ± 9.1 | Pre: 35.9 ± 7.2 | Δ – 20.4, p < .05 MMPI PTSD subscale; 30 months follow up | NF: 80% | - | + | + | + – | + | - |
| CL: 0/14 | Post: 10.5 ± 6.2 | Post: 36.2 ± 5.3 | Cl: 0% | |||||||||
| Δ – 20.1 (−66%) | Δ + 0.3 (1%) | p < .05 between groups | ||||||||||
| Kelson, 2013 | Combat PTSD | NF: 0/5 | Pre: 72.8 ± 12.6 | Pre: 69.4 ± 10.0 | Δ – 38.0, p < .01 | NF: 100% | + | - | - | - | + | - |
| CL: 0/5 | Post: 44.2 ± 9.6 | Post: 78.8 ± 9.0 | Non-validated PTSD questionnaire; | CI: 0% | ||||||||
| Δ – 28.6 (−39%) | Δ + 9.4 (12%) | No follow up | ||||||||||
| van der Kolk et al., 2016 | Multiple treatment resistant traumas (developmental trauma and domestic violence) | NF: 6/28 | Pre: 79.5 ± 16.9 | Pre: 76.2 ± 16.9 | Δ – 26.8, p < .001 | NF: 73% Cl: 32% p = .007 |
+ | + | + | + | + | + |
| CL: 2/24 | Post: 43.0 ± 20.2 | Post: 66.5 ± 20.6 | CAPS-4; | |||||||||
| Δ – 36.5 (−46%) | Δ – 9.7 (−13%) | 30 days follow up | ||||||||||
| Pre: 67.3 ± 9.7 | Pre: 63.0 ± 10.5 | Δ – 18.3, p < .001 | ||||||||||
| Post: 44.2 ± 8.4 | Post: 58.2 ± 8.9 | DTS; | ||||||||||
| Δ – 23.1 (−34%) | Δ – 4.8 (−8%) | 30 days follow up | ||||||||||
| Noohi et al., 2017 | Combat PTSD | NF: 0/15 | Pre: 47.2 ± 7.6 | Pre: 51.1 ± 5.4 | Δ – 16.8, p < .001 | Not reported | + – | - | - | - | + | - |
| CL: 0/15 | Post: 30.4 ± 6.2 | Post: 51.1 ± 6.2 | IES-R; | |||||||||
| Δ – 16.8 (−36%) | Δ 0.0 (0%) | 43 days follow up | ||||||||||
| Bell et al., 2019 | Combat PTSD | NF: 0/12 | Pre: 46.17 ± 14.23 | Pre: 49.82 ± 10.16 | Δ – 9.45, p > .5 | Not reported | - | + | + | + | + | - |
| Cl: 1/11 | Post: 18.08 ± 12.65 | Post: 31.18 ± 13.53 | PCL-5; | |||||||||
| Δ – 28.09 (−61%) | Δ – 18.64 (−37%) | No follow up | ||||||||||
| Nicholson, Ros, Jetly, et al., 2020 | Mixed treatment resistant trauma (developmental, military, first responders) | NF: 0/18 | Pre: 36.8 ± 10.3 | Pre: 39.94 ± 7.83 | Δ – 5.3, | NF: 61.1% Cl: 33.3% p = .040 |
+ | + | + | + | + | + |
| CL:0/18 | Post: 24.3 ± 15.6 | Post: 32.78 ± 12.27 | CAPS-5; | |||||||||
| Δ – 12.5 (−34%) | Δ – 7.2 (−18%) | 3 months follow up | ||||||||||
| Askovic et al., 2020 | Refugee and war trauma | NF: 0/13 | Pre: 2.8 ± 0.4 | Pre: 3.2 ± 0.5 | Δ – 0.8, p > .002 | NF: 92% Cl: 8% |
- | + | ? | - | + | - |
| CL: 0/13 | Post:1.9 ± 0.5 | Post: 3.1 ± 0.6 | HTQ-16; | |||||||||
| Δ −0.9 (−32%) | Δ −0.1 (−3%) | No follow up | ||||||||||
| Leem et al., 2021 | Mixed trauma: domestic violence (16), traffic accidents (2), school violence (1) | NF: 1/11 | Pre: 44.3 ± 10.8 | Pre: 35.1 ± 18.5 | Δ – 20.8, p < .01 | Not reported | + | + | - | + | + | - |
| Cl: 2/11 | Post: 19.4 ± 7.8 | Post: 31.0 ± 14.9 | PCL-5-K; | |||||||||
| Δ – 24.9 (−56%) | Δ – 4.1 (−12%) | 30 days follow up | ||||||||||
| Pre: 47.5 ± 16.8 | Pre: 34.6 ± 16.9 | Δ – 18.4 p < .05 | ||||||||||
| Post: 25.6 ± 10.5 | Post: 31.1 ± 16.6 | IES-R-K; | ||||||||||
| Δ – 21.9 (−46%) | Δ – 3.5 (−10%) | 30 days follow up | ||||||||||
| du Bois et al., 2021 | Victims of genocide | NF: 0/10 | Pre: 38.9 ± 16.7 | Pre: 34.4 ± 23.8 | Δ – 22.2, p < .01 | NF: 70% CL: not reported |
- | + | + | +- | + | - |
| CL: 0/10 | Δ – 27.9 (−72%) | Δ – 5.7 (−17%) | No follow up | |||||||||
| Post: 11.0 ± 5.5 | Post: 28.7 ± 20.1 | PCL-5; | ||||||||||
| Pre: 2.2 ± 0.5 | Pre: 2.1 ± 0.7 | Δ – 0.7, p < .01 | ||||||||||
| Post: 1.3 ± 0.2 | Post: 1.9 ± 0.6 | HTQ; | ||||||||||
| Δ – 0.9 (−41%) | Δ – 0.2 (−10%) | No follow up | ||||||||||
| Pre: 3.2 ± 1.1 | Pre: 3.0 ± 1.7 | Δ – 2.3, p < .01 | ||||||||||
| Post: 0.3 ± 0.7 | Post: 2.4 ± 2.0 | PC-PTSD; | ||||||||||
| Δ – 2.9 (−94%) | Δ – 0.6 (−20%) | No follow up | ||||||||||
| Winkeler et al., 2022 | Multiple traumas with first trauma happened in childhood (sexual, physical and emotional abuse, neglect) | NF: 0/18 | Pre: 11.1 ± 0.6 | Pre: 11.2 ± 0.7 | Δ – 0.6, p = .05 | NF: not reported Cl: not reported |
+ | + | + | +- | + | +- |
| CL: 2/18 | Post: 10.3 ± 1.0 | Post: 11.0 ± 1.1 | PCL-5; | |||||||||
| Δ – 0.8 (−7%) | Δ – 0.2 (−2%) | No follow up | ||||||||||
Abbreviations: PTSD, posttraumatic stress disorder; N.F., neurofeedback; CI, control intervention; Δ, difference; A negative between-group difference in change indicates a difference in favour of neurofeedback; MMPI, Minnesota Multiphasic Personality Inventory; CAPS, Clinician Administered PTSD Scale; intervention; IES-R, Impact of Event Scale-Revised;. PCL, PTSD Checklist; HTQ, Harvard Trauma Questionnaire; rp, randomisation process; dii, deviation from intended intervention; md, missing outcome data; mo, measurement of the outcome; srr, selection of the reported result; o, overall risk of bias; –,high risk of bias; +, low risk of bias; + -, some concerns of bias.
Secondary outcomes included changes in other symptoms (such as anxiety and depression), social and executive functioning changes, significant side effects, self-harm, suicidal behaviour, medication, remission rate, and associated neurophysiological changes. We also included the effect size, mean, confidence intervals, changes from baseline and follow-up, the difference between intervention and control groups, and statistical significance.
2.4. Risk of bias and certainty of evidence
The primary reviewer assessed the risk of bias for the primary outcome, and then the second reviewer undertook a quality check. The RCTs were assessed by the Cochrane Risk of Bias Tool 2 (Higgins et al., 2022) and NRSIs by Cochrane's ROBINS-I tool (Sterne et al., 2016).
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to assess the overall certainty of evidence (Schünemann et al., 2013). The primary reviewer assessed the overall certainty of the evidence, and then the second reviewer undertook a quality check.
2.5. Meta-analyses
We conducted a meta-analysis to examine the effects of NFB on the severity of PTSD symptoms. Although non-randomised and randomised controlled trials were all included in the review, only RCTs were used in the meta-analyses. We separately analysed RCTs with a low and high risk of bias to further check the validity of findings. Statistical analyses were completed in RevMan Version 5 (RevMan Web, 2020). We assessed the heterogeneity of studies by their tau-squared value, the chi-squared test, and the I-squared value. Linear mixed-effects models were implemented to assess the overall effect of the intervention. Studies were weighted inversely proportional to their variance. The overall effect was described by the corresponding p-value, and the individual effect of each study was described by a standardised mean difference and 95% confidence interval. A forest plot summarised this information.
In addition, we used the narrative synthesis approach (Ryan, 2013) to summarise data that we could not analyse using meta-analysis.
3. Results
3.1. Search results
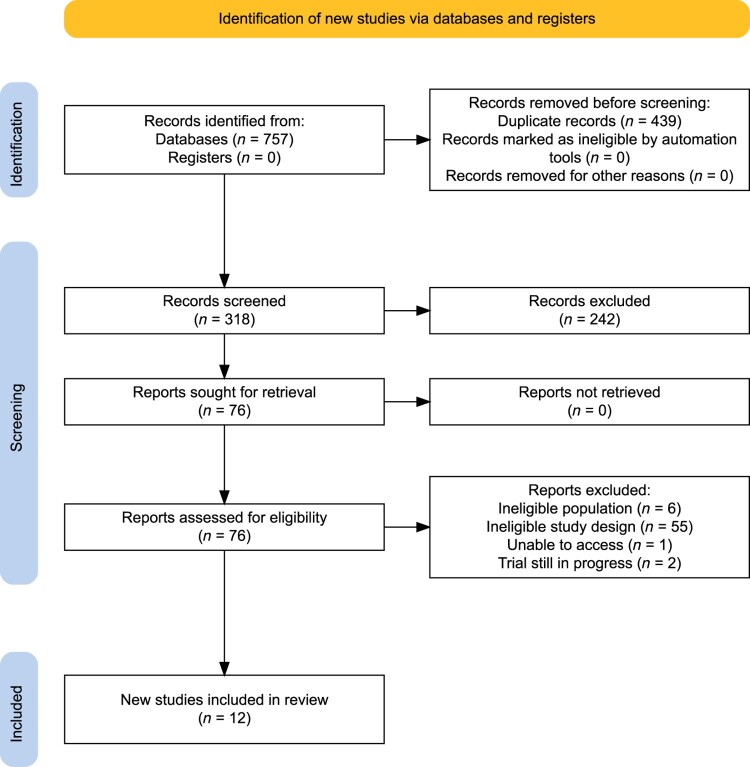
The literature search identified 318 articles after the removal of duplicates. After reading the abstracts, 242 articles were excluded. Another 64 articles were excluded by two authors (M.A. and N.S.) in consensus after reading the articles in full text. The remaining twelve articles were included for further analysis.
A flowchart of the study selection process is presented in Figure 1.
Figure 1.
Flow diagram of identification, screening, and eligibility of the systematic review.
This review includes twelve studies, consisting of seven randomised controlled trials (RCTs) and three non-randomised studies of intervention (NRSIs), and two additional papers with the analysis of secondary outcomes (Nicholson et al., 2023: Shaw et al., 2023) based upon the original study by Nicholson, Ros, Densmore, et al. (2020). All studies were published in peer-reviewed journals and involved a total of 293 participants (128 male) between the ages of 25–60. The studies have been conducted in different countries, including the United States of America, Australia, Canada, Iran, South Korea, and Rwanda. Participants experienced symptoms of PTSD resulting from various forms of trauma, such as combat (veterans), childhood abuse or neglect, domestic violence, first responders, traffic accidents, school violence, war, genocide, and refugee trauma. The time post-trauma ranged from six months to several decades. The majority of participants across all studies had experienced multiple traumas over a prolonged period of time. Seven studies required participants to meet diagnostic criteria for PTSD, while one study required participants to score above the cut-off of a self-rating PTSD measure, and one study selected participants on the basis of a non-validated PTSD symptom questionnaire. Comorbid psychiatric disorders were reported in four studies, including Bipolar Disorder, Eating Disorder, Alcohol Use Disorder, Mood Disorders, Anxiety, and Somatic Symptoms Disorder.
Comparators in the studies varied, with three studies comparing Neurofeedback to a waitlist group that continued to receive treatment as usual, and four studies comparing Neurofeedback with another intervention (heart rate variability biofeedback, motor imagery, media-supported relaxation, and traditional medicine). One study used sham control, one compared Neurofeedback to no treatment, and another did not specify the control group. The risk of bias was significant in eight studies, while only two studies met all quality criteria. Key characteristics of the included studies are summarised in Table 1.
Table 1.
Characteristics of the study population, design and treatment intervention.
| Study (author, year) | Study design | Population/type of Trauma | No of participants/Gender | Age | Additional Diagnosis | Exclusion Criteria | Duration and frequency of treatment/Neurofeedback Protocol/Sensor Placement | Adjunct interventions | Control Intervention |
|---|---|---|---|---|---|---|---|---|---|
| Peniston & Kulkosky, 1991 | RCT | Vietnam combat veterans with PTSD | N = 29; 29 male | 36.68 ± 2.72 | Not reported | Psychotic symptoms; organic dysfunction | 30 sessions of Alpha/Theta training, 5 days a week; 30 min session; Sensor placement: O1 | Experimental group only: Pre-training: 8 × 30-min temperature biofeedback, autogenic training and rhythmic breathing technique. Both groups were on psychotropic medications: Tricyclic antidepressants, anxiolytics and antipsychotics. | Traditional medicine: psychotropic medications combined with individual and group therapy |
| Kelson, 2013 | RCT | Army veterans living in poverty (homeless or nearly homeless) | N = 10; 10 male | 25–60 y | Bipolar disorder or drug/alcohol addiction | Psychosis | 20 session over 4 weeks, 30 min session of Infra Low Frequency Training; Sensors placements based on the Othmer Protocol Guide (2012) with T3–T4 and T4–P4 as starting protocols | All were on psychotropic medication. | Not receiving EEG Biofeedback |
| van der Kolk et al., 2016 | RCT | Adults exposed to multiple traumas (childhood caregiver emotional abuse; sexual abuse; domestic violence) and treatment resistant PTSD | N = 52; 7 male | 44.40 ± 13.15 | Not reported | Unstable medical condition; Disability benefits; Suicide risk; Psychotic or bipolar disorder; TBI; Seizure disorder; SUD; DV; Changing ongoing treatment during study; GAF score <40. | 24 bi-weekly sessions; 30 min session of High alpha training Starting reward frequency of 10–13 Hz and inhibit frequencies of 2–6 and 22–36 Hz. Adjustment of the reward band was based on subjects’ responses. Sensor placement: T4–P4 | Required to continue all ongoing treatments (psychotherapeutic and pharmacological) with no changes to their treatment regimens. Reported medication: SSRIs, benzodiazepines, anxiolytics, Bupropion, SNRI tricyclic antidepressant, stimulants, antipsychotics. | Waitlist receiving psychotherapy and medication |
| Noohi et al., 2017 | RCT | Adult patients (war/combat) with PTSD referred to hospital | N = 30; 30 male | 25–60 y | Not reported | Psychotic and bipolar disorders; Serious limiting physical illness, such as cancer or kidney problems | 25 sessions four times week; 30–40 min sessions of Alpha Theta training; Sensor placement: Pz | Not reported | Not reported |
| Bell et al., 2019 | NRSI | Traumatized individuals (childhood abuse or neglect; domestic violence; first-responders; military veterans) with PTSD and at least 6 months post traumatic event | N = 23; 23 male | 44 ± 16 | MDD; Anxiety disorder; ADD, Fibromyalgia/Chronic Pain; Bipolar Disorder OCD; Dysthymic Disorder | Personality disorders (Axis II DSM-V); Suicidal ideation; Psychosis; TBI; Seizure disorder; significant unstable medical conditions; Pregnancy; Personality disorder. | 15 bi-weekly sessions; 20 min session of Low Resolution Electromagnetic Tomography Analysis (LORETA) Z-score neurofeedback training targeting 3 brain networks (Default Mode Salience and Central Executive Network). Sensor placement: 19 channel corresponding to the 10–20 international system | Concurrent psychotherapy and medication 18 participants on psychotropic medication, not specified. | HRV Biofeedback |
| Nicholson, Ros, Jetly, et al., 2020 | RCT double-blind | Traumatised individuals (military veterans; first responders; physical/sexual abuse or neglect) who had not responded to at least six months of trauma-focused psychotherapy | N = 36; 10 male | 42.18 ± 11.63 | MDD; Somatisation disorder Specific phobia | SUD; bipolar or psychotic disorders; in another primary trauma focused treatment; previous biofeedback treatment; suicidal ideation Unstable living conditions; DV; Noncompliance with 3 Tesla fMRI safety standards; Significant untreated medical illness; Pregnancy; Neurological or pervasive developmental disorders; TBI | 20 weekly sessions; 20 min session of down-regulation of alpha rhythm (8–12hz); Sensor placement: Pz | Psychotropic medication: Antidepressants; SSRIs; SNRIs; tricyclics; atypical antipsychotics; sedatives; benzodiazepines; cyclopyrrolone and stimulants (methylphenidate). | Sham neurofeedback |
| Askovic et al., 2020 | NRSI, retrospective | Adult refugees with chronic PTSD | N = 26; 17 male | 44.85 ± 9.9 | Anxiety; Depression | Current substance use disorder, severe neurological conditions, developmental delay, or need for urgent medical care. | 27 (SD 12) sessions over 46 weeks (SD 32 weeks); 20 min session of individualised neurofeedback training protocols to target hyperarousal symptoms (anxiety, fear, insomnia), instability and problems with attention. Sensor placement: T4–P4 T3–T4 Cz–A2 or C4–A2 Fz-A1 |
Trauma counselling and medication. 13 participants on psychotropic medication, not specified. | Waitlist receiving trauma counselling |
| Leem et al., 2021 | RCT | Traumatized individuals, traumatic events occurred more than 6 months before recruitment. | N = 22; 2 male | 43.98 ± 16.35 | Not reported | Severe mental disease (past or recent); when it is necessary to administer continuously a substance that is judged to have an effect on the induction of symptoms. | 16 bi-weekly sessions; 50 min session of Alpha-theta training; Sensor placement: Pz | Allowed to continue on any drugs or nonpharmacological treatments that were previously being taken. | Waitlist receiving treatment as usual and life style intervention |
| du Bois et al., 2021 | NRSI (3 arms) | Genocide survivors in Rwanda, high scores for PTSD in a previous study on transgenerational transmission of PTSD | N = 29; 29 female | 53.72 ± 6.094 | Not reported | Not reported | 7 sessions; 25 min session of down-regulation of alpha rhythm (8–12hz); Sensor placement: Pz | Not reported | No treatment/Motor Imagery |
| Winkeler et al., 2022 | RCT | Adults admitted to an inpatient treatment programme for eating disorders diagnosed with PTSD, with a history of childhood trauma | N = 36; 36 female | 27.11 ± 5.28 | Eating disorder; and frequent diagnosis of depression and emotionally unstable personality disorder | Treatment experience with NFB as well as epileptic seizures in patients' history | 12 sessions; 30 min of Infra-low frequency training; Sensor placement: T4–P4, T3–T4, and T4–FP2 | Regular inpatient treatment programme (individual psychotherapy 75 min per week, group psychotherapy 150 min per week + body awareness therapy, creative therapy, physical activity adapted to the physical condition, psychoeducation, nutritional counselling, and mealtime support as needed.) | Media Supported Relaxation |
3.2. Characteristics of neurofeedback intervention
The majority of reviewed studies (Askovic et al., 2020; du Bois et al., 2021; Nicholson, Ros, Jetly, et al., 2020; Noohi et al., 2017; Peniston & Kulkosky, 1991; van der Kolk et al., 2016 and Leem et al., 2021) were based on the EEG amplitude NFB training (Perl & Perl, 2019), also called frequency/power NFB (Marzbani et al., 2016) with standard inhibit and reward frequencies (1–36hz). In a review by Perl and Perl (2019), EEG amplitude NFB training composes most (over 70%) of all reviewed NFB studies. In frequency/power NFB included in our review, varieties of alpha/theta training protocols were used in three studies (Leem et al., 2021; Noohi et al., 2017; Peniston & Kulkosky, 1991), while three studies were focused on the modulation of alpha rhythm (du Bois et al., 2021; Nicholson, Ros, Densmore, et al., 2020; van der Kolk et al., 2016). The Askovic et al. (2020) study began by rewarding sensory motor rhythm (12–15 Hz) and progressing to training alpha and theta rhythms.
Two studies (Kelson, 2013; Winkeler et al., 2022) employed infra-low frequency neurofeedback (ILF NF) based on very slow electrical potential shifts (below 0.1 Hz) that are extracted from the EEG signal to create the feedback. Unlike frequency/power NFB which utilises an operant conditioning approach, ILF NF initiates an implicit learning process by providing continuous real-time feedback on brain activity within the infra-low frequency range. This process specifically targets the fundamental level of arousal and the degree of excitability within the central nervous system (Kirk, 2020).
The research conducted by Bell et al. (2019) utilised LORETA Z-score neurofeedback, which involved analysing participants’ individual EEG data using LORETA imaging. The analysis was aimed at identifying particular brain regions displaying abnormal activity patterns, and subsequently quantifying the extent of deviation from the norm using Z-scores. During the neurofeedback training, participants received feedback based on these z-scores, with the objective of guiding their brain activity toward a more optimal range.
3.3. Publication bias
We extended the search using our initial search terms to three ‘grey literature’ databases (MetaRegistry of Controlled Trials, OpenGrey, Index to Thesis). The search returned no additional articles different from the initial search.
3.4. Risk of bias and certainty of evidence
Effects on PTSD symptoms were assessed in seven RCT and three NRSI studies (Table 2). Only RCTs were included in the meta-analysis. We performed a sensitivity analysis based on the risk of bias. We separated Low Risk of Bias (LRB) from High Risk of Bias (HRB) studies and listed all reported effect sizes while focusing on the LRB studies when interpreting results. Studies by van der Kolk et al. (2016) and Nicholson, Ros, Densmore, et al. (2020) had an LRB with a well-described randomisation process, no deviation from the intended intervention, and no missing data; both applied gold-standard primary outcome measures and did not deviate from the registered protocol. Nicholson, Ros, Densmore, et al. (2020) conducted a double-blind, sham-controlled randomised trial, which is considered a reliable and unbiased study design.
Although these two studies were rated as having a low risk of bias, they were downgraded for imprecision, indicating moderate certainty of evidence (Table 3). In this case, we judged the certainty of the evidence lower than it otherwise would have been considered because of the sample size.
Table 3.
Summary of findings with estimated certainty of evidence.
| Outcome | Number and type of studies (participants), risk of bias | Absolute effect estimates | Certainty of evidence – GRADE a |
|---|---|---|---|
| PTSD symptoms | 2 RCTs (n = 88) with Low Risk of Bias |
CAPS Standardised mean difference at end of treatment in favour of NFB – 0.88 (95% CI −1.42, −0.35), p = .001 |
⊕ ⊕ ⊕ ◯ b |
| 5 RCTs (n = 127) with High Risk of Bias |
IES-R/PCL-5/MMPI-PTSD/Non-validated PTSD Questionnaire Standardised mean difference at end of treatment in favour of NFB –2.39 (95% CI −3.87. −0.90), p = .00001 |
⊕ ◯ ◯ ◯ c | |
| Symptoms of Depression | 2 RCTs (n = 49) and 1 NRSI (n = 26) with High Risk of Bias |
Beck Depression Inventory/HSCL-D Standardised mean difference at end of treatment in favour of NFB −1.37 (95% CI −2.21 to −0.53), p = .001 |
⊕ ◯ ◯ ◯ d |
| Symptoms of Anxiety | 1 RCT (n = 19) and 2 NRSI (n = 49) with High Risk of Bias |
Beck Anxiety Inventory /HSCL-A Standardised mean difference at end of treatment in favour of NFB −1.00 (95% CI −1.51 to −0.49), p = .0001 |
⊕ ◯ ◯ ◯ e |
| Medication use | 1 RCT (28) and 1 NRSI (n = 13) | Number of patients with decreased medication use NFB vs CL: Decrease: 22/22 vs. 1/18 Between-group difference: Chi2 = 36.14, p < .001 |
⊕ ◯ ◯ ◯ f |
| ⊕⊕⊕⊕ – High certainty (we are very confident that the true effect lies close to that of the estimate of the effect) | |||
| ⊕⊕⊕ ◯ Moderate certainty (we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different) | |||
| ⊕⊕ ◯ ◯ Low certainty (our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect) | |||
| ⊕ ◯ ◯ ◯ Very low certainty (we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect) | |||
a, certainty of evidence; b, downgraded one step for imprecision (due to a small number of participants and only 2 events); c,d,e,f downgraded three steps for serious risk of bias and study limitations (missing outcome data, unclear randomisation, deviation from intended intervention and bias in measurement of outcomes), high heterogeneity, indirectness, and serious imprecision.
Five studies were assessed to have a HRB (Kelson, 2013; Leem et al., 2021; Noohi et al., 2017; Peniston & Kulkosky, 1991; Winkeler et al., 2022). They were downgraded for serious risk of bias imprecision, indicating a very low certainty of evidence.
3.5. Heterogeneity
HRB studies had significantly higher heterogeneity (I2 = 89%) than the LRB studies (I2 = 32%), demonstrating larger variation in study outcomes between studies.
Studies by Peniston and Kulkosky (1991), Kelson (2013), and Noohi et al. (2017) focused on study populations with combat trauma from active military service. In contrast, studies by van der Kolk et al. (2016), Nicholson, Ros, Densmore, et al. (2020), Leem et al. (2021), and Winkeler et al. (2022) focused on a study population with civilian trauma, predominantly developmental trauma. Compared to the whole group (I2 = 86%), both the veterans and civilian groups had significantly lower heterogeneity (I2 = 0%). This needs to be tempered, given the uncertainty that comes from having a small number of studies (von Hippel, 2015).
3.6. Primary outcomes – changes in PTSD symptoms
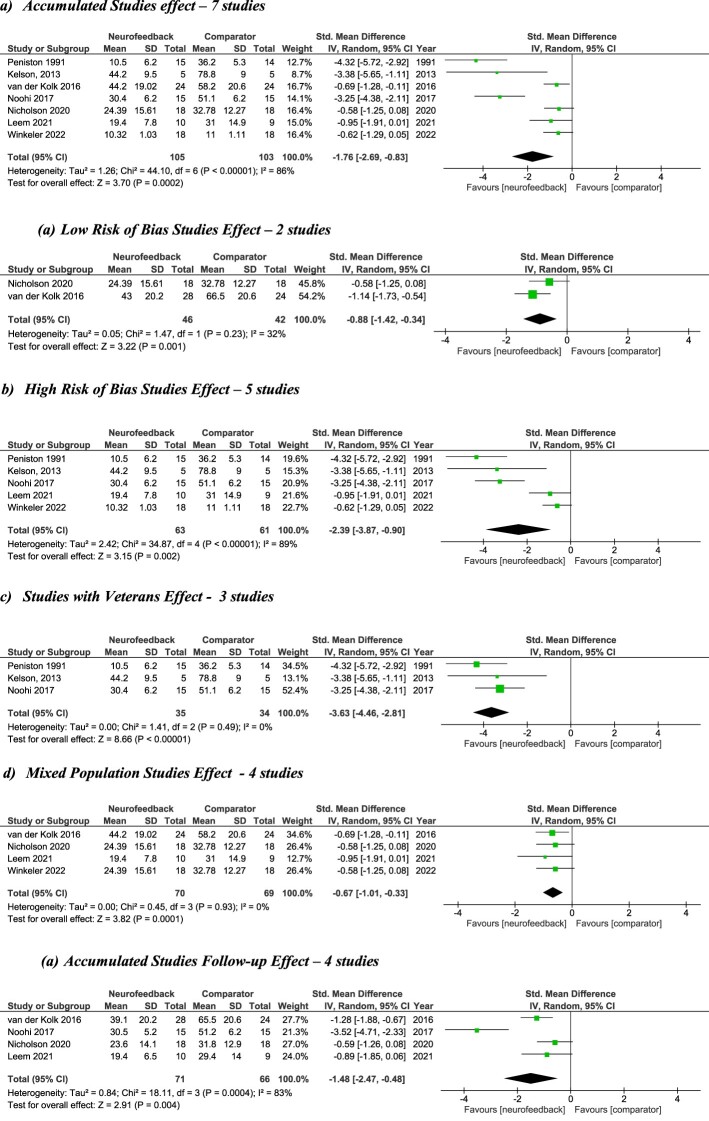
All studies showed the advantage of treatment with NFB. The NFB groups showed a reduction in PTSD symptoms post-treatment of between 7% and 72% (median 42.5%), compared with changes in the control groups ranging from a decrease of 37% to an increase of 12% (Table 2). Meta-analysis of the pooled data (HRB and LRB studies combined) shows a significant SMD of −1.76 (95% CI −2.69, −0.83; p < .01) post-treatment, demonstrating large effect size, with very low certainty of evidence. The remission rate reported in six studies (Askovic et al., 2020; du Bois et al., 2021: Kelson, 2013; Nicholson, Ros, Densmore, et al., 2020; Peniston & Kulkosky, 1991; van der Kolk et al., 2016) was higher in the NFB group (79.3%) compared to the control group (24.4%) (Figure 2).
Figure 2.
Forest plots showing change in severity of symptoms of PTSD after treatment with Neurofeedback vs control conditions. ‘Std. Mean Difference’ indicates the effect size, with 95% confidence intervals (C.I.s). The Z value and associated p value indicate whether the effect size differs significantly from zero. The squares in the figure indicate the weight of the particular study in the meta-analysis. SD, Standard deviation; IV, inverse variance; df, degrees of freedom.
3.7. Sensitivity study
3.7.1. LRB studies effect
PTSD symptoms post-treatment were significantly lower in the NFB group than the Control group (SMD = −0.88; 95% CI [−1.42; −0.34], p < .01) in the LRB studies. In the NFB group, based on six studies that reported remission rate (see Table 2), 79% of participants remitted with clinically meaningful changes (>30% reduction; Halvorsen, 2016), comparable to the 62% reported in meta-analyses of other PTSD treatment studies (Bradley et al., 2005).
3.7.2. HRB studies effect
The four HRB studies showed significantly lower PTSD symptoms in the NFB group compared to controls (−2.39; 95% CI [−3.87, −0.90], p < .01); however, the differing study design and methodology were associated with considerable heterogeneity of results. Heterogeneity was statistically significant (Chi2 = 34.87) and represented a meaningful variation in standardised mean differences (Tau2 = 2.42; I2 = 89%).
Based on GRADE, we found that the beneficial effects of NFB on symptoms of PTSD were moderate, but very low certainty of evidence. The effect of NFB persisted when studies were partitioned by the risk of bias (HRB and LRB studies combined Z = 3.70; HRB studies Z = 3.15 and LRB studies Z = 3.22), increasing our confidence (moderate certainty) that NFB compared with controls had a moderate effect on the severity of PTSD symptoms in adult patients (Table 3). This is comparable to the results reported for the best evidence-based treatments for PTSD (Watts et al., 2013).
3.8. Effect of the study population
When the effect of NFB on PTSD symptoms was considered within the veterans’ studies, PTSD symptoms were significantly lower in veterans when treated with NFB as compared to the control group (SMD −3.63; 95%, p < .01). There was no statistically significant presence of heterogeneity (Chi2 = 1.41; Tau2 = 0) and confidence intervals were relatively narrow.
When the effect of NFB on PTSD symptoms was considered in civilian participants, PTSD symptoms were also significantly lower in civilians treated with NFB as compared to a control group (SMD –0.67; p < .01), with similar heterogeneity (Chi2 = 0.45; Tau2 = 0) and confidence intervals comparable, proportional to the magnitude.
When comparing veterans to civilians, the magnitude of the standardised mean difference was greater in veterans (−3.63 vs. −0.67), suggesting a larger effect of NFB in treating combat trauma compared to civilian trauma.
4. Secondary outcomes
4.1. Changes in symptoms of depression and anxiety
Depression was measured by the Beck Depression Inventory (BDI) in two studies (Leem et al., 2021; Noohi et al., 2017) and the Hopkins Symptom Checklist −25 (HSC-25) in one study (Askovic et al., 2020). All three studies showed a significant improvement in the NFB group. As measured by the BDI, the NFB group showed a reduction in symptoms of depression pre to post-treatment ranging between 12% and 38% (median 25%), compared with changes in the control group ranging from a decrease of 12% to a minor increase of 0.4%. Meta-analysis of the pooled data shows a significant SMD of −9.00 (95% CI −16.28 to −1.72; p = .02) post-treatment; however, they had moderate to high heterogeneity (I2 = 61%).
In the study conducted by Askovic et al. (2020), it was reported that, compared with treatment as usual, the NFB group had a greater reduction of symptoms of Anxiety, F(1, 25) = 5.4, P = .030 post-therapy as measured by the HSC-25. The study conducted by Bell et al. (2019) showed a significant decrease in anxiety symptoms pre–post NFB as measured by the Beck Anxiety Inventory. There was no difference (p = .214) between the NFB and control group, although the effect of group type on anxiety was large, Cohen's d = .94. The very low certainty of evidence (based on GRADE), limits our ability to make a conclusion whether NFB compared to control intervention reduces depression and anxiety symptoms in adult patients with PTSD.
We could not analyse changes in social and executive functioning, self-harm, and suicidal behaviour, as they were reported inconsistently in the small number of studies, resulting in very little certainty of evidence.
4.2. Changes in the use of psychotropic medication
Only three studies reported medication use. While Peniston and Kulkosky (1991) and Askovic et al. (2020) indicated less need for medication following NFB, Nicholson, Ros, Jetly, et al. (2020) tried to keep medication stable during the trial to control for the medication effect.
Peniston and Kulkosky (1991) reported a significant reduction in the use of psychotropic medication in the NFB arm. Askovic et al. (2020) reported that all participants treated with NFB and none controls ceased psychotropic medication at the end of treatment. However, the very low certainty of evidence limits our ability to conclude whether NFB reduces medication use in adult patients with chronic PTSD.
4.3. Long-term effect of neurofeedback
Five of the six studies included follow-ups ranging from 1–30 months (Nicholson, Ros, Jetly, et al., 2020; Noohi et al., 2017; Peniston & Kulkosky, 1991; van der Kolk et al., 2016 and Leem et al., 2021). All studies reported continued benefits of NFB at follow-up and favourable outcomes compared to the control intervention. Meta-analysis of the pooled data (Leem et al., 2021; Nicholson, Ros, Densmore, et al., 2020; Noohi et al., 2017; van der Kolk et al., 2016) shows a significant SMD of −1.48 (95% CI −2.47, −0.48; p < .01) at follow-up. In the longest (30 months) follow-up study (Peniston & Kulkosky, 1991), only four of the twenty participants in the NFB arm had a few instances of recurrence of the nightmares/flashbacks, which resolved with booster NFB sessions (p < .05 between groups). However, due to the low quality of evidence and variability in the follow-up periods, long-lasting of effects of neurofeedback remain unclear from this analysis.
4.4. Acceptability of NFB
The acceptability of NFB treatment was measured by the dropout rate and reported adverse effects. The dropout rate across all participants in NFB treatment was 5% (7/144). This dropout rate compares favourably to the 20.9% dropout from RCTs of psychological therapies for PTSD (Varker et al., 2021). Only one participant dropped out of the study due to an adverse effect of flashbacks following NFB (van der Kolk et al., 2016). Other studies reported a temporary increase in symptoms (Bell et al., 2019; Noohi et al., 2017), which did not affect the positive outcomes of the treatment. These findings indicate that NFB is an acceptable adjunct treatment among individuals with PTSD.
4.5. Changes in neurophysiological functioning
Changes in neurophysiological functioning following neurofeedback training were investigated in six studies (Askovic et al., 2020; Leem et al., 2021; Nicholson et al., 2023; Nicholson, Ros, Jetly, et al., 2020; Peniston & Kulkosky, 1991 and Shaw et al., 2023). In all but one study (Leem et al., 2021), significant changes in neurophysiological functioning following NFB were found.
The study conducted by Peniston and Kulkosky (1991) found that alpha-theta NFB led to significant increases in synchrony between brain channel pairs in the frontal and parieto-occipital lobes of the cerebral cortex in their patients. The mean amplitudes of alpha and theta brainwaves displayed a ‘Crossover’ pattern across trials, where theta waves increased and alpha waves decreased, indicating a state of consciousness that promotes hypnagogic imagery. This state allowed previously inaccessible traumatic memories to be revisited and resolved from a lower level of arousal. The study's participants reported anxiety-free episodes during a 26-month follow-up period, and almost all participants reported the disappearance of episodes of flashbacks and nightmares.
The alpha-desynchronisation NFB study by Nicholson, Ros, Jetly, et al. (2020) observed a shift towards normalisation of Default Mode Network (DMN) and Salience Network (SN) connectivity post-neurofeedback, which was correlated with a decrease in PTSD severity and improved performance during neurofeedback training. Greater reductions in PTSD severity scores were associated with less SN connectivity with the supplementary motor cortex (SMC). At the same time, better neurofeedback training performance correlated with an increase of anterior DMN connectivity with the right posterior insula post-NFB compared to baseline. The results of this study expand upon the single session of alpha-desynchronizing EEG-NFB study (Kluetsch et al., 2014), which found that increased posterior insula connectivity post-NFB was associated with an increased subjective experience of calmness. Another alpha-desynchronisation study (du Bois et al., 2021) evaluated changes in alpha amplitude during and following NFB training compared to baseline. They demonstrated both local (Pz) and global (all EEG channels) increase in resting-state absolute alpha amplitude following NFB, compared to baseline. The observed increase in resting-state absolute alpha amplitude was consistent with previous studies that described the ‘alpha-rebound effect’ following alpha desynchronisation training associated with reductions in anxiety and hyperarousal symptoms among individuals with PTSD, and normalisation of the resting-state connectivity patterns within the DMN and SN (Kluetsch et al., 2014; Nicholson et al., 2016; Ros et al., 2017). In their randomised controlled trial, Nicholson et al. (2023) observed that alpha resynchronisation occurred within the dorsomedial prefrontal cortex, the same region that had reduced alpha power among PTSD patients at baseline. This finding suggests that alpha desynchronisation NFB can restore resting-state alpha rhythms altered in PTSD, leading to the establishment of excitatory/inhibitory balance that could be a critical neurobiological mechanism underlying the therapeutic effects of NFB in PTSD.
Two studies investigated changes in neurocognitive functioning following NFB (Askovic et al., 2020; Shaw et al., 2023).
The Askovic et al. (2020) study assessed changes in neurocognitive functioning (inhibitory control and attention) pre to post-NFB during simultaneous measurement of Event-Related Potentials (ERPs) and behavioural performance using the Go/NoGo paradigm. Askovic et al. (2020) found that neurofeedback training normalised the amplitude of P3 NoGo event-related potentials. This study's findings suggest improved cognitive control as a top-down regulatory process may underlie the alleviation of symptoms observed in PTSD patients (White et al., 2018) after neurofeedback. They also observed increased sustained attention post-neurofeedback, with a strong correlation between decreased omission errors and increased P3 NOGO (r = −0.83, P < .001).
This finding is in line with a single-session NFB study by Deiber et al. (2021) that provided mechanistic evidence of the effect of NFB on the main P300 component amplitude, which correlated with improved executive functioning in ADHD patients.
Shaw et al. (2023) conducted a study that investigated the effects of NFB on neuro-cognitive functioning under emotionally loaded tasks employed to engage top-down control of emotions. The neuroimaging results showed that alpha-down NFB improved the engagement of top-down cognitive and emotional control centres, such as the dorsolateral prefrontal cortex (dlPFC), and facilitated better integration of the anterior and posterior parts of the default mode network (DMN). Additionally, their findings suggest that improved alpha-down NFB performance correlated with increased activity in brain regions responsible for top-down control and consciousness/embodied processing of self, including the temporo-parietal junction and posterior insula.
5. Discussion
This review examined the effectiveness of NFB as an intervention for PTSD symptoms in adult patients. The results of the literature search yielded twelve articles that met the inclusion criteria, consisting of seven randomised controlled trials (RCTs), two additional outcomes papers, and three non-randomised studies of intervention (NRSIs). The studies involved a total of 293 participants between the ages of 25–60, with diverse backgrounds and experiences of trauma. The sample sizes of the individual studies varied, ranging from 10 participants to more extensive studies with over 50 participants. All studies reported high levels of comorbidities resembling the complexity of patients seen in clinical practice.
The studies employed different neurofeedback protocols, including frequency/power NFB (such as alpha/theta training and modulation of alpha rhythm), infra-low frequency neurofeedback (ILF NF), and LORETA Z-score neurofeedback. This variety highlights the adaptability of NFB to individual patients’ needs, (as different protocols can be used to target specific brainwave patterns or electrical potential shifts) as well as the lack of clarity regarding the optimal NFB treatment approach.
The remission rates observed in the NFB groups were notably higher when compared to control groups. These benefits were sustained, suggesting that the positive effects of NFB persist over time. Notably, no significant adverse effects were reported. This is particularly noteworthy considering the complex nature of PTSD and the multiple traumas experienced by the participants in the reviewed studies.
These beneficial effects are congruent with previous reviews, which all indicated the positive effects of NFB in patients with PTSD, but with a higher degree of certainty. This meta-analysis has doubled the number of study participants compared to previous meta-analyses in this area (Hong & Park, 2022; Panisch & Hai, 2020; Reiter et al., 2016; Steingrimsson et al., 2020) and a series of sensitivity analyses were also conducted, resulting in more robust and precise outcomes.
The effect size of symptom reduction from NFB shown in this meta-analysis is comparable to that found in a recent systematic review and meta-analysis of other interventions for PTSD (Coventry et al., 2020). This meta-analysis found that psychological interventions reduce PTSD symptoms more than inactive control (k = 46; n = 3,389; standardised mean difference [SMD] = −0.82, 95% confidence interval [CI] −1.02 to −0.63) and active control (k-9; n = 662; SMD = −0.35, 95% CI −0.56 to −0.14). Importantly, this meta-analysis found that multiple component interventions were the most successful approach in the treatment of PTSD.
6. Clinical implications
The effectiveness of NFB in reducing PTSD symptoms suggests that it can be considered a viable treatment option alongside existing interventions or an alternative or adjunctive treatment modality. Clinicians may consider incorporating NFB at the beginning of treatment to reduce and stabilise nervous system arousal and improve connectivity within the Default Mode and Salience Networks. This brain-based approach allows for greater accessibility and response to psychological interventions. Integrating NFB with other modalities can lead to a more holistic and individualised approach to PTSD treatment, addressing both the psychological and neurophysiological dysregulations associated with the sequale of trauma.
Additionally, the positive impact of NFB on symptoms of depression and anxiety further supports its clinical value. While the certainty of evidence for these secondary outcomes was generally low, the observed improvements in symptoms highlight the potential of NFB to address comorbid conditions often associated with PTSD.
The potential therapeutic effect of NFB in restoring neurophysiological functioning and alleviating PTSD symptoms makes it a valuable adjunctive treatment to trauma-focused interventions. It holds particular promise for individuals with chronic and complex PTSD, who often exhibit limited treatment responses from conventional treatment modalities.
7. Neurophysiological mechanisms underlying NFB
The reviewed studies reported significant improvements in brainwave synchrony (Peniston & Kulkosky, 1991), normalisation of network connectivity (Nicholson, Ros, Jetly, et al., 2020), and changes in neurophysiological functioning (Askovic et al., 2020; Shaw et al., 2023) following NFB, which are associated with the amelioration of PTSD symptoms.
These neurophysiological changes observed following NFB reflect the restoration of the brain's excitatory/inhibitory balance (Shaw et al., 2023), leading to improvement in patients’ ability to self-regulate their emotions and responses to trauma-related triggers. This targeted approach has the potential to yield meaningful and sustainable improvements in symptom severity for patients with PTSD.
However, it is important to note that while the evidence supports the association between neurophysiological changes and symptom improvement, the specific mechanisms underlying these changes have just begun to emerge. Further research is needed to deepen our understanding of the neurobiological effects of NFB, different treatment protocols, and their relationship to PTSD symptom reduction.
8. Limitations
While the findings regarding the effectiveness of neurofeedback (NFB) as an intervention for PTSD symptoms are promising, there are important limitations to consider. Firstly, this review has methodological limitations as only one person assessed the risk of bias, potentially introducing the first reviewer's influence. As limited search terms were used, there is also a possibility of studies being missed, creating a risk of bias.
Additionally, the studies included in this review utilised various types of NFB interventions, making it challenging to determine the most effective approach. The lack of standardised protocols, treatment procedures, and duration further complicates the comparison of results across studies. This highlights the need to establish optimal NFB protocols and treatment parameters for enhanced effectiveness and consistency, which becomes more challenging when we consider neurofeedback as a form of individualised medicine.
Heterogeneity was observed across the included studies, attributed to differences in participant characteristics, trauma histories, comorbidities, and variations in the implementation of NFB interventions. These factors need to be considered when interpreting the results and generalising the findings to broader populations. The assessment of outcomes in the included studies varied, with different measures used to evaluate PTSD symptoms, depression, anxiety, and other related symptoms. To provide more robust evidence regarding the benefits of NFB, standardised clinical measures and consistent assessment of clinical changes across studies would be beneficial.
The small sample sizes in most studies included in this analysis limit the generalizability and statistical power of the findings.
9. Research implications – future directions
It is important to note that while the reviewed studies provide promising evidence for the effectiveness of NFB, the overall certainty of the results varied from moderate to very low. This highlights the need for further research, particularly well-designed multicentre randomised controlled trials (RCTs) with larger sample sizes, diverse populations, consistent treatment protocols, and long-term follow-up assessments. These efforts are crucial to strengthen the evidence base and confirm the clinical benefits of NFB for PTSD treatment.
Expanding the scope of outcome measures beyond symptom reduction is crucial. Future studies should consider measuring changes in cognitive functioning, affect regulation, salience detection, and arousal, among other relevant dimensions. This comprehensive understanding of the clinical benefits following NFB will provide insights into the broader impact of NFB on various aspects of PTSD and individuals’ overall well-being.
Investigating the technical aspects of NFB protocols is necessary to determine optimal parameters, including the duration and intensity of treatment and the potential need for booster sessions. This information will contribute to refining treatment protocols and optimising the delivery of NFB interventions.
Incorporating measures of therapeutic engagement in future studies can help explore the impact of the therapeutic relationship and the role of highly trained trauma-informed clinicians in NFB outcomes. Understanding the influence of supportive relationships on treatment efficacy can guide the development of effective therapeutic frameworks and inform clinical practice.
Further integration of advanced neuroimaging techniques, including functional magnetic resonance imaging (fMRI) and quantitative electroencephalography (QEEG), can deepen our understanding of the neural circuitry abnormalities linked to post-traumatic stress disorder (PTSD). Subsequently, efficacy studies on neurofeedback (NFB) can further clarify NFB's ability to effectively modulate these pathological circuits and examine potential correlations between brain-related changes and positive clinical outcomes.
Future research in neurofeedback and PTSD should adopt a multidimensional approach, encompassing standardised measures, long-term follow-up, expanded outcome assessment, technical optimisation, considerations of therapeutic engagement, and integration with advanced neuroimaging techniques. These efforts will contribute to the development of evidence-based practices, improve treatment outcomes, and further establish neurofeedback as a valuable intervention in the field of PTSD.
10. Conclusions
The findings of this review support the effectiveness of NFB as an intervention for reducing chronic PTSD symptoms, as well as associated anxiety and depression in adult patients. Mechanistic evidence suggests that NFB leads to therapeutic changes in brain functioning. Further well-designed research with larger sample sizes, diverse populations, consistent treatment protocols, and long-term follow-up assessments is crucial to strengthen the evidence base and confirm the clinical benefits of NFB for PTSD treatment.
Acknowledgements
We thank the NSW Service for the Treatment and Rehabilitation of Torture and Trauma Survivors for ongoing support with our research study.
Funding Statement
This work was not supported by any specific funding.
Open Scholarship



This article has earned the Center for Open Science badges for Open Data, Open Materials and Preregistered. The data and materials are openly accessible at https://osf.io/c72b6/, https://osf.io/c72b6/ and https://osf.io/c72b6/registrations.
Disclosure statement
Prof. Harris has recently received financial support from the Australian Research Council, Balnaves Foundation, the National Health and Medical Research Council, Alto Neuroscience, Janssen Australia, Medical Research Futures Fund, Lundbeck Australia, Seqirus, and Takeda Pharmaceuticals USA. He is also the chair of One Door Mental Health. Mirjana Askovic currently holds the positions of Neurofeedback Program Coordinator and Director of the Australian Neurofeedback Institute at STARTTS. The other co-authors do not have any conflicts of interest to declare.
Data availability statement
The data supporting the results and analyses presented in this paper can be found on: 10.6084/m9.figshare.22110620.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Askovic, M., Watters, A. J., Coello, M., Aroche, J., Harris, A. W. F., & Kropotov, J. (2020). Evaluation of neurofeedback for posttraumatic stress disorder related to refugee experiences using self-report and cognitive ERP measures. Clinical EEG and Neuroscience, 51(2), 79–86. 10.1177/1550059419849170 [DOI] [PubMed] [Google Scholar]
- Bell, A. N., Moss, D., & Kallmeyer, R. J. (2019). Healing the neurophysiological roots of trauma: A controlled study examining LORETA Z-score neurofeedback and HRV biofeedback for chronic PTSD. NeuroRegulations, 6(2), 54–70. 10.15540/nr.6.2.54 [DOI] [Google Scholar]
- Bradley, R., Greene, J., Russ, E., Dutra, L., & Westen, D. (2005). A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry, 162(2), 214–227. 10.1176/appi.ajp.162.2.214 [DOI] [PubMed] [Google Scholar]
- Breukelaar, I. A., Bryant, R. A., & Korgaonkar, M. S. (2021). The functional connectome in posttraumatic stress disorder. Neurobiology of Stress, 14, 100321. 10.1016/j.ynstr.2021.100321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnstein, A. (1986). Treatment noncompliance in patients with posttraumatic stress disorder. Psychosomatics, 27, 37–40. 10.1016/S0033-3182(86)72741-2 [DOI] [PubMed] [Google Scholar]
- Clancy, K., Ding, M., Bernat, E., Schmidt, N. B., & Li, W. (2017). Restless ‘rest’: Intrinsic sensory hyperactivity and disinhibition in posttraumatic stress disorder. Brain: A Journal of Neurology, 140(7), 2041–2050. 10.1093/brain/awx116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clancy, K. J., Andrzejewski, J. A., Simon, J., Ding, M., Schmidt, N. B., & Li, W. (2020). Posttraumatic stress disorder is associated with α dysrhythmia across the visual cortex and the default mode network. eNeuro, 7(4), ENEURO.0053-20.2020. 10.1523/ENEURO.0053-20.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo, M. A., Ramautar, J. R., Wei, Y., Gomez-Herrero, G., Stoffers, D., Wassing, R., Benjamins, J. S., Tagliazucchi, E., van der Werf, Y. D., Cajochen, C., & Van Someren, E. J. (2016). Wake high-density electroencephalographic spatiospectral signatures of insomnia. Sleep, 39(5), 1015–1027. 10.5665/sleep.5744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa, D. M., Zanatta, G., Ziegelmann, F. B., Soares Barros, P. K., & Mello, A. J., & F, C . (2020). Pharmacological treatments for adults with post-traumatic stress disorder: A network meta-analysis of comparative efficacy and acceptability. Journal of Psychiatric Research, 130, 412–420. 10.1016/j.jpsychires.2020.07.046 [DOI] [PubMed] [Google Scholar]
- Coventry, P. A., Meader, N., Melton, H., Temple, M., Dale, H., Wright, K., Cloitre, M., Karatzias, T., Bisson, J., Roberts, N. P., Brown, J. V. E., Barbui, C., Churchill, R., Lovell, K., McMillan, D., & Gilbody, S. (2020). Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: Systematic review and component network meta-analysis. PLoS Medicine, 17(8), e1003262. 10.1371/journal.pmed.1003262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels, J. K., McFarlane, A. C., Bluhm, R. L., Moores, K. A., Clark, C. R., Shaw, M. E., Williamson, P. C., Densmore, M., & Lanius, R. A. (2010). Switching between executive and default mode networks in posttraumatic stress disorder: Alterations in functional connectivity. Journal of Psychiatry and Neuroscience, 35(4), 258–266. 10.1503/jpn.090175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, J. P., Prindle, J., Saba, S., Lee, D. S., Leightley, D., Tran, D. D., Sedano, A., Fitzke, R., Castro, C. A., & Pedersen, E. R. (2023). Childhood adversity, combat experiences, and military sexual trauma: A test and extension of the stress sensitization hypothesis. Psychological Medicine, 1–9. Advance online publication. 10.1017/S0033291722000733 [DOI] [PubMed] [Google Scholar]
- Deiber, M. P., Ammann, C., Hasler, R., Colin, J., Perroud, N., & Ros, T. (2021). Electrophysiological correlates of improved executive function following EEG neurofeedback in adult attention deficit hyperactivity disorder. Clinical Neurophysiology, 132(8), 1937–1946. 10.1016/j.clinph.2021.05.017 [DOI] [PubMed] [Google Scholar]
- du Bois, N., Bigirimana, A. D., Korik, A., Kéthina, L. G., Rutembesa, E., Mutabaruka, J., Mutesa, L., Prasad, G., Jansen, S., & Coyle, D. H. (2021). Neurofeedback with low-cost, wearable electroencephalography (EEG) reduces symptoms in chronic posttraumatic stress disorder. Journal of Affective Disorders, 295, 1319–1334. 10.1016/j.jad.2021.08.071 [DOI] [PubMed] [Google Scholar]
- Enriquez-Geppert, S., Huster, R. J., & Herrmann, C. S. (2017). EEG-Neurofeedback as a tool to modulate cognition and behavior: A review tutorial. Frontiers in Human Neuroscience, 11, 51. 10.3389/fnhum.2017.00051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gapen, M., van der Kolk, B. A., Hamlin, E., Hirshberg, L., Suvak, M., & Spinazzola, J. (2016). A pilot study of neurofeedback for chronic PTSD. Applied Psychophysiology and Biofeedback, 41(3), 251–261. 10.1007/s10484-015-9326-5 [DOI] [PubMed] [Google Scholar]
- Halvorsen, JØ. (2016). Defining clinically significant change. British Journal of Psychiatry, 209(1), 85. 10.1192/bjp.209.1.85 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., Savović, J., Page, M. J., Elbers, R. G., & Sterne, J. A. C. (2022). Chapter 8: Assessing risk of bias in a randomized trial. In Higgins J. P. T., Thomas J., Chandler J., Cumpston M., Li T., Page M. J., & Welch V. A. (Eds.), Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane. Available from www.training.cochrane.org/handbook. [Google Scholar]
- Hong, J., & Park, J. H. (2022). Efficacy of neuro-feedback training for PTSD symptoms: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 19(20), 13096. 10.3390/ijerph192013096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, M. X., Yurgil, K. A., Robb, A., Angeles, A., Diwakar, M., Risbrough, V. B., Nichols, S. L., McLay, R., Theilmann, R. J., Song, T., Huang, C. W., Lee, R. R., & Baker, D. G. (2014). Voxel-wise resting-state MEG source magnitude imaging study reveals neurocircuitry abnormality in active-duty service members and veterans with PTSD. NeuroImage: Clinical, 5, 408–419. 10.1016/j.nicl.2014.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaycox, L. H. F., & Foa, E. B. (1996). Obstacles in implementing exposure therapy for PTSD: Case discussions and practical solutions. Clinical Psychology & Psychotherapy, 3(3), 176–184. [DOI] [Google Scholar]
- Jellestad, L., Vital, N. A., Malamud, J., Taeymans, J., & Mueller-Pfeiffer, C. (2021). Functional impairment in posttraumatic stress disorder: A systematic review and meta-analysis. Journal of Psychiatric Research, 136, 14–22. 10.1016/j.jpsychires.2021.01.039 [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., Hyland, P., Maercker, A., Ben-Ezra, M., Coventry, P., & Mason-Roberts, S. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. Epub 2019/03/13. 10.1017/S0033291719000436 [DOI] [PubMed] [Google Scholar]
- Kay, D. B., & Buysse, D. J. (2017). Hyperarousal and beyond: New insights to the pathophysiology of insomnia disorder through functional neuroimaging studies. Brain Sciences, 7(3), 23. 10.3390/brainsci7030023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelson, C. Y. (2013). The impact of EEG biofeedback on veterans’ symptoms of posttraumatic stress disorder (PTSD) (Order No. 3606174). Available from ProQuest One Academic. (1492137060). http://ezproxy.library.usyd.edu.au/login?url=https://www.proquest.com/dissertations-theses/impact-eeg-biofeedback-on-veterans-symptoms/docview/1492137060/se-2
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., Degenhardt, L., de Girolamo, G., Dinolova, R. V., Ferry, F., Florescu, S., Gureje, O., Haro, J. M., Huang, Y., Karam, E. G., Kawakami, N., Lee, S., Lepine, J. P., Levinson, D., … Koenen, K. C. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk, H. W. (Ed.). (2020). Restoring the Brain: Neurofeedback as an Integrative Approach to Health (2nd ed.). Routledge. [Google Scholar]
- Kluetsch, R. C., Ros, T., Théberge, J., Frewen, P. A., Calhoun, V. D., Schmahl, C., Jetly, R., & Lanius, R. A. (2014). Plastic modulation of PTSD resting-state networks and subjective wellbeing by EEG neurofeedback. Acta Psychiatrica Scandinavica, 130(2), 123–136. 10.1111/acps.12229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenen, K. C., Ratanatharathorn, A., Ng, L., McLaughlin, K. A., Bromet, E. J., Stein, D. J., Karam, E. G., Meron Ruscio, A., Benjet, C., Scott, K., Atwoli, L., Petukhova, M., Lim, C. C. W., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Bunting, B., Ciutan, M., de Girolamo, G., … Kessler, R. C. (2017). Posttraumatic stress disorder in the world mental health surveys. Psychological Medicine, 47(13), 2260–2274. 10.1017/S0033291717000708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius, R. A., Frewen, P. A., Tursich, M., Jetly, R., & McKinnon, M. C. (2015). Restoring large-scale brain networks in PTSD and related disorders: A proposal for neuroscientifically-informed treatment interventions. European Journal of Psychotraumatology, 6(1), 27313. 10.3402/ejpt.v6.27313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leem, J., Cheong, M. J., Lee, H., Cho, E., Lee, S. Y., Kim, G. W., & Kang, H. W. (2021). Effectiveness, cost-utility, and safety of neurofeedback self-regulating training in patients with posttraumatic stress disorder: A randomized controlled trial. Healthcare (Basel, Switzerland), 9(10), 1351. 10.3390/healthcare9101351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, C., Roberts, N. P., Andrew, M., Starling, E., & Bisson, J. I. (2020). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1729633. 10.1080/20008198.2020.1729633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddell, B. J., Nickerson, A., Felmingham, K. L., Malhi, G. S., Cheung, J., Den, M., Askovic, M., Coello, M., Aroche, J., & Bryant, R. A. (2019). Complex posttraumatic stress disorder symptom profiles in traumatized refugees. Journal of Traumatic Stress, 32(6), 822–832. 10.1002/jts.22453 [DOI] [PubMed] [Google Scholar]
- Marzbani, H., Marateb, H. R., & Mansourian, M. (2016). Methodological note: Neurofeedback: A comprehensive review on system design, methodology and clinical applications. Basic and Clinical Neuroscience Journal, 7(2), 143–158. 10.15412/J.BCN.03070208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane, A. C. (2010). The long-term costs of traumatic stress: Intertwined physical and psychological consequences. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 9(1), 3–10. 10.1002/j.2051-5545.2010.tb00254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62(10), 1006–1012. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Nicholson, A. A., Densmore, M., Frewen, P. A., Neufeld, R. W. J., Théberge, J., Jetly, R., Lanius, R. A., & Ros, T. (2023). Homeostatic normalization of alpha brain rhythms within the default-mode network and reduced symptoms in post-traumatic stress disorder following a randomized controlled trial of electroencephalogram neurofeedback. Brain Communications, 5(2), fcad068. 10.1093/braincomms/fcad068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson, A. A., Ros, T., Densmore, M., Frewen, P. A., Neufeld, R. W. J., Théberge, J., Jetly, R., & Lanius, R. A. (2020). A randomized, controlled trial of alpha-rhythm EEG neurofeedback in posttraumatic stress disorder: A preliminary investigation showing evidence of decreased PTSD symptoms and restored default mode and salience network connectivity using fMRI. NeuroImage: Clinical, 28, 102490. 10.1016/j.nicl.2020.102490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson, A. A., Ros, T., Frewen, P. A., Densmore, M., Théberge, J., Kluetsch, R. C., Jetly, R., & Lanius, R. A. (2016). Alpha oscillation neurofeedback modulates amygdala complex connectivity and arousal in posttraumatic stress disorder. NeuroImage: Clinical, 12, 506–516. 10.1016/j.nicl.2016.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson, A. A., Ros, T., Jetly, R., & Lanius, R. A. (2020). Regulating posttraumatic stress disorder symptoms with neurofeedback: Regaining control of the mind. Journal of Military, Veteran and Family Health, 6(Suppl 1), 3–15. 10.3138/jmvfh.2019-0032 [DOI] [Google Scholar]
- Noohi, S., Miraghaie, A. M., & Arabi, A. (2017). Effectiveness of neuro-feedback treatment with alpha/theta method on PTSD symptoms and their executing function. Biomedical Research, 28, 2019–2027. [Google Scholar]
- Pacella, M. L., Hruska, B., & Delahanty, D. L. (2013). The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders, 27(1), 33–46. 10.1016/j.janxdis.2012.08.004 [DOI] [PubMed] [Google Scholar]
- Panisch, L. S., & Hai, A. H. (2020). The effectiveness of using neurofeedback in the treatment of post-traumatic stress disorder: A systematic review. Trauma, Violence, & Abuse, 21(3), 541–550. doi:. 10.1177/1524838018781103. Epub 2018 Jun 11. PMID: 29890906. [DOI] [PubMed] [Google Scholar]
- Peniston, E. G., & Kulkosky, P. J. (1989). Alpha-theta brainwave training and beta-endorphin levels in alcoholics. Alcoholism: Clinical and Experimental Research, 13(2), 271–279. 10.1111/j.1530-0277.1989.tb00325.x [DOI] [PubMed] [Google Scholar]
- Peniston, E. G., & Kulkosky, P. J. (1990). Alcoholic personality and alpha-theta brainwave training. Medical Psychotherapy: An International Journal, 3, 37–55. [Google Scholar]
- Peniston, E. G., & Kulkosky, P. J. (1991). Alpha-theta brainwave neuro-feedback therapy for Vietnam veterans with combat-related posttraumatic stress disorder. Medical Psychotherapy: An International Journal, 4, 47–60. [Google Scholar]
- Perl, M., & Perl, D. (2019). EEG amplitude neurofeedback: A review of the research. Asia Pacific Journal of Neurotherapy, 1(1), 44–55. [Google Scholar]
- Popescu, M., Popescu, E. A., DeGraba, T. J., & Hughes, J. D. (2023). Cognitive flexibility in posttraumatic stress disorder: Sustained interference associated with altered modulation of cortical oscillatory activity during task-switching. NeuroImage: Clinical, 37, 103297. Advance online publication. 10.1016/j.nicl.2022.103297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter, K., Andersen, S. B., & Carlsson, J. (2016). Neurofeedback treatment and posttraumatic stress disorder. Journal of Nervous & Mental Disease, 204(2), 69–77. 10.1097/NMD.0000000000000418 [DOI] [PubMed] [Google Scholar]
- Review Manager Web (RevMan Web) . (2020). Version 5. The Cochrane Collaboration, 2020. revman.cochrane.org.
- Ros, T., Baars, J., Lanius, B., & & Vuilleumier, R. A. (2014). Tuning pathological brain oscillations with neurofeedback: A systems neuroscience framework. Frontiers in Human Neuroscience, 8, 1008. 10.3389/fnhum.2014.01008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ros, T., Frewen, P., Théberge, J., Michela, A., Kluetsch, R., Mueller, A., Candrian, G., Jetly, R., Vuilleumier, P., & Lanius, R. A. (2017). Neurofeedback tunes scale-free dynamics in spontaneous brain activity. Cerebral Cortex, 27(10), 4911–4922. 10.1093/cercor/bhw285 [DOI] [PubMed] [Google Scholar]
- Ros, T., Théberge, J., Frewen, P. A., Kluetsch, R., Densmore, M., Calhoun, V. D., & Lanius, R. A. (2013). Mind over chatter: Plastic up-regulation of the fMRI salience network directly after EEG neurofeedback. NeuroImage, 65, 324–335. 10.1016/j.neuroimage.2012.09.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan, R. (June 2013). Cochrane consumers and communication review group. Cochrane consumers and communication review group: data synthesis and analysis. http://cccrg.cochrane.org. (accessed on 16th May 2023).
- Saxby, E., & Peniston, E. G. (1995). Alpha-theta brainwave neurofeedback training: An effective treatment for male and female alcoholics with depressive symptoms. Journal of Clinical Psychology, 51(5), 685–693. [DOI] [PubMed] [Google Scholar]
- Schünemann, H., Brożek, J., Guyatt, G., & Oxman, A. (Eds.). 2013. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. guidelinedevelopment.org/handbook.
- Shaw, S. B., Nicholson, A. A., Ros, T., Harricharan, S., Terpou, B., Densmore, M., Theberge, J., Frewen, P., & Lanius, R. A. (2023). Increased top-down control of emotions during symptom provocation working memory tasks following a rct of alpha-down neurofeedback in ptsd. NeuroImage: Clinical, 37, 103313. 10.1016/j.nicl.2023.103313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steingrimsson, S., Bilonic, G., Ekelund, A. C., Larson, T., Stadig, I., Svensson, M., Vukovic, I. S., Wartenberg, C., Wrede, O., & Bernhardsson, S. (2020). Electroencephalography-based neurofeedback as treatment for posttraumatic stress disorder: A systematic review and meta-analysis. European Psychiatry, 63(1), e7. 10.1192/j.eurpsy.2019.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne, J. A. C., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., Boutron, I., Carpenter, J. R., Chan, A. W., Churchill, R., Deeks, J. J., Hróbjartsson, A., Kirkham, J., Jüni, P., Loke, Y. K., Pigott, T. D., … Higgins, J. P. T. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355, i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terpou, B. A., Densmore, M., Théberge, J., Frewen, P., McKinnon, M. C., Nicholson, A. A., & Lanius, R. A. (2020). The hijacked self: Disrupted functional connectivity between the periaqueductal gray and the default mode network in posttraumatic stress disorder using dynamic causal modeling. NeuroImage: Clinical, 27, 102345. 10.1016/j.nicl.2020.102345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Kolk, B. A., Hodgdon, H., Gapen, M., Musicaro, R., Suvak, M. K., Hamlin, E., & Spinazzola, J. (2016). A randomized controlled study of neurofeedback for chronic PTSD. PloS one, 11(12), e0166752. 10.1371/journal.pone.0166752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varker, T., Jones, K., Arjmand, H.-A., Hinton, M., Hiles, S., Freijah, I., Forbes, D., Kartal, D., Phelps, A., Bryant, R., Mcfarlane, A., Hopwood, M., & O’Donnell, M. (2021). Dropout from guideline-recommended psychological treatments for posttraumatic stress disorder: A systematic review and meta-analysis. Journal of Affective Disorders Reports, 4), 10.1016/j.jadr.2021.100093 [DOI] [Google Scholar]
- von Hippel, P. T. (2015). The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Medical Research Methodology, 15(1), 35. 10.1186/s12874-015-0024-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter, K. H., Levine, J. A., Highfill-McRoy, R. M., Navarro, M., & Thomsen, C. J. (2018). Prevalence of posttraumatic stress disorder and psychological comorbidities among U.S. active duty service members, 2006–2013. Journal of Traumatic Stress, 31(6), 837–844. 10.1002/jts.22337 [DOI] [PubMed] [Google Scholar]
- Watts, B. V., Schnurr, P. P., Mayo, L., Young-Xu, Y., Weeks, W. B., & Friedman, M. J. (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry, 74(6), e541–e550. 10.4088/JCP.12r08225 [DOI] [PubMed] [Google Scholar]
- White, S. F., Costanzo, M. E., Thornton, L. C., Mobley, A. M., Blair, J. R., & Roy, M. J. (2018). Increased cognitive control and reduced emotional interference is associated with reduced PTSD symptom severity in a trauma-exposed sample: A preliminary longitudinal study. Psychiatry Research: Neuroimaging, 278, 7–12. 10.1016/j.pscychresns.2018.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkeler, A., Winkeler, M., & Imgart, H. (2022). Infra-Low frequency neurofeedback in the treatment of patients with chronic eating disorder and comorbid post-traumatic stress disorder. Frontiers in Human Neuroscience, 16, 890682. 10.3389/fnhum.2022.890682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2019). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/
- Zeynali, M., & Seyedarabi, H. (2019). EEG-based single-channel authentication systems with optimum electrode placement for different mental activities. Biomedical Journal, 42(4), 261–267. 10.1016/j.bj.2019.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the results and analyses presented in this paper can be found on: 10.6084/m9.figshare.22110620.