Abstract
Youth e-cigarette use has rapidly increased in the last few years. Susceptibility is a validated measure associated with future tobacco use. We examined trends in e-cigarette susceptibility across five years (2014–2018) of the National Youth Tobacco Survey among youth e-cigarette never users. We observed increases in overall e-cigarette susceptibility from 2014 to 2016 and decreases from 2016 to 2018. Generally, sociodemographic variables were not associated with trend effects; however, there was an interaction between linear trends with both race/ethnicity and other tobacco product (OTP) use. The percentage of youth who were susceptible to using e-cigarettes ranged from 32.9% in 2014 to 33.2% in 2018 with a high of 36.7% in 2016. We also examined the prevalence of e-cigarette susceptibility by race/ethnicity, sex, school level, OTP use, and e-cigarette harm perception. E-cigarette susceptibility was associated with race, school level, OTP ever use, and e-cigarette harm perceptions. Hispanic youth, those in high school, and OTP ever users were more likely to be susceptible to e-cigarette use compared to their counterparts across all years. E-cigarette susceptibility was most prevalent among those who perceived e-cigarettes to pose “no harm” in 2014 and “little harm” in 2018 when compared to other item response options in 2014 and 2018, respectively. This study is the first to document trends in e-cigarette susceptibility among youth. Understanding antecedents of e-cigarette use and identifying youth subgroups vulnerable to e-cigarette use is valuable to developing effective prevention efforts.
Disclaimer: The findings and conclusions in this publication are those of the authors and do not necessarily represent the official position of the Food and Drug Administration or the Centers for Disease Control and Prevention.
1. Introduction
Youth e-cigarette use rapidly increased over the last few years. National Youth Tobacco Survey (NYTS) data show that current e-cigarette use (defined as use on one or more days in the past 30 days) increased from 2016 to 2019 among middle school (4.33% to 10.5%) and high school (11.3% to 27.55%) students; e-cigarettes are now the most commonly used tobacco product among youth (Gentzke et al., 2019; Jamal et al., 2017).
Nicotine use during adolescence can cause addiction, prime the brain for addiction to other substances, and harm the developing brain (U.S. Surgeon General 2016; Yuan et al. 2015). Additionally, longitudinal studies have found that adolescent e-cigarette use is associated with future cigarette smoking (Chaffee et al. 2018; Miech et al. 2017; Wills et al. 2017).
With most tobacco use beginning during adolescence and young adulthood, understanding the antecedents to initiation is valuable for prevention (U. S. Surgeon General 2016). Susceptibility is a validated measure among non-users (Pierce et al. 1996) that indicates lack of a firm commitment not to use tobacco products and has been associated with other tobacco use risk factors (Sawdey et al. 2019) and future tobacco use (Pierce et al. 1996; Strong et al. 2015). Pierce found that among youth 12 to 17 years of age, susceptibility to use e-cigarettes was associated with current e-cigarette use approximately one year later (National Institutes of Health, 2018; Pierce et al. 2018). A longitudinal study among Connecticut middle and high school students also showed that e-cigarette susceptibility predicted subsequent e-cigarette initiation and past 30-day e-cigarette use six months later (Bold et al. 2017). Similar results were found among middle and high school students in Texas; those susceptible to e-cigarette use at baseline were more likely to report e-cigarette ever use at six-, 12-, and 18-month follow-up versus those who were not susceptible (Carey et al. 2018). These findings, coupled with the recent increases in youth e-cigarette use, imply increasing trends in youth e-cigarette susceptibility in prior years; however, to our knowledge, no studies have examined that claim.
National surveillance data show that prevalence of youth e-cigarette use varies by school level as a proxy for age, race/ethnicity and sex (Jamal et al., 2017; Odani et al., 2018; Perikleous et al. 2018). In 2020, 19.6% of high school and 4.7% of middle school students currently used e-cigarettes. In 2019, 23.1% of White, non-Hispanic, 18.7% of Hispanic, 13.6% of Black, non-Hispanic, and 13.6% of other, non-Hispanic middle and high school students currently used e-cigarettes (Wang et al. 2019). Although there are documented trends of racial and ethnic differences in cigarette smoking susceptibility (Carey et al. 2018; Choi and Forster 2014; El-Toukhy et al. 2016), studies have not examined trends by demographic groups to assess differences in susceptibility to e-cigarette use with a national sample.
Prior studies have shown that youth perceive e-cigarettes to be less harmful than cigarettes (Ambrose et al. 2014; Pokhrel et al. 2015) and that lower harm perceptions are associated with increased e-cigarette use (Choi and Forster 2014). Research has also documented that susceptibility varies by harm perceptions: among 18 to 23-year-old never e-cigarette users in New York, individuals with lower harm perceptions were more susceptible to future e-cigarette use (Saddleson et al. 2015). While these findings suggest an association between e-cigarette harm perceptions and e-cigarette use among young adults, less is known among youth and whether these associations have changed over time due to the increased popularity of e-cigarettes.
This paper examines trends in e-cigarette use susceptibility among youth never users of e-cigarettes across five years (2014–2018) (Centers for Disease Control and Prevention 2018). We examined prevalence of e-cigarette use susceptibility by race/ethnicity, sex, school level, other tobacco product (OTP) use, and levels of perceived harm of intermittent e-cigarette use by survey year. We also tested for trends in e-cigarette use susceptibility across the survey years. Last, we examined whether e-cigarette use susceptibility trends varied by race/ethnicity, sex, school level, OTP use, and perceived e-cigarette harm.
2. Methods
2.1. Sample
Data came from five years (2014–2018)1 of NYTS, a cross-sectional, school-based, pencil-and-paper questionnaire self-administered to U.S. middle and high school students. A three-stage cluster sampling procedure was used to generate a nationally representative sample of U.S. students in grades 6–12 who attend public and private schools. The overall response rates ranged from 63.4% (2015) to 73.3% (2014). A description of NYTS sampling procedures is available online (Centers for Disease Control and Prevention 2018). The Centers for Disease Control and Prevention (CDC) Human Research Protection Office and the Office of Management and Budget approved the NYTS protocol and data collection.
All analyses were restricted to never e-cigarette users, resulting in the following analytic sample sizes for each year: 2014 (n = 17,286), 2015 (n = 12,727), 2016 (n = 15,801), 2017 (n = 13,754), and 2018 (n = 14,572) and an overall sample of 74,140.
Measures.
Respondents indicating they had never tried an e-cigarette were classified as never users. Respondents who were never e-cigarette users and answered “Yes” to ever trying or using OTPs (cigarettes; little cigars, cigars or cigarillos; tobacco from a hookah or waterpipe; pipe filled with tobacco; chewing tobacco, snuff, or dip; and bidis) were classified as OTP ever users.
Susceptibility was assessed using Pierce’s validated measure (Pierce et al. 1996; Strong et al. 2015) and standardized Cronbach’s alpha coefficients calculated using unweighted data ranged from 0.90–0.93 across the years. Respondents were classified as either susceptible or not susceptible based on responses to three questions: (1)“Have you ever been curious about using an e-cigarette?,” (2) “Do you think that you will try an e-cigarette soon?,” and (3) “If one of your best friends were to offer you an e-cigarette, would you use it?” Response options for all three questions included “Definitely yes,” “Probably yes,” “Probably not,” and “Definitely not.” Consistent with previous research, respondents who answered anything other than “Definitely not” to any of the three questions were classified as susceptible to e-cigarette use (Pierce et al. 1996; Strong et al. 2015); also consistent with previous research (Sawdey et al. 2019), respondents who had a combination of missing information and responses other than the strongest rejection (answering “definitely not”) on the three susceptibility measures were classified as susceptible. To prevent misclassification, respondents with a combination of “definitely not” and missing information were classified as missing.
Harm perceptions of intermittent e-cigarette use were measured with the question “How much do you think people harm themselves when they use e-cigarettes some days but not every day?” Response options included: “No harm,” “Little harm,” “Some harm,” and “A lot of harm.”
Assessed demographic characteristics included: sex (female or male), school level (middle school or high school) and race/ethnicity (Non-Hispanic White [NH-White], Non-Hispanic Black [NH-Black], Hispanic, or Non-Hispanic Other [NH-Other]). NH-Other included participants who identified as Non-Hispanic Asian, Non-Hispanic American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander. Survey year denotes what year respondents completed the survey (2014, 2015, 2016, 2017, or 2018).
2.2. Data analysis
Weighted proportions and corresponding confidence intervals (CIs) of demographic characteristics and prevalence of e-cigarette susceptibility were obtained for all survey years using survey procedures in SAS 9.4 software (SAS Institute Inc, 2013). The procedures used Taylor series linearization method to estimate the variance of the estimators. Under this method, a linear approximation to the estimator of interest is obtained by Taylor series approximation and then the variance estimate for this approximation is used to estimate the variance of the estimator (Verma and Betti 2011; Woodruff 1971). In the case of a stratified design, the procedure pools stratum variance to compute the overall variance estimate. The stratum variance is estimated from the variation among primary sampling units. Given the evidence that demographic factors (sex, school level, race/ethnicity) relate to youth e-cigarette use and susceptibility (Bold et al. 2017; Dai and Hao 2017; McMillen et al. 2014; Saddleson et al. 2015; U.S. Surgeon General 2016), the models controlled for these covariates. We also controlled for OTP ever use and e-cigarette harm perceptions, given that these variables may influence e-cigarette use (Choi and Forster 2014; Saddleson et al. 2015). E-cigarette susceptibility prevalence estimates were adjusted for covariates and determined using predicted marginal probabilities from logistic regression models. Chi-square analyses tested bivariate associations between e-cigarette susceptibility and the covariates for each survey year. We conducted logistic regression modeling for our multivariable models and obtained odds ratios of e-cigarette susceptibility with corresponding 95% CIs. The adjusted prevalence by survey year was obtained using survey logistic procedures in R 3.5 (R Core Team 2018) which allowed us to conduct trend analyses. Susceptibility prevalence estimates for each level of a covariate were adjusted for the other covariates.
To assess the linear and quadratic trends in e-cigarette susceptibility over the five survey years, orthogonal polynomial coefficients were included in the logistic regression models. A joinpoint regression analysis was conducted to identify the change points in the overall susceptibility prevalence trend. Joinpoint regression analysis assumes that data can be divided into subsets with their own distinctive linear trend (Gillis and Edwards 2019). By fitting the simplest joinpoint model that the data allow, we can identify the time point(s) at which the trend changes (i.e., joinpoints) and the line segments joined at these junctures (National Cancer Institute 2019). We examined the slopes and direction of linear trends in susceptibility before and after the change points. To further understand trends in susceptibility by subgroup (i.e., sex, race/ethnicity, and school level), we tested for interaction effects. Therefore, we included the covariates by orthogonal polynomial coefficient interactions in the logistic model. These analyses were performed in R 3.5. Missing data were assumed to be missing at random and deleted listwise.
3. Results
Table 1 shows the demographic characteristics, OTP ever use status, and e-cigarette harm perceptions of youth never e-cigarette users by survey year. Distributions in sex, race/ethnicity, and school level are similar across survey years.
Table 1.
Weighted sample characteristics, youth never e-cigarette users, National Youth Tobacco Survey, United States, 2014–2018 (n = 74,140).
| Year | 2014 (n = 17,286) % (95% CI) | 2015 (n = 12,727; % (95% CI) | 2016 (n = 15,801; % (95% CI) | 2017 (n = 13,754; % (95% CI) | 2018 (n = 14,572; % (95%CI) |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 49.0 (47.1, 50.9) | 49.3 (47.6, 51.1) | 49.1 (48.0, 50.3) | 50.2 (48.8, 51.5) | 49.4 (48.0,50.8) |
| Female | 51.0 (49.1, 52.9) | 50.7 (48.9, 52.4) | 50.9 (49.7, 52.0) | 49.8 (48.5, 51.2) | 50.6 (49.2, 52.0) |
| Race/ethnicity | |||||
| NH-White | 58.0 (52.1, 64.0) | 57.6 (51.6, 63.6) | 55.6 (49.8, 61.4) | 55.5 (48.2, 62.9) | 53.5 (48.4, 58.7) |
| NH-black | 16.2 (12.3, 20.2) | 15.2 (10.8, 19.6) | 14.1 (10.4, 17.9) | 14.4 (11.0, 17.8) | 14.6 (11.3, 17.9) |
| Hispanic | 20.9 (17.2, 24.5) | 22.0 (17.5, 26.5) | 24.3 (19.8, 28.8) | 23.7 (17.9, 29.6) | 25.2 (20.7, 29.7) |
| NH-other | 4.9 (3.5, 6.2) | 5.2 (4.1, 6.4) | 5.6 (4.7, 7.3) | 6.4 (4.7, 8.1) | 6.7 (5.0, 8.4) |
| School | |||||
| Middle | 49.1 (42.9, 55.4) | 52.3 (45.3, 59.3) | 50.3 (44.6, 55.9) | 50.6 (44.7, 56.5) | 52.4 (47.3, 57.5) |
| High | 50.9 (44.6, 57.1) | 47.7 (40.7, 54.7) | 49.7 (44.1, 55.4) | 49.4 (43.5, 55.3) | 47.6 (42.5, 52.7) |
| OTP ever use | |||||
| Yes | 19.2 (17.4, 21.0) | 13.8 (11.7, 15.9) | 13.9 (12.5, 15.4) | 11.6 (10.3, 12.9) | 11.2 (9.9, 12.5) |
| No | 80.8 (79.0, 82.6) | 86.2 (84.1, 88.3) | 86.1 (84.6, 87.5) | 88.4 (87.1, 89.7) | 88.8 (87.5, 90.2) |
| E-cigarette harm perception | |||||
| No harm | 12.2 (11.3, 13.1) | 9.6 (8.3, 10.9) | 6.3 (5.5, 7.1) | 5.4 (4.7, 6.2) | 6.4 (5.7, 7.2) |
| Little harm | 29.5 (28.5, 30.5) | 26.7 (25.2, 28.2) | 22.3 (21.3, 23.3) | 21.2 (20.0, 22.3) | 20.6 (19.6 21.7) |
| Some harm | 34.1 (32.8, 35.4) | 34.3 (32.8, 35.9) | 40.0 (38.8, 41.3) | 39.2 (37.8, 40.5) | 38.6 (37.2, 40.0) |
| A lot of harm | 24.2 (22.8, 25.6) | 29.4 (28.0, 30.9) | 31.4 (30.1, 32.7) | 34.2 (32.7, 35.8) | 34.3 (32.6, 36.0) |
% = percent of youth by demographic categories, 95% CI = 95% confidence interval.
The overall adjusted prevalence of susceptibility to e-cigarettes and adjusted estimates of prevalence by sex, school level, race/ethnicity, OTP ever use, and e-cigarette harm perception are shown in Fig. 1.
Fig. 1.
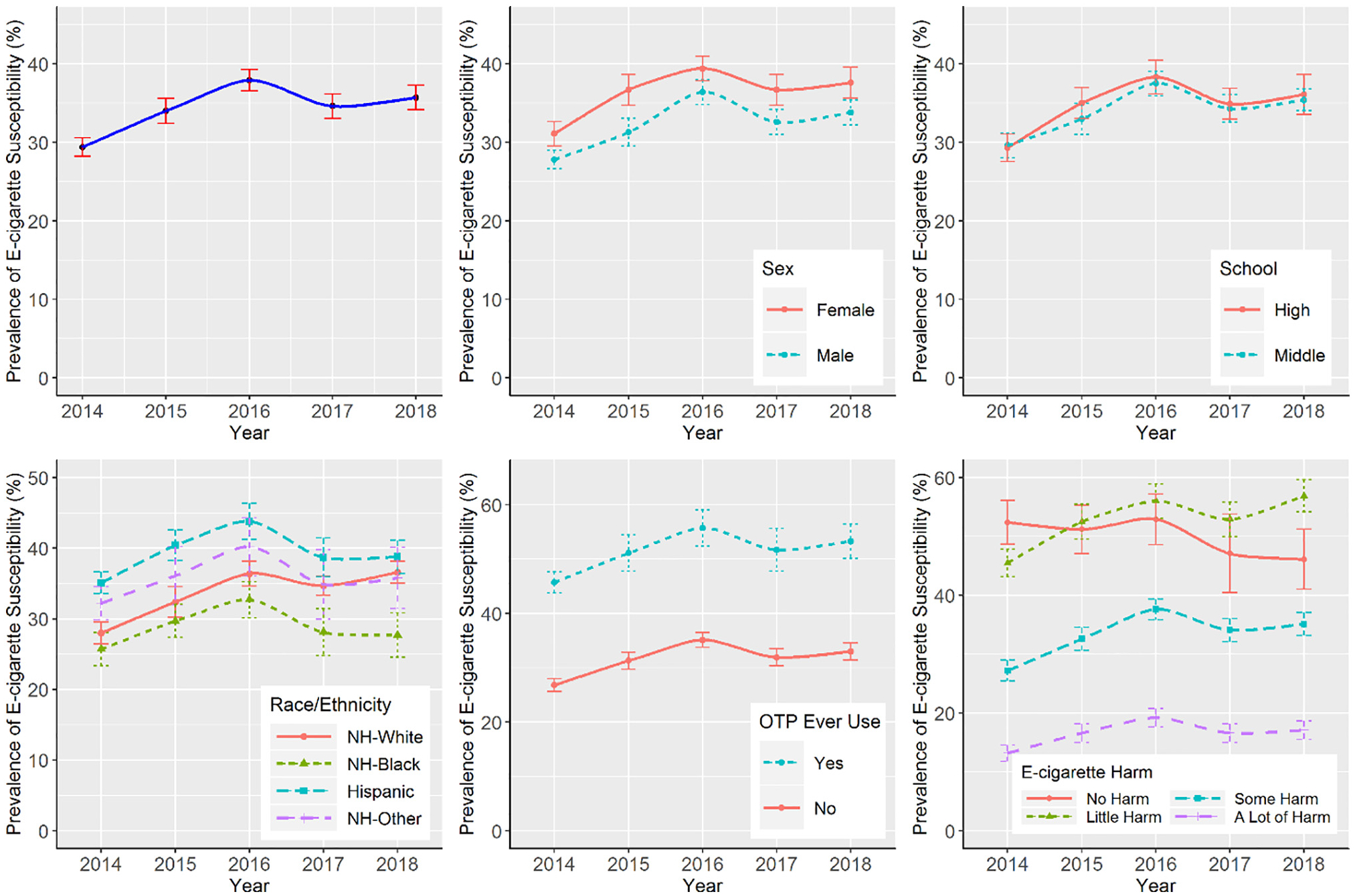
Adjusted e-cigarette susceptibility prevalence from 2014 to 2018 by overall (top left), sex (top middle), school level (top right) race/ethnicity (bottom left), OTP ever use (bottom middle), and e-cigarette harm perceptions (bottom right).
We tested for linear, quadratic and cubic trends in e-cigarette susceptibility prevalence using orthogonal polynomial coefficients. Overall, findings indicated linear and quadratic trends, but no cubic trends in e-cigarette susceptibility over time. The joinpoint analysis identified one joinpoint at year 2016, and the trend analysis of two time segments (before and after 2016) shows that there was a linear increase in prevalence of e-cigarette susceptibility between 2014 and 2016 (β: 0.30, 95% CI: 0.24–0.36) and then a linear decrease between 2016 and 2018 (β: −0.08, 95%CI: −0.14 - −0.01).
Table 2 shows the unadjusted weighted estimates of overall and marginal prevalence of e-cigarette susceptibility by survey year. E-cigarette susceptibility was associated with race, school level, OTP ever use, and e-cigarette harm perceptions across all survey years. The overall percentage of youth who were susceptible to e-cigarettes ranged from a low of 32.0% in 2017 to a high of 36.7% in 2016. Youth susceptibility to e-cigarette use increased from 2014 to 2016 (32.9% to 36.7%) and decreased to 32.0% in 2017. In 2018, susceptibility slightly increased to 33.2%. E-cigarette susceptibility was highest among Hispanic youth, high school youth, and OTP ever users when compared to their counterparts across all survey years. Lastly, the proportion of e-cigarette susceptible youth was highest among those who perceived e-cigarettes to pose “no harm” in 2014 and “little harm” in 2018 when compared to those who selected other response options in 2014 and 2018, respectively.
Table 2.
Unadjusted weighted estimates of prevalence of e-cigarette susceptibility among middle and high school students who are never e-cigarette users, National Youth Tobacco Survey, United States, 2014–2018.
| Unadjusted E-cigarette susceptibility | |||||
|---|---|---|---|---|---|
| Year | 2014% (95%CI) | 2015% (95%CI) | 2016% (95%CI) | 2017% (95%CI) | 2018% (95%CI) |
| Overall | 32.9 (31.5, 34.3) | 34.9 (33.1, 36.8) | 36.7 (35.3, 38.0) | 32.0 (30.5, 33.4) | 33.2 (31.8, 34.7) |
| Sex | |||||
| Male | 33.1 (31.5, 34.7) | 33.7 (31.4, 36.0) | 36.2 (34.8, 37.6) | 31.2 (29.6, 32.8) | 32.3 (30.6, 34.0) |
| Female | 32.7 (31.0, 34.4) | 36.2 (34.0, 38.3) | 37.2 (35.4, 38.9) | 32.8 (30.8, 34.7) | 34.2 (32.2, 36.1) |
| Race/ethnicity | |||||
| NH-White | 31.8 (29.8, 33.8) | 32.8 (30.0, 35.5) | 34.6 (32.7, 36.5) | 32.0 (30.4, 33.5) | 34.2 (32.6, 35.8) |
| NH-black | 31.0 (28.4, 33.6) | 36.0 (32.7, 39.2) | 34.9 (32.0, 37.7) | 27.8 (24.5, 31.1) | 27.4 (24.5, 30.2) |
| Hispanic | 39.1 (37.3, 40.9) | 40.8 (38.8, 42.8) | 43.7 (41.3, 46.1) | 35.6 (33.2, 38.1) | 37.2 (34.7, 39.7) |
| NH-other | 32.3 (28.9, 35.8) | 34.5 (30.2, 38.8) | 37.1 (33.5, 40.8) | 30.1 (25.0, 35.5) | 30.8 (26.4, 35.2) |
| School | |||||
| Middle | 30.5 (28.7, 32.2) | 31.8 (29.4, 34.3) | 34.4 (32.9, 35.9) | 29.5 (27.9, 31.3) | 31.4 (29.8, 33.0) |
| High | 35.2 (33.4, 37.0) | 38.3 (36.3, 40.2) | 38.9 (36.8, 41.0) | 34.5 (32.7, 36.4) | 35.2 (32.7, 37.7) |
| OTP ever use | |||||
| Yes | 53.0 (50.6, 55.4) | 57.7 (54.3, 61.2) | 58.7 (55.4, 62.1) | 53.6 (49.9, 57.2) | 54.9 (51.8, 58.1) |
| No | 28.2 (26.7, 29.6) | 31.1 (29.3, 32.9) | 33.0 (31.7, 34.4) | 29.2 (27.7, 30.7) | 30.4 (28.9, 32.0) |
| E-cigarette harm perception | |||||
| No harm | 55.1 (51.6, 58.7) | 52.5 (48.3, 56.6) | 54.7 (51.0, 58.4) | 46.6 (40.5, 52.8) | 45.7 (41.0, 50.4) |
| Little harm | 46.3 (44.0, 48.6) | 52.7 (50.2, 55.5) | 56.3 (53.7, 58.9) | 52.6 (49.9, 55.2) | 56.1 (53.5, 58.8) |
| Some harm | 27.9 (26.2, 29.6) | 32.3 (30.1, 34.4) | 37.3 (35.5, 39.2) | 33.2 (31.1, 35.4) | 34.3 (32.4, 36.1) |
| A lot of harm | 13.3 (11.9, 14.7) | 15.8 (14.3, 17.4) | 18.7 (17.1, 20.2) | 16.0 (14.2, 17.7) | 16.3 (14.8, 17.8) |
% = percent of youth susceptible to e-cigarettes, 95%CI = 95% confidence interval.
The results of the interaction analyses showed that sex, school level, and OTP ever use did not moderate the trends of e-cigarette susceptibility over time (Fig. 2). However, there were interactions between linear trends and race/ethnicity and e-cigarette harm perceptions, indicating that linear trends in e-cigarette susceptibility differed across various racial/ethnic groups and levels of e-cigarette harm perceptions. Among NH-White (β: 0.37, 95%CI: 0.29–0.46) participants, there was an increasing linear trend, whereas among NH-Black, Hispanic, and NH-Other participants, there was no such trend. The predicted probability of e-cigarette susceptibility for the linear trend among NH-White participants increased from 26.4% in 2014 to 36.5% in 2018. Fig. 2 (top left) shows the predicted linear trend in susceptibility for the race/ethnicity categories. The trend lines for NH-Black, Hispanic, and NH-Other participants are nearly flat, indicating no change in trends among these groups. E-cigarette harm perceptions also moderated the linear trends found in e-cigarette susceptibility. There was an increasing linear trend in the prevalence of e-cigarette susceptibility among youth who perceived e-cigarettes to be a little harmful (β: 0.32, 95%CI: 0.21–0.42), somewhat harmful (β: 0.25, 95%CI: 0.17–0.34), or a lot harmful (β: 0.17, 95%CI: 0.06–0.28) and a decreasing linear trend among those who perceived e-cigarettes to be not harmful (β:−0.17, 95% CI: −0.34–0.01 (Fig. 2, top right).
Fig. 2.
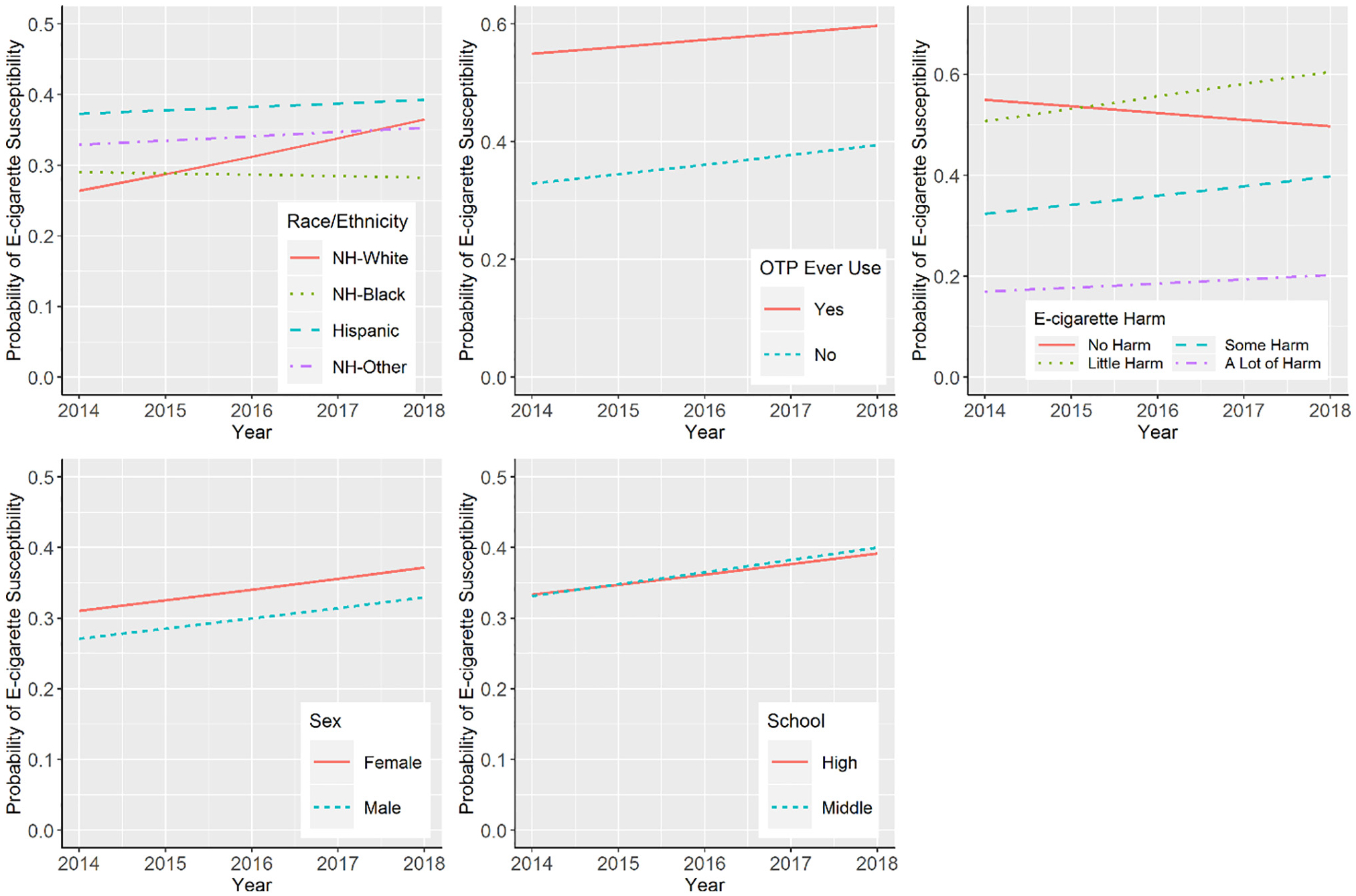
Predicted probabilities of e-cigarette susceptibility for linear trends by categories of race/ethnicity (top left), OTP ever use (top middle), e-cigarette harm perceptions (top right), sex (bottom left), and school level (bottom right) computed at average level of other variables.
The adjusted odds ratios of susceptibility to e-cigarettes obtained from the multivariable logistic model are shown in Table 3. Compared to males, females had higher odds of being susceptible across all survey years, with adjusted odds ratios ranging from a low of 1.14 (95% CI:1.05–1.25) in 2016 to a high of 1.29 (95%CI: 1.17–1.43) in 2015. Compared to all other racial/ethnic groups, Hispanic youth generally had higher odds of being susceptible. Compared to Hispanic youth, NH-Black youth had lower odds of being susceptible across all survey years with adjusted odds ratios ranging from 0.58 (95%CI: 0.48–0.69) in 2018 to 0.63 (95%CI: 0.55–0.73) in 2014; NH-White youth had lower odds of being susceptible than Hispanic youth across survey years (AOR: 0.65–0.80) except for 2018. NH-Other youth had lower odds of susceptibility than Hispanic youth in 2014 (AOR = 0.84, 95% CI: 0.73–0.98) and 2015 (AOR = 0.79, 95%CI: 0.64–0.97). The odds of susceptibility in youth who used any OTP were more than twice that of youth who did not use any OTPs across all survey years (AOR: 2.60–2.71). The youth who perceived e-cigarettes cause “some” or “a lot” of harm had lower odds of being susceptible to e-cigarette use than youth who perceived e-cigarettes to cause no harm. School level was not associated with e-cigarette susceptibility across survey years.
Table 3.
Adjusted odds ratio of e-cigarette susceptibility among middle and high school students who are never users of e-cigarettes, National Youth Tobacco Survey, United States, 2014–2018.
| Adjusted odds ratio (95%CI) | |||||
|---|---|---|---|---|---|
| Year | 2014 | 2015 | 2016 | 2017 | 2018 |
| Sex | |||||
| Female | 1.18 (1.09, 1.27) | 1.29 (1.17, 1.43) | 1.14 (1.05, 1.25) | 1.23 (1.12, 1.36) | 1.21 (1.09,1.34) |
| Male (REF) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Race/ethnicity | |||||
| NH-black | 0.63 (0.55, 0.73) | 0.60 (0.52, 0.70) | 0.59 (0.50, 0.70) | 0.59 (0.50, 0.71) | 0.58 (0.48, 0.69) |
| NH-White | 0.67 (0.59, 0.76) | 0.65 (0.57, 0.75) | 0.68 (0.60, 0.78) | 0.80 (0.69, 0.92) | 0.88 (0.77, 1.00) |
| NH-other | 0.84 (0.73, 0.98) | 0.79 (0.64, 0.97) | 0.84 (0.68,1.04) | 0.82 (0.64, 1.05) | 0.86 (0.69, 1.08) |
| Hispanic (REF) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| School | |||||
| Middle | 1.03 (0.91, 1.17) | 0.93 (0.81, 1.06) | 0.97 (0.85, 1.10) | 0.99 (0.88, 1.12) | 0.98 (0.85, 1.12) |
| High (REF) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| OTP ever use | |||||
| Yes | 2.62 (2.38, 2.87) | 2.60 (2.17, 3.11) | 2.62 (2.25, 3.05) | 2.60 (2.17, 3.13) | 2.71 (2.31, 3.18) |
| No (REF) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| E-cigarette harm perception | |||||
| No harm (REF) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Little harm | 0.74 (0.62, 0.89) | 1.03 (0.86, 1.23) | 1.14 (0.93, 1.39) | 1.22 (0.93, 1.60) | 1.51 (1.24, 1.84) |
| Some harm | 0.32 (0.27, 0.38) | 0.43 (0.36, 0.52) | 0.52 (0.44, 0.63) | 0.55 (0.42, 0.71) | 0.60 (0.48, 0.74) |
| A lot of harm | 0.13 (0.13, 0.16) | 0.17 (0.14, 0.21) | 0.20 (0.17, 0.24) | 0.21 (0.15, 0.28) | 0.23 (0.18, 0.29) |
REF = reference, 95% CI = 95% confidence interval. Odds ratio adjusted for other covariates.
4. Discussion
With adolescent use of e-cigarettes increasing sharply in recent years (Cullen et al., 2018; Gentzke et al., 2019; Jamal et al., 2017), understanding antecedents and identifying subgroups more vulnerable to e-cigarette use are important to developing effective prevention efforts. E-cigarette susceptibility is an important indicator of future e-cigarette use among youth (Bold et al. 2017; Carey et al. 2018; Cole et al. 2019). The present study is the first to document trends in e-cigarette susceptibility among youth; susceptibility increased from 2014 to 2016, decreased in 2017, and rose again slightly in 2018. Similar trends were found for male, female, NH-White students, and middle and high school students. In addition, there was an increasing linear trend in e-cigarette susceptibility among youth who perceived e-cigarettes to be a little harmful, somewhat harmful, or a lot harmful. Among youth who perceive e-cigarettes to be not harmful, there was a decreasing linear trend in e-cigarette susceptibility. These results may be surprising as past research has found that youth who perceive e-cigarettes to be less harmful are more likely to use e-cigarettes (Amrock et al. 2014; Parker et al. 2018). However, it is possible that youth who perceive e-cigarettes to pose some harm are experiencing trend increases in susceptibility. Youth who perceive e-cigarettes to pose no harm are the most susceptible and may initiate e-cigarette use, which would lead to their removal from analyses due to their ineligibility to be susceptible after initial use. As result, this may lead to artificial decreases of associative measures of susceptibility among youth who perceive e-cigarettes to pose no harm.
Although we cannot compare e-cigarette susceptibility trends to e-cigarette use trends (Cullen et al. 2018) with cross-sectional data (Kelloway and Francis 2013), longitudinal studies have found that e-cigarette susceptibility predicts subsequent use at 6, 12, and 18 month follow-up (Bold et al. 2017; Carey et al. 2018; Pierce et al. 2018; Strong et al. 2015). Future research may consider longitudinal data that would further clarify the relationship between susceptibility and e-cigarette use and whether this relationship varies by demographic factors.
Findings indicated that Hispanic students and female students had higher odds of being susceptible compared to their counterparts. Prior research shows that racial/ethnic differences in tobacco product susceptibility may be driven by sex. One recent study found that Hispanic youth had higher levels of cigarette susceptibility compared to White youth over time, and that these differences became more pronounced for Hispanic females (Kamke et al. 2020). Other research analyzing data from the PATH Study Wave 1 found that non-Hispanic Black adolescents and Hispanic adolescents who had never used any tobacco product were more likely (versus non-Hispanic White youth) to be susceptible to future tobacco product use of any type (Trinidad et al. 2017). Additionally, the disparities in tobacco product susceptibility found for Hispanic youth may be attributed to disproportionate tobacco marketing targeting lower SES and minority neighborhoods (Lee et al. 2015; Ribisl et al. 2017)). Interestingly, e-cigarette susceptibility was not associated with school level, a proxy for age. Recent studies have found that being older, NH-White, and male was associated with reporting e-cigarette use (Gentzke et al., 2019). Therefore, the present study’s findings may indicate the changing composition of future e-cigarette users.
Youth e-cigarette use in the U.S. has reached epidemic proportions (U.S. Health and Human Services, 2019; U.S. Surgeon General 2016); thus, identifying susceptible subpopulations is useful for targeted prevention interventions. The measures used in the present study were adapted from those developed by Pierce et al. (1996) to identify youth susceptibility to cigarette smoking and have demonstrated high predictive validity (Cole et al. 2019). Several longitudinal studies have demonstrated that response patterns indicating susceptibility on two (Bold et al. 2017) or all three of the susceptibility items (Carey et al. 2018; Pierce et al. 2018; Pierce et al. 2017; U.S. Surgeon General 2016) are associated with e-cigarette ever use at follow-up. Additional factors have been associated with future e-cigarette use, suggesting that there may be domains in addition to those quantified in the modified Pierce measures that could improve the ability to identify youth susceptible to future e-cigarette use. For example, Camenga et al. (2018a, b) found that exposure to e-cigarette advertising, cigarette smoking, age, and White race at baseline are associated with e-cigarette ever use at six-month follow-up. In the future, it may be informative to examine such additional measures in concert with the Pierce validated susceptibility measures to determine the optimal approach to identify youth susceptible to e-cigarettes.
Recent studies have also focused on factors that are associated with susceptibility. In one longitudinal study, students were more likely to be susceptible to e-cigarettes if they had: family members who used e-cigarettes, poor school performance, and beliefs that using e-cigarettes are acceptable and common (Carey et al. 2019). A cross-sectional study analyzing data from the 2016–17 NYTS found that secondhand e-cigarette aerosol exposure is associated with youth e-cigarette and cigarette use susceptibility (Agaku et al. 2020). Youth data from the PATH study show that e-cigarette susceptibility is associated with psychological problems, rebelliousness, other substance use, and household exposure to secondhand smoke (Kwon et al. 2018) and that receptivity to tobacco advertising was associated with progression towards e-cigarette use (Pierce et al. 2017).
Despite considerable declines in American youth cigarette smoking, increasing e-cigarette use among youth has emerged as an urgent public health priority (U.S Food and Drug Administration 2018; U.S. Food and Drug Administration 2019; U.S. Surgeon General 2018). Recent data from NYTS indicate that unprecedented numbers of middle and high school youth reported current use of e-cigarettes in 2019 and that most exclusive e-cigarette users reported use of flavored e-cigarettes. To address the rise in flavored e-cigarette use among youth, several strategies have been implemented to prevent youth e-cigarette access. On January 2, 2020, FDA issued a policy prioritizing enforcement against unauthorized cartridge-based e-cigarette products in flavors that appeal to youth, including fruit and mint flavors (U.S Food and Drug Administration, 2020). FDA also expanded the tobacco prevention campaign, The Real Cost, to reach youth who have used e-cigarettes or are open to trying them and educate them about the risks (U.S Food and Drug Administration 2019). The U.S. Surgeon General has also called for aggressive action at the state and local levels including restricting young peoples’ access to e-cigarettes in retail settings, licensing retailers, implementing price policies, including e-cigarettes in smoke-free indoor air policies, and developing educational initiatives targeting young people to reduce youth e-cigarette use and prevent future addiction (U.S. Surgeon General 2018). Similar to the actions taken by the FDA, hundreds of American municipalities have enacted local ordinances aimed at preventing youth e-cigarette use (Barraza et al. 2017; Preventing Tobacco Addiction Foundation 2019) including several state and local governments that have temporarily banned e-cigarette flavors (Campaign for Tobacco Free Kids, 2020).
4.1. Limitations
This study has some limitations. First, data were collected from youth who attended either public or private schools and might not be generalizable to all middle and high school-aged youth, including those who have dropped out of school or are being home-schooled. However, in 2017, 97.8% of those 10 to 13 years of age, 98.2% of those 14 and 15 years old, and 92.9% of those 16 and 17 years of age were enrolled in a traditional school (National Center for Education Statistics, 2018). Second, the data were self-reported and may be influenced by response and social desirability biases.
Another potential limitation is that issues such as identifying subpopulations of youth susceptible to e-cigarette use is a novel area of research that has emerged only recently as a growing concern. The measures used in the present study were adapted from those developed by Pierce et al. (1996) to identify youth susceptibility to cigarette smoking and have been found to have high predictive validity (Bold et al. 2017; Carey et al. 2018; Cole et al. 2019; Pierce et al. 2017; U.S. Surgeon General 2016). There are also other factors such as exposure to e-cigarette advertising, cigarette smoking, demographic factors, normative beliefs about e-cigarettes, and school performance that are associated with future e-cigarette use (Agaku et al. 2020; Camenga et al., 2018a, b; Carey et al. 2019; Kwon et al. 2018) that were not included in this study.
5. Conclusion
This study examined differences in susceptibility to e-cigarette use over time and found that the percentage of youth susceptible to using e-cigarettes ranged from 32.9% in 2014 to 33.2% in 2018 with a high of 36.7% in 2016. E-cigarette susceptibility was associated with race/ethnicity, school level, OTP ever use, and e-cigarette harm perceptions. These findings build on the existing literature that is often limited to a snapshot in time and reinforce the need to reduce youth use of all tobacco products, including e-cigarettes. These findings may also be useful for monitoring shifts in use patterns and identifying vulnerable subgroups for targeted prevention efforts.
Footnotes
The survey mode for NYTS changed in 2019; therefore, data are assessed through 2018 to ensure comparability.
Declaration of Competing Interest
The corresponding author declares the following financial or other relationships with companies or organizations that are stakeholders on the topic of the manuscript.
References
- National Center for Education Statistics, 2018. Percentage of the Population 3 to 34 Years Old Enrolled in School, by Sex, Race/Ethnicity, and Age Group: Selected Years, 1980 through 2017. Digest of Education Statistics Retrieved from. https://nces.ed.gov/programs/digest/d18/tables/dt18_103.10.asp. [Google Scholar]
- National Institutes of Health, 2018. PATH Population Assessment of Tobacco and Health Retrieved from. https://pathstudyinfo.nih.gov/UI/HomeMobile.aspx.
- Campaign for Tobacco Free Kids, 2020. States and localities that have restricted the sale of flavored tobacco products Retrieved from. https://www.tobaccofreekids.org/assets/factsheets/0398.pdf.
- U.S Food and Drug Administration, 2018. FDA takes new steps to address epidemic of youth e-cigarette use, including a historic action against more than 1,300 retailers and 5 major manufacturers for their roles perpetuating youth access Retrieved from. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm620184.htm.
- U.S Food and Drug Administration, 2019. FDA launches new campaign: “The Real Cost” youth e-cigarette prevention campaign Retrieved from. https://www.fda.gov/tobacco-products/real-cost-campaign/fda-launches-new-campaign-real-cost-youth-e-cigarette-prevention-campaign.
- U.S Food and Drug Administration, 2020. FDA finalizes enforcement policy on unauthorized flavored cartridge-based e-cigarettes that appeal to children, including fruit and mint Retrieved from. https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children.
- Agaku IT, Perks SN, Odani S, Glover-Kudon R, 2020. Associations between public e-cigarette use and tobacco-related social norms among youth. Tob. Control 29 (3), 332–340. 10.1136/tobaccocontrol-2018-054728. [DOI] [PubMed] [Google Scholar]
- Ambrose BK, Rostron BL, Johnson SE, Portnoy DB, Apelberg BJ, Kaufman AR, Choiniere CJ, 2014. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am. J. Prev. Med 47 (2 Suppl 1), S53–S60. 10.1016/j.amepre.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amrock SM, Zakhar J, Zhou S, Weitzman M, 2014. Perception of E-cigarette harm and its correlation with use among U.S. adolescents. Nicotine Tob. Res 17 (3), 330–336. 10.1093/ntr/ntu156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barraza LF, Weidenaar KE, Cook LT, Logue AR, Halpern MT, 2017. Regulations and policies regarding e-cigarettes. Cancer 123 (16), 3007–3014. 10.1002/cncr.30725. [DOI] [PubMed] [Google Scholar]
- Bold K, Kong G, Cavallo D, Camenga D, Krishnan-Sarin S, 2017. E-cigarette susceptibility as a predictor of youth initiation of e-cigarettes. Nicotine Tob. Res 20 (1), 140–144. 10.1093/ntr/ntw393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camenga D, Gutierrez KM, Kong G, Cavallo D, Simon P, Krishnan-Sarin S, 2018a. E-cigarette advertising exposure in e-cigarette naive adolescents and subsequent e-cigarette use: a longitudinal cohort study (1873–6327 (electronic)). [DOI] [PMC free article] [PubMed]
- Camenga D, Gutierrez KM, Kong G, Cavallo D, Simon P, Krishnan-Sarin S, 2018b. E-cigarette advertising exposure in e-cigarette naïve adolescents and subsequent e-cigarette use: a longitudinal cohort study. Addict. Behav 81, 78–83. 10.1016/j.addbeh.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey FR, Wilkinson AV, Harrell MB, Cohn EA, Perry CL, 2018. Measurement and predictive value of susceptibility to cigarettes, e-cigarettes, cigars, and hookah among Texas adolescents. Addict. Behav. Rep 8, 95–101. 10.1016/j.abrep.2018.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey FR, Rogers SM, Cohn EA, Harrell MB, Wilkinson AV, & Perry CL (2019). Understanding susceptibility to e-cigarettes: a comprehensive model of risk factors that influence the transition from non-susceptible to susceptible among e-cigarette naïve adolescents. Addictive Behaviors, 91, 68–74. Doi: 10.1016/j.addbeh.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2018. National Youth Tobacco Survey (NYTS) Retrieved from. https://www.cdc.gov/tobacco/data_statistics/surveys/nyts/.
- Chaffee BW, Watkins SL, Glantz SA, 2018. Electronic cigarette use and progression from experimentation to established smoking. Pediatrics 141 (4). Retrieved from. http://pediatrics.aappublications.org/content/141/4/e20173594.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K, Forster JL, 2014. Beliefs and experimentation with electronic cigarettes: a prospective analysis among young adults. Am. J. Prev. Med 46 (2), 175–178. 10.1016/j.amepre.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole AG, Kennedy RD, Chaurasia A, Leatherdale ST, 2019. Exploring the predictive validity of the susceptibility to smoking construct for tobacco cigarettes, alternative tobacco products, and E-cigarettes. Nicotine Tob. Res 21 (3), 323–330. 10.1093/ntr/ntx265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team, 2018. R: A Language and Environment for Statistical Computing R Foundation for Satistical Computing, Vienna, Austria. Retrieved from. http://www.R-project.org/. [Google Scholar]
- Cullen A, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA, 2018. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students - United States 2011–2018. Morbity and Mortality Weekly Report 67, 1276–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Hao J, 2017. Electronic cigarette and marijuana use among youth in the United States. Addict. Behav 66, 48–54. 10.1016/j.addbeh.2016.11.005. [DOI] [PubMed] [Google Scholar]
- El-Toukhy S, Sabado M, Choi K, 2016. Trends in susceptibility to smoking by race and ethnicity. Pediatrics 138 (5), e20161254. 10.1542/peds.2016-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentzke A, Creamer M, Cullen KA, Ambrose BK, Willis G, Jamal A, King BA, 2019. Vital signs: tobacco product use among middle and high school students — United States, 2011–2018. Morbidity and Mortality Weekly Report (MMWR) 65 (6), 157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillis D, Edwards BPM, 2019. The utility of joinpoint regression for estimating population parameters given changes in population structure. Heliyon 5 (11), e02515. 10.1016/j.heliyon.2019.e02515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Health and Human Services, 2019. Trump Administration Combating Epidemic of Youth E-Cigarette Use with Plan to Clear Market of Unauthorized, Non-TobaccoFlavored E-Cigarette Products Retrieved from. https://www.hhs.gov/about/news/2019/09/11/trump-administration-combating-epidemic-youth-ecigarette-use-plan-clear-market.html.
- Jamal A, Gentzke A, Hu SS, Cullen KA, Apelberg BJ, Homa DM, King BA, 2017. Tobacco use among middle and high school studetns - United States 2011–2016. Morbity and Mortality Weekly Report 66 (23), 597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamke K, Sabado-Liwag M, Rodriquez EJ, Pérez-Stable EJ, El-Toukhy S, 2020. Adolescent smoking susceptibility: gender-stratified racial and ethnic differences, 1999–2018. Am. J. Prev. Med 58 (5), 666–674. 10.1016/j.amepre.2019.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelloway EK, Francis L, 2013. Longitudinal research and data analysis. In: Research Methods in Occupational Health Psychology: Measurement, Design, and Data Analysis Routledge/Taylor & Francis Group, New York, NY, US, pp. 374–394. [Google Scholar]
- Kwon E, Seo D-C, Lin H-C, Chen Z, 2018. Predictors of youth e-cigarette use susceptibility in a U.S. nationally representative sample. Addict. Behav 82, 79–85. 10.1016/j.addbeh.2018.02.026. [DOI] [PubMed] [Google Scholar]
- Lee JGL, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM, 2015. A systematic review of neighborhood disparities in point-of-Sale tobacco marketing. Am. J. Public Health 105 (9), e8–e18. 10.2105/AJPH.2015.302777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen R, Wilson K, Schaefer R, Klein J, Winickoff J, 2014. Susceptibility to electronic cigarette use among current nonsmokers. In: Paper Presented at the American Public Health Association Conference New Orleans, LA. [Google Scholar]
- Miech R, Patrick ME, Malley PM, Johnston LD, 2017. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob. Control 26 (e2), e106. Retrieved from. http://tobaccocontrol.bmj.com/content/26/e2/e106.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute, 2019, February 25. Joinpoint Trend Analysis Software Retrieved from. https://surveillance.cancer.gov/joinpoint/.
- Odani S, Armour BS, Agaku IT, 2018. Racial/ethnic disparities in tobacco product use among middle and high school students - United States, 2014–2017. Morbity and Mortality Weekly Report 67 (34), 952–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Villanti AC, Quisenberry AJ, Stanton CA, Doogan NJ, Redner R, Higgins ST, 2018. Tobacco Product Harm Perceptions and New Use. Pediatrics 142 (6), e20181505. 10.1542/peds.2018-1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perikleous EP, Steiropoulos P, Paraskakis E, Constantinidis TC, Nena E, 2018. E-cigarette use among adolescents: an overview of the literature and future perspectives. Front. Public Health 6, 86. 10.3389/fpubh.2018.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce J, Choi W, Gilpin E, Farkas A, Merritt R, 1996. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol 15 (5), 355–361. [DOI] [PubMed] [Google Scholar]
- Pierce J, Sargent J, White M, Borek N, Portnoy D, Green V, Messer K, 2017. Receptivity to tobacco advertising and susceptibility to tobacco products. Pediatrics 139 (6), e20163353. 10.1542/peds.2016-3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce J, Sargent J, Portnoy D, White M, Noble M, Kealey S, Hyland A, 2018. Association Between Receptivity to Tobacco Advertising and Progression to Tobacco Use in Youth and Young Adults in the PATH StudyReceptivity to Tobacco Advertising and Progression to Tobacco Use in Youth and Young AdultsReceptivity to Tobacco Advertising and Progression to Tobacco Use in Youth and Young Adults. JAMA Pediatrics 172 (5), 444–451. 10.1001/jamapediatrics.2017.5756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P, Fagan P, Kehl L, Herzog TA, 2015. Receptivity to e-cigarette marketing, harm perceptions, and e-cigarette use. Am. J. Health Behav 39 (1), 121–131. 10.5993/ajhb.39.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preventing Tobacco Addiction Foundation, 2019. Tobacco Twenty-one Retrieved from. https://tobacco21.org/e-cigarettes-teens/.
- Ribisl KM, D’Angelo H, Feld AL, Schleicher NC, Golden SD, Luke DA, Henriksen L, 2017. Disparities in tobacco marketing and product availability at the point of sale: results of a national study. Prev. Med 105, 381–388. 10.1016/j.ypmed.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saddleson ML, Kozlowski LT, Giovino GA, Hawk LW, Murphy JM, MacLean MG, Mahoney MC, 2015. Risky behaviors, e-cigarette use and susceptibility of use among college students. Drug and Alcohol Dependence 149, 25–30. 10.1016/j.drugalcdep.2015.01.001. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc, 2013. SAS® 9.4. SAS Institute Inc., Cary, NC. Retrieved from. https://www.sas.com/en_us/legal/editorial-guidelines.html. [Google Scholar]
- Sawdey MD, Day HR, Coleman B, Gardner LD, Johnson SE, Limpert J, Ambrose BK, 2019. Associations of risk factors of e-cigarette and cigarette use and susceptibility to use among baseline PATH study youth participants (2013–2014). Addictive Behaviors 91, 51–60. 10.1016/j.addbeh.2018.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong DR, Hartman SJ, Nodora J, Messer K, James L, White M, Pierce J, 2015. Predictive Validity of the Expanded Susceptibility to Smoke Index. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco 17 (7), 862–869. 10.1093/ntr/ntu254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Surgeon General, 2016. E-cigarette use among youth and young adults Retrieved from Rockville, MD. [Google Scholar]
- U.S. Surgeon General, 2018. Surgeon General’s advisory on e-cigarette use among youth Retrieved from. https://e-cigarettes.surgeongeneral.gov/documents/surgeon-generals-advisory-on-e-cigarette-use-among-youth-2018.pdf.
- Trinidad DR, Pierce JP, Sargent JD, White MM, Strong DR, Portnoy DB, Messer K, 2017. Susceptibility to tobacco product use among youth in wave 1 of the population Assessment of tobacco and health (PATH) study. Preventive Medicine 101, 8–14. 10.1016/j.ypmed.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma V, Betti G, 2011. Taylor linearization sampling errors and design effects for poverty measures and other complex statistics. J. Appl. Stat 38 (8), 1549–1576. 10.1080/02664763.2010.515674. [DOI] [Google Scholar]
- Wang TW, Gentzke AS, Creamer MR, Cullen KA, Holder-Hayes E, Sawdey MD, … Neff LJ (2019). Tobacco product use and associated factors among middle and high school students - United States, 2019. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C. : 2002), 68(12), 1–22. Doi: 10.15585/mmwr.ss6812a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ, 2017. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob. Control 26 (1), 34. Retrieved from. http://tobaccocontrol.bmj.com/content/26/1/34.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodruff RS, 1971. A simple method for approximating the variance of a complicated estimate. J. Am. Stat. Assoc 66 (334), 411–414. 10.1080/01621459.1971.10482279. [DOI] [Google Scholar]
- Yuan M, Cross SJ, Loughlin SE, Leslie FM, 2015. Nicotine and the adolescent brain. J. Physiol 593 (16), 3397–3412. 10.1113/JP270492. [DOI] [PMC free article] [PubMed] [Google Scholar]


